Abstract
Patients with poorly controlled diabetes, coronary heart disease, and depression have an increased risk of adverse outcomes. In a randomized, controlled trial, we tested an intervention designed to improve disease control outcomes for diabetes and/or heart disease and coexisting depression. Patients with one or more parameters of poor medical disease control (ie, HbA1c ≥8.5, or SBP >140, or LDL >130) and a Patient Health Questionnaire-9 (PHQ-9) ≥10 were randomized to the TEAMcare intervention or usual care (N = 214). This article will describe the TEAMcare health services model that has been shown to improve quality of care and medical and psychiatric outcomes.
Keywords: care management, collaborative care depression, diabetes, heart disease, multicondition, primary care, treat-to-target
Chronic diseases are very common in aging populations. Forty-eight percent of all Americans have a chronic condition; 87% of Medicare beneficiaries have a chronic condition. Almost half of the people with chronic conditions have multiple chronic conditions (Partnership for Solutions, 2004). Disease management interventions that focus on single conditions including diabetes, coronary artery disease, or depression have been shown to improve control of that chronic condition (McAlister et al., 2001; Shojania et al., 2006). However, interventions focused on only one disease can seem fragmented to patients and are costly for health care systems to provide.
People with chronic disease are more likely to be depressed than people without chronic disease (Moussavi et al., 2007). Depressed people have a harder time managing disease-related, self-care strategies, such as medication adherence, smoking cessation, weight loss, or exercise (Katon et al., 2010; Lin et al., 2004); face a higher risk of disability and early death (Katon et al., 2005; Lin et al., 2010); have high personal health care costs; and use a high percentage of national health care resources (Partnership for Solutions, 2004). Since the majority of health care spending (83%) is used for the care of people with chronic conditions, there is a clear need to find effective interventions for enhancing the health of this population (Partnership for Solutions, 2004).
One way to help improve health and control health care costs of a population of depressed patients with chronic disease would be to focus on enhancing management of patients with natural clusters of diseases. Natural clusters of diseases are those that commonly occur together that have poor outcomes in usual care and that have similar treatment approaches. Coronary heart disease and diabetes have similar guideline-level recommendations and are prevalent and often cooccur in primary care patients. Additionally, both these disorders are associated with a high prevalence of coexisting depression, which adversely affects disease control and outcomes. Depression has been linked to: high cortisol levels, increased proinflammatory factors, lack of insulin sensitivity, and changes in autonomic nervous system homeostasis (Katon, 2003). Depression's psychobiologic effects and negative impact on adherence to self-care behaviors may lead to higher medical symptom burden, additive functional impairment (Katon et al., 2004; Lin et al., 2004; Ludman et al., 2004; Von Korff et al., 2005), increased risk of complications and mortality (Lin et al., 2010), and increased medical costs (Ciechanowski et al., 2000, Simon 2005).
It would seem logical that enhanced treatment of depression for patients with comorbid depression and diabetes would improve diabetes outcomes. However, in 3 previous randomized clinical trials that studied the effect of treatment of depression in people with diabetes, symptoms of depression improved, but control of diabetes (HbA1C), and quality of self-care activities were not changed (Ell et al., 2010; Katon et al., 2005; Williams et al., 2004). This article describes a new health services model that has been shown to improve quality of depression and medical care, disease control for depression and medical diseases, among patients with comorbid depression and diabetes and/or CHD with evidence of poor control of HbA1c, SBP and/or LDL levels (Katon et al., 2010).
METHODS
Setting
The TEAMcare Study was conducted in Group Health (GH) Cooperative, a large health maintenance organization in Washington State. The TEAMcare intervention was based in 14 GH primary care clinics in Western Washington.
Recruitment and randomization
Patients were recruited by using GH electronic medical records (EMR) data to identify patients with diabetes or CHD and markers of poor disease control (SBP >140, HbA1c ≥8.5, or LDL >130). Patients meeting these criteria were mailed a one-page screener that included a short mental health screening tool [the Patient Health Questionaire-2 (PHQ-2)] (Kroenke et al., 2003) and an invitation letter. This initial screen was followed by a second baseline interview for patients scoring ≥3 on the PHQ-2. This interview included a longer depression questionnaire, the PHQ-9 (Kroenke et al., 2001). Patients were required to have a score of ≥10 to be eligible for the trial. A total of 214 patients were randomized to the intervention or usual care. The development and methodologic challenges in the design of the TEAMcare study have been published in detail elsewhere (Katon et al., 2010).
Usual care
Primary care physicians (PCPs) of patients randomized to usual care were informed of a patient's PHQ-9 score, the presumptive depression diagnosis, and evidence of poor medical disease control. “Usual care patients”were asked to see their primary care physician for follow-up care.
TEAMcare INTERVENTION
This 12-month intervention aimed to improve disease control for both medical and psychological illnesses by focusing on patients with poor glycemic, blood pressure, or lipid control, and coexisting depression. This multicondition collaborative care management intervention was developed by synthesizing collaborative care for depression (Gilbody et al., 2006; Katon et al., 1995; Unützer et al., 2002), with chronic care model (Bodenheimer et al., 2002a, 2002b) and added a treat-to-target strategy initially developed for diabetes (Riddle et al., 2003).
This patient-centered intervention is integrated into primary care by applying one treatment approach across 3 chronic illnesses (CHD, diabetes, and depression). Disease-specific treatment recommendations combined Group Health evidence-based guidelines with the treat-to-target program for diabetes from the Kaiser Care Management Institute. Resources for TEAMcare can be find at http://teamcarehealth.org.
THE TEAMcare INTERVENTION TEAM
The TEAMcare team consisted of our patients, the TEAMcare Nurse Care Managers (TCM), the patient's PCP and that PCP's care team, and the TEAMcare consultants.
The patients
All of the TEAMcare patients had probable major depression (PHQ-9 ≥10), and all had one or more parameters of uncontrolled diabetes and/or coronary heart disease: SBP >140 mmHg, LDL >130 mg/dL and/or HbA1c at least 8.5%. All patients were ambulatory, spoke English, had adequate hearing (were able to have telephone conversations), and planned to continue GH enrollment for 12 months. Patients with psychiatric diagnoses of bipolar disorder, schizophrenia, or confusion that suggested dementia were excluded. A majority of TEAMcare patients were female (57%), white (75%), and middle aged (mean age 57.4); had had some college education (61%); and were employed (52%). Most of our TEAMcare patients had been treated at the same GH Primary Care Clinic for years and often were well known to their primary care teams. These patients were often viewed as having poor self-care skills and as being unlikely to follow-up with care suggestions.
The TEAMcare nurse care managers
At GH, use of the EMR is limited to staff working in established clinical settings. Because documentation in the GH EMR was an essential communication tool, all of our TCMs were chosen from nursing staff already working in GH Primary Care Clinics with full access to the EMR. All of the TCMs were registered nurses who had experience counseling medical patients in person and by phone. Most had many years of experience working with people with diabetes and all were well known to the PCPs and staff in the primary care clinics. In all, we used 1.75 full-time equivalents of nursing staff (3 part-time staff) with half-time nurses treating 30 to 40 patients per year. Study nurses were funded by the NIMH grant. During the intervention, we had turnover in nursing staff because of nurses being recruited to another position, having major surgery or moving out of the area.
TEAMcare nurses received a 2-day training course on depression management and behavioral strategies including motivational interviewing, behavioral activation and problem solving as well as training in glycemic, blood pressure, and lipid control. Reinforcement of TCM training and clinical skills also occurred weekly, with detailed case discussions during which the care of individual patients was reviewed and supervised by the TEAMcare physician consultants.
Prior to first TEAMcare visit, the TCM reviewed the patient's EMR, discussed the patient with the TEAMcare physician consultants, then followed up with the PCP to review the intervention, discuss the patient, and receive an initial patient management plan. Although the protocols allowed a focused discussion with the PCP about options for beginning treatment, the PCPs treatment choices were not limited by the protocols.
TEAMcare treat-to-target focus meant that TCMs were expected to help patients and their PCPs frequently titrate medications until treatment goals were reached, unless the patient's status precluded a change. Consistent change was expected until the patient reached their individual treatment goals.
The primary care physicians
All PCPs worked in GH Primary Care Clinics. All had access to evidence-based clinical guidelines for a variety of chronic conditions and chronic disease patient tracking systems. At the time this intervention started, most PCPs had worked with the GH EMR for at least 2 years. A number of the PCPs had participated in the previous collaborative care for depression studies [IMPACT (Unützer et al., 2002) or Pathways (Katon et al., 2004)] lead by the TEAMcare research group. Primary care physicians were initially consulted to prioritize patient's treatment goals, to direct subsequent treatment titration, and to specify needed laboratories and specialty consultations to help patients achieve treatment targets.
The TEAMcare consultants
The TEAMcare investigators developed this intervention and provided weekly caseload review with the TCMs. These TEAMcare clinician consultants included 2 psychiatrists, an internist, a family medicine physician, and a psychologist. Specialty consultations with a diabetologist and a cardiologist were available when patients had complex insulin management regimes or when patients had complicated cardiac presentations.
TEAMcare assessment of depression
The first patient visit with the TCM included screening for depression and other psychiatric illnesses. The focus of this visit was to begin to form a relationship with the patient and to provide a thorough assessment to enable the psychiatrist supervisors to suggest initial antidepressant regimes. The visit included assessment of:
Current status of depression (using the PHQ-9) and depression history,
Current or past use of antidepressants, family history of psychiatric disorders,
Psychosocial strengths and stressors, and
Screening for anxiety disorders and panic attacks.
Antidepressant treatment
After discussing the TEAMcare psychiatric consultant's antidepressant recommendations with the PCP, the TCM talked with the patient about the suggested antidepressant. The TCM(S) took particular care to describe timing of therapeutic effects and types and timing of side effects. A majority of TEAMcare patients were willing to try the medications suggested by their PCP and the TEAMcare psychiatrist supervisors. The usual antidepressant regimes suggested were:
Start citalopram or buproprion SR for patients who had not taken antidepressants previously;
Increase antidepressant dosage for persistently-depressed patients receiving subtherapeutic doses of antidepressant medicines;
Start buproprion SR, citalopram, or fluoxetine for patients who had received prior pharmacotherapy
Start citalopram for patients with coexisting anxiety;
Start buproprion SR for patients with moderate to severe neuropathy or sexual dysfunction; and
Change to venlafaxine XR for patients not responding to an SSRI and buproprion SR.
TEAMcare approach to enhancing medication adherence
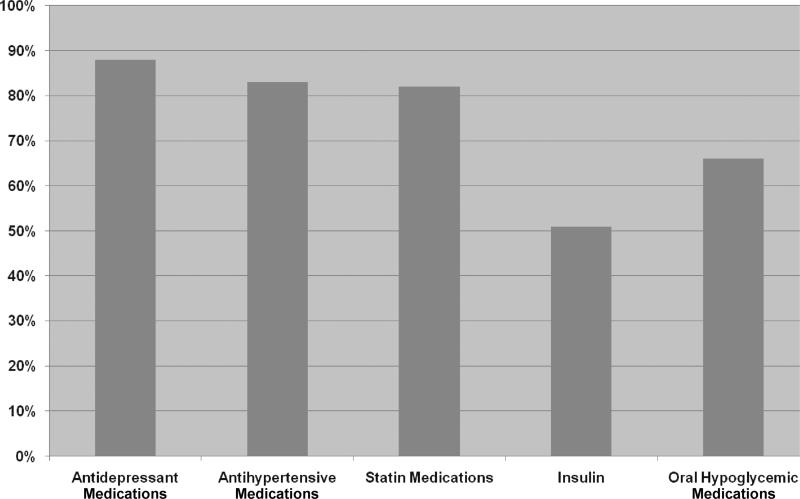
At every visit, TCMs reviewed medication regimens with patients to check how often they had managed to take each medication, to check if they were taking the ordered dosage, and to discuss any concerns or problems. The TCMs approach was to ask patients in a nonjudgmental way how often they miss doses: “I know it must be difficult to take all your medications regularly. How often do you miss taking them?”Figure 1 describes how frequently TCMs discussed medication adherence for each class of drugs.
Figure 1.
Percentage of patients with >1 discussion of medication adherence by medication class.
Many of the TEAMcare patients were taking at least 3 medications; most were taking 5 or more medications. To enhance medication self-management, TCMs worked to simplify dosage schedules, to tie taking medications to other daily tasks, or to eliminate medications. Whenever possible, patients were started on combination medications, like prinzide, that combined a diuretic and ACE inhibitor in one pill.
Most GH patients have insurance coverage for medications. However, even with coverage, copayments, and Medicare “doughnut hole” gaps often made affording all medications difficult. When patients mentioned concerns about costs, TCMs worked with them to make sure that medications were ordered in generic form and that they were ordered through a pharmacy that offered very low co-payments.
TEAMcare approach to pain assessment and treatment
Many TEAMcare patients had complaints of chronic pain. Pain can be exacerbated by depression and vice versa (Lin, 2003). Treatment plans included validation of the patient's pain, setting and review of specific goals for improving function, social reactivation, and self-pacing of activity. The primary pain medication recommended by TEAMcare was sustained-release acetaminophen taken on a regularly-scheduled basis.
Behavioral activation
Behavioral activation aimed to motivate patients, enhance disease self-management activities, increase social contacts and pleasurable activities, and facilitate decision-making. At each session, the TCM and patient discussed current functional status and worked together to design a practical, individualized, written plan to increase self-care activities. The TCMs used problem-solving techniques to help patients learn to effectively solve their own problems, thereby increasing the patient's confidence and self-efficacy.
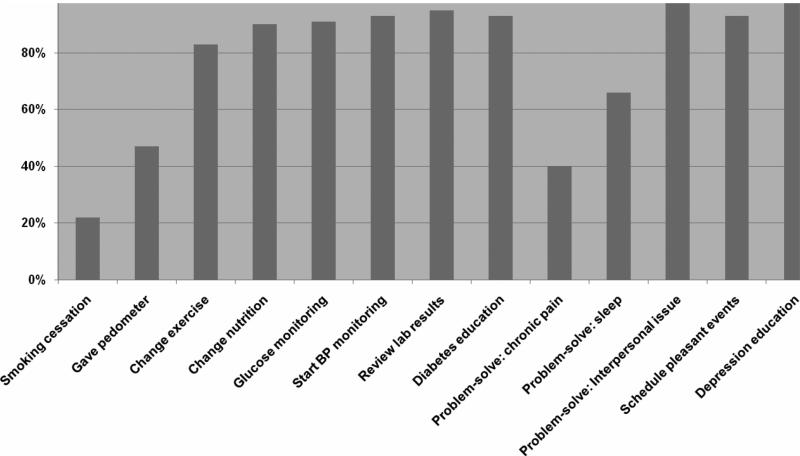
TEAMcare approach to self-care strategies
Figure 2 describes the percentage of patients receiving interventions to improve self-care, including medication adherence and self-monitoring. Patients often had a variety of conditions that could be monitored at home. Patients who were working to improve their blood pressure were given a blood pressure monitor and optimum blood pressure measurement technique and strategies for monitoring were discussed. Patients who were in an active phase of titration of antihypertensive medications often chose to check their blood pressure every morning. Patients could also email their providers with the home blood pressure readings and receive treatment adjustments.
Figure 2.
TEAMcare self-care interventions.
Patients with diabetes receive blood glucose meters and strips from GH. Nurses ensured that the glucose meters worked properly and that patients knew how to use them. The glucose meters readings could be transmitted to GH providers to provide a “glucose map” to help the patient see the change in readings over time. If the patient was in a phase of titration using metformin or evening NPH, they were encouraged to check fasting morning blood glucose. TCMs did not recommend checking readings 4 times a day unless the patient was on premeal fast-acting insulin or unless the patient was very motivated to check blood glucose readings.
Pleasurable activities
One of the hardest self-care behaviors for many of the TEAMcare patients to identify was a pleasurable activity. Depression can lead to an ever-tightening circle of withdrawal from social events, inactivity, and increased inertia to try anything. The notion of doing something for fun often seemed foreign. During the early visits, TCMs often used a list of pleasurable activities to help people review “fun” activities that they might be willing to try before the next visit.
Smoking cessation
When working with patients who smoked, a high priority goal was to help them quit smoking. Because frequent reminders about smoking have been shown to enhance smoking cessation, the TCMs asked about readiness to quit at most visits. If patients were interested in further discussion, TCMs used motivation techniques (creating ambivalence, realistic goal setting) to encourage change. Free and Clear, a smoking cessation program, was offered to patients who were interested.
Physical activity
Few TEAMcare patients had regular exercise programs that met the recommended 30 minutes of exercise on at least 5 days a week or 10 000 steps per day. Patients who were this active received verbal reinforcement related to its effect on their depression, disease risk and health, and our pride in their performance. Most patients were inactive. All inactive patients knew that they should exercise regularly, but felt that they could not manage to do it or could not imagine how to begin. A discussion with an inactive patient included checking for readiness to change and simple, practical plans for beginning exercise. Patients, who were interested, were given pedometers. Often the first task they chose was to wear a pedometer for a week to determine the average number of steps they took per day. The follow-up plan included increasing the average number of steps/day by 100 steps/day.
Healthy eating
Most TEAMcare patients were overweight and knew that they did not eat the recommended amount of vegetables, ate too much fat, and too much food. Most had been exposed to a variety of “diet plans” including the American Diabetes Association diet and carbohydrate counting. The majority found these structured complex plans overwhelming. For many, initial steps in their eating strategies were very basic—such as, not eating in the late evening or substituting water for the quart of juice they regularly drank. The TCMs emphasis was on diet strategies that had worked in the past, eating healthy foods, and limiting portion sizes and “unimportant foods” (high fat or sugar foods that were not important to the patient). When more complex diet plans, like carbohydrate counting, were appropriate and acceptable to patients, TCMs worked to help the patient learn to integrate the plans into their lives. However, the majority of our patients made improvements using simple strategies.
Treating insomnia
Many TEAMcare patients had some trouble getting to sleep or staying asleep. The TCMs primary interventions were behavioral. Discussion about good sleep hygiene and use of low dose trazodone were often tried.
TEAMcare care planning: my better health plan
TCMs and patients jointly filled out self-care goals and targets for improvement with input from their PCP (see Supplemental Digital Content Figures 3 and 4 available at http://links.lww.com/JACM/A4 My Better Health Plan).
TEAMcare care plans were designed to assure that:
Plans were individually tailored and emphasized patient control and choices.
Behavioral strategies and life-style changes were consistently reviewed and updated;
Treatment goals (PHQ-9, HbA1c, SBP, and lipid levels) were clear, congruent (ie, TCM, PCP, and patient shared the same goals), and regularly reviewed;
Collaborative self-monitoring goals for monitoring progress were clearly defined;
Clarification of the medication regimen and revising of the EMR's medication lists reflected what the patient was actually taking; and
The next appointment time was included.
TEAMcare patient education materials
TEAMcare patient education materials were limited, practical and focused on the same primary clinical outcomes. The materials included: The Depression Helpbook (Katon et al., 2003) and a patient pamphlet developed by the lead nurse and research team: Tools for Managing Your Chronic Disease.
TEAMcare visits
Patients were generally seen in person until the collaborative TCM-patient relationship was established and the patient was making progress toward their goals. Initial visit frequency was usually weekly. When patients were starting new, more complex insulin regimes, phone follow-up might occur between weekly visits. With established patients who were making progress toward goals, visit frequency was decreased to biweekly. Patients had access to the TCM's cell phones, but rarely chose to call between visits. During the 12-month intervention, the mean number of in-person visits was 10 and the mean number telephone visits was 10. (Most in-person visits occurred in the first 6 months, followed by monthly telephone contacts once the patient achieved treat-to-target goals. Patients were then prepared to transition back to care with their PCP team.)
Transition to maintenance care
We developed a priori parameters to guide transition from acute phase to maintenance and relapse prevention, phase. Once patients achieved targeted levels for relevant disease parameters, the TCM and patient developed a maintenance plan including behavioral goals and medication routines. The TCMs then followed patients with telephone calls every 4 to 6 weeks to complete a PHQ-9 and review disease control, medication adherence, and laboratory test results. Patients showing worsening of depression, hyperlipidemia, hyperglycemia, or blood pressure, were offered more frequent in-person or phone visits.
Relapse prevention
When patients had achieved their disease control goals for more than 1 month or when they were approaching the end of the year-long intervention, a relapse prevention plan was crafted with the patient. This plan was designed to identify:
Home measures (blood pressure or blood glucose) or laboratory measures (lipid levels or HgAlc) that met individual goals,
Prodromal symptoms associated with poor depression control;
Ordered dosage of medications and specific self-care activities such as exercising for 30 minutes every other day, and
Plans for “getting back on track.”
Returning patient to usual care
At the end of the intervention, EMR notes were written to the PCP describing the patient's initial and ending clinical status and self-care plans. The relapse prevention plan was also included in the EMR.
Care management information system
The TEAMcare research team developed an ACCESS-based care management tracking system to operationalize key elements of systematic chronic illness care such as proactive monitoring of outcomes, alerts for patients lost to follow-up, and highlighting patients who have not achieved their targets (Supplemental Digital Content Figure 5 available at http://links.lww.com/JACM/A4). Every week, TCMs captured the most current patient outcomes for PHQ-9, SBP, LDL or HbA1c, and average weekly blood glucose levels. A weekly clinical progress summary sheet displayed the earlier-mentioned disease control parameters for each patient. The ACCESS database supplemented the GH EMR.
Weekly caseload review
For TCMs, the weekly clinical review sessions were different than their previous practices. Initially, the TCMs described the degree of feedback as somewhat overwhelming. The team soon developed a style that was not threatening, helped inform patient care and was an efficient use of time. Each week, the TCMs met in a central location to discuss their patients with the TEAMcare caseload consultants. The priorities for supervision sessions were:
Newly enrolled patients, including a review of the EMR with a focus on depression and chronic disease risk,
Patients with persistent poor disease control,
Patients who have not been successfully contacted for a defined number of weeks,
Patients who were a concern to the TCMs or to the supervisors,
Patients who presented relationship challenges to the TCMs, and
Patients with PCPs who were more challenging to work with.
Nurses participated in weekly caseload reviews with a study psychiatrist, a consulting family medicine physician or internist, and a psychologist to review new cases and patient progress (behavioral and chronic disease control measures). The supervising physicians recommended initial choices and changes in medications tailored to patient history and clinical response, which the TCMs communicated to the patients’ PCPs, who decided on the treatment changes. Weekly supervision also offered a time to review aspects of behavioral intervention, relationship strategies, depression care, diabetes, or coronary heart disease management.
APPLICATION OF THE TEAMcare INTERVENTION
The following case demonstrates the practical application of this intervention with a study patient.
Mr. T. was an elderly appearing, married 64-year-old man. He was retired from long-term employment at a large aviation manufacturer and currently worked part-time at a marine parts store. When the TCM first saw Mr. T, his chief complaint was fatigue. At that time, his PHQ-9 score was 19 of 27 (diagnostic of moderate to severe major depression) and he had not felt well for more than 2 years. Other complaints included insomnia and difficulty concentrating. Mr. T. had diagnoses of type 2 diabetes, hypertension, hypothyroidism, psoriasis, and gout. His chronic disease measures demonstrated poor disease control: HbA1c = 9.6% and blood pressure = 174/94 mm Hg. Prescribed medications included: glyburide, NPH insulin, lisinopril, atenolol, atorvastatin, and levothyroxine. Mr. T. described his struggle managing diabetes self-care routines: he was not taking insulin as prescribed; he was obese (body mass index = 39.7 kg/m2), but unable to lose weight; and he had poor nutritional habits (skipping meals with associated hypoglycemic episodes, emotional eating, and eating high fat foods).
During the first visit, Mr. T. agreed to start taking citalopram 20 mg daily. During the following month, the citalopram dose was titrated to 60 mg daily. His depression improved (PHQ-9 score dropped to 14, but he was still bothered by sadness, trouble concentrating, and fatigue). Buproprion SR 100 mg daily was added to his antidepressant regime. Within 4 weeks, his PHQ-9 score dropped to 3.
At an early visit, Mr. T. agreed to begin taking the prescribed NPH insulin, began testing his blood glucose levels consistently, and began trying dietary and exercise interventions. After 3 months of intervention, Mr. T's HbA1c dropped to 6.9%. Mr. T also began monitoring his blood pressure with a home blood pressure cuff. His lisinopril dosage was titrated from 10 mg to 40 mg daily. At the end of the intervention, Mr. T had a PHQ-9 score of 0, an HbA1c of 6.1, and a blood pressure reading of 116/68.
CHALLENGES AND SUCCESSES OF THE TEAMcare CARE MANAGER ROLE
The TEAMcare nurse care manager role was different from any work that the TCMs had previously participated in during their extensive primary care experience. The principle differences were:
Treat-to-target focus: focused algorithm for care with medication titration plans;
Nurse, patient, and TEAMcare consultant accountability for reaching clinical treatment goals;
Focus on evidence-based interventions
Weekly caseload review with TEAMcare consultants.
Integrated multicondition disease management focus (depression, diabetes, and heart disease) rather than single disease, high cost or utilization focus; and
Focus on patient-centered care (ie, explicit patient control over goals, educational materials, and interventions chosen).
When the intervention began, TCMs had a number of concerns. First, all were concerned about their knowledge and skills related to depression. Initially, TCMs were overwhelmed by the number and variety of antidepressants, the indications and the side effects of each. In the first few months after the initial training and supervision sessions, each TCM gained a familiarity with the medications and focused on the several medications that were most commonly recommended. Other concerns about depression treatment were lack of confidence about motivational interviewing and behavior change techniques. Because the TCMs demonstrated interest in and concern about their patients, generally patients gave TCMs latitude when learning these skills. With practice and weekly supervision discussions, the TCMs became more facile with therapeutic communication and behavioral activation skills.
Clinical documentation was another challenge for the TCMs. All TCMs were capable users of the EMR. However, because the EMR did not include a tracking system that captured all outcome criteria and did not include a care plan, TCMs documented in both an ACCESS database and in the EMR. Initially, documenting in both systems took almost as much time as the first patient visits. Although TCMs became faster at using both documentation systems, double documentation remained a time-intensive process.
TEAMcare Nurse Care Managers were also challenged by remaining optimistic with some of the most treatment-resistant patients or by patients whose mental health issues, such as anxiety or irritability aroused adverse feelings in TCMs. Working with the psychiatrists and the psychologist helped the TCMs to consider other ways to approach patients and helped TCMs manage their own concerns.
Two of the TCMs had worked in primary care clinics as diabetes educators. These TCMs were concerned about seeing patients that they had previously seen but had been unable to help change their clinical outcomes. Both the TCMs and their previously seen patients were surprised by the difference in the interactions and outcomes with the addition of a patient-centered, motivational interviewing/behavior activation intervention, and initial focus on improving depression outcomes. In addition, focused patient-teaching materials, patient-centered care plans and intervention protocol were deemed helpful.
DISCUSSION
TEAMcare is a care management intervention that integrated collaborative depression care with systematic chronic illness care and treat-to-target interventions designed to improve multi-conditions (diabetes, depression, and coronary heart disease). Key components of the intervention are a patient-centered focus, collaborative goal setting, practical care planning, and consistent targeted patient educational materials. The TCMs work collaboratively with PCPs to enhance care by using treat-to-target interventions for each condition until disease control goals are reached.
Although the TEAMcare intervention targeted people with depression, diabetes and heart disease, it may be well suited to people with poorly controlled diabetes and heart disease and no coexisting depression. When screened, a number of these people would be found to have undiagnosed depression. For those without depression, a patient-centered, treat-to-target focus would help facilitate an organized, collaborative, and practical approach to care. The TEAMcare intervention has the potential to be widely adopted as a practical approach to managing multiple chronic diseases among patients with or without comorbid depression.
Supplementary Material
Acknowledgments
This study was supported by grants MH041739 and MH069741 from the National Institute of Mental Health Services Division, Bethesda, MD.
Footnotes
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.ambulatorycaremanagement.com).
REFERENCES
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Journal of the American Medical Association. 2002a;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. Journal of the American Medical Association. 2002b;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Archives of Internal Medicine. 2000;160(21):3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- Ell K, Aranda MP, Xie B, Lee PJ, Chou CP. Collaborative depression treatment in older and younger adults with physical illness: pooled comparative analysis of three randomized clinical trials. American Journal of Geriatric Psychiatry. 2010;18(6):520–530. doi: 10.1097/JGP.0b013e3181cc0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- Katon W, Lin EH, Von Korff M, Ciechanowski P, Ludman E, Young B, et al. Integrating depression and chronic disease care among patients with diabetes and/or coronary heart disease: the design of the TEAMcare study. Contemporary Clinical Trials. 2010;31(4):312–322. doi: 10.1016/j.cct.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W, Ludman E, Simon G. The Depression Helpbook. Bull Publishing Company; Boulder, CO: 2003. [Google Scholar]
- Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. Journal of the American Medical Association. 1995;273(13):1026–1031. [PubMed] [Google Scholar]
- Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry. 2003;54(3):216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- Katon WJ, Lin EHB, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. New England Journal of Medicine. 2010;363:2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon WJ, Lin EH, Russo J, Von Korff M, Ciechanowski P, Simon G, et al. Cardiac risk factors in patients with diabetes mellitus and major depression. Journal of General Internal Medicine. 2004;19(12):1192–1199. doi: 10.1111/j.1525-1497.2004.30405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28(11):2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- Katon WJ, Von Korff M, Lin EH, Simon G, Ludman E, Russo J, et al. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Archives of General Psychiatry. 2004;61(10):1042–1049. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–2160. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- Lin EH, Katon W, Von Korff M, Tang L, Williams JW, Jr, Kroenke K, et al. IMPACT Investigators Effect of improving depression care on pain and func tional outcomes among older adults with arthritis: a randomized controlled trial. The Journal of American Medical Association. 2003;290(18):2428–2429. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, et al. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33(2):264–269. doi: 10.2337/dc09-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludman EJ, Katon W, Russo J, Von Korff M, Simon G, Ciechanowski P, et al. Depression and diabetes symptom burden. General Hospital Psychiatry. 2004;26(6):430–436. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]
- McAlister FA, Lawson FM, Teo KK, Armstrong PW. Randomised trials of secondary prevention programmes in coronary heart disease: systematic review. British Medical Journal. 2001;323(7319):957–962. doi: 10.1136/bmj.323.7319.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Partnership for Solutions Chronic Conditions: Making the Case for Ongoing Care Johns Hopkins University and The Robert Wood Johnson Foundation. 2004 Available: http://www.partnershipforsolutions.org/November 30, 2010]
- Riddle MC, Rosenstock J, Gerich J. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26(11):3080–3086. doi: 10.2337/diacare.26.11.3080. [DOI] [PubMed] [Google Scholar]
- Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. Journal of the American Medical Association. 2006;296(4):427–440. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- Simon GE, Katon WJ, Lin EH, Ludman E, VonKorff M, Ciechanowski P, et al. Diabetes complications and depression as predictors of health service costs. General Hospital Psychiatry. 2005;27(5):344–351. doi: 10.1016/j.genhosppsych.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Jr., Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. Journal of the American Medical Association. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Von Korff M, Katon W, Lin EH, Simon G, Ludman E, Oliver M, et al. Potentially modifiable factors associated with disability among people with diabetes. Psychosomatic Medicine. 2005;67(2):233–240. doi: 10.1097/01.psy.0000155662.82621.50. [DOI] [PubMed] [Google Scholar]
- Williams JW, Jr., Katon W, Lin EH, Noel PH, Worchel J, Cornell J, et al. The effectiveness of depression care management on diabetes-related outcomes in older patients. Annals of Internal Medicine. 2004;140(12):1015–1024. doi: 10.7326/0003-4819-140-12-200406150-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.