Abstract
We describe two frameworks in which personality dimensions relevant to health, such as Conscientiousness, can be used to inform interventions designed to promote health aging. First, contemporary data and theory do not suggest that personality is “immutable”, but instead focus on questions of who changes, in what way, why, when, and how. In fact, the notion that personality could be changed was part and parcel of many schools of psychotherapy, which suggested that long term and meaningful change in symptoms could not be achieved without change in relevant aspects of personality. We review intervention research documenting change in personality. Based on an integrative view of personality as a complex system, we describe a “bottom-up” model of change in which interventions to change basic personality processes eventuate in changes at the trait level. A second framework leverages the descriptive and predictive power of personality to tailor individual risk prediction and treatment, as well as refine public health programs, to the relevant dispositional characteristics of the target population. These methods dovetail with and add a systematic and rigorous psychosocial dimension to the personalized medicine and patient-centeredness movements in medicine. In addition to improving health through earlier intervention and increased fit between treatments and persons, cost-effectiveness improvements can be realized by more accurate resource allocation. Numerous examples from the personality, health, and aging literature on Conscientiousness and other traits are provided throughout, and we conclude with a series of recommendations for research in these emerging areas.
Keywords: personality, intervention, health, personality change, lifespan
Personality Change and Public Health
The Big Five dimension of Conscientiousness (hereafter “C”), a family of interrelated traits reflecting industriousness, order, self-control, responsibility, traditionalism, and virtue (Roberts et al., 2005), has emerged as one of the most important personality factors in lifespan health (B. W. Roberts, Kuncel N., Shiner R. N., Caspi A., & Goldberg, 2007). Presuming that personality tendencies are, like other human attributes, normally distributed in the population, roughly 16% of people in the US fall at minus one standard deviation or lower in C. A risk factor with both strong links to numerous pernicious outcomes and substantial prevalence is particularly concerning from a population health perspective (Rothman, 2008).
An equally strong set of findings has accumulated over the last decade suggesting that personality is much more malleable naturalistically than was believed during the 1980s and 1990s (Roberts 2000, 2006). The presence of change in the absence of intervention raises intriguing question about the kind of change possible with interventions. This article lays out a framework for personality-informed interventions to promote healthy aging.
Personality has been called “The last bastion of the generalist” in psychology (Revelle, 2011) because it encompasses such a wide subject matter. While the Big 5 C dimension is important, it is embedded in the broader personality system, several other elements of which have implications for healthy aging. Beginning with general principles, most define personality as individual differences in thought, behavior, and affect that are relatively stable over time and across situations. Although a dizzying variety of “camps” or paradigms have appeared in personality research, modern views favor an integration of trait, social cognitive process, personal narrative and self-identity, psychodynamic, motivational, and other approaches to personality (McAdams & Pals, 2006). We invoke these distinctions only when relevant, and use terms such as personality qualities, dispositions, characteristics, elements, patterns, and habits to refer to general aspects of the integrated personality system.
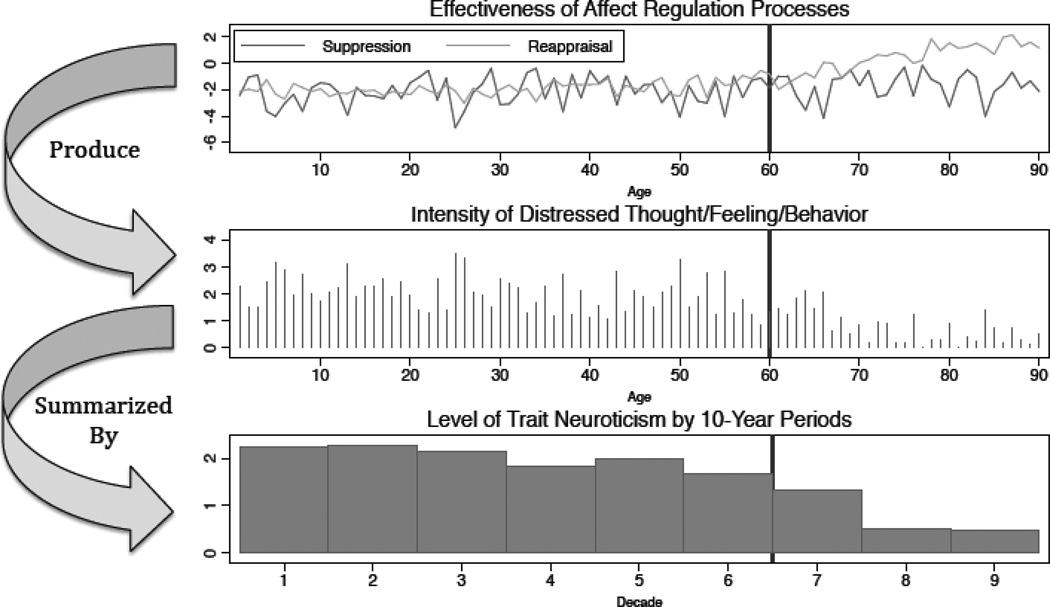
We reserve the term “personality process” to refer to ongoing operations of the personality system that guide, produce, or maintain moment-to-moment individual differences in thought, affect, and behavior (Mischel & Shoda, 1999). Processes operate based on parameters that represent “default” modes of functioning—that is, patterns of response to environmental demands, steady states or “set-points” to which they return after perturbation, ranges of variation about set-points, and manner of connection or interface with other processes in the personality system. These default settings are a function of genetic endowment combined with learning, and arise as a function of the personality system’s goal of adaptation to the environment (Hettema, 1989). Processes drive patterns of feeling, thought, and action aimed at achieving this objective. By “trait”, we mean a summary across at least a moderate period of time of some domain, type, or class of cognitions, affects, and behaviors (Fleeson, 2001; Fleeson & Gallagher, 2009). By summarizing patterns of thought, feeling, and action, traits thus reflect how personality processes are operating.1 Figure 1 provides an example of the associations of two personality processes (emotion suppression and relabeling), corresponding patterns of distressed thought, feeling and behavior, and a broad trait (Neuroticism) summarizing these patterns over ten year spans.
Figure 1.
Lifespan dynamics of one aspect of a hypothetical individual’s personality system. Y axes represent a Z-score metric. Emotion suppression and reappraisal fluctuate in effectiveness over the first part of life in conjunction with changing situations and life circumstances. However, these fluctuations are within a relatively consistent range of generally poor affect regulation (effectiveness Z-scores of 1 – 2). As a result, the intensity or frequency of distressed affects, behaviors, and cognitions, though variable, tends to be high. Scores on a trait, Neuroticism, summarize average levels of these distressed thoughts, affects, and behaviors over ten year periods. Later, the effectiveness of reappraisal improves as a result of treatment focused on this process (average climbs to Z-scores near 2 toward the end of life), causing distressed cognition, affect, and behavior diminish in relative frequency, and as a result trait Neuroticism decreases. This reflects the general pattern of decreasing Neuroticism over the lifespan (B. W. Roberts, Walton, & Viechtbauer, 2006a), coupled with increasing effectiveness of affect regulation(Mather & Knight, 2005)
By “personality-informed interventions”, we mean a broad approach to changing health outcomes that involves at least some attention to individual differences in personality. The first and most obvious method of informing interventions based on personality is to endeavor to change some element(s) of personality itself. While this prospect may seem astonishing in the context of present thinking, personality change has in fact been discussed for years in the psychotherapy and adult development and aging fields. A systems theory of personality affords a practical and powerful explanatory model for change in aspects of personality. A second way in which interventions may be personality-informed is less obvious but equally important. Standardized interventions of the sort used in public health and medicine, much like those in mental health, show differential effectiveness across individuals, even when they work on average in a group of persons. Personality is sometimes tied to this differential effectiveness, particularly in interventions involving behavioral components. This too has been known for some time and led to proposals that interventions for various behaviors be differentially prescribed or modified, based on an individual’s existing personality configuration. A parallel movement in health sciences, personalized medicine, has focused on a similar type of tailoring based on genotype, rather than phenotype.
The remainder of this paper is divided into three sections: The first considers how health-damaging personality tendencies such as low C might themselves be altered. The second considers the role of personality in tailoring and personalizing health interventions. The third and final section provides a set of recommendations for further research in these areas.
Personality As a Target for Intervention
Changing Thinking About Personality Change
The belief that personality is utterly immutable in adulthood is actually a caricature of the original “stability” argument in trait psychology, which was based on stability coefficients around .7 to .8 observed over moderate to long periods of time. These correlations lead to descriptions of personality in adulthood as relatively stable, not utterly immutable, with the qualification that personality could be changed via psychotherapy (R. R. McCrae & Costa, 2003) (p. 9–10). Moreover, trait change is a complex phenomenon assumes four forms: rank order changes (stability correlations < 1), mean level changes (average trait levels changing in a cohort), factorial changes (the inter-individual structure of personality changing, as in changes in the number or character of factors, or differentiation or de-differentiation between factors), and ipsative change (individual or within-person changes in trait profiles or configurations) (A. Caspi, Roberts, & Shiner, 2005). Given the qualifications of original claims of trait stability, and the unappreciated complexity of personality change, how did the general assumption of immutability arise?
First, only a small fraction of psychologists study personality and thus few in the field actually had reason to look at the data closely. Even experienced researchers are likely to default to inaccurate “lay theories of personality” (Plaks, 2009) or strong claims without studying evidence, because no one has time to exhaustively review literature outside their field. For data adduced in evidence of naturalistic stability, readers are referred to (Costa & McCrae, 2003) and for data adduced as evidence of naturalistic malleability to (Roberts et al., 2000; 2006), and for spirited debate over the issue to (P. T. Costa, Jr. & R. R. McCrae, 2006; B. W. Roberts, Walton, & Viechtbauer, 2006b) (P. T. Costa & R. R. McCrae, 2006). Interestingly, there has been little disagreement among experts that maximal stability estimates in adulthood peak in the neighborhood of the .7’s to .8’s (usually including measurement error correction), for various traits over various time spans in the neighborhood of 10 years. No one claims stability coefficients over moderate time spans are .1 – .2, or .9 – 1.0. The question instead is how naturalistic stability coefficients of this magnitude should be interpreted.
Framing and anchoring effects sway interpretations of stability estimates. Relative to Mischel’s early claim (now retracted) that there is no personality (i.e., a stability coefficient of 0), explaining 50% or even 65% of the present sample variance in a disposition by standing on the same disposition a decade earlier is a lot--certainly enough to repudiate the over-exuberant excesses of earlier claims. Psychologists of all stripes thus owe a debt to stability theorists, for their work reminds us that our field can scientifically self-correct. It seems, in fact, that something of an overcorrection occurred, with the pendulum of belief swinging to an apogee of personality permanence unseen since James’ now-infamous declaration that “by the age of thirty, character has set like plaster, never to soften again” (James, 1890). Yet, relative to an almost completely stable trait like height, in which prior measures count for close to 100% of the variance in future measures, a 50–65% figure is rather modest and leads logically to the question of what accounts for the remaining 35–50% of future personality variance.2
An alternative view not born of the need to refute extremist claims is that modest stability coefficients simply validate the conceptualization of personality as complex system charged with producing general adaptation. If individuals were one person one minute, then suddenly a completely different person the next (i.e., no personality stability), real world functioning would be impossible. At the same time, machine-like inflexibility (i.e., personality immutability) is also maladaptive.
A second issue that has led to mistaken perceptions of immutability is that few explicitly calibrate their expectations of stability coefficients by the naturalistic, rather than intervention, nature of longitudinal studies. If a .7 value arises from a group of persons not actively trying to change, what would such estimates look like among a group seeking and receiving focused intervention? The state of a system in the absence of perturbation often conveys no information on how it will behave when perturbed. A related issue concerns differential plasticity across persons (A. Caspi, et al., 2005), across different personality tendencies, and situations (Avshalom Caspi & Moffitt, 1993). Even in the face of a single, summary stability estimate of .7, some individuals are changing, and indeed the entire cohort may shift levels on a trait over time and yield a stability estimate of 1. It is thus crucial to parse the monolithic question of personality change into more nuanced considerations: who changes, when, in what ways, and how?
Third, the Axis II system has contributed to an exaggerated perception of personality immutability by defining personality disorders as “relatively enduring”. The intractability of the personality patterns exemplified by Axis II constructs are part of what make them disorders. The implication that non-disordered persons exhibit greater flexibility in patterns of affect, behavior, and thought seems to have been lost on most psychologists. As well, even if Axis II tendencies are considered largely entrenched, they express extreme configurations of Big 5 personality traits (Widiger & Costa, 2003) rare in the population. And even in this pocket of individuals, the question has become what elements of personality change and what do not (M. F. Lenzenweger, & Willett, J.B., 2007, 2009). This is a critical issue; the term “personality intervention” does not imply a complete, general personality overhaul. Rather it refers to focal treatment of one or more specific disposition(s) identified by a person who wants to change, such as C.
Fourth, the genetic component of personality has also lead to exaggerated perceptions of stability. While adult personality traits emerge from the biological foundation of temperament (A. Caspi, et al., 2005) (see also Eisenberg, Duckworth, Spinrad, & Valiente, this issue), the adult personality phenotype is the product of genes, social environments, and their interaction (South & Krueger, this issue). The environmental modulation of gene expression suggests that the mere possession of polymorphisms underlying complex traits like low C does not guarantee the phenotype (Charney, in press), meaning personality exhibits greater phenotype plasticity (Dali, 2004) than was once thought. In a complex systems view of personality, genetic endowment is only one factor influencing “set points”, variability, and other parameters structuring the operation of personality processes. Environmental experience contributes as much, if not more to the settings or system defaults for personality process.
In turn, this leads to a critical principal: experience can alter the functioning of personality processes. Since traits represent “running averages” of the thoughts, behavior, and affect arising from processes, change in personality processes will result in a change in personality traits. This idea has been called the “bottom-up” theory of personality change (see Roberts et al., this issue). Trait change is a higher-order, aggregate measure of change in psychological and behavioral patterns governed by personality processes. For instance, to change C, specific social-cognitive process underlying C, such as self-monitoring and self-regulation (see Eisenberg et al., this issue), must be changed. The naturalistic stability of personality processes and the corresponding trait is not a mystical or ineluctable property, but the result of learned experience within a genetic endowment, the genes of which are expressed within a social-environmental context—all combined with lack of concerted efforts to change.
Rationale for Targeting Personality in Interventions
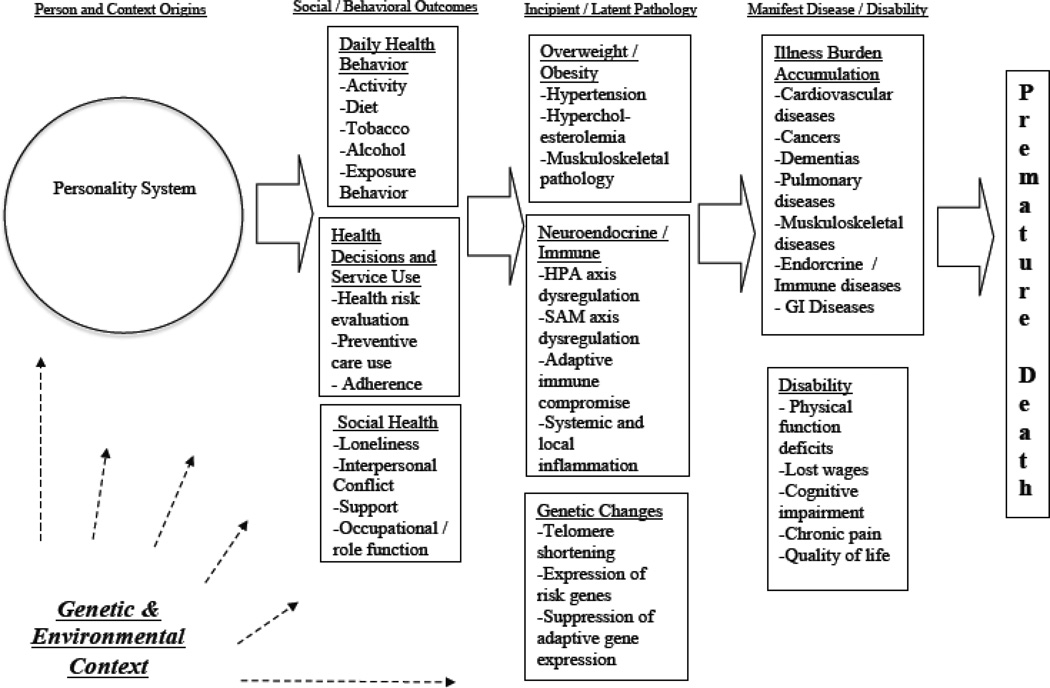
It is not enough to establish that health-damaging personality tendencies can be altered in theory. It must also make sense to treat them in particular, when a wide number of other intervention targets are also available. The primary justification is that personality tendencies function as a “root cause”, or common origin, of many pathways implicated in poor health outcomes. Figure 2 illustrates several of the known epidemiologic risk chains (Ben-Shlomo & Kuh, 2002; Kuh, Ben-Shlomo, Lynch, Hallqvist, & Power, 2003), or postulated causal sequences, connecting a personality trait such as low C to an undesired outcome. A number of intervention principals based on those outlined in the National Institutes of Health (NIH) Science of Behavior Change Meeting Summary (NIH, 2009b) are apparent here. First, personality represents one causal root of numerous problem behaviors and their health consequences (Krueger, Caspi, & Moffitt, 2000). Treating a common cause of multiple problem behaviors, such as low C, is the behavioral intervention equivalent of the medical desiderata to treat underlying pathology rather than manifest symptoms (NIH, 2009b). For instance, preventing the development of cynical hostility earlier in life may partially mitigate an entire range behavioral and physiological intermediaries that ultimately contribute to the development of cardiovascular disease (CVD) (Smith, Glazer, Ruiz, & Gallo, 2004).
Figure 2.
Lifecourse risk chain model. The personality system gives rise to a multifaceted cascade of health problems which progress from behavioral to biological to fatal. The model is simplified, with recursive feedback loops omitted among columns. Typical examples of constructs, rather than exhaustive lists are provided. Personality moderation of disease progression pathways is not shown, nor are interactions among other elements of the model.
Second, careful consideration is needed in deciding at which point in a risk chain one can effectively “leverage” change with some type of intervention. If it is not feasible to target the source of a causal chain itself (i.e., a particular aspect of personality cannot be directly changed in a particular person), the links in the chain should be carefully evaluated for alternative points of intervention. Personality may moderate the strength of other links, and/or provide helpful psychological and behavioral characterization of target populations at other points of intervention in Figure 1. This principle is discussed in the second part of our paper. Third, cost effectiveness must be considered in selecting an intervention point. For instance, alerting persons to the amount of calories they are consuming may achieve some weight reduction for a given intervention cost (Berman & Lavizzo-Mourey, 2008), but altering a general propensity such as low C by focusing on self-regulation skills may achieve more global health behavior change; cost-benefit ratios of the two intervention strategies must be carefully weighed. We now turn to modalities of intervention for maladaptive personality tendencies. We devote the most time to psychotherapy, since it illustrates several general principles of inducing personality change. However, other types of interventions are also noted and briefly discussed.
Psychotherapy and Personality
The notion that psychotherapy changes personality is not new (Dollard & Miller, 1950; Kelly, 1955; Rogers, 1955). In fact, many classical theories of psychotherapy are rooted in theories of personality, because the therapeutic desideratum of meaningful and lasting change in particular target areas was often thought to involve change in particular aspects of personality (Rychlak, 1973). The thinking was to treat the person, not a diagnosis or symptom pattern that might reappear without meaningful change in the personality system (Singer, 2005).2
For this reason, a number of early studies focused on how to produce and measure personality change during psychotherapy. Psychotherapy of various types induced improvement in hysteria (i.e., proclivities toward exaggerated emotional response) and psychasthenia (i.e., habitual low-grade anxiety) (Rashkis & Shaskan, 1946); improved affective tone (i.e., trait affect) (Snyder, 1945); reduced maladaptive interpersonal patterns (Leary & Harvey, 1956); decreased ineffective or immature coping strategies or defenses (Coons & Peacock, 1970; Schafer, 1955); increased correspondence between actual and ideal personality attributes (Butler, 1954; Cartwright, 1957); and improved self-awareness (Vargas, 1954), self-concept (Raimy, 1948) and self-acceptance (Raskin, 1949; Stock, 1949). These dispositional constructs are not what would today be called “Axis I” treatment targets (i.e., psychopathological syndromes presumed distinct from, though often partially due to, personality). Moreover, the express purpose of these therapy studies was adaptive change in one more elements of habitual disposition (Rychlak, 1973).
In the 1960s however, therapy began to shift away from a personality focus, toward the more fashionable emphasis on behaviorism. The personality theoretic roots of psychotherapy were dismissed in favor of Skinnerian principals. Rychlak (1968) foresaw the consequences of this--a modern era in which the idea of therapeutic change in elements of personality is met with astonishment or doctrinaire dismissal: “Personality theory has been shifting its locus of generation from the consulting room to the laboratory….there is a certain danger, for theory is then constructed to meet the needs of an extraspective observer …there are pitfalls in conceptualization which may so distort the image of man we seek to capture that a complete violation of our data may result.” (p. 198).
Later, several phenomenon coincided which all but eliminated the direct study of general personality change in psychotherapy: the rise of manualized psychotherapies, which were typically brief and symptom focused; separation of personality and non-personality, or “Axis I” and “Axis II” diagnoses, by the Diagnostic and Stastical Manual of Mental Disorders (we do not refer to a particular edition); the procrustean treatment strictures imposed by insurance agencies and other entities based on business models, rather than treatment models; and increasing emergence of “set like plaster” interpretations of personality arising from naturalistic longitudinal studies. Changing personality began to be characterized as impossible as irrelevant, and interest waned; a chapter entitled “Personality change and psychotherapy” (Messer & Warren, 1990) appearing in the 1990 first edition of the Handbook of Personality: Theory and Research was not reprinted in the 1999 second edition (Pervin, 1999). Treatment research during the 1980s and 1990s did, however, hint at personality change indirectly (Lambert & Supplee, 1997). Trait measures of constructs such as anxiety or anger were often included in outcome assessment batteries, and analyzed along with “state” versions of the same measures; interpersonal styles were still regarded as a legitimate focus of interpersonal psychotherapy. Lambert and Supplee (1997) provide a review of the “background” personality constructs examined during this period.
The 1980 advent of the first DSM also bifurcated personality into “pathology” (Axis II disorders), vs. “normal” traits to be studied by non-clinical personality psychologists. While the concepts of various personality disorders have deep roots in psychodynamic theory, the transition from normalcy to pathology was gradual and a matter of degree. The juxtaposition of “disordered” and normal version of personality (now subject to calls for reunification; (Widiger & Trull, 2007) did however legitimize the development of manualized psychotherapy specifically for Axis II personality constructs. Meta-analytic evidence from these therapy studies suggests that both psychodynamic and cognitive behavioral therapies (CBTs) are somewhat effective treatments of personality disorders, with a range of effect sizes (Cohen’s d) across therapeutic approaches and disorders, many over .5 and even .8 (Leichsenring & Leibing, 2003). A more recent treatment study conducted by the third author on borderline personality disorder evaluated three therapeutic modalities over the course of a year: dialectical behavior therapy, which focuses on skills training in emotion regulation and social interaction; transference-oriented therapy, which aims to educate patients about how their past experience cause maladaptive relational patterns toward new persons; and supportive treatment, which involves providing encouragement and empathy, without skills training or the interpretation of transference patterns (Clarkin, 2007). Depression and anxiety, linked to by the Big Five dimensions of Neuroticism, improved across all therapies. Impulsivity—a hallmark of low C—improved in both transference-focused and supportive treatment arms. Irritability, anger, and verbal assault, cardinals feature of both low Agreeableness and high Neuroticism in the Big Five model, improved for patients receiving transference-oriented therapy. Effect Sizes (r) were almost uniformly large. In the main, the modern psychotherapy emphasis on personality disorders indicates that, in the “worst case scenario” of an extreme form of personality maladaptation, positive changes in personality qualities can be achieved.
Other modern studies have reported personality changes observed in the context of a treatment for some Axis I disorder or non-personality outcome. In a placebo-control randomized clinical trial (RCT) for depressed patients, Tang (2009) noticed some reduction in Neuroticism and increase in Extraversion (d’s .46–.56) after eight weeks of CBT. A year-long intervention with primary care physicians designed to reduce burnout through increasing mindfulness also reduced Neuroticism (d = .49) and increased C (d = .29), changes that were maintained at three-month follow-up (Krasner et al., 2009). In another placebo controlled treatment trial focused on a mental stimulation and skills program to stave off cognitive decline, Big Five Openness to Experience increased over 16 weeks (d = .39), changes maintained at 30 weeks (Jackson, 2012). Work in progress by the first author’s group (B. P. Chapman, Roberts, B., Duberstein, P.R., & Talbot, N., 2012) shows reductions in traumatized women’s levels of Neuroticism and improvements in C after 16 weeks of either Interpersonal Psychotherapy or generic therapy (four week follow-up effect sizes Neuroticism d = .59, C d = .27 across both forms of therapy). Other work has linked therapeutically induced dispositional changes to improved health. A small placebo-controlled RCT targeting hostility effectively reduced this trait (d = .69) in men with coronary artery disease (Gidron, Davidson, & Bata, 1999), with hostility changes coinciding with reduced blood pressure. In a similar sample with an active control condition (standard medical treatment after a heart-attack), a three month cardiac rehabilitation program including both group and individual psychotherapy targeted and reduced chronic negative affect (Denollet & Brutsaert, 2001). This reduction in negative affect was linked to improved survival chances at nine-year follow-up. Antiemotionality or the suppression of emotion, defined as a dispositional tendency linked to overcontrol (van der Ploeg et al., 1989), has been reduced in trials of supportive-expressive psychotherapy with cancer patients (Giese-Davis et al., 2002). The same treatment, which targets this trait, has also engendered improvements in cancer patient distress (Classen et al., 2001) and survival (Goodwin et al., 2001; Spiegel, Bloom, Kraemer, & Gottheil, 1989). However, other trials have produced more ambiguous results (Spiegel et al., 2007) and the connection of dispositional factors and their treatment to cancer survival has been debated (Petticrew, 2002; Watson M, 2003) and is an active area of research (Spiegel, 2011).
Taken as a whole, the psychotherapy literature suggests four overarching considerations about interventions targeting personality. First, not only do data indicate that psychotherapy changes elements of personality in many people, the notion of personality change was traditionally part and parcel to psychotherapeutic approaches. It therefore should not be regarded as a revolutionary or controversial idea to intervene at the level of personality—only a forgotten idea. A corollary is that no intervention changes everyone, and psychotherapy requires active participation on the part of a person desiring change. Thus, the general question of “does it work” must be asked in this context, not under the erroneous assumption that therapy is a procedure performed on or “done to” a person.
Second, regarding the mechanisms by which psychotherapy changes elements of personality, it is unlikely that any one process is essential to change (Gabbard, 2009), and it has been difficult so far to isolate the operative elements in change. A conservative view at the present is that common elements across the treatments, such as an organized, structured approach to the patient with encouragement for attitudinal and behavioral change, is essential. General principals of change have been described in work such as (Mahoney, 1991). In general, psychotherapy can be seen as effecting personality change by focusing on personality processes. When these processes change, habitual behavioral and psychological patterns change, and change is observed at the trait level. Whatever the personality processes targeted, and whatever the technique used by a therapy or therapist, some effort is made to alter or change the system parameters that guide the process—that is, the “set-point” or default mode of functioning, random variability or specific fluctuation in response to environmental inputs, and so forth. Since these system parameters are a function not simply of genetic or biological factors, but also of learning and environment, the therapy process provides corrective experiences able to modify the functioning of personality processes. This has been called the “bottom-up” model of personality change (see also Roberts et al., this issue) because change at aggregate, summary markers of thought, affect, and behavior like traits is achieved by modifying relevant personality processes.
Consider, for example, the CBT emphasis on altering cognitive processes believed to produce dysfunctional behavior and affect. The CBT pantheon of “cognitive distortions” has many parallels in the collection of social-cognitive personality processes. The infamous CBT “depressive triad” (Beck, 1979) consists of beliefs that (a) the self is incapable, (b) the future is hopeless, and (c) others are hostile and untrustworthy. Cognitive tendency (a) corresponds closely the classic concept of self-efficacy (Bandura, 1986), (b) to affective forecasting bias (Hoerger, Chapman, Epstein, & Duberstein, 2012), and (c) to anxious attachment styles (see Fearon et al., this issue). The CBT goal ultimately is to change the “core beliefs” or cognitive schemata—”set points” or defaults of social cognitive processes—and maps onto Dweck’s work on core belief change as a key element of personality change (Dweck, 2008). Since the psychotherapy and personality literatures are somewhat fragmented some more general linkage between similar concepts would help to shed light on mechanisms of personality change (Mayer, 2004). For instance, Britton has explained how Motivational Interviewing, a type of therapy designed to deal with ambivalence about change, works through altering the Self-Determination Theory motivational personality constructs (Britton, 2008).
Third, the issue of mechanisms of change is related to the question about the maintenance of change. Whether or not the changes noted in the psychotherapy trials above persist over time is still an open question. The follow-up periods of those studies have been months, not years. In the personality disorders arena, one follow-up study has found a retention of treatment changes over an eight year period, but this study is an exception (Bateman & Fonagy, 2009). However, the amount of change occurring in published results does not seem trivial, and was typically effectuated in a year or less. Just as with other targets of psychotherapy, there is probably a dose-response relationship between the amount of therapy received, the amount of change, and the duration of change—major and long-term modification of maladaptive personality patterns has never been conceptualized as a short process. Current perspectives on time are now completely based on brief, manualized therapy approaches, arbitrary symptom remission criteria, and insurance company reimbursement limits. The irony is that when such brief treatments are inadequate, symptoms recur, and costs arising from future health care utilization and lost work and productivity may well offset any short-term cost savings.
With respect to lifecourse timing of an intervention, most of the interventions above have dealt with adult samples with mean ages in the midlife period (40–60). From a lifespan point of view, this is important for two reasons. First, midlife represents a time of high or even peak naturalistic personality stability (B. W. Roberts & DelVecchio, 2000). Traditionally, skepticism has prevailed about whether interventions could change personality much after age 30. The data above suggest that such doubt may be unwarranted. Second, midlife is in many ways a “critical period” dictating the timing of emergence for chronic diseases of aging (or the rate of progression of these diseases if they are already present). Thus, change in health damaging traits like low C is likely to serve and important preventive role. This does not mean that later life does not deserve at least some consideration as well—Jackson’s work (2012) indicates that trait change is possible then too. Another recent study found that older persons were as likely as younger to show change on personality dimensions of the 16-PF during therapy (Bialas, 2009). Since personality influences quality of life (B. P. Chapman, Franks, Duberstein, & Jerant, 2009; Pedersen & Denollet, 2003) and cognitive function (Duberstein et al., 2010; Wilson, Schneider, Arnold, Bienias, & Bennett, 2007), which are critical in later life, the reduction of maladaptive personality tendencies in older age deserves consideration.
Fourth, there is a “criterion problem” in modern psychotherapy research in that it is aimed at symptom clusters and DSM Axis-I entities, rather than the underlying elements of personality that give rise to these phenomena. Long term change on these sorts of criterion measures may well reflect change in underlying personality processes (Lambert & Supplee, 1997). For instance, in people with episodic depression, it seems unlikely that lasting and robust improvement could be achievement without changes in personality processes like affect regulation, which in turns will manifest as changes in Neuroticism trait measures. Also, of the four types of personality change noted above, only mean level change is typically examined. All would seem relevant, particularly ipsative or person-centered change.5 In general, a strong need exists for more comprehensive measurement of change (Shedler, 2010), with both symptom-based and personality-processed based outcomes. A number of these types of measures have been devised and utilized recently (Blagov, Bi, Shedler, & Westen, 2012; Hilsenroth, 2004; Itzhar-Nabarro, Silberschatz, & Curtis, 2009). These measures provide a convenient bridge between personality and psychotherapy theory and between “normal” and “abnormal” personality, and measure a variety of adaptive characteristics relevant to C including responsibility, organization, self-control, and goal achievement motivation.
Pharmacotherapy and Personality
The advent of modern selective serotonin reuptake inhibitors (SSRIs) like Prozac sparked much speculation about whether personality itself was changed by these agents (Kramer, 1992). Within the last decade, recent studies have documented effects of pharmacotherapy on personality. For instance, in one trial depressed patients who did not respond to a 14–26 week trial of anti-depressants showed no personality change, while those who responded to the medication showed decreased Neuroticism, and increased Extraversion, Openness, Agreeableness, and C (P. T. Costa, Bagby, Herbst, & McCrae, 2005). Eight-week placebo controlled anti-depressant-induced increases in Extraversion and reductions in Neuroticism have also been recently reported (Tang, 2009). Another eight-week placebo-controlled anti-depressant trial with patients selected for high hostility found that drug treatment reduced this trait (Kamarck et al., 2009). Effect sizes in these studies were medium to large (d’s .5 to greater than .8 in some cases), and authors interpreted their findings as evidence that the biological bases of traits could be targeted effectively.
With respect to C-related traits in particular, interest has arisen in the role of the serotonin system in self-regulation (Carver, Johnson, & Joormann, 2009). To the extent that molecular genetic research in personality can link phenotypes to pathways of gene expression related to neurotransmitter systems and basic neurobehavioral systems (M. F. Lenzenweger & Willett, 2007), a better understanding of neurotransmitter therapeutic targets will emerge.
Systems Level Interventions
The broader systems and social structures within which persons live also offer the potential to alter personality. Parenting and familial functioning have lasting effects on personality development (A. Caspi, et al., 2005), raising the question of whether family systems interventions change personality. While this area has been studied with respect to personality development in childhood (see, e.g., Shannahan, Hill, Roberts, Eccles, & Friedman, and Eisenberg and colleagues, both this issue), it has been largely neglected with respect to mid and later life. Another consideration is that if personality change in the at-risk family member is not possible, it may be possible to alter aspects of personality in family members to achieve benefits in the identified patient. For instance, spouses with higher C may mitigate some of the health risk incurred by individuals with low C (B. W. Roberts, Smith, Jackson, & Edmonds, 2009).
Evidence has emerged that not only behavioral outcomes of personality such as smoking (Christakis & Fowler, 2008) and obesity (Christakis & Fowler, 2007) are transmitted through extra-familial social networks, but also the personality characteristic of positive affect (Fowler & Christakis, 2008). How to induce such personality change through social networks has not received much, if any formal consideration. One possible model for social network interventions comes from a study in which increased suicide awareness was propagated throughout a school network by identifying “peer leaders”, or influential members of the social network, and using them to leverage change in others (Wyman et al., 2010). This raises interesting possibilities about altering group norms or attitudes related to personality characteristics like C. The question is the members of a network can be “steered” toward more adaptive tendencies in some area by “seeding” the network with change in influential persons. A different strategy would be to inoculate those in the network most susceptible to the contagion of unhealthy behavior.
The possibility of neighborhood level interventions should also not be neglected. Neighborhood environments influence a variety of health outcomes (Kawachi & Berkman, 2003), and as well as the development of maladaptive personality tendencies (Hart, Atkins, & Matsuba, 2008; Jaffee, Caspi, Moffitt, Polo-Tomas, & Taylor, 2007) (Leventhal & Brooks-Gunn, 2003a). Poverty, crime, and local norms for behaviors, as well as physical aspects of neighborhoods, may account for these effects.4 One neighborhood intervention program attempted to change the negative psychological effects of high-poverty neighborhoods by moving low-income families out of these areas. Although parental and child distress decreased (Leventhal & Brooks-Gunn, 2003b), educational outcomes did not appear to be enhanced (Leventhal, Fauth, & Brooks-Gunn, 2005), and relocated children had greater hyperactivity and substance use problems, as well as receiving harsher parenting, than those remaining in poverty (Fauth, Leventhal, & Brooks-Gunn, 2007). Although this trial evidenced mixed results, policy-level interventions striving to improve a neighborhood’s psycho-social milieu may conceivably be altering personality processes, including those relevant to C. Shannahan and Eccles (this issue) provide a thorough analysis of other social-environmental factors that may influence C.
At a broader level, the educational system may also shape personality. While it is true that personality influences educational attainment (John, Caspi, Robins, Moffitt, & et al., 1994) (Sarah E. Hampson, Goldberg, Vogt, & Dubanoski, 2007), education also influences personality (Borghans L, 2008; K. A. Miller, Kohn, & Schooler, 1986). Formal education develops self-discipline, planning, organization, goal-setting, and a number of other personality processes that are “bottom-up” avenues for improved C. Head start data indicated that early educational enrichment benefits such C personality processes as much as actual knowledge (Cunha & Heckman, 2009; Heckman, 2006). A meta analysis of evaluations of 73 after-school programs indicated that they have positive effects on children’s feelings and attitudes, behavioral adjustment, in addition to school performance (Durlak et al., 2007). These are critical components of personality. Other programs delivered to children in the educational system focus on cognitive control (Diamond, Barnett, Thomas, & Munro, 2007), affecting competencies in the C domain such as self-management, responsible decision making, maintaining attention, and planning ahead. Eisenberg et al. (this issue) provides further review of these issues. In both the Terman cohort (Kern & Friedman, 2008) and in a population-based Finnish cohort (Pulkki et al., 2003), personality later in life partially mediates the association between early educational achievement and later health outcomes. The major task, therefore, is to increase understanding of what aspects of education have the most powerful impact on personality by building personality batteries into existing infrastructures of educational evaluation.
After the completion of formal schooling, jobs and careers also affect personality characteristics such as intellectual flexibility (the Big 5 Openness) and self-directedness (a C-related trait; (Kohn & Schooler, 1978, 1982; J. Miller, Slomczynski, & Kohn, 1985). Other studies have documented effects of job characteristics on Big Five Neuroticism, Extraversion, and Agreeableness (Sutin, Costa, Miech, & Eaton, 2009) (Sutin & Costa, 2010) (B. W. Roberts, Caspi, & Moffitt, 2003; Scollon & Diener, 2006). Each job has particular qualities and tasks that draw on numerous personality processes (for instance, effortful control in meeting work deadlines). Thus, in order to adapt to the requirements of a job, key personality processes must be developed. Workplace programs and policies may provide environmental scaffolding that supports the growth of C (Engbers, van Poppel, Chin, & van Mechelen, 2005) through facilitating responsible behavior. Broadly speaking, very little is known about how familial, social network, neighborhood, educational, or occupational interventions might affect personality, but there is a sound rationale for examining each. We now turn from the possibility of changing personality itself to the use of personality to inform other interventions.
Putting the Person in Personalized Medicine: Targeting and Tailoring Existing Prevention and Intervention Programs
A great many health interventions focus on constructs in the columns of Figure 2, rather than personality. Even when these interventions improve people on average, considerable heterogeneity in response is nearly always observed. For this reason, interest has arisen in tailoring or personalizing health treatment to individuals (NIH, 2009a) under the rubric of personalized medicine (Hamburg & Collins, 2010). We discuss three aspects of this general movement in which personality may play an important role: individualized prediction of future health risks, modification of standard interventions according to personality characteristics, and targeted and tailored public health programs, including preventive communications.
Personalizing Clinical Risk Evaluation
An ideal of personalized medicine is to identify those at risk for health problems before these problems develop, so that preventive efforts can be successfully implemented. Prognostic models are being increasingly utilized for this purpose. Prognostic models are complex regression equations developed for maximum predictive capacity (not necessarily driven by the p-values of individual predictors), and are typically based on an individual’s genes, demographics, and clinical data (e.g., current diseases, blood pressure, lab test results). The first author’s group has proposed adding personality and other important psychosocial predictors of health to such models in order to improve their effectiveness and more fully characterize the individual (B. P. Chapman, Roberts, & Duberstein, 2011). It is irrelevant whether such predictive factors change, only that they carry actuarial predictive power for the outcome in question. In fact, changeable predictors enable repeated risk scores to determine whether preventive efforts reduce the risk of a future outcome. Improved accuracy in these models will allow physicians to better detect disease before it emerges, not only improving health outcomes, but reducing systemic burden and cost by preventing or delaying disease onset (Garber & Tunis, 2009).
For example, one of the most widely used prognostic models in medicine is the Framingham Risk Score, various versions of which provides a probability or risk level for myocardial infarction (MI; e.g., heart attack) or death from CVD, typically over a five or ten-year time horizon (Cook, Moons, & Harrell, 2010). Based on a person’s Framingham score, clinicians may adopt different modes of clinical intervention. The prognostic model underlying the Framingham score involves demographics and a handful of well-known cardiovascular risk factors, but much effort has gone into improving the accuracy of the model by adding biomedical predictors (i.e., inflammatory markers, candidate genes) (Schlendorf, Nasir, & Blumenthal, 2009). There is, however, need to balance prediction improvement against the costs of new predictors (Greenland, 2008). Work in progress by the first author’s group has discovered that multiple facet scales within the Eysenck Personality Inventory (EPI), some of which resemble elements of C (B. P. Chapman, Weiss, A.K., & Duberstein, P.R., in press), enhance predictive accuracy of the Framingham model over a 25-year period time horizon in a UK population sample (B. P. Chapman, Weiss, A.K., Fiscella, K.F., Duberstein, P.R., 2012).
Personalizing Clinical Treatment
For some time researchers have known that personality predicts differential change across general approaches to psychotherapy (Anderson, 1998; Bagby, 2008; Conte, Plutchik, Buck, Picard, & et al., 1991; Conte, Plutchik, Picard, & Karasu, 1991; Fiorot, Boswell, & Murray, 1990; Talbot, Duberstein, Butzel, Cox, & Giles, 2003; Zuckerman, Prusoff, Weissman, & Padian, 1980). The same is likely to be true for virtually any behavioral intervention, since the personality system is intricately involved in the acquisition and maintenance of behavior. Even pharmacologic and biological interventions can be affected by behavior through adherence—that is, taking medicines as prescribed, attending appointments, and so forth. Truly personalizing medicine involves taking these factors into account.
For example, chronic disease patients with more maladaptive personality tendencies seem more likely to benefit from an intervention designed to help them manage their diseases better through teaching self-efficacy (Franks, Chapman, Duberstein, & Jerant, 2009; Jerant, Chapman, Duberstein, & Franks, 2010). Other studies have concluded that lower C dialysis patients may need more structured and supervised interventions, while higher C people can benefit by maintaining a sense of personal control in interventions with less external structure (Christensen, 2000); Hostile individuals appear to benefit more from exercise to prevent future heart attacks than less hostile persons (Lavie & Milani, 1999); and, in the area of C, behavior dyscontrol in children can be more effectively treated by tailoring the approach to their temperament (McClowry, Snow, & Tamis-LeMonda, 2005).
One practical implication of these findings is that health interventions might be rendered more effective by administering them only to persons who are more likely to respond, rather than to all comers. This is to some extent already considered in medical treatment planning, but on the basis of demographics and clinical characteristics. Personalized medicine has added a genetic dimension to predicting treatment response, and personality can add a helpful phenotypic dimension—which may be particularly powerful for heavily behavioral interventions. Matching individuals to the best treatments will mean that money spent dispensing the intervention will lead to greater net benefit, resulting in greater cost effectiveness. Differing versions of interventions might be developed—that is, if standard post-heart attack exercise programs are more beneficial to hostile patients, how can another version of the program be developed to benefit less hostile people? This sort of differential response is somewhat understudied because most interventionists are focused on the main effects of their treatments. However, the goal of a generally effective treatment in no way relegates the question of “what works for who” to a secondary, treatment-moderator based aim on which to fall back in the absence of main effects.6 In fact, the new desideratum of “patient-centered care” involves prioritizing the patient’s desires, wishes, priorities, and attitudes—all influenced by personality. The goal is to improve the treatment process, via better relationships and communication, and thereby improve outcomes.
Personalizing Public Health Programs and Communication
Although personalized medicine typically refers to individual patient-level tailoring, tailoring public health programs to the characteristics of their target population can also increase their effectiveness and cost-effectiveness (Kreuter & Wray, 2003) (Noar SM, 2007). Data suggests that such tailoring can be done in part based on personality tendencies of the program recipients (Dutta, 2000; Dutta-Bergman, 2003). For instance, health messages about the synergistic risk of lung cancer resulting from smoking in homes with above-threshold levels of radon gas had only modest overall effects on smoking outcomes (Lichtenstein, Andrews, Lee, Glasgow, & Hampson, 2000). However, the perceived risk of the combination of smoking and radon predicted a reduction in cigarettes smoked in the home only for those high on C (S. E. Hampson, Andrews, Barckley, Lichtenstein, & Lee, 2000). In turn, greater perceived risk of cancer predicted quitting for more conscientiousness women but not men (Sarah E. Hampson, Andrews, Barckley, Lichtenstein, & Lee, 2006). These findings suggest that such messages need to be modified to be effective for those lower on C. More generally, basic correlation research between personality and various health behaviors such as smoking, poor diet, and inactivity can be used to inform interventions for these behaviors because characteristics of the target population are better understood.
Recent examples of tailoring an intervention to the underlying psychological and behavioral dispositions of a target group have focused, for instance, on promotion or prevention based regulatory focus (Kim, 2006) and approach/avoidance motivation (Sherman, 2006). Recently, effectiveness of a persuasive advertisement about a cellular phone has been successfully tailored to the Big Five in an on-line context using this approach (Hirsh, 2012). Work translating this idea into the public health arena is needed. For instance, Extraversion entails needs for social stimulation, but also greater likelihood of smoking (Terracciano & Costa, 2004). A smoking reduction program or public health message might thus emphasize high levels of social activity in a smoke-free lifestyle, while repeatedly pairing smoking with images of a solitary smoker (B. Chapman, Fiscella, Duberstein, & Kawachi, 2009). As messaging in general and health messaging in particular are increasingly implemented on line, it may be possible to capture personality information either directly (web-based questionnaires) or indirectly (records of purchases, etc., which marketing researchers have linked to various “personality profiles”) and then target particular “risk-prone” personality configurations.
The broader difficulty is that, off-line, public health departments cannot get mass-measurements of personality. Targeting is usually based on demographic characteristics. An alternative strategy may be to develop universally applicable interventions that are effective for those most at risk. This approach is particularly appropriate for school-based programs where it is more egalitarian and practical to apply the same intervention to all children. The second author and her colleagues are currently evaluating the efficacy of a school-based smoking prevention program consisting of components that were each shown to change smokingrelated outcomes in prior laboratory studies. To be included in the final version of the program, each component had to be effective for either the group as a whole, or for one or more at-risk subgroups. High sensation seeking defined one of these at-risk groups. In a randomized controlled trial, the program significantly reduced children’s intentions and willingness to smoke, and was particularly efficacious for sensation seekers (Andrews, 2011).
Ultimately, these three areas, all critical for healthy aging—personalizing risk prediction and prognosis, tailoring treatments and individualizing care, and increasing the relevance of public health programs and communications to target population characteristics—are all potential beneficiaries of personality-based refinements. This class of “personality-informed” interventions is quite independent of whether or not personality changes, because it relies only on the descriptive and predictive power of personality. In cases where personality may change over the course of a tailored intervention, tailoring may be done according to these changes. For instance, persons whose self-regulatory processes improve in the course of a self-control intervention may benefit from increasingly difficult regulatory goals, while those who do not see improvement would likely benefit from continued focus on more modest goals in order to improve self-efficacy and expectancy beliefs. As an example, psychotherapists are used to preparing the patient for improvement in general disposition accompanying improvement in the focal area of a presenting problem (for instance, “As you [avoid groups of people less / gain greater control over the impact of family on your depression / improve your concentration and work habits], you may [feel more confident in general / view other things in a more positive light / find that you are more reliable and motivated across the board].”) Personalizing according to a changing characteristic amounts to risk prediction / treatment / public health interventions that tailor in an ongoing or dynamic way.
Recommendations For Further Study
Personality and Psychotherapy
Psychotherapeutic change of personality is not a new and astounding notion, but rather a venerable one that fell out of intellectual fashion. There is a pressing need for collaborations between interventionists and personality researchers to resume study of this issue where the field left off several years ago: What mechanisms of change affect what personality processes, and how do these translate into change at the trait level? How can prevention and intervention findings inform understanding of change mechanisms (Howe, Reiss, & Yuh, 2002)? How can a modern, integrative approach to personality as a complex system be adopted in understanding and studying personality change? How can personality be measured in a reliable way that is sensitive to change during these studies? What is the theoretical and empirical correspondence between change in treatment targets in psychotherapy and change in personality processes underlying broad traits such as C? Does individual readiness or openness to change, existing personality configuration, or environmental context influence the degree of personality change observed in trials? How much intervention is needed in different modalities to affect meaningful change? How long are these changes maintained, and what differentiates those who successfully maintain change from those who revert to previous maladaptive dispositions? Are there optimal modalities of intervention for different lifecourse periods, different personality trait or process targets? How are personality changes from interventions translated into long-term improvements in health? How can the cost-effectiveness of interventions be optimized?
Personality Change in Other Intervention Modalities
It is possible, if not likely, that pharmacologic, family system, social network, educational, neighborhood, and occupational interventions may impact personality. Do different system “levels”, in the sense of increasingly broad ecological context, fare better or worse in affecting individual personality change? Can interventions exerting a small impact on the personality of many people yield more effective, and cost-effective improvements in population health outcomes than those that effect larger personality changes in smaller numbers of people? How can the assessment of relevant personality characteristics be incorporated into existing systems and structures that collect outcome data to evaluate policies and programs?
Personality and Personalized Medicine
The personalized medicine and patient-centered care movements have not yet considered personality in any meaningful sense, but their success may be critically dependent on incorporating health-relevant personality dispositions such as C. How can clinical health risk prediction be improved through leveraging the predictive power of personality? What new assessment methods are needed to briefly yet accurately capture elements of personality relevant to a particular health outcome? How can personality data be incorporated into the patient-centered care movements to guide health-care providers’ understanding of their patients? What current health behavioral interventions show the greatest heterogeneity in treatment response, and what elements of personality are linked to this heterogeneity? How can “packaged” interventions be flexibly modified to personal characteristics of various subgroups? At what point in Figure 2 risk chains is it most effective to tailor interventions? How can public health prevention programs, whether they involve messaging or the uptake of preventive services, be improved through targeting and tailoring based on personality factors? How can universal prevention programs be constructed to be particularly effective in persons most needing them, such as those low in C-relevant traits?
Pragmatic, “Real World” Studies
The most pressing need is for translational work bridging psychological and health science (Woolf, 2008). In what medical settings and how can intervention programs focused on remediating traits such as low C be dispensed? How can such programs be designed to qualify for insurance reimbursement for preventive health services? Should such programs stand alone, or be incorporated as components into intervention programs that are already established within health, educational, or workplace systems? How can programs targeting traits like low C be explained to decision makers and stake holders in other areas (e.g., programs to “increase personal responsibility”)? How can tailoring existing intervention programs on the basis of personality be made feasible and scalable? How can increasingly complex health care information systems be leveraged to capture relevant personality data?
Many of these questions may be addressed in a practically feasible, preliminary form using existing data (for instance, psychotherapy trials that collected personality data). This can provide an initial base of knowledge from which new studies can be launched. It is, however, an ideal time to pursue studies endeavoring to induce change in maladaptive areas of personality such as low C. The deleterious consequences of these characteristics on healthy aging is well documented, a more nuanced and moderate understanding of naturalistic personality stability has emerged, personality theory has advanced to a more integrated form suggesting a “bottom-up” model of personality change, and the health sciences are eager to focus upon individual differences as a means of improving treatment and prevention. Personality intervention represents an innovative and significant avenue for new research.
Footnotes
The Big 5 are a classification taxonomy of personality constructs, not a tool meant to be used to the exclusion of other approaches. Thus, the personality qualities discussed in this paper, regardless of whether they fall under the rubrics of process, motivation, etc. can all be mapped onto the Big 5 personality dimensions—for instance, low self-esteem, poor self-concept, and similar qualities are highly correlated with Neuroticism (Judge, Erez, Bono, & Thoresen, 2002), interpersonal circumplex dimensions of love and dominance are combinations of Extraversion and Agreeableness (R. R. McCrae & Costa, 1989), trait affects are definitional to Neuroticism (negative affects like anxiety and depression) and Extraversion (positive affect) (Watson, 1992), motivational constructs such as Murray’s needs correlate logically with corresponding Big 5 dimensions (i.e., need for achievement and C) (P. T. Costa, & McCrae, R.R., 1988), insight, mindfulness, and self-monitoring are encompassed by the Openness domain (Robert R. McCrae, 1994), anger and hostility are captured by both high Neuroticism and low Agreeableness (Dembroski & Costa, 1987), cognitive schemata or core belief structures underlie the Big 5 (Langston & Sykes, 1997), various coping / defensive mechanisms are associated Big 5 domains (Carver & Connor-Smith, 2010), ego functioning (Kurtz & Tiegreen, 2005) and personality disorders have been mapped to various configurations of the Big 5 (P. T. Costa, Jr. & Widiger, 2002). Roberts et al. and other articles in this issue note the association between C and other constructs such as self-regulation, and Fearon and colleagues consider the correspondence between C and attachment styles.
A naïve argument is that “if it changes, it’s not personality.” We assume that the circularity is apparent in defining personality as “that which does not change”, then appealing to this definition to justify immutability claims.
As a colleague said when discussing an earlier draft of this paper, “If we can’t change a person’s longstanding patterns and tendencies, then why did I get a PhD in clinical psychology?”
For instance, the “broken window effect” is a phenomenon in which a single unrepaired broken window is thought to establish a set of norms encouraging social disorder (Keizer, Lindenberg, & Steg, 2008).
The case study represents a classical design for studying ipsative change (Baughman, Shands, & Hawkins, 1959), and remains a potentially informative form of personality change research (Finn, 2011). Vaillant illustrated the power of a case series of change in illuminating ipsative change (Vaillant, 1977). Finally, Block’s UC Berkley growth studies promulgated a quantitative “person-centered” approach to personality change, which focuses on patterns of ipsative change in a group of individuals (Block & Haan, 1971).
One noteworthy effort to examine differential change across different types of people was Project Match, an intervention study that attempted to pair specific forms of a drug and alcohol treatment with different types of patients, defined in part by personality characteristics (Project Match Research Group, 1988). Although treatment outcomes were improved by matching treatment variation to individual based on four out of 20 possible matching variables, a general impression arose from the study that tailoring was not helpful, retarding progress in this area. In our view, the generality of skepticism this study seems to have engendered is not commensurate with either its results or its implications for other types of tailoring in other types of treatment.
References
- Anderson KW. Utility of the five-factor model of personality in psychotherapy aptitude-treatment interaction research. Psychotherapy Research. 1998;8(1):54–70. [Google Scholar]
- Andrews JA, Gordon JS, Hampson SE, Christiansen SM, Gunn B, Slovic P, Severson HH. Short-term efficacy of Click City Tobacco: changing etilogical mechanisms related to the onset of tobacco use. Prevention science : the official journal of the Society for Prevention Research. 2011;12:89–102. doi: 10.1007/s11121-010-0192-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagby R, Quilty LC, Segal ZV, McBride CC, Kennedy SH, Costa PT., Jr Personality and differential treatment response in major depression: A randomized controlled trial comparing cognitive-behavioural therapy and pharmacotherapy. The Canadian Journal of Psychiatry / La Revue canadienne de psychiatrie. 2008;56(3):361–370. doi: 10.1177/070674370805300605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Vol. 617. rentice-Hall; 1986. [Google Scholar]
- Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. The American Journal of Psychiatry. 2009;166(12):1355–1364. doi: 10.1176/appi.ajp.2009.09040539. [DOI] [PubMed] [Google Scholar]
- Baughman E, Shands HC, Hawkins DR. Intensive psychotherapy and personality change: Psychological test evaluation of a single case. Psychiatry: Journal for the Study of Interpersonal Processes. 1959;22:296–301. doi: 10.1080/00332747.1959.11023183. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: The Guilford Press; 1979. [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International journal of epidemiology. 2002;31(2):285–293. [PubMed] [Google Scholar]
- Berman M, Lavizzo-Mourey R. Obesity prevention in the information age: caloric information at the point of purchase. JAMA : the journal of the American Medical Association. 2008;300(4):433–435. doi: 10.1001/jama.300.4.433. [DOI] [PubMed] [Google Scholar]
- Bialas A. Psychotherapy effectiveness and the possibility of personality traits changes depending on the patients' age. Archives of Psychiatry and Psychotherapy. 2009;11(1):11–19. [Google Scholar]
- Blagov PS, Bi W, Shedler J, Westen D. The Shedler-Westen Assessment Procedure (SWAP): Evaluating psychometric questions about its reliability, validity, and impact of its fixed score distribution. Assessment. 2012;19(3):370–382. doi: 10.1177/1073191112436667. [DOI] [PubMed] [Google Scholar]
- Block J, Haan N. Lives through time. Lawrence Erlbaum; 1971. [Google Scholar]
- Borghans L DALHJJ, ter Weel B. The economics and psychology of personality traits. Journal of Human Resources. 2008;43(4):972–1059. [Google Scholar]
- Britton PC, Williams GC, Conner KR. Self-determination theory, motivational interviewing, and the treatment of clients with acute suicidal ideation. Journal of clinical psychology. 2008;64(1):52–66. doi: 10.1002/jclp.20430. [DOI] [PubMed] [Google Scholar]
- Butler JM, Haigh GV. Changes in the relation between self concepts and ideal concepts consequent upon client-centered counseling. In: Dymond CRRRF, editor. Psychotherapy and Personality Change. Chicago, IL: University of Chicago Press; 1954. [Google Scholar]
- Cartwright RD. Effects of psychotherapy on self consistency. Journal of Counseling Psychology. 1957;4:15–22. [Google Scholar]
- Carver CS, Connor-Smith J. Personality and coping. Annual Review of Psychology. 2010;61:679–704. doi: 10.1146/annurev.psych.093008.100352. [DOI] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, Joormann J. Two-mode models of self-regulation as a tool for conceptualizing effects of the serotonin system in normal behavior and diverse disorders. Current Directions in Psychological Science. 2009;18(4):195–199. doi: 10.1111/j.1467-8721.2009.01635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE. When do individual differences matter? A paradoxical theory of personality coherence. Psychological Inquiry. 1993;4(4):247–271. [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: stability and change. Annu Rev Psychol. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Chapman B, Fiscella K, Duberstein P, Kawachi I. Education and smoking: confounding or effect modification by phenotypic personality traits. Ann Behav Med. 2009;38(3):237–248. doi: 10.1007/s12160-009-9142-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Franks P, Duberstein PR, Jerant A. Differences between individual and societal health state valuations: any link with personality. Med Care. 2009;47(8):902–907. doi: 10.1097/MLR.0b013e3181a8112e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Roberts B, Duberstein P. Personality and longevity: knowns, unknowns, and implications for public health and personalized medicine. Journal of aging research. 2011;2011:759170. doi: 10.4061/2011/759170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Roberts B, Duberstein PR, Talbot N. Personality change in a randomized clinical trial of psychotherapies. Rochester, NY: University of Rochest Medical Center; 2012. Unpublished data. Psychiatry. [Google Scholar]
- Chapman BP, Weiss AK, Duberstein PR. Hierarchical structure of the Eysenck Personality Inventory in a large populaton sample: Goldberg's trait-tier mapping procedure. Personality and individual differences. in press doi: 10.1016/j.paid.2012.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Weiss AK, Fiscella KF, Duberstein PR. Inexpensive adjunct predictors for the Charlson and Framingham models: Psychological phenotype and socioeconomic status; Working Papers. Psychiatry.; Rochester, New York: University of Rochester School of Medicine and Dentisry; 2012. [Google Scholar]
- Charney E. Behavior genetics and postgenomics. Behavioral and Brain Sciences. in press doi: 10.1017/S0140525X11002226. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen AJ. Patient-by-treatment context interaction in chronic disease: a conceptual framework for the study of patient adherence. Psychosom Med. 2000;62(3):435–443. doi: 10.1097/00006842-200005000-00017. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: A multiwave study. American journal of psychiatry. 2007;164:922–928. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- Classen C, Butler LD, Koopman C, Miller E, DiMiceli S, Giese-Davis J, Spiegel D. Supportive-expressive group therapy and distress in patients with metastatic breast cancer: a randomized clinical intervention trial. Archives of general psychiatry. 2001;58(5):494–501. doi: 10.1001/archpsyc.58.5.494. [DOI] [PubMed] [Google Scholar]
- Conte HR, Plutchik R, Buck L, Picard S, et al. Interrelations between ego functions and personality traits: Their relation to psychotherapy outcome. American journal of psychotherapy. 1991;45(1):69–77. doi: 10.1176/appi.psychotherapy.1991.45.1.69. [DOI] [PubMed] [Google Scholar]
- Conte HR, Plutchik R, Picard S, Karasu T. Can personality traits predict psychotherapy outcome. Comprehensive psychiatry. 1991;32(1):66–72. doi: 10.1016/0010-440x(91)90071-j. [DOI] [PubMed] [Google Scholar]
- Cook NR, Moons KG, Harrell FE., Jr Assessing predictive performance beyond the Framingham risk score. JAMA. 2010;303(14):1368–1369. doi: 10.1001/jama.2010.389. author reply 1369. [DOI] [PubMed] [Google Scholar]
- Coons W, Peacock E. Interpersonal interaction and personality change in group psychotherapy. The Canadian Psychiatric Association Journal / La Revue de l'Association des psychiatres du Canada. 1970;15(4):347–355. doi: 10.1177/070674377001500403. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. From catalog to classification: Murray's needs and the five-factor model. Journal of personality and social psychology. 1988;55(2):258–265. [Google Scholar]
- Costa PT, Bagby RM, Herbst JH, McCrae RR. Personality self-reports are concurrently reliable and valid during acute depressive episodes. Journal of affective disorders. 2005;89(1–3):45–55. doi: 10.1016/j.jad.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Age changes in personality and their origins: comment on Roberts, Walton, and Viechtbauer (2006) Psychological bulletin. 2006;132(1):26–28. doi: 10.1037/0033-2909.132.1.26. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, Widiger TA. Personality disorders and the five-factor model of personality. 2nd ed. 2002. p. 493. [Google Scholar]
- Costa PT, McCrae RR. Age changes in personality and their origins: Comment on Roberts, Walton, and Viechtbauer (2006) Psychological bulletin. 2006;132(1):26–28. doi: 10.1037/0033-2909.132.1.26. [DOI] [PubMed] [Google Scholar]
- Cunha F, Heckman JJ. The Economics and Psychology of Inequality and Human Development. J Eur Econ Assoc. 2009;7(2):320–364. doi: 10.1162/jeea.2009.7.2-3.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dali SRX, Houston AI, McNamara JM. The behavioural ecology of personality: consistent individual differences from an adaptive perspective. Ecology Letters. 2004;7:734–739. [Google Scholar]
- Dembroski TM, Costa PT., Jr Coronary prone behavior: components of the type A pattern and hostility. J Pers. 1987;55(2):211–235. doi: 10.1111/j.1467-6494.1987.tb00435.x. [DOI] [PubMed] [Google Scholar]
- Denollet J, Brutsaert DL. Reducing emotional distress improves prognosis in coronary heart disease - 9-year mortality in a clinical trial of rehabilitation. Circulation. 2001;104(17):2018–2023. doi: 10.1161/hc4201.097940. [DOI] [PubMed] [Google Scholar]
- Diamond A, Barnett WS, Thomas J, Munro S. Preschool program improves cognitive control. Science. 2007;318(5855):1387–1388. doi: 10.1126/science.1151148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dollard J, Miller NE. Personality and psychotherapy; an analysis in terms of learning, thinking, and culture. 1950:488. [Google Scholar]
- Duberstein PR, Chapman BP, Tindle HA, Sink KM, Bamonti P, Robbins J, Franks P. Personality and risk for Alzheimer's disease in adults 72 years of age and older: A 6-year follow-up. Psychol Aging. 2010 doi: 10.1037/a0021377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durlak JA, Taylor RD, Kawashima K, Pachan MK, DuPre EP, Celio CI, Weissberg RP. Effects of positive youth development programs on school, family, and community systems. American Journal of Community Psychology. 2007;39(3-4):269–286. doi: 10.1007/s10464-007-9112-5. [DOI] [PubMed] [Google Scholar]
- Dutta M, Vanacker B. Effects of personality on persuasive appeals in health communication. ADVANCES IN CONSUMER RESEARCH. 2000;27:119–124. [Google Scholar]
- Dutta-Bergman MJ. The linear interaction model of personality effects in health communication. Health Commun. 2003;15(1):101–115. doi: 10.1207/S15327027HC1501_5. [DOI] [PubMed] [Google Scholar]
- Dweck CS. Can Personality Be Changed? The Role of Beliefs in Personality and Change. Current Directions in Psychological Science. 2008;17(6):391–394. [Google Scholar]
- Engbers LH, van Poppel MN, Chin APMJ, van Mechelen W. Worksite health promotion programs with environmental changes: a systematic review. American journal of preventive medicine. 2005;29(1):61–70. doi: 10.1016/j.amepre.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Fauth RC, Leventhal T, Brooks-Gunn J. Welcome to the neighborhood? Long-term impacts of moving to low-poverty neighborhoods on poor children's and adolescents' outcomes. Journal of Research on Adolescence. 2007;17(2):249–284. [Google Scholar]
- Finn SE. Journeys through the valley of death: Multimethod psychological assessment and personality transformation in long-term psychotherapy. Journal of personality assessment. 2011;93(2):123–141. doi: 10.1080/00223891.2010.542533. [DOI] [PubMed] [Google Scholar]
- Fiorot M, Boswell P, Murray EJ. Personality and response to psychotherapy in depressed elderly women. Behavior, Health, & Aging. 1990;1(1):51–63. [Google Scholar]
- Fleeson W. Toward a structure- and process-integrated view of personality: Traits as density distributions of states. Journal of Personality and Social Psychology. 2001;80(6):1011–1027. [PubMed] [Google Scholar]
- Fleeson W, Gallagher P. The implications of Big Five standing for the distribution of trait manifestation in behavior: Fifteen experience-sampling studies and a meta-analysis. Journal of Personality and Social Psychology. 2009;97(6):1097–1114. doi: 10.1037/a0016786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler JH, Christakis NA. Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart Study. BMJ. 2008;337:a2338. doi: 10.1136/bmj.a2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franks P, Chapman B, Duberstein P, Jerant A. Five factor model personality factors moderated the effects of an intervention to enhance chronic disease management self-efficacy. Br J Health Psychol. 2009;14(Pt 3):473–487. doi: 10.1348/135910708X360700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbard GO. Textbook of psychotherapeutic treatments. Arlington, VA: American Psychiatric Association; 2009. [Google Scholar]
- Garber AM, Tunis SR. Does comparative-effectiveness research threaten personalized medicine. N Engl J Med. 2009;360(19):1925–1927. doi: 10.1056/NEJMp0901355. [DOI] [PubMed] [Google Scholar]
- Gidron Y, Davidson K, Bata I. The short-term effects of a hostility-reduction intervention on male coronary heart disease patients. Health Psychol. 1999;18(4):416–420. doi: 10.1037//0278-6133.18.4.416. [DOI] [PubMed] [Google Scholar]
- Giese-Davis J, Koopman C, Butler LD, Classen C, Cordova M, Fobair P, Spiegel D. Change in emotion-regulation strategy for women with metastatic breast cancer following supportive-expressive group therapy. Journal of consulting and clinical psychology. 2002;70(4):916–925. doi: 10.1037//0022-006x.70.4.916. [DOI] [PubMed] [Google Scholar]
- Goodwin PJ, Leszcz M, Ennis M, Koopmans J, Vincent L, Guther H, Hunter J. The effect of group psychosocial support on survival in metastatic breast cancer. The New England journal of medicine. 2001;345(24):1719–1726. doi: 10.1056/NEJMoa011871. [DOI] [PubMed] [Google Scholar]
- Greenland S. The need for reorientation toward cost-effective prediction: comments on 'Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond' by M. J. Pencina et al., Statistics in Medicine (DOI: 10.1002/sim.2929) Stat Med. 2008;27(2):199–206. doi: 10.1002/sim.2995. [DOI] [PubMed] [Google Scholar]
- Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363(4):301–304. doi: 10.1056/NEJMp1006304. [DOI] [PubMed] [Google Scholar]
- Hampson SE, Andrews JA, Barckley M, Lichtenstein E, Lee ME. Conscientiousness, perceived risk, and risk-reduction behaviors: A preliminary study. Health Psychology. 2000;19(5):496–500. [PubMed] [Google Scholar]
- Hampson SE, Andrews JA, Barckley M, Lichtenstein E, Lee ME. Personality traits, perceived risk, and risk-reduction behaviors: A further study of smoking and radon. Health Psychology. 2006;25(4):530–536. doi: 10.1037/0278-6133.25.4.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson SE, Goldberg LR, Vogt TM, Dubanoski JP. Mechanisms by Which Childhood Personality Traits Influence Adult Health Status: Educational Attainment and Healthy Behaviors. Health Psychology. 2007;26(1):121–125. doi: 10.1037/0278-6133.26.1.121. Ameran Psyhooga Assn. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart D, Atkins R, Matsuba M. The association of neighborhood poverty with personality change in childhood. Journal of Personality and Social Psychology. 2008;94(6):1048–1061. doi: 10.1037/0022-3514.94.6.1048. [DOI] [PubMed] [Google Scholar]
- Heckman JJ. Skill Formation and the Economics of Investing in Disadvantaged Children. Science. 2006;312(5782):1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- Hettema PJE. Personality and environment: Assessment of human adaptation. Oxford, England: John Wiley & Sons; 1989. [Google Scholar]
- Hilsenroth MJ. An Introduction to the Special Issue on Personality Assessment and Psychotherapy. Journal of personality assessment. 2004;83(3):187–189. [Google Scholar]
- Hirsh JB, Kang SK, Boenhausen GV. Personalizing persuasion: tailoring persuasive appeals to recipients' personality traits. Psychological science. 2012 doi: 10.1177/0956797611436349. [DOI] [PubMed] [Google Scholar]
- Hoerger M, Chapman BP, Epstein RM, Duberstein PR. Emotional intelligence: A theoretical framework for individual differences in affective forecasting. Emotion. 2012 doi: 10.1037/a0026724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe GW, Reiss D, Yuh J. Can prevention trials test theories of etiology. Dev Psychopathol. 2002;14(4):673–694. doi: 10.1017/s0954579402004029. [DOI] [PubMed] [Google Scholar]
- Itzhar-Nabarro Z, Silberschatz G, Curtis JT. The Adjective Check List as an outcome measure: Assessment of personality change in psychotherapy. Psychotherapy Research. 2009;19(6):707–717. doi: 10.1080/10503300902988760. [DOI] [PubMed] [Google Scholar]
- Jackson JJ, Hill PL, Payne BR, Roberts BW, Stine-Morrow AL. Can an old dog learn (and want to experience) new tricks? Cognitive training increases openness to experience in older adults. Psychology and aging. 2012;27(2):286–292. doi: 10.1037/a0025918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Polo-Tomas M, Taylor A. Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: A cumulative stressors model. Child Abuse & Neglect. 2007;31(3):231–253. doi: 10.1016/j.chiabu.2006.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James W. Principles of Psychology. Cambridge, MA: Harvard University Press; 1890. [Google Scholar]
- Jerant A, Chapman B, Duberstein P, Franks P. Effects of personality on self-rated health in a 1-year randomized controlled trial of chronic illness self-management. Br J Health Psychol. 2010;15(Pt 2):321–335. doi: 10.1348/135910709X464353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John OP, Caspi A, Robins RW, Moffitt TE, et al. The “little five”: Exploring the nomological network of the five-factor model of personality in adolescent boys. Child development. 1994;65(1):160–178. [PubMed] [Google Scholar]
- Judge TA, Erez A, Bono JE, Thoresen CJ. Are measures of self-esteem, neuroticism, locus of control, and generalized self-efficacy indicators of a common core construct. Journal of Personality and Social Psychology. 2002;83(3):693–710. doi: 10.1037//0022-3514.83.3.693. [DOI] [PubMed] [Google Scholar]
- Kamarck TW, Haskett RF, Muldoon M, Flory JD, Anderson B, Bies R, Manuck SB. Citalopram intervention for hostility: results of a randomized clinical trial. Journal of consulting and clinical psychology. 2009;77(1):174–188. doi: 10.1037/a0014394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Neighborhoods and Health. New York: Oxford University Press; 2003. [Google Scholar]
- Keizer K, Lindenberg S, Steg L. The Spreading of Disorder. Science. 2008;322(5908):1681–1685. doi: 10.1126/science.1161405. [DOI] [PubMed] [Google Scholar]
- Kelly GA. The psychology of personal constructs. Vol. 1. A theory of personality. Clinical diagnosis and psychotherapy. 1955;Vol. 2:2. [Google Scholar]
- Kern ML, Friedman HS. Early educational milestones as predictors of lifelong academic achievement, midlife adjustment, and longevity. J Appl Dev Psychol. 2008;30(4):419–430. doi: 10.1016/j.appdev.2008.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YJ. The role of regulatory focus in message framing in antismoking advertisements for adolescents. Journal of Advertising. 2006;35:143–151. [Google Scholar]
- Kohn ML, Schooler C. The reciprocal effects of the substantive complexity of work and intellectual flexibility: A longitudinal assessment. American Journal of Sociology. 1978;84(1):24–52. [Google Scholar]
- Kohn ML, Schooler C. Job conditions and personality: A longitudinal assessment of their reciprocal effects. American Journal of Sociology. 1982;87(6):1257–1286. [Google Scholar]
- Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, Quill TE. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA : the journal of the American Medical Association. 2009;302(12):1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27:S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE. Epidemiological personology: the unifying role of personality in population-based research on problem behaviors. J Pers. 2000;68(6):967–998. doi: 10.1111/1467-6494.00123. [DOI] [PubMed] [Google Scholar]
- Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. Journal of epidemiology and community health. 2003;57(10):778–783. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz JE, Tiegreen SB. Matters of conscience and conscientiousness: The place of ego development in the five-factor model. Journal of personality assessment. 2005;85(3):312–317. doi: 10.1207/s15327752jpa8503_07. [DOI] [PubMed] [Google Scholar]
- Lambert MJ, Supplee EC. Trends and practices in psychotherapy outcome assessment and their implications for psychotherapy and applied personality. Hogan, Robert [Ed] 1997:947–967. [Google Scholar]
- Langston CA, Sykes WE. Beliefs and the big five: Cognitive bases of broad individual differences in personality. Journal of Research in Personality. 1997;31(2):141–165. [Google Scholar]
- Lavie CJ, Milani RV. Effects of cardiac rehabilitation and exercise training programs on coronary patients with high levels of hostility. Mayo Clin Proc. 1999;74(10):959–966. doi: 10.4065/74.10.959. [DOI] [PubMed] [Google Scholar]
- Leary T, Harvey JS. A methodology for measuring personality changes in psychotherapy. Journal of clinical psychology. 1956;12:123–132. doi: 10.1002/1097-4679(195604)12:2<123::aid-jclp2270120205>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Leibing E. The effectiveness of psychodynamic therapy and cognitive behavior therapy in the treatment of personality disorders: a meta-analysis. The American journal of psychiatry. 2003;160(7):1223–1232. doi: 10.1176/appi.ajp.160.7.1223. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Willett JB. Modeling individual change in personality disorder features as a function of simultaneous individual change in personality dimensions linked to neurobehavioral systems: The Longitudinal Study of Personality Disorders. Journal of abnormal psychology. 2007;116(4):684–700. doi: 10.1037/0021-843X.116.4.684. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Willett JB. Does change in temperament predict change in schizoid personality disorder? A methodological framework and illustration from the Longitudinal Study of Personality Disorders. Development & Psychopathology. 2009;21:1211–1231. doi: 10.1017/S0954579409990125. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Willett JB. Predicting individual change in personality disorder features by simultaneous individual change in personality dimensions linked to neurobehavioral systems: The longitudinal study of personality disorders. Journal of abnormal psychology. 2007;116(4):684–700. doi: 10.1037/0021-843X.116.4.684. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. Children and youth in neighborhood contexts. Current Directions in Psychological Science. 2003a;12(1):27–31. [Google Scholar]
- Leventhal T, Brooks-Gunn J. Moving to Opportunity: An Experimental Study of Neighborhood Effects on Mental Health. American Journal of Public Health. 2003b;93(9):1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal T, Fauth RC, Brooks-Gunn J. Neighborhood poverty and public policy: A 5-year follow-up of children's educational outcomes in the New York City moving to opportunity demonstration. Developmental Psychology. 2005;41(6):933–952. doi: 10.1037/0012-1649.41.6.933. [DOI] [PubMed] [Google Scholar]
- Lichtenstein E, Andrews JA, Lee ME, Glasgow RE, Hampson SE. Using radon risk to motivate smoking reduction: evaluation of written materials and brief telephone counselling. Tob Control. 2000;9(3):320–326. doi: 10.1136/tc.9.3.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney M. Human Change Processes: The Scientific Principals of Psychotherapy. New York: Basic Books; 1991. [Google Scholar]
- Mather M, Knight M. Goal-directed memory: the role of cognitive control in older adults' emotional memory. Psychology and aging. 2005;20(4):554–570. doi: 10.1037/0882-7974.20.4.554. [DOI] [PubMed] [Google Scholar]
- Mayer JD. How Does Psychotherapy Influence Personality? A Theoretical Integration. Journal of clinical psychology. 2004;60(12):1291–1315. doi: 10.1002/jclp.20076. [DOI] [PubMed] [Google Scholar]
- McAdams DP, Pals JL. A new Big Five: fundamental principles for an integrative science of personality. Am Psychol. 2006;61(3):204–217. doi: 10.1037/0003-066X.61.3.204. [DOI] [PubMed] [Google Scholar]
- McClowry SG, Snow DL, Tamis-LeMonda CS. An evaluation of the effects of INSIGHTS on the behavior of inner city primary school children. J Prim Prev. 2005;26(6):567–584. doi: 10.1007/s10935-005-0015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae RR. Openness to Experience: Expanding the boundaries of Factor V. European Journal of Personality. 1994;8(4):251–272. [Google Scholar]
- McCrae RR, Costa PT. Personality in Adulthood. Vol. 2nd. New York: Guilford; 2003. [Google Scholar]
- McCrae RR, Costa PT., Jr The structure of interpersonal traits: Wiggins's circumplex and the five-factor model. Journal of personality and social psychology. 1989;56(4):586–595. doi: 10.1037//0022-3514.56.4.586. [DOI] [PubMed] [Google Scholar]
- Messer SB, Warren S. Personality change and psychotherapy. Pervin, Lawrence A [Ed] 1990:371–398. [Google Scholar]
- Miller J, Slomczynski KM, Kohn ML. Continuity of learning-generalization: The effect of job on men's intellective process in the United States and Poland. American Journal of Sociology. 1985;91(3):593–615. [Google Scholar]
- Miller KA, Kohn ML, Schooler C. Educational self-direction and personality. American Sociological Review. 1986;51(3):372–390. [Google Scholar]
- Mischel W, Shoda Y. Integrating dispositions and processing dynamics within a unified theory of personality: The cognitive-affective personality system. Pervin, Lawrence A [Ed] 1999:197–218. [Google Scholar]
- NIH. NIH Science of Behavior Change Meeting Summary. 2009a
- NIH. NIH Science of Behavior Change Meeting Summary. Bethesda, Maryland: National Institutes of Heath; 2009b. [Google Scholar]
- Noar SM BC, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological bulletin. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Pedersen SS, Denollet J. Type D personality, cardiac events, and impaired quality of life: a review. European Journal of Cardiovascular Prevention & Rehabilitation. 2003;10(4):241–248. doi: 10.1097/00149831-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Pervin LA, John OP, editors. Handbook of Personality: Theory and Research. New York: Guilford Press; 1999. [Google Scholar]
- Petticrew M, Bell R, Hunter D. Influence of psychological coping on survival and recurrence in people with cancer: Systematic review. British Medical Journal. 2002;325:1066–1075. doi: 10.1136/bmj.325.7372.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plaks JE, Levy SR, Dweck CS. Lay theories of personality: cornerstones of meaning in social cognition. Social & Personality Psychology Compass. 2009;3:1069–1081. [Google Scholar]
- Pulkki L, Kivimaki M, Keltikangas-Jarvinen L, Elovainio M, Leino M, Viikari J. Contribution of adolescent and early adult personality to the inverse association between education and cardiovascular risk behaviours: prospective population-based cohort study. International journal of epidemiology. 2003;32(6):968–975. doi: 10.1093/ije/dyg097. [DOI] [PubMed] [Google Scholar]
- Raimy VC. Self reference in counseling interviews. Journal of Consulting Psychology. 1948;12:153–163. doi: 10.1037/h0056600. [DOI] [PubMed] [Google Scholar]
- Rashkis H, Shaskan D. The effects of group psychotherapy on personality inventory scores. American Journal of Orthopsychiatry. 1946;16:345–349. doi: 10.1111/j.1939-0025.1946.tb05388.x. [DOI] [PubMed] [Google Scholar]
- Raskin NJ. An analysis of six parrallel studies of the therapeutic process. Journal of Consulting Psychology. 1949;13:206–221. doi: 10.1037/h0057159. [DOI] [PubMed] [Google Scholar]
- Revelle W. Psychology Faculty Profile: William Revelle. 2011 Retrieved December 11, 2005, from http://www.wcas.northwestern.edu/psych/people/faculty/faculty_individual_pages/Revelle.htm.
- Roberts BW, Caspi A, Moffitt TE. Work experiences and personality development in young adulthood. Journal of Personality and Social Psychology. 2003;84(3):582–593. [PubMed] [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological bulletin. 2000;126(1):3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Kuncel N, Shiner RN, Caspi A, Goldberg L. The power of personality: A comparative analysis of the predictive validity of personality traits, SES, and IQ. Perspectives in Psychological Science. 2007;4(2):313–346. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Smith J, Jackson JJ, Edmonds G. Compensatory conscientiousness and health in older couples. Psychological Science. 2009;20(5):553–559. doi: 10.1111/j.1467-9280.2009.02339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological bulletin. 2006a;132(1):1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Personality traits change in adulthood: reply to Costa and McCrae (2006) Psychol Bull. 2006b;132(1):29–32. doi: 10.1037/0033-2909.132.1.29. [DOI] [PubMed] [Google Scholar]
- Rogers CR. Personality change in psychotherapy. International Journal of Social Psychiatry. 1955;1(1):31–41. [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- Rychlak JF. Introduction to personality and psychotherapy: A theory-construction approach. 1973:562. [Google Scholar]
- Schafer R. Psychological test evaluation of personality change during intensive psychotherapy. Psychiatry: Journal for the Study of Interpersonal Processes. 1955;18:175–192. doi: 10.1080/00332747.1955.11023004. [DOI] [PubMed] [Google Scholar]
- Schlendorf KH, Nasir K, Blumenthal RS. Limitations of the Framingham risk score are now much clearer. Prev Med. 2009;48(2):115–116. doi: 10.1016/j.ypmed.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Scollon CN, Diener E. Love, work, and changes in extraversion and neuroticism over time. Journal of Personality and Social Psychology. 2006;91(6):1152–1165. doi: 10.1037/0022-3514.91.6.1152. [DOI] [PubMed] [Google Scholar]
- Shedler J. The efficacy of psychodynamic psychotherapy. American Psychologist. 2010;65(2):98–109. doi: 10.1037/a0018378. [DOI] [PubMed] [Google Scholar]
- Sherman DK, Mann T, Updegraff JA. Approach / avoidance motivation, message framing, and health behavior: Understanding the congruency effect. Motivation and Emotion. 2006;30:164–168. doi: 10.1007/s11031-006-9001-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JA. Personality and psychotherapy: Treating the whole person. New York: Guilford; 2005. [Google Scholar]
- Smith TW, Glazer K, Ruiz JM, Gallo LC. Hostility, anger, aggressiveness, and coronary heart disease: An interpersonal perspective on personality, emotion, and health. Journal of Personality. 2004;72(6):1217–1270. doi: 10.1111/j.1467-6494.2004.00296.x. [DOI] [PubMed] [Google Scholar]
- Snyder WU. An investigation of the nature of nondirective psychotherapy. Journal of General Psychology. 1945;13:169–175. doi: 10.1080/00221309.1945.10544506. [DOI] [PubMed] [Google Scholar]
- Spiegel D. Mind matters in cancer survival. JAMA : the journal of the American Medical Association. 2011;305(5):502–503. doi: 10.1001/jama.2011.69. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2(8668):888–891. doi: 10.1016/s0140-6736(89)91551-1. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Butler LD, Giese-Davis J, Koopman C, Miller E, DiMiceli S, Kraemer HC. Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer: a randomized prospective trial. Cancer. 2007;110(5):1130–1138. doi: 10.1002/cncr.22890. [DOI] [PubMed] [Google Scholar]
- Stock D. The self concept and feeling toward others. Journal of Consulting Psychology. 1949;13:176–180. doi: 10.1037/h0059697. [DOI] [PubMed] [Google Scholar]
- Sutin AR, Costa PT., Jr Reciprocal influences of personality and job characteristics across middle adulthood. Journal of Personality. 2010;78(1):257–288. doi: 10.1111/j.1467-6494.2009.00615.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Costa PT, Jr, Miech R, Eaton WW. Personality and career success: Concurrent and longitudinal relations. European Journal of Personality. 2009;23(2):71–84. doi: 10.1002/per.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot NL, Duberstein PR, Butzel JS, Cox C, Giles DE. Personality traits and symptom reduction in a group treatment for women with histories of childhood sexual abuse. Comprehensive psychiatry. 2003;44(6):448–453. doi: 10.1016/S0010-440X(03)00142-1. [DOI] [PubMed] [Google Scholar]
- Tang TZDRJHSDAJSRSB. Personality change during depression treatment. Archives of General Psychiatry. 2009;66(12):1322–1330. doi: 10.1001/archgenpsychiatry.2009.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Costa PT., Jr Smoking and the Five-Factor Model of personality. Addiction. 2004;99(4):472–481. doi: 10.1111/j.1360-0443.2004.00687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaillant GE. Adaptation to life. Harvard University Press; 1977. [Google Scholar]
- van der Ploeg HM, Kleijn WC, Mook J, van Donge M, Pieters AM, Leer JW. Rationality and antiemotionality as a risk factor for cancer: concept differentiation. Journal of psychosomatic research. 1989;33(2):217–225. doi: 10.1016/0022-3999(89)90049-4. [DOI] [PubMed] [Google Scholar]
- Vargas MJ. Changes in self-awareness during client-centered therapy. In: Dymond CRRRF, editor. Psychotherapy and Cersonality Change. Chicago, IL: University of Chicago Press; 1954. [Google Scholar]
- Watson D. On traits and temperament: General and specific factors of emotional experience and their relation to the Five-Factor Model. Journal of personality. 1992;60:441–446. doi: 10.1111/j.1467-6494.1992.tb00980.x. [DOI] [PubMed] [Google Scholar]
- Watson M D-HJ, Haviland J, Bliss J. Psychological coping and cancer: Study results should not have been dismissed. British Medical Journal. 2003;326:598. doi: 10.1136/bmj.326.7389.598/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. American Psychologist. 2007;62(2):71–83. doi: 10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Schneider JA, Arnold SE, Bienias JL, Bennett DA. Conscientiousness and the incidence of Alzheimer disease and mild cognitive impairment. Arch Gen Psychiatry. 2007;64(10):1204–1212. doi: 10.1001/archpsyc.64.10.1204. [DOI] [PubMed] [Google Scholar]
- Woolf SH. The meaning of translational research and why it matters. JAMA. 2008;299(2):211–213. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
- Wyman PA, Brown CH, LoMurray M, Schmeelk-Cone K, Petrova M, Yu Q, Wang W. An outcome evaluation of the Sources of Strength suicide prevention program delivered by adolescent peer leaders in high schools. American journal of public health. 2010;100(9):1653–1661. doi: 10.2105/AJPH.2009.190025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman DM, Prusoff BA, Weissman MM, Padian NS. Personality as a predictor of psychotherapy and pharmacotherapy outcome for depressed outpatients. Journal of consulting and clinical psychology. 1980;48(6):730–735. doi: 10.1037//0022-006x.48.6.730. [DOI] [PubMed] [Google Scholar]