Abstract
Drugged driving is a safety issue of increasing public concern. Using data from the Fatality Analysis Reporting System for 1999–2010, we assessed trends in alcohol and other drugs detected in drivers who were killed within 1 hour of a motor vehicle crash in 6 US states (California, Hawaii, Illinois, New Hampshire, Rhode Island, and West Virginia) that routinely performed toxicological testing on drivers involved in such crashes. Of the 23,591 drivers studied, 39.7% tested positive for alcohol and 24.8% for other drugs. During the study period, the prevalence of positive results for nonalcohol drugs rose from 16.6% in 1999 to 28.3% in 2010 (Z = −10.19, P < 0.0001), whereas the prevalence of positive results for alcohol remained stable. The most commonly detected nonalcohol drug was cannabinol, the prevalence of which increased from 4.2% in 1999 to 12.2% in 2010 (Z = −13.63, P < 0.0001). The increase in the prevalence of nonalcohol drugs was observed in all age groups and both sexes. These results indicate that nonalcohol drugs, particularly marijuana, are increasingly detected in fatally injured drivers.
Keywords: accidents, alcohol consumption, cannabinoids, drug users, motor vehicles, prescription drugs, safety, traffic
Over the past several years, popular media and traffic safety studies have increasingly recognized drugged driving as an important public health problem. From 2005 to 2009, nearly a third of fatally injured drivers in the United States tested positive for nonalcohol drugs (1). There is a growing body of evidence linking nonalcohol drugs, particularly cannabis, benzodiazepines, and stimulants, to deleterious driving performance, increased crash involvement, and crash culpability (2–7).
The time trends in drugged driving and the specific drugs involved are less clear, and findings from previous studies are inconsistent (1, 8–12). A study of US high school seniors from 2001 to 2006 did not find an increasing trend in driving under the influence of drugs or riding with a driver who used marijuana or other nonalcohol drugs (9). A more recent study of US high school seniors from to 2001 to 2011 found that the trend of driving under the influence of nonalcohol drugs was stable, whereas the prevalence of driving after marijuana use increased in recent years (12). Data from the National Survey on Drug Use and Health indicate that self-reported driving under the influence of illicit drugs in the United States declined slightly from 4.8% during 2002–2005 to 4.3% during 2006–2009 (11). Conversely, toxicological testing data suggest that the prevalence of involvement of nonalcohol drugs in fatal motor vehicle crashes has increased significantly in recent years (1, 13). Given the high prevalence and the increasing evidence of the hazards that nonalcohol drugs pose to driving safety, it is important to better understand the epidemiologic patterns of drugged driving. In the present study, we examined the time trends in alcohol and nonalcohol drugs detected in drivers who died within 1 hour of a motor vehicle crash in 6 states in the United States that routinely test such drivers for drugs.
METHODS
Data
Data for this study came from the Fatality Analysis Reporting System (FARS). This data system is maintained by the National Highway Traffic Safety Administration (Washington, DC) and is a census of fatal motor vehicle crashes occurring on public roadways in the United States. Fatalities include all deaths resulting from injuries within 30 days of a crash (13). The FARS data contain detailed information on the vehicles and individuals involved in the crash, as well as the crash circumstances (14). These data are acquired from police reports, state administrative files, and medical records by trained data analysts who use standardized protocols to extract pertinent information (14). Automated error checking and data monitoring ensure that data values fall within logical ranges (14). Data elements include driver characteristics, such as sex, race, and drug and alcohol test results. Although FARS has been recording testing results for nonalcohol drugs since 1991, drug testing was performed on only approximately 30% of fatally injured drivers nationwide (13, 14). A select number of states, however, have routinely tested fatally injured drivers for drugs (14, 15).
Study sample
The study sample consisted of drivers who died within 1 hour of a crash between January 1, 1999, and December 31, 2010, in 6 states that performed toxicological testing on more than 80% of their fatally injured drivers (California, Hawaii, Illinois, New Hampshire, Rhode Island, and West Virginia). Drivers who survived for more than 1 hour after the crash (n = 13,342) or with missing data on time of death (n = 638) were excluded from this study because of concerns about the accuracy and reliability of drug testing data for these drivers. Prolonged survival after the crash could introduce both false negatives and false positives into the postmortem drug testing results, because drugs taken before the crash might become undetectable due to metabolization, and drugs administered after the crash by medical personnel might be detected but indistinguishable from those taken before the crash. Of the 25,951 drivers in the study sample, 2,360 (9.1%) were excluded from the analysis because of a lack of drug testing data.
Drug testing assessments
Drug tests were performed on blood and/or urine specimens (14–16). Overall, 94.3% of the drug tests were based on blood specimens. The presence of up to 4 drugs, including alcohol, was recorded for each driver. When multiple drugs were reported, nonalcohol drugs were logged in the FARS data in the following priority order: narcotics, depressants, stimulants, marijuana, and other licit drugs (15–17). Drugs were categorized according to the FARS coding manual (17) and grouped into the following categories: alcohol, cannabinol, stimulant, narcotic, and depressant (exclusive of alcohol). Because of small numbers, drugs defined by FARS as hallucinogens, phencyclidine, anabolic steroids, inhalants, or “other” were combined and were referred to as “other drugs.” Drugs administered after the crash were not included (13, 17).
Statistical analysis
The prevalence of alcohol and other drugs detected in drivers who died within 1 hour of a crash was calculated by calendar year, driver characteristics, and drug class. Blood alcohol concentration was measured in grams per deciliter, and a blood alcohol concentration of 0.01 g/dL or greater was considered alcohol positive. Other drugs were categorized into the following 5 classes: narcotics, stimulants, cannabinol, depressants, and other drugs. The Cochran-Armitage test for trend was used to determine the statistical significance of trends in binomial proportions of the involvement of alcohol and other drugs over time. Data analyses were performed using SAS, version 9.3, software (SAS Institute, Inc., Cary, North Carolina) and Stata/SE, version 11.2, software (StataCorp LP, College Station, Texas).
RESULTS
Overall, 23,591 (90.9%) of the 25,951 drivers who died within 1 hour of a crash in these 6 states underwent toxicological testing. Drivers who were tested for drugs were similar in crash circumstances to those who were not tested, but they appeared to be slightly younger (mean age = 39.4 (standard deviation, 19.4) years vs. 43.4 (standard deviation, 27.7) years), more likely to be male (77.7% vs. 75.8%), more likely to be involved in nighttime crashes (51.4% vs. 47.0%), and more likely to have been involved in a crash in the previous 3 years (15.7% vs. 13.9%) than those who were not tested.
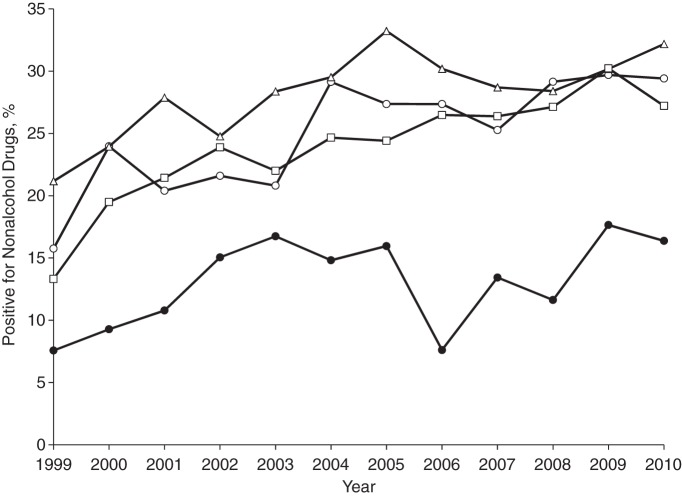
Of the 23,591 drivers tested, 39.7% were positive for alcohol, and 24.8% tested positive for other drugs. The prevalence of alcohol involvement was stable at approximately 39% from 1999 to 2010 (Z = −1.4, P = 0.16). Alcohol involvement was more prevalent in men (43.6%) than in women (26.1%), but trends were stable for both sexes (Table 1). In contrast, the prevalence of nonalcohol drugs showed a statistically significant increasing trend over the study period, rising from 16.6% (95% confidence interval (CI): 14.8, 18.4) in 1999 to 28.3% (95% CI: 26.0, 30.7) in 2010 (Z = −10.19, P < 0.0001). The prevalence rates of nonalcohol drugs and 2 or more nonalcohol drugs increased significantly over the study period in both sexes (Table 1). The prevalence of nonalcohol drug use increased significantly across all age groups (Figure 1).
Table 1.
Prevalence of Alcohol and Other Drugs in Drivers Who Died Within 1 Hour of a Motor Vehicle Crash by Drug Category and Sexa, Fatality Analysis Reporting System, Selected States, 1999–2010
| Drug Category | Men |
Women |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | Prevalence Difference | Z Statisticb | P Value | % | Prevalence Difference | Z Statisticb | P Value | |||||
| 1999–2002 (n = 5,924) | 2003–2006 (n = 6,747) | 2007–2010 (n = 5,656) | 1999–2002 (n = 1,743) | 2003–2006 (n = 2,017) | 2007–2010 (n = 1,503) | |||||||
| Any drug | 54.2 | 56.9 | 57.7 | 3.5 | −3.8 | 0.0002 | 38.3 | 41.0 | 46.0 | 7.7 | −4.4 | <0.0001 |
| Alcoholc,d,e | 43.5 | 43.6 | 43.7 | 0.2 | −0.3 | 0.77 | 26.5 | 24.7 | 27.7 | 1.2 | −0.7 | 0.51 |
| BAC 0.01–0.079 g/dL | 6.8 | 6.1 | 5.1 | −1.7 | 5.0 | 4.8 | 3.6 | −1.4 | ||||
| BAC ≥0.08 g/dL | 36.7 | 37.5 | 38.6 | 1.9 | 21.5 | 19.9 | 24.1 | 2.6 | ||||
| Nonalcohol drug | 21.3 | 26.8 | 27.0 | 5.7 | −7.1 | <0.0001 | 19.7 | 24.5 | 28.2 | 8.5 | −5.7 | <0.0001 |
| Cannabinol | 6.1 | 10.7 | 12.3 | 6.2 | −11.3 | <0.0001 | 2.8 | 5.9 | 7.5 | 4.7 | −5.9 | <0.0001 |
| Stimulant | 10.8 | 12.4 | 9.5 | −1.3 | 2.1 | 0.04 | 7.3 | 9.3 | 8.9 | 1.6 | −1.7 | 0.10 |
| Narcotic | 2.2 | 3.4 | 4.0 | 1.8 | −5.6 | <0.0001 | 4.3 | 5.0 | 7.6 | 3.3 | −4.0 | <0.0001 |
| Depressant (excluding alcohol) | 2.1 | 2.6 | 3.2 | 1.1 | −3.9 | 0.0001 | 3.6 | 3.9 | 4.8 | 1.2 | −1.8 | 0.08 |
| Other | 4.4 | 4.7 | 4.7 | 0.3 | −0.7 | 0.47 | 5.6 | 6.7 | 8.0 | 2.4 | −2.7 | 0.01 |
| Any alcohol and other drug(s) | 10.5 | 13.3 | 13.0 | 2.5 | −4.2 | <0.0001 | 8.0 | 8.1 | 9.9 | 1.9 | −1.9 | 0.06 |
| Two or more nonalcohol drugs | 4.5 | 7.3 | 7.3 | 2.8 | −6.2 | <0.0001 | 4.7 | 6.8 | 9.2 | 4.5 | −5.1 | <0.0001 |
Abbreviation: BAC, blood alcohol concentration.
a Excluding 1 driver with missing data on sex.
b Cochran-Armitage χ2 test for trend where the null hypothesis is no change over time.
c Alcohol corresponds to a driver having a BAC of 0.01 g/dL or greater.
d Data on BAC were missing for 55 men.
e Data on BAC were missing for 14 women.
Figure 1.
Prevalence of nonalcohol drugs in drivers who died within 1 hour of a crash by year and age group, Fatality Analysis Reporting System, selected states, 1999–2010. Unfilled circle, <25 years; unfilled triangle, 25–44 years; unfilled square, 45–64 years; filled circle, ≥65 years.
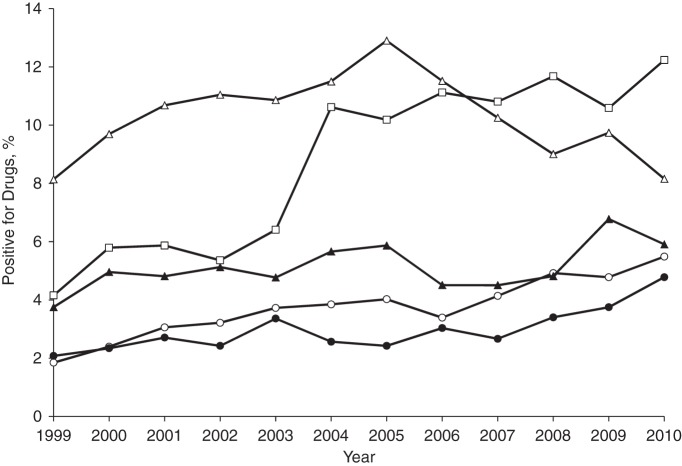
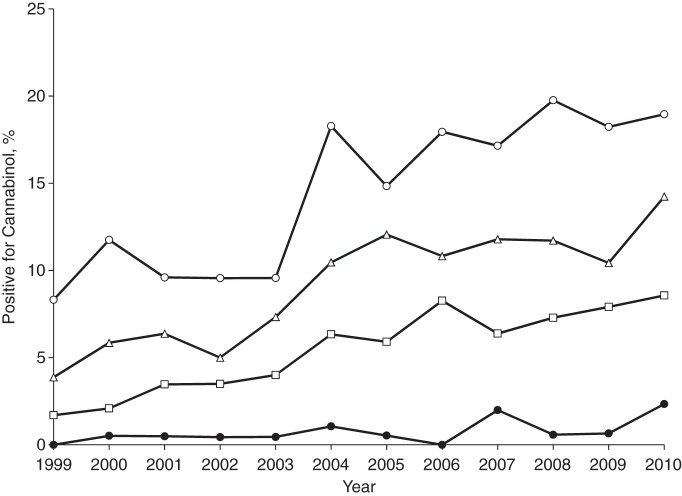
When time trends of nonalcohol drugs were examined by drug class, the prevalence of narcotics tripled during the study period, increasing from 1.8% in 1999 (95% CI: 1.3, 2.6) to 5.4% (95% CI: 4.4, 6.8) in 2010 (Z = −7.07, P < 0.0001, Figure 2), and the increase occurred in both sexes (Table 1). The prevalence of depressants (excluding alcohol) and other drugs also increased significantly over the study period (Z = −4.54, P < 0.0001, and Z = −2.61, P = 0.01, respectively). There was not a monotonic trend in the prevalence of stimulants during the study period (Figure 2). Overall, the prevalence of cannabinol nearly tripled over the study period, increasing from 4.2% (95% CI: 3.3, 5.2) in 1999 to 12.2% (95% CI: 10.6, 14.1) in 2010 (Z = −13.63, P < 0.0001, Figure 2), and the upward trends in the prevalence of cannabinol were similar for men and women (Table 1). By the end of the study period, cannabinol became the most prevalent nonalcohol drug detected in fatally injured drivers (Figure 2). The prevalence of cannabinol increased significantly across age groups (Figure 3). The increase in the prevalence of cannabinol was most pronounced among fatally injured drivers less than 25 years of age (Figure 3).
Figure 2.
Prevalence of drug involvement in drivers who died within 1 hour of a crash by year and drug category, Fatality Analysis Reporting System, selected states, 1999–2010. Unfilled circle, narcotics; unfilled triangle, stimulants; unfilled square, cannabinol; filled circle, depressants (excluding alcohol); filled triangle, other drugs.
Figure 3.
Prevalence of cannabinol involvement in drivers who died within 1 hour of a crash by year and age group, Fatality Analysis Reporting System, selected states, 1999–2010. Unfilled circle, <25 years; unfilled triangle, 25–44 years; unfilled square, 45–64 years; filled circle, ≥65 years.
DISCUSSION
The results of this study indicate that nonalcohol drugs have been increasingly detected in fatally injured drivers in recent years, whereas the prevalence of alcohol has remained stable at approximately 39%. These findings are important because increased crash risk has been linked to several psychoactive substances (8, 18–21). A recent case-control study found that, relative to drivers using neither alcohol nor drugs, drivers with positive blood alcohol concentrations were 13 times as likely to be involved in a fatal crash, and drivers testing positive for nonalcohol psychoactive drugs were twice as likely to be involved in a fatal crash (22). Additionally, studies have found that the use of nonalcohol drugs is associated with increased crash risk and crash culpability (23–27). In the current study, increases in the prevalence of narcotics and cannabinol detected in fatally injured drivers were particularly apparent. Although narcotic use has been found to be associated with impairments in driving performance and crash risk (8, 18–22, 28), trends in narcotic use have been understudied. Given that the annual number of opioid prescriptions rose from approximately 75 million to approximately 210 million from 1991 to 2010, and that narcotic use has been associated with poorer driving outcomes, understanding the role of controlled substances in motor vehicle crashes is of public health importance (29, 30). Stimulant use, particularly methamphetamine and amphetamine use, has been linked to more risk-taking behaviors (31, 32). The effect of stimulant use on driving safety is of special concern because prescriptions for stimulants have increased substantially in recent years (30, 33).
Several studies have noted an increased crash risk among drivers using cannabis (2, 6, 8, 22). An active ingredient in marijuana, δ-9-tetrahydrocannabinol, has been found to be associated with poorer driving performance, longer response times, and slower driving speeds in a dose-response fashion (34). In driving simulation studies, combined cannabis and alcohol use, even at low levels, was linked to greater impairment than use of alcohol or cannabis alone or the absence of both alcohol and cannabis (35). In addition, regular cannabis users had higher plasma concentrations of δ-9-tetrahydrocannabinol and poorer driving performance than nonregular users (35). Drivers using both alcohol and cannabis also had higher plasma concentrations of δ-9-tetrahydrocannabinol than drivers using cannabis alone (35).
Recent research has reported increased cannabis use by drivers in California from 2007 to 2010 (36) and increased marijuana use by patients treated in Colorado health care settings (37). The marked increase in the prevalence of cannabinol reported in the present study is likely germane to the growing decriminalization of marijuana. Over the last 17 years, 20 states and Washington, DC, have enacted legislation, and 4 more states have legislation pending, to decriminalize marijuana for medical use (38, 39). Although each of these states has laws that prohibit driving under the influence of marijuana, it is still conceivable that decriminalization of marijuana may result in increases in crashes involving marijuana. Three of the states assessed in our study enacted laws permitting medical marijuana use; California in 1996 (implemented in 2004), Hawaii in 2000, and Rhode Island in 2006. In the present study, the rise in the prevalence of detected cannabinol was particularly pronounced from 2003 to 2004 and is largely attributable to increases in cannabinol detected in California during this period. Although other studies have assessed the effects of state medical marijuana laws on adolescent marijuana use and report conflicting effects (40–43), studies of the effect of laws decriminalizing marijuana and state legislation permitting medical marijuana use on driving under the influence of marijuana and marijuana-involved crashes are scant (44). Nevertheless, a time-series analysis conducted by the California Department of Motor Vehicles (Sacramento, California) showed that the prevalence of cannabinoids in drivers in fatal crashes in California increased 2.1 percentage points—a 196% increase—from preimplementation to postimplementation of the medical marijuana law (44). In this report, statistically significant increases in the prevalence of detected cannabinoids were also found after implementation of medical marijuana laws in Hawaii and Washington state (44). Notably, this study found 1-time increases with the implementation of medical marijuana laws and not increasing trends (44).
Limitations
Although this study provides compelling evidence that the prevalence of nonalcohol drugs in fatally injured drivers has increased significantly since 1999, it is worth noting several limitations. First, this study is based on data from only 6 states, and the findings may not be generalizable to other states. To enhance the internal validity, we examined only data from states that consistently performed toxicological testing on fatally injured drivers who died within 1 hour of a crash. The prevalence of nonalcohol drugs reported in this study is higher than in other studies conducted in young drivers or non–fatally injured drivers (9, 11–12, 45). Second, the effects of drugs on driving performance and crash risk vary by drug type, dosage, and driver's physiological response and tolerance level. There is no universally accepted definition of drug impairment (46). Further, in this study, a positive drug test could represent an inactive drug metabolite resulting from past use. It is possible for a driver to test positive for cannabinol in the blood up to 1 week after use (47). Thus, the prevalence of nonalcohol drugs reported in this study should be interpreted as an indicator of drug use, not necessarily a measurement of drug impairment. Third, drug testing protocols may vary by state, and some states tested for fewer drugs than others (48–50). The variation in toxicological testing practices within the 6 states included in this study is likely minimal because these states have well-established statewide or regional medical examiner systems under which toxicological testing is performed using liquid-gas chromatography, mass spectrometry, and radioimmunoassay techniques following widely accepted forensic pathology procedures (51). The testing methods and specimens may not be exactly the same across the states. The possible bias resulting from different specimens, however, is unlikely to pose a serious threat to the validity of this study, given that 94% of the study sample had at least 1 test based on a blood specimen.
Conclusions
There has been a marked increase in the prevalence of nonalcohol drugs detected in fatally injured drivers in the United States between 1999 and 2010. During the study period, the proportion of fatally injured drivers testing positive for narcotics and cannabinol has tripled. These results suggest that drugged driving, specifically driving under the influence of cannabinol and narcotics, may be playing an increasing role in fatal motor vehicle crashes. To control the ongoing epidemic of drugged driving, it is imperative to strengthen and expand drug testing and intervention programs for drivers.
ACKNOWLEDGMENTS
Author affiliations: Department of Anesthesiology, College of Physicians and Surgeons, Columbia University, New York, New York (Joanne E. Brady, Guohua Li); Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York (Joanne E. Brady, Guohua Li); and Center for Injury Epidemiology and Prevention, Columbia University Medical Center, New York, New York (Joanne E. Brady, Guohua Li).
This research was supported in part by the National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention (grant 1 R49 CE002096) and by the National Institute on Drug Abuse (grant R21 DA029670) of the National Institutes of Health.
We thank Barbara Lang for her editorial and administrative assistance.
The contents of the manuscript are solely the responsibility of the authors and do not necessarily reflect the official views of the funding agency.
Conflict of interest: none declared.
REFERENCES
- 1.Brady JE, Li G. Prevalence of alcohol and other drugs in fatally injured drivers. Addiction. 2013;108(1):104–114. doi: 10.1111/j.1360-0443.2012.03993.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:E536. doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bogstrand ST, Gjerde H, Normann PT, et al. Alcohol, psychoactive substances and non-fatal road traffic accidents–a case-control study. BMC Public Health. 2012;12:E734. doi: 10.1186/1471-2458-12-734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dassanayake T, Michie P, Carter G, et al. Effects of benzodiazepines, antidepressants and opioids on driving: a systematic review and meta-analysis of epidemiological and experimental evidence. Drug Saf. 2011;34(2):125–156. doi: 10.2165/11539050-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 5.Dubois S, Bédard M, Weaver B. The impact of benzodiazepines on safe driving. Traffic Inj Prev. 2008;9(5):404–413. doi: 10.1080/15389580802161943. [DOI] [PubMed] [Google Scholar]
- 6.Li M-C, Brady JE, DiMaggio CJ, et al. Marijuana use and motor vehicle crashes. Epidemiol Rev. 2012;34(1):65–72. doi: 10.1093/epirev/mxr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rapoport MJ, Lanctôt KL, Streiner DL, et al. Benzodiazepine use and driving: a meta-analysis. J Clin Psychiatry. 2009;70(5):663–673. doi: 10.4088/JCP.08m04325. [DOI] [PubMed] [Google Scholar]
- 8.Kuypers KP, Legrand SA, Ramaekers JG, et al. A case-control study estimating accident risk for alcohol, medicines and illegal drugs. PLoS One. 2012;7(8):E43496. doi: 10.1371/journal.pone.0043496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O'Malley PM, Johnston LD. Drugs and driving by American high school seniors, 2001–2006. J Stud Alcohol Drugs. 2007;68(6):834–842. doi: 10.15288/jsad.2007.68.834. [DOI] [PubMed] [Google Scholar]
- 10.Orriols L, Queinec R, Philip P, et al. Risk of injurious road traffic crash after prescription of antidepressants. J Clin Psychiatry. 2012;73(8):1088–1094. doi: 10.4088/JCP.11m07624. [DOI] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The NSDUH Report: State Estimates of Drunk and Drugged Driving. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2012. [Google Scholar]
- 12.O'Malley PM, Johnston LD. Driving after drug or alcohol use by US high school seniors, 2001–2011. Am J Public Health. 2013;103(11):2027–2034. doi: 10.2105/AJPH.2013.301246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Highway Traffic Safety Administration. Traffic Safety Facts: Drug Involvement of Fatally Injured Drivers. Washington, DC: US Department of Transportation; 2010. (DOT HS 811 415) [Google Scholar]
- 14.National Highway Traffic Safety Administration. Fatality Analysis Reporting System Analytical Users Manual 1975–2011. Washington, DC: US Department of Transportation; 2012. (DOT HS 811 693) [Google Scholar]
- 15.Office of National Drug Control Policy. Drug Testing and Drug-Involved Driving of Fatally Injured Drivers in the United States: 2005–2009. Washington, DC: Office of the National Drug Control Policy; 2011. (HHSP 233-2009-5632 WC) [Google Scholar]
- 16.Kaplan J, Kraner J, Paulozzi L. Alcohol and other drug use among victims of motor-vehicle crashes—West Virginia, 2004–2005. MMWR Morb Mortal Wkly Rep. 2006;55(48):1293–1296. [PubMed] [Google Scholar]
- 17.National Highway Traffic Safety Administration. FARS Coding and Validation Manual 2009. Washington, DC: US Department of Transportation; 2010. (DOT HS 811 356) [Google Scholar]
- 18.Gjerde H, Normann PT, Christophersen AS, et al. Alcohol, psychoactive drugs, and fatal road traffic accidents in Norway: a case-control study. Accid Anal Prev. 2011;43(3):1197–1203. doi: 10.1016/j.aap.2010.12.034. [DOI] [PubMed] [Google Scholar]
- 19.Mathijssen R, Houwing S. The Prevalence and Relative Risk of Drink and Drug Driving in the Netherlands: A Case-Control Study in the Tilburg Police District. Leidschendam, Netherlands: SWOV Institute for Road Safety Research; 2005. (SWOV publication R-2005-9. 2nd ed.) [Google Scholar]
- 20.Movig KL, Mathijssen MP, Nagel PH, et al. Psychoactive substance use and the risk of motor vehicle accidents. Accid Anal Prev. 2004;36(4):631–636. doi: 10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- 21.Mura P, Kintz P, Ludes B, et al. Comparison of the prevalence of alcohol, cannabis and other drugs between 900 injured drivers and 900 control subjects: results of a French collaborative study. Forensic Sci Int. 2003;133(1-2):79–85. doi: 10.1016/s0379-0738(03)00052-5. [DOI] [PubMed] [Google Scholar]
- 22.Li G, Brady JE, Chen Q. Drug use and fatal motor vehicle crashes: a case-control study. Accid Anal Prev. 2013;60:205–210. doi: 10.1016/j.aap.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Gjerde H, Christophersen AS, Normann PT, et al. Associations between substance use among car and van drivers in Norway and fatal injury in road traffic accidents: a case-control study. Transp Res F Traffic Psychol Behav. 2013;17:134–145. [Google Scholar]
- 24.Haleem K, Gan A. Identifying traditional and nontraditional predictors of crash injury severity on major urban roadways. Traffic Inj Prev. 2011;12(3):223–234. doi: 10.1080/15389588.2011.557110. [DOI] [PubMed] [Google Scholar]
- 25.Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478–492. doi: 10.1373/clinchem.2012.194381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soderstrom CA, Dischinger PC, Kufera JA, et al. Crash culpability relative to age and sex for injured drivers using alcohol, marijuana or cocaine. Annu Proc Assoc Adv Automot Med. 2005;49:327–341. [PMC free article] [PubMed] [Google Scholar]
- 27.Romano E, Pollini RA. Patterns of drug use in fatal crashes. Addiction. 2013;108(8):1428–1438. doi: 10.1111/add.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strand MC, Fjeld B, Arnestad M, et al. Can patients receiving opioid maintenance therapy safely drive? A systematic review of epidemiological and experimental studies on driving ability with a focus on concomitant methadone or buprenorphine administration. Traffic Inj Prev. 2013;14(1):26–38. doi: 10.1080/15389588.2012.689451. [DOI] [PubMed] [Google Scholar]
- 29.National Institute on Drug Abuse. Prescription Drug Abuse. http://www.drugabuse.gov/publications/topics-in-brief/prescription-drug-abuse. Updated December 2011. Accessed November 27, 2013. [Google Scholar]
- 30.Volkow ND. Scientific Research on Prescription Drug Abuse. Statement Before the Subcommittee on Crime and Drugs of the Senate Judiciary Committee, 110th Congress, 2nd Session. .; http://www.hhs.gov/asl/testify/2008/03/t20080312a.html. Updated June 18, 2013. Accessed November 27, 2013. [Google Scholar]
- 31.Couper FJ, Logan BK. Drugs and Human Performance Factsheets. Washington, DC: National Highway Traffic Safety Administration; 2004. (DOT HS 809 725) [Google Scholar]
- 32.Romano E, Voas RB. Drug and alcohol involvement in four types of fatal crashes. J Stud Alcohol Drugs. 2011;72(4):567–576. doi: 10.15288/jsad.2011.72.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olfson M, Blanco C, Wang S, et al. Trends in office-based treatment of adults with stimulants in the United States. J Clin Psychiatry. 2013;74(1):43–50. doi: 10.4088/JCP.12m07975. [DOI] [PubMed] [Google Scholar]
- 34.Ronen A, Gershon P, Drobiner H, et al. Effects of THC on driving performance, physiological state and subjective feelings relative to alcohol. Accid Anal Prev. 2008;40(3):926–934. doi: 10.1016/j.aap.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 35.Downey LA, King R, Papafotiou K, et al. The effects of cannabis and alcohol on simulated driving: influences of dose and experience. Accid Anal Prev. 2013;50:879–886. doi: 10.1016/j.aap.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 36.Johnson MB, Kelley-Baker T, Voas RB, et al. The prevalence of cannabis-involved driving in California. Drug Alcohol Depend. 2012;123(1-3):105–109. doi: 10.1016/j.drugalcdep.2011.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richmond MK, Page K, Rivera LS, et al. Trends in detection rates of risky marijuana use in Colorado health care settings. Subst Abus. 2013;34(3):248–255. doi: 10.1080/08897077.2012.755146. [DOI] [PubMed] [Google Scholar]
- 38.ProCon.org. Medical Marijuana: 20 Legal Medical Marijuana States and DC. http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881. Updated September 16, 2013. Accessed November 27, 2013.
- 39.ProCon.org. Medical Marijuana: Four States with Pending Legislation to Legalize Medical Marijuana. http://medicalmarijuana.procon.org/view.resource.php?resourceID=002481. Updated August 21, 2013. Accessed October 4, 2013.
- 40.Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(3):207–212. doi: 10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 41.Wall MM, Poh E, Cerdá M, et al. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–716. doi: 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wall MM, Poh E, Cerdá M, et al. Commentary on Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(7):536–537. doi: 10.1016/j.annepidem.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013;103(8):1500–1506. doi: 10.2105/AJPH.2012.301117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guenzburger GV, Masten SV. Changes in Driver Cannabinoid Prevalence Associated with Implementing Medical Marijuana Laws in 14 US States. Elk Grove, CA: California Office of Traffic Safety; 2013. (Report No. CAL-DMV-RSS-13-242) [DOI] [PubMed] [Google Scholar]
- 45.Lacey JH, Kelley-Baker T, Furr-Holden D, et al. 2007 National Roadside Survey of Alcohol and Drug Use by Drivers: Drug Results. Washington, DC: National Highway Traffic Safety Administration; 2009. (DOT HS 811 249) [Google Scholar]
- 46.Voas RB, DuPont RL, Talpins SK, et al. Towards a national model for managing impaired driving offenders. Addiction. 2011;106(7):1221–1227. doi: 10.1111/j.1360-0443.2010.03339.x. [DOI] [PubMed] [Google Scholar]
- 47.Skopp G, Potsch L. Cannabinoid concentrations in spot serum samples 24–48 hours after discontinuation of cannabis smoking. J Anal Toxicol. 2008;32(2):160–164. doi: 10.1093/jat/32.2.160. [DOI] [PubMed] [Google Scholar]
- 48.Houwing S, Hagenzieker M, Mathijssen RPM, et al. Random and systematic errors in case-control studies calculating the injury risk of driving under the influence of psychoactive substances. Accid Anal Prev. 2013;52:144–153. doi: 10.1016/j.aap.2012.12.034. [DOI] [PubMed] [Google Scholar]
- 49.The Walsh Group. The Feasibility of per se Drugged Driving Legislation: Consensus Report. Bethesda, MD: The Walsh Group; 2002. [Google Scholar]
- 50.Walsh JM, de Gier JJ, Christopherson AS, et al. Drugs and driving. Traffic Inj Prev. 2004;5(3):241–253. doi: 10.1080/15389580490465292. [DOI] [PubMed] [Google Scholar]
- 51.Li L. Forensic pathology. In: Li G, Baker SP, editors. Injury Research: Theories, Methods, and Approaches. New York, NY: Springer; 2012. pp. 89–109. [Google Scholar]