Abstract
Presence of portosystemic collateral veins (PSCV) is common in portal hypertension due to cirrhosis. Physiologically, normal portosystemic anastomoses exist which exhibit hepatofugal flow. With the development of portal hypertension, transmission of backpressure leads to increased flow in these patent normal portosystemic anastomoses. In extrahepatic portal vein obstruction collateral circulation develops in a hepatopetal direction and portoportal pathways are frequently found. The objective of this review is to illustrate the various PSCV and portoportal collateral vein pathways pertinent to portal hypertension in liver cirrhosis and EHPVO.
Keywords: collateral pathways, portal hypertension, varices
Abbreviations: PSCV, portosystemic collateral veins; EHPVO, extrahepatic portal vein obstruction; PPCV, portoportal collateral vein; PV, portal vein; SV, splenic vein; SMV, superior mesenteric vein; AV, azygos vein; SRV, superior rectal vein; IRV, inferior rectal veins; GEV, gastroepiploeic vein; LGEV, left gastroepiploic vein; RGEV, right gastroepiploic; GV, gastric varices; DV, duodenal varices; LGV, left gastric vein; RGV, right gastric vein; PSPDV, posterior superior pancreatico duodenal vein; AIPDV, anterior inferior pancreatico duodenal vein; PIPDV, posterior inferior pancreatico duodenal vein; IPDV, inferior pancreatico duodenal vein; MCV, middle colic vein; ASPDV, anterior superior pancreatico duodenal vein; IVC, inferior vena cava; SVC, superior vena cava; SMV, superior mesenteric vein; IMV, inferior mesenteric vein; ERVP, extrinsic rectal venous plexus; IRVP, intrinsic rectal venous plexus; PHB, portal hypertensive biliopathy; PACD, paracholedochal; ECD, epicholedochal; CBD, common bile duct; GT, gastrocolic trunk; FJT, first jejunal trunk; LPV, left portal vein; CT, computed tomography; US, ultrasonography; PVT, portal vein thrombosis; PUV, paraumbilical vein; BCS, Budd–Chiari syndrome
Almost any vein in the abdomen may serve as a potential collateral channel to the systemic circulation. Presence of abnormal collateral vessels appears to be one of the most sensitive (70–83%) and specific sonographic signs for the diagnosis of portal hypertension.1 When blood flow through a vessel or a vascular bed is obstructed due to occlusion, as in EHPVO, or distortion, as in liver cirrhosis, collateral pathways open up as blood bypasses the occlusion or obstruction, always flowing down a pressure gradient from a high pressure to a low-pressure vessel or bed. The formation of portosystemic pathways occurs due to reopening of collapsed embryonic channels or reversal of the flow within existing adult veins.2,3 The number of collateral channels depends on the severity of portal hypertension i.e. the differential gradient driving the flow between the portal and the systemic circulations and the duration of portal hypertension. The more severe and more prolonged the portal hypertension, the higher are the number of portosystemic pathways. However, this traditional hypothesis has been challenged and it has been suggested that the formation of portosystemic collateral circulation may be due in part to angiogenesis driven by vascular endothelial growth factor.4,5
Almost 50 years have passed since the first detailed description of portosystemic collateral veins (PSCV) in portal hypertension appeared.6 Precise mapping of PSCV is essential to therapeutic decisions and multidetector computerized tomography (MDCT) is sometimes used for cartography of PSCV.7 EUS is increasingly being used for evaluation of PSCV and additionally provides an option for performing therapeutic interventions.8 In addition to PSCV, PPCV pathways are frequently found in extrahepatic portal vein obstruction (EHPVO). The objective of this review is to illustrate the various PSCV and PPCV pathways pertinent to portal hypertension in liver cirrhosis and EHPVO.
Normal portosystemic anastomoses
The left gastric vein (LGV) anastomoses with the esophageal veins, which in turn drain into the azygos vein (AV). The superior rectal vein (SRV) anastomoses with the middle and inferior rectal veins (IRV), which are, respectively, tributaries of the internal iliac and the pudendal veins. The paraumbilical vein (PUV) anastomoses with subcutaneous veins in the anterior abdominal wall. In the retroperitoneal region, tributaries of the splenic and pancreatic veins anastomose with the left renal vein. Short veins also connect the splenic and colic veins to the lumbar veins of the posterior abdominal wall. The veins of the bare area of the liver also communicate with those of the diaphragm, as well as the right internal thoracic vein.9
The direction of collateral flow
The direction of collateral flow is always to bypass the occluded portion of the vessel. When vascular obstruction is intrahepatic, collateral vessels drain away from the liver (hepatofugal collateral circulation). When the obstruction is extrahepatic, the collateral circulation usually develops toward the portal vein beyond the site of obstruction and thus drains toward the liver (hepatopetal collateral circulation). However in cirrhosis hepatopetal pathways can be present and in EHPVO hepatofugal pathways can be found.
Order of appearance of collateral
The vascular structure of the bowel wall is complex. There are intraepithelial channels, a superficial venous plexus, and deep submucosal and adventitial veins. In addition, perforating veins connect the adventitial and deep submucosal veins. Backpressure transmitted through the tributaries of the portal vein results in the engorgement of the collaterals outside the gut wall in a para-esophageal, para-gastric para-rectal or paracholedochal location.10–12 In turn, this is followed by dilatation of veins on the surface of the visceral wall in a peri-esophageal, peri-gastric or perirectal location. Presence of perforating veins allows the transmission of this backpressure to the ‘backwaters’ of the gut wall and results in the formation of varices in a submucosal or subepithelial location. These submucous veins are, thus, the first sites of ‘bloodlogging’ and become varicose before those upon the outer surface of esophagus in portal hypertension (Figure 1).13
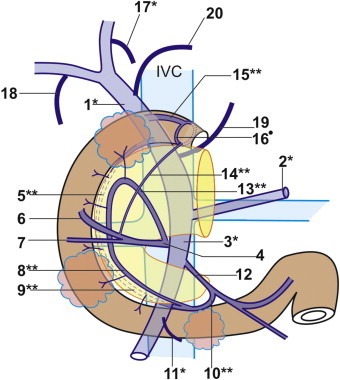
Figure 1.
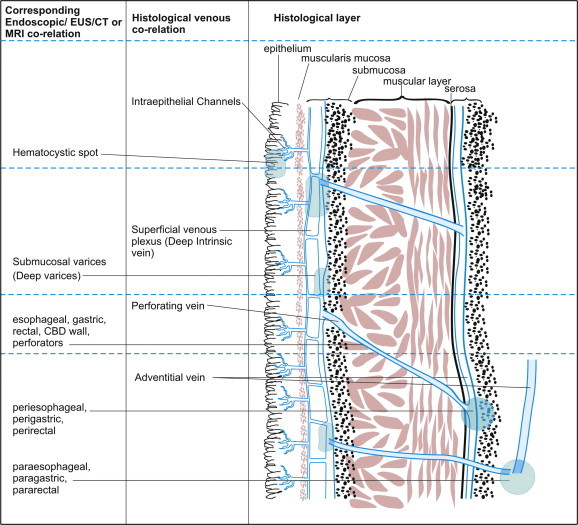
Venous anatomy in portal hypertension. Backpressure results in formation of varices on or outside the wall of the gut. The varices outside the wall are called para-in location and varices adjacent to the muscular layer are called peri-in location. From these locations the blood travels through the muscular layer via perforators to the deep intrinsic veins, which lie in submucosa. The hematocystic spots represent focal weakness on the variceal wall.
In patients with oesophageal varices dilated deep intrinsic veins displace the superficial venous plexus, assume a subepithelial position and are easily seen on endoscopy as the red color sign on varices i.e. telangiectasiae, cherry red spots, hemocystic spots and red wale markings or as the varices themselves. PSCV present in the peri-esophageal, peri-gastric and perirectal areas are easily seen by EUS.14–18 Veins on the mucosal aspect can cause gastrointestinal luminal bleeding and those outside the wall may cause extraluminal i.e. pleural or peritoneal bleeding.19,20
Classification of collateral pathways
The simplest classification of PSCV puts esophagogastric varices into one group and all other varices as ectopic varices. Ectopic varices are defined as large PSCV occurring anywhere in the gastrointestinal tract other than the esophagogastric region. Such ectopic varices are located predominantly in the duodenum, jejunum, ileum, colon, rectum, omentum, gallbladder, bile duct, uterus, vagina, diaphragm and urinary bladder and at enterostomy stoma and anastomotic sites.21 Some authors describe PSCV according to their drainage into either the superior vena cava (SVC) or the inferior vena cava (IVC).7
Esophageal varices
Venous Drainage of Esophagus
The venous drainage of thoracic esophagus to systemic veins occurs mainly through the azygos (AV) and hemiazygos venous system.22 The drainage to AV caudal to the arch of the AV occurs by eight to ten veins, which drain from right border of esophagus to join the medial aspect of AV. The veins on left side of esophagus drain into hemiazygos veins. Partial drainage of the esophagus also occurs into bronchial and pulmonary veins. The bronchial vein ultimately drains into AV or pulmonary veins. Direct drainage of esophagus also occurs into pulmonary veins.23 The venous drainage of abdominal esophagus occurs predominantly to the left gastric vein (LGV) a tributary of the portal venous system and partly to IVC via superior and inferior phrenic veins. Physiologically, the LGV drains the major part of the esophageal–cardiac area and a part of the fundic area before joining the portal vein. LGV has two branches.24 The anterior branch of LGV drains the cardiac region and the posterior branch terminates by joining the AV, the right posterior bronchial vein, or the venous plexus on the surface of the right bronchus. Para-esophageal veins are present on the side of esophagus and are connected with the posterior branch of the LGV (Figure 2).10,23,25
Figure 2.
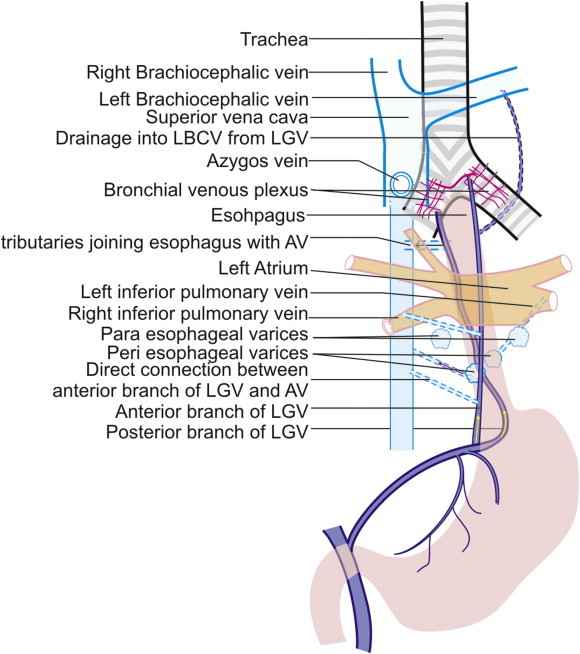
Efferents from esophageal varices. Posterior branch of LGV runs a spiral course on the posterior surface of esophagus to reach its right border close to right bronchus where it terminates by joining the azygos vein, the right posterior bronchial vein or the venous plexus on the right bronchus. The posterior branch can join the para-esophageal varices directly. The anterior branch of LGV can join the EVandGOV-1 located at cardia and terminates in the hemiazygous vein or the left posterior bronchial vein. The efferents of EV can drain into azygous vein, bronchial vein or pulmonary veins.
The Afferent to Esophageal Varices
In majority of cirrhotics, LGV is the afferent to esophageal varices (EV).
The Efferent from Esophageal Varices
-
1.
In 78% of cases, the LGV connects to the AV and SVC via esophageal and para-esophageal varices.
-
2.
In 12% of cases, they drain into IVC. Exceptionally, the LGV may anastomose directly with the IVC26
-
3.
LGV drains into AV and left brachiocephalic vein in an almost equal percentage. In a series of 324 cases, the drainage vein was the AV in 228 cases and the subclavian–brachiocephalic vein in 166 cases. Some cases had dual drainage27
-
4.
The channels between the LGV and the AV can have direct connections also and in such cases the flowing blood participates in formation of para-esophageal collaterals only without formation of EV
-
5.
The efferents of EV can drain into the pulmonary veins directly, more often on the left side. The bronchial and pulmonary veins are connected through preexisting bronchial venous plexuses. It has been speculated that tracheal and bronchial varices may develop through collateral channels, which normally exist between the tracheal and esophageal venous systems28–30
Gastric varices
Applied Anatomy and Venous Drainage of Stomach
Gastric varices (GV) are generally defined as cardiac or fundic according to their location. This location is consistent with the boundary line of portosystemic shunting.7 This area of shunting is mainly in posterior wall of the cardiac or the fundic area, which is fixed to the retroperitoneum and is the closest site to the systemic circulation. Isolated GV are related to gastroepiploic (GEV) veins and are located in body of stomach.31,32 As the esophagus pierces the diaphragm, several small esophageal veins join the superior and inferior phrenic veins, which drains the diaphragm and abdominal esophagus into the IVC.
The stomach drains either directly or indirectly into the portal vein as follows:
-
1.
Short gastric veins drain from the fundus to the splenic vein
-
2.
Left gastroepiploic vein (LGEV) moves along greater curvature to splenic vein
-
3.
Right gastroepiploic (RGEV) moves from the right end of greater curvature to superior mesenteric vein
-
4.
Left gastric vein moves from the lesser curvature of the stomach to the portal vein
-
5.
Right gastric vein moves from the lesser curvature of the stomach to the portal vein
The Afferents to Gastric Varices
The afferents to GV come from left gastric vein, short gastric veins and posterior gastric vein. Cardiac varices form from three to four submucosal branches of the anterior branch of the left gastric vein, which penetrate the gastric wall at the level of the cardia. These cardiac varices are contiguous with submucosal varices of the lower part of the esophagus (Figure 3).10,33
Figure 3.
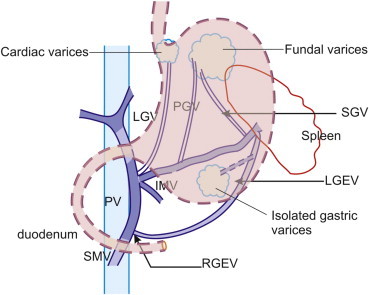
Afferents to gastric varices. The afferents to GV come from left gastric vein, short gastric veins and posterior gastric vein the left gastric vein mainly contributes to formation of cardiac varices whereas the short gastric vein and posterior gastric vein contribute to formation of fundal varices. Isolated gastric varices are more likely to be related to gastroepiploeic veins.
There are usually several short gastric veins. The short gastric veins course along the greater curvature on the medial side of the spleen to empty into the splenic vein.26 The posterior gastric vein is a distinct vein localized between the left and short gastric veins, which runs superiorly in the retroperitoneum and gastrophrenic ligament and joins GV.27
The Efferents from Gastric Varices
GV can enter systemic veins through several channels (Figure 4).
-
1.
In ∼84% of cases, they are connected to the superior vena cava via the esophageal varices.
-
2.
Majority of GV form the gastrorenal shunt (80–85% of cases) while 10–15% form the gastrocaval shunt.7 The gastrorenal shunt is formed mainly by lower branch of inferior phrenic vein, which can open into the renal vein directly (spleno-gastro-phreno-renal shunt) or via left adrenal vein. The gastrocaval shunt drains via the upper branch of inferior phrenic vein into IVC and is frequently contiguous with the phrenicopericardial vein.32,34–39 The communication with phrenicopericardial vein ultimately drains into brachiocephalic vein.39–41
-
3.
Rarely the GV can drain into azygos venous system via ascending lumbar vein, and vertebral plexus.
-
4.
The gastrorenal shunt can participate in formation of gastrogonadal collaterals as the left gonadal vein joins the lower border of left renal vein.34
-
5.
Direct splenorenal shunts constitute a direct communication between the splenic vein and the left renal vein, sometimes through the splenic capsule. This type of direct portosytemic shunting can be considered analogous to direct shunting of blood from posterior branch of LGV to para-esophageal veins and AV without formation of esophageal varices.34 Sometimes a direct shunt can exist between the spleen and adrenal vein bypassing the gastric area (spleno-adrenalo-renal shunt).
-
6.
Spontaneous, indirect splenorenal shunts; characterized by presence of a complete neurovascular pedicle traversing the gastrophrenic ligament can exist in some cases. In such cases the gastric collateral vein is connected to the left renal vein via the inferior phrenic vein and the middle capsular vein, and is called as ‘‘gastro-phreno-capsulo-renal shunt’’.42
-
7.
The GV located in fundus can sometimes communicate with and drain into hemiazygos vein but they rarely communicate with the azygos venous system.
-
8.
In patients with isolated GV, the main afferent venous drainage is via the posterior gastric or short gastric veins alone, and the efferent venous drainage is mainly via the gastric/splenorenal shunt and the inferior phrenic vein to the inferior vena cava.43
-
9.
In exceptional cases spleno-gonado-renal collateral vessels can drain from the splenic vein to the left renal vein via a gonadal vein.44
Figure 4.
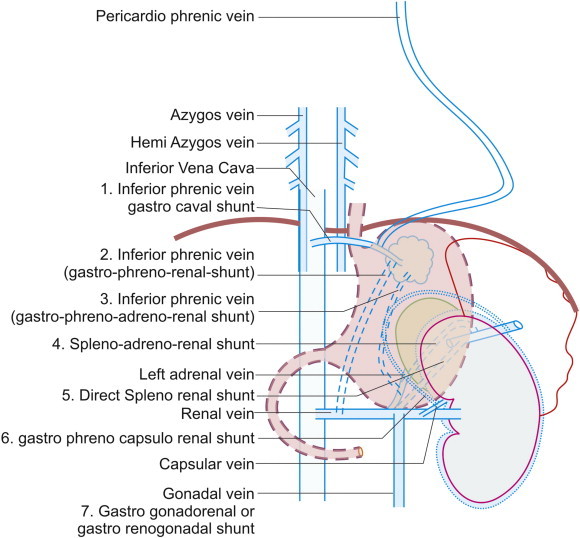
Efferents from gastric varices. The efferent of gastric varices can enter the superior vena cava via azygos venous system by continuing upwards as esophageal varices or by joining ascending lumbar veins. The drainage into inferior vena cava occurs by direct shunts or via one of the tributaries joining inferior vena cava (1). Commonly the gastric varices join the renal vein by the shunts shown in the figure (2, 3, 4, 5, 6 and 7). The left inferior phrenic vein can join the renal vein directly or via the adrenal vein. It can also go anteriorly to esophagus to join in IVC.
Ectopic varices in duodenum
Venous Drainage of Duodenum
Duodenal varices (DV) account for 1–3% of all varices in patients with portal hypertension.10 The rare occurrence of bleeding from DV, in contrast to esophageal varices, may be related to their smaller diameter, shorter length and deeper location on the outer wall of the duodenum (paraduodenal varices).45,46 The paraduodenal varices may enter through perforators into submucosa of the duodenum. After entering the submucosa they may be endoscopically inevident initially when they appear as thickened duodenal folds but generally become endoscopically evident before they bleed.
Main tributaries of portal venous system (portal vein, superior mesenteric vein and splenic vein) drain the duodenum and pancreas. Four small pancreatico duodenal veins drain the head of the pancreas and the adjacent second and third portions of the duodenum. The four veins regularly form an anterior and sometimes a posterior arcade through anastomoses between the superior and inferior veins. These anastomoses are usually small, although an arcade occasionally is as large as its draining veins. The superior veins are larger than the inferior veins and drain a larger portion of the head of the pancreas. The posterior superior pancreatico duodenal vein joins the portal vein. The anterior superior pancreatico duodenal and both the anterior and posterior inferior pancreatico duodenal veins are related either to superior mesenteric vein (SMV) or one of the two major tributaries of the SMV. The two major tributaries of the SMV are the gastrocolic trunk and the first jejunal trunk which join the SMV roughly at the same level but on opposite sides. This multiplicity of communications suggests that no one vessel is indispensable as a collateral pathway.47
The Afferents to Duodenal Varices
The afferents to DV are related to pancreatico duodenal venous arcades, which are in communication with portal venous system.48 The afferent channels for duodenal varices can be formed by any of the tributaries of portal venous system and the veins marked by stars (*) in Figure 5 have been demonstrated to act as afferent channels of duodenal varices pathway. The veins marked by two stars (**) represent sub-tributaries of main portal venous system tributaries that have been shown to act as afferent channels of duodenal varices pathway (Figure 5).14
Figure 5.
Venous drainage of duodenum and afferents to duodenal varices. 1. PV* = portal vein, 2. SV* = splenic vein 3. SMV* = superior mesenteric vein 4. GT = gastrocolic trunk 5. PSPDV** = posterior superior pancreatico duodenal vein 6. RGEV = right gastroepiploic vein 7. RCV = right colic vein, 8. AIPDV** anterior inferior pancreatico duodenal vein, 9. PIPDV** posterior inferior pancreatico duodenal vein, 10. IPDV** inferior pancreatico duodenal vein, 11. Middle colic vein* 12. Ist jejunal trunk 13. ASPDV** = anterior superior pancreatico duodenal vein, 14. Duodenal vein—subpyloric vein** 15. Duodenal vein—Suprapyloric vein** 16. Prepyloric vein of Mayo 17. Paraumbilical vein* 18. Cystic vein 19. Left gastric vein 20. Right gastric vein.  Duodenal varix.
Duodenal varix.
The Efferents from Duodenal Varices
The efferents from DV reveal two different patterns. In cirrhosis, they are formed in the descending or transverse parts of the duodenum and flow hepatofugally via retroperitoneal shunts (also called veins of Retzius) into the IVC via the following veins (Figure 6) 14:
-
1.
Right renal vein (mesenterorenal shunt)
-
2.
Gonadal vein (mesenterogonadal shunt)
-
3.
Lumbar veins
-
4.
Iliac vein
-
5.
Right suprarenal vein
-
6.
Right inferior phrenic vein
-
7.
Tributary of right renal vein–right inferior adrenal vein
Figure 6.
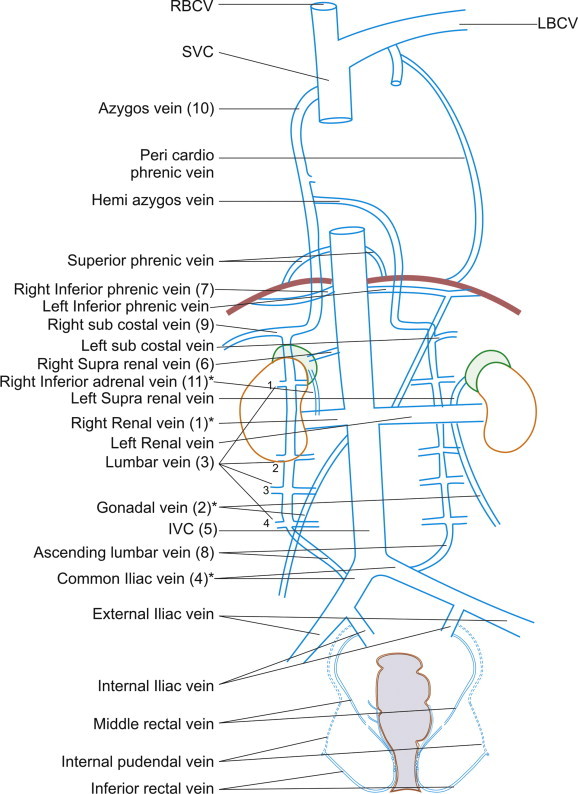
Efferents (hepatofugal) from duodenal varices. The efferent from DV can be hepatopetal or hepatofugal. The figure shows hepatofugal pathways from the duodenal varices which can go to following tributaries. 1. Right renal vein (mesentero renal shunt)* 2. gonadal vein (mesentero gonadal shunt)* 3. lumbar veins 4. iliac vein* 5. IVC = inferior vena cava, 6. right suprarenal vein 7. right inferior phrenic vein 8. Ascending lumbar vein 9. Right subcostal vein 10. Azygos vein 11. Tributary of right renal vein–right inferior adrenal vein*. The veins marked by stars (*) have been demonstrated to act as hepatofugal collaterals of duodenal varices.
Duodenal varices can also drain by subcostal vein and ascending lumbar vein into vertebrolumbar-azygos pathway and SVC (Figure 6).
Portoportal Efferents of Duodenal Varices
In extrahepatic portal vein obstruction (EHPVO) efferents of DV are formed in the duodenal bulb which flow hepatopetally via portoportal collaterals into the liver.14,49–52 Portoportal collaterals develop from either preformed venous plexuses near the common bile duct (CBD) or from the patent tributaries of portal vein above the occluded part of the portal venous system53 (Figure 7).
Figure 7.
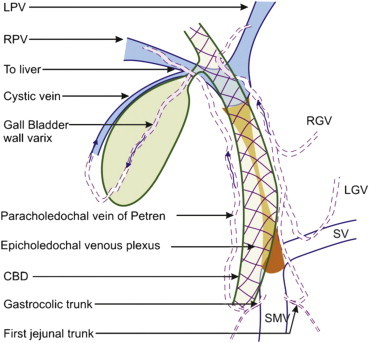
Para and pericholedochal collaterals. The hepatopetal collaterals use the venous plexus on or around the bile duct to reach liver. The venous drainage of the common bile duct is mostly by veins that ascend along the common bile duct and both hepatic ducts, forming an epicholedochal venous plexus of Saint, and enter the liver to break up into capillaries. Veins from the lower part apparently empty into the portal vein into paracholedochal venous plexus, which lies on the right and left side of common bile duct. The right-sided plexus can communicate with gastrocolic trunk (GT) and pancreatico duodenal vein to the cystic vein or directly to liver. The left sided plexus can communicate with first jejunal trunk (FJT), left and right gastric vein (LGV and RGV) and with the left portal vein (LPV).
Ectopic varices in small intestine
Venous Drainage of Jejunoileal Varices
Mesenteric collateral vessels may arise from the superior (SMV) and inferior mesenteric veins (IMV) and may ultimately drain into the IVC via the retroperitoneal or pelvic veins. Veins of Retzius are various veins in the dorsal wall of the abdomen forming anastomoses between the inferior vena cava and the superior and inferior mesenteric veins. Such anastomoses between the portal and the systemic venous system can exist even under normal conditions. Ibukuro et al identified veins of Retzius at CT arterio-portography in approximately similar proportions of patients with and without liver cirrhosis.49 In contrast to other portosystemic shunts, even in patients with portal hypertension the veins of Retzius are often not dilated and hence not well recognized. Various pathways of veins of Retzius are sometimes defined according to the receiving vein (mesenteric-gonadal, mesenteric-caval, mesenteric-renal or mesenteric-iliac.) An ileocolic vein draining into the IVC or the right renal vein through the right gonadal vein (mesenteric-gonadal varices) is the most frequently demonstrated pathway among the veins of Retzius. More rarely, anastomosis may occur with the left gonadal vein via a venous network developed from the inferior mesenteric vein.
Retroperitoneal shunts predominantly related to gastric and duodenal varices have been discussed in detail above. There are other retroperitoneal shunts where the tributaries of SMV can contribute as an afferent vessel to jejunal, ileal and colonic varices. The tributaries of IMV can make a major contribution toward formation of rectal varices.54,55
Jejunoileal varices are frequently associated with prior abdominal surgery. The development of these varices is often due to collateral circulation through postoperative adhesions between the jejunum or ileum and the abdominal wall. Adhesions tend to bring the parietal surface of the viscera in contact with the abdominal wall, and portal hypertension results in the formation of varices.
Afferents to Jejunal and Ileal Varices
Jejunal and ileal veins (tributaries of SMV).
Efferents from Jejunal and Ileal Varices
The efferents of small bowel varices generally drain into abdominal wall. They may also drain into veins of Retzius.25
Ectopic varices in large intestine
Applied Anatomy of Colonic and Rectal Varices
Colonic varices, are usually located in the cecum, and recto-sigmoid region. They are usually found in a segmental distribution and are often associated with cirrhosis or portal vein obstruction. Less common causes of colonic varices are congestive heart failure, mesenteric vein thrombosis, pancreatitis with splenic vein thrombosis, adhesions and mesenteric vein compression.56–58
Conventional EUS (7.5 or 12 MHz) reveals rectal varices as rounded, oval, or longitudinal echo-free structures in the submucosa and also shows perirectal veins outside the rectal wall. Sato et al demonstrated that intramural rectal varices, perirectal collateral veins, and the communicating veins between intramural rectal varices and perirectal collateral veins could be observed clearly via an ultrasonic microprobe.15,59–62
The right colon is drained by three tributaries of SMV, which include the ileocolic, right colic and middle colic veins. Tributaries joining inferior mesenteric vein drain the rest of the colon.
Venous drainage of rectum requires more detailed description as pelvic veins contribute to formation of two plexuses in the wall of rectum, the extrinsic and intrinsic venous plexuses (Figure 8).
Figure 8.
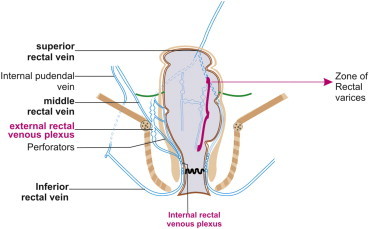
Afferents to rectal varices. The blood from superior rectal vein goes to extrinsic rectal venous plexus (ERVP). From the ERVP the blood flows into intrinsic rectal venous plexus (IRVP). The rectal varices are formed from the superior group of submucosal veins of IRVP.
Colonic Varices
Afferents to Colonic Varices
Following vessels can act as afferent:
-
1.
Ileocolic vein
-
2.
Right colic vein
-
3.
Middle colic vein
-
4.
Sigmoid colonic vein
Efferents from Colonic Varices
Efferents can drain into veins of Retzius, which include:
-
1.
Right gonadal vein
-
2.
Right renal vein
-
3.
Systemic lumbar veins
-
4.
A part of the veins of the ascending colon drain via the right renal capsular vein into the IVC.63
Rectal Varices
Afferents to Rectal Varices
Inferior mesenteric vein (IMV) continues as the superior rectal vein and acts as afferent to rectal varices. In a nation wise survey in Japan the most frequent afferent vessel was the inferior mesenteric vein, followed in order by the superior rectal vein.14 The blood from superior rectal vein goes to extrinsic rectal venous plexus (ERVP), which lies outside rectum below the level of peritoneal reflection. From the ERVP the blood flows by perforators through the muscularis propria into intrinsic rectal venous plexus (IRVP) which consists of two groups of veins – the superior group lying in the rectal submucosa and the inferior group lying in the corresponding anal subcutaneous tissue. The superior group of veins has a plexiform arrangement in the anal column where they form zone of internal hemorrhoids in the submucosa and pass up for a distance of about 10 cm above the pectinate line to form the superior rectal vein after piercing the muscular wall. The superior rectal vein provides the venous drainage of rectum in the upper part. The rectal varices are formed from this superior group of upper submucosal veins of IRVP. The inferior group of IRVP lying in the anal subcutaneous tissue passes down to form the inferior rectal vein and contribute to formation of external hemorrhoids60 (Figure 8).
Efferents from Rectal Varices
Rectal varices represent portal systemic collaterals that are manifested as discrete dilated submucosal veins and constitute a pathway for portal venous flow between the superior rectal veins of the inferior mesenteric system and the middle and inferior rectal veins of the iliac system. On IMV venography the blood in RV flows from superior rectal vein to middle and inferior rectal veins.64–66 In a nation-wide survey in Japan, it was reported that the efferent vessel for rectal varices included the internal iliac vein and the inferior rectal vein.14 In this series the hemodynamic profile was unknown in about 50% of cases with rectal varices. Portal hemorrhoidal blood flows from both ERVP and IRVP into the systemic circulation through the recto genital and inter-rectal portosystemic shunts. The recto genital communication connects the rectal venous plexus with vesico-prostatic or vaginal venous plexus. The inter-rectal communications occur between the three rectal veins both in ERVP and IRVP60 (Figure 9).
Figure 9.
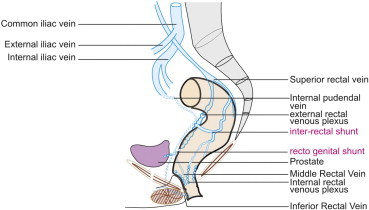
Efferents from rectal varices. From both ERVP and IRVP the portal hemorrhoidal blood works into systemic circulation through two portosystemic shunts (recto genital and inter-rectal).
Ectopic varices: omental collateral vessels
Numerous collateral vessels can pass thought the greater omentum before connecting to the systemic circulation. They usually have a small diameter.
Afferents to Omental Varices
-
1.
Superior or inferior mesenteric veins
Efferents from Omental Varices
-
1.
The retroperitoneal or pelvic veins.
-
2.
Omental veins may also drain into GEV.
Ectopic varices: veins of Sappey
Veins of Sappey
In 1883, Sappey described accessory portal veins entering the liver capsule from different locations. These vessels play a role in the origin of transhepatic portosystemic shunts and are sometimes the only PSCV capable of transporting portal blood into the liver in EHPVO. The different locations are:
-
1.
Upper part of falciform ligament -superior veins of Sappey,
-
2.
Lower part of falciform ligament–inferior veins of Sappey
-
3.
Ligamentum teres in the central part of falciform ligament-the recanalized umbilical vein
-
4.
Left triangular ligament–left inferior phrenic vein and intercostal vein
-
5.
Right triangular ligament–right inferior phrenic vein
-
6.
Gastrohepatic omentum (cystic veins and branches of left gastric veins)
-
7.
Diaphragmatic veins (bare area of liver)
-
8.
Ligamentum venosum–patent ductus venosus if present
The paraumbilical veins are also called inferior veins of Sappey. They accompany ligamentum teres (obliterated left umbilical vein) in the falciform ligament and connect anterior parietal veins (superior and inferior epigastric veins in the rectus sheath and thoracoepigastric vein in subcutaneous tissue) at umbilicus with left branch of portal vein. Paraumbilical veins connected with numerous subcutaneous vessels of the anterior abdominal wall, create a ‘‘caput medusae’’ pattern.
Superior veins of Sappey are present in the upper part of falciform ligament connecting the convex anterosuperior surface of liver to diaphragm and connect with internal thoracic veins through diaphragm.
Similarly portosystemic communication occurs through bare area of liver with right inferior phrenic vein and through left triangular ligament with left intercostal veins, left pericardiacophrenic vein and left inferior phrenic veins. Dilated right epigastric vein (caput medusae) has also been shown to connect to a varicose vein in the anterior right thigh where they have been responsible for presence of varicose vein in lower extremities.67
Afferent to Umbilical Varices
The left branch of portal vein receives the umbilical and paraumbilical veins to form umbilical varices by the recanalised ligamentum teres in the falciform ligament.
Efferents from Umbilical Varices
Superior and inferior epigastric veins are the efferents of umbilical varices. The most common path of drainage of paraumbilical veins is through the inferior epigastric veins, which follow the posterior face of the rectus abdominis muscles to finally reach the external iliac veins. However, paraumbilical vessels may also anastomose with internal thoracic veins and drain into the superior vena cava.
Ectopic varices: vesical varices
Vesical varices are rare in patients with portal hypertension because the bladder wall is an unusual collateral route for the venous splanchnic blood. Generally reported cases of vesical varices have a history of abdominal surgery.68–71
Ectopic varices: vaginal and uterine varices
Venous Drainage of Vagina and Uterus
The anatomy of the vagina and uterus makes them unlikely locations to develop varices as the uterus has an extensive venous plexus, which primarily drains into the uterine veins and later into the internal iliac vein (part of systemic circulation). The vagina also has a venous plexus, which similarly drains into the internal iliac vein via bilateral vaginal veins. The plexuses are in communication with each other and with the vesical and hemorrhoidal plexuses.
Afferent to Vaginal and Uterine Varices
Superior portion of the hemorrhoidal plexus.72,73
Efferent from Vaginal and Uterine Varices
Venous plexuses of uterus and vagina, internal iliac vein and uterine veins.
Ectopic varices: gallbladder varices
Gallbladder Varices
Gallbladder varices are present in ∼12% of patients with portal hypertension but are more frequent in those with extrahepatic portal hypertension (30%). The GB wall varices refer to presence of varices in or outside the wall of GB in a pericholecystic location.74
Afferents to Gallbladder Varices
Cystic vein, branch of the right portal vein.
Efferents from Gallbladder Varices
They may drain to hepatic vein or intrahepatic portal vein; they may also drain into systemic anterior abdominal wall collaterals.75
Ectopic varices: biliary varices
Biliary Varices
Extrahepatic obstruction of the portal vein (EHPVO) may cause extensive collateral venous circulation at the porta hepatis. Portal hypertensive biliopathy (PHB) refers to abnormalities of the biliary tract in patients due to these portoportal collaterals.76,77 These collateral veins are related to 2 preformed venous systems near the extrahepatic bile ducts: the paracholedochal (PACD) veins of Petren, and the epicholedochal (ECD) venous plexus of Saint. The PACD venous plexus of Petren runs parallel to the CBD, and the ECD plexus of Saint veins form a reticular mesh on the surface of the CBD.78,79 Early changes of PB occur with engorgement of the paracholedochal veins of Petren and the epicholedochal venous plexus of Saint, which lie adjacent to and within the biliary duct walls, respectively. The PACD collaterals, if dilated, may cause extrinsic compression and protrusion into the thin and pliable CBD, and the ECD collaterals, if dilated, may make the normally smooth intraluminal surface of the CBD irregular80,81 Venous compensation through the paracholedochal veins in the setting of chronic PVT results in scalloped or smooth indentations in the ductal lumen that can be seen by ERCP or MRCP. Engorgement of the smaller epicholedochal veins results in thickened, enhancing bile duct walls on cross-sectional images.82 EUS in portal hypertension has shown that collaterals enter subepithelial layer of CBD after perforating the fibromuscular layer of CBD wall and lie as intracholedochal varices (ICDV).83 The origin of these perforators from PACD collaterals acted as the link between veins outside the muscular wall of the CBD and those inside the muscular wall. Saint's anatomic studies suggest that dilatation of the PACD veins will occur first in portal hypertension, and ECD varices related to Saint venous plexus have not been described without accompanying PACD varices.84 The varices have been labeled as intracholedochal varices and currently EUS appears to be the investigation of choice in tracing the origin, caliber, entry, and course of ICD varices throughout the CBD.85 ICDV can temporarily disappear during controlled hypotension with nitroglycerin infusion and allow therapeutic completion of ERCP in PHB.8
Portoportal Connections of Biliary Varices
The right-sided plexus can communicate with gastrocolic trunk (GT) and pancreatico duodenal vein to the cystic vein or directly to liver. The left sided plexus can communicate with first jejunal trunk (FJT), left and right gastric vein (LGV and RGV) and with the left portal vein (LPV). Generally the flow occurs toward the branches of portal vein in the liver.78,81
Ectopic varices: anastomotic and stomal varices
A detailed evaluation of collateral pathways after surgery is beyond the scope of this review and some of salient features are mentioned.
-
1.
Surgery involving apposition of abdominal structures (drained by systemic veins) to the bowel (drained by portal tributaries) may result in the formation of collaterals at unusual sites.86
-
2.
The knowledge that ectopic varices predominantly develop at postoperative or inflammatory adhesions may contribute to localization of the bleeding source.87,88
-
3.
Hashimoto et al89 found dilated communicating veins between hepaticojejunostomies (communicating jejunal veins and intrahepatic portal veins in five of nine subjects with portal vein occlusion). Computed tomographic arterial portography (CTAP) revealed hepatopetal flow into the liver with adequate portal flow to perfuse the entire liver. Similar collaterals that are the result of surgery or inflammatory adhesions between the liver capsule and the mesentery have been discovered with ultrasonography (US) and have been termed transcapsular collaterals.
-
4.
Transcapsular collaterals are especially common in patients who had undergone hepatobiliary surgery and who had chronic PVT. The explanation for development of transcapsular collaterals in some of these patients, who had undergone liver transplantation, was the surgical dissection of preformed vessel structures in the hepatoduodenal ligament and the gallbladder bed—which are needed for cavernoma formation as one classic pathway of collateralization.90
Approximately 50% of patients with surgical digestive stoma in a context of portal hypertension have stomal varices. Ileostomies and colostomies create a communication between the venous network of the mesentery (high pressure system) and that of the abdominal wall (low-pressure system).91–93
Ectopic varices: diaphragm
Venous Drainage of Diaphragm
Superior surface of diaphragm is drained by pericardiophrenic and musculophrenic veins, which drain into the internal thoracic vein. Inferior phrenic veins drain the inferior surface. The right inferior phrenic vein usually opens into the inferior vena cava whereas the left inferior phrenic vein joins the IVC and or left renal or suprarenal vein. Cardiophrenic varices particularly on the right side are usually located at a cardiophrenic angle, and rupture is rare.
Afferent to Diaphragmatic Varices
Cardiophrenic varices, are collaterals from the paraumbilical vein.
Efferents from Diaphragmatic Varices
Internal mammary vein.
Interportal communications
The word interportal communication is different from portoportal communications. The conceptual difference between portoportal and interportal collateral is that a portoportal collateral will be connected to the portal vein on entry and/or exit whereas an interportal collateral goes from one part of portal venous system into another part of portal venous system. Interportal communication indicates flow of blood that bypasses an obstructed segment of the portal venous system. This occurs mainly in EHPVO where the collaterals have a tendency to go toward the portal venous system after bypassing the site of obstruction. These include the portoportal collaterals that have been already described in biliary varices. However no formal classification of interportal pathways exists and in a large venography series, interportal communications were seen with the left gastric vein, left portal vein, gastroepiploic vein and from a branch of superior mesenteric vein.26
In EHPVO some of the most important collaterals to develop are along the gastroepiploic pathway. Direction of flow along these collaterals depends on the site of occlusion, whether splenic or superior mesenteric or both. In cases of isolated splenic vein narrowing or occlusion, flow in the left gastric vein is hepatopetal toward a low-pressure system in the portal vein. Patterns of collateral pathways in extrahepatic portal hypertension have been demonstrated by multidetector computed tomography.94
Collateral pathways in Budd–Chiari syndrome
Three types of obstruction can occur in Budd–Chiari syndrome (BCS), which include obstruction to the major hepatic veins alone (Type I), obstruction to the suprahepatic IVC alone (Type II) and combined obstruction to the major hepatic veins and IVC (Type III).95 Development of collateral pathways depends on the type and location of obstruction in BCS and can occur in intra and extrahepatic locations.
Intrahepatic Collaterals
Two forms of intrahepatic collaterals may develop: those that communicate with systemic veins via the subcapsular vessels and those that shunt blood from the occluded to the non-occluded segments of the hepatic vein. The subcapsular vessels originate as intrahepatic collaterals but become extrahepatic after going through the capsule of liver and communicate with left inferior phrenic vein. Intrahepatic collaterals, which remain inside liver, develop as comma shaped collaterals between the adjacent right and left hepatic vein.95
Extrahepatic Collaterals
The extrahepatic collaterals include, renal-inferior phrenic-pericardiophrenic collaterals, esophageal veins, left renal-hemiazygos pathway, vertebrolumbar-azygos pathway and superficial collaterals of the abdominal wall.96
Inferior Phrenic-pericardiophrenic Collaterals
The right inferior phrenic vein usually drains directly into IVC, whereas the left inferior phrenic vein has two branches: one ending in the left renal vein and the other ending in the IVC. In about 75% of cases the ostia of left hepatic vein and left inferior phrenic veins are close to each other or the former terminates at the latter.97 The inferior phrenic-pericardiophrenic collaterals can be formed via both intrahepatic and extrahepatic collaterals in BCS where the intrahepatic collaterals come via subcapsular collaterals and the extrahepatic collaterals come via left renal vein (Figure 4). The pericardiophrenic vein, a tributary of the brachiocephalic vein, has diaphragmatic branches that anastomose with the inferior phrenic vein (Figure 7) and in case the blockage extends above the joining of inferior phrenic veins in IVC one of collateral channel can be directed through the pericardiophrenic veins as inferior phrenic-pericardiophrenic collaterals (Figure 4).39,40
Left Renal-hemiazygos Pathway
Anatomically, the left renal vein is more complex than the right because of multiple vessels (the inferior phrenic, Capsular, adrenal and gonadal veins) that join the left renal vein (Figure 6). In addition, the left renal vein communicates with the retroperitoneal vein by the lumbar, ascending lumbar, and hemiazygos veins in two thirds of cases. Rarely, the left renal hemiazygos route may constitute the main central pathway of flow toward the heart in the BCS.97
Vertebrolumbar-azygos Pathway
Venous flow within the IVC reverses to the common iliac vein and then continues through the ascending lumbar vein, anastomosing with the azygos system. This collateral pathway is the one most commonly seen in BCS. Flow may reverse through the left renal vein to the gonadal, ureteric, or capsular vein (perirenal collaterals), onward to the iliac vein, and then to the vertebral venous system. The flow may also be directed through the intravertebral, paraspinal and extravertebral plexuses (Batson's plexus). The ascending lumbar veins parallel the spine as they ascend through the retroperitoneum. These veins lie anteriorly or anterolaterally to the spine and posterolaterally to the aorta and vena cava (Figure 6).97
Abdominal Wall
The superficial collateral system of the abdominal wall involves the inferior epigastric, circumflex iliac, and superficial epigastric veins, which arise from the external iliac and common femoral veins. The inferior epigastric vein, arising from the external iliac vein, anastomoses with the superior epigastric vein above the umbilicus and with the internal mammary vein to reach the subclavian vein. Flow may follow the common femoral vein through the superficial circumflex iliac vein to the superficial epigastric vein anastomosing with the lateral thoracic vein. The inferior epigastric vein runs within the lateral umbilical peritoneal fold, and then passes to the posterior surface of the musculus rectus abdominis.98,99
Conclusion
It is of importance to delineate variceal hemodynamic profiles to understand the pathophysiology of ectopic varices and establish therapies for them. MR angiography, multidetector-row CT, CT angiography and EUS are essential imaging examination. A description of PSCV pathways is given above. This information can be useful in management and evaluation of portal hypertension.
Conflicts of interest
All authors have none to declare.
References
- 1.Al-Nakshabandi N.A. The role of ultrasonography in portal hypertension. Saudi J Gastroenterol. 2006;12:111–117. doi: 10.4103/1319-3767.29750. [DOI] [PubMed] [Google Scholar]
- 2.Menon K.V., Kamath P.S. Regional and systemic hemodynamic disturbances in cirrhosis. Clin Liver Dis. 2001:617–627. doi: 10.1016/s1089-3261(05)70184-7. [DOI] [PubMed] [Google Scholar]
- 3.Cichoz-Lach H., Celinski K., Slomka M. Pathophysiology of portal hypertension. J Physiol Pharmacol. 2008;59:231–238. [PubMed] [Google Scholar]
- 4.Fernandez M., Mejias M., Angermayr B. Inhibition of VEGF receptor-2 decreases the development of hyperdynamic splanchnic circulation and portal-systemic collateral vessels in portal hypertensive rats. J Hepatol. 2005;43:98–103. doi: 10.1016/j.jhep.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 5.Moreau R. VEGF induced angiogenesis drives collateral circulation in portal hypertension. J Hepatol. 2005;43:6–8. doi: 10.1016/j.jhep.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Johns T.N., Evans B.B. Collateral pathways in portal hypertension. Ann Surg. 1962;155:838–845. doi: 10.1097/00000658-196206000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moubarak E., Bouvier A., Boursier J. Portosystemic collateral vessels in liver cirrhosis: a three-dimensional MDCT pictorial review. Abdom Imaging. 2011;Oct 15 doi: 10.1007/s00261-011-9811-0. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Sharma M., Babu C.S., Dhiman R.K. Induced hypotension in management of acute hemobilia during therapeutic ERCP in a patient with portal biliopathy. Gastrointest Endosc. 2010;72:1317–1319. doi: 10.1016/j.gie.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 9.Ibukuro K., Tsukiyama T., Mori K. Transhepatic portosystemic shunts: CT appearance and anatomic correlation. AJR Am J Roentgenol. 2000;175:153–157. doi: 10.2214/ajr.175.1.1750153. [DOI] [PubMed] [Google Scholar]
- 10.Hashizume M., Kitano S., Sugimachi K. Three-dimensional view of the vascular structure of the lower esophagus in clinical portal hypertension. Hepatology. 1988;8:1482–1487. doi: 10.1002/hep.1840080603. [DOI] [PubMed] [Google Scholar]
- 11.Vianna A., Hayes P.C., Moscoso G. Normal venous circulation of the gastroesophageal junction. A route to understanding varices. Gastroenterology. 1987;93:876–889. doi: 10.1016/0016-5085(87)90453-7. [DOI] [PubMed] [Google Scholar]
- 12.Bergele Christina Th., Avgerinos Alexandros Ch. Endoscopic ultrasonography in portal hypertension. Hosp Chron. 2006;1:36–41. doi: 10.1016/j.dld.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 13.Irisawa A., Obara K., Sato Y. EUS analysis of collateral veins inside and outside the esophageal wall in portal hypertension. Gastrointest Endosc. 1999;50:374–380. doi: 10.1053/ge.1999.v50.97777. [DOI] [PubMed] [Google Scholar]
- 14.Sanyal A.J. The value of EUS in the management of portal hypertension. Gastrointest Endosc. 2000;52:575–577. doi: 10.1067/mge.2000.108483. [DOI] [PubMed] [Google Scholar]
- 15.Caletti G.C., Brocchi E., Ferrari A. Value of endoscopic ultrasonography in the management of portal hypertension. Endoscopy. 1992;24(suppl 1):342–346. doi: 10.1055/s-2007-1010496. [DOI] [PubMed] [Google Scholar]
- 16.Schiano T.D., Adrain A.L., Vega K.J. High−resolution endoluminal sonography assessment of the hematocystic spots of esophageal varices. Gastrointest Endosc. 1999;49:424–427. doi: 10.1016/s0016-5107(99)70037-4. [DOI] [PubMed] [Google Scholar]
- 17.Sharma M., Somasundaram A. Massive lower GI bleed from an endoscopically inevident rectal varices diagnosis and management by endoscopic ultrasound. Gastrointest Endosc. 2010;72:1106–1108. doi: 10.1016/j.gie.2010.02.054. [DOI] [PubMed] [Google Scholar]
- 18.Shertsinger A.G., Manuk'ian G.V., Manuk'ian V.G. Pathogenesis of esophageal and gastricvaricose veins formation in patients with liver cirrhosis. Eksp Klin Gastroenterol. 2011;6:73–78. [PubMed] [Google Scholar]
- 19.Watanabe N., Toyonaga A., Kojima S. Current status of ectopic varices in Japan: results of a survey by the Japan Society for Portal Hypertension. Hepatol Res. 2010;40:763–776. doi: 10.1111/j.1872-034X.2010.00690.x. [DOI] [PubMed] [Google Scholar]
- 20.Aslam N., Waters B., Riely C.A. Intraperitoneal rupture of ectopic varices: two case reports and a review of literature. Am J Med Sci. 2008;335:160–162. doi: 10.1097/MAJ.0b013e318068b273. [DOI] [PubMed] [Google Scholar]
- 21.Norton I.D., Andrews J.C., Kamath P.S. Management of ectopic varices. Hepatology. 1998;28:1154–1158. doi: 10.1002/hep.510280434. [DOI] [PubMed] [Google Scholar]
- 22.Butler H. The veins of esophagus. Thorax. 1951;6:276–296. doi: 10.1136/thx.6.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Youssef A.I., Escalante-Glorsky S., Bonnet R.B. Hemoptysis secondary to bronchial varices associated with alcoholic liver cirrhosis and portal hypertension. Am J Gastroenterol. 1994;89:1562–1563. [PubMed] [Google Scholar]
- 24.Arakawa M., Masuzaki T., Okuda K. Pathomorphology of esophageal and gastric varices. Semin Liver Dis. 2002;22:73–82. doi: 10.1055/s-2002-23208. [DOI] [PubMed] [Google Scholar]
- 25.Kang H.K., Jeong Y.Y., Choi J.H. Three-dimensional multi-detector row CT portal venography in the evaluation of portosystemic collateral vessels in liver cirrhosis. Radiographics. 2002;22(5):1053–1061. doi: 10.1148/radiographics.22.5.g02se011053. [DOI] [PubMed] [Google Scholar]
- 26.Widrich W.C., Srinivasan M., Semine M.C. Collateral pathways of the left gastric vein in portal hypertension. AJR Am J Roentgenol. 1984;142:375–382. doi: 10.2214/ajr.142.2.375. [DOI] [PubMed] [Google Scholar]
- 27.Kimura K., Ohto M., Matsutani S. Relative frequencies of portosystemic pathways and renal shunt formation through the “posterior” gastric vein: portographic study in 460 patients. Hepatology. 1990;12(4 Pt 1):725–728. doi: 10.1002/hep.1840120417. [DOI] [PubMed] [Google Scholar]
- 28.Nagahiro I., Toda D., Andou A. A case of bronchial varices due to extrahepatic portal hypertension. Respiration. 2007;74:460–461. doi: 10.1159/000088356. [DOI] [PubMed] [Google Scholar]
- 29.Loukas M., Louis R.G., Jr., Hullett J. An anatomical classification of the variations of the inferior phrenic vein. Surg Radiol Anat. 2005;27(6):566–574. doi: 10.1007/s00276-005-0029-0. [DOI] [PubMed] [Google Scholar]
- 30.Murakami G., Adachi N., Sato I. Venous drainage of the thoracic esophagus toward the pulmonary vein. Okajimas Folia Anat Jpn. 1994;71:13–19. doi: 10.2535/ofaj1936.71.1_13. [DOI] [PubMed] [Google Scholar]
- 31.Yamagami T., Tanaka O., Yoshimatsu R. Value of embolisation of collateral veins from gastric varices before balloon-occluded retrograde transvenous obliteration. J Med Imaging Radiat Oncol. 2011;55:26–32. doi: 10.1111/j.1754-9485.2010.02226.x. [DOI] [PubMed] [Google Scholar]
- 32.Irani S., Kowdley K.V., Kozarek R.A. Gastric varices: an updated review of management. J Clin Gastroenterol. 2011;45:133–148. doi: 10.1097/MCG.0b013e3181fbe249. [DOI] [PubMed] [Google Scholar]
- 33.Chikamori F., Kuniyoshi N., Kawashima T. Gastric varices with gastrorenal shunt: combined therapy using transjugular retrograde obliteration and partial splenic embolization. AJR Am J Roentgenol. 2008;191:555–559. doi: 10.2214/AJR.07.3356. [DOI] [PubMed] [Google Scholar]
- 34.Koito K., Namieno T., Nagakawa T. Balloon-occluded retrograde transvenous obliteration for gastric varices with gastrorenal or gastro caval collaterals. AJR Am J Roentgenol. 1996;167:1317–1320. doi: 10.2214/ajr.167.5.8911204. [DOI] [PubMed] [Google Scholar]
- 35.Bhatia V. Endoscopic ultrasound (EUS) for esophageal and gastric varices: how can it improve the outcomes and reduce complications of glue injection. J Clin Exp Hepatol. 2012;1:70–74. doi: 10.1016/S0973-6883(12)60083-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kiyosue H., Tanoue S., Kondo Y. Balloon-occluded retrograde transvenous obliteration of complex gastric varices assisted by temporary balloon occlusion of the splenic artery. J Vasc Interv Radiol. 2011;22:1045–1048. doi: 10.1016/j.jvir.2010.12.028. [DOI] [PubMed] [Google Scholar]
- 37.Hirota S., Kobayashi K., Maeda H. Balloon-occluded retrograde transvenous obliteration for portal hypertension. Radiat Med. 2006;24:315–320. doi: 10.1007/s11604-006-2407-x. [DOI] [PubMed] [Google Scholar]
- 38.Saraswat V.A., Verma A. Gluing gastric varices in 2012: lessons learnt over 25 years. J Clin Exp Hepatol. 2012;1:55–69. doi: 10.1016/S0973-6883(12)60088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maruyama H., Okugawa H., Yoshizumi H. Hemodynamic features of gastrorenal shunt: a Doppler study in cirrhotic patients with gastric fundal varices. Acad Radiol. 2008;15:1148–1154. doi: 10.1016/j.acra.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 40.Kutlu R., Alkan A., Sigirci A. Pericardiacophrenic shunt: imaging finding of rare splenosystemic collateral. Surg Radiol Anat. 2006;28:426–428. doi: 10.1007/s00276-006-0116-x. [DOI] [PubMed] [Google Scholar]
- 41.Okugawa H., Maruyama H., Kobayashi S. Therapeutic effect of balloon occluded retrograde transvenous obliteration for gastric varices in relation to hemodynamics in the short gastric vein. BJR. 2009;82:930–935. doi: 10.1259/bjr/28956799. [DOI] [PubMed] [Google Scholar]
- 42.Wind P., Alves A., Chevallier J.M. Anatomy of spontaneous splenorenal and gastrorenal venous anastomoses. Review of the literature. Surg Radiol Anat. 1998;20:129–134. [PubMed] [Google Scholar]
- 43.Zhao L.Q., He W., Ji M. 64-row multidetector computed tomography portal venography of gastric variceal collateral circulation. World J Gastroenterol. 2010;16:1003–1007. doi: 10.3748/wjg.v16.i8.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kapoor S., Paik E., Rezaei A. Where there is blood, there is a way: unusual collateral vessels in superior and inferior vena cava obstruction. Radiographics. 2010;30:67–68. doi: 10.1148/rg.301095724. [DOI] [PubMed] [Google Scholar]
- 45.Nardone G., Budillon G. Treatment of duodenal varices by endoscopic sclerotherapy. Gastrointest Endosc. 1991;37:407–408. doi: 10.1016/s0016-5107(91)70757-8. [DOI] [PubMed] [Google Scholar]
- 46.Stephan G. Bleeding of duodenal varices in portal hypertension. Bruns Beitr Klin Chir. 1973 Aug;220(5):467–474. [PubMed] [Google Scholar]
- 47.Skandalakis J.E. Surgical anatomy 2 vol set: the embryologic & anatomic basis of modern surgery (Skandalakis, surgical anatomy 2 vol set) PMP. 2004:1115–1229. [Google Scholar]
- 48.Sharma M., Rameshbabu C.S., Garg S. Portal venous system and its tributaries: a radial endosonographic assessment. Endoscopic Ultrasound. 2012 Aug;1(2):96–107. doi: 10.7178/eus.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ibukuro K., Tsukiyama T., Mori K. Veins of Retzius at CT during arterial portography: anatomy and clinical importance. Radiology. 1998 Dec;209(3):793–800. doi: 10.1148/radiology.209.3.9844676. [DOI] [PubMed] [Google Scholar]
- 50.McAlister V.C., Al-Saleh N.A. Duodenal dearterialization and stapling for severe hemorrhage from duodenal varices with portal vein thrombosis. Am J Surg. 2005;189(1):49–52. doi: 10.1016/j.amjsurg.2004.04.011. Original research article. [DOI] [PubMed] [Google Scholar]
- 51.Perchik L., Max T.C. Massive hemorrhage from varices of the duodenal loop in cirrhotic patient. Radiology. 1963 June;80:641–644. [Google Scholar]
- 52.Yeh Y.Y., Hou M.C., Lin H.C. Case report: successful obliteration of a bleeding duodenal varix using endoscopic ligation. J Gastroenterol Hepatol. 1998 Jun;13(6):591–593. doi: 10.1111/j.1440-1746.1998.tb00695.x. [DOI] [PubMed] [Google Scholar]
- 53.Vellar I.D. Preliminary study of the anatomy of the venous drainage of the intrahepatic and extrahepatic bile ducts and its relevance to the practice of hepatobiliary surgery. ANZ J Surg. 2001 Jul;71(7):418–422. doi: 10.1046/j.1440-1622.2001.02150.x. [DOI] [PubMed] [Google Scholar]
- 54.Lebrec D., Benhamou J.P. Ectopic varices in portal hypertension. Clin Gastroenterol. 1985 Jan;14(1):105–121. [PubMed] [Google Scholar]
- 55.Lim L.G., Lee Y.M., Tan L. Percutaneous paraumbilical embolization as an unconventional and successful treatment for bleeding jejunal varices. World J Gastroenterol. 2009 Aug 14;15(30):3823–3826. doi: 10.3748/wjg.15.3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Feldman M., Sr, Smith V.M., Warner C.G. Varices of the colon. Report of three cases. JAMA. 1962;179:729–730. doi: 10.1001/jama.1962.03050090057014b. [DOI] [PubMed] [Google Scholar]
- 57.Weingart J., Hochter W., Ottenjann R. Varices of the entire colon-an unusual cause of recurrent intestinal bleeding. Endoscopy. 1982;14(2):69–70. doi: 10.1055/s-2007-1021582. [DOI] [PubMed] [Google Scholar]
- 58.Francois F., Tadros C., Diehl D. Pan-colonic varices and Idiopathic portal hypertension. J Gastrointestin, Liver Dis. 2007, Sep;16(3):325–328. [PubMed] [Google Scholar]
- 59.Sato T. Transabdominal color Doppler ultrasonography for the diagnosis of small intestinal and vesical varices in a patient successfully treated with percutaneous transhepatic obliteration. Clin J Gastroenterol. 2010;3(Number 4):214–218. doi: 10.1007/s12328-010-0164-y. [DOI] [PubMed] [Google Scholar]
- 60.Hollinshead W.H. 2nd ed. vol. 2. Hoeber Medical Division, Harper & Row; 1971. The rectum and anal canal. (Anatomy for Surgeons). 676–720. [Google Scholar]
- 61.Yachha S.K., Dhiman R.K., Gupta R. Endosonographic evaluation of the rectum in children with extrahepatic portal venous obstruction. J Pediatr Gastroenterol Nutr. 1996 Nov;23(4):438–441. doi: 10.1097/00005176-199611000-00014. [DOI] [PubMed] [Google Scholar]
- 62.Dhiman R.K., Saraswat V.A., Choudhuri G. Endosonographic, endoscopic and histologic evaluation of alterations in the rectal venous system in patients with portal hypertension. Gastrointest Endosc. 1999 Feb;49(2):218–227. doi: 10.1016/s0016-5107(99)70490-6. [DOI] [PubMed] [Google Scholar]
- 63.Terayama N., Matsui O., Kobayashi S. Portosystemic shunt on CT during arterial portography: prevalence in patients with and without liver cirrhosis. Abdom Imaging. 2008 Jan–Feb;33(1):80–86. doi: 10.1007/s00261-007-9196-2. [DOI] [PubMed] [Google Scholar]
- 64.Shudo R., Yazaki Y., Sakurai S. Combined endoscopic variceal ligation and sclerotherapy for bleeding rectal varices associated with primary biliary cirrhosis: a case showing a long-lasting favorable respons. Gastrointest Endosc. 2001 May;53(6):661–665. doi: 10.1067/mge.2001.113278. [DOI] [PubMed] [Google Scholar]
- 65.Hsieh J.S., Huang C.J., Huang Y.S. Demonstration of rectal vanices by transhepatic inferior mesenteric venography. Dis Colon Rectum. 1986;29(7):459–461. doi: 10.1007/BF02561586. [DOI] [PubMed] [Google Scholar]
- 66.Hiller R.I. Internal hemorrhoids: their pathogenesis and rationale of injection therapy. Am J Surg. 1932;16:64. [Google Scholar]
- 67.Jung S.C., Lee W., Chung J.W. Unusual causes of varicose veins in the lower extremities: CT venographic and Doppler US findings. Radiographics. 2009 Mar-Apr;29(2):525–536. doi: 10.1148/rg.292085154. [DOI] [PubMed] [Google Scholar]
- 68.Sano K., Shuin T., Takebayashi S. A case of vesical varices as a complication of portal hypertension and manifested gross hematuria. J Urol. 1989 Feb;141(2):369–371. doi: 10.1016/s0022-5347(17)40771-3. [DOI] [PubMed] [Google Scholar]
- 69.Lugagne P.M., Castaing D., Conort P. Portal hypertension: a rare cause of hematuria. Prog Urol. 1992 Apr;2(2):294–298. [PubMed] [Google Scholar]
- 70.Loganathan G., Shyamkumar N.K., Kurian G. Vesical varix in cirrhosis of liver. Indian J Gastroenterol. 2000 Oct-Dec;19(4):193–194. [PubMed] [Google Scholar]
- 71.Gaspar Y., Detry O., de Leval J. Vesical varices in a patient with portal hypertension. N Engl J Med. 2001 Nov 15;345(20):1503–1504. doi: 10.1056/NEJM200111153452018. [DOI] [PubMed] [Google Scholar]
- 72.McHugh P.P., Jeon H., Gedaly R. Vaginal varices with massive hemorrhage in a patient with nonalcoholic steatohepatitis and portal hypertension: successful treatment with liver transplantation. Liver Transpl. 2008 Oct;14(10):1538–1540. doi: 10.1002/lt.21506. [DOI] [PubMed] [Google Scholar]
- 73.Williams P.L. 38th ed. Churchill Livingstone; New York, NY: 1999. Veins of the abdomen and pelvis: hepatic portal system; pp. 1602–1604. (Gray's Anatomy). [Google Scholar]
- 74.Chawla Y., Dilawari J.B., Katariya S. Gallbladder wall varices in portal vein thrombosis. AJR Am J Roentgenol. 1994 Mar;162(3):643–645. doi: 10.2214/ajr.162.3.8109513. [DOI] [PubMed] [Google Scholar]
- 75.Gabata T., Matsui O., Kadoya M. Gallbladder varices: demonstration of direct communication to intrahepatic portal veins by color doppler sonography and CT during arterial portography. Abdom Imaging. 1997 Jan-Feb;22(1):82–84. doi: 10.1007/s002619900145. [DOI] [PubMed] [Google Scholar]
- 76.Sarin S.K., Agarwal S.R. Extrahepatic portal vein obstruction. Semin Liver Dis. 2002 Feb;22(1):43–58. doi: 10.1055/s-2002-23206. [DOI] [PubMed] [Google Scholar]
- 77.Shin S.M., Kim S., Lee J.W. Biliary abnormalities associated with portal biliopathy: evaluation on MR cholangiography. AJR Am J Roentgenol. 2007 Apr;188(4):W 341–W 347. doi: 10.2214/AJR.05.1649. [DOI] [PubMed] [Google Scholar]
- 78.Petren T. The veins of the extrahepatic biliary system and their pathologic anatomic significance. Vert Anat Ges. 1932;41:139–143. [Google Scholar]
- 79.Saint J.H. The epicholedochal venous plexus and its importance as a means of identifying the common duct during operation on extrahepatic biliary tract. Br J Surg. 1961; Mar;48:489–498. doi: 10.1002/bjs.18004821104. [DOI] [PubMed] [Google Scholar]
- 80.Don S.J., Trian J.S., Cohen B.A. Common bile duct varices: cholangiographic demonstration of a hazardous portosystemic communication. Am J Gastroenterol. 1983;78(1):42–43. [PubMed] [Google Scholar]
- 81.Sharma M. Bleeding after endoscopic biliary sphincterotomy. J Clin Exp Hepatol. 2011;1(1):45–47. doi: 10.1016/S0973-6883(11)60117-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Walser E.M., Runyan B.R., Heckman M.G. Extrahepatic portal biliopathy: proposed etiology on the basis of anatomic and clinical features. Radiology. 2011 Jan;258(1):146–153. doi: 10.1148/radiol.10090923. [DOI] [PubMed] [Google Scholar]
- 83.Sharma M., Pathak A. Perforators of common bile duct wall in portal hypertensive Biliopathy (with videos) Gastrointest Endosc. 2009 Nov;70(5):1041–1043. doi: 10.1016/j.gie.2009.03.040. [DOI] [PubMed] [Google Scholar]
- 84.Kim S., Chew F.S. Choledochal varices. AJR Am J Roentgenol. 1988 Mar;150(3):578–580. doi: 10.2214/ajr.150.3.578. [DOI] [PubMed] [Google Scholar]
- 85.Sharma M., Pathak A. Intracholedochal varices in portal hypertensive biliopathy. Eur J Radiol Extra. December 2009;72(3):119–123. [Google Scholar]
- 86.Helmy A., Al Kahtani K., Al Fadda M. Updates in the pathogenesis, diagnosis and management of ectopic varices. Hepatol Int. 2008 Sep;2(3):322–334. doi: 10.1007/s12072-008-9074-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Perea García J., Lago Oliver J., Muñoz Jiménez F. Low gastrointestinal bleeding due to ectopic varices as a result of adhesions. Gastroenterol Hepatol. 2000; Jun–Jul;23(6):287–289. [in Spanish] [PubMed] [Google Scholar]
- 88.Fee H.J., Taylor J.B., O’Connell T.X. Bleeding intestinal varices associated with portal hypertension and previous abdominal surgery. Am Surg. 1977 Nov;43(11):760–762. [PubMed] [Google Scholar]
- 89.Hashimoto M., Heianna J., Yasuda K. Portal flow into the liver through veins at the site of biliary-enteric anastomosis. Eur Radiol. 2005 Jul;15(7):1421–1425. doi: 10.1007/s00330-005-2667-3. [DOI] [PubMed] [Google Scholar]
- 90.Seeger M., Günther R., Hinrichsen H. Chronic portal vein thrombosis: transcapsular hepatic collateral vessels and communicating ectopic varices. Radiology. 2010 Nov;257(2):568–578. doi: 10.1148/radiol.10100157. [DOI] [PubMed] [Google Scholar]
- 91.Choi J.W., Lee C.H., Kim K.A. Ectopic varices in colonic stoma: MDCT findings. Korean J Radiol. 2006 Oct–Dec;7(4):297–299. doi: 10.3348/kjr.2006.7.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fucini C., Wolff B.G., Dozois R.R. Bleeding from peristomal varices: perspectives on prevention and treatment. Dis Colon Rectum. 1991 Dec;34(12):1073–1078. doi: 10.1007/BF02050064. [DOI] [PubMed] [Google Scholar]
- 93.Shibata D., Brophy D.P., Gordon F.D. Transjugular intrahepatic portosystemic shunt for treatment of bleeding ectopic varices with portal hypertension. Dis Colon Rectum. 1999 Dec;42(12):1581–1585. doi: 10.1007/BF02236211. [DOI] [PubMed] [Google Scholar]
- 94.Kamel I.R., Lawler L.P., Corl F.M. Patterns of collateral pathways in extrahepatic portal hypertension as demonstrated by multidetector row computed tomography and advanced image processing. J Comput Assist Tomogr. 2004 Jul–Aug;28(4):469–477. doi: 10.1097/00004728-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 95.Chandrasekaran S., Cherian J.V., Muthusamy A.K. Alternate pathways in hepatic venous outflow obstruction by color doppler imaging. Ann Gastroenterol. 2007;20(3):218–222. [Google Scholar]
- 96.Fu Y., Sun Y.L., Ma X.X. Necessity and indications of invasive treatment for Budd–Chiari syndrome. Hepatobiliary Pancreat Dis Int. 2011 Jun;10(3):254–260. doi: 10.1016/s1499-3872(11)60042-8. [DOI] [PubMed] [Google Scholar]
- 97.Cho O.K., Koo J.H., Kim Y.S. Collateral pathways in Budd–Chiari syndrome CT and venographic correlation. AJR Am J Roentgenol. 1996 Nov;167(5):1163–1167. doi: 10.2214/ajr.167.5.8911174. [DOI] [PubMed] [Google Scholar]
- 98.Lin J., Chen X.H., Zhou K.R. Budd–Chiari syndrome: diagnosis with three-dimensional contrast-enhanced magnetic resonance angiography. World J Gastroenterol. 2003 Oct;9(10):2317–2321. doi: 10.3748/wjg.v9.i10.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pagaini J.J., Thomas J.L., Berhardino M.E. Computed tomographic manifestations of abdominal and pelvic venous collaterals. Radiology. 1982 Feb;142(2):415–419. doi: 10.1148/radiology.142.2.6459608. [DOI] [PubMed] [Google Scholar]


