Abstract
Background
An in-depth understanding of risk factors for revision TKA is needed to minimize the burden of revision surgery. Previous studies indicate that hospital and community characteristics may influence outcomes after TKA, but a detailed investigation in a diverse population is warranted to identify opportunities for quality improvement.
Questions/purposes
We asked: (1) What is the frequency of revision TKA within 10 years of primary arthroplasty? (2) Which patient demographic factors are associated with revision within 10 years of TKA? (3) Which community and institutional characteristics are associated with revision within 10 years of TKA?
Methods
We identified 301,955 patients who underwent primary TKAs in New York or California from 1997 to 2005 from statewide databases. Identifier codes were used to determine whether they underwent revision TKA. Patient, community, and hospital characteristics were analyzed using multivariable regression modeling to determine predictors for revision.
Results
The frequency of revision was 4.0% at 5 years after the index arthroplasty and 8.9% at 9-years. Patients between 50 and 75 years old had a lower risk of revision than patients younger than 50 years (hazard ratio [HR], 0.47; 95% CI, 0.44, 0.50). Black patients were at increased risk for needing revision surgery (HR, 1.39; 95% CI, 1.29, 1.49) after adjustment for insurance type, poverty level, and education. Women (HR, 0.82; 95% CI, 0.79, 0.86) and Medicare recipients (HR, 0.82; 95% CI, 0.79, 0.86) were less likely to undergo revision surgery, whereas those from the most educated (HR, 1.09; 95% CI, 1.02, 1.16) and the poorest communities (HR, 1.08; 95% CI, 1.01, 1.15) had modest increases in risk of revision. Mid-volume hospitals (200–400 annual cases) had a reduction of early revision (HR, 0.91; 95% CI, 0.83, 0.99) compared with those performing less than 200 cases annually, whereas higher-volume hospitals (greater than 400 cases) showed little effect compared with low-volume hospitals.
Conclusions
Patient, community, and institutional characteristics affect the risk for revision within 10 years of index TKA. These data can be used to develop process improvement and implant surveillance strategies among high-risk patients.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
The prevalence of all-cause revision TKAs in the United States was 8.2% from 1990 to 2002 [20]. Although the percentage of patients undergoing revision TKAs remains relatively stable [18], the volume of revisions will continue to grow as primary TKAs are performed more frequently. The technical challenge [18], increased medical complications [18], and increased financial burdens [25] associated with revision TKAs underscore the need to better understand the circumstances surrounding the procedure and to develop approaches that minimize its occurrence.
Previous investigations have provided substantial insight into the reasons for reoperation after primary TKA, specifically infection, aseptic loosening, instability, and polyethylene wear [2, 5, 24]. Research has identified patient factors such as age, sex, obesity, and comorbidities that may increase the risk for revision TKA [18, 31]. Some authors [13, 23, 34] have indicated that characteristics related to the hospital and the surrounding community may affect outcomes after TKA. However, these studies provided a relatively limited assessment of these characteristics and focused exclusively on the Medicare population [13, 23] or one state [34]. A comprehensive assessment of hospital and community characteristics in a broader payer mix is needed to further characterize their influence on the delivery of care for TKA.
In the current investigation, we sought to overcome these shortcomings by using administrative databases from two states (California and New York) to evaluate the following research questions: (1) What is the frequency of revision TKA within 10 years of primary arthroplasty? (2) Which patient demographic factors are associated with early revision TKA? (3) Which community and institutional characteristics are associated with early revision TKA?
Patients and Methods
Study Population and Data Sources
The New York State Department of Health Statewide Planning and Research Cooperative System collects information on all discharges from nonfederal acute-care hospitals in the state. We used this system’s data from 1997 to 2005, as the recording of unique patient identifiers for patients began in 1997. The California Office of Statewide Health Planning and Development maintains a similar database, from which we used data from 1997 to 2005.
The American Hospital Association (AHA) Annual Survey provides information on hospital characteristics. These data were linked to the New York and California discharge data using AHA hospital identifiers and Healthcare Utilization Project linkage files, enabling us to identify teaching status, number of beds, and rurality. US Census Bureau data were used to estimate community poverty and educational levels based on the patient’s residential zip code.
The index cohort was defined as New York and California residents undergoing a primary TKA (ICD-9-CM Procedure Code 81.54) between 1997 and 2005 with no diagnosis code indicating a prior knee arthroplasty (ICD-9-CM Code V43.65). A total of 301,955 primary TKAs were identified as eligible for this project after applying these criteria (186,773 [62%] in California; 115,182 [38%] in New York).
The median age for patients undergoing primary TKA was 69 years (interquartile range, 61–76 years). The majority (68%) of patients were between 50 and 75 years, male (64%), and white (82%) (Table 1). Medicare was the most common insurance type (60%), followed by private insurance (31%). Osteoarthritis was the most common diagnosis (94%), followed by inflammatory arthritis (5%).
Table 1.
Patient demographics at the time of index TKA (n = 301,955)
| Patient factors | Number of patients (%) |
|---|---|
| Age | |
| < 50 years | 18,351 (6) |
| 50–75 years | 205,191 (68) |
| > 75 years | 78,413 (26) |
| Sex | |
| Female | 109,440 (36) |
| Male (missing for 11 patients) | 192,504 (64) |
| Race | |
| White | 247,561 (82) |
| Black | 19,279 (6.4) |
| Other | 23,338 (8) |
| Unknown | 11,777 (4) |
| Insurance type | |
| Medicare | 181,721 (60) |
| Medicaid | 11,097 (4) |
| Private | 91,977 (31) |
| Self-pay | 1126 (0.4) |
| Other | 16,034 (5) |
| Indication for total joint arthroplasty | |
| Osteoarthritis | 282,194 (94) |
| Inflammatory arthritis | 14,301 (4.7) |
| Avascular necrosis | 2408 (1) |
| Congenital | 206 (0.1) |
| Fracture | 1180 (0.4) |
| Neoplasm | 1054 (0.3) |
| Other | 612 (0.2) |
| Elixhauser comorbidities | |
| Congestive heart failure | 7376 (2) |
| Valvular disease | 10,902 (4) |
| Peripheral vascular disease | 3817 (1) |
| Other neurologic disorders | 5457 (2) |
| Chronic obstructive pulmonary disease | 32,899 (11) |
| Diabetes | 42,194 (14) |
| Hypothyroidism | 32,459 (11) |
| Obesity | 30,887 (10) |
| Coagulopathy | 2557 (1) |
| Fluid and electrolyte disorders | 14,903 (5) |
| Depression | 14,100 (5) |
| Hypertension | 163,802 (54) |
Primary TKA was performed most commonly in nonteaching hospitals (79%), urban hospitals (93%), and low-volume centers (< 200/year, 62%), with 11% performed in high-volume centers (> 400/year) (Table 2). The median percentage of people with a college degree in the patients’ communities was 22%, the median household income was USD 36,905, and the median percentage of people below the poverty level in the patients’ communities was 8% (Table 2).
Table 2.
Hospital and community factors from the index TKA (n = 301,955)
| Factor | Categories | Number (%) |
|---|---|---|
| Hospital | ||
| Annual TKA volume | ≤ 200 | 187,111 (62) |
| 201–400 | 81,993 (27) | |
| > 400 | 32,851 (11) | |
| Number of beds | ≤ 50 | 6878 (2.3) |
| 51–200 | 91,758 (30) | |
| 201–400 | 137,471 (46) | |
| > 400 | 65,848 (22) | |
| Teaching hospital | Teaching | 62,924 (21) |
| Nonteaching | 239,031 (79) | |
| Urban/rural hospital | Urban | 279,940 (93) |
| Rural | 22,015 (7) | |
| Community | ||
| Education (% college graduate) | Quartile 1 | 15% |
| Median | 22% | |
| Quartile 3 | 35% | |
| Median household income | Quartile 1 | $26,744 |
| Median | $36,905 | |
| Quartile 3 | $51,660 | |
| Poverty level (%) | Quartile 1 | 5% |
| Median | 8% | |
| Quartile 3 | 12% | |
| Population density (per square mile) | Quartile 1 | 450 |
| Median | 2753 | |
| Quartile 3 | 7276 | |
Comprehensiveness of Data Sources
All nonfederal acute care facilities in New York are required to report inpatient and outpatient data to the New York State Department of Health, Statewide Planning and Research Cooperative System (SPARCS) in a designated format within 60 days after the month of patient discharge. One hundred percent of the facility’s data is due 180 days after the end of the facility’s fiscal year. The quality and completeness of the data reported by each hospital are reviewed by SPARCS administrators and the Data Quality Unit of the state’s Bureau of Biometrics. Similar reporting requirements and regulatory audits are used in California to ensure completeness of data in the Office of Statewide Health Planning and Development (OSHPD) database.
Although SPARCS data have been used in numerous published studies in the orthopaedic and general medical literature, the validity of the procedural code data has not been reported. We queried SPARCS for all TKAs performed at our institution from January 1, 2009 to December 1, 2009. Compared with our institution’s register, SPARCS captured 99% of all TKAs performed at our institution in 2009.
SPARCS and OSPHD provide data only for facilities in New York and California, respectively. Data are not available if patients seek followup care at institutions outside these states. To minimize the potential effect of missing out-of-state followups on our estimates of revision after TKA, we limited our analysis to in-state residents of New York and California. From 1997 to 2005, 2.7% of patients who underwent a primary TKA in New York or California were out-of-state residents and subsequently were excluded from our cohort.
Endpoint of Analysis
Revision TKA was defined among patients identified in the index cohort as having one of the revision TKA procedure codes (ICD-9-CM Codes 00.80–00.84, 81.55) either on a subsequent day during the same admission (in-hospital revision before discharge) or in a subsequent admission during the study period. Given that 10-year survivorship for primary TKAs has exceeded 97% in several long-term studies [9, 29, 36], a cutoff point of revision within 10 years was used.
Patients not undergoing revision TKAs were censored at the time of in-hospital death (in the index or a subsequent admission) or at the end of the study period (December 31, 2006), whichever came first. Owing to concerns for out-of-hospital mortality, which is not captured in these data, we used CDC life tables to estimate censoring data for patients not expected to live to the end of the followup period. Patients also were censored if they underwent a subsequent primary TKA before their revision TKA to minimize potential misclassification of revision laterality [17]. This censoring occurred only at the time of any revision surgery.
Definitions of Predictors
The patient demographics age in years, sex, race, surgical diagnosis, comorbidity index, insurance status, education level, and household income were considered potential patient- and community-level predictors of early revision TKA. Race is a mandatory data field in California but is a voluntarily reported field in New York. Race was defined as white, black, Hispanic, Asian/Pacific Islander, Native American, or other.
Surgical diagnosis for primary TKA was defined as osteoarthritis (OA), inflammatory arthritis (eg, rheumatoid arthritis), trauma, avascular necrosis, or other based on the ICD-9-CM diagnosis fields. The “other” category was used only when none of the aforementioned diagnoses were coded. When a second diagnosis was coded in addition to OA, the non-OA diagnosis was given primacy. This was done to minimize overreporting of OA as the primary reason for TKA.
Comorbidity scores were calculated using the Elixhauser comorbidity index [10]. Expected payer (insurance status) was defined as private, health maintenance organization, self-pay, Medicare, Medicaid, no charge, or other.
Community and institutional characteristics including education level, household income, percentage below poverty level, and population density were estimated based on patient residential zip code using US Census Bureau data from the 2000 US Census. Hospital TKA volume was calculated for the four quarters before the quarter of the index surgery for each patient. The number of hospital beds and teaching status were identified using the 2010 AHA Annual Survey (American Hospital Association; Chicago, IL, USA) for each institution. The designation of the hospital as urban or rural was based on the Rural-Urban Commuting Area Codes from the US Census Bureau.
Reason for Revision
The reason for revision was determined from review of diagnosis coding at the time of revision. ICD-9-CM codes were used to categorize reasons for revision as acute fracture, septic failure, aseptic failure, and other (Table 3).
Table 3.
Reasons for revision (ICD-9 coding)
| Reason | Number of Revisions (% of all revisions) |
|---|---|
| Acute fracture | 272 (3%) |
| 821 Fracture of other and unspecified parts of femur | |
| 822 Fracture of patella | |
| 823 Fracture of tibia and fibula | |
| 827 Other, multiple, and ill-defined fractures of lower limb | |
| 733.15 Pathologic fracture of other specified part of femur | |
| 733.8 Malunion and nonunion of fracture | |
| 733.9 Other and unspecified disorders of bone and cartilage | |
| Septic failure | 2623 (27%) |
| 996.60 Infection and inflammatory reaction due to unspecified device, implant and graft | |
| 996.66 Infection and inflammatory reaction due to internal joint prosthesis | |
| 996.67 Infection and inflammatory reaction due to other internal orthopedic device, implant and graft | |
| 996.69 Infection and inflammatory reaction due to other internal prosthetic device, implant, and graft | |
| 998.51 Infected postoperative seroma | |
| 998.59 Other postoperative infection | |
| Aseptic failure | 6603 (67%) |
| 998 Other complications of procedures, not elsewhere classified | |
| 999 Complications of medical care, not elsewhere classified | |
| 996.4 Mechanical complication of internal orthopedic device, implant, and graft | |
| 996.59 Mechanical complication due to other implant and internal device, not elsewhere classified | |
| 719.6 Other and unspecified disorders of joint (lower leg) | |
| 718.4 Other derangement of joint | |
| 718.5 Ankylosis of joint | |
| 718.6 Unspecified intrapelvic protrusion of acetabulum | |
| 996.7 Other complications of internal prosthetic device, implant, and graft | |
| Other | 331 (3%) |
| 715.96 Osteoarthrosis, unspecified whether generalized or localized (lower leg) | |
| 715.36 Osteoarthrosis, localized, not specified whether primary or secondary (lower leg) | |
| 736.6 Other acquired deformities of knee | |
Statistical Analysis
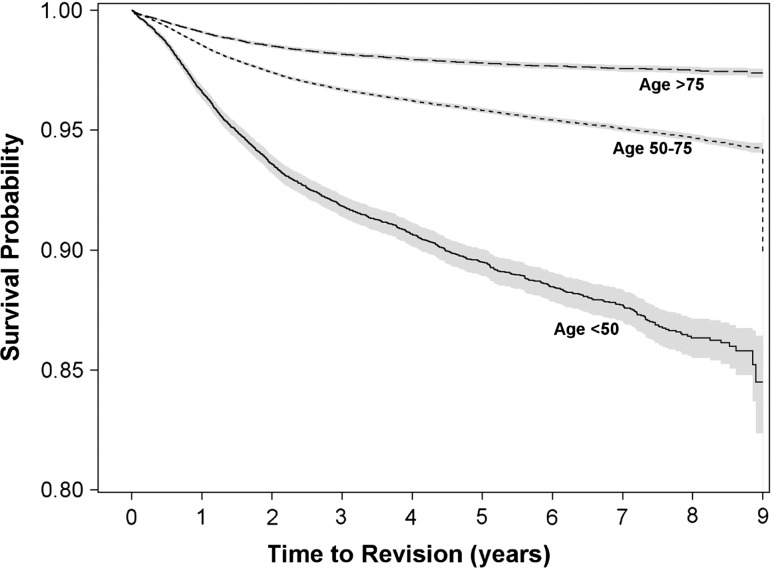
Patient, community, and institutional variables found to be associated with early revision TKA in univariate analysis were included in a Cox proportional hazards model evaluating time to revision TKA in the overall cohort. Hazard ratios indicating the relative risk of early revision TKA (compared with a reference group) were calculated for each patient, community, and institutional characteristic studied (while controlling for the other variables in the model). The probability of undergoing revision TKA was calculated using Kaplan-Meier methods for the entire cohort and stratified by age group (younger than 50 years, 50–75 years, older than 75 years). The threshold for statistical significance was set at p < 0.05. All statistical analyses were performed using SAS 9.2 (SAS Institute; Cary, NC, USA).
Results
Frequency of and Reasons for Early Revision
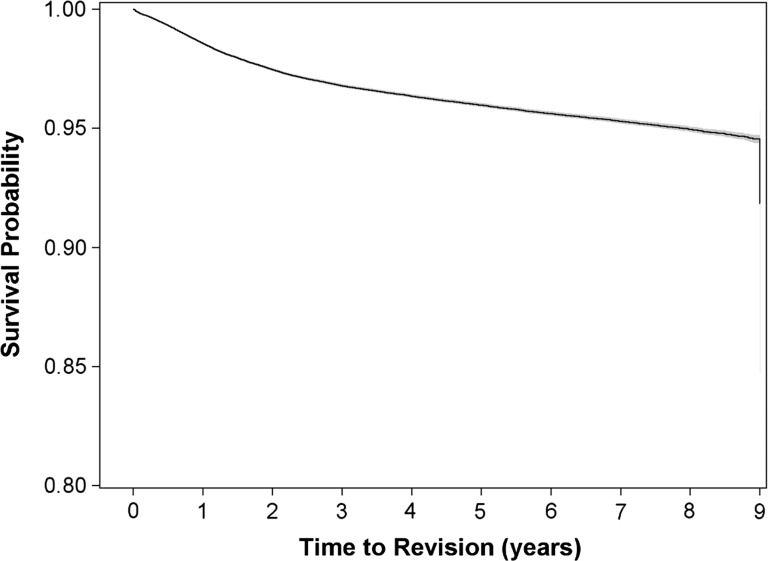
The most common reason for early revision was aseptic failure (67%), followed by septic failure (27%) (Table 3). Kaplan-Meier analysis showed revision rates of 4% and 8.9% at 5 and 9 years after index surgery, respectively (Fig. 1).
Fig. 1.
The Kaplan-Meier survivorship curve shows revision TKA rates of 4% and 8.9% at 5 and 9 years after index surgery, respectively.
Patient Demographics and Early Revision
Patients 50 to 75 years old had a 53% (hazard ratio [HR], 0.47; 95% CI, 0.44, 0.50) reduced risk of revision TKA compared with patients younger than 50 years (controlling for all other factors in the model), whereas the oldest patients (75+ years) had a 73% reduced risk (HR, 0.27; 95% CI, 0.25, 0.30) (Fig. 2). Female patients were 18% less likely to undergo revision surgery than male patients (HR, 0.82; 95% CI, 0.79, 0.86). Black patients were 39% more likely to undergo revision TKA than white patients (HR, 1.39; 95% CI, 1.29, 1.49). Medicare recipients were 18% less likely to have a revision TKA than those with private insurance (HR, 0.82; 95% CI, 0.79, 0.86). There was no association between Medicaid and early revision TKA. Patients with a diagnosis of inflammatory arthritis at the time of the primary TKA were 21% less likely to undergo revision TKA than patients with osteoarthritis (HR, 0.79; 95% CI, 0.72, 0.87). However, fracture, neoplasm, and other diagnoses at the time of the primary TKA carried increased risks of revision. The most frequent diagnoses in the ‘other’ category were chronic osteomyelitis and aseptic necrosis. Patients with a comorbid diagnosis of depression had a 12% increased risk of early revision (HR, 0.47; 95% CI, 1.02,1.24), whereas patients with chronic obstructive pulmonary disease, coagulopathy, and diabetes had 16% (HR, 1.16; 95% CI. 1.09,1.23), 22% (HR, 1.22; 95% CI, 1.00,1.49), and 7% (HR, 1.07; 95% CI, 1.01,1.13) increased risk of early revision, respectively (Table 4). Obesity did not significantly affect the risk of revision.
Fig. 2.
The Kaplan-Meier survivorship curves show revision TKA rates categorized by age group (younger than 50 years, 50–75 years, older than 75 years). Patients 50 to 75 years old and patients older than 75 years had lower revision TKA rates compared with patients younger than 50 years.
Table 4.
Patient factors associated with early revision TKA (n = 301,955)
| Factor | Hazard ratio | 95% CI | p value |
|---|---|---|---|
| Age | |||
| 50–75 years versus < 50 years | 0.47 | 0.44, 0.50 | < 0.001 |
| > 75 years versus < 50 years | 0.27 | 0.25, 0.30 | < 0.001 |
| Female versus male sex | 0.82 | 0.79, 0.86 | < 0.001 |
| Race | |||
| Black versus white | 1.39 | 1.29, 1.49 | < 0.001 |
| Other versus white | 0.96 | 0.89, 1.04 | 0.315 |
| Unknown versus white | 1.07 | 0.96, 1.18 | 0.219 |
| Insurance | |||
| Medicare versus private | 0.82 | 0.79, 0.86 | < 0.001 |
| Medicaid versus private | 0.98 | 0.88, 1.08 | 0.654 |
| Self-pay versus private | 0.93 | 0.69, 1.26 | 0.634 |
| Other versus private | 1.53 | 1.43, 1.64 | < 0.001 |
| Indication for TKA | |||
| Inflammatory arthritis versus osteoarthritis | 0.79 | 0.72, 0.87 | < 0.001 |
| Avascular necrosis versus osteoarthritis | 1.11 | 0.89, 1.37 | 0.358 |
| Congenital versus osteoarthritis | 0.86 | 0.43, 1.71 | 0.657 |
| Acute fracture versus osteoarthritis | 1.73 | 1.37, 2.18 | < 0.001 |
| Neoplasm versus osteoarthritis | 1.92 | 1.55, 2.38 | < 0.001 |
| Other versus osteoarthritis | 1.54 | 1.13, 2.10 | 0.007 |
| Elixhauser comorbidity | |||
| Congestive heart failure | 1.07 | 0.93, 1.23 | 0.324 |
| Valvular disease | 0.96 | 0.85, 1.08 | 0.476 |
| Peripheral vascular disease | 1.09 | 0.91, 1.32 | 0.355 |
| Other neurologic disorders | 1.04 | 0.90, 1.21 | 0.579 |
| Chronic obstructive pulmonary disease | 1.16 | 1.09, 1.23 | < 0.001 |
| Diabetes | 1.07 | 1.01, 1.13 | 0.027 |
| Hypothyroidism | 1.04 | 0.97, 1.12 | 0.279 |
| Coagulopathy | 1.22 | 1.00, 1.49 | 0.047 |
| Obesity | 1.02 | 0.95, 1.09 | 0.578 |
| Fluid and electrolyte disorders | 1.00 | 0.91, 1.10 | 0.972 |
| Depression | 1.12 | 1.02, 1.24 | 0.018 |
| Hypertension | 0.96 | 0.92, 1.00 | 0.058 |
Community Factors, Institutional Factors, and Early Revision
Mid-volume hospitals (201–400 annual cases) had a 9% reduced risk of revision (HR, 0.91; 95% CI, 0.83, 0.99) compared with hospitals performing 200 or less cases annually, but there was no difference between the highest (> 400 annual cases) and lowest volume categories (Table 5). There was an increased risk of revision with increasing number of beds (> 400 beds versus ≤ 50 beds; HR, 1.21; 95% CI, 1.04, 1.42). Patients undergoing TKAs in California had a 10% decreased risk of revision compared with patients undergoing TKAs in New York (HR, 0.90; 95% CI, 0.86, 0.94). Patients from communities with the highest education level (HR, 1.09; 95% CI, 1.02, 1.16) and the most poverty-stricken communities (HR, 1.08; 95% CI, 1.01, 1.15) also had a modestly increased risk of revision TKA (Table 5).
Table 5.
Community and hospital factors associated with early revision TKA (n = 301,955 patients)
| Factor | Hazard ratio | 95% CI | p value |
|---|---|---|---|
| Hospital | |||
| TKA volume | |||
| > 400 versus < 200 | 1.00 | 0.95, 1.05 | 0.973 |
| 200–400 versus < 200 | 0.91 | 0.83, 0.99 | 0.025 |
| Bed size | |||
| 50–200 versus < 50 | 1.16 | 1.00, 1.35 | 0.049 |
| 200–400 versus < 50 | 1.18 | 1.01, 1.36 | 0.034 |
| > 400 versus < 50 | 1.21 | 1.04, 1.42 | 0.015 |
| Teaching versus nonteaching | 0.95 | 0.89, 1.01 | 0.087 |
| Urban versus rural | 0.94 | 0.87, 1.02 | 0.167 |
| California versus New York | 0.90 | 0.86, 0.94 | < 0.001 |
| Community | |||
| Education | |||
| 50th versus 25th percentile | 1.03 | 0.97, 1.09 | 0.306 |
| 75th versus 25th percentile | 1.01 | 0.95, 1.07 | 0.836 |
| 100th versus 25th percentile | 1.09 | 1.02, 1.16 | 0.011 |
| Poverty | |||
| 50th versus 25th percentile | 1.03 | 0.97, 1.09 | 0.336 |
| 75th versus 25th percentile | 1.04 | 0.98, 1.11 | 0.225 |
| 100th versus 25th percentile | 1.08 | 1.01, 1.15 | 0.023 |
Discussion
An in-depth understanding of risk factors for early revision TKA is needed to minimize the burden of revision surgery, particularly as use of primary TKA expands. Previous investigations of the influence of hospital characteristics on TKA outcomes largely focused on procedural volume [23, 34], while evaluation of community characteristics has been based primarily on urban or rural status [13]. Additionally, the populations studied were either exclusively Medicare patients [13, 23] or from one state [34]. We have addressed these shortcomings by using multiple-payer data from two states to provide a comprehensive assessment of patient, hospital, and community characteristics and their influence on the risk of revision within 10 years of primary TKA. The frequency of revision among a cohort of patients who underwent primary TKA in New York or California from 1997 to 2005 was 4.0% at 5 years and 8.9% at 9 years. The most pronounced risk factors for revision in our cohort included younger age, male sex, race (black), and lower hospital volume.
Our study has limitations, specifically those inherent to the use of administrative databases in health services research. As mentioned above, we were unable to follow patients who sought subsequent care outside the state of their index procedure. We attempted to reduce this potential bias by limiting our cohort to residents of the states who would be more likely to have revision in the state in which they live. Nevertheless, this likely leaves us with a relatively conservative estimate of the frequency of early revision TKA. Additionally, owing to the time of our data (1997 to 2005), we were unable to incorporate detailed ICD-9-CM diagnosis coding of reason for revision (introduced on October 1, 2005). Although our categorization of complications (done by grouping ICD-9-CM codes) is less precise than the updated codes, our rate of infection as a reason for revision (26.7%) is similar to that reported in a study using the updated coding (25.2%) [5]. The uncertainties of this aspect of our data make it difficult to draw conclusions regarding reasons for early revision, but the associations we report can provide insight to shape future prospective research. Furthermore, the time of our study (1997 to 2005) may limit the direct applicability to the current practice environment, as practice patterns and community characteristics may have changed in the interim. Demographic shifts in communities may affect patterns of patient migration to specific institutions and may influence other social determinants of health. Additionally, our reliance on administrative data does not allow us to evaluate the association between individual income and education levels on risk for early revision. We are able to evaluate only the association of the surrounding community’s poverty and education levels with the risk of early revision after TKA. Using census-based approaches to indirectly measure socioeconomic status has been validated against individual data of a large health plan [19], and this approach has been used in previous studies regarding the use of arthroplasties [7, 12, 33]. Finally, our cutoff for followup was arbitrarily designated as 10 years. This was done to allow for a larger sample size and larger number of revisions to be included in the study, therefore increasing the statistical power of the study. Despite these drawbacks, using statewide databases offers an important advantage. Our inclusion of statewide data from two diverse states allows us to expand on prior investigations limited by age and payer type [8, 13, 18]. The significant differences in risk for revision noted by payer type and location show the importance of including patients from an expanded geographic and payer mix. This diversity allows our findings to provide additional perspective on the circumstances surrounding early revision TKA.
Frequency of and Reasons for Early Revision
In this study, which surveyed two large administrative databases and which included more than 300,000 primary TKAs, we found that survivorship was 96% and 91% at 5 and 9 years after the index arthroplasty, respectively. This is lower than commonly reported in single-center intermediate-term studies [4, 28], but in the range of what has been reported in systematic reviews of large national registries [21, 26]. The discrepancy between our results and those of single-center series is found elsewhere in the literature and may be at least partially explained by selection bias in studies published from institutions with expert surgeons and/or surgeons involved in product development [26]. Our population-based results have greater generalizability than single-center series and provide surgeons with data that are suitable for patient counseling, particularly in the United States.
Patient Demographics and Revision Within 10 Years
Our study showed an increased risk of revision within 10 years of index TKA in black patients, even after controlling for insurance type, poverty level, and education. Some studies have outlined disparities in access to [3] and use of [32] TKA, but less attention has been directed toward disparities in complications after TKA. Although differences in length of stay [6], infection [22, 34], medical complications [34], and mortality [22, 34] have been reported in black patients after TKA, our results add to the existing literature by showing an increased risk of revision after carefully controlling for other characteristics that may confound the effect of race. Although previous studies indicate that black patients are less likely to undergo primary TKA, our results indicate that they are more likely to undergo revision surgery. Patient perceptions of disease [14] and physician bias [3] contribute to disparities in the use of primary TKA and also may contribute to the frequency of revision arthroplasty. The influence of race on the risk of revision deserves closer attention in future clinical studies.
Our study confirms prior findings that male [8, 18] and younger [8, 30, 31] patients are at increased risk of early revision TKA. When viewed in the context that TKAs are being performed more frequently in younger patients [1], this finding suggests a need for continued efforts to improve outcomes in this population. Surgeons may find this information helpful in counseling their younger patients regarding the risk of revision TKA. Our analysis of comorbidities indicates that patients with coagulopathy, chronic obstructive pulmonary disease, depression, and diabetes are at increased risk for revision within 10 years of the index TKA. A diagnosis of obesity did not significantly influence the risk of revision, but this may be attributable to the dichotomous nature of this variable in our dataset (as opposed to reporting BMI on a continuous scale).
Community Factors, Institutional Factors, and Revision Within 10 Years
Our finding that patients from the most impoverished regions had a higher risk of early revision suggests the need for further evaluation of the role of social support in postoperative outcomes. The finding that patients from communities with the highest education levels had a higher risk of early revision TKA was relatively unexpected, given a previous study showed higher education levels to be predictive of improved functional outcomes after THA [37]. However, previous research suggests that patients with higher education levels are more likely to return for followup [27, 35]. These return visits provide patients with additional opportunities to discuss their progress with their surgeon, potentially providing a more sensitive way to identify patients who would benefit from revision TKA.
Previous investigations on the relationship between hospital volume and TKA have shown decreased medical complications [15, 34] and improved functional outcomes [16] among patients who undergo total joint arthroplasties at higher-volume hospitals. However, the relationship between hospital volume and implant survivorship has not been as commonly addressed. By showing an increased risk of early revision in lower-volume hospitals in a dataset of multiple payers, we have expanded on the prior report of Manley et al. [23] of increased risk for revision TKA in low-volume hospitals among the Medicare population. Although these findings may increase interest in concentrating patient referrals for TKAs exclusively to high-volume centers, it is important to consider the implications of such recommendations on patient travel distance and access to care [11]. While additional investigation is underway to evaluate the relationship between hospital volume and long-term outcomes after total joint arthroplasty, policymakers and healthcare leaders should continue to strive for improvement in the quality of care at lower-volume centers. The relationship between volume and risk of early revision is not completely linear, as we did not find a significant difference in the risk of early revision between centers that performed more than 400 TKAs annually and those that performed fewer than 200 TKAs annually. This may be related to referral bias: large-volume hospitals may attract more complex primary cases, which may increase the risk of early revision and dampen the benefits of higher volume. It is difficult to establish case complexity with administrative data, and future clinical studies evaluating the risk of early revision should account for case complexity.
Our study confirms that patient-, community-, and institutional-level characteristics are associated with the frequency of early revision TKA. The increased risk for early revision in black patients lends additional support for continued research into the circumstances contributing to healthcare disparities. Although many of the risk factors that we have identified are not modifiable or may be difficult to control, our findings can be used to identify patients at the highest risk for failure of TKA. Broad, multidisciplinary strategies should be developed to optimize preoperative health status, improve coordination of care, maximize institutional efficiency, and ensure appropriate longitudinal implant surveillance among high-risk patients. These strategies have the potential to drive system-wide improvement in quality of care. Decreasing the risk of early revision can produce substantial cost savings during a time in which the use of arthroplasties is increasing and healthcare resources are increasingly strained. Proactive and anticipatory development of programs to mitigate the risk of early TKA failure will be essential to the continued delivery of high-value orthopaedic care.
Acknowledgments
We thank Timothy Wright PhD, Hospital for Special Surgery, New York, NY, for guidance in the development of the research questions and scientific approach, and Huong Do MA, Hospital for Special Surgery, New York, NY, for assistance with preparation of the data for further analysis.
Footnotes
One of the authors (CJD) certifies that he has received, during the study period, funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (Bethesda, MD, USA) (Grant T32-AR07281). One of the authors (SL) certifies that he has received, during the study period, funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (Grant R03 AR05063) and the Agency for Healthcare Research and Quality (Rockville, MD, USA) (Grant U18-HS16075). Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Hospital for Special Surgery, New York, NY, USA.
References
- 1.Bang H, Chiu YL, Memtsoudis SG, Mandl LA, Della Valle AG, Mushlin AI, Marx RG, Mazumdar M. Total hip and total knee arthroplasties: trends and disparities revisited. Am J Orthop (Belle Mead NJ). 2010;39:E95–E102. [PubMed] [Google Scholar]
- 2.Berend ME, Davis PJ, Ritter MA, Keating EM, Faris PM, Meding JB, Malinzak RA. “Thicker” polyethylene bearings are associated with higher failure rates in primary total knee arthroplasty. J Arthroplasty. 2010;25(6 suppl):17–20. doi: 10.1016/j.arth.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 3.Borkhoff CM, Hawker GA, Kreder HJ, Glazier RH, Mahomed NN, Wright JG. The effect of patients’ sex on physicians’ recommendations for total knee arthroplasty. CMAJ. 2008;178:681–687. doi: 10.1503/cmaj.071168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bozic KJ, Kinder J, Meneghini RM, Zurakowski D, Rosenberg AG, Galante JO. Implant survivorship and complication rates after total knee arthroplasty with a third-generation cemented system: 5 to 8 years followup. Clin Orthop Relat Res. 2005;430:117–124. doi: 10.1097/01.blo.0000146539.23869.14. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collins TC, Daley J, Henderson WH, Khuri SF. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230:251–259. doi: 10.1097/00000658-199908000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cram P, Vaughan-Sarrazin MS, Rosenthal GE. Hospital characteristics and patient populations served by physician owned and non physician owned orthopedic specialty hospitals. BMC Health Serv Res. 2007;7:155. doi: 10.1186/1472-6963-7-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curtin B, Malkani A, Lau E, Kurtz S, Ong K. Revision after total knee arthroplasty and unicompartmental knee arthroplasty in the Medicare population. J Arthroplasty. 2012;27:1480–1486. doi: 10.1016/j.arth.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 9.Duffy GP, Trousdale RT, Stuart MJ. Total knee arthroplasty in patients 55 years old or younger: 10- to 17-year results. Clin Orthop Relat Res. 1998;356:22–27. doi: 10.1097/00003086-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 11.FitzGerald JD, Soohoo NF, Losina E, Katz JN. Potential impact on patient residence to hospital travel distance and access to care under a policy of preferential referral to high-volume knee replacement hospitals. Arthritis Care Res (Hoboken). 2012;64:890–897. doi: 10.1002/acr.21611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Francis ML, Scaife SL, Zahnd WE, Cook EF, Schneeweiss S. Joint replacement surgeries among medicare beneficiaries in rural compared with urban areas. Arthritis Rheum. 2009;60:3554–3562. doi: 10.1002/art.25004. [DOI] [PubMed] [Google Scholar]
- 13.Heck DA, Melfi CA, Mamlin LA, Katz BP, Arthur DS, Dittus RS, Freund DA. Revision rates after knee replacement in the United States. Med Care. 1998;36:661–669. doi: 10.1097/00005650-199805000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: a comparison between African American and white patients. Arthritis Rheum. 2001;45:340–345. doi: 10.1002/1529-0131(200108)45:4<340::AID-ART346>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 15.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909–1916. doi: 10.1302/0301-620X.86B7.14358. [DOI] [PubMed] [Google Scholar]
- 16.Katz JN, Mahomed NN, Baron JA, Barrett JA, Fossel AH, Creel AH, Wright J, Wright EA, Losina E. Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56:568–574. doi: 10.1002/art.22333. [DOI] [PubMed] [Google Scholar]
- 17.Katz JN, Wright EA, Baron JA, Corbett KL, Nti AA, Malchau H, Wright J, Losina E. Predictive value of Medicare claims data for identifying revision of index hip replacement was modest. J Clin Epidemiol. 2011;64:543–546. doi: 10.1016/j.jclinepi.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khatod M, Inacio M, Paxton EW, Bini SA, Namba RS, Burchette RJ, Fithian DC. Knee replacement: epidemiology, outcomes, and trends in Southern California: 17,080 replacements from 1995 through 2004. Acta Orthop. 2008;79:812–819. doi: 10.1080/17453670810016902. [DOI] [PubMed] [Google Scholar]
- 19.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–710. doi: 10.2105/AJPH.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 21.Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293–297. doi: 10.1302/0301-620X.93B3.25467. [DOI] [PubMed] [Google Scholar]
- 22.Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87:1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 23.Manley M, Ong K, Lau E, Kurtz SM. Total knee arthroplasty survivorship in the United States Medicare population: effect of hospital and surgeon procedure volume. J Arthroplasty. 2009;24:1061–1067. doi: 10.1016/j.arth.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 24.Mulhall KJ, Ghomrawi HM, Scully S, Callaghan JJ, Saleh KJ. Current etiologies and modes of failure in total knee arthroplasty revision. Clin Orthop Relat Res. 2006;446:45–50. doi: 10.1097/01.blo.0000214421.21712.62. [DOI] [PubMed] [Google Scholar]
- 25.Oduwole KO, Molony DC, Walls RJ, Bashir SP, Mulhall KJ. Increasing financial burden of revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:945–948. doi: 10.1007/s00167-010-1074-8. [DOI] [PubMed] [Google Scholar]
- 26.Pabinger C, Berghold A, Boehler N, Labek G. Revision rates after knee replacement: cumulative results from worldwide clinical studies versus joint registers. Osteoarthritis Cartilage. 2013;21:263–268. doi: 10.1016/j.joca.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 27.Psaty BM, Cheadle A, Koepsell TD, Diehr P, Wickizer T, Curry S, VonKorff M, Perrin EB, Pearson DC, Wagner EH. Race- and ethnicity-specific characteristics of participants lost to follow-up in a telephone cohort. Am J Epidemiol. 1994;140:161–171. doi: 10.1093/oxfordjournals.aje.a117226. [DOI] [PubMed] [Google Scholar]
- 28.Rand JA, Ilstrup DM. Survivorship analysis of total knee arthroplasty: cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am. 1991;73:397–409. [PubMed] [Google Scholar]
- 29.Ritter MA, Worland R, Saliski J, Helphenstine JV, Edmondson KL, Keating EM, Faris PM, Meding JB. Flat-on-flat, nonconstrained, compression molded polyethylene total knee replacement. Clin Orthop Relat Res. 1995;321:79–85. [PubMed] [Google Scholar]
- 30.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975-1997: an update with special emphasis on 41,223 knees operated on in 1988-1997. Acta Orthop Scand. 2001;72:503–513. doi: 10.1080/000164701753532853. [DOI] [PubMed] [Google Scholar]
- 31.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51:428–436. [PMC free article] [PubMed] [Google Scholar]
- 32.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 33.Skinner J, Zhou W, Weinstein J. The influence of income and race on total knee arthroplasty in the United States. J Bone Joint Surg Am. 2006;88:2159–2166. doi: 10.2106/JBJS.E.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006;88:480–485. doi: 10.2106/JBJS.E.00629. [DOI] [PubMed] [Google Scholar]
- 35.Tejwani NC, Takemoto RC, Nayak G, Pahk B, Egol KA. Who is lost to followup?: a study of patients with distal radius fractures. Clin Orthop Relat Res. 2010;468:599–604. doi: 10.1007/s11999-009-0968-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Worland RL, Johnson GV, Alemparte J, Jessup DE, Keenan J, Norambuena N. Ten to fourteen year survival and functional analysis of the AGC total knee replacement system. Knee. 2002;9:133–137. doi: 10.1016/S0968-0160(01)00146-6. [DOI] [PubMed] [Google Scholar]
- 37.Young NL, Cheah D, Waddell JP, Wright JG. Patient characteristics that affect the outcome of total hip arthroplasty: a review. Can J Surg. 1998;41:188–195. [PMC free article] [PubMed] [Google Scholar]