Abstract
Newcastle disease virus (NDV), the prototype member of the Avulavirus genus of the family Paramyxoviridae1, is a non-segmented, negative-sense, single-stranded, enveloped RNA virus (Figure 1) with potential applications as a vector for vaccination and treatment of human diseases. In-depth exploration of these applications has only become possible after the establishment of reverse genetics techniques to rescue recombinant viruses from plasmids encoding their complete genomes as cDNA2-5. Viral cDNA can be conveniently modified in vitro by using standard cloning procedures to alter the genotype of the virus and/or to include new transcriptional units. Rescue of such genetically modified viruses provides a valuable tool to understand factors affecting multiple stages of infection, as well as allows for the development and improvement of vectors for the expression and delivery of antigens for vaccination and therapy. Here we describe a protocol for the rescue of recombinant NDVs.
Keywords: Immunology, Issue 80, Paramyxoviridae, Vaccines, Oncolytic Virotherapy, Immunity, Innate, Newcastle disease virus (NDV), MVA-T7, reverse genetics techniques, plasmid transfection, recombinant virus, HA assay
Introduction
Newcastle disease virus (NDV), an avian paramyxovirus belonging to the Avulavirus genus1, is an economically relevant and thus widely researched and surveilled zoonotic agent, which can severely affect poultry farming all around the world. Although not a human pathogen, NDV has also been thoroughly studied beyond the veterinarian field both as a model paramyxovirus and due to its highly interesting, natural oncolytic properties6. Research on NDV greatly benefited from the development of reverse genetics techniques for single-stranded, non-segmented negative-sense RNA viruses, first described for rabies virus by Conzelmann and coleagues2. A variety of genetically modified NDVs, carrying foreign genes or modifications of their wild type genome have been widely studied ever since. Work with these recombinant viruses has been critical to characterize different virulence factors not only of NDV but also of other relevant human pathogens such as influenza A virus7 - or the emergent Nipah virus8. Furthermore, a number of different studies have explored the use of these techniques to improve the innate antitumoral activity of NDV6,9,10, mostly by enhancing the immunostimulatory properties of the virus. Other relevant area of research on recombinant NDVs has been the generation of vaccine candidates against other viral diseases such as influenza5,11,12, HIV13, measles14, SARS15, or that caused by the respiratory sincytial virus (RSV)16. Amongst the various noteworthy advantages provided by NDV are the lack of preexisting immunity in human populations, the stability of the foreign genetic inserts, a lack of recombinatory activity and overall a high safety profile combined with the aforementioned natural immunostimulatory properties17. It's also noteworthy the potential use of recombinant bivalent vaccines in poultry, protective against both NDV and highly pathogenic avian influenza viruses11,12. This may be an excellent way to decrease the chances of the latter spreading from wild to domesticated animals, thus also helping to prevent a possible inter-specific jump of the dreaded avian influenza to humans. Finally, reporter-expressing NDV have been used for the evaluation of innate immune responses as well as the identification of interferon antagonist encoded by multiple viruses18-27.
The rescue process of a recombinant, non-segmented, negative-stranded RNA virus basically consists on artificially forcing a viral replication cycle in a producing cell by transfecting cDNA encoding the minimal infective molecular machinery, known as ribonucleoprotein or RNP (Figure 2). The RNPs consist of the viral polymerase (P and L proteins), the nucleoprotein (NP) and the full-length antigenomic RNA of the virus. This RNA+ antigenome is the template required for the generation of the complementary RNA- genomes, which, also associated with the rest of the proteins of the viral RNP, recapitulates the same infectious complex that a natural virus would release on the cytoplasm of the cell upon infection (Figure 2A). From this step onwards, the viral cycle can proceed naturally and recombinant virions, encapsidating the modified genomes, will be generated (Figure 2B). Remarkably, transfection of the genomic cDNA instead of the antigenomic cDNA greatly impairs or completely abolishes rescue efficiency2,28-30. Even when antigenomic cDNA is transfected, the efficiency of the encapsidation of the recombinant RNA into RNPs in transfected cells is probably very low. Because of this, rescue protocols for NDV often include different steps for the amplification of the few viral particles released from the originally transfected cells by coculturing them with permissive cells and/or by the infection of embryonated eggs.
Prior to the rescue, the cDNA can be manipulated by standard cloning procedures in order to generate the desired modifications. While specific mutations of the different gene products and regulatory sequences of the virus can be straightforwardly achieved this way, many of the published work involving recombinant NDV has required the addition of a new transcriptional unit into the NDV genome. Like other members of the paramyxovirus family, the NDV genome encodes eight different proteins into six transcriptional units, which are differentially expressed depending on their location respect to the 3' end in a decreasing gradient critical for the viral life cycle1. Because of this, the location of the new transcriptional unit within the genome must be carefully chosen to achieve a balance between expression of the transgene and impairment of viral replication. Insertion between P and M genes has been used the most, though other sites have also been tested13,31.
Whatever the insert, the cloning into NDV cDNA needs to follow some rules to generate a rescuable construct: (i) any new gene to be included into the NDV genome has to be under control of the appropriate signals for the viral RNA-dependent-RNA polymerase. These sequences must be added upstream of the new open reading frame (ORF) so the polymerase can recognize the end of the previous gene (GE) and the beginning of the new transgene (GS), spaced by a single nucleotide intergenic sequence (IG). Addition of a valid Kozak (K) sequence to improve eukaryotic ribosomal translation is also recommended for better foreign protein expression32; (ii) efficient replication of NDV, as for most members of the Paramyxoviridae family, is dependent on the genome length being multiple of six33; therefore, any insertion into the NDV has to follow this "rule of six". If necessary, required additional nucleotides can be added downstream the new ORF; and (iii) the sequence of the transgene should be checked to find possible GE and GS like sequences which could impair rescue efficiency, transgene expression and/or virus viability. If present, these sequences must be removed by silent mutagenesis. The generation of recombinant full length cDNA following aforementioned rules is the first step in order to efficiently produce a genetically modified NDV as detailed here.
In the system all DNA constructs are under control of the T7 RNA polymerase promoter (Figure 3). This cytoplasmic polymerase is provided in trans by coinfection with a recombinant modified vaccinia Ankara virus (MVA-T7)34. Figure 3A show the pNDV-B1 plasmid, which encodes the full-length antigenomic cDNA5. Figure 3B shows pTM1 plasmids encoding NP, P and L ORFs. Plasmids pCITE-GFP, which encodes, under the T7 promoter, the Green Fluorescent Protein (GFP), and pCAGGs GFP18, which encodes the same ORF under the chicken beta actin promoter 35, are used as controls. In this protocol we show the procedure to rescue recombinant NDV from the cDNA of the lentogenic NDV strain Hitchner B15 (Figure 4).
Protocol
1. Preparation of Mammalian Cells (Figure 4A, Day 1)
Split HEp-2 or A549 cells the day before transfection in 6-well plates. Density of the cells should reach 80-90% confluence the following day. Usually, a confluent 100 mm dish can be split into 8 wells (around 1 x 106 cells per well). For each virus to be rescued, 2-4 different wells should be included, as well as 2 extra wells for the controls pCAGGs-GFP and pCITE-GFP18, aimed to monitor transfection and MVA-T7 infection efficiencies, respectively.
2. Infection of Mammalian Cells with the Recombinant Modified Vaccinia Ankara Virus Expressing the Bacteriophage T7 RNA Polymerase (MVA-T7) (Figure 4A, Day 2)
Warm up PBS 1x/BA/PS and media at 37 °C.
Wash cells, twice, with 1 ml of PBS 1x/BA/PS.
Infect the cultured mammalian cells with the MVA-T7 virus at a multiplicity of infection (moi) of 1 pfu/cell in a final volume of 200 μl in PBS/BA/PS for 1 hr at room temperature.
During viral infection incubation, prepare the transfection mix as described in 3.
3. Transfection of Mammalian Cells (Figure 4A, Day 2)
Preparation of Lipofectamine: Mix 1-2 μg of LPF2000 with 250 μl of OptiMEM per rescue attempt and incubate for 5 min at room temperature.
Preparation of DNA: Make a plasmid cocktail for each rescue in 50 μl of OptiMEM. Add 0.4 μg of pTM1-NP, 0.2 μg of pTM1-P, and 0.2 μg of pTM1-L per tube. Add 1 μg of the full-length cDNA clone of NDV to be rescued to each tube. Also prepare two control transfections, one with 2 μg of pCAGGs-GFP (to check transfection efficiency) and the other with 2 μg of pCITE-GFP (to check T7 polymerase driven expression by the MVA-T7).
After the LPF2000-OptiMEM solution has been preincubated for 5 min (step 3.1), add 250 μl of the solution to the DNA tubes (step 3.2) and incubate for 20-30 min at room temperature.
After incubation with MVA-T7, remove the virus inoculum by aspiration and replace with the DNA-LPF2000 transfection mix (step 3.3).
Add 1 ml of DMEM 10% FBS/PS to each dish.
Incubate the infected/transfected cells for 6-8 hr (or overnight) at 37 °C, 5% CO2 and then replace the transfection media with 1.5 ml of fresh DMEM 10% FBS/PS.
At 24 hr post-transfection, control wells can be observed under a fluorescence microscope to assess transfection efficiency (pCAGGs-GFP) and T7 polymerase activity (pCITE-GFP) (Figure 5A). Proceed with the co-culture of the infected/transfected cells with avian fibroblasts as described below.
4. Co-culture of Mammalian Cells with Avian Cells (Figure 4A, Day 3)
Usually, a confluent 100 mm tissue culture dish of chicken (CEFs) or duck (DEFs) embryo fibroblasts is used per two transfected wells. Be sure to prepare, in advance, enough 100 mm tissue culture dishes of avian cells per all rescue attempts. For efficient rescue of the virus, DMEM 10% FBS/PS media is supplemented with 5% of allantoic fluid and 30 mM MgCl2. At this point, 24 hr p.i., mammalian cells may start showing cytopathic effect (CPE) due to MVA-T7 infection, asevident in Figure 5A.
Warm up PBS 1x and media to 37 °C.
Wash mammalian cells, 2x, with 1 ml of PBS 1x.
Trypsinize mammalian cells with 0.2 ml of EDTA-trypsin until they detached. Resuspend the cells in 1 ml of DMEM 10% FBS/PS, 5% allantoic fluid, 30 mM MgCl2 and transfer to a 100 mm tissue culture dish. Add 3 ml of same media.
Wash avian cells, twice, with 4 ml of PBS 1x.
Trypsinize avian cells with 1 ml of EDTA-trypsin and incubate for 1-2 min at 37 °C until cells detach. Resuspend the cells adding 8 ml of DMEM 10% FBS/PS, 5% allantoic fluid, 30 mM MgCl2 and add 4 ml of the trypsinized cells to the mammalian cells in the co-cultured 100 mm tissue culture dish for a total volume of 8 ml (4 ml mammalian, 4 ml avian cells).
Gently shake by hand the co-cultured cells in the 100 mm dish in order to have a uniform distribution and then place them in the incubator at 37 °C for 3-4 days. The criteria for infecting eggs 3 or 4 days after co-culture of mammalian and avian cells depends on how much cytopathic effect (cell rounding, death, detachment from the surface, etc.) is observed in the MVA-T7 viral infection.
5. Infection of Chicken Embryonated Eggs (Figure 4A, Days 6-7)
After 3-4 days of co-culture of mammalian and avian cells, remove 1 ml of the tissue culture supernatant and add to an Eppendorf tube.
Centrifuge the tissue culture supernatant for 1 min at 12,000 rpm in a bench top centrifuge to remove cellular debris.
Candle the eggs using a light candling box to see the interface between the air sac and the allantoic cavity. Make a mark on the interface border avoiding blood vessel localization. Spray 70% ethanol over the eggs to establish sterile conditions. Gently make a hole in the eggshell on the marked spot and inoculate 500 μl of the supernatant using an insulin (1 ml) syringe, aiming the needle vertically and directly into the allantoic cavity. (Figure 4B).
Seal the nick in the eggshell with melted wax or paraffin.
Incubate the eggs for 2-3 days at 37 °C.
6. Harvest of Allantoic Fluid from Infected Chicken Embryonated Eggs (Figure 4A, Days 8-10)
Incubate the infected eggs for 2-4 hr or overnight at 4 °C in order to kill the chicken embryo and coagulate the blood.
Spray the eggs with 70% ethanol (to maintain sterile conditions).
Carefully tap the apical section of the egg, over the air cavity, with a spoon. Once the eggshell is cracked, remove the fragments with forceps and fully expose the allantoic membrane.
Expose the allantoic cavity by excising the allantoic membrane with forceps and scissors, avoiding damage to the blood vessels and the yolk.
Carefully push down the embryo with a spatula and collect the upflowing allantoic fluid (8-12 ml per egg) with a 10 ml pipette. Avoid damaging the yolk membrane. Transfer the allantoic fluid to a 15 ml centrifuge tube on ice (use one tube per egg).
Clarify the allantoic fluid by centrifuging for 5 min at 1,500 rpm. Transfer the supernatant to a fresh tube without disturbing the pellet.
Store samples at 4 °C for up to 1 week, until checking them for presence of NDV by hemagglutination assay.
7. Hemagglutination (HA) Assay
The presence of virus in the allantoic fluid from infected eggs can be determined macroscopically by their ability to hemagglutinate turkey red blood cells (RBC). In the case of NDV, approximately 106 plaque forming units (pfu) per ml are required to give a positive signal in the HA assay. HA assays are carried out in V-bottom 96-well plates. Negative (PBS 1x, uninfected allantoic fluid) as well as positive (allantoic fluid from any NDV virus) control samples should always be included in any HA assay to validate it. To perform an HA assay:
Pipette 50 μl of PBS 1x per well in a V-bottom 96-well plate.
Pipette 50 μl of the allantoic fluid samples into the wells on the first column of the plate. Perform 2-fold serial dilutions through the rest of the plate and discard the last, extra 50 μl from wells in the last column.
Dispense 50 μl of 0.5% turkey RBC in PBS 1x per well. Gently shake the plate by tapping.
Incubate the plate at 4 °C (or ice) for 30-45 min or until a clear pellet is formed in the negative control wells.
Representative Results
Rescue of NDV is a well-established procedure, routinely performed in the laboratories that have access to the complete cDNA of the virus. However, the intrinsic stochastic nature of the method makes it difficult to achieve 100% rescue efficiency. Monitoring the early steps of the process, specially the transfection efficiency and the infection with MVA-T7, helps identifying possible problems. Figure 5A shows standard transfection and transfection/infection efficiencies that are enough for a successful NDV rescue. After the rounds of amplification in avian-mammalian co-cultures and embryonated eggs, presence of rescued virus is detected by positive wells in the HA assay. NDV induces hemagglutination by linking erythrocytes and thus prevents their sedimentation in the bottom of the V-shaped well. Therefore, lack of HA activity can easily be distinguished by the formation of a red, round pellet of RBC (Figure 5B). Negative results in the HA assay can be due to an insufficient titer of virus in the allantoic fluid: a minimum titer of approximately 106 pfu/ml is required to have a positive HA result. Lower viral titers can still be detected by immunofluorescence assay (IFA) using specific anti NDV antibodies. A new passage on eggs for further amplification of the virus present in the first inoculated eggs is recommended in these cases.
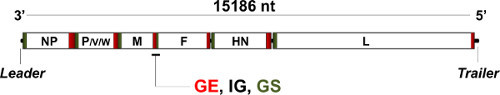 Figure 1. Genome organization of Newcastle disease virus (NDV). The non-segmented, single-stranded negative-sense RNA genome of NDV is 15,186 nucleotides (nt) long and encodes eight different polypeptides in six transcriptional units: NP, P, M, F, HN and L plus V and W proteins, originated after shifts in the reading frame of the P ORF during transcription. Noncoding, regulatory sequences flank the genome in its 3' (leader) and 5' (trailer) ends. Further noncoding gene end (GE), intergenic (IG) and gene start (GS) sequences regulate the viral polymerase activity in between the different ORFs. Expression levels of the different genes on the viral genome depend on their relative location respect to the 3' end (i.e. NP transcripts are the most abundant, L transcripts the least), effectively creating a gradient critical for the virus' life cycle1.
Figure 1. Genome organization of Newcastle disease virus (NDV). The non-segmented, single-stranded negative-sense RNA genome of NDV is 15,186 nucleotides (nt) long and encodes eight different polypeptides in six transcriptional units: NP, P, M, F, HN and L plus V and W proteins, originated after shifts in the reading frame of the P ORF during transcription. Noncoding, regulatory sequences flank the genome in its 3' (leader) and 5' (trailer) ends. Further noncoding gene end (GE), intergenic (IG) and gene start (GS) sequences regulate the viral polymerase activity in between the different ORFs. Expression levels of the different genes on the viral genome depend on their relative location respect to the 3' end (i.e. NP transcripts are the most abundant, L transcripts the least), effectively creating a gradient critical for the virus' life cycle1.
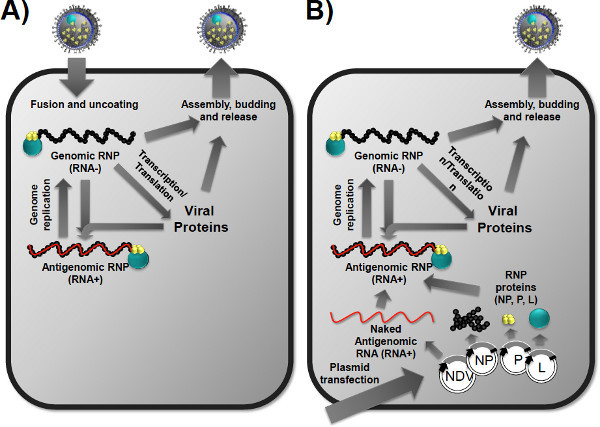 Figure 2. Basis of NDV rescue from cloned DNA. Schematic comparison between a natural (A) and the artificially-induced (B) cycle during the rescue process. (A) After attaching to the target cell, the virus releases its genomic content into the cytoplasm encapsidated in RNPs. The RNA polymerase transcribes the RNA- genome into the different mRNAs of the viral proteins and into a complementary, full length antigenomic RNA+ copy, which is template for the production of multiple copies of the original genome that will be incorporated into nascent virions. (B) During the rescue process, the components of the RNPs (NP, P and L proteins, as well as a full-length, usually modified antigenomic RNA) are provided by cDNA transfection. Upon reconstitution of the antigenomic RNPs in the cytoplasm of the transfected cell, they can produce the complementary, recombinant genomic RNPs and a whole cycle can then start anew, ending with the release of recombinant viruses.
Figure 2. Basis of NDV rescue from cloned DNA. Schematic comparison between a natural (A) and the artificially-induced (B) cycle during the rescue process. (A) After attaching to the target cell, the virus releases its genomic content into the cytoplasm encapsidated in RNPs. The RNA polymerase transcribes the RNA- genome into the different mRNAs of the viral proteins and into a complementary, full length antigenomic RNA+ copy, which is template for the production of multiple copies of the original genome that will be incorporated into nascent virions. (B) During the rescue process, the components of the RNPs (NP, P and L proteins, as well as a full-length, usually modified antigenomic RNA) are provided by cDNA transfection. Upon reconstitution of the antigenomic RNPs in the cytoplasm of the transfected cell, they can produce the complementary, recombinant genomic RNPs and a whole cycle can then start anew, ending with the release of recombinant viruses.
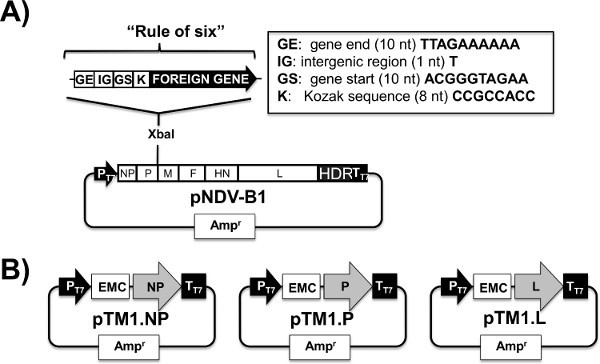 Figure 3. T7-driven expression plasmids for the generation of recombinant NDV. (A) Full length viral cDNA: The full length pNDV-B1 ampicillin resistance plasmid driving expression of the lentogenic NDV strain Hitchner B1 antigenome under the T7 promoter (PT7) and the T7 terminator sequence (TT7) containing the Hepatitis Delta Ribozyme (HDR) cleavage. The pNDV-B1 was originally designed to carry foreign inserts between P and M genes5. Insertion of a new gene (XbaI site) requires the addition of the regulatory gene end (GE), intergenic (IG) and gene start (GS) sequences to allow its functional recognition by the viral polymerase. Expression efficiency of the transgene can be improved with the addition of a Kozak (K) sequence upstream the start codon32. The whole cassette introduced into the NDV cDNA needs to have a total number of nucleotides divisible by six to follow the "rule of six"33 that drives efficient replication of most paramyxovius genomes. (B) Protein expression plasmids: Viral NP, P, and L ORFs, flanked by the T7 promoter (PT7), the UTR of the encephalomyocarditis virus (EMC) and the T7 terminator (TT7) sequences were cloned into the pTM1 backbone ampicillin resistance vector5,36.
Figure 3. T7-driven expression plasmids for the generation of recombinant NDV. (A) Full length viral cDNA: The full length pNDV-B1 ampicillin resistance plasmid driving expression of the lentogenic NDV strain Hitchner B1 antigenome under the T7 promoter (PT7) and the T7 terminator sequence (TT7) containing the Hepatitis Delta Ribozyme (HDR) cleavage. The pNDV-B1 was originally designed to carry foreign inserts between P and M genes5. Insertion of a new gene (XbaI site) requires the addition of the regulatory gene end (GE), intergenic (IG) and gene start (GS) sequences to allow its functional recognition by the viral polymerase. Expression efficiency of the transgene can be improved with the addition of a Kozak (K) sequence upstream the start codon32. The whole cassette introduced into the NDV cDNA needs to have a total number of nucleotides divisible by six to follow the "rule of six"33 that drives efficient replication of most paramyxovius genomes. (B) Protein expression plasmids: Viral NP, P, and L ORFs, flanked by the T7 promoter (PT7), the UTR of the encephalomyocarditis virus (EMC) and the T7 terminator (TT7) sequences were cloned into the pTM1 backbone ampicillin resistance vector5,36.
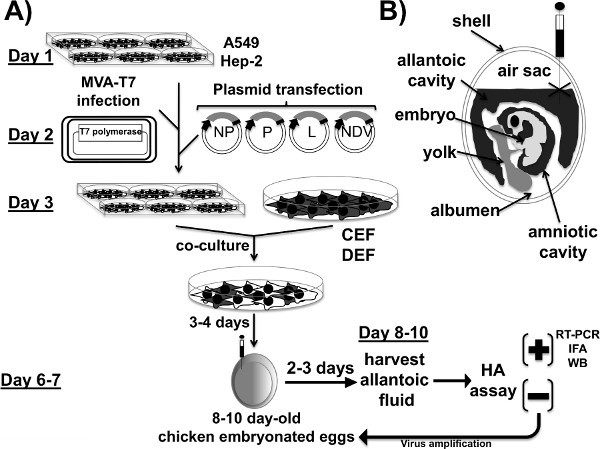 Figure 4. Plasmid-based reverse genetics techniques for the generation of recombinant Newcastle Disease Virus. (A) Viral rescue: A549 or HEp-2 cells are infected with the modified vaccinia virus Ankara expressing the bacteriophage T7 polymerase (MVA-T7). After viral infection, cells are co-transfected with the expression plasmid required for replication and transcription of the NDV viral genome (NP, P, and L), together with the full length NDV cDNA, under the T7 promoter. Twenty-four hours post-infection/transfection, mammalian cells are co-cultured with chicken or duck embryo fibroblasts (CEF and DEF, respectively). Three-to-four days after co-culture, 8-10 day-old chicken embryonated eggs are inoculated with the tissue culture supernatants of the co-culture cells for further amplification. Two-to-three days after incubation of the 8-10 day-old eggs at 37 °C, allantoic fluid from the eggs is harvested and analyzed for successful rescue of the recombinant virus by HA assay. Positive (+) rescue viruses are further characterized at genomic (RT-PCR) and protein (e.g. immunofluorescence assay (IFA) and western blot (WB) levels. Negative (-) HA results may be due to the lack of enough viruses to be detected by HA. Reinfection of fresh chicken embryonated eggs to amplify the virus is indicated. (B) Infection of chicken embryonated eggs: 8-10 chicken embryonated eggs are candled to mark the interface between the air sac and the allantoic cavity. With an insulin (1 ml) syringe, eggs are infected with the tissue culture supernatant inside the allantoic cavity, as indicated.
Figure 4. Plasmid-based reverse genetics techniques for the generation of recombinant Newcastle Disease Virus. (A) Viral rescue: A549 or HEp-2 cells are infected with the modified vaccinia virus Ankara expressing the bacteriophage T7 polymerase (MVA-T7). After viral infection, cells are co-transfected with the expression plasmid required for replication and transcription of the NDV viral genome (NP, P, and L), together with the full length NDV cDNA, under the T7 promoter. Twenty-four hours post-infection/transfection, mammalian cells are co-cultured with chicken or duck embryo fibroblasts (CEF and DEF, respectively). Three-to-four days after co-culture, 8-10 day-old chicken embryonated eggs are inoculated with the tissue culture supernatants of the co-culture cells for further amplification. Two-to-three days after incubation of the 8-10 day-old eggs at 37 °C, allantoic fluid from the eggs is harvested and analyzed for successful rescue of the recombinant virus by HA assay. Positive (+) rescue viruses are further characterized at genomic (RT-PCR) and protein (e.g. immunofluorescence assay (IFA) and western blot (WB) levels. Negative (-) HA results may be due to the lack of enough viruses to be detected by HA. Reinfection of fresh chicken embryonated eggs to amplify the virus is indicated. (B) Infection of chicken embryonated eggs: 8-10 chicken embryonated eggs are candled to mark the interface between the air sac and the allantoic cavity. With an insulin (1 ml) syringe, eggs are infected with the tissue culture supernatant inside the allantoic cavity, as indicated.
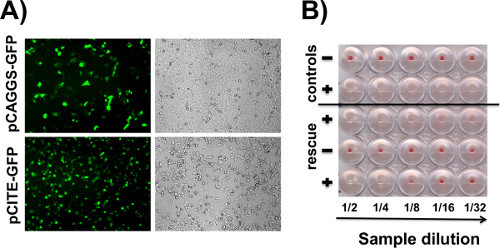 Figure 5. Representative results. (A) Transfection and MVA-T7 infection efficiencies: representative fluorescent (left) and bright (right) fields of A549 cells transfected with pCAGGS-GFP (top) or infected with MVA-T7 and transfected with pCITE-GFP (bottom) are illustrated. Constitutive GFP expression driven by pCAGGS is an indicator of transfection efficiency, whereas T7 promoter driven GFP expression by pCITE is a control for MVA-T7 infection and T7 polymerase activity. Cells were imaged at 24 hr post-transfection/post-infection (B) Hemagglutination assay (HA): Presence of viral particles in allantoic fluid induces hemagglutination, which is shown by a lack of pellet in the bottom of a V shaped well. Absence of virus allows the formation of a red pellet in the bottom of the well. Figure shows both the controls needed for any HA assay (negative, clean allantoic fluid; positive, an already characterized NDV sample), and the results of three unknown samples obtained after a rescue, with two positive (+) and one negative (-) result.
Figure 5. Representative results. (A) Transfection and MVA-T7 infection efficiencies: representative fluorescent (left) and bright (right) fields of A549 cells transfected with pCAGGS-GFP (top) or infected with MVA-T7 and transfected with pCITE-GFP (bottom) are illustrated. Constitutive GFP expression driven by pCAGGS is an indicator of transfection efficiency, whereas T7 promoter driven GFP expression by pCITE is a control for MVA-T7 infection and T7 polymerase activity. Cells were imaged at 24 hr post-transfection/post-infection (B) Hemagglutination assay (HA): Presence of viral particles in allantoic fluid induces hemagglutination, which is shown by a lack of pellet in the bottom of a V shaped well. Absence of virus allows the formation of a red pellet in the bottom of the well. Figure shows both the controls needed for any HA assay (negative, clean allantoic fluid; positive, an already characterized NDV sample), and the results of three unknown samples obtained after a rescue, with two positive (+) and one negative (-) result.
Discussion
Several factors are to be considered to achieve good results while rescuing NDV. First, the full-length cDNA construct to be used needs to be designed to allow the functional incorporation of the new transgenes/modifications into the NDV genome. This means, as stated above, that (i) appropriate gene end (GE), intergenic (IG) and gene start (GS) sequences are to be added if required; (ii) there are no putative GE or GS sequences into the foreign gene, and (iii) the full recombinant genome follows the "rule of six".
As for the rescue process, quality of plasmid preparations, the MVA-T7 stocks as well as proper maintenance of cells are critical. For most of the cases, standard maxiprep purification of the plasmid DNA is enough, although difficult cloning and rescue processes, due to the size or nature of the transgenes, may be improved by purifying DNA through CsCl density gradient centrifugation. Transfection efficiency using Lipofectamine is usually enough for a successful rescue, though other transfection methods such as nucleofection can also be used. In any case, the ratio of the different plasmids needs to be strictly maintained (0.4:0.2:0.2:1 for NP-P-L-pNDV, respectively). Due to the laborious and somehow stochastic nature of the rescue process, at least 2-4 different wells should be transfected per construct to be rescued, and different clones of the same construct should be assayed.
In the protocol that we have described here, we use MVA-T7 to provide in trans the T7 polymerase required for the expression of the viral cDNA constructs. While this is the standard procedure in our laboratory, it is not the only possible approach. For example, other groups have successfully rescued NDV and other non-segmented, negative strand RNA viruses by using cell lines constitutively expressing high levels of T7 polymerase4,37. The availability of a recombinant vector or cell line encoding T7 polymerase, as well as the specific performance of either approach in a given laboratory, should be considered when establishing anew the rescue system for NDV.
After determination of NDV presence in the allantoic fluid by HA, further studies are to be performed to fully characterize the newly rescued virus, such as RT-PCR followed by sequencing of the viral genome, IFA and Western-blotting (WB) to determine expression of the foreign gene (if applicable). Depending on the nature of the modifications that the recombinant viruses are carrying, other kind of biochemical and functional assays could also be needed.
The rescue of recombinant NDV from cDNA is an useful technique for multiple reasons. First and most obvious, this technique provides with the ability to analyze the biology of NDV, an economically relevant virus for the avian industry, by experimentally altering its genes and regulatory sequences. NDV is a paramyxovirus closely related to human pathogens like measles, mumps or respiratory syncytial viruses, as well as the emergent, highly pathogenic Hendra and nipah viruses; research on the basic life cycle of this family of viruses is important to understand their biology. Beyond basic research, recombinant NDVs have a great potential as vaccine and oncolytic vectos, combining the possibility of carrying foreing genes in their genomes with a well assessed biosafety profile. For all of these reasons, The NDV rescue protocol can be a valuable asset for many laboratories worldwide interested in virus research, vaccine development and cancer treatment.
Disclosures
Adolfo García-Sastre is an inventor of patents on recombinant Newcastle disease viruses that are owned by the Icahn School of Medicine at Mount Sinai.
Acknowledgments
Authors would like to thank past and present members in the laboratories of Drs. Peter Palese and Adolfo García-Sastre for the development of NDV reverse genetics techniques and for technical assistance. Research in Newcastle disease virus in AG-S laboratory is partially funded by NIAD grant R01AI088770 and by the Department of Homeland Security Science & Technology Center of Excellence for Emerging and Zoonotic Animal Diseases (CEEZAD, award number 2010-ST-061-AG001). Research in LM-S laboratory is funded by the NIH grants RO1 AI077719, R21NS075611-01, R03AI099681-01A1, the NIAID Centers of Excellence for Influenza Research and Surveillance (HHSN266200700008C), and The University of Rochester Center for Biodefense Immune Modeling (HHSN272201000055C).
References
- Lamb RA, Parks GD. In: Fields Virology. Howley PH, Knipe DM, editors. Lippincott Williams & Wilkins; 2007. pp. 1647–1689. [Google Scholar]
- Schnell MJ, Mebatsion T, Conzelmann KK. Infectious rabies viruses from cloned cDNA. EMBO J. 1994;13:4195–4203. doi: 10.1002/j.1460-2075.1994.tb06739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters BP, de Leeuw OS, Koch G, Gielkens AL. Rescue of Newcastle disease virus from cloned cDNA: evidence that cleavability of the fusion protein is a major determinant for virulence. J. Virol. 1999;73:5001–5009. doi: 10.1128/jvi.73.6.5001-5009.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer-Oberdorfer A, Mundt E, Mebatsion T, Buchholz UJ. Generation of recombinant lentogenic Newcastle disease virus from cDNA. J. Gen. Virol. 1999;80(Pt 11):2987–2995. doi: 10.1099/0022-1317-80-11-2987. [DOI] [PubMed] [Google Scholar]
- Nakaya T, et al. Recombinant Newcastle disease virus as a vaccine vector. J. Virol. 2001;75:11868–11873. doi: 10.1128/JVI.75.23.11868-11873.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamarin D, Palese P. Oncolytic Newcastle disease virus for cancer therapy: old challenges and new directions. Future Microbiol. 2012;7:347–367. doi: 10.2217/fmb.12.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park MS, Garcia-Sastre A, Cros JF, Basler CF. Newcastle disease virus V protein is a determinant of host range restriction. J. Virol. 2003;77:9522–9532. doi: 10.1128/JVI.77.17.9522-9532.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park MS, et al. Newcastle disease virus (NDV)-based assay demonstrates interferon-antagonist activity for the NDV V protein and the Nipah virus V, W, and C proteins. J. Virol. 2003;77:1501–1511. doi: 10.1128/JVI.77.2.1501-1511.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamarin D, et al. Enhancement of oncolytic properties of recombinant newcastle disease virus through antagonism of cellular innate immune responses. Mol. Ther. 2009;17:697–706. doi: 10.1038/mt.2008.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigil A, et al. Use of reverse genetics to enhance the oncolytic properties of Newcastle disease virus. Cancer Res. 2007;67:8285–8292. doi: 10.1158/0008-5472.CAN-07-1025. [DOI] [PubMed] [Google Scholar]
- Swayne DE, et al. Recombinant paramyxovirus type 1-avian influenza-H7 virus as a vaccine for protection of chickens against influenza and Newcastle disease. Avian Dis. 2003;47:1047–1050. doi: 10.1637/0005-2086-47.s3.1047. [DOI] [PubMed] [Google Scholar]
- Park MS, Steel J, Garcia-Sastre A, Swayne D, Palese P. Engineered viral vaccine constructs with dual specificity: avian influenza and Newcastle disease. Proc. Natl. Acad. Sci. U.S.A. 2006;103:8203–8208. doi: 10.1073/pnas.0602566103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnero E, et al. Optimization of human immunodeficiency virus gag expression by newcastle disease virus vectors for the induction of potent immune responses. J. Virol. 2009;83:584–597. doi: 10.1128/JVI.01443-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, et al. Induction of type I interferon secretion through recombinant Newcastle disease virus expressing measles virus hemagglutinin stimulates antibody secretion in the presence of maternal antibodies. J. Virol. 2011;85:200–207. doi: 10.1128/JVI.01624-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNapoli JM, et al. Newcastle disease virus, a host range-restricted virus, as a vaccine vector for intranasal immunization against emerging pathogens. Proc. Natl. Acad. Sci. U.S.A. 2007;104:9788–9793. doi: 10.1073/pnas.0703584104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Sobrido L, et al. Protection against respiratory syncytial virus by a recombinant Newcastle disease virus vector. J. Virol. 2006;80:1130–1139. doi: 10.1128/JVI.80.3.1130-1139.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukreyev A, Collins PL. Newcastle disease virus as a vaccine vector for humans. Curr. Opin. Mol. Ther. 2008;10:46–55. [PubMed] [Google Scholar]
- Martinez-Sobrido L, Zuniga EI, Rosario D, Garcia-Sastre A, de la Torre JC. Inhibition of the type I interferon response by the nucleoprotein of the prototypic arenavirus lymphocytic choriomeningitis virus. J. Virol. 2006;80:9192–9199. doi: 10.1128/JVI.00555-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings S, Martinez-Sobrido L, Garcia-Sastre A, Weber F, Kochs G. Thogoto virus ML protein suppresses IRF3 function. Virology. 2005;331:63–72. doi: 10.1016/j.virol.2004.10.015. [DOI] [PubMed] [Google Scholar]
- Kochs G, Garcia-Sastre A, Martinez-Sobrido L. Multiple anti-interferon actions of the influenza A virus NS1 protein. J. Virol. 2007;81:7011–7021. doi: 10.1128/JVI.02581-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munoz-Jordan JL, et al. Inhibition of alpha/beta interferon signaling by the NS4B protein of flaviviruses. J. Virol. 2005;79:8004–8013. doi: 10.1128/JVI.79.13.8004-8013.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardenas WB, et al. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J. Virol. 2006;80:5168–5178. doi: 10.1128/JVI.02199-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mibayashi M, et al. Inhibition of retinoic acid-inducible gene I-mediated induction of beta interferon by the NS1 protein of influenza A virus. J. Virol. 2007;81:514–524. doi: 10.1128/JVI.01265-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopecky-Bromberg SA, Martinez-Sobrido L, Frieman M, Baric RA, Palese P. Severe acute respiratory syndrome coronavirus open reading frame (ORF) 3b, ORF 6, and nucleocapsid proteins function as interferon antagonists. J. Virol. 2007;81:548–557. doi: 10.1128/JVI.01782-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose KM, Elliott R, Martinez-Sobrido L, Garcia-Sastre A, Weiss SR. Murine coronavirus delays expression of a subset of interferon-stimulated genes. J. Virol. 2010;84:5656–5669. doi: 10.1128/JVI.00211-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth-Cross JK, Martinez-Sobrido L, Scott EP, Garcia-Sastre A, Weiss SR. Inhibition of the alpha/beta interferon response by mouse hepatitis virus at multiple levels. J. Virol. 2007;81:7189–7199. doi: 10.1128/JVI.00013-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson I, et al. Crimean-Congo hemorrhagic fever virus delays activation of the innate immune response. J. Med. Virol. 2008;80:1397–1404. doi: 10.1002/jmv.21222. [DOI] [PubMed] [Google Scholar]
- Lawson ND, Stillman EA, Whitt MA, Rose JK. Recombinant vesicular stomatitis viruses from DNA. Proc. Natl. Acad. Sci. U.S.A. 1995;92:4477–4481. doi: 10.1073/pnas.92.10.4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato A, et al. Initiation of Sendai virus multiplication from transfected cDNA or RNA with negative or positive sense. Genes Cells. 1996;1:569–579. doi: 10.1046/j.1365-2443.1996.d01-261.x. [DOI] [PubMed] [Google Scholar]
- Durbin AP, et al. Recovery of infectious human parainfluenza virus type 3 from cDNA. Virology. 1997;235:323–332. doi: 10.1006/viro.1997.8697. [DOI] [PubMed] [Google Scholar]
- Zhao H, Peeters BP. Recombinant Newcastle disease virus as a viral vector: effect of genomic location of foreign gene on gene expression and virus replication. J. Gen. Virol. 2003;84:781–788. doi: 10.1099/vir.0.18884-0. [DOI] [PubMed] [Google Scholar]
- Kozak M. At least six nucleotides preceding the AUG initiator codon enhance translation in mammalian cells. J. Mol. Biol. 1987;196:947–950. doi: 10.1016/0022-2836(87)90418-9. [DOI] [PubMed] [Google Scholar]
- Calain P, Roux L. The rule of six, a basic feature for efficient replication of Sendai virus defective interfering RNA. J. Virol. 1993;67:4822–4830. doi: 10.1128/jvi.67.8.4822-4830.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt LS, Moss B, Rozenblatt S. Replication-deficient vaccinia virus encoding bacteriophage T7 RNA polymerase for transient gene expression in mammalian cells. Virology. 1995;210:202–205. doi: 10.1006/viro.1995.1332. [DOI] [PubMed] [Google Scholar]
- Niwa H, Yamamura K, Miyazaki J. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene. 1991;108:193–199. doi: 10.1016/0378-1119(91)90434-d. [DOI] [PubMed] [Google Scholar]
- Moss B, Elroy-Stein O, Mizukami T, Alexander WA. Product review. New mammalian expression vectors. Nature. 1990;348:91–92. doi: 10.1038/348091a0. [DOI] [PubMed] [Google Scholar]
- Conzelmann KK. Reverse genetics of mononegavirales. Curr. Top. Microbiol. Immunol. 2004;283:1–41. doi: 10.1007/978-3-662-06099-5_1. [DOI] [PubMed] [Google Scholar]


