Single-port laparoscopic parastomal hernia repair with a modified Sugarbaker technique is suggested to be feasible and safe and provides an alternative to multi-port surgery.
Keywords: Parastomal hernia, Single-incision laparoscopic surgery (SILS), Modified Sugarbaker technique
Abstract
Introduction:
Laparoscopic parastomal hernia repair with modified Sugarbaker technique has become increasingly the operation of choice because of its low recurrence rates. This study aimed to assess feasibility, safety, and efficiency of performing the same operation with single-incision laparoscopic surgery.
Materials and Methods:
All patients referred from March 2010 to February 2013 were considered for single-port laparoscopic repair with modified Sugarbaker technique. A SILS port (Covidien, Norwalk, Connecticut, USA) was used together with conventional straight dissecting instruments and a 5.5- mm/52-cm/30° laparoscope. Important technical aspects include modified dissection techniques, namely, “inline” and “chopsticks” to overcome loss of triangulation, insertion of a urinary catheter into an ostomy for ostomy limb identification, safe adhesiolysis by avoiding electocautery, saline -jet dissection to demarcate tissue planes, dissection of an entire laparotomy scar to expose incidental incisional hernias, adequate mobilization of an ostomy limb for lateralization, and wide overlapping of defect with antiadhesive mesh.
Results:
Of 6 patients, 5 underwent single-port laparoscopic repair, and 1 (whose body mass index [BMI] of 39.4 kg/m2 did not permit SILS port placement) underwent multiport repair. Mean defect size was 10 cm, and mean mesh size was 660 cm2 with 4 patients having incidental incisional hernias repaired by the same mesh. Mean operation time was 270 minutes, and mean hospital stay was 4 days. Appliance malfunction ceased immediately, and pain associated with parastomal hernia disappeared. There was no recurrence with a follow-up of 2 to 36 months.
Conclusion:
Compared with multiport repair, single-port laparoscopic parastomal repair with modified Sugarbaker technique is safe and efficient, and it may eventually become the standard of care.
INTRODUCTION
Parastomal hernias have been shown to occur in up to 48% of patients with a colostomy or 36% for patients with an ileostomy, with the rate rising the longer the follow-up.1,2 This is not surprising given the fact that the stoma is essentially a hernia (Figure 1). The best treatment for a parastomal hernia is, of course, reversal of the ostomy. However, for patients with a terminal ostomy, this reversal is not an option, and surgical options up to now have proven disappointing. For this reason, the indications for repair have been narrow.
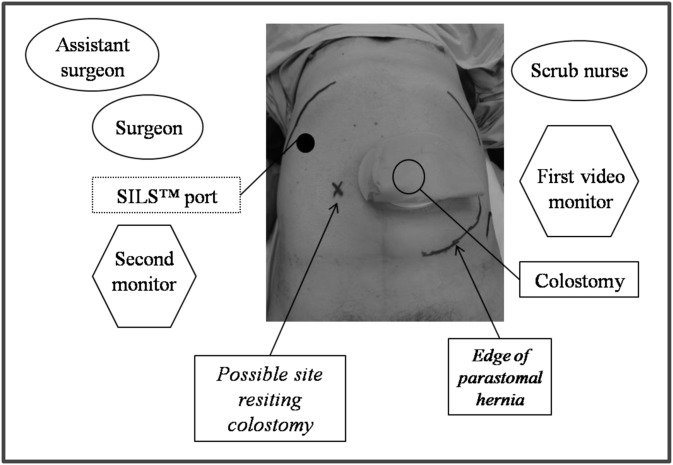
Figure 1.

Typical patient with a large parastomal hernia after an anterior resection complicated by an anastomotic leak resulting in a Hartman's procedure 5 years ago, with insets showing computed tomography scans in coronal section (left) and sagittal section (right).
Indications for the repair include incarceration causing pain, obstruction, bleeding, and stoma appliance malfunction. The latter can be extremely distressing to some patients, have negative psychological effects, and destroy the patient's relationships. Until now, surgical options have been limited, in addition to having significant morbidity and high recurrence rates. Because most parastomal hernias are still being repaired via a laparotomy incision, this type of repair alone implies a lifetime risk of an incisional hernia formation of up to 30%. Basically, treatment options include resiting the ostomy, which has a recurrence rate of up to 76%; however, there is an added risk of an incisional hernia at the ostomy site and onlay mesh repair with recurrence rates up to 70%.3,4 Open techniques involving placement of the mesh intraperitoneally with a hole for the stoma suffer from an intrinsic fault that the hole will allow herniation sooner or later, especially given that all meshes will shrink to some extent with time, further enlarging the hole and thus encouraging herniation.5,6
In 1980, Sugarbaker7 described a technique for parastomal hernia repair via a laparotomy in which a nonslit polypropylene mesh is placed intraperitoneally over the hernia with lateralization of the bowel. He reported a series of 7 patients with no recurrence with a follow-up at 4 years. Parallel with recent advances in laparoscopic ventral hernia repair, laparoscopic parastomal hernia repair with a modified Sugarbaker technique compared with the “keyhole” technique has offered these patients real hope of a permanent solution.9,10 Laparoscopic repair of a parastomal hernia with a modified Sugarbaker technique is the laparoscopic repair of the stomal hernia with a nonslit mesh covering the hernia defect with at least a 5-cm overlap; with lateralization of the colon/ileum going into the stoma, that treatment has been shown to have the lowest rates of recurrence.11,12
In an attempt to further reduce parietal trauma, single-incision laparoscopic surgery (SILS) has become increasingly popular in many surgical disciplines, including herniology, although conclusive evidence of its superiority over conventional multiport surgery still awaits prospective randomized controlled studies. Our unit began to perform single-incision laparoscopic repair routinely for virtually all inguinal and ventral hernias since December 2009. We aimed to evaluate the feasibility, safety, and success with single-incision laparoscopic parastomal hernia repair using the modified Sugarbaker technique. The Independent Review Board of Holroyd Private Hospital approved this study for the purpose of data collection and follow-up of patients.
MATERIALS AND METHODS
All referred patients with parastomal hernias from March 2010 to February 2013 underwent single-incision laparoscopic repair. Preoperatively all patients were bowel-prepped as for colonoscopy or colon resection. A single dose of cefazolin and metronidazole was given during induction of anesthesia. Nasogastric intubation and urinary catheterization (for nonurostomy patients) were standard intraoperative procedures. Additionally, a 16-F urinary catheter was placed inside the ostomy, and water (5 mL for urostomy and 10 mL for colostomy) was injected into the balloon to ensure that it could be tugged gently without dislodging it (Figure 2). This procedure assisted with intraoperative identification of the ostomy limb as it exited the skin.
Figure 2.
Position of the SILS port (Covidien, Norwalk, Connecticut, USA), surgeons, scrub nurse, and equipment for laparoscopic repair of a parastomal hernia with modified Sugarbaker technique of a left-sided ostomy; insert (of another patient) showing insertion of a urinary catheter to assist with identification of the ostomy limb during laparoscopy.
Patients were placed supine with both arms tucked in along the sides to allow monitors to be placed close to the patient. Because of the possibility of extensive adhesions and the lateral nature of mesh placement, the patients were restrained at the chest and pelvis so that the operating table could be tilted. All patients were always preoperatively marked on the opposite site of the abdomen by a stoma nurse in case the stoma had to be resited. The patients were prepped widely with iodine, dried, draped, and covered with iodine-impregnated plastic drape. This is the standard preparation for all our patients undergoing laparoscopic ventral hernia repair.
The positioning of the surgeon, assistant, scrub nurse, and video equipment for a left-sided stoma is shown in Figure 2. A SILS port (Covidien, Norwalk, Connecticut, USA) was inserted in the upper outer quadrant, opposite to the ostomy, in the anterior axillary line, just inferior to the ninth rib, with an open technique under direct vision with a muscle-splitting incision. Initially, one 10-mm trocar and two 5-mm trocars were placed with a 10-mm/30° videoscope introduced anteriorly. This process allowed clear visualization and inspection of abdominal contents, in particular, where the adhesiolysis needed to be performed. During the dissection, the 10-mm trocar was replaced by a 5-mm trocar for insertion of a 5.5-mm laparoscope because this decreased the clashing of dissecting instruments and increased maneuverability. In addition, the use of dissecting instruments of different lengths further minimized clashing of the handles (Figure 3).
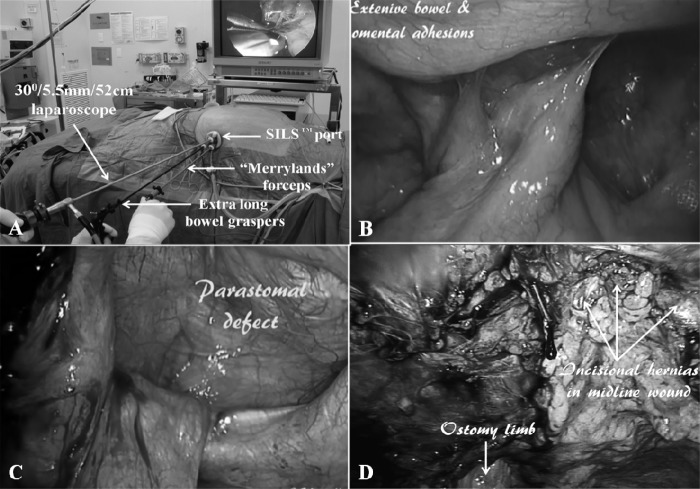
Figure 3.
A, SILS port (Covidien, Norwalk, Connecticut, USA) with an extralong laparoscope that keeps the side arm away from the handles of straight dissecting instruments of different lengths to overcome clashing of the handles. B, Extensive omental and small bowel adhesions. C, Parastomal defect with ileal conduit. D, Three incidental incisional hernias in the midline wound.
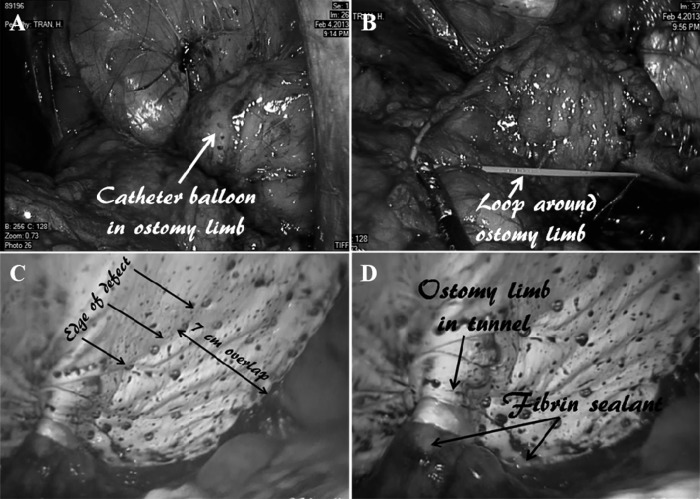
The most difficult part of any laparoscopic parastomal/ventral hernia repair is the safe division of adhesions, and extreme care must taken to avoid electrocautery. Liberal use of sharp dissection under direct vision, clipping of bleeding points, as well as the use of saline-jet dissection, which helps with demarcating tissue planes when bowel adhesions are encountered, must be included in this part of the procedure. For SILS, modified dissection techniques, namely, “inline” and “chopstix,” were used to overcome the relative lack of triangulation. Because of the nature of previous major surgery in the formation of the ostomy, dense adhesions were to be expected; hence meticulous dissection with division of adhesions strand by strand and in millimeter increments played in favor of SILS owing to its relative lack of triangulation. According to our routine practice in laparoscopic ventral hernia repairs, if the adhesions were deemed too dense, we would not hesitate to perform a mini-laparotomy to safely divide the adhesions, and then the laparotomy wound would be closed before recommencing the laparoscopic hernia repair. The entire midline laparotomy wound was dissected free to allow identification of incidental incisional hernias (Figure 3) because these can be covered with the same mesh, which must have a margin of at least 5 cm larger than the defect. The content of the hernial sac was reduced, and the ostomy limb and its mesentery must be dissected free enough for lateralization without a kink or tension as the ostomy limb entered into the tunnel. The catheter balloon helped with identification of the ostomy limb as it exited the skin as it can be tugged externally (Figure 4). Another useful maneuver was to place a temporary Vessiloop (Getz Bros, Chicago, Illinois, USA) around the most inferior aspect of the ostomy limb as it entered into the tunnel, with the loop pulled outside the skin with suture passer (Figure 4). This helped to ensure sufficient laxity of the lateralized limb and to assist with mesh placement (see below).
Figure 4.
A, Balloon of urinary catheter in ostomy limb for ease of identification. B, Vessiloop (Getz Bros, Chicago, Illinois, USA) around ostomy limb to aid its lateralization. C, Extensive overlapping of the parastomal hernia defect with mesh. D, ostomy limb in tunnel under mesh and fibrin sealant sprayed along mesh–ostomy interface, periphery of mesh, and staples.
Sizing of the mesh to be used is an inexact science and is helped with the use of a spinal needle, and the abdomen deflates to 4 mm Hg to minimize the chance that too large a mesh may be used. As with laparoscopic ventral hernia repair, only microporous or coated meshes should be used. We used a microporous ePTFE mesh (Gore-Tex Dualmesh Plus, WL Gore, Flagstaff, Arizona, USA) in 5 patients, and C-QUR mesh (Atrium Medical Corporation, Hudson, New Hampshire, USA) was used in 1 patient. Orientation marks were placed on the medial and superior aspects of the mesh. Most parastomal hernias that caused symptoms were large; the mesh that was used was correspondingly large. Placement of the mesh into the peritoneal cavity usually meant either temporary removal of the SILS port (Covidien) when the mesh could be inserted under direct vision with a pair of Rampleys sponge forceps and the SILS port would then be reintroduced, or placement of a 15-mm port into the SILS port after having partially withdrawn one 5-mm trocar to increase the space within the SILS port. When the latter method was used, a 5.5-mm laparoscope was placed in the remaining 5-mm port for direct visualization of mesh entry into the peritoneal cavity. Transfascial O PDS sutures (Ethicon, Inc, Radnor, Pennsylvania, USA) were placed well away from the stoma medially, superiorly, and inferiorly. As with laparoscopic ventral hernia repair, a “double-crown” technique was used. Unlike laparoscopic ventral hernia repair procedures in which the outer crown was placed first, in laparoscopic parastomal hernia repair, the inner crown was placed first. Unlike laparoscopic ventral hernia repair, where there is no bowel anterior to the mesh and the mesh can be stapled without negative effects, extreme care must be taken with every staple (Protack, Autosutures, Tyco Health Care Group, Norwalk, Connecticut, USA) that was placed on the inner “crown” to avoid accidental stapling into the ostomy limb. To aid the handling of a potentially large piece of mesh, usually at least a 20- to 30-cm piece of mesh, the mesh was rolled, with the smooth/coated peritoneal side inward, and temporary sutures are placed at 5-cm intervals. This process allowed the mesh to be flipped upward more easily so that the bowel could clearly be seen before a staple was placed. The inner crown was done sequentially on both sides, placing the bowel in the tunnel, and the temporary sutures keeping the mesh rolled up were cut to allow further unrolling of the mesh. This process was repeated until the bowel had been adequately lateralized (Figure 4). The outer crown was then completed, and additional transfascial sutures were placed. Herniation of bowel loops into the tunnel and adhesions to the periphery of the mesh and staples could be minimized by application of 4 mL of fibrin sealant (Tisseel Duo, Baxter AG, Vienna, Austria), which was sprayed copiously along the mesh–ostomy interface and sparsely along the periphery of the mesh and the staple line (Figure 4). The upper quadrant wound was closed in layers with No. O PDS sutures (Ethicon) and dissolvable sutures subcutaneously and subcuticularly.
RESULTS
There were 6 patients between March 2010 and February 2013: 2 with paracolostomal hernias and 4 with paraurostomal hernias (1 patient had had two previous open repairs). Of the latter patients, 1 had originally had a Hartman's procedure, cystectomy, and formation of ileal conduit due to colon cancer invading the bladder. The colostomy was subsequently closed, but the patient also developed an incisional hernia at this site. This hernia was repaired as an open procedure, but it soon recurred. The mean diameter of the defects was 10 cm (range 6–15 cm), and the mean mesh size was 660 cm2 (range 520–780 cm2). Half of the patients also had incidental midline incisional hernias that were repaired with the same mesh. The mean operation time was 270 minutes (range 210–360 minutes). However, the mean time to complete the division of adhesions and free the ostomy limb for lateralization was 180 minutes (range 120–210 minutes). The mean length of hospital stay was 4 days (range 1–9 days); 2 of the 6 patients stayed in hospital only overnight.
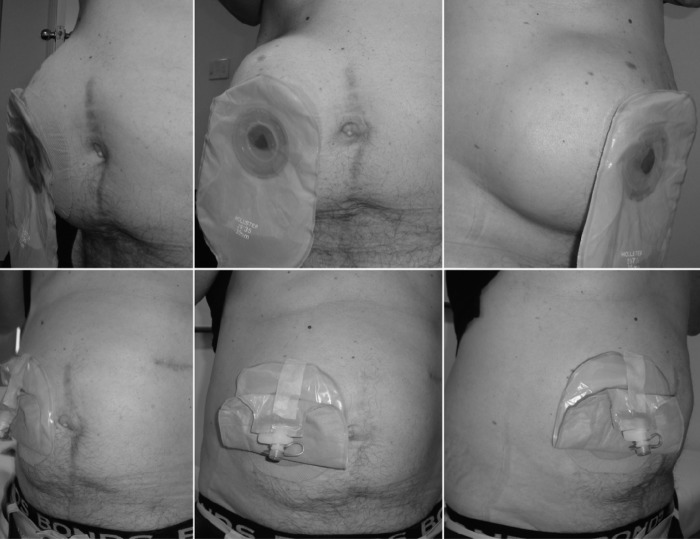
In the 3 patients with paracolostomal hernias, stoma-appliance malfunctioning resulting in fecal soiling stopped immediately. The pain related to the bulge had also disappeared, and the bulge had almost disappeared in all patients (Figure 5), and the ostomy diameter decreased from a mean of 45 mm (range 40–50 mm) preoperatively to 35 mm (range 30–40 mm) postoperatively. There was no evidence of a recurrence with a mean follow-up of 12 months (range 1–36 months). There was no morbidity or mortality.
Figure 5.
Preoperative appearance of patient with parastomal hernia (top photos) compared with appearance 6 months postoperatively (bottom photos) after single-incision laparoscopic repair with modified Sugarbaker technique.
DISCUSSION
The natural progression of hernias—including parastomal hernias—is one of progressive enlargement with time. Parastomal hernias can cause typical problems, including incarceration, obstruction, and a cosmetically unpleasant bulge. However, as the parastomal hernias enlarge during the day during periods of mobility, the ostomy appliance when applied during this period tends to become dislodged at nighttime when some or all of the parastomal hernia contents reduce. This circumstance causes highly unpleasant fecal/urinary soiling in bed, which can lead to psychological distress and relationship problems. This aspect of parastomal hernia complications is often underappreciated. Until now, the treatment options and results have been extremely limited and poor. Consequently, although ventral/incisional hernias are being repaired routinely to prevent complications, the laparoscopic repair has revolutionized repair practices by significantly reducing complications and improving success rates to >95%.13,14 The poor results of conventional surgical options, including resiting and open underlay or onlay mesh repair with a slit technique, mean that most surgeons would contemplate parastomal hernia repair only for significant symptoms as mentioned above. Guzman-Valdivia et al15 reported a series of an anterior onlay mesh repair in 25 patients with parastomal hernias with a recurrence of 8.8% with a follow-up period of just 12 months, surgical wound infection of 8%, and seroma formation of 8%. Safadi16 reported a series of 9 patients undergoing laparoscopic repair with the “keyhole” technique. He reported an operation time of 243 minutes (range 135–360 minutes), an average range of hospital stay of 4.7 days (range 2–7 days), morbidity of 33.3%, recurrence of 44.4%, and a prolapsed stoma in 1 patient; all of these failures occurred within 6 months of the operation.
In 1980, Sugarbaker7 first reported his series of 7 patients; his technique remained unused for >20 years, until the advent of laparoscopic hernia repair. The laparoscopic repair of parastomal hernias using the modified Sugarbaker technique with a nonslit mesh and lateralization of the bowel has shown great promise. Stelzner et al8 reported a recurrence rate of 15% with a 3.5-year follow-up using a modified Sugarbaker technique. Craft et al17 reported their study of a series of 21 patients treated by this method and reported a recurrence of just 5%, which parallels the best results obtainable for laparoscopic ventral/incisional hernia repair.12 A recent multi-institutional series (Mancini et al11) involving 5 highly experienced surgeons in laparoscopic ventral hernia repair over a period of 5 years with 25 patients showed a recurrence in just 1 patient (4%) with a follow-up of 19 months (range 2–38 months). There was, however, one death and the morbidity was 23%, with one mesh infection requiring removal. Such results have been replicated by Le Blanc et al18 and Hansson et al.12 The latter authors have also shown that the slit mesh repair resulted in significant higher recurrence rates compared with the nonslit mesh repair.
Our experience with 6 patients over a 3-year period represents a significant workload of parastomal hernias, given that most highly experienced laparoscopic hernia surgeons would perform only one to two parastomal hernia repairs per year.19 Despite the fact that SILS is still in its relative infancy, we have demonstrated operation times similar to those involving conventional multiport nonslit mesh repair. Most of the operation time was in fact spent on the safe division of adhesions, given that a previous major surgery was required to perform the ostomy. The relative loss of triangulation was overcome easily by modified dissection techniques, the use of a smaller and longer laparoscope, as well as the use of dissecting instruments with different lengths. Sharp dissection with avoidance of electocautery and use of a saline jet allowed safe division of adhesions without the need to perform a laparotomy. Identification of the ostomy limb was facilitated by the insertion of a urinary catheter into the ostomy, and the use of a temporary sling across the ostomy limb, together with sequential unrolling of the mesh, allowed safe mesh fixation. These important techniques allowed us to achieve success that was similar to that of multiport surgery, with no recurrence to date and with no morbidity or mortality.
An important advantage of SILS is that the dissecting instruments are inserted “in-line” with the laparoscope with little fear of accidental damage to bowel loops as the laparoscope is merely pulled slightly out, and then it follows the instruments in. In contrast, safe insertion of dissecting instruments in multiport surgery requires direct visualization every time, especially when the patient is tilted over to the port side, and that can be time-consuming.
CONCLUSION
Single-incision laparoscopic repair of parastomal hernia using the modified Sugarbaker technique is safe and efficient. In addition, it represents a natural progression and extension of the increasingly popular technique of SILS. This represents the next level of technical innovation in laparoscopic surgery in minimizing parietal trauma while achieving the same success rates as those achieved by conventional multiport laparoscopic repair. We predict that the rate of parastomal hernia repair will rise significantly as hernia specialists become more involved with parastomal hernia treatment and as colorectal surgeons learn to master skills in laparoscopic ventral/parastomal hernia repair.
Contributor Information
Hanh Tran, Discipline of Surgery, Sydney Medical School, University of Sydney, Westmead Hospital, Westmead, NSW, Australia..
Isidro Turingan, The Sydney Hernia Specialists Clinic, Sydney, NSW, Australia..
Marta Zajkowska, The Sydney Hernia Specialists Clinic, Sydney, NSW, Australia..
Kim Tran, The Sydney Hernia Specialists Clinic, Sydney, NSW, Australia..
References:
- 1. Carne PWG, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg. 2003;90:784–793 [DOI] [PubMed] [Google Scholar]
- 2. Pearl RK. Parastomal hernias. World J Surg. 1994;13:569–574 [DOI] [PubMed] [Google Scholar]
- 3. Janes A, Cengiz Y, Israelsson LA. Randomized clinical trial of the use of a prosthetic mesh to prevent parastomal hernia. Br J Surg. 2004;91:280–282 [DOI] [PubMed] [Google Scholar]
- 4. van Sprundel TC., Gerritsen van der Hoop A. Modified technique for parastomal hernia repair in patients with intractable stoma-care problems. Colorectal Dis. 2005;7(5):445–449 [DOI] [PubMed] [Google Scholar]
- 5. Lüning TH, Spilllenaar-Bilge EJ. Parastomal hernia: complications of extra-peritoneal onlay mesh placement. Hernia. 2009;13(5):487–490 [DOI] [PubMed] [Google Scholar]
- 6. Vijayasekar C, Marimuthu K, Jadhav V, Mathew G. Parastomal hernia: is prevention better than cure? Use of preperitoneal polypropylene mesh at the time of stoma formation. Tech Coloproctol. 2008;12(4):309–313 [DOI] [PubMed] [Google Scholar]
- 7. Sugarbaker PH. Prosthetic mesh repair of large hernias at the site of colonic stomas. Surg Gynecol Obstet. 1980;150:576–578 [PubMed] [Google Scholar]
- 8. Stelzner S, Hellmich G, Ludwig K. Repair of paracolostomy hernias with a prosthetic mesh in the intraperitoneal onlay position: modified Sugarbaker technique. Dis Colon Rectum. 2004;47:185–191 [DOI] [PubMed] [Google Scholar]
- 9. Bickel A, Shinkarevsky E, Eitan AJ. Laparoscopic repair of paracolostomy hernia. Laparoendosc Adv Surg Tech A. 1999;9:353–355 [DOI] [PubMed] [Google Scholar]
- 10. García-Vallejo L, Concheiro P, Mena E, Baltar J, Baamonde I, Folgar L. Parastomal hernia repair: laparoscopic ventral hernia meshplasty with stoma relocation. The current state and a clinical case presentation. Hernia. 2011;15(1):85–91 [DOI] [PubMed] [Google Scholar]
- 11. Mancini GJ, McClusky DA, III, Khaitan L, et al. Laparoscopic parastomal hernia repair using a non-slit mesh technique. Surg Endosc. 2007;21(9):1487–1491 [DOI] [PubMed] [Google Scholar]
- 12. Hansson BM, Slater NJ, van der Velden AS, et al. Surgical techniques for parastomal hernia repair: a systematic review of the literature. Ann Surg. 2012;255(4):685–695 [DOI] [PubMed] [Google Scholar]
- 13. Henniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years' experience with 850 consecutive cases. Ann Surg. 2003;238(3):391–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kaoutzanis C, Leichtle SW, Mouawad NJ, et al. Postoperative surgical site infections after ventral/incisional hernia repair: a comparison of open and laparoscopic outcomes. Surg Endosc. 2013; 27(6):2221–2230 [DOI] [PubMed] [Google Scholar]
- 15. Guzmán-Valdivia G, Guerrero TS, Laurrabaquio HV. Parastomal hernia-repair using mesh and an open technique. World J Surg. 2008;32(3):465–470 [DOI] [PubMed] [Google Scholar]
- 16. Safadi B. Laparoscopic repair of parastomal hernias: early results. Surg Endosc. 2004;12(4):676–680 [DOI] [PubMed] [Google Scholar]
- 17. Craft RO, Huguet KL, McLemore EC, Harold KL. Laparoscopic parastomal hernia repair. Hernia. 2007;12(2):137–140 [DOI] [PubMed] [Google Scholar]
- 18. Le Blanc KA, Bellanger DE, Whitaker JM, Hausmann MG. Laparoscopic parastomal hernia repair. Hernia. 2005;9:140–144 [DOI] [PubMed] [Google Scholar]
- 19. Banerjee A, Beck C, Narula VK, et al. Laparoscopic ventral hernia repair: does primary repair in addition to placement of mesh decrease recurrence? Surg Endosc. 2012;26(5):1264–1268 [DOI] [PubMed] [Google Scholar]