Abstract
Acute liver cell failure can occur by diffuse infiltration of malignant cells in liver parenchyma. The malignant cells might be either primary hepatocellular carcinoma or metastatic liver disease. Mostly, CT abdomen with intravenous contrast fails to detect liver malignancy. We report a case of liver metastasis masquerading as fulminant hepatic failure.
Keywords: fulminant hepatic failure, liver cancer, liver transplantation
Abbreviations: CECT, contrast enhancing computed tomography; FHF, fulminant hepatic failure; HCC, hepatocellular carcinoma; IHC, immunohistochemical staining; INR, international standardized ratio; LT, liver transplantation
The interval between the onset of jaundice and altered sensorium in the background of normal liver, if it is less than 8 weeks, it is known as acute hepatic failure (AHF). AHF is a surgical emergency. AHF is often due to viral infection, toxins and drug-induced hepatotoxicity. Moreover, chronic liver diseases might also present like AHF due to acute flare (ex: autoimmune hepatitis, Wilson's disease). Very rarely, diffuse infiltration of malignant cells in liver parenchyma may cause AHF.
Case details
A 56-year-old lady was admitted with features of cholestatic jaundice and altered sensorium. There was no history of abdominal pain, edema legs, abdominal distension or bleeding diathesis. On examination patient was icteric, drowsy with mild alteration in sensorium. She was afebrile. There were no peripheral signs of chronic liver disease. On examination of the abdomen, liver and spleen were not palpable and there was no ascites. Cardiovascular and respiratory systems were normal. She had asterixis and was in grade II encephalopathy.
Investigations on admission included: hemoglobin 9.8 g/dL, total leukocyte count of 26 × 109/L, and platelet count 199 × 109/L; liver functions tests – total serum bilirubin 8.8 mg/dL, conjugated bilirubin 6.1 mg/dL, alanine aminotransferase 1118 IU/L, aspartate aminotransferase AST 3490 IU/L, alkaline phosphatase 190 IU/L, albumin 3.6 gm/dL, and international normalized ratio 2.28; serum lactate 7.1 mmol/L; serum creatinine 1.9 mg/dL; blood (aerobic and anaerobic) and urine cultures were sterile; serology tests for hepatitis A to E, human immunodeficiency virus (HIV) and dengue virus were negative; laboratory tests excluded copper, iron-related metabolic disorders and autoimmune liver disease and triple phase contrast-enhanced computerized tomography (CECT) was normal. Provisional diagnosis was fulminant hepatic failure (FHF); the etiology was not clear.
Despite supportive care in the liver intensive care unit, there was a progressive deterioration in the patient's general condition and she expired 2 days later.
Postmortem liver biopsy on hematoxylin and eosin study showed extensive hepatocyte necrosis and diffuse infiltration of the liver parenchyma with tumor cells (Figure 1). Immunohistochemistry was positive for cytokeratin 7 (Figure 2A) and cytokeratin 19-9 (Figure 2B); and negative for HEP-1 (Figure 3A) and CA 125 (Figure 3B). These markers are specific for a metastatic adenocarcinoma probably of pancreatico–biliary origin.
Figure 1.

Diffuse infiltration of metastatic adenocarcinoma (H & E stain).
Figure 2.
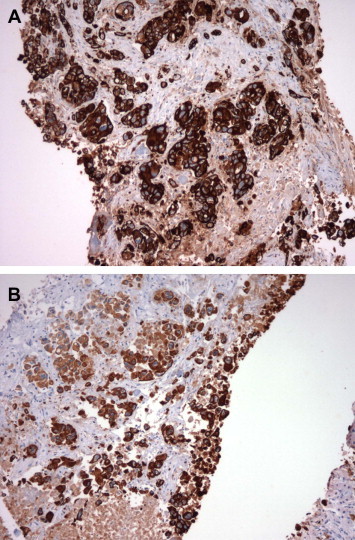
A and B: Immunohistochemistry CK 7, 19-9 positive in metastatic adenocarcinoma.
Figure 3.
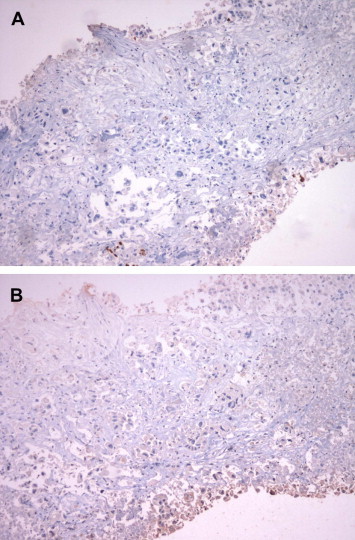
A and B: Immunohistochemistry negative for HEP-1 and CA 125.
Discussion
Metastatic liver disease masquerading as FHF is not uncommon. There are reports in literature of hematological1–7 and non hematological malignancies8–17 presenting as FHF. In a study of 4020 histological specimen of FHF, 0.44% showed evidence of a hematological malignancy.18 To our knowledge, there are no reports of liver metastasis of pancreatico–biliary origin presenting as FHF.
In the present case CECT failed to detect metastases within the liver. Similar observations of poor yield of CECT in diagnosis of hepatocellular carcinoma or metastatic liver disease in FHF have been reported.19–22 This may be partly related to the diffuse infiltration of the tumor cells due to loss of adhesion protein E-cadherin and CD 4422 or to a massive hepatocyte necrosis in FHF.
Isolated severe lactic acidosis has been reported as a prognostic marker in malignancies.23,24 In our patient we found a disproportionate rise in serum lactate levels compared to prothrombin time prolongation. We believe this observation may serve as a clue to predict malignancy-induced FHF.
The present case highlights the poor role of triple phase CECT in diagnosing metastatic liver disease in FHF. The disproportionate increase in serum lactate levels in comparison to degree of prothrombin time prolongation may have a role in diagnosis of metastatic liver disease presenting as FHF. Transjugular liver biopsy is recommended in select cases when liver transplant is being contemplated.
Conflicts of interest
All authors have none to declare.
References
- 1.Kader A., Vara R., Egberongbe Y., Height S., Dhawan A. Leukaemia presenting with fulminant hepatic failure in a child. Eur J Pediatr. 2004;163:628–629. doi: 10.1007/s00431-004-1510-1. [DOI] [PubMed] [Google Scholar]
- 2.Yasin M., Hartranft T.H. Primary hepatic lymphoma: unusual presentation and clinical course. Am Surg. 1997;63:951–953. [PubMed] [Google Scholar]
- 3.Vardareli E., Dündar E., Aslan V., Gülbaş Z. Acute liver failure due to Hodgkin’s lymphoma. Med Princ Pract. 2004;13:372–374. doi: 10.1159/000080477. [DOI] [PubMed] [Google Scholar]
- 4.Ghosh P., Fox I.J., Rader A.M. Fulminant hepatic failure as the initial manifestation of non-Hodgkins lymphoma. Am J Gastroenterol. 1995;90:2207–2209. [PubMed] [Google Scholar]
- 5.Morali G.A., Rozenmann E., Ashkenazi J., Munter G., Braverman D.Z. Acute liver failure as the sole manifestation of relapsing non-Hodgkin's lymphoma. Eur J Gastroenterol Hepatol. 2001;13:1241–1243. doi: 10.1097/00042737-200110000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Cofre P., Valera J.M., Smok G., Regonessi C., Brahm J. Fulminant liver failure associated with T-cell non-Hodgkin's lymphoma and hepatitis C virus: a case report. Gastroenterol Hepatol. 2006;29:542–545. doi: 10.1157/13094349. [DOI] [PubMed] [Google Scholar]
- 7.Padilla G.F., Garibay M.A., Hummel H.N., Avila R., Méndez A., Ramírez R. Fulminant non-Hodgkin lymphoma presenting as lactic acidosis and acute liver failure: case report and literature review. Acta Gastroenterol Latinoam. 2009;39:129–134. [PubMed] [Google Scholar]
- 8.Nieto Y., Alonso J.L., Ayala F. End-stage acute hepatic failure as clinical presentation of liver metastases from breast cancer. Tumori. 1998;84:616–617. doi: 10.1177/030089169808400523. [DOI] [PubMed] [Google Scholar]
- 9.Martelli O., Coppola L., De Quarto A.L., Palma M., Sarmiento R., Foggi C.M. Fulminant hepatic failure caused by diffuse intrasinusoidal metastatic liver disease: a case report. Tumori. 2000;86:424–427. doi: 10.1177/030089160008600512. [DOI] [PubMed] [Google Scholar]
- 10.Bilavsky E., Yarden-Bilavsky H., Stein G.Y., Fradin Z., Zeidmian A. Acute hepatic failure as a presenting sign of breast carcinoma. Harefuah. 2005;144:836–838. [PubMed] [Google Scholar]
- 11.Gilbert J., Rutledge H., Koch A. Diffuse malignant infiltration of the liver manifesting as a case of acute liver failure. Nat Clin Pract Gastroenterol Hepatol. 2008;5:405–408. doi: 10.1038/ncpgasthep1154. [DOI] [PubMed] [Google Scholar]
- 12.Iyaaki H., Ichikawa T., Taura N. Diffuse liver metastasis of small cell lung cancer causing marked hepatomegaly and fulminant hepatic failure. Intern Med. 2010;49:1383–1386. doi: 10.2169/internalmedicine.49.3296. [DOI] [PubMed] [Google Scholar]
- 13.Lanzas P., Alonso C., Guate O. Fulminant hepatic insufficiency caused by diffuse intrasinusoidal liver metastases in a patient with transitional-cell carcinoma of the bladder. Arch Esp Urol. 2002;55:547–551. [PubMed] [Google Scholar]
- 14.Alcalde M., Garcia-Diaz M., Pecellin J. Acute liver failure due to diffuse intrasinusoidal metastases of urothelial carcinoma. Acta Gastroenterol Belg. 1996;59:163–165. [PubMed] [Google Scholar]
- 15.Boyiadzis M., Nam M., Dahut W. Fulminant hepatic failure secondary to metastatic prostate cancer. Urol Int. 2005;74:185–187. doi: 10.1159/000083293. [DOI] [PubMed] [Google Scholar]
- 16.Shakir F.A., Madhoun M., Whorton J., Harty R. Metastatic prostatic carcinoma presenting as fulminant hepatic failure. South Med J. 2008;101:1049–1050. doi: 10.1097/SMJ.0b013e31817c74c3. [DOI] [PubMed] [Google Scholar]
- 17.Ales N.C., Daniels J.T., Frizell E.R., Koff J.M., Kaplan K.J., Wortmann G.W. Multiple myeloma-associated amyloidosis manifesting as fulminant hepatic failure. South Med J. 2001;94:1036–1038. [PubMed] [Google Scholar]
- 18.Rowbotham D., Julia W., Williams R. Acute liver failure secondary to hepatic infiltration: a single centre experience of 18 cases. Gut. 1998;42:576–580. doi: 10.1136/gut.42.4.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levy L.J., Swinburne L.M., Boulton R.P., Losowsky M.S. Primary hepatocellular carcinoma presenting as fulminant hepatic failure in a young women. Postgrad Med J. 1986;62:1135–1137. doi: 10.1136/pgmj.62.734.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mas M.R., Simsek I., Can C. Fulminant hepatic failure as the initial manifestation of primary hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2000;12:575–578. doi: 10.1097/00042737-200012050-00017. [DOI] [PubMed] [Google Scholar]
- 21.Silverstein N., Forouhar F., Rossi L. An unusual presentation of hepatocellular carcinoma: case report and review. Conn Med. 2005;69:133–138. [PubMed] [Google Scholar]
- 22.Allison Kimberly H., Fligner Corinne L., Parks W. Tony. Radiographically occult, diffuse intrasinusoidal hepatic metastases from primary breast carcinomas. Arch Pathol Lab Med. 2004;128:1418–1423. doi: 10.5858/2004-128-1418-RODIHM. [DOI] [PubMed] [Google Scholar]
- 23.Cheng J.C., Esparza S.D., Knez V.M., Sakamoto K.M., Moore T.B. Severe lactic acidosis in a 14-year-old female with metastatic undifferentiated carcinoma of unknown primary. J Pediatr Hematol Oncol. 2004;26:780–782. doi: 10.1097/00043426-200411000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Wall B.M., Mansour N., Cooke C.R. Acute fulminant lactic acidosis complicating metastatic cholangiocarcinoma. Am J Med Sci. 2000;319:126–129. doi: 10.1097/00000441-200002000-00011. [DOI] [PubMed] [Google Scholar]


