Abstract
Objective
This study sought to analyze recent trends over time in heart failure (HF) hospitalization rates, length of stay (LOS), and in-hospital mortality by age groups using a large national dataset of U.S. hospital discharges.
Background
HF hospitalization rates, LOS, and mortality have fallen over the past decade for older Medicare beneficiaries, but whether this holds true for younger adults is unknown.
Methods
From the National Inpatient Sample (NIS), we calculated HF hospitalization rates, LOS, and in-hospital mortality from 2001–2009 using survey data analysis techniques.
Results
1,686,089 hospitalizations with a primary discharge diagnosis of HF were identified from NIS data between 2001 and 2009. The overall national hospitalization rate decreased from 633 to 463 hospitalizations per 100,000 persons, (− 26.9%, p-for-trend<0.001). However, statistically significant declines (p<0.001) were only observed for patients age 55–64 years (−36.5%) 65–74 years (−37.4%), and ≥75 years (−28.3%), but not for patients age 18–44 years (−12.8%, p=0.57) or 45– 55 years (−16.2%, p=0.04). Statistically significant declines in LOS were only observed for patients age 65 years and older. Overall in-hospital mortality fell from 4.5% to 3.3%, a relative decline of 27.4%, (p-for-trend <0.001), but patients age 18 to 44 years did not exhibit a significant decline (−8.1%, p-for-trend=0.18). In secondary analyses significant declines in HF hospitalization rate over time were observed for white men, white women, and black women, but not for black men (−9.5%, p-for-trend=0.43).
Conclusions
Younger patients have not experienced comparable declines in HF hospitalization, LOS, and in-hospital mortality as older patients. Black men remain a vulnerable population for HF hospitalization.
Journal subject codes: congestive heart failure, epidemiology, hospitalization, mortality
Introduction
The heart failure (HF) hospitalization rate has dropped substantially over the past decade in the Medicare population (1) —nearly 30% from 1998 to 2008—implying some success in preventative efforts. However, the etiology of HF often differs between younger adults and older Medicare beneficiaries. Hypertension is the most common etiology of HF in the younger adults, (2) while coronary artery disease becomes a more common risk factor for HF among middle-aged and older patients. (3,4). In addition, as age increases, the prevalence of HF with preserved ejection fraction rises dramatically, in conjunction with comorbid risk factors such as hypertension, atrial fibrillation, diabetes mellitus, and renal insufficiency. (3,5,6) As such, declines in the HF hospitalization rate observed for older Medicare patients may not necessarily indicate a corresponding decrease for younger populations. Whether HF hospitalization rates differ across age groups in the U.S. population is unknown, and the focus of this study.
In addition, we have a limited understanding of how HF hospitalization rates have changed over time across race-sex groups. One study of the Medicare population found that HF hospitalization rates declined at a slower rate for black men compared with other groups. (1) However, black patients are more likely to develop HF at younger ages than white patients, (2) and whether this affects differences across race with respect to declines in HF hospitalizations is unknown. Furthermore, black patients represent a higher proportion of the uninsured and Medicaid enrollees, (7) which may potentially lead to differences in HF hospitalizations across race compared with studies examining Medicare data alone. As such, confirming whether black men had slower declines in HF hospitalization rate in the general population is important, as it may indicate that this group is a particularly vulnerable population that would benefit from targeted preventative efforts against HF risk factors. (8,9)
Accordingly, we analyzed data from the National Inpatient Sample (NIS), a large national dataset of acute care hospitalizations that includes all age groups and all types of health insurance coverage to examine changes across patient age categories in HF hospitalization rates, length of stay (LOS), and in-hospital mortality between 2001 and 2009. Secondary analyses examined trends in HF hospitalization by race-sex categories.
Methods
Data
The NIS, collected by the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project, is the largest all-payer inpatient database publicly available in the U.S. Consisting of discharge data from over 1,000 hospitals across 44 states, the NIS was designed to approximate a 20% stratified sample of U.S. community hospitals.(10) Statistical sampling weights provided by the NIS allows extrapolation to calculate expected hospitalization rates for the nation.(11) NIS data was collected on all patients regardless of health insurance provider. The following NIS fields were used for this analysis: patient age, sex, race, principal and secondary diagnosis codes, admission date, discharge date, in-hospital death, insurance status, and state of hospitalization. Secondary analyses stratified by race-sex categories were conducted in a subset of patients hospitalized in states that reported complete data on patient race across all years to the NIS.
Study Cohort
A total of 71,371,439 hospital discharges were reported to the NIS from 2001–2009 from 44 states reporting data to NIS. We excluded the following hospitalizations: discharges in which patient age was less than 18 years (n=12,091,363), those with missing data on patient age, sex, admission date, discharge date, or in-hospital death (n=252,617), discharges in which patients were admitted and discharged alive the same day as such events may not have truly represented hospitalizations for acute conditions (n=1,0373,079), and discharges from states that did not report data for each year of the study period (n=9,648,462). HF hospitalizations were classified as those with a principal discharge diagnosis of HF based on the following International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes: 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, and 428.xx.
Statistical analyses
We conducted a pre-specified analysis calculating population-based HF hospitalization rates per 100,000 persons for each calendar year, with the numerator representing the number of HF hospitalizations and the denominator representing the population age 18 years and older from U.S. Census estimates for each state.(12) Survey analysis methods were employed that used hospital-level discharge weights provided by the NIS to estimate the number of HF hospitalizations on a national level.(13) HF hospitalization rates were calculated for the overall cohort and for subgroups of age (18–45, 45–54, 55–64, 65–74, and ≥75 years), sex, and, insurance status (Medicare, Medicaid, private insurance [including health maintenance organizations], self-pay, no charge, and other). Because a denominator population of individuals specifying particular types of health insurance could not be constructed for each year, differences in HF hospitalization rate by insurance status were not estimated. Differences in LOS and in-hospital mortality rates were able to be evaluated by insurance status as calculation of these rates used the hospitalization as the unit of analysis. Comorbidities were identified from ICD-9-CM secondary diagnosis codes and were classified according to hierarchical condition categories, similar to those used by the Centers for Medicare and Medicaid Services for calculating their 30-day HF mortality measure.(14) To evaluate whether HF hospitalization rates declined faster than the overall hospitalization rate any cause, we calculated the hospitalization rate per 100,000 persons for all principal diagnoses over the study period.
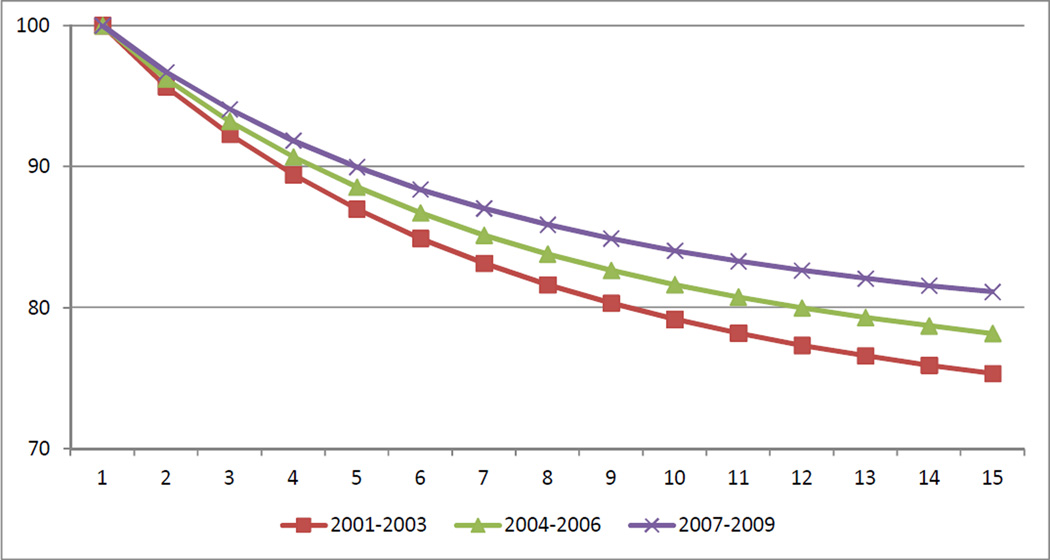
In-hospital survival curves were constructed that assumed that the discharge date recorded in NIS was the date of death, where the denominator represented the number of patients still hospitalized on a given hospital day, and the numerator represented the number of patients who were not recorded as having an in-hospital death on that hospital day. Survival curves were generated for three-year periods (2001–2003, 2004–2006, and 2007–2009) to examine how aggregate in-hospital mortality changed over the study period.
Statistical significance of the annual changes in HF hospitalization rate and in-hospital mortality were assessed using Poisson regression that included a variable representing the linear trend from the baseline year of 2001; a similar analysis was conducted for LOS using linear regression. All p-values were two-sided with a significance threshold of p<0.001. Statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, North Carolina).
Results
Our analytic cohort consisted of 48,305,918 hospitalizations for any principal discharge diagnosis across 29 states that reported data for each year between 2001 to 2009, of which 1,686,089 hospitalizations were for a principal discharge diagnosis of HF. After applying sampling weights to calculate the number of national discharges for HF from the NIS sample, this represents an estimated 8,249,759 HF hospitalizations in the U.S. from 2001–2009. HF patients were predominantly elderly with slightly more than half of the cohort aged 75 years and older. (Table 1) In 2001 there were slightly more women than men (55.0% v 45.0%) which diminished by 2009 (50.6% v 49.4%). White patients comprised the majority of patients; the proportion of patients with unknown race decreased from 27.7% to 10.7% as more states reported race data to NIS over the study period.
Table 1.
Characteristics of patients hospitalized for heart failure
| Description | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | p-for-trend |
|---|---|---|---|---|---|---|---|---|---|---|
| N (HF hospitalizations) | 999801 | 948849 | 946043 | 970085 | 965377 | 931124 | 882364 | 803318 | 802796 | <0.001 |
| Age (years) | ||||||||||
| 18 to <45 | 3.7% | 4.0% | 4.0% | 4.2% | 4.2% | 4.4% | 4.5% | 4.3% | 4.1% | 0.048 |
| 45 to <55 | 7.2% | 7.9% | 7.8% | 8.2% | 8.1% | 8.8% | 8.9% | 8.5% | 8.6% | 0.004 |
| 55 to <65 | 13.0% | 13.5% | 14.1% | 14.1% | 13.7% | 14.1% | 14.4% | 14.3% | 14.3% | 0.005 |
| 65 to <75 | 22.9% | 22.7% | 22.0% | 21.5% | 21.0% | 20.4% | 20.4% | 20.0% | 20.3% | <0.001 |
| >=75 | 53.2% | 52.0% | 52.1% | 52.0% | 53.0% | 52.2% | 51.9% | 52.9% | 52.7% | 0.942 |
| Gender | ||||||||||
| Male | 45.0% | 45.6% | 46.1% | 47.1% | 48.3% | 48.7% | 48.9% | 49.3% | 49.4% | <0.001 |
| Female | 55.0% | 54.4% | 53.9% | 52.9% | 51.7% | 51.3% | 51.1% | 50.7% | 50.6% | <0.001 |
| Race | ||||||||||
| White | 51.6% | 51.3% | 49.3% | 51.3% | 53.3% | 50.1% | 50.3% | 54.6% | 58.9% | 0.080 |
| Black | 12.2% | 14.1% | 13.7% | 15.0% | 12.0% | 14.9% | 15.7% | 15.3% | 17.2% | 0.019 |
| Hispanic | 5.9% | 6.3% | 8.3% | 6.6% | 6.4% | 7.7% | 6.9% | 6.9% | 8.2% | 0.167 |
| Other | 2.6% | 3.1% | 2.9% | 3.0% | 2.7% | 2.9% | 3.5% | 4.5% | 5.0% | 0.008 |
| Unknown | 27.7% | 25.2% | 25.8% | 24.1% | 25.5% | 24.3% | 23.6% | 18.8% | 10.7% | 0.009 |
| Primary Insurance | ||||||||||
| Medicare | 75.6% | 76.0% | 76.4% | 75.2% | 76.5% | 75.4% | 74.0% | 73.8% | 73.8% | 0.014 |
| Medicaid | 6.6% | 6.9% | 7.4% | 7.5% | 7.3% | 7.7% | 7.6% | 7.5% | 8.0% | 0.003 |
| Private including HMO | 13.7% | 12.8% | 11.9% | 12.4% | 11.5% | 11.6% | 12.7% | 13.5% | 12.5% | 0.780 |
| Self Pay | 2.5% | 2.5% | 2.3% | 3.0% | 3.1% | 3.2% | 3.3% | 3.1% | 3.8% | 0.001 |
| No charge | 0.2% | 0.2% | 0.3% | 0.4% | 0.3% | 0.4% | 0.5% | 0.4% | 0.4% | 0.003 |
| Other | 1.4% | 1.5% | 1.6% | 1.6% | 1.2% | 1.7% | 1.8% | 1.7% | 1.5% | 0.241 |
| Census Region | ||||||||||
| New England | 4.6% | 5.3% | 5.0% | 6.6% | 6.1% | 6.4% | 6.9% | 5.6% | 5.6% | 0.161 |
| Mid Atlantic | 10.9% | 11.7% | 13.0% | 15.3% | 15.8% | 17.4% | 16.1% | 12.2% | 14.0% | 0.215 |
| South Atlantic | 24.2% | 26.1% | 26.4% | 25.3% | 24.9% | 24.4% | 25.0% | 26.5% | 26.7% | 0.340 |
| West South Central | 17.8% | 13.1% | 11.9% | 11.3% | 10.8% | 10.7% | 12.1% | 13.0% | 12.1% | 0.174 |
| East South Central | 6.6% | 7.1% | 8.2% | 7.4% | 7.5% | 7.4% | 5.5% | 6.4% | 5.8% | 0.122 |
| West North Central | 10.8% | 10.5% | 10.5% | 9.8% | 9.4% | 10.4% | 9.4% | 10.3% | 9.9% | 0.133 |
| East North Central | 10.5% | 9.4% | 9.7% | 9.9% | 10.5% | 8.5% | 9.7% | 9.3% | 9.5% | 0.243 |
| Mountain | 1.3% | 1.7% | 1.5% | 1.6% | 1.4% | 1.4% | 1.6% | 2.0% | 1.6% | 0.157 |
| Pacific | 13.1% | 15.1% | 13.9% | 12.8% | 13.5% | 13.3% | 13.8% | 14.8% | 14.7% | 0.395 |
| Cardiovascular | ||||||||||
| PCI | 4.3% | 4.5% | 4.6% | 4.8% | 5.4% | 5.9% | 6.4% | 7.2% | 7.2% | <0.001 |
| CABG | 13.7% | 13.5% | 13.1% | 13.3% | 13.5% | 13.8% | 13.6% | 14.0% | 13.9% | 0.111 |
| Acute Myocardial Infarction | 2.4% | 2.4% | 2.5% | 2.4% | 2.5% | 2.2% | 2.3% | 2.3% | 2.4% | 0.244 |
| Unstable Angina | 4.0% | 3.8% | 3.5% | 3.3% | 3.1% | 2.9% | 2.7% | 2.7% | 2.5% | <0.001 |
| Chronic atherosclerosis | 47.9% | 48.1% | 48.8% | 49.4% | 50.1% | 49.8% | 50.8% | 52.0% | 52.4% | <0.001 |
| Cardio-respiratory failure and shock | 7.2% | 7.4% | 7.6% | 7.8% | 7.2% | 9.0% | 11.4% | 12.3% | 15.7% | 9.002 |
| Valvular or Rheumatic Heart Disease | 17.7% | 18.4% | 19.2% | 19.7% | 20.8% | 21.2% | 21.6% | 21.0% | 21.9% | <0.001 |
| Comorbidity | ||||||||||
| Hypertension | 39.7% | 42.3% | 43.4% | 43.9% | 43.5% | 43.6% | 54.3% | 57.1% | 59.0% | <0.001 |
| Stroke | 0.5% | 0.5% | 0.5% | 0.5% | 0.5% | 0.5% | 0.4% | 0.5% | 0.5% | 0.031 |
| Renal Failure | 11.7% | 13.2% | 14.9% | 16.8% | 21.8% | 32.7% | 37.6% | 40.8% | 44.4% | <0.001 |
| COPD | 29.1% | 30.1% | 30.5% | 31.2% | 31.7% | 31.5% | 32.1% | 30.5% | 31.1% | 0.064 |
| Pneumonia | 7.2% | 7.7% | 8.1% | 8.3% | 9.7% | 11.8% | 12.9% | 14.0% | 14.6% | <0.001 |
| Diabetes and Complications | 39.8% | 40.5% | 40.7% | 40.5% | 40.3% | 40.5% | 41.8% | 42.2% | 42.8% | 0.002 |
| Protein-Calorie Malnutrition | 1.6% | 1.5% | 1.6% | 1.9% | 2.0% | 1.9% | 2.3% | 2.8% | 3.4% | <0.001 |
| Dementia and Senility | 5.9% | 6.2% | 6.3% | 6.5% | 6.8% | 7.2% | 7.7% | 8.4% | 8.6% | <0.001 |
| Hemiplegia, Paralysis, Functional Disability | 3.1% | 3.2% | 3.0% | 3.0% | 2.9% | 2.9% | 3.1% | 3.6% | 3.6% | 0.132 |
| Vascular or Circulatory Disease | 8.9% | 9.2% | 9.0% | 9.5% | 9.8% | 10.0% | 10.9% | 11.7% | 11.7% | <0.001 |
| Metastatic Cancer and Acute Leukemia | 1.4% | 1.4% | 1.4% | 1.4% | 1.4% | 1.4% | 1.5% | 1.6% | 1.6% | 0.003 |
| Trauma | 2.2% | 2.5% | 1.4% | 1.5% | 1.5% | 1.5% | 1.7% | 1.9% | 1.9% | 0.415 |
| Major Psychological Disorders | 1.8% | 1.8% | 1.8% | 1.9% | 1.8% | 2.0% | 2.1% | 2.5% | 2.5% | 0.002 |
| Liver and Biliary Disease | 1.3% | 1.5% | 1.5% | 1.7% | 1.6% | 1.9% | 1.9% | 1.9% | 2.1% | <0.001 |
Abbreviations: CABG, coronary artery bypass surgery; COPD, chronic obstructive pulmonary disease; HMO, health maintenance organization; HF, heart failure; PCI, percutaneous coronary intervention
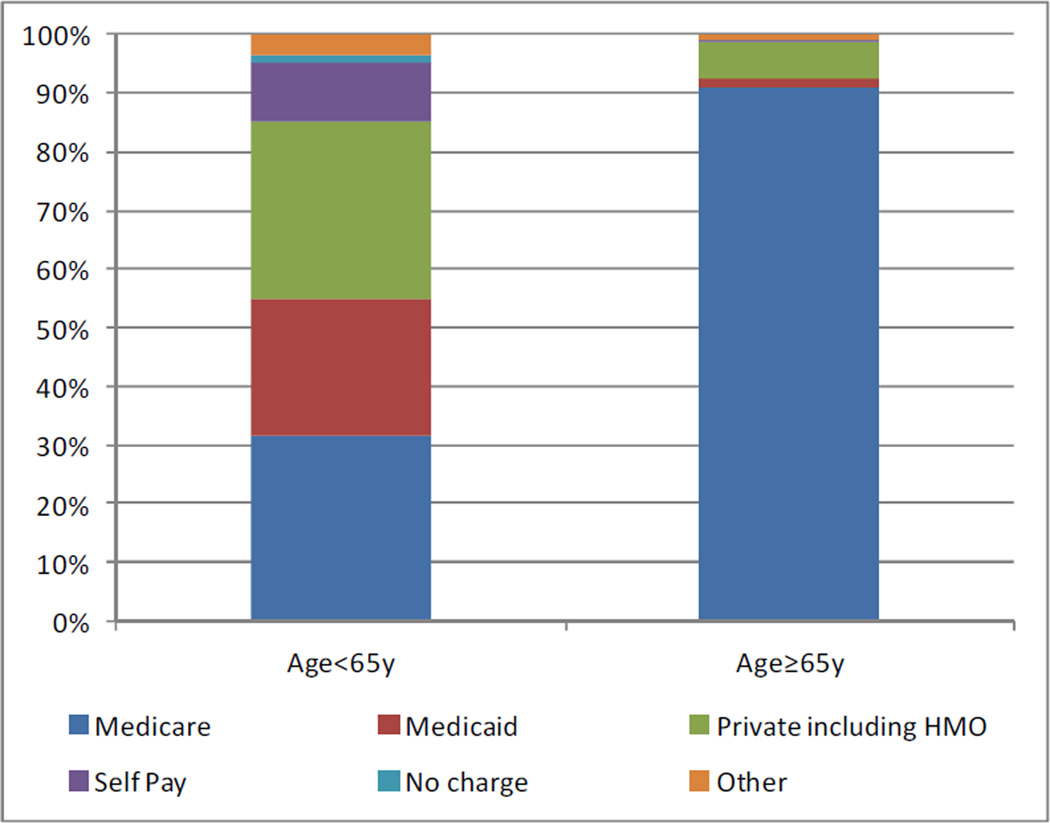
Approximately three-quarters of the patients hospitalized with HF had Medicare insurance coverage. The majority (90.9%) of HF patients age 65 years and older were insured by Medicare; the majority of HF patients younger than 65 were covered by insurance other than Medicare (69.6%) including private health insurance (30.4%) and Medicaid (23.5%). (Figure 1)
Figure 1.
Distribution health insurance status, by age≥65y and age<65y
Several comorbidities were more prevalent over the study period, including renal failure (from 11.7% to 44.4%, p-for-trend<0.001), hypertension (39.7% to 59.0%, p-for-trend<0.001), and cardio-respiratory failure or shock (7.2% to 15.7%, p-for-trend=0.002).
HF hospitalization rate
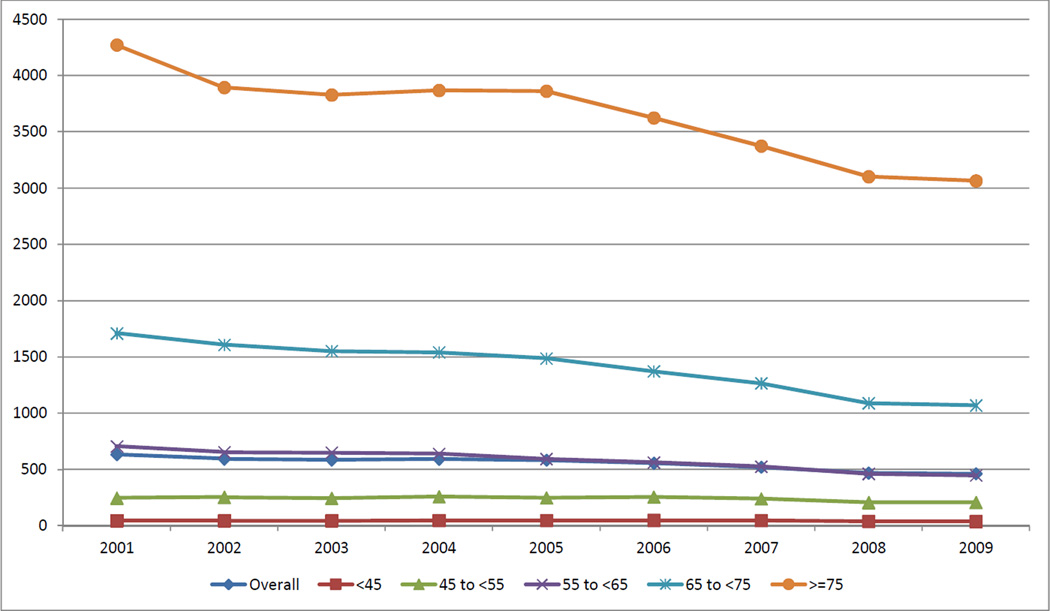
The national HF hospitalization rate declined from 633 to 463 hospitalizations per 100,000 persons from 2001 to 2009, a relative 26.9% decrease (p-for-trend<0.001). (Table 2) The aggregate hospitalization rate for any principal diagnosis also fell (from 17,087 to 14,183 per 100,000 persons, p-for-trend<0.001), a relative 17.0% decrease that was not statistically different than the HF hospitalization rate (p=0.002). Statistically significant declines in the HF hospitalization rate were observed for patients aged 55–64 years (from 704 to 447 per 100,000 persons, −36.5%, p-for-trend<0.001), 65–74 years (from 1709 to 1070 per 100,000 persons, −37.4%, p-for-trend <0.001) and ≥75 years (from 4272 to 3064 per 100,000 persons, −28.3%, p-for-trend<0.001). No statistically significant changes in HF hospitalization rates were observed for ages 18–44 (from 44 to 38 per 100,000 persons, −12.8%, p-for-trend =0.57) or 45–54 years (from 247 to 207 per 100,000 persons, −16.2%, p-for-trend=0.04). (Figure 2) The HF hospitalization rate declined for women (from 676 to 457 per 100,000 persons, −32.3%, p-for-trend <0.0001, while also declined for men but did not reach statistical significance (from 588 to 469 per 100,000 persons, −20.2%, p-for-trend=0.003). Statistically significant declines in the HF hospitalization rate were observed in five of the nine U.S. census regions.
Table 2.
Heart failure hospitalization rate per 100,000
| Description | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | relative change |
p-for-trend |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (2001–2009) | |||||||||||
| Overall | 633 | 594 | 586 | 593 | 584 | 556 | 521 | 469 | 463 | −26.9% | <0.001 |
| Age Categories | |||||||||||
| 18 to <45 | 44 | 45 | 45 | 48 | 48 | 49 | 47 | 41 | 38 | −12.8% | 0.570 |
| 45 to <55 | 247 | 254 | 245 | 259 | 248 | 257 | 241 | 207 | 207 | −16.2% | 0.036 |
| 55 to <65 | 704 | 653 | 649 | 640 | 593 | 563 | 526 | 462 | 447 | −36.5% | <0.001 |
| 65 to <75 | 1709 | 1608 | 1552 | 1541 | 1487 | 1372 | 1266 | 1089 | 1070 | −37.4% | <0.001 |
| >=75 | 4272 | 3894 | 3827 | 3868 | 3861 | 3624 | 3373 | 3102 | 3064 | −28.3% | <0.001 |
| Gender | |||||||||||
| Male | 588 | 558 | 557 | 575 | 580 | 557 | 523 | 474 | 469 | −20.2% | 0.003 |
| Female | 676 | 627 | 613 | 611 | 588 | 556 | 520 | 464 | 457 | −32.3% | <0.001 |
| Census Region | |||||||||||
| New England | 521 | 567 | 528 | 721 | 660 | 664 | 672 | 492 | 490 | −5.9% | 0.551 |
| Mid Atlantic | 526 | 530 | 583 | 700 | 716 | 757 | 663 | 452 | 518 | −1.5% | 0.804 |
| South Atlantic | 723 | 728 | 724 | 698 | 670 | 623 | 594 | 567 | 563 | −22.1% | <0.001 |
| West South Central | 861 | 597 | 537 | 517 | 491 | 465 | 497 | 482 | 450 | −47.8% | <0.001 |
| East South Central | 891 | 901 | 1024 | 939 | 942 | 884 | 606 | 640 | 578 | −35.1% | <0.001 |
| West North Central | 810 | 738 | 730 | 695 | 660 | 695 | 589 | 581 | 555 | −31.5% | <0.001 |
| East North Central | 687 | 569 | 577 | 597 | 619 | 472 | 499 | 424 | 424 | −38.2% | <0.001 |
| Mountain | 277 | 329 | 284 | 308 | 263 | 249 | 253 | 289 | 226 | −18.3% | 0.011 |
| Pacific | 395 | 427 | 385 | 359 | 374 | 353 | 342 | 330 | 322 | −18.5% | 0.003 |
Figure 2.
Heart failure hospitalization rate by age category, per 100,000 (2001–2009)
Sensitivity analyses that examined age categories in 5-year intervals and found that patients aged 55 years and older had statistically significant declines in the HF hospitalization rate (p<0.001) with marginal statistical significance for patients aged 45–49 and 50–54 years (p=0.07 and 0.01, respectively); no statistically significant declines in HF hospitalization rates were found for patients in 5-year age categories <45 years (all p>0.54).
In secondary analyses of 36,229,163 patients hospitalized in the 20 states that reported complete data on patient race, the overall decline in HF hospitalization rate was 24.7%, (p-for-trend <0.001) comparable to the primary analysis examining all states. Statistically significant declines were observed for white and black women (white women, −33.5%; black women −30.9%). White men had a non-statistically significant decrease in HF hospitalization rate (− 24.7%, p-for-trend=0.003), while black men did not have a statistically significant change in HF hospitalization rate (− 9.5%, p-for-trend=0.43) over the study period. Among patients age 75 years or older, there was no significant difference (p=0.59) between the change in HF hospitalization rate over time between black men (−29.8%, p-for-trend <0.001) and white men (−26.0%, p-for-trend <0.001). (Supplemental Table) While changes in HF hospitalization rate over time were not statistically significant for either black or white men younger than 55 years, there was essentially no change in the point estimates of relative change of HF hospitalization rate for black men 18–44 years (−2.7%, p-for-trend=0.70) or 45–54 years (+3.7%, p-for-trend=0.02) in contrast to white men 18–44 years (−21.0%, p-for-trend=0.55) or 45–54 years (− 17.6%, p-for-trend=0.08).
Length of stay
Observed mean LOS for HF hospitalization fell from 5.6 days to 5.3 days, a relative 6.4% decline (p-for-trend <0.001) (Table 3). Median LOS was 3.7 days in 2001 (25th to 75th percentile 2.1 to 6.3 days) which declined to 3.5 days (25th to 75th percentile 2.0 to 5.9 days) by 2009, (p-for-trend <0.001). Examined across patient age, statistically significant declines in LOS were only observed for those 75 years and older (− 8.5%, p-for-trend<0.001). Statistically significant declines in LOS for HF hospitalizations were observed for Medicare patients ( −7.1%, p-for-trend<0.001), while those with other insurance coverage was not associated with significant changes over time. The Mid Atlantic census region had the largest decline in LOS (−13.1%, p-for-trend <0.001). Secondary analyses were performed examining with renal failure or cardio-respiratory failure/shock, two comorbidities with large increases in prevalence over time. Patients with renal failure or cardio-respiratory failure/shock had significantly longer LOS (p<0.001) compared with patients without renal failure or cardio-respiratory failure/shock. Declines in LOS were steeper for patients with renal failure or cardio-respiratory failure/shock, compared with patients without renal failure or cardio-respiratory failure/shock.
Table 3.
Length of stay for heart failure hospitalization
| Description | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | relative change |
p-for- trend |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (2001–2009) | |||||||||||
| ALL | 5.6 | 5.6 | 5.6 | 5.6 | 5.5 | 5.4 | 5.4 | 5.3 | 5.3 | −6.4% | <0.001 |
| Age Categories | |||||||||||
| 18 to <45 | 5.1 | 5.1 | 5.1 | 5.0 | 5.0 | 4.9 | 5.0 | 5.3 | 5.0 | −2.0% | 0.559 |
| 45 to <55 | 5.2 | 5.2 | 5.2 | 5.2 | 5.1 | 5.0 | 5.0 | 5.1 | 5.1 | −1.8% | 0.553 |
| 55 to <65 | 5.6 | 5.6 | 5.5 | 5.6 | 5.3 | 5.3 | 5.4 | 5.4 | 5.5 | −2.7% | 0.061 |
| 65 to <75 | 5.7 | 5.7 | 5.6 | 5.6 | 5.5 | 5.5 | 5.4 | 5.4 | 5.4 | −5.0% | 0.007 |
| >=75 | 5.7 | 5.7 | 5.6 | 5.7 | 5.6 | 5.5 | 5.4 | 5.3 | 5.3 | −8.5% | <0.001 |
| Gender | |||||||||||
| Male | 5.6 | 5.5 | 5.5 | 5.5 | 5.4 | 5.3 | 5.3 | 5.3 | 5.2 | −5.5% | 0.003 |
| Female | 5.7 | 5.7 | 5.6 | 5.7 | 5.6 | 5.5 | 5.4 | 5.4 | 5.3 | −6.9% | <0.001 |
| Insurance status | |||||||||||
| Medicare | 5.7 | 5.7 | 5.6 | 5.6 | 5.5 | 5.5 | 5.4 | 5.4 | 5.3 | −7.1% | <0.001 |
| Medicaid | 6.1 | 5.9 | 6.0 | 5.9 | 5.8 | 5.6 | 5.9 | 5.7 | 5.6 | −7.3% | 0.074 |
| Private including HMO | 5.3 | 5.1 | 5.1 | 5.2 | 5.1 | 5.0 | 4.9 | 5.1 | 5.2 | −2.6% | 0.090 |
| Self Pay | 4.8 | 4.9 | 4.7 | 5.0 | 4.6 | 4.8 | 4.8 | 4.6 | 4.8 | −1.5% | 0.268 |
| No charge | 5.0 | 5.4 | 4.7 | 5.1 | 5.2 | 4.7 | 5.5 | 5.3 | 5.0 | 1.1% | 0.349 |
| Other | 5.0 | 5.4 | 5.4 | 4.9 | 4.9 | 4.9 | 5.1 | 4.9 | 4.9 | −2.1% | 0.396 |
| Census Region | |||||||||||
| New England | 5.6 | 5.3 | 5.2 | 5.4 | 5.4 | 5.2 | 5.4 | 5.6 | 5.1 | −8.4% | 0.787 |
| Mid Atlantic | 7.3 | 7.2 | 6.7 | 7.0 | 6.7 | 6.5 | 6.4 | 6.3 | 6.3 | −13.1% | <0.001 |
| South Atlantic | 5.4 | 5.4 | 5.5 | 5.3 | 5.2 | 5.2 | 5.2 | 5.2 | 5.2 | −4.1% | 0.131 |
| West South Central | 5.3 | 5.3 | 5.3 | 5.3 | 5.1 | 5.0 | 5.0 | 5.2 | 4.9 | −6.2% | 0.093 |
| East South Central | 5.5 | 5.7 | 5.5 | 5.5 | 5.4 | 5.3 | 5.2 | 5.2 | 5.1 | −6.7% | 0.436 |
| West North Central | 5.4 | 5.4 | 5.2 | 5.3 | 5.2 | 4.9 | 5.0 | 5.0 | 4.8 | −9.8% | 0.058 |
| East North Central | 6.0 | 5.9 | 5.9 | 5.7 | 5.6 | 5.4 | 5.4 | 5.4 | 5.5 | −8.5% | 0.056 |
| Mountain | 5.2 | 4.9 | 5.0 | 4.8 | 4.6 | 4.7 | 4.9 | 5.1 | 4.8 | −8.5% | 0.133 |
| Pacific | 5.3 | 5.2 | 5.2 | 5.1 | 5.1 | 5.1 | 5.0 | 5.2 | 5.1 | −3.8% | 0.635 |
| Selected comorbidities | |||||||||||
| Renal Failure | |||||||||||
| No | 5.3 | 5.2 | 5.1 | 5.1 | 4.9 | 4.7 | 4.7 | 4.6 | 4.6 | −13.7% | <0.001 |
| Yes | 8.5 | 8.5 | 8.2 | 8.1 | 7.4 | 6.7 | 6.5 | 6.4 | 6.2 | −26.6% | <0.001 |
| Cardio-respiratory failure and shock | |||||||||||
| No | 5.3 | 5.2 | 5.2 | 5.2 | 5.1 | 5.1 | 5.0 | 5.0 | 4.8 | −8.6% | <0.001 |
| Yes | 10.1 | 10.3 | 10.1 | 10.1 | 9.8 | 8.7 | 8.2 | 8.1 | 7.7 | −24.3% | <0.001 |
In secondary analyses among patients hospitalized states that reported complete race data, the overall decline in LOS was 7.9%, (p-for-trend <0.001). Statistically significant reductions in LOS were observed for white men (−7.1%), white women (−8.8%) and black women (−8.6%). LOS fell over time for black men (−7.8%, p-for-trend=0.18) but did not reach statistical significance.
In-hospital mortality
Observed in-hospital mortality for HF patients fell from 4.5% to 3.3%, a relative decline of 27.4%, (p-for-trend <0.001). There was increasingly higher survival during the HF hospitalization across the first, middle, and last thirds of the study period. (Figure 3) Statistically significant reductions in in-hospital mortality were observed for patients age 45 to 54 years (−21.7%), 55 to 64 years (−35.7%), 65 to 74 years (−29.0%) and 75 years or older (−25.4%); however patients age 18 to 44 years did not exhibit a significant decline in in-hospital mortality (−8.1%, p=0.18). (Table 4) Patients with Medicare, Medicaid, private insurance, and self pay coverage had significant declines in in-hospital mortality. Improvements in in-hospital mortality were observed across all census regions, except for the New England and Mountain regions. Similar to LOS, patients with renal failure or shock had significantly higher in-hospital mortality compared with patients without renal failure or shock, and faster rates of decline over the study period.
Figure 3.
In-hospital survival for HF hospitalization, by hospital day
Table 4.
In-hospital mortality for heart failure hospitalization, per 100
| Description | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | relative change | p-for- trend |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (2001−2009) | |||||||||||
| ALL | 4.5 | 4.3 | 4.2 | 4.0 | 3.8 | 3.6 | 3.3 | 3.3 | 3.3 | −27.4% | <0.001 |
| Age Categories | |||||||||||
| 18 to <45 | 1.7 | 1.6 | 1.6 | 1.7 | 1.2 | 1.4 | 1.4 | 1.4 | 1.5 | −8.1% | 0.181 |
| 45 to <55 | 1.6 | 1.7 | 1.7 | 1.7 | 1.6 | 1.3 | 1.3 | 1.3 | 1.3 | −21.7% | <0.001 |
| 55 to <65 | 2.7 | 2.4 | 2.3 | 2.4 | 1.9 | 1.9 | 1.7 | 1.6 | 1.7 | −35.7% | <0.001 |
| 65 to <75 | 3.6 | 3.5 | 3.3 | 3.2 | 2.9 | 2.8 | 2.5 | 2.5 | 2.5 | −29.0% | <0.001 |
| >=75 | 6.0 | 5.8 | 5.6 | 5.4 | 5.2 | 4.9 | 4.6 | 4.5 | 4.5 | −25.4% | <0.001 |
| Gender | |||||||||||
| Male | 4.7 | 4.5 | 4.2 | 4.1 | 3.8 | 3.5 | 3.2 | 3.3 | 3.3 | −30.5% | <0.001 |
| Female | 4.4 | 4.1 | 4.1 | 3.9 | 3.8 | 3.6 | 3.4 | 3.4 | 3.3 | −24.8% | <0.001 |
| Insurance status | |||||||||||
| Medicare | 4.9 | 4.7 | 4.5 | 4.3 | 4.1 | 3.9 | 3.6 | 3.6 | 3.6 | −27.4% | <0.001 |
| Medicaid | 2.6 | 2.5 | 2.6 | 2.3 | 1.8 | 1.8 | 1.8 | 1.8 | 1.7 | −32.5% | <0.001 |
| Private including HMO | 3.8 | 3.1 | 3.3 | 3.3 | 3.2 | 3.0 | 3.1 | 2.9 | 3.0 | −21.0% | 0.009 |
| Self Pay | 2.3 | 2.1 | 1.9 | 2.6 | 2.1 | 1.7 | 1.7 | 1.6 | 1.1 | −52.1% | <0.001 |
| No charge | 1.7 | 0.8 | 1.1 | 2.3 | 1.4 | 1.2 | 1.8 | 0.6 | 2.3 | 33.2% | 0.757 |
| Other | 4.6 | 5.2 | 6.5 | 5.1 | 4.7 | 3.7 | 3.8 | 4.8 | 6.0 | 31.2% | 0.660 |
| Census Region | |||||||||||
| New England | 5.0 | 4.6 | 4.1 | 4.1 | 3.9 | 4.0 | 3.4 | 3.7 | 3.8 | −23.3% | 0.001 |
| Mid Atlantic | 5.4 | 5.5 | 4.6 | 4.8 | 4.7 | 4.1 | 3.9 | 4.0 | 3.8 | −29.9% | <0.001 |
| South Atlantic | 4.3 | 3.8 | 3.9 | 3.7 | 3.2 | 3.1 | 2.9 | 2.8 | 3.1 | −28.8% | <0.001 |
| West South Central | 3.9 | 3.5 | 3.9 | 3.5 | 3.3 | 3.3 | 2.9 | 2.8 | 3.0 | −23.7% | <0.001 |
| East South Central | 4.5 | 4.7 | 4.6 | 4.5 | 4.1 | 3.6 | 3.6 | 3.7 | 3.4 | −23.5% | <0.001 |
| West North Central | 4.8 | 4.5 | 3.9 | 4.0 | 4.1 | 3.7 | 3.5 | 3.6 | 3.6 | −25.0% | <0.001 |
| East North Central | 4.8 | 4.4 | 4.2 | 3.8 | 3.5 | 3.4 | 3.1 | 2.9 | 2.9 | −39.5% | <0.001 |
| Mountain | 4.1 | 4.1 | 3.9 | 3.9 | 2.8 | 3.5 | 3.6 | 3.5 | 2.9 | −29.4% | 0.006 |
| Pacific | 4.6 | 4.3 | 4.4 | 4.0 | 3.9 | 3.7 | 3.6 | 3.8 | 3.3 | −27.9% | <0.001 |
| Selected comorbidities | |||||||||||
| Renal Failure | |||||||||||
| No | 3.6 | 3.3 | 3.2 | 3.0 | 2.8 | 2.6 | 2.3 | 2.5 | 2.3 | −36.8% | <0.001 |
| Yes | 11.3 | 10.5 | 9.7 | 9.0 | 7.2 | 5.5 | 4.9 | 4.6 | 4.5 | −60.0% | <0.001 |
| Cardio-respiratory failure and shock | |||||||||||
| No | 3.0 | 2.7 | 2.6 | 2.5 | 2.4 | 2.2 | 2.0 | 2.0 | 1.8 | −39.6% | <0.001 |
| Yes | 24.7 | 23.8 | 22.7 | 22.4 | 21.6 | 16.7 | 13.1 | 12.9 | 11.3 | −54.2% | <0.001 |
Abbreviations: HMO, health maintenance organization
In secondary analysis, the overall decline in in-hospital mortality restricted to states reporting complete patient race data was statistically significant (−29.1%, p-for-trend=<0.001) and similar to the primary analysis. All race-sex groups exhibited statistically significant declines in-hospital mortality: white men (−27.7%), white women (−24.6%), black men (−39.2%), and black women (−31.7%) (p-for-trend <0.001).
Discussion
Using a national all-payer database of hospital discharges in the U.S., we found that the overall national HF hospitalization rate fell by a relative 26.9% from 2001 to 2009. This decline is similar in magnitude to the 29.5% decrease in HF hospitalization rates observed in the Medicare population from 1998 to 2008.(1) However, our study adds to prior work by demonstrating the HF hospitalization rate did not decrease significantly for patients age 18–44 years and 45–55 years, indicating that trends for HF hospitalization rate observed for older Medicare patients do not necessarily apply to younger populations. An Australian study of HF hospitalization trends (15) also found that reductions in the HF hospitalization rate was predominately limited to older populations: from 1990–1993 to 2002–2005 the HF hospitalization rate fell by 44% for men and by 46.5% for women age 65–74 years, but the decline in HF hospitalization rate was much slower for women <65 years (−11.5%), and in fact increased slightly over time for men (+1.7%).
While the overall reduction in the HF hospitalization rate represents a success, our findings illustrate that challenges remain for ensuring comparable improvements for younger patients. One possible explanation for the lack of decline in HF hospitalization for younger patients is that HF risk factor control may have improved more in older patients. For example, hypertension is an important cause of diastolic HF, (16) but hypertension awareness and treatment is considerably lower for younger patients < 40 years compared with those ≥40 years. (17,18) Coronary artery disease is another major cause of HF that is more prevalent with older age, and the declines in ischemic heart disease events over the past decade in observed older patients (19) may have been less dramatic for younger patients. Other causes of heart failure, such as such as infectious etiologies and peripartum cardiomyopathy commonly manifest at younger ages,(20) and the incidence of these conditions may not have declined as rapidly as HF etiologies found more frequently in older patients.
Our overall findings of substantial decreases in HF hospitalization rates over time are consistent with reports from several countries. In Sweden (1988 to 2000),(21) the Netherlands (1980 to 1999), (22) New Zealand study (1988 to 2008),(23) and Scotland (1986 to 1999)(24) the HF hospitalizations rates peaked in the 1990s, and with significant declines afterwards. Two studies outside of the U.S. have evaluated HF hospitalization trends since 2000. In Canada (25) the overall age-standardized HF rate (including hospitalizations, outpatient clinic and emergency department visits) decreased by 25.1% from 1999 to 2007 (25); faster declines in HF hospitalization rate alone were observed. In New Zealand (23) the HF hospitalization rate peaked in 1998–1999 and decreased by 28.6% for men and 31.2% for women until 2008. Thus, the decline in the HF hospitalization rate over the most recent decade appears in line with observations from other developed nations.
Reasons for the decline in HF hospitalization rate are likely multi-factorial. One possibility is that control of risk factors leading to HF have improved over time. For example, hypertension control in the U.S. has increased from 27.3% from 1988–1994 to 50.1% in 2007–2008.(17) Incidence of ischemic heart disease has decreased dramatically over the past decade, (19,26) with parallel increases in the use of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, and statins in the U.S. (19) Another contributor to the decline in HF hospitalization rate may be due to shifting of location of HF care from hospitals to emergency department or outpatient settings. The Canadian study found a greater proportion of HF cases diagnosed in outpatient clinics and emergency department over time, with HF incidence rates declining faster for hospitals compared with other clinical settings; (25) nevertheless, the overall HF incidence rate from all locations fell over time suggesting that there has been some overall reduction in HF incidence as well in Canada. A U.S. study examining Medicare hospital and outpatient billing claims found a modest decline in overall HF incidence from 1994 to 2003, decreasing from 32 to 29 per 1000 person-years. (27)
Our study found that trends in LOS also diverged according to patient age. While patients of typical Medicare age (≥65 years) had statistically significant reductions in LOS over the study period, this was not the case for patients younger than 65 years. Understanding the reasons for the lack of decline in LOS in younger patients will ultimately require clinical data, but we speculate that it may be related in some part to differences in comorbidity burden. Older patients typically have multiple comorbidities, and thereby perhaps more opportunities to reduce LOS through more intensive use of skilled nursing facilities or increased referral to hospice, both of which have increased in the Medicare population over the past decade. (28)
Our study also noted divergence across age groups for in-hospital mortality, with no significant change for patients aged 18–44 years, but significant decreases for older patients. This may be due to differences in HF etiology or severity of illness in younger adults compared with older adults. Differences in discharge disposition may again play a role. While in-hospital mortality has decreased over the past decade among Medicare patients, 30-day mortality has decreased at a slower rate due to a greater proportion of deaths that occur after discharge from HF hospitalization. (28) As with LOS, the lack of improvement in in-hospital mortality may potentially be explained if a greater number of older patients were discharged to or died in non-hospital-based facilities, while younger patients were more likely to remain hospitalized until they died. Because the NIS does not track individual patients after hospital discharge, this hypothesis will need to be verified using other sources of data.
The prevalence of comorbidities of patients hospitalized for HF increased over time in our study sample. This is consistent with a study of the U.S. Veterans Administration population (29) demonstrating an increase in the comorbidity of hospitalized HF patients. Other countries have also documented increasing comorbidities. For example, in Western Australia the proportion of HF patients with renal failure increased from 6.3% to 17.3% and with diabetes mellitus increased from 18.5% to 26.9%; (15) in Scotland, the proportion of male HF patients with renal failure increased from 4.1% to 18.5%, and diabetes mellitus increased from 7.6% to 19.4%. (24) These findings either represent a true clinical increase in the burden of comorbidity, or are explained by the additional coding of secondary diagnoses over time. NHANES reports that the prevalence of several comorbidities has increased over time in HF patients—renal disease increased by 11.2 percentage points from 1988 to 2008, diabetes increased by 13.6 percentage points, and obesity increased by 14.0 percentage points. (30) This data, based on patient interviews and examination of subjects, strongly suggest that the comorbidity profile of HF patients has worsened over time. While it is possible that hospitals may have been more aggressive in coding secondary diagnoses over time for reimbursement purposes, such “upcoding” (31) seems unlikely to fully explain the increase in comorbidities seen in cohorts in Australia, Scotland and the U.S. Veterans Administration, given that these are government-run health care systems with little incentive to upcode for added reimbursement. Furthermore, substantial upcoding would alter the relationship between comorbidity and outcomes (such as mortality) as more patients with less severe comorbidities were included. However, this does not appear to be the case, at least in the Medicare population, as the coefficients of the CMS HF mortality model have remained stable from 2005 to 2008.(32,33)
Our secondary analyses of patients with renal failure or cardio-respiratory failure/shock confirm that patients with these comorbidities were indeed more complex, with higher LOS and in-hospital mortality than patients without these comorbidities. While the steeper decline over time in LOS and in-hospital mortality for patients with renal failure or cardio-respiratory failure/shock may potentially indicate that additional patients with less severe comorbidity were coded over time, this would also occur if patients with renal failure or cardio-respiratory failure/shock were more likely to be discharged to skilled nursing facilities or hospice over the study period. Ultimately, studies using clinical data will be required to determine whether the increase in comorbidities reflect a higher threshold for HF hospitalization, differences in coding of secondary diagnoses, or more intensive utilization of post-discharge facilities over time.
Secondary analyses also confirm that the HF hospitalization rate fell more slowly for black men compared with other race-sex groups. A prior study of Medicare beneficiaries(1) also reported that reductions in HF hospitalization rate lagged for black men, but until this time no large scale study had verified in a general non-Medicare population. A small study that analyzed hospital discharge data from Tennessee over 1997–2006, and reported that black men had 28.2% increase in age-adjusted HF hospitalization rate, (34) higher compared with other race-sex groups (range 4.0% to 11.7%). Taken together, these studies strongly suggest that black men represent a particularly vulnerable population for HF hospitalization.
We speculate that black men had a slower rate of decline in HF hospitalizations in part due to differences in risk factor management. The Multi-Ethnic Study of Atherosclerosis and the Coronary Artery Risk Development in Young Adults study suggested that the excess risk of developing HF among black patients was primarily due to higher rates of hypertension, obesity, and diabetes mellitus.(2,35) Prevalence of obesity and diabetes mellitus have increased faster in black men compared with other race-sex groups. (36,37) Hypertension has increased over the past two decades for men and black subjects, (17) yet black men have lower rates of blood pressure screening, awareness, treatment, and control of hypertension compared with other race-sex groups. (38,39) It was reassuring, however, to observe that the decline in in-patient mortality for black men hospitalized for HF was comparable to other race-sex groups. Of note, in-hospital mortality rates for black patients were lower than white patients, a finding also observed in other studies; (40,41) the reason for this phenomenon is not well understood as black HF patients have been found to receive comparable quality of HF care, as assessed by use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers; (41) the lower in-hospital mortality rate among black patients may represent differences in HF etiology, disease progression, or severity of HF among hospitalized patients.
Limitations
Our study was limited by the fact that HF hospitalizations were identified through ICD-9-codes and not clinically confirmed. ICD-9-CM codes have high specificity (~95%) and positive predictive value for HF (~95%), (42–49) but our findings would only be affected if HF coding patterns changed over time. Second, we were unable to examine subcategories of HF, i.e. systolic versus diastolic HF, and ischemic versus non-ischemic HF, nor were we able to assess severity of HF hospitalization such as use of care in the intensive care unit. Third, the NIS does not track individual patients over time, and as such we were unable to determine whether changes in HF hospitalization rates represented declines in unique individuals hospitalized or declines in readmission after index HF hospitalizations. Similarly we were unable to assess whether the decline in HF hospitalizations presented a decrease in incident or prevalent cases; however, studies of Medicare patients suggest that the decline in HF hospitalization rate was almost entirely due to new cases.(1) Lastly, we were only able to examine in-hospital outcomes and were not able to assess whether declines in inpatient mortality which may reflect shorter LOS; we were unable to examine whether post-discharge mortality increased to offset improved inpatient outcomes.
Conclusion
Using a large, all-payer population of U.S. adults, we observed a 26.9% decrease in the overall adjusted HF hospitalization rate from 2000 to 2009, but younger patients have not experienced comparable declines in HF hospitalization, LOS, and in-hospital mortality as older patients. Black men remain a vulnerable group with no significant decline in HF hospitalization rate over the past decade.
Supplementary Material
Acknowledgments
Acknowledgments and Funding Sources:
This work was supported by an Agency for Healthcare Research and Quality (AHRQ) Career Development Award (1K08HS018781-01) for Dr. Chen. Drs. Krumholz, Chen and Wang are supported by grant U01 HL105270-02 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. Dr. Dharmarajan is supported by an NIH T32 training grant in cardiovascular disease (2T32HL007854-16A1) from Columbia University.
Footnotes
Disclosures:
Dr. Krumholz reports that he chairs a cardiac scientific advisory board for UnitedHealth and is the recipient of a research grant from Medtronic, Inc. through Yale University.
References
- 1.Chen J, Normand S-LT, Wang Y, Krumholz HM. National and Regional Trends in Heart Failure Hospitalization and Mortality Rates for Medicare Beneficiaries, 1998–2008. JAMA: The Journal of the American Medical Association. 2011;306:1669–1678. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cody RJ, Torre S, Clark M, Pondolfino K. Age-Related Hemodynamic, Renal, and Hormonal Differences Among Patients With Congestive Heart Failure. Arch Intern Med. 1989;149:1023–1028. [PubMed] [Google Scholar]
- 4.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk Factors for Congestive Heart Failure in US Men and Women: NHANES I Epidemiologic Follow-up Study. Arch Intern Med. 2001;161:996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 5.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in Prevalence and Outcome of Heart Failure with Preserved Ejection Fraction. New England Journal of Medicine. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 6.Zile MR, Brutsaert DL. New Concepts in Diastolic Dysfunction and Diastolic Heart Failure: Part I. Circulation. 2002;105:1387–1393. doi: 10.1161/hc1102.105289. [DOI] [PubMed] [Google Scholar]
- 7.Kaiser Family Foundation. [Accessed July 18, 2012];Medicaid’s role for black Americans. 2011 Available at http://www.kff.org/medicaid/upload/8188.pdf.
- 8.Hess PL, Reingold JS, Jones J, et al. Barbershops as hypertension detection, referral, and follow-up centers for black men. Hypertension. 2007;49:1040–1046. doi: 10.1161/HYPERTENSIONAHA.106.080432. [DOI] [PubMed] [Google Scholar]
- 9.Victor RG, Ravenell JE, Freeman A, et al. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med. 2011;171:342–350. doi: 10.1001/archinternmed.2010.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. [Accessed October 18, 2011];Healthcare Cost & Utilization Project (HCUP) 2011 http://www.ahrq.gov/data/hcup/ [PubMed]
- 11.Healthcare Cost and Utilization Project. [Accessed October 18, 2011];HCUP Methods Series. 2011 Available at http://www.hcup-us.ahrq.gov/reports/methods/methods_topic.jsp.
- 12.U.S. Census Bureau. [Accessed October 18, 2011];Population estimates. 2011 http://www.census.gov/popest/states/
- 13.Healthcare Cost and Utilization Project. [Accessed October 18, 2011];Nationwide Inpatient Sample Trends Supplemental Files. 2011 http://www.hcup-us.ahrq.gov/db/nation/nis/nistrends.jsp.
- 14.Krumholz HM, Wang Y, Mattera JA, et al. An Administrative Claims Model Suitable for Profiling Hospital Performance Based on 30-Day Mortality Rates Among Patients With Heart Failure. Circulation. 2006;113:1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 15.Teng TH, Finn J, Hobbs M, Hung J. Heart failure: incidence, case fatality, and hospitalization rates in Western Australia between 1990 and 2005. Circ Heart Fail. 2010;3:236–243. doi: 10.1161/CIRCHEARTFAILURE.109.879239. [DOI] [PubMed] [Google Scholar]
- 16.Biello KB, Rawlings J, Carroll-Scott A, Browne R, Ickovics JR. Racial disparities in age at preventable hospitalization among U.S. Adults. Am J Prev Med. 2010;38:54–60. doi: 10.1016/j.amepre.2009.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egan BM, Zhao Y, Axon RN. US Trends in Prevalence, Awareness, Treatment, and Control of Hypertension, 1988–2008. JAMA: The Journal of the American Medical Association. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 18.Ostchega Y, Hughes JP, Wright JD, McDowell MA, Louis T. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens. 2008;21:159–165. doi: 10.1038/ajh.2007.32. [DOI] [PubMed] [Google Scholar]
- 19.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 20.Felker GM, Thompson RE, Hare JM, et al. Underlying Causes and Long-Term Survival in Patients with Initially Unexplained Cardiomyopathy. New England Journal of Medicine. 2000;342:1077–1084. doi: 10.1056/NEJM200004133421502. [DOI] [PubMed] [Google Scholar]
- 21.Schaufelberger M, Swedberg K, Koster M, Rosen M, Rosengren A. Decreasing one-year mortality and hospitalization rates for heart failure in Sweden; Data from the Swedish Hospital Discharge Registry 1988 to 2000. Eur Heart J. 2004;25:300–307. doi: 10.1016/j.ehj.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 22.Mosterd A, Reitsma JB, Grobbee DE. Angiotensin converting enzyme inhibition and hospitalisation rates for heart failure in the Netherlands,1980 to 1999: the end of an epidemic? Heart. 2002;87:75–76. doi: 10.1136/heart.87.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wasywich CA, Gamble GD, Whalley GA, Doughty RN. Understanding changing patterns of survival and hospitalization for heart failure over two decades in New Zealand: utility of 'days alive and out of hospital' from epidemiological data. Eur J Heart Fail. 2010;12:462–468. doi: 10.1093/eurjhf/hfq027. [DOI] [PubMed] [Google Scholar]
- 24.Jhund PS, Macintyre K, Simpson CR, et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009;119:515–523. doi: 10.1161/CIRCULATIONAHA.108.812172. [DOI] [PubMed] [Google Scholar]
- 25.Ezekowitz JA, Kaul P, Bakal JA, Quan H, McAlister FA. Trends in heart failure care: has the incident diagnosis of heart failure shifted from the hospital to the emergency department and outpatient clinics? Eur J Heart Fail. 2010;13:142–147. doi: 10.1093/eurjhf/hfq185. [DOI] [PubMed] [Google Scholar]
- 26.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 27.Curtis LH, Whellan DJ, Hammill BG, et al. Incidence and prevalence of heart failure in elderly persons, 1994–2003. Arch Intern Med. 2008;168:418–424. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 28.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heidenreich PA, Sahay A, Kapoor JR, Pham MX, Massie B. Divergent trends in survival and readmission following a hospitalization for heart failure in the Veterans Affairs health care system 2002 to 2006. J Am Coll Cardiol. 2010;56:362–368. doi: 10.1016/j.jacc.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 30.Wong CY, Chaudhry SI, Desai MM, Krumholz HM. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med. 2011;124:136–143. doi: 10.1016/j.amjmed.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silverman E, Skinner J. Medicare upcoding and hospital ownership. J Health Econ. 2004;23:369–389. doi: 10.1016/j.jhealeco.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 32.Bernheim SM, Wang Y, Bhat KR, et al. Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measures. New Haven, CT: Yale-New Haven Health Services Corporation / Center for Outcomes Research & Evaluation; 2010. [Accessed March 11, 2011]. Available at: http://www.qualitynet.org. [Google Scholar]
- 33.Grosso LM, Schreiner GC, Wang Y, et al. Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measures. New Haven, CT: Yale-New Haven Health Services Corporation / Center for Outcomes Research & Evaluation; 2009. [Accessed March 11, 2011]. Available at http://www.qualitynet.org. [Google Scholar]
- 34.Husaini BA, Mensah GA, Sawyer D, et al. Race, sex, and age differences in heart failure-related hospitalizations in a southern state: implications for prevention. Circ Heart Fail. 2011;4:161–169. doi: 10.1161/CIRCHEARTFAILURE.110.958306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boyle JP, Honeycutt AA, Narayan KMV, et al. Projection of Diabetes Burden Through 2050. Diabetes Care. 2001;24:1936–1940. doi: 10.2337/diacare.24.11.1936. [DOI] [PubMed] [Google Scholar]
- 37.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 38.Blanchard J, Lurie N. Preventive care in the United States: are blacks finally catching up? Ethn Dis. 2005;15:498–504. [PubMed] [Google Scholar]
- 39.Victor RG, Leonard D, Hess P, et al. Factors associated with hypertension awareness, treatment, and control in Dallas County, Texas. Arch Intern Med. 2008;168:1285–1293. doi: 10.1001/archinte.168.12.1285. [DOI] [PubMed] [Google Scholar]
- 40.Gordon HS, Nowlin PR, Maynard D, Berbaum ML, Deswal A. Mortality after hospitalization for heart failure in blacks compared to whites. Am J Cardiol. 2010;105:694–700. doi: 10.1016/j.amjcard.2009.10.051. [DOI] [PubMed] [Google Scholar]
- 41.Rathore SS, Foody JM, Wang Y, et al. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. 2003;289:2517–2524. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- 42.Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002;144:290–296. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- 43.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 44.Goff DC, Jr., Pandey DK, Chan FA, Ortiz C, Nichaman MZ. Congestive heart failure in the United States: is there more than meets the I(CD code)? The Corpus Christi Heart Project. Arch Intern Med. 2000;160:197–202. doi: 10.1001/archinte.160.2.197. [DOI] [PubMed] [Google Scholar]
- 45.Lee DS, Donovan L, Austin PC, et al. Comparison of coding of heart failure and comorbidities in administrative and clinical data for use in outcomes research. Med Care. 2005;43:182–188. doi: 10.1097/00005650-200502000-00012. [DOI] [PubMed] [Google Scholar]
- 46.Kumler T, Gislason GH, Kirk V, et al. Accuracy of a heart failure diagnosis in administrative registers. Eur J Heart Fail. 2008;10:658–660. doi: 10.1016/j.ejheart.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 47.Quan H, Li B, Saunders LD, et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–1441. doi: 10.1111/j.1475-6773.2007.00822.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rosamond WD, Chang PP, Baggett C, et al. Classification of Heart Failure in the Atherosclerosis Risk in Communities (ARIC) Study / Clinical Perspective. Circulation: Heart Failure. 2012;5:152–159. doi: 10.1161/CIRCHEARTFAILURE.111.963199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saczynski JS, Andrade SE, Harrold LR, et al. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):129–140. doi: 10.1002/pds.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.