Abstract
Objective
To compare labor progression in twin vs singleton gestations.
Study Design
Retrospective review of electronic database created by Consortium on Safe Labor, reflecting labor and delivery information from 12 clinical centers 2002-2008. Women with twin gestations, cephalic presentation of presenting twin, gestational age ≥34 weeks, with ≥2 cervical examinations were included. Exclusion criteria were fetal anomalies or demise. Singleton controls were selected by the same criteria. Categorical variables were analyzed by χ2; continuous by Student t test. Interval censored regression was used to determine distribution for time of cervical dilation in centimeters, or “traverse times,” and controlled for confounding factors. Repeated-measures analysis constructed mean labor curves by parity and number of fetuses.
Results
A total of 891 twin gestations were compared with 100,513 singleton controls. Twin gestations were more often older, white or African American, earlier gestational age, increased prepregnancy body mass index, and with lower birthweight. There was no difference in number of prior cesarean deliveries, induction, or augmentation, or epidural use. Median traverse times increased at every centimeter interval in nulliparous twins, in both unadjusted and adjusted analysis (P < .01). A similar pattern was noted for multiparas in both analyses. Labor curves demonstrated a delayed inflection point in the labor pattern for nulliparous and multiparous twin gestations.
Conclusion
Both nulliparous and multiparous women have slower progression of active phase labor with twins even when controlling for confounding factors.
Keywords: labor curves, pregnancy, twins
The rate of multiple gestations has dramatically risen over the past 2 decades, due both to increasing maternal age and to the widespread use of assisted reproductive technologies (ART).1,2 With this increase in twin gestations comes an increased risk of morbidity to both mother and neonate; one important source of morbidity is cesarean delivery. According to Lee et al, a dramatic increase in cesarean delivery rates among twin gestations has been observed, rising from 53.4% to 75.0% between 1995 and 2008.3 Although some of the rise in cesarean rates could be from provider choice to forego labor altogether, those women undergoing induction of labor were also noted to have an increase in cesarean delivery from 26.3% to 32.5%.3
Because the inaugural paper in the 1950s, obstetricians have referred to the Friedman curves to define labor progression; but labor progress in twin gestations was not addressed in Friedman's original work.4,5 Recent published literature suggests a need for revised labor curves in the general obstetric population.6-8 This may be true for 2 different reasons. Our contemporary population and obstetric practice, such as the widespread use of epidural analgesia, may affect labor progress.7 Growing recognition for customized curves to fit specific situations, such as obese patients,9 may be warranted. Similarly, further understanding of labor progress and risk factors for labor abnormalities in twin gestations may help providers manage twin labor better and ultimately decrease the rate of cesarean delivery. The purpose of this work was to investigate labor patterns of twin gestations as compared with their singleton counterparts, when controlling for important factors that may impact labor progress.
Materials and Methods
We identified a retrospective cohort from the electronic database created by the Consortium on Safe Labor, reflecting labor and delivery information from 12 clinical centers (19 hospitals) and 9 American College of Obstetricians and Gynecologists (ACOG) US districts from 2002-2008 (most from 2005-2007).6,8,10 This observational study was designed to study contemporary labor and delivery practice across the country. It used 8 university affiliated hospitals, 9 community teaching hospitals, and 2 nonteaching hospitals, each selected by location, spanning the continental United States, and availability of electronic medical records. All births greater than 23 weeks were included in this database. Data extraction from the electronic medical records was performed from each center for maternal demographics, complete medical, surgical, and obstetric history, as well as maternal and neonatal outcomes. Further details regarding this study are provided elsewhere.8 This project was approved by the institutional review board at all participating institutions.
For our analysis, we included all women with twin gestations, cephalic presentation of presenting twin, gestational age ≥34 weeks, undergoing trial of labor. We defined a trial of labor as a gravida laboring with ≥2 cervical examinations. Exclusion criteria were presence of fetal anomalies or fetal demise. Singleton controls were selected by the same criteria. Maternal demographic variables were extracted from the database for both the study group of twin gestations and the control group of singletons. Maternal demographic variables collected included maternal age, gestational age at delivery, body mass index, and race. Information regarding cervical examinations and labor were also extracted and included cervical dilation and effacement, number of cervical examinations, induction or augmentation of labor, epidural usage, prior cesarean deliveries, and prior cesarean for failure to progress. Birthweight of singleton and the presenting twin was also extracted and included for analysis.
Categorical variables were analyzed by χ2 and continuous by the Student t test. Interval censored regression analysis was used to determine distribution of times to progress from 1 integer of cervical dilation in centimeters to the next, assuming log normal distribution, to estimate the duration of active phase labor. This centimeter by centimeter estimate of cervical dilation in labor was extrapolated from cervical examinations on admission and those subsequent examinations performed in labor. If 2 or more cervical examinations were available the data were included in this centimeter estimate, regardless of whether full dilation was reached or the mode of delivery. These “traverse times” were calculated as median and 95th percentiles. The median traverse times were then controlled for confounding factors, including birthweight of singleton and presenting twin, maternal age, race, gestational age at delivery, prepregnancy body mass index (BMI), admission dilation, and rates of cesarean delivery. We used repeated-measures analysis with eighth degree polynomial model to construct mean labor curves by parity and number of fetuses for those who ultimately progressed to 10 centimeters. This was done in the same fashion as Zhang et al6,8 with the curves using the starting point of time = 0 when the dilation reached 10 cm and the time calculated backward; after computation the axis was reverted to a positive value. Therefore, only those gravidas who reached full dilation, regardless of the delivery mode, were included in the labor curve analysis. Labor curves were constructed beginning at 4 centimeters to reflect current practice of many institutions not admitting patients until greater than 4 centimeters. P values were reported and statistical significance was defined as P < .05. SAS version 9.2 (SAS Institute, Cary, NC) was used for analysis.
Results
Of the total of 233,730 deliveries reviewed for eligibility, a total of 891 twin gestations met inclusion and exclusion criteria and were compared with 100,513 singleton controls (Figure 1). Table 1 depicts the baseline characteristics of twin and singleton gestations. Women with twin gestations were more often older (29.4 ± 6.5 vs 27.2 ± 6.2 years), white or African American, had delivery at earlier gestational age (36.5 ± 1.5 vs 39.1 ± 1.5 weeks), and increased prepregnancy BMI (26.0 ± 6.8 vs 25.1 ± 6.0 kg/m2). There was an almost 800 g greater birthweight in singletons compared with the presenting twins with mean weights 3326 ± 477 and 2567 ± 401 g, respectively. Table 2 compares labor and cervical examination characteristics of both groups. Singletons presented with more cervical dilation, however, there were no differences in effacement or number of examinations performed in labor. Eighty percent of singleton and 71% of twin gravidas had greater than 4 cervical examinations. Of note, there were no differences in number of prior cesarean deliveries, induction, or augmentation of labor, or epidural use between the 2 groups. When comparing cesarean births, twin gestations were almost twice as likely to have cesarean births (30.5% vs 16.1%); however, they were statistically less likely to be performed for failure to progress (P <.01).
Figure 1. Eligibility criteria.
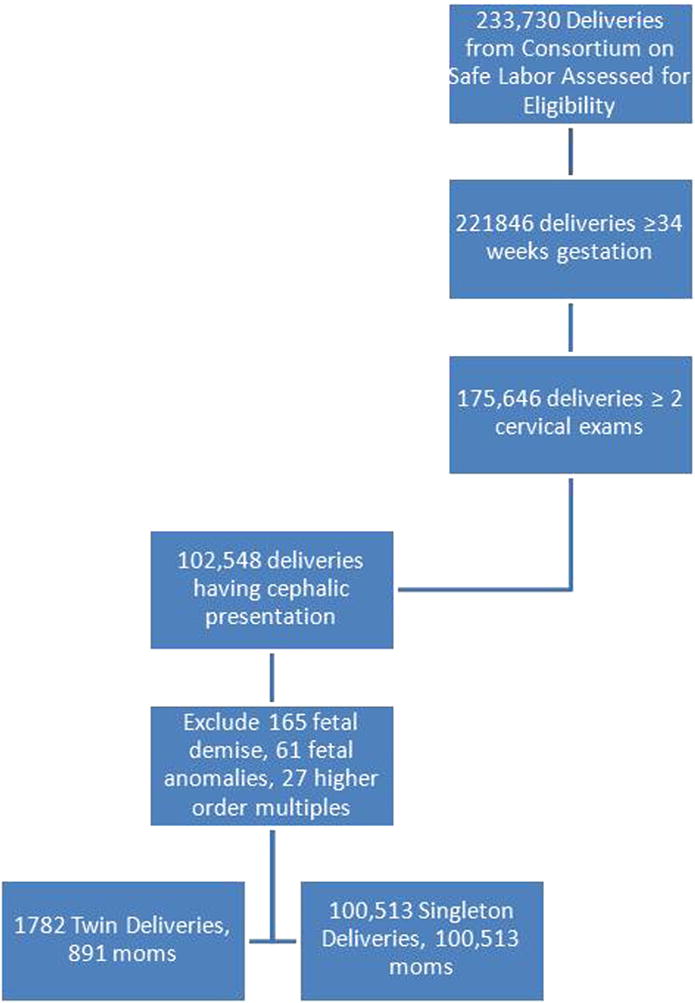
Table 1. Maternal demographicsa.
| Demographic | Singleton gestationb (n = 100,513) |
Twin gestationb (n = 891) |
|---|---|---|
| Maternal age, y | 27.2 ± 6.2 | 29.4 ± 6.5 |
| Gestational age, wks | 39.1 ± 1.5 | 36.5 ± 1.5 |
| Body mass index, kg/m2 | 25.1 ± 6.0 | 26.0 ± 6.8 |
| Race | ||
| White | 51.6 (49,297) | 57.1 (481) |
| African American | 23.5 (22,456) | 27.0 (227) |
| Hispanic | 16.8 (16,045) | 11.2 (94) |
| Asian/Pacific Islander | 5.0 (4808) | 2.1 (18) |
| Other | 3.0 (2872) | 2.6 (22) |
All P < .01;
Data expressed as mean ± SD or % (n).
Table 2. Labor characteristics.
| Characteristic | Singleton gestation (n = 100,513)a |
Twin gestation (n = 891)a |
P value |
|---|---|---|---|
| Induction | 39.8 (38,795) | 40.9 (355) | .53 |
| Augmentation | 31.7 (22,423) | 28.3 (172) | .08 |
| Epidural use | 79.6 (51,826) | 82.2 (462) | .13 |
| Cervical dilation, cm | 3.7 ± 2.4 | 3.3 ± 2.2 | < .01 |
| Cervical effacement | 75.3 ± 4.1 | 75.2 ± 23.3 | .95 |
| Number of cervical examinations | 7.1 ± 3.2 | 6.9 ± 3.6 | .13 |
| Prior CD | 6.2 (5804) | 7.3 (60) | .19 |
| CD | 16.1 (16,166) | 30.5 (272) | < .01 |
| Failure to progress as indication for CD | 47.5 (7683) | 25 (68) | < .01 |
| Neonatal birthweight, g | 3326 ± 477 | 2567 ± 401 | < .01 |
CD, cesarean delivery.
Data expressed as mean ± SD or % (n).
Labor progression was slower in the nulliparous twin gestations, as noted by greater median traverse times at every centimeter interval compared with singleton nulliparous pregnancies (Table 3), which continued to be the case when controlling for potentially confounding factors (Table 4). Similarly for multiparas, significantly increased median traverse times for twin gestations were noted centimeter by centimeter up to 7 centimeters in the unadjusted analyses (Table 3). From 7-10 cm, there were too few cervical examinations to evaluate median traverse times adequately, likely because of the rapid progress through these last few centimeters of dilation. A similar pattern was noted for multiparas in the adjusted analysis (Table 4). Labor curves demonstrate this same delayed labor progression for nulliparous twin gestations compared with singleton controls (Figure 2); for example nulliparous twins required 1 more hour than nulliparous singletons to complete the first stage of labor. There appears to be a lack of inflection point in the nulliparous twins, reflected also by their significantly longer traverse times. Multiparous twin labor curves revealed an even slower labor compared with multiparous singletons requiring approximately 2-3 hours more to complete the first stage of labor. However, an inflection point was evident for multiparous laboring women, both twin and singletons, at approximately 6.5 cm.
Table 3. Unadjusted duration of labor, singleton vs twin gestation (h).
| Cervical dilation, cm | Nulliparas | Multiparas | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Singleton gestationa | Twin gestationa | P value | Singleton gestationa | Twin gestationa | P value | |
| 3-4 | 4.8 (10.6) | 6.0 (11.9) | < .01 | 5.8 (12.3) | 7.7 (14.2) | < .01 |
|
| ||||||
| 4-5 | 3.5 (8.4) | 3.8 (8.6) | < .01 | 3.5 (8.1) | 4.4 (9.1) | < .01 |
|
| ||||||
| 5-6 | 2.4 (5.9) | 2.7 (6.2) | < .01 | 2.2 (5.6) | 2.6 (6.0) | < .01 |
|
| ||||||
| 6-7 | 1.7 (4.0) | 1.8 (4.1) | < .01 | 1.5 (4.2) | 1.6 (4.3) | < .01 |
|
| ||||||
| 7-8 | 1.3 (3.0) | 1.5 (3.2) | < .01 | 1.1 (3.0) | 1.1 (3.1) | —b |
|
| ||||||
| 8-9 | 1.2 (2.6) | 1.3 (2.7) | < .01 | 1.0 (2.6) | 1.0 (2.7) | —b |
|
| ||||||
| 9-10 | 1.2 (2.6) | 1.3 (2.8) | < .01 | 0.9 (2.3) | 0.9 (2.3) | —b |
|
| ||||||
| 4-10 | 8.8 (18.0) | 10.7 (20.0) | < .01 | 8.2 (17.4) | 9.7 (18.9) | < .01 |
Validity of the model fit is questionable.
Data expressed as median (95%);
Results shown are based on the last maximum likelihood iteration.
Table 4. Adjusted duration of labor, singleton vs twin gestation (h)a.
| Cervical dilation, cm | Nulliparas | Multiparas | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Singleton gestationb | Twin gestationb | P value | Singleton gestationb | Twin gestationb | P value | |
| 3-4 | 5.2 (11.2) | 6.4 (12.3) | < .01 | 7.6 (14.4) | 9.5 (16.2) | < .01 |
|
| ||||||
| 4-5 | 3.8 (8.9) | 4.4 (9.5) | < .01 | 4.2 (9.2) | 5.6 (10.6) | < .01 |
|
| ||||||
| 5-6 | 2.6 (6.4) | 3.3 (7.1) | < .01 | 2.5 (6.3) | 2.8 (6.6) | .07 |
|
| ||||||
| 6-7 | 1.8 (4.3) | 2.1 (4.6) | < .01 | 1.7 (4.6) | 2.0 (4.9) | .30 |
|
| ||||||
| 7-8 | 1.4 (3.2) | 1.6 (3.4) | < .01 | 1.3 (3.5) | 1.5 (3.7) | .90 |
|
| ||||||
| 8-9 | 1.3 (2.8) | 1.5 (3.0) | < .01 | 1.1 (2.9) | 1.2 (3.0) | .06 |
|
| ||||||
| 9-10 | 1.4 (2.9) | 1.6 (3.2) | < .01 | 1.0 (2.6) | 1.1 (2.8) | < .01 |
|
| ||||||
| 4-10 | 9.6 (18.4) | 12.7 (21.5) | < .01 | 10.0 (18.7) | 12.4 (21.2) | < .01 |
Data adjusted for birthweight of singleton and presenting twin, maternal age, race, gestational age at delivery, prepregnancy body mass index, admission dilation, and cesarean delivery;
Data expressed as median (95%).
Figure 2. Labor curves for singleton and twin gestations.
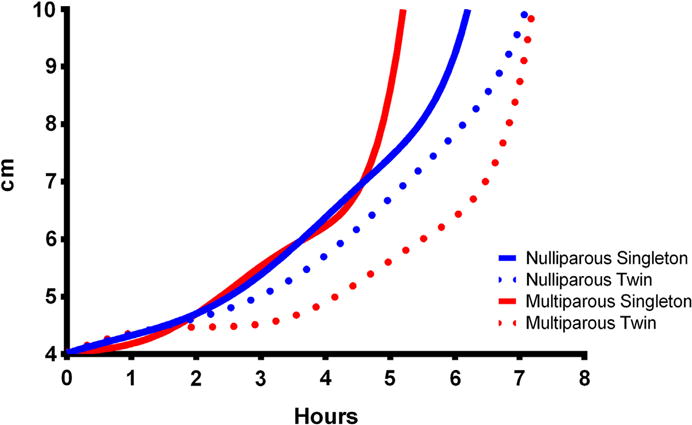
A comparison of labor curves for nulliparous and multiparous singleton (solid lines) and twin (dotted lines) gestations.
Comment
Our findings demonstrate that twin gestations labor more slowly than their singleton counterparts. This observation remained true when controlling not only birthweight but other confounding factors in both nulliparous and multiparous women. This finding is especially pertinent because the population of parturients studied represents a contemporary group of women, similar to those patients we currently care for on a day to day basis.
When evaluating previous work on labor progression in singleton vs twin gestations, the literature is sparse and contradictory. In support of our findings, Silver et al11 noted that twin active phase labor progressed slower than their singleton counterparts. This retrospective study was performed to evaluate labor in triplets gestations and comparing them with labor in twin and singleton gestations. They evaluated a total of 64 twin gestations matched to controls for gestational age, parity, and epidural use.11 They showed twin active phase dilation proceeds at a slower rate, 1.7 cm/hr vs 2.3 cm/hr in their singleton counterparts, estimating approximately 3.5 hours to progress from 4-10 centimeters; however, less than our median traverse time of 9.7 hours. Friedman also concurred with these findings in a later investigation of 184 twin gestations from 1956-1960, documenting shortened latent phase and lengthened active and second stage.12 He hypothesized that the shortened latent phase was secondary to the greater prelabor dilatation identified in his twin population. Of note, our twin gestation cohort had significantly less cervical dilation on admission but our conclusions remained similar in the active first stage of labor. Interestingly in our work multiparous twin gestations had similar inflection points in active labor to multiparous singleton gestations as noted by Zhang et al,8 although nulliparous twins and singletons did not.
In contrast to our findings, Schiff et al13 retrospectively reviewed 163 term twin gestations in spontaneous labor and found that twin gestations had a significantly shorter first stage of labor compared with their matched singleton control gestations. These women delivered from 1984-1996, similar in time to Silver et al,11 but many exclusion criteria resulted in a twin population quite different from our twin cohort, excluding women with oxytocin augmentation, delivery <37 weeks, birthweight <2500 g, diabetes or hypertension and short stature. To support these findings, they hypothesized that shorter labor may be a result of an overly distended uterus contracting more effectively than a less distended singleton uterus. This is refuted by earlier work done by Caldeyro-Barcia and Poseiro14 whose work on the physiology of the uterine contraction revealed that when the uterus is overstretched in cases of polyhydramnios, the uterine tone is abnormally elevated, however the intensity of contractions are decreased. As Silver et al examined a very small subset of twin deliveries and the above hypothesized mechanisms of longer labor are unproven theories, we chose to reexamine the labor patterns of twin gestations compared to singletons, controlling not only for birthweight but many other factors suggested to affect labor progression to adequately answer this specific question.
Our findings support the clinical suspicion that labor progression in twin gestations is prolonged compared with their singleton counterparts. Strengths of our investigation include the large number of twin gestations studied as our work included over 3 times more twin gestations than any of the aforementioned twin studies. Furthermore, in our study, we controlled not only for birthweight but also many other factors that may alter labor progression. In addition, this study was based on a modern population, representing women across the country who were older, had larger BMI, increased epidural and oxytocin use in comparison to studies done by Friedman 50 years ago. We also had fewer exclusion criteria, making these findings more generalizable.
We recognize limitations of our study including the use of a database designed to answer a different research question; however, the Safe Labor project was created to evaluate labor in a contemporary population, readily lending itself to a secondary analysis of twin labor. Other limitations might include the subjectivity of cervical examinations and the lack of uniform labor protocols. It is also important to recognize the possibility of selection bias, with provider choice on management of labor for twin gestations.
The impact of our work in defining longer duration of labor for twin gestations may be in the management of those trying to achieve a vaginal delivery. Ultimately, to adequately address whether implementation of this management would decrease cesarean delivery rates, a randomized controlled trial should be performed. However, until then, in the active phase of labor, allowing an additional 2-3 hours for nulliparous and multiparous twin gestations could possibly lead to fewer cesarean deliveries for failure to progress.
Acknowledgments
Supported by the Intramural Research Program, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through contract no. HHSN267200603425C; University of Illinois at Chicago (UIC) Center for Clinical and Translational Science (CCTS), award no. UL1RR029879 from the National Center for Research Resources.
Footnotes
The authors report no conflict of interest.
Presented at the 33rd annual meeting of the Society for Maternal-Fetal Medicine, San Francisco, CA, Feb 11-16, 2013.
Contributor Information
Heidi K. Leftwich, Division of Maternal-Fetal Medicine, University of Illinois at Chicago, Chicago, IL.
Mary N. Zaki, Department of Obstetrics and Gynecology, University of Illinois at Chicago, Chicago, IL.
Isabelle Wilkins, Division of Maternal-Fetal Medicine, University of Illinois at Chicago, Chicago, IL.
Judith U. Hibbard, Division of Maternal-Fetal Medicine, University of Illinois at Chicago, Chicago, IL.
References
- 1.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep. 2003;52:1–102. [PubMed] [Google Scholar]
- 2.Jewell SE, Yip R. Increasing trends in plural birth in the United States. Obstet Gynecol. 1995;85:229–32. doi: 10.1016/0029-7844(94)00354-g. [DOI] [PubMed] [Google Scholar]
- 3.Lee HC, Gould JB, Boscardin WJ, El-Sayed YY, Blumenfeld YJ. Trends in cesarean delivery for twin births in the United States. Obstet Gynecol. 2001;118:1095–101. doi: 10.1097/AOG.0b013e3182318651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Friedman EA. Labor: clinical evaluation and management. 2nd. New York: Appleton-Century-Crofts; 1978. pp. 30–6. [Google Scholar]
- 5.Friedman EA. The graphic analysis of labor. Am J Obstet Gynecol. 1954;68:1568–75. doi: 10.1016/0002-9378(54)90311-7. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J, Landy HJ, Branch W, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2009;116:1281–7. doi: 10.1097/AOG.0b013e3181fdef6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alexander JM, Sharma SK, McIntire DD, Leveno KJ. Epidural analgesia lengthens the Friedman active phase of labor. Obstet Gynecol. 2002;100:46–50. doi: 10.1016/s0029-7844(02)02009-4. [DOI] [PubMed] [Google Scholar]
- 8.Zhang J, Troendle J, Reddy U, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203:326.e1–10. doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kominiarek MA, Zhang J, Vanveldhuisen P, Troendle J, Beaver J, Hibbard JU. Contemporary labor patterns: the impact of maternal body mass index. Am J Obstet Gynecol. 2011;205:244.e1–8. doi: 10.1016/j.ajog.2011.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laughon SK, Branch DW, Beaver J, et al. Changes in labor patterns over 50 years. Am J Obstet Gynecol. 2012;206:419.e1–9. doi: 10.1016/j.ajog.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silver RK, Haney EI, Grobman WA, MacGregor SN, Casele HL, Neerhof MG. Comparison of active phase labor between triplet, twin, and singleton gestations. J Soc Gynecol Investig. 2000;7:297–300. [PubMed] [Google Scholar]
- 12.Friedman EA, Sachtleben MR. The effect of uterine over distention on labor. Obstet Gynecol. 1964;23:164–72. [PubMed] [Google Scholar]
- 13.Schiff E, Cohen SB, Dulitzky M, et al. Progression of labor in twin versus singleton gestations. Am J Obstet Gynecol. 1998;179:1181–5. doi: 10.1016/s0002-9378(98)70128-0. [DOI] [PubMed] [Google Scholar]
- 14.Caldeyro-Barcia R, Poseiro JJ. Physiology of the uterine contraction. Clinical Obstet Gynecol. 1960;3:386–408. [Google Scholar]


