Abstract
Background
In Canada, the rise of private-pay assisted living facilities is changing the long-term care landscape. Even so, few clinical implications of having these facilities in the spectrum of care have been studied. Our objective was to compare events and symptoms that might predispose and precipitate a move of older adults to assisted living or to a nursing home.
Methods
Cross-sectional, descriptive Nova Scotia survey of residents and family members on admission. Health-care use and dementia diagnosis were recorded from the admission record. Dementia was staged using the Global Deterioration Scale and the Dependence Scale. The SymptomGuide, a standardized dementia symptom inventory, was used to assay which symptoms were most influential in the decision to seek long term care. Caregiver stress was elicited by a self-report questionnaire.
Results
Of 353 people admitted during the enrolment period, 174 (49%) took part in the survey. Most (97; 55.7%) were involved in a move from the community to a nursing home, 54 (31.0%) from the community to assisted living, and 23 (13.2%) from assisted living to a nursing home. In each setting, dementia was the commonest predisposing factor (seen in >90%) with a precipitating event seen in 120 (69%) people. The precipitating events included a medical illness (n = 97; 55%) or caregiver illness, death or move (33; 19%). Dependence was associated with place of care, with more severely impaired people more commonly represented in people who moved to nursing homes.
Conclusions
People move from the community chiefly due to dementia, and often with a precipitant. Compared with a move to assisted living, moving to nursing homes generally indicates greater dependence, and typically worse dementia severity. Even so, assisted-living facilities are not just for the “worried well”, but are used by people with dementia, caregiver stress, and recent hospitalization.
Keywords: aging, dementia, long-term care, hospitalization, frailty
INTRODUCTION
In Canada, as in much of the western world, institutional long-term care continues to occupy an important part of the care spectrum for older adults, especially those with dementia.(1) Such care is provided in several settings, including acute care hospitals.(2) Even so, the spectrum of care is changing, particularly with the advent of fully private assisted living facilities.(3) Such facilities offer “shelter and care to physically and cognitively frail older persons … offering a protected residential living arrangement, with 24-hour awake staff, meals, congenial social situations, scheduled and unscheduled help with everyday activities, medication management and sometimes health or nursing related services”.(4)
How assisted living is impacting health care is unclear.(4) Advocates point to its ability to provide care more in line with client/patient expectations, and to free up capacity in publically funded long-term care. Sceptics discount each part of this, as well as the desirability of the latter. Understanding the impact on dementia care can be helpful in understanding how assisted living fits. In general, dementia is a potent risk for admission to institutional care.(5,6) Whether this remains so in the face of a growing assisted living sector is not clear. Given that population projections suggest that demand will outstrip projected supply in relation to the need for institutional care for people with dementia,(3) it is important to understand their place in the spectrum of care.
Assisted living facilities typically apply entry requirements which favour people with less dependence, fewer needs, and the financial means to purchase private care within a supervised setting. Even so, dementia illnesses tend to be progressive, which might account for why variability in care needs of people who reside in assisted living facilities is common; many have marked dependency,(7) often reflecting an ability to pay for additional services.(4)
To begin to understand where assisted living facilities fit in the Canadian care continuum, we were interested to understand care profiles of people as they were moved from the community either into assisted living or nursing homes, and of people moved from assisted living into nursing homes. In this exploratory, descriptive study we focused on profiles of need, as well as on events associated with such a move. Specifically, our objective was to describe events and symptoms that might predispose and precipitate a move of older adults to assisted living, compared with a move to a nursing home.
METHODS
Design, Setting, Sample
The sample came from ten nursing homes and five assisted living facilities, all in Nova Scotia. For eight nursing homes and three assisted living facilities, the data came from the admission interview, using health record, facility interview, and personal interview data. For the remainder, interviews were conducted by one of us (KR) with a memory clinic nurse. All data came from patients and family members (who were typically care partners). For people who had moved from an assisted living facility to a nursing home, information about which symptoms prompted the move was provided by the staff member responsible for resident discharge/transfers. As an exploratory study, we sought to evaluate about 200 subjects, including at least 50 from assisted living. The sample was estimated to allow for both an estimation of the proportion with moderate severe dementia in nursing homes (assumed to be 60% ± 10%, with power = 0.8 and alpha = 0.05) and estimation of at least a two-fold difference in the proportion with moderate-to-severe dementia, assuming that such people constituted 60% of the nursing home fraction.(8) Individuals were recruited over a two-month period from March 2011 to May 2011.
Instruments
Diagnosis of the cognitive state came from the Medical Admission Form, which requires this information. Staging followed the Global Deterioration Scale (GDS).(9) The GDS recognizes 7 stages of cognitive impairment, from 1 (no subjective or objective impairment) to 3 (equivalent to Mild Cognate Impairment – MCI), 4 (mild dementia), 5 (moderate dementia), 6 (moderately severe dementia), and 7 (severe dementia). In addition, based on the interview, the resident’s level of dependency was scored using and the Dependence Scale.(10) The Dependence Scale is scored using an algorithm that counts responses to 13 questions about patient dependence and need for care and supervision; scores range from 0–15, with a higher score indicating worse dependence. The SymptomGuide,(11) a standardized dementia symptom inventory, was used to assay which symptoms were most influential in the decision to seek long term care. It has been validated clinically, and against the Dependence Scale.(12) The symptom interview also distinguished between symptoms that predisposed towards the decision to move and those that might have precipitated the move. Recognizing that some symptoms could be both predisposing and precipitating, we also asked about worsening in relation to the decision to move. Any events that arose at the time of the decision to move, as well as information about caregiver stress, were elicited by a self-report questionnaire.
Analysis
We chiefly report descriptive statistics. To test differences between admission by residence status (assisted living; nursing home from community or assisted living), we used analysis of variance for differences in means and chi-square for differences in proportions.
Ethics
All patients provided written informed consent. The protocol was approved by the Research Ethics Committee of the Capital District Health Authority, Halifax, Nova Scotia.
Sponsorship
Given the potential for identification of participants due to small numbers, the data are not disaggregated to levels with fewer than five people, and where numbers are only slightly larger, we report approximate proportions rather than exact numbers. The study was sponsored by Pfizer Canada and DGI Clinical, which produced a report on which this paper is based. Additional funds for write-up came from the DGI Clinical, Inc., of which KR is founder and a shareholder, and from the Dalhousie Medical Research Fund, which provides career support to KR as the Kathryn Allen Weldon Professor of Alzheimer Research. The Principal Author (KR) has access to all data and takes responsibility for every part of the paper.
RESULTS
During the recruitment period, 353 people were admitted, of whom 174 (49%) took part in the survey. Most (97, 56%) moved from the community to a nursing home, 54 (31%) from the community to assisted living, and 23 (13%) from assisted living to a nursing home. In each setting, dementia was seen in most people, who typically were women in the ninth decade (Table 1). Only a minority of people who moved to nursing homes were taking anti-dementia drugs (usually a cholinesterase inhibitor), compared with just over two-thirds of those admitted to an assisted living facility (Table 1).
TABLE 1.
Demographic and clinical characteristics of the sample
| Community to Assisted Living Facility (n = 54) | Community to Nursing Home Facility (n = 97) | Assisted Living to Nursing Home Facility (n = 23) | |
|---|---|---|---|
| Average Age (Standard Deviation) | 85.3, (6.4) | 83.1, (6.5) | 85.2, (6.5) |
| % Female | 69.10% | 79.10% | 83.30% |
| Diagnosed with Dementia | 83% | 91% | 23 (100%) |
| Taking Anti-Dementia Drug(s) | 71% | 42% | 43% |
Predisposing Factors
Dementia Stage
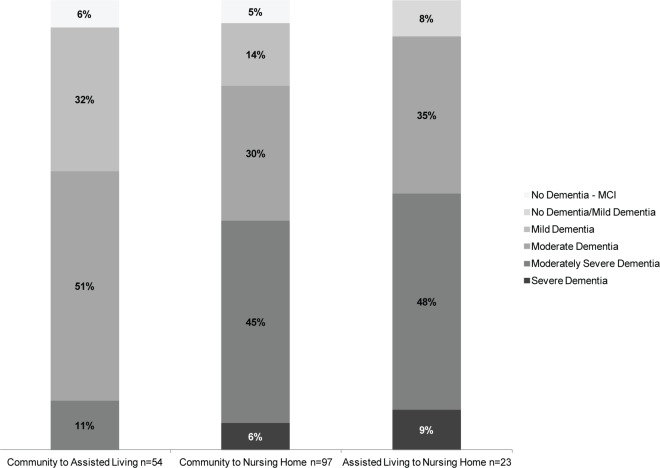
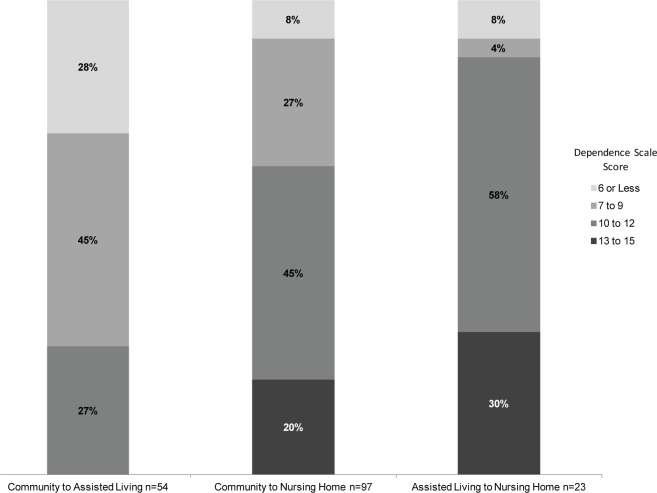
In each setting, most newly admitted people had at least moderate dementia; the proportion with moderately severe to severe dementia was highest (just over half) in nursing homes (Figure 1). Similarly, most people who moved to nursing homes showed marked dependency (scores ≥ 10; Figure 2).
FIGURE 1.
Dementia stage in relation to destination and residence
Note that due to small numbers, the categories No Dementia, MCI, and Mild Dementia were combined in people moving from assisted living to a nursing home.
FIGURE 2.
Dementia stage in relation to dependence scale prior to admission
Predisposing Symptoms
The symptoms that most predisposed to a move reflect chiefly dementia, but also problems in mobility and balance. In keeping with the data on dementia staging independence, there is little overlap in the ten most common symptoms across settings; indeed, only one (impaired recent memory) is shared by all three (Table 2). People moving to a nursing home commonly showed signs of worse dementia, and particularly impaired executive function in those moving from assisted living.
TABLE 2.
Predisposing symptoms leading to transfer
| Symptoms | Community to Assisted Living Facility (n = 54) | Community to Nursing Home Facility (n = 97) | Assisted Living to Nursing Home Facility (n = 23) |
|---|---|---|---|
| Problems with Recent Memory | 44% | 34% | 26% |
| Poor Personal Care/Hygiene | 26% | 43% | |
| Mobility Problems | 25% | 35% | |
| Disorientation to Time | 21% | 30% | |
| Balance Problems | 35% | ||
| Incontinence | 30% | ||
| Judgement | 30% | ||
| Disorientation to Place | 26% | ||
| Impaired Comprehension/Understanding | 22% | ||
| Impaired Memory for Names and Faces | 21% | ||
| IADL Impairment | 22% |
Caregiver Factors
Caregivers (or their survivors) reported important predisposing factors in the great majority (93%) of nursing home admission, and in 43% of transfers from community to assisted living (p < .01). For individuals transferring from community to nursing homes, most (71%) of the transfers were caused by caregiver stress. The trend was not significantly different for community to assisted living (with stress cited in 65% of transfers).
Precipitating Factors
Worsening of Medical Condition
Although dementia stage typically changes gradually, acute medical illnesses from which the patient does not recover, with or without a formal diagnosis of delirium, appear to be common. Indeed, in 59% of individuals who moved from the community to a nursing home, a medical illness was identified as being associated with the move. Likewise, half of those who transferred from community to assisted living cited a medical condition, as did half of those who transferred from assisted living to a nursing home.
Hospital Use
Despite medical illnesses being associated with just over half of all moves, fewer moves (about one third) directly followed hospitalization. Of the individuals who had transferred from the community to a nursing home, 32% had been in a hospital for less than one month, 27% from 1 to 2 months, and 42% for more than 2 months. This last is longer than what was seen with transfers to from the community to assisted living, where only 8% stayed in hospital for more than two months before admission. Even so, only 17% moved within a month, and 75% after having been hospitalized for 1 to 2 months. People moving from assisted living to a nursing home who were admitted to hospital were roughly evenly distributed between stays of less than one month, 1–2 months, and more than 2 months.
Precipitating Symptoms
In general, people identified fewer precipitating than predisposing symptoms. This was especially the case for transfers from assisted living to long-term care, where only one symptom (poor personal hygiene) occurred commonly enough to be reported (i.e., occurred in more than five people). This factor would not be welcome by other residents of the private facility. Of the other most common symptoms, only one overlapped between those entering a nursing home and those moving to assisted living. Impaired IADLs (especially meal preparation) was the single, most common symptom to precipitate a move, seen in about one in five people.
Caregiver Events
Transfer from the community to a nursing home was often associated with caregiver illness or death (19%). Other caregiver precipitants chiefly were a move (or other cause of unavailability) of the caregiver (10%). These proportions were not significantly different from those moving to assisted living. Caregiver factors had little influence on the move to nursing homes from assisted living facilities.
Wait Time for Admission
Wait times to move from the community to a nursing home were on average longer (4.5 months ± standard deviation = 3.7 months) than the waits for a move to assisted living (1.1 ± 0.7 months, p < .01). The wait for transfer from assisted living to nursing homes was 4.4 (± 5.1 months). Times spent in hospital are not included in these estimates.
DISCUSSION
In this exploratory, descriptive survey of people who had newly moved to a nursing or an assisted living facility, we found that moderate (or more severe) dementia was common in both settings. For people who were moving from the community, in each setting, either or both of a worsening of dementia or a medical illness was common, as was a change in caregiver health or availability. A common pathway out of the community was via the acute care hospital. Although assisted living facilities are sometimes advertised and seen as for people at risk (the “worried well”(4)), our data suggest that, at least in Nova Scotia, they commonly are used by people with dementia, caregiver stress, and recent hospitalization.
In Nova Scotia, public home care services are task-related, rationed, and wait-listed due to shortages of home support staff to provide the care. As a consequence, people with the financial means to do so can arrange for care in the home at a level that can forestall placement in a nursing home facility. In that context, assisted living facilities, which offer housekeeping, meals, medication, laundry, and supervision, are a viable competitor. Although they are typically more expensive than care in the home, mitigating factors include the ability to capitalize assets by selling the house; again, this is an option for those who can afford it. Typical base charges vary, but one facility offers many levels of Assisted Living within different residences or Halls, and also by room size. Rates vary from entry level $2,415–$4,180 (1 meal), $2,940–$4,125 (3 meals + medication administration), $3,780–$4,260 (meds + ADL), $4,410–$4,595 (licensed care), $7,410–$8,340 (dementia care). Costs can go higher if additional services are purchased.
By contrast, the costs of nursing home placement are shared between the Department of Health and Wellness and the patient, with consideration for the remaining spouse. The nursing home fee is based on income, and calculated on a sliding scale to maximum cost that a patient would pay as $102.50 daily or $3,075 monthly.
Our data must be interpreted with caution. At 174, the sample size is slightly smaller than had anticipated, but still large enough for the sample size calculations. All the data come from a single province, making generalizability uncertain. In addition, we relied chiefly on self-report data, and emphasized symptoms and functions over cognitive test scores. Many cognitive screening tests lack information about executive dysfunction,(13) which can powerfully contribute to caregiver stress and to institutionalization.(2) Despite these issues, the preponderance of moderate-to-severe dementia often exposes commonly used cognitive test scores to significant floor effects, so that staging that employs function has long been recognized as appropriate, and often preferred.(14,15) We did not have data on individual income, except for the general point that admission to assisted living is a private-pay option for which people commonly are required to have sufficient funds for at least one year.
We did not have enough information to document the sequence of how medical illness and hospitalization were related to the move from the community. Clinically, several patterns are seen. Someone with mild dementia, on a stable course, has sudden worsening. It might be due to delirium, or some other factor, but the suddenness of the change prompts hospitalization. Once in hospital, the viability of continuing to stay at home is questioned, either because the problem does not settle, or the caregiver can no longer cope, or a risk-adverse institution or team does not want to discharge the patient home, especially if the patient will spend significant parts of the day alone. Understanding which of these forces come into play, and how often they exist, is vital to seeing how they might be changed—and a focus for further inquiry. Likewise, the interpretation of why there were fewer precipitating events in people who had moved from assisted living to a nursing home is not clear; given that there is no public subsidy for assisted living, financial incentives seem likely, but again this requires additional detail and further study. Such inquiry would be in keeping with the proposal that local areas carefully review their own service networks to identify potential gaps or obstacles to effective dementia care, including effective flow through the health-care system.(16)
The proportion of people for whom caregiver illness, death or absence precipitated a move was substantial in our study, with 59% of respondents reporting that caregiver-related factors contributed to the move—chiefly stress and, to a lesser extent, caregiver death, illness or unavailability. Even so, the figure was smaller than what was described in a 1994 study from Nova Scotia, where caregiver death or illness was the most common caregiver factor.(17) It also contrasts with a report that people choose private dwelling types based more on social than health characteristics.(18) That study analyzed data from 2002; so, like the 1994 report, it might reflect change in how such facilities are being used.
The relationship between more advanced dementia, precipitating symptoms, and events and breakdown in community support is not surprising, as this is a routine part of the landscape, in Canada and elsewhere.(2) How the long-term care sector is evolving does not always appear to reflect this reality. Many long-term care facilities feel that they cannot readily cope with people with more advanced dementia, especially those with behavioural and psychological symptoms of dementia. As assisted living facilities become a more common part of the landscape, their ability to provide care for people with more severe dementia will be important to offering care to that part of the population. This will require relevant training for their care workers and front line staff throughout the long-term care sector, many of whom feel that such care affects their own emotional wellbeing.(19) There also appear to be opportunities to provide care in assisted living more efficiently. For example, at present, the care requirement posed by dementia patients with behavioural problems is often met in assisted living facilities by one-on-one help from personal care workers. This is an expensive means of providing care, but for some people, is viable. For others, the amount of care can be reduced as the symptoms settle, either spontaneously or as the result of intervention. Regardless, the remedy of constant one-on-one care can exhaust funds quickly. When funds run out, patients commonly are admitted to nursing homes, often via an acute care hospital, where under the designation of being “subacute” patients, they can spend weeks or months.(20) Formally understanding that people with moderate-to-moderately severe dementia are a common constituency of assisted living, and that the natural history includes progression and a higher risk of behavioural problems, might allow insights into how best to structure public policy, including policies about transfers to the acute care hospital. Such considerations are motivating additional inquires by our group.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors declare that no conflicts of interest exist.
REFERENCES
- 1.Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int Psychogeriatr. 2010;22(7):1025–39. doi: 10.1017/S1041610210000608. [DOI] [PubMed] [Google Scholar]
- 2.Health Quality Ontario Caregiver- and patient-directed interventions for dementia: an evidence-based analysis. Ont Health Technol Assess Ser. 2008;8(4):1–98. [PMC free article] [PubMed] [Google Scholar]
- 3.Canadian Life and Health Insurance Association inc . CLHIA report on long-term care policy: improving the accessibility, quality and sustainability of long-term care in Canada. Toronto, ON: CLHIA; 2012. Available from: http://www.clhia.ca/domino/html/clhia/CLHIA_LP4W_LND_Webstation.nsf/resources/Content_PDFs/$file/LTC_Policy_Paper.pdf Accessed 2013 June 7. [Google Scholar]
- 4.Golant SM, Hyde J, editors. The assisted living residence: a vision for the future. Baltimore, MD: The John Hopkins University Press; 2008. [Google Scholar]
- 5.Rockwood K, Stolee P, McDowell I. Factors associated with institutionalization of older people in Canada: testing a multifactorial definition of frailty. J Am Geriatr Soc. 1996;44(5):578–82. doi: 10.1111/j.1532-5415.1996.tb01446.x. [DOI] [PubMed] [Google Scholar]
- 6.Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39(1):31–38. doi: 10.1093/ageing/afp202. [DOI] [PubMed] [Google Scholar]
- 7.Golant SM. Do impaired older persons with health care needs occupy U.S. assisted living facilities? An analysis of six national studies. J Gerontol B Psychol Sci Soc Sci. 2004;59(2):S68–79. doi: 10.1093/geronb/59.2.S68. [DOI] [PubMed] [Google Scholar]
- 8.Kelsey JL, Whittemore AS, Evans AS, et al., editors. Methods in observational epidemiology. 2nd edition. Oxford: Oxford University Press; 1996. Methods of sampling and estimation of sample size, Chap. 12. [Google Scholar]
- 9.Reisberg B, Ferris SH, de Leon MJ, et al. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–39. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 10.Stern Y, Albert SM, Sano M, et al. Assessing patient dependence in Alzheimer’s disease. J Gerontol. 1994;49(5):M216–22. doi: 10.1093/geronj/49.5.M216. [DOI] [PubMed] [Google Scholar]
- 11.Rockwood K. An individualized approach to tracking and treating Alzheimer’s disease. Clin Pharmacol Ther. 2010;88(4):446–49. doi: 10.1038/clpt.2010.68. [DOI] [PubMed] [Google Scholar]
- 12.Rockwood K, Zeng A, Leibman C, et al. Validation of an informant-reported web-based data collection to assess dementia symptoms. J Med Internet Res. 2012;14(2):e42. doi: 10.2196/jmir.1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ismail Z, Mulsant BH, Herrmann N, et al. Canadian Academy Of Geriatric Psychiatry survey of brief cognitive screening instruments. Can Geriatr J. 2013;16(2):54–60. doi: 10.5770/cgj.16.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen-Mansfield J, Reisberg B, Bonnema J, et al. Staging methods for the assessment of dementia: perspectives. J Clin Psychiatry. 1996;57(5):190–98. [PubMed] [Google Scholar]
- 15.Desai AK, Grossberg GT, Sheth DN. Activities of daily living in patients with dementia: clinical relevance, methods of assessment and effects of treatment. CNS Drugs. 2004;18(13):853–75. doi: 10.2165/00023210-200418130-00003. [DOI] [PubMed] [Google Scholar]
- 16.Aminzadeh F, Molnar FJ, Dalziel WB, et al. A review of barriers and enablers to diagnosis and management of persons with dementia in primary care. Can Geriatr J. 2012;15(3):85–94. doi: 10.5770/cgj.15.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glazebrook K, Rockwood K, Stolee P, et al. A case control study of the risks for institutionalization of elderly people in Nova Scotia. Can J Aging. 1994;13(1):104–17. doi: 10.1017/S0714980800006590. [DOI] [Google Scholar]
- 18.Perks T, Haan M. The dwelling-type choices of older Canadians and future housing demand: an investigation using the Aging and Social Support Survey (GSS16) Can J Aging. 2010;29(3):445–63. doi: 10.1017/S0714980810000413. [DOI] [PubMed] [Google Scholar]
- 19.Cook C, Fay S, Rockwood K. A meta-ethnography of paid dementia care workers’ perspectives on their jobs. Can Geriatr J. 2012;15(4):127–36. doi: 10.5770/cgj.15.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elbourne HF, Hominick K, Mallery L, et al. Characteristics of patients described as sub-acute in an acute care hospital. Can J Aging. 2013;32(2):203–06. doi: 10.1017/S0714980813000214. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]