Hepatocellular adenomas are rare benign liver tumors that, if not smaller than 5 cm and asymptomatic, do, in general, not require surgical intervention.1 However, larger tumors should be resected since there is a risk of hemorrhage or malignant transformation.1 We present here a case of abdominal and hepatic splenosis mimicking hepatocellular adenoma.
Case report
A 39-year-old woman presented at our department with a history of mild recurrent abdominal pain unrelated to meals. The patient did not report weight loss or fever. In a previously performed computerised tomography scan a tumor mass in the left upper abdomen adjacent to the major curvature of the stomach (3.4 cm × 2.2 cm) and a tumor in the 2nd liver segment (3.2 cm × 2.0 cm) were visualized. Although no biopsy was performed at the time, the focal liver lesion was suspected to be an adenoma. Therefore, left hemi-hepatectomy and surgical exploration of the other upper abdominal lesion were recommended. However, since the patient was reluctant to undergo surgery, she was referred to our institution for second opinion. Given a history of splenectomy after traumatic spleen rupture in childhood, we considered a diagnosis of two-site splenosis, which was substantiated by the absence of Howell–Jolly bodies in a blood smear. Therefore, we performed an abdominal magnetic resonance imaging (MRI) study (Figure 1A–D) and a scintigraphy with technetium-99m-labeled heat-damaged erythrocytes (Figure 2A, B). These examinations demonstrated the presence of splenic tissues in the liver and in the initial spleen location in the upper left abdomen. Hence, we recommended a conservative strategy instead of surgical intervention. At 3-months follow-up, the patient presented without symptoms.
Figure 1.
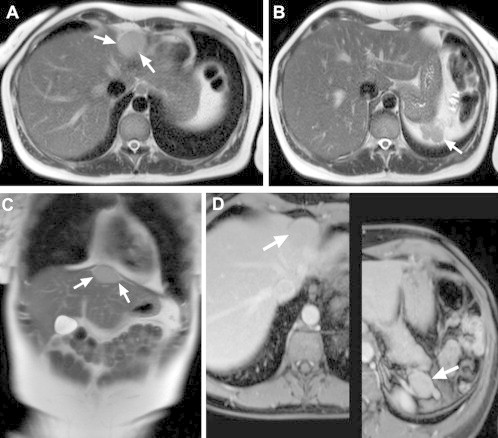
T2-weighted half-Fourier acquisition single shot turbo spin echo (HASTE) sequences in axial (A, B) and coronal (C) orientation. MR imaging reveals a round-shaped sharply demarcated hyperintense lesion at the left liver lobe (arrows in A, C). Additional lesions with comparable signal intensity are seen dorsal to the stomach (arrows in B) that look typical for regenerative splenic tissue; in addition note the absence of the spleen. The T1-weighted fat suppressed images (D) post contrast medium (MultiHance 0.05 mmol/kg) show homogeneous enhancement of the described lesions, consistent with splenic tissue.
Figure 2.
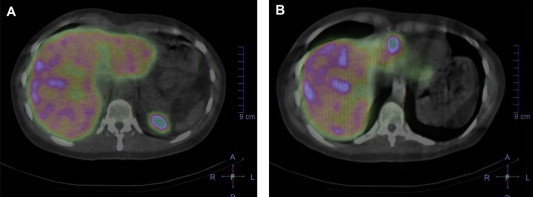
Scintigraphy with technetium-99m-labeled heat-damaged erythrocytes demonstrates the presence of a lesion at the initial spleen location (A) and in the left liver lobe (B) indicative for the abdominal and hepatic splenosis.
Splenosis, i.e. heterotopic autotransplantation of splenic tissue after trauma or surgical intervention is not uncommon,2 however hepatic splenosis is rare and so far less than 35 cases of this condition have been documented in the literature. In most of the reported patients the presence of adenoma, hepatocellular carcinoma or metastases was suspected.3 Hence, most of the patients were scheduled for invasive procedures, which are, in general, not indicated in this setting. Indeed, several case reports of patients with hepatic splenosis that were operated have been reported,3 one of them also presented in The Lancet4 in a currently not-existing section named ‘Uses of Error’. According to the review of the literature published by Mescoli et al.,3 in at least 17 out of 26 patients with hepatic splenosis that were reported till 2010, unnecessary biopsy or surgical excision of the liver mass were performed. However, surgery should be considered only in rare instances where hepatic and/or abdominal splenosis cause persistent symptoms, e.g. abdominal pain. In the current case the presence of concurrent hepatic and abdominal nodules of splenic tissue supported the diagnosis, which was suggested by MRI and, finally, confirmed by scintigraphy. In particular, functional imaging by red cell scintigraphy leads to the definitive non-invasive diagnosis of splenosis.5 This case illustrates that in patients with a history of splenectomy who are diagnosed with nodular hepatic lesions, the diagnostic work-up should include MRI and scintigraphy to exclude presence of spleen tissue within the liver and to avoid invasive procedures and surgical interventions.
Conflicts of interest
All authors have nothing to declare.
Acknowledgements
We would like to thank Dr. Matthias Maier (Knappschaft Hospital, Püttlingen) for cooperation in taking care of this patient.
References
- 1.Terkivatan T., de Wilt J.H., de Man R.A. Indications and long-term outcome of treatment for benign hepatic tumors: a critical appraisal. Arch Surg. 2001;136:1033–1038. doi: 10.1001/archsurg.136.9.1033. [DOI] [PubMed] [Google Scholar]
- 2.Brancatelli G., Vilgrain V., Zappa M., Lagalla R. Case 80: splenosis. Radiology. 2005;234:728–732. doi: 10.1148/radiol.2343030695. [DOI] [PubMed] [Google Scholar]
- 3.Mescoli C., Castoro C., Sergio A., Ruol A., Farinati F., Rugge M. Hepatic spleen nodules (HSN) Scand J Gastroenterol. 2010;45:628–632. doi: 10.3109/00365521003587812. [DOI] [PubMed] [Google Scholar]
- 4.Gamulin A., Oberholzer J., Rubbia-Brandt L., Mentha G. An unusual, presumably hepatic mass. Lancet. 2002;360:2066. doi: 10.1016/S0140-6736(02)11999-4. [DOI] [PubMed] [Google Scholar]
- 5.Varughese N., Duong A., Emre S., Xu M., Lee A.I. Clinical problem-solving. Venting the spleen. N Engl J Med. 2013;369:1357–1363. doi: 10.1056/NEJMcps1210943. [DOI] [PubMed] [Google Scholar]


