Abstract
Background
The use of TKAs in young patients is increasing. Demographic characteristics and activity levels among this patient group may affect implant selection, performance, and survivorship. Patient age (≤ 55 years) and preoperative diagnosis have been used to define this patient group, with the presumption that these patients are more active than older patients with similar indications for TKA.
Questions/purposes
We questioned whether (1) demographic features of young patients support high activity expectations after TKA, and (2) preoperative or postoperative functional activity measures support projections that young patients are active after TKA.
Methods
We retrospectively compared demographic characteristics (gender, BMI, diagnosis) and functional activity profile (as determined by preoperative and postoperative UCLA activity score and functional subscores of The Knee Society and WOMAC instruments) for 150 patients 55 years old or younger (181 TKAs) and 262 patients who were between 65 to 75 years old (314 TKAs) at the time of surgery.
Results
Younger patients having TKAs were significantly more likely than older patients to be female (74% versus 60%, p < 0.001) and to have diagnoses other than osteoarthritis (18% versus 3%, p < 0.001). BMI was significantly greater among younger female patients than among other age and gender combinations (35 kg/m2 versus 31 kg/m2, p < 0.001). Male patients had higher mean postoperative UCLA activity scores (5.5 versus 4.4, p < 0.001), Knee Society function subscores (80.2 versus 66.4, p < 0.001), and WOMAC function subscores (82.8 versus 74.2, p < 0.01) compared with female patients, but these were not different in older versus younger patients.
Conclusions
Sustained high activity levels are not likely to be a principal cause of revision TKAs among younger patients when considering age and diagnosis alone. Determining the effect of activity on survivorship of prosthetic designs and techniques should be based on measured functional activity instead of using age and diagnosis as surrogates for activity.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
More than 600,000 TKAs are performed each year in the United States, including more than 70,000 performed for patients 55 years old or younger. Patients between 45 to 55 years old have been identified as the most rapidly growing age-defined subpopulation undergoing total knee replacement during the past decade [21]. Although reported clinical and functional scores among younger patients undergoing TKAs generally are satisfactory, TKAs for this patient group have been associated with higher revision rates when compared with rates in regional and national registries for patients older than 65 years [13–15, 26, 28, 33]. Specific factors associated with an increased risk of revision surgery include male sex, unicompartmental arthroplasty, and the use of cementless fixation [3–5]. Surgeons and investigators may attribute failures among younger patients to the effects of higher activity levels sustained over a longer time; however, studies have not agreed that the causes of failure among younger patients are related to wear, suggesting that the supposed relationship of youth, high activity, and wear-related failure may not be so direct [3, 20, 25, 31].
Even so, younger patients have been considered a unique patient cohort, and a preponderance of studies have used age as a surrogate for activity level, generally that increased activity levels may contribute to higher incidence of failure [5, 8–10, 12, 19, 27, 30, 32, 34]. Defining activity levels among young patients is difficult to determine from the current literature owing to the inclusion of heterogenous patients with respect to preoperative diagnosis [15, 17, 19, 23, 24] and nonuniform age definition of young patients. The majority of studies have accepted a chronologic age of 55 years [5, 7, 9, 10, 12, 13, 19, 27, 30, 32, 34, 35], but others have reported using other increments: 40 years [22, 24], 45 years [6], 50 years [16, 18, 24], and 60 years [14, 26]. Furthermore, activity level generally has not been compared between younger and older patient groups to validate the assumption that younger patients will be more active.
Therefore, we assessed the (1) demographic characteristics and (2) activity level profile (as determined by the UCLA score [1] and the functional subscores of The Knee Society [11] and WOMAC instruments [2] before and after TKAs in younger (≤ 55 years old) and older (65–75 years) patients treated at a large, urban, academic teaching hospital. The purposes of the study were to assess: (1) whether demographic features of younger patients who have had TKAs support high activity expectations after TKA, and (2) whether preoperative or postoperative functional activity measures support projections that these younger patients are active after surgery.
Patients and Methods
After obtaining institutional review board approval, we retrospectively assessed institutional joint repository data for all patients who had a TKA performed between January 2000 and December 2009 and had returned for followup at a minimum of 12 months after their TKA. Our review identified 150 patients 55 years or younger (181 TKAs) with a mean followup of 36 months (range, 12–118 months) and 262 patients between 65 to 75 years old (314 TKAs) with a mean followup of 31 months (range, 12–110 months). During the observation period, 324 TKAs were performed for 263 patients 55 years or younger and 615 TKAs were performed for 505 patients who were between 65 to 75 years old at the time of their surgery. Therefore, the study population represented 57% of younger patients and 52% of older patients who had a TKA during the study period. None of the included patients had undergone revision TKA. The surgeons at our institution independently indicate patients for arthroplasty, but general guidelines for surgery include the presence of advanced clinical symptoms including pain with or without stiffness, malalignment or mechanical symptoms, advanced radiographic disease, and failure of appropriate nonoperative treatment measures. Before 2010, patients were not excluded from surgical intervention based on BMI, hemoglobin A1C level, or other potentially modifiable parameters. Implant selection reflected surgeon preference and showed similar distributions between the younger patients (53% posterior stabilized, 30% cruciate retaining, 16% medial pivot, 1% constrained condylar) and the older patients (50% posterior stabilized, 32% cruciate retaining, 16% medial pivot, and 2% constrained condylar). Demographic information including age, sex, BMI, and surgical diagnosis was obtained from the data repository. Preoperative activity level was determined from patient self-assessment surveys that included the UCLA activity scale [1]. Functional measures were extracted from The Knee Society [11] and WOMAC [2] instruments. All preoperative assessments were obtained within 6 months before the TKA. Postoperative UCLA activity scores, Knee Society function subscores, and WOMAC physical function subscores were obtained at elective followups that occurred at a minimum of 12 months after surgery (range, 12–118 months). When multiple followups were identified for an individual patient, the latest available followup was selected. To create a categorical distribution of activity, the UCLA activity scale was subclassified into different levels: sedentary (1–2), mildly active (3–4), moderately active (5–7), and highly active (8–10). Patients in younger and older age groups were stratified based on sex to assess the relationship of gender on activity before or after surgery. Statistical analysis was accomplished using a two-tailed Student’s t-test for continuous variables and either the chi-square or Fisher’s exact test for categorical variables.
Results
Comparing Demographics Between Younger and Older Patients
The predominant indication for TKA among the younger patient group was osteoarthritis (79%) with inflammatory arthropathy (10.0%), osteonecrosis (7.7%), and posttraumatic arthritis (3.3%) contributing discrete minority groups. The indications for TKA among patients 65 to 75 years old included osteoarthritis (95%), followed by inflammatory arthropathy (3%) and posttraumatic arthritis (2%). Similar proportions of patients had either staged bilateral or simultaneous bilateral TKAs in the younger and older groups (17.1% versus 16.5%, p = 0.90). Women predominated both groups, but the percentage of female patients in the young patient group was significantly higher (74% versus 60%, p < 0.0001). The mean age of the patients at surgery was similar for male and female patients in the younger-age group (48.2 versus 49.3 years) and in the older-age group (70.2 versus 69.8 years.) Mean BMI was lower among men than women (31 versus 33 kg/m2, p < 0.001) and highest among women 55 years or younger (35 kg/m2, p < 0.001). Using WHO criteria for obesity [36], there were significantly more morbidly obese patients (BMI > 40 kg/m2) in the younger patient group compared with the older patient group (27% versus 9%, p < 0.001). Heavier patients were less active before surgery; among younger patients undergoing TKAs with a UCLA score greater than 5, the mean BMI was 31 kg/m2 (range, 18.8–50.7 kg/m2), whereas among patients with a UCLA activity score of 4 or less, the mean BMI was 35 kg/m2 (range, 15.0–76.3 kg/m2; p < 0.001). Among older patients with a UCLA score greater than 5, the mean BMI was 30.6 (range 21.6 – 44.9), whereas among patients with a UCLA activity score of 4 or less, the mean BMI was 31.5 (range 13.8–54.5, p = 0.22) (Table 1).
Table 1.
Preoperative demographics and functional level of the patients
| Patient subgroup | Followup (months) | Age (years) | BMI (kg/m2) | Preoperative UCLA score | Preoperative Knee Society function score | Preoperative WOMAC function score |
|---|---|---|---|---|---|---|
| All patients 65 to 75 years old | 30.8 | 69.9 | 31.5 | 3.8 | 48.3 | 53.8 |
| Males | 29.4 | 70.2 | 30.4 | 4.4 | 55.6 | 58.5 |
| Females | 31.8 | 69.8 | 31.8 | 3.6 | 43.3 | 50.8 |
| All patients 55 years or younger | 36.1 | 49.0 | 34.4 | 3.4 | 44.5 | 41.7 |
| Males | 33.3 | 48.3 | 31.4 | 4.0 | 54.0 | 47.5 |
| Females | 37.1 | 49.2 | 35.4 | 3.2 | 41.2 | 39.5 |
| All males | 30.5 | 62.3 | 31.1 | 4.1 | 55.2 | 55.0 |
| All females | 34.0 | 58.5 | 33.3 | 3.4 | 42.4 | 46.0 |
Comparing Activity Level and Function Between Younger and Older Patients
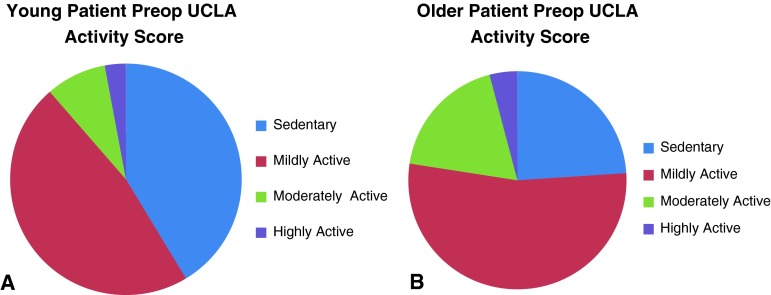
Before surgery, more patients 55 years or younger were either sedentary or mildly active compared with patients older than 65 years (87% versus 77%, p < 0.01). Only 13% of patients 55 years or younger reported being moderately or highly active before their TKA compared with 23% of patients who were 65 to 75 years old (p < 0.001) (Fig. 1) Although the majority of younger patients (57%) and older patients (65%) experienced an increase in UCLA activity level after TKA, a substantial percentage of patients in both groups (29% of younger and 23% of older patients undergoing TKA) did not increase activity level, and 14% of patients in both groups experienced a decline in activity in an average of 33 months after TKA. The majority of patients in the younger and older TKA groups remained either sedentary or mildly active (56% versus 52%, p = 0.35) with only 10% of patients 55 years old or younger and 12% of patients 65 to75 years old returning to regular recreational or competitive athletic activity (Fig. 2). Although mean values for all three functional activity measures increased after surgery for male and female patients in both age groups, absolute mean postoperative values for each functional measure were clinically and statistically higher for male patients: UCLA activity score (5.5 versus 4.4, p < 0.001), Knee Society function subscore (80.2 versus 66.4, p < 0.001), and WOMAC function subscore (82.8 versus 74.2, p < 0.01) (Table 2). When considering the combined effects of age and gender, the only clinical or statistically significant differences were the findings of higher functional activity subscores in older female versus younger female patients for The Knee Society (66 versus 60 points, p = 0.03) and WOMAC (79 versus 68 points, p < 0.001) function scores (Table 2).
Fig. 1A–B.
The categorical distributions of the preoperative UCLA activity scores are shown for (A) younger and (B) older patients undergoing TKAs.
Fig. 2A–B.
The categorical distributions of the postoperative UCLA activity scores are shown for (A) younger and (B) older patients undergoing TKAs.
Table 2.
Postoperative changes in mean activity and function scores
| Patient subgroup | Postoperative UCLA activity score | Change in UCLA activity score | Postoperative Knee Society function score | Change in Knee Society function score | Postoperative WOMAC function score | Change in WOMAC function score |
|---|---|---|---|---|---|---|
| All patients 65–75 years old | 4.9 | 1.1 | 71.6 | 23.3 | 80.7 | 26.9 |
| Males | 5.5 | 1.1 | 79.7 | 24.1 | 83.4 | 24.9 |
| Females | 4.5 | 0.9 | 66.0 | 22.7 | 78.8 | 28.0 |
| All patients 55 years and younger | 4.6 | 1.2 | 65.4 | 20.9 | 71.6 | 25.1 |
| Males | 5.7 | 1.7 | 81.4 | 27.4 | 81.3 | 23.8 |
| Females | 4.2 | 1.0 | 59.8 | 18.6 | 67.7 | 28.2 |
| All males | 5.5 | 1.4 | 80.2 | 26.2 | 82.8 | 27.8 |
| All females | 4.4 | 1.0 | 63.4 | 21.0 | 74.2 | 28.2 |
| p value (males versus females) | < 0.001 | 0.02 | < 0.001 | 0.03 | < 0.01 | 0.99 |
| p value (younger versus older) | 0.15 | 0.36 | < 0.01 | 0.21 | < 0.001 | 0.07 |
| p value (younger versus older females) | 0.18 | 0.37 | 0.02 | 0.12 | < 0.001 | 0.23 |
| p value (younger versus older males) | 0.46 | 0.34 | 0.63 | 0.92 | 0.50 | 0.15 |
Although the presence of diagnoses other than osteoarthritis were more prevalent in the younger patients and may contribute to longer-term differences in implant performance, there were no differences in activity level when compared with age- and gender-matched patients with osteoarthritis. Diagnoses of osteonecrosis and inflammatory arthritis contributed to lower preoperative UCLA activity scores when compared with a diagnosis of osteoarthritis (2.6 versus 3.3, p < 0.003), but postoperative UCLA activity levels were clinically and statistically equal (4.7 versus 4.8, p = 0.80), indicating greater postoperative improvement in activity level for patients with these diagnoses compared with other young patients with osteoarthritis undergoing TKAs.
Discussion
The use of TKA has increased substantially during the past two decades, particularly among younger patients [1, 3]. Considerations regarding patient optimization, implant selection, surgical technique, and perioperative management are uniquely relevant for this patient group because their longevity will likely exceed the durability of contemporary prosthetic implants. Several studies have identified increased rates of revision surgery in this younger patient group [1, 3, 5]. We therefore sought to compare the (1) demographics and (2) activity level profile (as determined by the UCLA score and the functional subscores of The Knee Society and WOMAC) before and after TKAs in younger (55 years or younger) and older (65 to 75 years) patients treated at a large, urban, academic teaching hospital.
There are several notable limitations of this study. We did not specifically address for concurrent musculoskeletal disease that may have affected activity levels in either group. Although we generally would anticipate a higher prevalence of systemic disease among older patients, we did not specifically address this consideration and this could influence study findings. While the proportion of patients with staged or simultaneous TKAs was similar in each group, we did not address the potential affect of differences in timing of bilateral procedures and whether this may have had any affect on functional activity measurements. Use of scores available at the latest followup potentially could reduce functional activity measures and create lower estimations of patient activity. However, these differences also would be expected to be most substantial among older patients, who were, on average, 21 years older than the younger patients at the time of surgery. The minimum followup also is shorter than ideal for assessing potential effects related to a minority of implants that might be failing. However, as the purpose of this study was attempting to address functional activity levels rather than implant survivorship, the 12 month minimum followup was accepted as an adequate time for functional activity to recover to a predisease or presurgical baseline. In a previous study [4], there were challenges reported in having adequate patient followup between the first and second postoperative years and followup in the current study reflects rates for clinical care among patients in our institution. Although the overall proportion of patients who returned for followup was similar in both groups, a relatively large number of patients had not returned at or beyond the 12-month postoperative followup, and this may result in exclusion of patients who were either more or less active than the study population.
Younger patients generally are perceived to have the potential for higher levels of activity after TKA. Our study findings suggest that the younger cohort generally is characterized by female sex, obesity, and low activity levels before and after TKA. Although inflammatory arthritis and osteonecrosis are minority diagnoses, they were six times more common in the younger patients than among older patients. While differences in postoperative activity were not specifically noted in our study, these patients likely represent a unique subpopulation that is less likely to sustain high activity levels with time. In addition, one in four younger patients in our study was morbidly obese, which is three times more common than the rate among older patients. Considering the demographic characteristics noted in our study, long-term failure from bearing surface wear and osteolysis may have a less significant affect for the majority of younger patients undergoing TKA. Assessment of the literature on TKA in a younger patient population is limited by the heterogeneity of patient indications in early studies that incorporated patients with osteoarthritis and inflammatory arthritis [6, 10, 12, 27, 33]. Studies have not substantially delineated demographic features of this patient group with age and diagnosis predominantly used as surrogates for activity level. Obesity may have a significant affect on the risk of revision surgery in the younger patient population including increased risks for infection [17, 23] and component malposition [26, 29] which could predispose some lower-activity patients to early failure.
Functional activity scores increased for all patients, regardless of age and gender. However, the younger group had a high proportion of patients who were substantially less active before surgery, and there were less than 10% of younger patients who attained a highly active status after TKA. The younger patient group was characterized by heavier patients who were less active before and after surgery, but male patients were significantly more active than female patients before and after TKA. Although the literature on younger patients undergoing TKAs has not stratified outcomes relative to activity level, two studies focused on very young patients with a greater potential for return to higher levels of activity. Lonner et al. [22] reported improved mean Knee Society clinical scores (47 to 88 points) but modestly improved mean functional scores (45 to 70 points) for 32 patients (32 TKAs) in this subpopulation. Mont et al. [24] reported substantially improved clinical and functional scores for 33 patients (38 TKAs), but additional procedures, especially closed manipulation for knee stiffness (24%), were commonly required in the treatment of these younger patients. Their implant survival rate was 97% although this was at a limited followup of less than 5 years [24].
A TKA is an effective procedure for improving pain and function. The durability of a TKA in younger patients may be affected by elevated activity levels or by other factors that may affect joint mechanics or biologic responses around prosthetic joint replacements. Although activity level and functional scores increase for the majority of patients, these increases are not substantially greater for younger patients than for older patients.
Enhancements in implant designs that are intended to allow greater durability under high activity levels may have an effect for as few as 10% to 15% of all patients undergoing TKAs. Sustained high activity levels are not likely to be a principal cause of revision TKAs among younger patients when considering age and diagnosis alone. Determining the effect of activity on survivorship of prosthetic designs and techniques should be based on measured patient function levels instead of using age as a surrogate for activity.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 3.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clohisy JC, Kamath GV, Byrd GD, Steger-May K, Wright RW. Patient compliance with clinical follow-up after total joint arthroplasty. J Bone Joint Surg Am. 2008;90:1848–1854. doi: 10.2106/JBJS.G.00856. [DOI] [PubMed] [Google Scholar]
- 5.Crowder AR, Duffy GP, Trousdale RT. Long-term results of total knee arthroplasty in young patients with rheumatoid arthritis. J Arthroplasty. 2005;20(7 suppl 3):12–16. doi: 10.1016/j.arth.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 6.Dalury DF, Ewald FC, Christie MJ, Scott RD. Total knee arthroplasty in a group of patients less than 45 years of age. J Arthroplasty. 1995;10:598–602. doi: 10.1016/S0883-5403(05)80202-5. [DOI] [PubMed] [Google Scholar]
- 7.Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriguez D. Total knee replacement in young, active patients: long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997;79:575–582. doi: 10.2106/00004623-199704000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Dowsey MM, Choong PF. Obesity is a major risk factor for prosthetic infection after primary hip arthroplasty. Clin Orthop Relat Res. 2008;466:153–158. doi: 10.1007/s11999-007-0016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duffy GP, Berry DJ, Rand JA. Cement versus cementless fixation in total knee arthroplasty. Clin Orthop Relat Res. 1998;356:66–72. doi: 10.1097/00003086-199811000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Duffy GP, Crowder AR, Trousdale RR, Berry DJ. Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty. 2007;22(6 suppl 2):67–70. doi: 10.1016/j.arth.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 12.Gill GS, Chan KC, Mills DM. 5- to 18-year follow-up study of cemented total knee arthroplasty for patients 55 years old or younger. J Arthroplasty. 1997;12:49–54. doi: 10.1016/S0883-5403(97)90046-2. [DOI] [PubMed] [Google Scholar]
- 13.Gioe TJ, Novak C, Sinner P, Ma W, Mehle S. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res. 2007;464:83–87. doi: 10.1097/BLO.0b013e31812f79a9. [DOI] [PubMed] [Google Scholar]
- 14.Harrysson OL, Robertsson O, Nayfeh JF. Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Relat Res. 2004;421:162–168. doi: 10.1097/01.blo.0000127115.05754.ce. [DOI] [PubMed] [Google Scholar]
- 15.Himanen AK, Belt E, Nevalainen J, Hamalainen M, Lehto MU. Survival of the AGC total knee arthroplasty is similar for arthrosis and rheumatoid arthritis: Finnish Arthroplasty Register report on 8,467 operations carried out between 1985 and 1999. Acta Orthop. 2005;76:85–88. doi: 10.1080/00016470510030373. [DOI] [PubMed] [Google Scholar]
- 16.Hungerford DS, Krackow KA, Kenna RV. Cementless total knee replacement in patients 50 years old and under. Orthop Clin North Am. 1989;20:131–145. [PubMed] [Google Scholar]
- 17.Jamsen E, Nevalainen P, Eskelinen A, Huotari K, Kalliovalkama J, Moilanen T. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012;94:e101 1–9. [DOI] [PubMed]
- 18.Hofmann AA, Heithoff SM, Camargo M. Cementless total knee arthroplasty in patients 50 years or younger. Clin Orthop Relat Res. 2002;404:102–107. doi: 10.1097/00003086-200211000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Keeney JA, Eunice S, Pashos G, Wright RW, Clohisy JC. What is the evidence for total knee arthroplasty in young patients?: a systematic review of the literature. Clin Orthop Relat Res. 2011;469:574–583. doi: 10.1007/s11999-010-1536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koh IJ, Cho WS, Choi NY, Kim TK; The Kleos Korea Research Group. Causes, risk factors, and trends in failures after TKA in Korea over the past 5 years: a multicenter study. Clin Orthop Relat Res. 2013 Aug 28. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 21.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lonner JH, Hershman S, Mont M, Lotke PA. Total knee arthroplasty in patients 40 years of age and younger with osteoarthritis. Clin Orthop Relat Res. 2000;380:85–90. doi: 10.1097/00003086-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Malinzak RA, Ritter MA, Berend ME, Meding JB, Olberding EM, Davis KE. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty. 2009;24:84–88. doi: 10.1016/j.arth.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 24.Mont MA, Sayeed SA, Osuji O, Johnson AJ, Naziri Q, Delanois RE, Bonutti PM. Total knee arthroplasty in patients 40 years and younger. J Knee Surg. 2012;25:65–69. doi: 10.1055/s-0031-1299667. [DOI] [PubMed] [Google Scholar]
- 25.Odland AN, Callaghan JJ, Liu SS, Wells CW. Wear and lysis is the problem in modular TKA in the young OA patient at 10 years. Clin Orthop Relat Res. 2011;469:41–47. doi: 10.1007/s11999-010-1429-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2003;85:1968–1973. doi: 10.2106/00004623-200310000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Ranawat CS, Padgett DE, Ohashi Y. Total knee arthroplasty for patients younger than 55 years. Clin Orthop Relat Res. 1989;248:27–33. [PubMed] [Google Scholar]
- 28.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85:259–265. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93:1588–1596. doi: 10.2106/JBJS.J.00772. [DOI] [PubMed] [Google Scholar]
- 30.Ritter MA, Lutgring JD, Davis KE, Faris PM, Berend ME. Total knee arthroplasty effectiveness in patients 55 years old and younger: osteoarthritis vs. rheumatoid arthritis. Knee. 2007;14:9–11. doi: 10.1016/j.knee.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 31.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper: Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Stern SH, Bowen MK, Insall JN, Scuderi GR. Cemented total knee arthroplasty for gonarthrosis in patients 55 years old or younger. Clin Orthop Relat Res. 1990;260:124–129. [PubMed] [Google Scholar]
- 33.Stuart MJ, Rand JA. Total knee arthroplasty in young adults who have rheumatoid arthritis. J Bone Joint Surg Am. 1988;70:84–87. [PubMed] [Google Scholar]
- 34.Tai CC, Cross MJ. Five- to 12-year follow-up of a hydroxyapatite-coated, cementless total knee replacement in young, active patients. J Bone Joint Surg Br. 2006;88:1158–1163. doi: 10.1302/0301-620X.88B9.17789. [DOI] [PubMed] [Google Scholar]
- 35.W-Dahl A, Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients. Acta Orthop. 2010;81:161–164. doi: 10.3109/17453670903413186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization, Division of Noncommunicable Diseases, World Health Organization, Programme of Nutrition, Family and Reproductive Health. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity. Geneva, Switzerland; 1998:29. Available at: http://apps.who.int/iris/handle/10665/63854. Accessed October 30, 2013.