Abstract
Systemic lupus erythematosus (SLE) is known as the ‘great imitator’ mimicking a myriad of conditions often resulting in a delayed diagnosis. We report a case with multisite adenopathy radiologically suggestive of lymphoma who initially was referred to the ‘Cancer of Unknown Primary’ team. Following a re-evaluation of the case the patient was diagnosed with SLE and was started on appropriate therapy. Many conditions presenting to oncology may mimic cancer which needs to be borne in mind when assessing referred cases.
Background
In response to the National Institute of Health and Care Excellence guidelines published in 2010 addressing the ‘Diagnosis and Management of Metastatic Malignant Disease of Unknown Primary Origin’ recommendations were made that every hospital with a cancer centre or unit should establish a ‘Carcinoma of Unknown Primary (CUP) team’.1 Patients should be referred to the CUP team on the basis of limited imaging which is suggestive of metastatic disease (eg, chest X-ray with lung metastases, ultrasound abdomen suggesting liver metastases). It is the role of the CUP team to ensure that for each referral a management plan exists which includes:
Appropriate investigations
Symptom control
Access to psychological support and
Providing information.
The aim of this service is to ensure this particular group of patients is investigated promptly.
It is always important to remember, however, that a certain percentage of these patients may ultimately not go onto have a cancer diagnosed and as always, taking a thorough history is crucial to making the diagnosis.
This case report illustrates the importance of revisiting the clinical history and performing a focused examination. In particular connective tissue disorders can involve almost any body system2 and as a result, they can often present with symptoms also found in patients with metastatic disease including fatigue and weight loss.3
Case presentation
A 30-year-old woman presented to the emergency department with a 3-month history of pleuritic chest pain and acute shortness of breath. Her only other reported symptoms, at that stage, were unintentional weight loss of 4 kg over the same time period and a 4-week history of night sweats. She had a medical history of iron-deficiency anaemia secondary to menorrhagia and was on iron supplement, the only medication she was taking. She denied any contact with tuberculosis (TB), had recently travelled abroad to Slovakia and was a non-smoker. There was no other significant social or family history. Clinical examination revealed her to look well. She was feverish at 38°C and had a sinus tachycardia of 120 bpm; blood pressure was within normal limits, respiratory rate of 18/min and oxygen saturations of 100%. Cardiovascular and respiratory examinations were otherwise unremarkable. Pregnancy test was negative.
Investigations
In terms of baseline blood tests, she had a low haemoglobin count of 99 g/dL (normal 118–148 g/dL), and a raised white cell count of 14×109/L (normal 3.5–11×109/L). The differentials were neutrophil of 11.9×109/L (normal 2–7.5×109/L), lymphocyte 1.45×109/L (normal 1–3.5×109/L) and eosinophil 0.09×109/L (normal 0–0.4×109/L). Platelet count and clotting screen were normal except for a positive D-dimer of 838 ng/mL (normal <130 ng/mL). Her C reactive protein was elevated at 145 mg/L (normal <5 mg/L) and her biochemistry profile was otherwise unremarkable. Her arterial blood gas on room air demonstrated a mild hypoxaemia with arterial oxygen tension of 9.73 kPa (normal >10 kPa) and a normal arterial carbon dioxide tension.
In terms of radiological investigations, she initially had a chest X-ray that reported a soft tissue lesion in the left upper lobe of the lung measuring 27 mm and subsequently went onto have a CT pulmonary angiogram (CTPA), primarily to rule out pulmonary embolic disease. This was reported as demonstrating significant abnormalities with bulky axillary and mediastinal lymphadenopathy (figure 1) and soft tissue deposits in keeping with malignancy and in particular lymphoma (figure 2). Recommendation was thus made for a CT of the chest/abdomen/pelvis which demonstrated small volume cervical, aortocaval and pelvic lymphadenopathy. Further mention was made of an 8×7 cm fairly prominent centrally necrotic ‘almost malignant appearing mass’ within the pelvis (figure 3).
Figure 1.
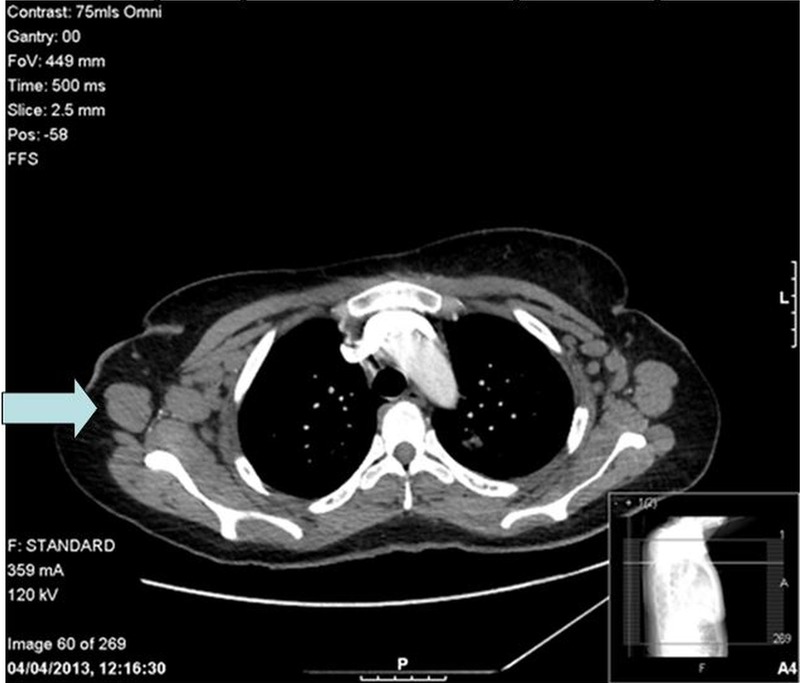
CT pulmonary angiogram demonstrating bulky axillary lymphadenopathy.
Figure 2.
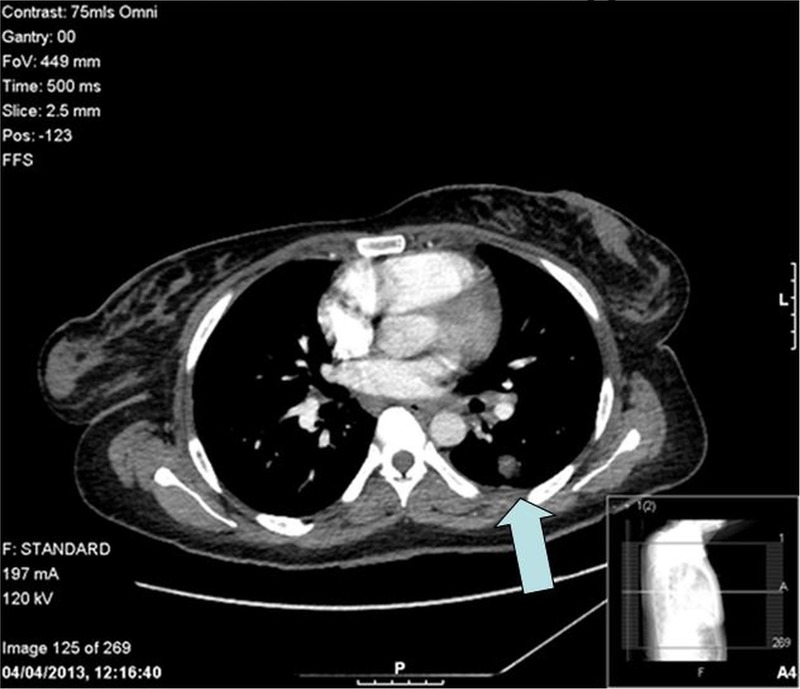
CT pulmonary angiogram demonstrating soft tissue deposits within the lung.
Figure 3.

CT of the chest/abdomen/pelvis demonstrating the pelvic mass.
At this stage in view of the radiological findings and the clinical history she was referred to the hospital CUP team and an ultrasound-guided trucut biopsy of an enlarged 3.3 cm right axillary lymph node was undertaken.
Differential diagnosis
When this patient was seen in the emergency department, the differential diagnoses for her shortness of breath and pleuritic chest pain included pulmonary embolism and atypical pneumonia. Antibiotic therapy with intravenous co-amoxiclav and oral clarithromycin was initiated. However, with the concomitant history of night sweats and weight loss, TB and malignancy were also raised as possibilities.
Outcome and follow-up
However, when she was reviewed by the consultant medical oncologist (member of the CUP team) she gave a more detailed prolonged 1 year history of malaise, lymph nodes palpable in the neck, headaches as well as arthralgia. The history of chest pain and shortness of breath, in fact, had been much more acute. The history was therefore felt to be very atypical for a solid tumour malignancy and although lymphoma did remain a possibility, the possibility of a connective tissue disorder was also considered. She therefore went onto have an autoantibody screen requested.
In view of the more detailed history the original CT scans were reviewed and the consensus was that while the chest changes and lymph nodes could be lymphomatous they could also be explained by a connective tissue disorder. Furthermore, once malignancy was felt to be much lower on the list of differentials the pelvic imaging was reviewed by a gynaecology-specialist radiologist and the pelvic mass was felt more to represent a pedunculated fibroid. The mass was encapsulated situated in the pouch of Douglas and was in continuity with the posterior uterine fundus. It had a central cystic degeneration and was unlikely to be related to the lymphadenopathy seen on CT but responsible for her history of menorrhagia.
The lymph node was reported as demonstrating reactive features alone with no evidence of lymphoma or TB. Finally the results of the autoimmune screen demonstrated the patient to have a highly positive antinuclear antibody (ANA) of >1 : 1000 (normal <1 : 40), a high antidouble-stranded DNA antibody (anti-dsDNA) titre of >200 IU/mL (normal range 0–40 IU/mL), a low complement C4 of 13 mg/dL (normal range 16–54 mg/dL), and a normal complement C3 of 114 mg/dL (normal range 70–165 mg/dL). Furthermore, she had a raised erythrocyte sedimentation rate of 128 mm/h (range 0–20 mm/h).
She was subsequently reviewed by the rheumatologists and diagnosed with likely systemic lupus erythematosus (SLE) with a super-imposed chest infection. The Systemic Lupus International Collaborating Clinics (SLICC) classification system4 was used and this patient fulfilled the clinical criteria of arthralgia and three of the recognised immunological criteria—ANA above laboratory reference range, anti-dsDNA above laboratory reference range and low C4 complement. Since the patient did not want to receive steroids she was started on hydroxychloroquine. The superimposed chest infection resolved with a week of co-amoxiclav with clarithromycin and she was discharged from hospital. One month later she was reviewed in the rheumatology outpatient department and, although she was symptomatically much better, in view of a persistently elevated anti-dsDNA titre of >200 IU/mL, mycophenolate was added to her treatment. She continues to remain under close follow-up by the rheumatologists. No imaging studies were repeated after therapy. She is not currently under follow-up by the gynaecologists for her uterine fibroid.
Discussion
SLE is a chronic autoimmune disease which can involve almost any body system.5 As a result, its presentation and progression can vary significantly, ranging from indolent to fulminant. Fatigue, skin rash and/or musculoskeletal symptoms are cardinal presenting symptoms of SLE6 while other signs and symptoms of SLE have also been reported, such as serositis,7 and generalised lymphadenopathy.8
This case report illustrates the importance of ensuring that relevant detailed history is obtained and equally importantly that this information is fed back to the radiologists reporting the imaging since their conclusions will undoubtedly be influenced by the clinical history. Interestingly although this patient had imaging which could have been suggestive of malignant disease, she described a much more prolonged history of non-specific symptoms and yet continued to remain systemically well up until the time of admission. Although this patient was referred correctly to the CUP team and an urgent lymph node biopsy was carried out which did not show lymphoma it would have been a very unusual presentation for a patient with malignancy. We can only come to this conclusion by taking an appropriate clinical history.
Learning points.
Thorough history taking and focused examination are crucial in making a correct diagnosis.
Patients presenting to Cancer of Unknown Primary team can have very broad differentials.
Systemic lupus erythematosus is an important differential diagnosis in any patient with symptoms and/or signs suggestive of a multisystem disorder.
Footnotes
Contributors: RG and WYCS assessed and diagnosed the patient. WYCS obtained consent to write the case report. WYCS and RG both contributed equally to the manuscript with the final version edited by RG.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.National Institute for Health and Clinical Excellence. Metastatic malignant disease of unknown primary origin (CG104). July 2013. http://www.nice.org.uk/CG104 (accessed 11 Aug 2013).
- 2.Fernandes N, Gomes G, Capela C. Presentation of systemic lupus erythematosus (SLE) in emergency department: a case report. BMC Res Notes 2013;6:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cabral DA, Tucker LB. Malignancies in children who initially present with rheumatic complaints. J Paediatr 1999;134:53–7 [DOI] [PubMed] [Google Scholar]
- 4.Petri M, Orbai AM, Alarcon GS, et al. Derivation and validation of Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 2012;64:2677–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenbaum E, Krebs E, Cohen M, et al. The spectrum of clinical manifestations, outcome and treatment of pericardial tamponade in patients with systemic lupus erythematosus: a retrospective study and literature review. Lupus 2009;6:608–12 [DOI] [PubMed] [Google Scholar]
- 6.Edworthy SM. Clinical manifestations of systemic lupus erythematosus. In: Harris ED, Budd RC, Firestein GS, et al. eds. Kelley's textbook of rheumatology. 7th edn Philadelphia, PA: WB Saunders, 2005:1201–24 [Google Scholar]
- 7.Man BL, Mok CC. Serositis related to systemic lupus erythematosus: prevalence and outcome. Lupus 2005;6:822–6 [DOI] [PubMed] [Google Scholar]
- 8.Al-Hashimi H, Bhowmik A. Generalised lymphadenopathy as the first manifestation of lupus nephritis. BMJ Case Rep. Published online: 22 Apr 2010. doi:10.1136/bcr.08.2009.2221 [DOI] [PMC free article] [PubMed] [Google Scholar]


