Adherence to rheumatoid arthritis (RA) medications varies widely but is frequently suboptimal1 and is particularly poor among racial/ethnic minority patients,2 which may help to explain the growing evidence of disparities in RA clinical outcomes.2 Beliefs about medications and self-efficacy perceptions (i.e., confidence) regarding medication taking behavior are two modifiable patient factors that have been associated with adherence to RA medications in largely Caucasian study samples.1 Minority RA patients report more negative medication beliefs and lower self-efficacy compared with Caucasians,3–5 but to our knowledge, the relationship between these psychological factors and medication adherence in these groups has not been reported.
We addressed this question in a cross-sectional study of 56 urban Hispanic and African American RA patients recruited consecutively from the waiting rooms of two NYU-affiliated rheumatology clinics in New York City (Bellevue Hospital and Hospital for Joint Diseases) between November 2012 and January 2013. All patients meeting the 1987 diagnostic criteria for RA who self-identified as Hispanic or African American were eligible. Analysis of clinic registry data (N=231) revealed that patients who participated were similar to the overall Hispanic and African American clinic populations with regard to age (P=0.40), gender (P=0.48), the proportion of Hispanic vs. African American patients (P=0.38), and disease activity (P=0.58). A research assistant administered the Morisky medication adherence scale (MMAS6), Beliefs about Medicines Questionnaire (BMQ7) and an RA-adapted version of the Medication Adherence Self-Efficacy Scale (MASES8) via patient interviews. Demographic, disease and treatment variables were collected via patient interview, chart review and clinical assessment.
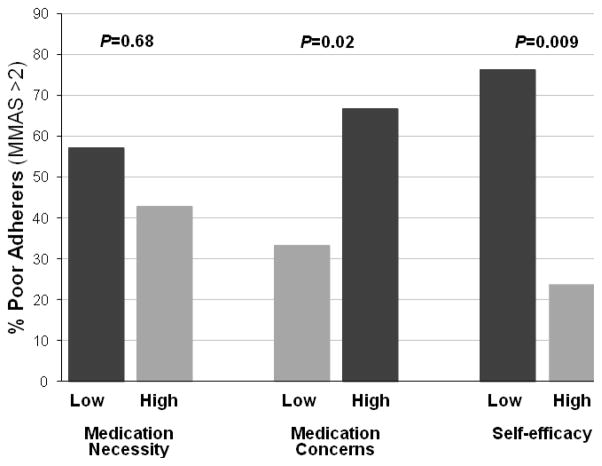
Sample characteristics are shown in Table 1. Figure 1 shows the relationship between medication beliefs and self-efficacy (dichotomized using median splits) and medication adherence. Twice as many patients with high vs. low medication concerns (66.7% vs. 33.3%, χ2=5.53, P=0.02) and three times as many patients with low vs. high self-efficacy (76.2% vs. 23.8%, χ2=6.91, P=0.009) were classified as poor adherers (MMAS>2)6. Belief in the necessity of RA medications was high but was not significantly related to adherence (P=0.68). Among the set of potential covariates in Table 1, only shorter disease duration and higher pain were associated with poorer adherence (Ps≤0.05). After adjustment for these covariates in a multivariable logistic regression analysis (N=50), higher medication concerns (P=0.04) and lower self-efficacy (P=0.007) each remained significantly and independently associated with poor medication adherence. Pain was marginally statistically significant in the multivariable model (P=0.08); disease duration was no longer significant (P=0.36).
Table 1.
Sample Characteristics
| Characteristic | % (N) | Mean ± SD | Range | N |
|---|---|---|---|---|
| Age (years) | 51.5 ± 12.8 | 21–73 | 56 | |
| Gender (female) | 89.3% (50) | 56 | ||
| Race/Ethnicity | 56 | |||
| Hispanic | 87.5% (49) | |||
| African American | 12.5% (7) | |||
| College educated | 32.1% (18) | 54 | ||
| Disabled a | 55.4% (31) | 56 | ||
| Medicaid | 64.3% (36) | 55 | ||
| Disease duration (years) | 15.4 ± 10.3 | 2–45 | 50 | |
| Methotrexate use b | 71.4% (40) | 56 | ||
| Methotrexate dose (mg) b | 16.6 ± 4.3 | 10–25 | 38 | |
| Any DMARD use b | 80.4% (45) | 56 | ||
| Biologic drug use b | 51.8% (29) | 56 | ||
| Corticosteroid use b | 33.9% (19) | 56 | ||
| NSAID use b | 8.9% (5) | 56 | ||
| Disease activity (CDAI) c | 17.0 ± 14.2 | 0–49.5 | 56 | |
| Remission/LDAS (CDAI ≤ 10) d | 42.9% (24) | 56 | ||
| Pain e | 5.1 ± 2.9 | 0–10 | 56 | |
| Comorbidities f | 0.8 ± 0.9 | 0–3 | 50 | |
| Medication adherence (MMAS) g | 2.2 ± 2.0 | 0–8 | 56 | |
| Poor adherence (MMAS>2) | 37.5% (21) | 56 | ||
| Medication beliefs: Necessity h | 4.2 ± 0.7 | 1.2–5.0 | 56 | |
| Medication beliefs: Concerns i | 3.1 ± 0.9 | 1.0–5.0 | 56 | |
| Self-efficacy j | 3.4 ± 0.4 | 2.4–4.0 | 56 |
Notes:
Based on patient-reported employment status.
All drug variables refer to current use.
CDAI=Clinical Disease Activity Index.
LDAS=low disease activity state.
Pain was rated on a 10-point visual analog scale.
Comorbidities include hypertension, diabetes, hypercholesterolemia.
MMAS=Morisky Medication Adherence Scale; higher scores indicate poorer adherence.
Mean scores range from 1 (strongly disagree) to 5 (strongly agree) where higher scores indicate greater belief in the necessity of RA medications.
Mean scores range from 1 (strongly disagree) to 5 (strongly agree) where higher scores indicate greater concerns about RA medications.
Mean scores range from 1 (not at all sure) to 4 (extremely sure) where higher scores indicate greater confidence in one’s ability to take RA medications.
Figure 1. Rates of poor adherence by medication beliefs and self-efficacy (N=56).
Medication beliefs and self-efficacy were each dichotomized using median splits. P values correspond to results of chi-squared tests.
These findings are consistent with previous studies in predominantly Caucasian samples1 but to our knowledge, ours is the first study to document these relationships in Hispanic and African American RA patients. Limitations of the present study include the cross-sectional design, small convenience sample and lack of objective adherence measures. Although the predictive validity of the MMAS has been demonstrated,6 the use of both RA therapies and painkillers complicates the assessment of adherence in this population. Larger studies are needed to confirm these findings and to explore the role of other possible contributors to poor adherence (e.g., economic, cognitive, cultural, psychosocial factors). Still, the associations we observed are consistent with prior research in both non-minority RA samples1 and minority patients with other chronic diseases,9,10 and the magnitude of these associations increases our confidence in the results. Given the sample studied, the generalizability of these findings may be limited; the relationship between medication beliefs and self-efficacy with adherence in other minority groups both within and beyond the U.S. should be explored.
In conclusion, high medication concerns and low self-efficacy are associated with poor medication adherence in urban Hispanic and African American RA patients and are promising targets for interventions to improve adherence and health outcomes in this population.
Acknowledgments
The authors thank Lucy Alvarado for her assistance with recruitment and data collection.
FUNDING
This study was supported in part by grant UL1 TR000038 from the National Center for the Advancement of Translational Science (NCATS), National Institutes of Health.
Footnotes
CONTRIBUTORS
TMS, JDG: study conception and design, data analysis and interpretation, drafting the article. GO, LRH, JP: data analysis and interpretation, critical revision of article. JS, PR: data acquisition and interpretation, critical revision of article. All authors gave final approval of the version to be published.
LICENSE FOR PUBLICATION
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd to permit this article (if accepted) to be published in ARD and any other BMJPGL products and sublicences such use and exploit all subsidiary rights, as set out in our licence (http://group.bmj.com/products/journals/instructions-for-authors/licence-forms).
COMPETING INTEREST
None declared
References
- 1.van den Bemt BJ, Zwikker HE, van den Ende CH. Medication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literature. Expert Rev Clin Immunol. 2012;8:337–51. doi: 10.1586/eci.12.23. [DOI] [PubMed] [Google Scholar]
- 2.McBurney CA, Vina ER. Racial and ethnic disparities in rheumatoid arthritis. Curr Rheumatol Rep. 2012;14:463–471. doi: 10.1007/s11926-012-0276-0. [DOI] [PubMed] [Google Scholar]
- 3.Constantinescu F, Goucher S, Weinstein A, et al. Understanding why rheumatoid arthritis patient treatment preferences differ by race. Arthritis Rheum. 2009;61:413–8. doi: 10.1002/art.24338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iren UT, Walker MS, Hochman E, et al. A pilot study to determine whether disability and disease activity are different in African-American and Caucasian patients with rheumatoid arthritis in St. Louis, Missouri, USA. J Rheumatol. 2005;32:602–8. [PubMed] [Google Scholar]
- 5.Kumar K, Gordon C, Toescu V, Buckley CD, Horne R, Nightingale PG, Raza K. Beliefs about medicines in patients with rheumatoid arthritis and systemic lupus erythematosus: a comparison bewteen patients of South Asian and White British origin. Rheumatology. 2008;47:690–7. doi: 10.1093/rheumatology/ken050. [DOI] [PubMed] [Google Scholar]
- 6.Morisky DE, Ang A, Krousel-Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7.Horne R, Weinman J, Haskins M. The Beliefs about Medicines Questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14:1–24. [Google Scholar]
- 8.Ogedegbe G, Mancuso CA, Allegrante JP, et al. Development and evaluation of a medication adherence self-efficacy scale in hypertensive African-American patients. J Clin Epidemiol. 2003;56:520–9. doi: 10.1016/s0895-4356(03)00053-2. [DOI] [PubMed] [Google Scholar]
- 9.Lewis LM, Schoenthaler AM, Ogedegbe G. Patient factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. J Clin Hypertens. 2012;14:250–5. doi: 10.1111/j.1751-7176.2012.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mann DM, Ponieman D, Leventhal H, et al. Predictors of adherence to diabetes medications: the role of disease and medication beliefs. J Behav Med. 2009;32:278–84. doi: 10.1007/s10865-009-9202-y. [DOI] [PubMed] [Google Scholar]