Abstract
Background
Collaborative networks of health organizations have received a great deal of attention in recent years as a way of enhancing the flow of information and coordination of services. However, relatively little is known about how such networks are formed and evolve, especially outside a local, community-based setting. This article is an in-depth discussion of the evolution of the North American Quitline Consortium (NAQC). The NAQC is a network of U.S. and Canadian organizations that provide telephone-based counseling and related services to people trying to quit smoking.
Methodology
The research draws on data from interviews, documents, and a survey of NAQC members to assess how the network emerged, became formalized, and effectively governed.
Findings
The findings provide an understanding of how multiregional public health networks evolve, while building on and extending the broader literature on organizational networks in other sectors and settings. Specifically, we found that the network form that ultimately emerged was a product of the back-and-forth interplay between the internal needs and goals of those organizations that would ultimately become network members, in this case, state-, and provincial-level tobacco quitline organizations. We also found that network formation, and then governance through a network administrative organization, was driven by important events and shifts in the external environment, including the impact and influence of major national organizations.
Practice Implications
The results of the study provide health care leaders and policy officials an understanding of how the activities of a large number of organizations having a common health goal, but spanning multiple states and countries, might be coordinated and integrated through the establishment of a formal network.
Keywords: collaboration, network evolution, organizational networks, tobacco quitlines
Organizational networks have become increasingly prevalent in public health and in health and human services, in general, where so many health issues, like smoking, obesity, HIV/AIDS, and mental health, cannot be effectively addressed by individual organizations acting on their own (Chaskin, Brown, Venkatesh, & Vidal, 2001; National Cancer Institute [NCI], 2007; Provan & Milward, 1995). In keeping with this trend, research on networks has increased dramatically since the early 1990s, especially as networks have become a critical component of health practice. A recent example is the creation of accountable care organizations (ACOs; cf. McClelland, McKethan, Lewis, Roski, & Fisher, 2010), which are an important component of the new Affordable Care Act. In most cases, ACOs will be multiorganizational networks of a hospital and other health providers, designed to improve health quality and limit costs.
However, despite increased attention paid to network arrangements, many questions remain unanswered, especially with regard to how health networks evolve and are sustained. This knowledge is especially important for health managers and policy officials at both the local and the national levels because efforts to form and build viable health networks are time-consuming, costly, and fraught with challenges (Weiner & Alexander, 1998). These challenges are significant particularly at the national level or international level, where geographical distances and the influence of local pressures and demands make meaningful collaboration difficult. Only by developing an understanding of how networks can successfully be formed and evolve can network and public health planners, funders, and participants begin to make the decisions required to ensure that networks fulfill their promise, resulting in the synergistic effects (Lasker, Weiss, & Miller, 2001) that enable networks to achieve “shared situational awareness” (Leischow & Milstein, 2006) or “collaborative advantage” (Huxham & Vangen, 2005).
To contribute to an understanding of how a large, geographically dispersed health network can successfully be established and evolve, this study examined the birth and early growth of the North American Quitline Consortium (NAQC). The NAQC is a multiregional network whose goal at the local level is to enhance the capacity of quitline organizations operating in every U.S. state and Canadian province to get people to quit smoking using telephone-based counseling and referral. Focusing on this one case, our research was guided by two questions. First, what were the key organizational and environmental conditions, especially those related to this particular health problem, that contributed to the emergence of the network? Second, what factors helped to shape the development of the form of network governance that was ultimately chosen?
Our research is largely qualitative, drawing on data from interviews and secondary sources but also including a 2009 survey of NAQC quitline organizations to demonstrate the current network structure of NAQC. We draw conclusions that have implications not only for network theory but also for practice, potentially enabling health managers, policy makers, and funders to build networks that can address complex public health problems more effectively.
Prior Research on Network Evolution
Due to the methodological challenges of collecting in-depth data on network evolution, especially over extended periods, the vast majority of studies on the evolution of goal-directed networks have been in the form of case studies or have been purely conceptual (D’Aunno & Zuckerman, 1987). Although the progression of this work has been marked by different theoretical frameworks, consistencies in findings across studies has allowed for a preliminary understanding of some key aspects of how networks evolve.
In a key early conceptual article, Ring and Van de Ven (1994) incorporated ideas of “roles,” along with assessments of efficiency and “fair-dealing,” to model a process for developing cooperative interorganizational relationships through negotiation, commitment, and execution of interactions. They suggested that when personal relationships have not yet been formed, people rely on institutionalized roles to guide interactions until personal relationships can be developed. The idea that roles facilitate cooperative interaction has been developed also by Bechky (2006).
In their theory of coevolution, Koza and Lewin (1999) extended early ideas on networks to the development of consciously formed, organized, goal-directed networks, or what Provan, Fish, and Sydow (2007) have referred to as “whole networks.” Whole networks are especially relevant in health, where the collective action of multiple organizations is often required to provide effective care. They differ from serendipitous networks (Kilduff & Tsai, 2003), which form and evolve spontaneously, focus on dyadic connections between social actors, and generally have no common theme or goal shared by network members (in a health context, cf. Christakis & Fowler, 2008, regarding social networks and smoking and Bahr, Browning, Wyatt, & Hill, 2009, and Christakis & Fowler, 2007, regarding social networks and obesity). Koza and Lewin identified a number of stages in the development of an international professional services network that were based on changes in the broader institutional and competitive environments in which the network operated. Key to the evolution of the network in their study were the selection of members and distribution of control based on expected rewards, as well as the development of governance structures and a network identity to promote homogeneity and cooperative behavior.
These studies suggested that interactions within networks evolve first from role-based interactions, to interactions based on personal relationships and trust over a series of negotiations. In contrast, van Raak and Paulus (2001) argued that instead of network interactions becoming less formal and more personal over time, the formalization of rules actually increased through a series of negotiations based on the power of actors after a change in the regulatory environment. Thus, although both perspectives consider network evolution to be a process of negotiations among members, the outcomes appear contradictory. In one case, relationships become more personalized over time, whereas in the other, increased formalization seems to occur. However, an analysis by Sydow (2004) helps to reconcile the two perspectives. In his 10-year study of industrial insurance brokers, Sydow focused specifically on the role of evaluation in the evolution of networks. He found that over time, network interactions regarding evaluation shifted from informal to highly formalized and then back to an informal, reflexive monitoring system.
Similar to Sydow (2004), Human and Provan (2000) drew from an institutional perspective to compare the evolution of two networks of small wood manufacturers. Although other studies only alluded to institutional concepts (Ring & Van de Ven, 1994), in their analysis, Human and Provan focused specifically on the building of legitimacy to explain the evolution of networks from the prenetwork field through to network maturity, culminating in the success of one network and the dissolution of another. From their analysis, they concluded that networks must gain legitimacy along three dimensions: network as form, entity, and interaction, drawing support from both internal and external constituencies. Their work tracked this process over time, finding that different approaches to building network legitimacy were most critical at different stages of network evolution, depending on both internal and external needs and demands.
From these studies, it is possible to get a sense of the current understanding of network evolution. Consistent in each study is a combination of internal pressures on organizations to perform their work more effectively and efficiently and external environmental pressure and change. These conditions are instrumental for spurring a group of otherwise autonomous organizations to begin interacting with one another in collaborative ways. These organizations then enter a process of negotiating the purpose and nature of their potential collaboration. Rather than being a clear path toward network growth and governance, the path depends both on key external events that occur as the network evolves and on the influence, incentives, and pressures of the organizations that are involved in the network-building process (Agranoff & McGuire, 2003). Thus, network evolution appears to be a back-and-forth process of coevolution, consistent with the ideas of Koza and Lewin (1999).
Although each of these studies describes some similar patterns of activities and behaviors, there is still considerable uncertainty about network formation and evolution. In particular, the few studies of network evolution offer only a limited understanding of (a) what conditions, both environmental and organizational, might lead to the need for and ultimate emergence of a network, and (b) based on this background, how the emergent network is actually formed and then governed in a way that might lead to accomplishment of network-level goals. Addressing these gaps in the literature is important and is consistent with recent calls expressed by public health scholars for research on network evolution as a key component of understanding and optimizing complex systems (Leischow et al., 2008; NCI, 2007). The health context is especially important for examining the issue of network evolution because in health services, both the sharing of evidence-based knowledge (Ferlie, Fitzgerald, Wood, & Hawkins, 2005) and integration across service areas (Lasker et al., 2001; Provan & Milward, 1995; Weiner & Alexander, 1998) are critical if provision of care is to be optimized while limiting costs. Thus, an understanding of how health networks emerge, evolve, and are governed can be extremely valuable for building and maintaining such networks.
Research Methods
To create the history of the evolution of NAQC, we relied on a variety of sources of information. Specifically, we drew primarily on news articles, journal articles, and the Web sites of NAQC and other tobacco control agencies for information on general quitline, NAQC, and tobacco control history. For a more detailed discussion and interpretation of events, we drew primarily on interviews with two key informants, both of whom were involved throughout the entire network creation process. Each informant played an entrepreneurial role in the network’s formation while they were involved with other organizations that were part of the broader tobacco control community. Each informant was interviewed once and asked a broad series of questions aimed at obtaining their overall impressions and recollections of how NAQC evolved, and the key events that were instrumental in shaping NAQC and the overall quitline movement. On the basis of their information, we then reviewed relevant documents about these key events and included them in our historical time-line. As we developed our thinking, we went back to our informants several times to fill in gaps in knowledge and to confirm or deny our interpretation of events.
Our first informant was initially involved with quit-lines as a director of the Center for Tobacco Cessation, a national project based in Washington, D.C. and funded by the American Cancer Society and the Robert Wood Johnson Foundation. She later went on to become, and continues to be, the first executive director (ED) of NAQC and has played a key role in the formation of the network and in building its legitimacy and viability as a network of relationships among quitlines. Early in the network’s evolution (2000–2005), our second key informant served in a leading role at the NCI as its Tobacco Control Research Branch director and was intimately involved in the formation of NAQC. Before joining NCI, he led the development of a state quitline, and after leaving NCI, he played a key leadership role in that state’s quitline and served in an advisory capacity to NAQC. Although this informant is also a coauthor, similar to Gephart (1978), we made every effort to ensure that his views were not biased by his author role. Specifically, he did not become involved as a coauthor until all the interviews were complete, initial conclusions were made, and the first draft of the article was written. In addition, the final article was thoroughly reviewed for accuracy and consistency of interpretation of findings by our first informant and by another individual who was heavily involved and familiar with the creation of NAQC, conforming to Yin’s (2009) recommendation to corroborate interview data.
Finally, as part of a large, multiyear grant from NCI to study NAQC, we collected quantitative data in summer 2009 from 85 of the 94 organizations participating in quit-lines (90.4% response rate), plus the network’s administrative organization, on their network interactions. Using a Web-based survey, data were collected from key informants in each organization, who were asked to indicate if their organization received information from each of the other quitline organizations (a list was provided) in each of four distinct categories: finances, general management, services, and outreach/promotion. For each category, respondents had to indicate the intensity of that relationship (low, moderate, or high). To enhance the reliability of the data, only moderate- to high-intensity interactions were considered for final analysis. We also collapsed the four categories so that a relationship was present if any of the four links were indicated. The data were coded and analyzed using UCINET 6 (Borgatti, Everett, & Freeman, 2002), a commonly used network analysis software package, and network plots, or graphs, were generated. Unlike the qualitative data, these data were not used to examine network evolution, but rather were used to show the structure of the network once it had evolved to reach relative maturity.
NAQC
North American Quitline Consortium is an international network of organizations and individuals involved in tobacco cessation efforts through the use of quitlines. Quitlines are telephone-based programs designed to help tobacco users quit smoking. Currently, quitlines exist in all 50 states, the District of Columbia, Puerto Rico, Guam, and the 10 Canadian provinces and three territories. Each quitline consists of at least one government funder (usually a department of public health) and a vendor/provider organization that provides the actual services. In 2009, 21 organizations provided quitline services for the 63 funding regions (states, provinces). The number of regions served by any one provider ranged from one to 18. Providers included public universities, nonprofit organizations, and for-profit firms. In addition to funders and providers, other organizations are and have been active members in NAQC, including national governmental organizations like Health Canada (HC), the Centers for Disease Control and Prevention (CDC), foundations, research institutions, and individual tobacco control researchers. When a membership fee was introduced in 2008, 19 organizations chose not to maintain their formal membership in NAQC. However, our research focuses on the full set of 94 quitline organizations because all are considered to be part of the broad network of quitlines, including those that chose not to maintain their official connection to NAQC.
In early 2004, NAQC was officially launched as a special program within the American Legacy Foundation (Legacy), which is a foundation formed as a direct result of the Tobacco Master Settlement. North American Quitline Consortium initially received its funding from a variety of sources, including The American Cancer Society (ACS), the Robert Wood Johnson Foundation, the NCI, the CDC, and HC. It remained a program of the Legacy for 2 years before becoming an independent entity, registering as a nonprofit 501(c)3 corporation in April 2006.
In this current form, NAQC is governed by an 11-member board consisting entirely of individuals active in the quitline community, elected directly by the members themselves. In addition, NAQC has an 18-member advisory committee, consisting of members not currently serving on the board, who focus specifically on program issues. Finally, the network employs two full-time (including the ED) and four part-time employees to work with, coordinate, and advise the various quitline programs and operations. The NAQC governance entity is what Provan and Kenis (2008) have referred to as a network administrative organization (NAO) mode of governance, where a separate and distinct entity is established, not to provide direct services but to facilitate, manage, and govern the network process for, and on behalf of, all network participants. The NAQC NAO also provides information about new quitline practices, collects and disseminates data about the entire network, and represents the needs and concerns of quitline members nationally and internationally. The structure is formalized, decision making is collaborative, and management is professionalized, unlike many networks which are governed either by the participants themselves or by a lead organization (Provan & Kenis, 2008). Over its lifespan, NAQC moved from an informal group of relationships to one with a lead organization and, finally, to its current structure as an independent NAO. To understand the evolution of NAQC, we focus first on the changing environment that gave rise to the quitline phenomenon.
The Evolution of NAQC
Consistent with the ideas of Koza and Lewin (1999) on the coevolution of networks, our data provided evidence that the main factors contributing to the evolution of NAQC were both internal, related to the needs of the quitline organizations themselves, and external, related to changes in the tobacco control environment and the national organizations that helped to shape that environment. Our examination of these internal and external factors led us to conclude, first, that the recognition in the tobacco control community of a problem, a solution, and the need for change in the existing social structure helped to shape a common, shared identity among quitline organizations, leading to the conditions for formation of the network (RQ1). Coevolution also helped to explain the form that the network took, once implemented. Specifically, we found that the diversity of roles in the network, the balance of power in the tobacco control community, and the need to build legitimacy for NAQC influenced how the network was ultimately governed (RQ2).
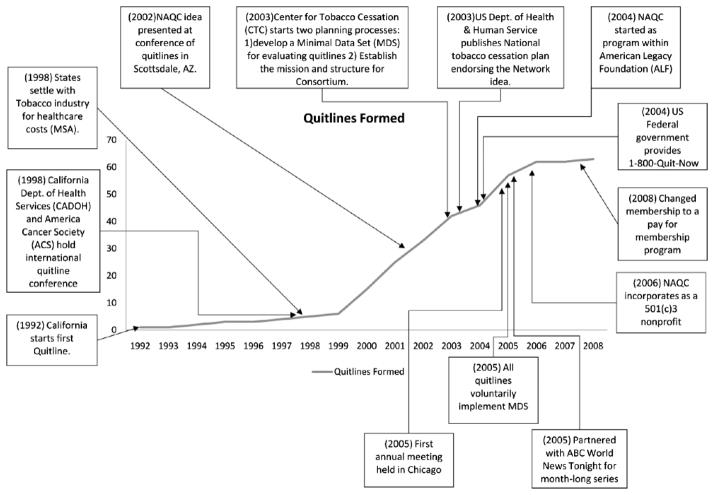
Emergence of a Shared Identity
One theme that has been emphasized by many who have studied goal-directed networks is that developing a shared identity is essential if a network is to be effective (cf. Agranoff and McGuire, 2003; Weiner & Alexander, 1998; Zakocs & Edwards, 2006). We also found this to be the case for NAQC. However, rather than simply stating this as a fact, our evidence pointed to three related factors that contributed to this sense of shared identity over time and, thus, to the eventual formation of the network. Each of these factors is discussed here, with the historical facts underlying them shown in Figure 1. The historical facts were woven together by our key informants and our own interpretation of events to form a coherent picture of why and how the network emerged.
Figure 1.
Evolution of tobacco quitlines with key historical events*
Note: *Vertical axis indicates total number of quitlines.
NAQC = North American Quitline Consortium; MSA = Master Settlement Agreement.
Common problem
The war on tobacco has not always been a unifying force in public health. Although there was awareness of the dangers of tobacco use as early as 1964, when the first report on smoking and health was released by the U.S. Surgeon General, the saliency of the problem in the United States and elsewhere was slow to develop. A year-by-year search for newspaper articles related to tobacco cessation using the Lexis-Nexis database revealed just how long it took for media awareness of the problem to grow. Using tobacco cessation, quitting tobacco, and quit smoking as key words for our search and confining the search to U.S. news media, we found that there was a significant increase in the number of news articles related to tobacco cessation, but not until the mid-1980s. From 1970, when the first “Great American Smokeout” was held, through 1982, the number of articles regarding the topic of quitting smoking remained below 100 per year. It took another 12 years to reach 1,000 articles on the topic annually. Since 1995, the number of news articles related to antismoking has continued to creep upward except for a small dip in 2000 and 2001.
Although a strong antitobacco norm in North America was undoubtedly encouraged through the efforts and informal communications among researchers and national public health policy officials, many of the efforts to combat the problem were conducted independently as various states, federal, and nonprofit organizations conducted their own initiatives. Although the awareness of the problem grew as a result of these efforts, formal collaborations did not expand significantly until the mid-1990s. For example, the first annual conference of the Society for Research on Nicotine and Tobacco was not held until 1994, and the first European Conference on Tobacco and Health was not held until 1998 (Anderson & Zhu, 2007). Once this common problem was clearly identified and then institutionalized, those groups and organizations that were working on the problem could recognize themselves as part of a tobacco control community.
Emergence of a common solution
At the same time as the problem of tobacco use was growing in saliency, organizations were developing many different methods for combating the problem. The ACS was promoting the Great American Smokeout, self-help and support groups were forming, researchers were investigating the effectiveness of various medications, and as early as 1988, some were investigating the use of telephone-based counseling as a means of helping people quit (see Anderson & Zhu, 2007, for a history of quitline practices and recommendations for future practice). While informal communication between organizations working against tobacco use was taking place, the hodgepodge of solutions being attempted meant that there was no real system of tobacco control in place. As a result, organizations throughout the United States, Canada, Europe, and elsewhere mostly addressed the problem independently with little coordination of effort. Although there was general agreement on the goal (i.e., getting people to quit smoking), there was little agreement or consistency in method.
However, in the early 1980s, a toll-free cancer hotline of the Cancer Information Service noticed that a growing number of callers were requesting information on quitting smoking. In response to this demand, the hotline developed the first telephone-based cessation services (Anderson & Zhu, 2007). Shortly thereafter, Quit Victoria in Australia (in 1985) and UK Quit (in 1988) formed the first telephone hotlines in their countries dedicated solely to helping people quit smoking. However, up to this point, no scientific evidence had been gathered to determine the effectiveness of these new programs. With the growing use of this novel technology, researchers began testing the efficacy of various quitline protocols. In 1992, the California Department of Health Services established the first publicly funded quitline in the United States. At the same time, in Washington State, a private insurer developed a private quitline specifically for its members using a different scientifically supported protocol (Ossip-Klein et al., 1991).
Continuing through the 1990s, quitlines such as those in Arizona, Massachusetts, and Nevada began to emerge in North America, as well as in Australia and Europe. In 1998, in response to increasing requests for assistance from prospective quitlines, the California Department of Health Services and the ACS hosted the first international quitline training conference in California. In 1999, the Second European Conference on Tobacco and Health was held, leading to formation of the European Network of Quitlines (ENQ) in 2001, with six initial members. In addition, new research on the effectiveness and reach of quitlines offered an alternative to the face-to-face approaches that were common, as did new technologies like the cellular phone.
While the idea of a quitline community was emerging in North America at the time, including greater interactions among quitline organizations, forming a network was premature, primarily due to the small number of organizations involved and the general lack of cooperation across states and countries. However, the facts that a common problem was now clearly identified and a common solution (i.e., use of quitlines) was becoming widely recognized meant that conditions were becoming favorable for both the rapid growth of quitlines and the need to integrate their activities.
Perceived Need for Change
In November 1998, 46 states reached a settlement with the tobacco industry requiring tobacco companies to make annual payments to the states to cover tobacco-related health care costs. At the time of settlement, the payments were estimated to reach $206 billion over the first 25 years (U.S. General Accounting Office, 2001). The settlement came in the wake of a previous settlement between four states and the tobacco industry, making funds available to all 50 states to combat the tobacco problem becoming ever more salient to the public. By early 2000, the first payments began coming in, and seven states and two provinces started new quitlines. This was the single largest yearly increase in quitlines, doubling the number of state-run quitlines in the United States. In 2001, another 10 quitlines were started in the United States, and by early 2002, when a quitline conference was held in Scottsdale, Arizona, 28 quitlines were in operation in North America.
In Canada, the first smoking helplines/quitlines were started in 1999. The first meeting of all Canadian quit-lines was held in September 2003, and the Canadian Network of Smokers’ Helplines (CNSH) was formed in 2004. The CNSH was initially separate from the U.S. effort and then for a short time was in competition with NAQC for quitline support. By 2007, however, support gradually developed for participation in a broad North American consortium, as long as the unique needs and perspective of the Canadian members could be maintained.
With the rapid growth in quitlines came the awareness that information and communication channels needed to be developed. The increase in the adoption of quitlines among the states led to an increased level of communication within the community as new members were searching out information and guidance on how best to run their particular operations. According to our key informant interviews, and consistent with other reports (Anderson & Zhu, 2007; Cummins, Bailey, Campbell, Koon-Kirby, & Zhu, 2007), this led to a wide variation in the practices adopted by the quitlines. Because an important value within the community was the adherence to strong evidence-based practices (Anderson & Zhu, 2007), the wide variation in the implementation of practices was viewed with concern. With all these changes coming together, when the idea of forming a quitline network was presented at the 2002 meetings in Arizona, it was widely supported (Anderson & Zhu, 2007). From that meeting, the NAQC’s ED, in her former position as the head of the Center for Tobacco Cessation and with funding from multiple sources (ACS, Robert Wood Johnson Foundation, and HC), was charged with moving forward on two key planning processes: “establish the mission and structure for the consortium” and “develop a minimal data set (MDS) for evaluating quitlines” (from an internal memo). Thus, by 2003, conditions were right for the development of a formal quitline network that could span both the United States and Canada. However, the exact form that the network would take, especially how it was to be governed, was not at all clear or widely accepted.
Network Governance Form and Mission
From the data we collected, three factors appeared to have been critical for explaining the actual establishment of NAQC and the NAO network governance form that ultimately emerged: role diversity, building support from the bottom–up, and network mission. To investigate the influence of these factors, it is useful to compare NAQC’s structure and mission with the structure and mission adopted by the ENQ, which formed in 2001.
Role Diversity
As discussed previously, the evolution of quitlines as a solution to an increasingly important public health problem was a worldwide process. Although the idea of using telephone-based counseling and referral as a method for promoting tobacco cessation appears to have originated in the United States, it was the UK and Australia that developed the first quitline organizations (Anderson & Zhu, 2007). In the years since the first quitlines were adopted, members of the worldwide quitline community regularly got together to share information regarding new research and best practices (www.enqonline.org). While these organizations interacted in the same informal network, when it came to formalizing and adopting a network structure, the European and North American organizations chose significantly different structures. Specifically, in 1999, the six European quitlines developed a shared, participative governance structure (Provan & Kenis, 2008) to achieve their objectives. As the network grew, a lead organization form was adopted, with UK Quit listed on their Web site as the “Lead Partner.” In contrast, the eventual formation of a North American quitline network resulted in a more elaborate and brokered NAO structure.
One key reason for the difference in structures had to do with the nature of the organizations participating in the network. The six original members of ENQ were all representatives of sovereign states and were established to fill a similar role in their specific countries. Although there may have been resource differences among the nations, the role of each quitline as a national provider of quitline services reinforced their common identity. This was not the case for NAQC. In a 2006 internal memo to the board, the ED identified at least four roles—researchers, state/provincial funders, federal funders, and service providers—existing in the network and referred to the tensions that were apparent across these groups in trying to execute an important early project. Because of this diversity of participants, neither a participative/shared governance model (due to the large size of the network and very different perspectives) nor a lead organization governance form (no single quitline would ever likely be accepted by all parties as playing a lead role; see Provan & Kenis, 2008) would likely succeed in accomplishing network-level goals. The ED recognized this at an early stage, describing one of the “critical roles of NAQC” as being a “trusted, neutral convener and broker.” To achieve this goal, NAQC had to develop a network governance entity that was viewed as a neutral “third party” that not only recognized the diversity of the network but also was able to draw on this diversity to build the effectiveness of the network as a whole for the benefit of all participants. This resulted in the formation of the NAO structure.
Building Support From the Bottom–Up
A second key factor that we identified from our data for explaining how the NAQC network emerged as it did, especially its governance form, is how support for the network was built. As with the evolution of ENQ and the network of insurance brokers studied by Sydow (2004), significant time elapsed between the recognition of a shared identity, the intention to form a network, and the actual formalization of a governance structure for NAQC. Specifically, just over 2 years elapsed between the 2002 meetings in Arizona and the 2004 formation of NAQC as a program of the American Legacy Foundation. During that time, two processes were taking place. First, a bottom–up network-building process was occurring, led by NAQC’s eventual ED and based on the extensive network of contacts she had developed among the quitlines as head of the Center for Tobacco Cessation. The second was a top–down process led by the Department of Health and Human Services (DHHS) in the United States and by HC. The DHHS approach was designed to create a national network of quitlines that could foster greater standardization and breadth of tobacco treatment. In addition, HC led a top–down process, establishing the CNSH. The CNSH provided funding to support the development and operation of quitlines in six provinces that did not have provincial funding. Health Canada also funded national mass media campaigns and supported local promotional efforts through grants and contribution agreements. Although leaders of both the bottom–up and top–down processes were concerned with promoting tobacco cessation, each took a different approach based on his or her role in the general tobacco control community. Both processes were necessary to accomplish NAQC’s early goals, but they were not compatible as forms of network governance.
As an illustration of the bottom–up strategy, once initial planning began for a North American quitline network, NAQC’s eventual director sought to include as many interested participants as possible in discussions regarding how to develop the mission, goals, and objectives of the network. As she noted in discussions with us:
During the initial “planning” year (2003/2004), we reached out to anyone we thought would be interested in the Consortium (all stakeholder groups) as well as our 1,000 person-plus mailing list from the Center for Tobacco Cessation. These are the people who provided input on the strategic plan for NAQC; mission, goals and objectives; and who helped provide input on the minimal data set. Our strategy was to be as inclusive as possible.
This bottom–up approach was consistent with how the quitline community had evolved informally over the prior 15 years. Although the approach was proving effective in gaining buy-in from the people already interested in quit-lines and tobacco cessation, it was, however, having little impact in getting new states to adopt the quitline technology. After the initial wave of adoptions following the Master Settlement Agreement, the number of states adopting quitline technologies had actually dwindled and the prospects of future new quitlines were bleak.
At the other end of the spectrum, a top–down perspective was also being considered. In an interview with our second key informant, whose assistance was critical for creating NAQC, he noted that during the 2002–2004 planning period, there was considerable discussion among the large national funders about whether a nationally run, centrally controlled quitline might be preferable to a more decentralized network of state quitlines, and if so, which of the various national agencies should be in charge of running it. Thus, the decision about what the new network would look like and how it would be governed was not apparent initially. The outcome would have important implications for who would control network-level decisions.
As part of the top–down strategy, the DHHS had commissioned a researcher from the University of Wisconsin to develop a National Action Plan for Tobacco Cessation (Fiore et al., 2004). In this plan, a number of recommendations were made, one of which was to establish a nationally funded tobacco quitline network by fiscal year 2005. With this recommendation, and in recognition that Congress was unlikely to pass legislation based on the National Action Plan recommendations, the Secretary of Health and Human Services began soliciting the participation of various federal agencies such as NCI and CDC to contribute funding for the network as well as a national “1-800 hotline” that could be used by all state quitlines. However, the Secretary’s efforts were met with some resistance by other federal agencies and national funders who had been forming plans of their own to develop a national quitline.
As a result of considerable discussion and negotiation, particularly between the Office of the Secretary, CDC’s Office on Smoking and Health, and NCI’s Tobacco Control Research Branch, a plan was developed to provide funding to assure that all states in the Unites States would implement a quitline via CDC funding. But the plan was developed in such a way that states could not discontinue their own funding from existing quitlines to access new federal funds to manage a quitline. In addition, a new toll-free number was identified and implemented by NCI (1-800-QUITNOW) that would allow calls made from any state to be automatically transferred to the quitline in that state. Thus, the large national organizations were trying to exert their influence to make the network a truly national endeavor, including a more centralized approach to governing the network.
To foster increased collaboration and communication between the increasing number of state quitlines, the parties finally agreed that a new NAO would be created by the American Legacy Foundation. The organization would be run by a separate entity (the NAO) with its own ED, and not by Legacy staff. Its goals were to create and develop a network of functionally linked quitline organizations to share information on quitline practices, to foster the creation and implementation of an MDS, and to improve the quality of quitline-based intervention. Making early progress on these goals was critical for NAQC’s NAO, first to legitimize the basic idea of a network, which was not necessarily accepted by everyone, and then to legitimize its own (the NAO) existence (cf. Human & Provan, 2000, regarding legitimizing the “network as form” and “network as entity”). In addition, rather than being hierarchically controlled by the NAO and its ED, the network would be highly participative. To ensure that this would be the case, NAQC’s governance structure would include an 11-member elected board and an 18-member advisory committee with participants representing each of the four key stakeholder groups identified earlier.
Thus, despite efforts by the large national organizations to establish a network governed from the top–down, such a model was not supported by the quitlines themselves. The network that emerged was a NAO governance model, which combined bottom–up participation through a board and advisory committee, coupled with facilitation of the network process and a national voice in the tobacco control community through a network ED. The struggles and compromises needed to reach this point in network evolution are illustrative of the tensions and challenges that are likely to emerge in building health networks, as discussed by Weiner and Alexander (1998) and van Raak and Paulus (2001), especially when there is diversity of roles.
Network Mission
The third factor that seemed to be especially important for explaining the development of NAQC and the NAO’s early success in building support among participants was its mission. Because of our focus on goal-directed networks, mission is critical because it is a key factor in distinguishing goal-directed whole networks from other, serendipitous networks. As stated in its Web site (www.naquitline.org/?page=MissionGoals), NAQC’s mission is to serve as a learning organization that:
Maximizes the access, use, and effectiveness of quit-lines in North America;
Provides leadership and a unified voice to promote quitlines; and
Offers a forum to link those interested in quitline operations.
These three points summarize the “neutral broker” NAQC plays as a NAO within the quitline community. The first point exemplifies the overall commitment of the NAO to the network as a whole and its goals, rather than to itself or to a subset of members. It also suggests the buffer role that the NAO plays between the top–down-focused national funders and the smaller state/provincial and private organizations. The second point illustrates the leadership role of the NAO, especially to those outside the network. The final point illustrates the role that the NAO plays in coordinating the flow of information about services, evidence-based practices, funding, and the like, especially among NAQC members, and also to others in the tobacco control community.
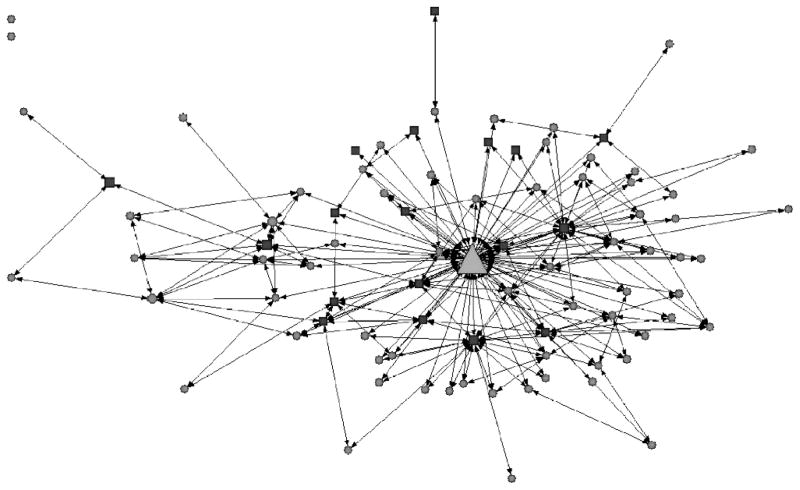
As evidence that NAQC, with its NAO structure, has been successful in accomplishing its mission, the data we have from the first phase of our NCI-sponsored research project indicate a high level of interaction between NAQC’s NAO and the quitline organizations (both funders and providers) regarding the sharing of information about finances, general management, services, and outreach/promotion. Figure 2 shows a network map of these relationships in 2009. The NAO is by far the most central organization in the network, based on both degree and betweenness centrality measures (Bonacich, 1987). In addition, the overall trust of the NAO, as evaluated by respondents in each of the quitline organizations studied, was high, with a mean score on a five-item survey-based trust scale (reliability α = .92) of 3.99 (scale from 1 = little trust to 5 = high trust).
Figure 2.
NAQC network map of reciprocated information sharing ties
Note: N = 86 Quitline organizations plus NAQC’s Network Administrative Organization (large triangle). Squares indicate the provider organizations and circles indicate funder organizations. Node size = betweenness centrality. NAQC = North American Quitline Consortium.
Finally, evidence of network effectiveness can be seen in the development and implementation of an MDS. The MDS is a standard data set for evaluating quitlines. It was the primary focus of one of the original three NAQC working groups, which consisted of members from each of the primary stakeholder groups (researchers, service providers, state/provincial funders, and members of national organizations). Achieving consensus on what would be included in the MDS, as well as getting buy-in from the quitlines to actually complete the annual survey and then being willing to share data across the network, was one of the first major tests of the developing network. The first of the annual surveys to build the MDS was sent out in September 2005, with a 100% response rate. Subsequent years of data have also been successfully completed and shared across NAQC.
Discussion and Conclusions
The goal of this article was to contribute to a deeper understanding of how whole, goal-directed networks evolve, focusing specifically on the example of the NAQC. Using qualitative data from interviews and secondary sources, we have shown how network emergence and its formalization into a NAO governance structure occurred through a process of coevolution. This conclusion is generally consistent with the findings of Human and Provan (2000), Koza and Lewin (1999), Sydow (2004), and others in a business setting; Provan, Huang, and Milward (2009), van Raak and Paulus (2001), and others in health and human services; and the few other scholars who have studied the evolution of goal-directed organizational networks. That is, the network form that ultimately emerges appears to be a product of the back-and-forth interplay between the internal needs and goals of nascent network participants, in this case-, state-, and provincial-level tobacco quitline organizations, coupled with important events and shifts in the external environment, including the impact and influence of major national organizations.
We found that NAQC was able to coalesce and develop as a network by first developing a shared identity around a common problem (tobacco cessation), for which there was a recognized solution (telephone-based counseling and referral) that was rapidly gaining acceptance in the tobacco control community. Within this context, and to establish the network, NAQC then developed a specific governance form, namely, a NAO, that was able to build cooperation and information sharing across a large number of organizations. The final outcome of this network, at least from a structural perspective, was shown using the quantitative network survey data we collected.
Broadly speaking, our findings are consistent with the conclusions of Human and Provan (2000) from their study on the evolution of two networks of small and medium-sized business firms. Both these networks were governed by a NAO. The main reason one network succeeded while the other failed was attributed to the efforts of the NAO and its leadership in building and maintaining legitimacy. Although we did not specifically examine the legitimacy of NAQC, it was clear from our data that NAQC and its NAO could not have been successful in bringing together the many quitlines in both the United States and Canada, as well as important national health organizations and researchers, without having high legitimacy. In this case, legitimacy came from many sources and was built through the efforts of a number of people who occupied leadership roles in both the United States and Canada. Based on our findings, the keys to being able to build sufficient legitimacy both to establish NAQC and to ensure its early success as a network were to draw on the diversity of roles in the network, build support for the network through a bottom–up strategy, and develop and implement a mission that was supportive of, and not in competition with, NAQC members. This mission was to enhance the overall effectiveness and viability of members, primarily through the acquisition and widespread distribution of information about quitline operations and services, enabling quitlines to do their job more effectively.
This research is not without limitations. Most notably, the description of NAQC evolution drew heavily on historical data and the recollections and views of two people who were heavily involved in the quitline movement and the birth and evolution of NAQC. Because this was not a large-scale qualitative study involving multiple interviews plus a systematic document analysis, and because it was a study of the evolution of a single network, the findings and conclusions we drew must be viewed as suggestive. We believe, however, that our assessment of events and our interpretation and categorization of these events are accurate, at least as they pertain to the evolution of NAQC. In addition, our findings, as noted previously, are generally consistent with past work on network evolution in non-health-care settings. The broader generalizability of our conclusions awaits additional work by researchers of other health networks.
Practice Implications
By focusing on NAQC, we have demonstrated how public health networks can be created and evolve successfully when organizational participants are widely scattered geographically and where individual organizations in the network must be responsive to strong but highly varied local pressures and expectations, in this case, from the states and provinces that fund each quitline. Our findings provide evidence that the successful creation of such a network is not only influenced by external conditions in the health care setting, but that governance, especially, involves addressing such issues as role diversity and the tensions that are likely to emerge from both bottom–up (i.e., participant initiated) and top–down efforts to shape the network. Thus, our work has important implications for practice regarding the evolution of other national or international networks in health, which may be critical for addressing such complex and widespread health problems as obesity, serious mental illness, substance abuse, pandemic outbreaks, and chronic disease. Of course, expansion of the quitline network concept into non-tobacco health issues would require adaptation to fit the setting and the nature of the particular problem being addressed. Our work here provides evidence of how such networks might be successfully established and governed in a way that encourages the autonomy of individual organizational participants while still ensuring that overall public health and network-level goals are achieved. Balancing this tension between narrow/organizational-and broad/network-level goals (Agranoff & McGuire, 2003; Huxham & Vangen, 2005) is something that public health and other health policy and management officials will need to address as they tackle the nation’s major public health concerns.
In this regard, as noted earlier, one important component of the new Affordable Care Act is the implementation of so-called ACOs (McClelland et al., 2010). Although much of the discussion of ACOs has focused on integrated, owned systems such as Geisinger, Mayo, and Kaiser, for the most part, these ACOs will not, in fact, be organizations at all, but rather multiorganizational networks consisting of independent health providers operating along the continuum of care. The goal is to get these organizations to work together to share information and improve service quality at the same time as slowing growth in spending. How these ACO networks would actually be established and evolve is not at all clear, however. The research we have conducted on the evolution of NAQC may provide some useful insights to both local health managers and national health officials about the complexities of forming, organizing, and governing ACOs and other types of integrated health systems.
Acknowledgments
Work on this article was funded by a grant from the National Cancer Institute (R01CA128638-03, with additional support from grant CCSG-CA023074).
The authors thank Linda Bailey and Sharon Campbell for their invaluable recollections, suggestions, and comments. They would also like to thank Gregg Moor and Jessie Saul for their overall contributions to the project.
Footnotes
The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
Contributor Information
Keith G. Provan, Email: kprovan@eller.arizona.edu, McClelland Professor of Management and Organizations, Eller College of Management and School of Government and Public Policy, University of Arizona, Tucson.
Jonathan E. Beagles, PhD Student, School of Government and Public Policy, University of Arizona, Tucson.
Scott J. Leischow, Professor, Family and Community Medicine, Arizona Cancer Center, University of Arizona, Tucson.
References
- Agranoff R, McGuire M. Collaborative public management: New strategies for local governments. Washington, DC: Georgetown University Press; 2003. [Google Scholar]
- Anderson CM, Zhu SH. Tobacco quitlines: Looking back and looking ahead. Tobacco Control. 2007;16(Suppl I):i81–i86. doi: 10.1136/tc.2007.020701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahr DB, Browning RC, Wyatt HR, Hill JO. Exploiting social networks to mitigate the obesity epidemic. Obesity. 2009;17:723–728. doi: 10.1038/oby.2008.615. [DOI] [PubMed] [Google Scholar]
- Bechky B. Gaffers, gofers, and grips: Role-based coordination in temporary organziations. Organization Science. 2006:3–21. [Google Scholar]
- Bonacich P. Power and centrality: A family of measures. American Journal of Sociology. 1987;92:1170–1182. [Google Scholar]
- Borgatti SP, Everett M, Freeman L. Ucinet for Windows: Software for social network analysis. Harvard, MA: Analytic Technologies; 2002. [Google Scholar]
- Chaskin RJ, Brown P, Venkatesh S, Vidal A. Building community capacity. New York: Aldine; 2001. [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. New England Journal of Medicine. 2008;358:2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins SE, Bailey L, Campbell S, Koon-Kirby C, Zhu SH. Tobacco cessation quitlines in North America: A descriptive study. Tobacco Control. 2007;16(Suppl I):i9–i15. doi: 10.1136/tc.2007.020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Aunno TA, Zuckerman HS. A life-cycle model of organizational federations: The case of hospitals. Academy of Management Review. 1987;12:534–545. [PubMed] [Google Scholar]
- Ferlie E, Fitzgerald L, Wood M, Hawkins C. The (non) spread of innovations: The mediating role of professionals. Academy of Management Journal. 2005;48(1):117–134. [Google Scholar]
- Fiore MC, Croyle RT, Curry SJ, Cutler CM, Davis RM, Gordon C, –Baker TB. Preventing 3 million premature deaths and helping 5 million smokers quit: A national action plan for tobacco cessation. American Journal of Public Health. 2004;94:205–210. doi: 10.2105/ajph.94.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gephart RP. Status degradation and organizational succession: An ethnomethodological approach. Administrative Science Quarterly. 1978;28:553–581. [Google Scholar]
- Human SE, Provan KG. Legitimacy building in the evolution of small firm multilateral networks: A comparative study of success and demise. Administrative Science Quarterly. 2000;45:327–365. [Google Scholar]
- Huxham C, Vangen S. Managing to collaborate. London: Routledge; 2005. [Google Scholar]
- Kilduff M, Tsai W. Social networks and organizations. London: Sage Press; 2003. [Google Scholar]
- Koza MP, Lewin AY. The coevolution of network alliances: A longitudinal analysis of an international professioal service network. Organization Science. 1999;10:628–653. [Google Scholar]
- Lasker R, Weiss ES, Miller R. Partnership synergy: A practical framework for studying and strengthening the collaborative advantage. Milbank Quarterly. 2001;79:179–205. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leischow SJ, Milstein R. Systems thinking and modeling for public health practice. American Journal of Public Health. 2006;96(3):403–405. doi: 10.2105/AJPH.2005.082842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leischow SJ, Best A, Trochim WM, Clark PI, Gallagher RS, Marcus SE, Matthews E. Systems thinking to improve the public’s health. American Journal of Preventive Medicine. 2008;35(2):S196–S203. doi: 10.1016/j.amepre.2008.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland M, McKethan AN, Lewis JL, Roski J, Fisher E. A national strategy to put accountable care into practice. Health Affairs. 2010;29:982–990. doi: 10.1377/hlthaff.2010.0194. [DOI] [PubMed] [Google Scholar]
- NAQC. n. d Retrieved December 10, 2009, from the North American Quitline Consortium Web site: http://www.naquitline.org.
- National Cancer Institute. Greater than the sum: Systems thinking in tobacco control. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2007. (Tobacco Control Monograph No. 18) NIH Pub. No. 06-6085. [Google Scholar]
- Ossip-Klein DJ, Giovino GA, Megahed N, Black PM, Emont SL, Stiggins J, –Moore L. Effects of a smokers’ hotline: Results of a 10-county self-help trial. Journal of Consulting and Clinical Psychology. 1991;59:325–332. doi: 10.1037//0022-006x.59.2.325. [DOI] [PubMed] [Google Scholar]
- Provan KG, Fish A, Sydow J. Interorganizational networks at the network level: A review of the empirical literature on whole networks. Journal of Management. 2007;33:479–516. [Google Scholar]
- Provan KG, Huang K, Milward HB. The evolution of structural embeddedness and organizational social outcomes in a centrally governed health and human services network. Journal of Public Administration Research and Theory. 2009;19:873–893. [Google Scholar]
- Provan KG, Kenis P. Modes of network governance: Structure, management, and effectiveness. Journal of Public Administration Research and Theory. 2008;18:229–252. [Google Scholar]
- Provan KG, Milward HB. A preliminary theory of interorganizational network effectiveness: A comparative study of four community mental health systems. Administrative Science Quarterly. 1995;40:1–33. [Google Scholar]
- Ring PS, Van de Ven AH. Development processes of cooperative interorganizational relationships. Academy of Management Review. 1994;19:90–118. [Google Scholar]
- Sydow J. Network development by means of network evaluation? Explorative insights from a case in the financial services industry. Human Relations. 2004;57:201–220. [Google Scholar]
- U.S. General Accounting Office. Tobacco settlement L states’ use of master settlement agreement payments (GAO-01-851) Wasington D.C: U.S. Government Printing Office; 2001. [Google Scholar]
- van Raak A, Paulus A. A sociological systems theory of interorganizational network development in health and social care. Systems Research and Behavioral Science. 2001;18:207–224. [Google Scholar]
- Weiner BJ, Alexander JA. The challenges of governing public-private community health partnerships. Health Care Management Review. 1998;23(2):39–55. doi: 10.1097/00004010-199804000-00005. [DOI] [PubMed] [Google Scholar]
- Yin RK. Case study research. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- Zakocs RC, Edwards EM. What explains community coalition effectiveness? A review of the literature. American Journal of Preventive Medicine. 2006;30:351–361. doi: 10.1016/j.amepre.2005.12.004. [DOI] [PubMed] [Google Scholar]