Abstract
Background
The number of obese patients undergoing THA is increasing. Previous studies have shown that obesity is associated with an increased likelihood of complications after THA, but there is little information regarding the impact of obesity on medical resource use and direct medical costs in THA.
Questions/purposes
We sought to examine the relationship between obesity, length of stay, and direct medical costs in a large cohort of patients undergoing THAs.
Methods
The study included 8973 patients who had undergone 6410 primary and 2563 revision THAs at a large US medical center between January 1, 2000, and September 31, 2008. Patients with bilateral procedures within 90 days after index admission and patients with acute trauma were excluded. Data regarding clinical, surgical characteristics, and complications were obtained from the original medical records and the institutional joint registry. Patients were classified into eight groups based on their BMI at the time of surgery. Direct medical costs were calculated by using standardized, inflation-adjusted costs for services and procedures billed during hospitalization and the 90-day window. Study end points were hospital length of stay, direct medical costs during hospitalization, and the 90-day window. End points were compared across the eight BMI categories in multivariable risk-adjusted linear regression models.
Results
Mean length of stay and the direct medical costs were lowest for patients with a BMI of 25 to 35 kg/m2. Increasing BMI was associated with longer hospital stays and costs. Every five-unit increase in BMI beyond 30 kg/m2 was associated with approximately USD $500 higher hospital costs and USD $900 higher 90-day costs in primary THA (p = 0.0001), which corresponded to 5% higher costs. The cost increase associated with BMI was greater in the revision THA cohort where every five-unit increase in BMI beyond 30 kg/m2 was associated with approximately USD $800 higher hospital costs and USD $1500 higher 90-day costs. These estimates remained unchanged after adjusting for comorbidities or complications.
Conclusions
Obesity is associated with longer hospital stays and higher costs in THA. The significant effect of obesity on costs persists even among patients without comorbidities but the increased costs associated with obesity may be balanced by the potential benefits of THA in the obese. Increasing prevalence of obesity likely contributes to the increasing financial burden of THA worldwide.
Level of Evidence
Level IV, economic and decision analyses. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
The prevalence of obesity in the United States increased dramatically during the last few decades [13]. Apart from its health burden, obesity is associated with higher healthcare costs [3, 12, 30, 44, 45]. Compared with normal-weight individuals, obese patients incur 46% higher inpatient costs and 27% more physician visits and outpatient costs [12]. Obesity is also associated with greater likelihood of osteoarthritis thus requiring THA [2]. Indisputably, more obese patients are undergoing THA today than 10 to 20 years ago [11]. In terms of effectiveness, obese patients seem to benefit from THA as much as their nonobese counterparts despite a slower recovery and lower functional scores [1, 7, 18, 20, 25, 27, 28, 41, 43, 46], yet in terms of adverse outcomes, obese patients undergoing THA are at greater risk for various short-term complications such as infections and dislocations [16, 17, 22–25, 29, 31, 32, 36–38].
Some previous studies examined the impact of obesity on healthcare use and costs in THA with discrepant findings [4, 10, 14, 19, 21, 33, 39], attributable in part to methodologic differences in terms of sample size and power, definition of obesity, ascertainment and costing of use data, and adjustment for potential confounders such as comorbidities. Obesity is a risk factor for several costly comorbidities. Controlling for comorbidities therefore may result in underestimation of the true incremental cost of obesity because costs attributable to comorbidities theoretically can be considered attributable to obesity.
With this background, we performed the current study to examine the association of obesity with length of stay and with costs among patients undergoing THAs, after controlling for comorbidities.
Patients and Methods
The study included primary and revision THAs performed at the Mayo Clinic, Rochester, MN, USA, between January 1, 2000, and September 31, 2008. Patients who had denied research authorization for use of their medical records in research, patients who had undergone bilateral procedures or revisions during the same hospitalization or up to 90 days after index admission, and patients with acute trauma were excluded. We also limited the procedures to Major Diagnostic Category 8 musculoskeletal diseases, which included only orthopaedic surgery admissions. Apart from the abovementioned exclusions, all primary and revision THAs were analyzed. This study was approved by the Mayo Clinic institutional review board.
Numerous institutional data sources were used for data collection. Demographic and THA-related clinical data were obtained from the Mayo Clinic Total Joint Registry and the patients’ medical records. As described elsewhere [5], the Mayo Clinic Total Joint Registry contains detailed baseline and followup data for all patients who had undergone an arthroplasty at the Mayo Clinic, Rochester, MN, USA. Routinely collected data elements include clinical and prostheses details, indications, examination dates and findings, and details of the complete spectrum of complications. All patients were followed up by the surgeon (either through a visit at the Mayo Clinic or mail communication by local orthopaedists) at least twice during the first postsurgical year to ascertain subsequent complications and revision surgeries. Indications for primary THA were grouped into three categories as degenerative arthritis, inflammatory arthritis, and other (eg, congenital conditions, avascular necrosis, fracture). Indications for revision THAs were grouped into five categories as prosthesis loosening, wear, and/or osteolysis, dislocation, infection, periprosthetic fractures, and others. Complications were captured under five categories as infections (deep and/or superficial), vascular complications (eg, myocardial infarction, stroke, gastrointestinal bleeding, local arterial complications), thrombotic complications (eg, pulmonary embolism, deep vein thrombosis), dislocation and/or instability, and fracture of the bone or prosthesis components. Serial height, weight, and BMI measurements were extracted from the electronic medical records. We recorded all weight and height measurements and calculated BMI (weight/height in kg/m2) for each surgical encounter. BMI at the time of index surgery was the primary exposure variable. We used the Elixhauser comorbidity algorithm to capture comorbidities using administrative data [9]. The Elixhauser algorithm is a commonly used risk adjustment instrument that relies on ICD-9 codes to identify 30 individual comorbidities.
We obtained healthcare use and cost data from an institutional research database [26] that contained line item details for every procedure or service billed to patients of the Mayo Clinic undergoing THA. Bottom-up microcosting valuation techniques were used to generate standardized inflation-adjusted estimates of the costs in constant dollars. Part A items, which consisted primarily of hospital-billed services and procedures, were valued by multiplying the billed charge for each item by the cost center-specific cost-to-charge ratio for the year in which the service was delivered. Cost-to-charge ratios for each cost center in each hospital were obtained from published Medicare cost reports. Part B services and procedures, which consisted primarily of services billed by physicians, were valued using national average Medicare reimbursement rates. The costing algorithm applied the gross domestic product price deflator (ie, an economic metric to account for inflation) for Part A and Part B services to express the costs for each year in 2010 US dollars.
The time window for costs was defined in two ways: index hospitalization period (ie, beginning 1 day before the index surgery to the day of discharge) and the 90-day period (ie, 90 days beginning 1 day before the index surgery). We used Berenson-Eggers Type of Service [6] codes to classify the line item data, which then were summed by type of service during the index hospitalization and the total 90-day period. We further grouped costs into clinically relevant categories such as room and board, operating room, and prostheses costs.
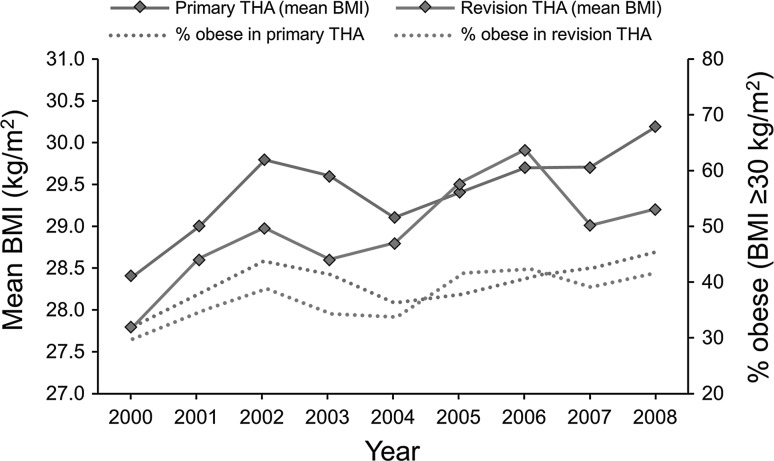
The study included 8973 patients who had undergone 6410 primary and 2563 revision THAs between January 1, 2000, and September 31, 2008. Overall, the mean age of the patients at the time of surgery was 64.5 years for those having primary THAs and 67.0 years for patients for patients having revision THAs. More than ½ the patients were female (Table 1). Mean BMI was 0.4 kg/m2 greater in patients with primary THAs than in patients with revision THAs. Mean BMI increased between 2000 and 2008 (Fig. 1). The size of the increase in mean BMI was 1.8 kg/m2 in the primary THA cohort and 1.4 kg/m2 in the revision THA cohort. The proportion of obese (BMI ≥ 30 kg/m2) patients in the primary THA cohort increased from 33% in 2000 to 46% in 2008. Similarly, the proportion of obese patients in the revision THA cohort increased from 30% in 2000 to 42% in 2008. The proportion of underweight patients was approximately 1.5% and remained relatively stable during the years.
Table 1.
Characteristics of patients in both cohorts
| Characteristic | Primary THA N = 6410 |
Revision THA N = 2563 |
|---|---|---|
| Age, years mean (SD) | 64.5 (14.6) | 67.0 (13.6) |
| Number (%) female | 3269 (51%) | 1358 (53%) |
| BMI mean (SD) | 29.4 (6.2) | 28.9 (6.0) |
| Median (25th and 75th quartiles) | 28.5 (25.3, 32.6) | 28.1 (24.8, 32.0) |
| BMI (kg/m2) categories*, N < 18.5 | 82 (1.3%) | 38 (1.5%) |
| 18.5–< 25 | 1400 (21.8%) | 644 (25.1%) |
| 25–< 30 | 2357 (36.8%) | 936 (36.5%) |
| 30–< 35 | 1542 (24.1%) | 599 (23.4%) |
| 35–< 40 | 622 (9.7%) | 214 (8.3%) |
| 40–< 45 | 262 (4.1%) | 82 (3.2%) |
| 45–< 50 | 77 (1.2%) | 29 (1.1%) |
| ≥ 50 | 49 (0.8%) | 16 (0.6%) |
| Length of stay, days | ||
| Mean (SD) | 4.6 (2.3) | 5.4 (2.9) |
| Median (25th & 75th quartile) | 4 (4, 5) | 5 (4, 6) |
| Percentage of patients with comorbidities | 68% | 71% |
| Number of comorbidities per patient, mean (SD)† | 1.20 (1.17) | 1.32 (1.23) |
| Number (%) of patients who experienced at least one complication | 648 (10%) | 507 (20%) |
* BMI unknown in 19 patients with primary THAs and five with revision THAs; †excluding obesity.
Fig. 1.
The trends in mean BMI and percentage of obese patients (BMI ≥ 30 kg/m2) undergoing THAs between 2000 and 2008 are shown.
Mean and median length of stay was 1 day longer for patients who had revision THAs (5.4 days versus 4.6 days; Table 1).
Statistical Methods
Patients were grouped under eight BMI categories based on their BMI at the time of the index THA hospitalization. Length of stay, costs, comorbidities, and complications were expressed as means with SDs, medians with interquartile ranges, and percentages. The study end points were hospital length of stay and direct medical costs during hospitalization and the 90-day window. Direct medical costs and categories of costs were calculated separately for the hospitalization period and 90-day period (ie, total costs). End points were compared across the eight BMI categories in unadjusted and multivariable risk-adjusted analyses. Linear regression models were used to determine the cost impact associated with increasing BMI categories and obesity. Numerous BMI cutoff values were examined (≥ 25 kg/m2, ≥ 30 kg/m2, ≥ 35 kg/m2) to determine the best fit for BMI data and other adjustment variables. Analyses were conducted for the (1) overall study population; (2) patients 25 years or older undergoing primary THA with degenerative arthritis and no recorded malignancies; and (3) patients 25 years or older undergoing revision THA with no recorded malignancies, and (4) restricting the analytical sample to patients without the selected comorbidities previously shown to be significantly associated with costs in this population. These comorbid conditions were congestive heart failure, valvular diseases, pulmonary circulation diseases (eg, pulmonary hypertension), paralysis, chronic pulmonary diseases (eg, asthma), diabetes with or without complications, renal failure, metastatic cancer, solid tumors without metastasis, coagulopathy, fluid and electrolyte disorders, liver disease, lymphoma, and alcohol or drug abuse. This exclusion also resulted in exclusion of 51% of patients having primary THAs and 30% having revision THAs. All statistical analyses were performed using SAS Version 9.3 (SAS Institute, Cary, NC, USA).
Results
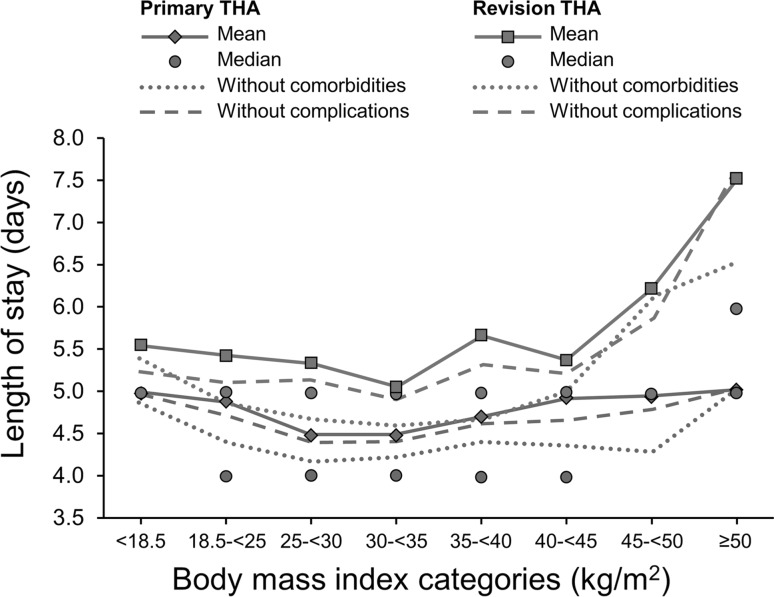
Relationship Between Obesity and Length of Stay
Mean length of stay was lowest for patients with a BMI 25 to 35 kg/m2 (Fig. 2). We observed a J-shaped relationship where the hospital stays were longer for patients at extreme ends of the BMI spectrum. In age- and sex-adjusted models, each five-unit increase in BMI greater than 30 kg/m2 was associated with an average of 0.16 more days in the hospital for patients having primary procedures and 0.27 days for patients having revision procedures (p = 0.0001 for both). This pattern persisted after excluding patients with selected cost-associated comorbidities and with complications.
Fig. 2.
The mean (median) lengths of stay by BMI categories among patients undergoing THA are shown.
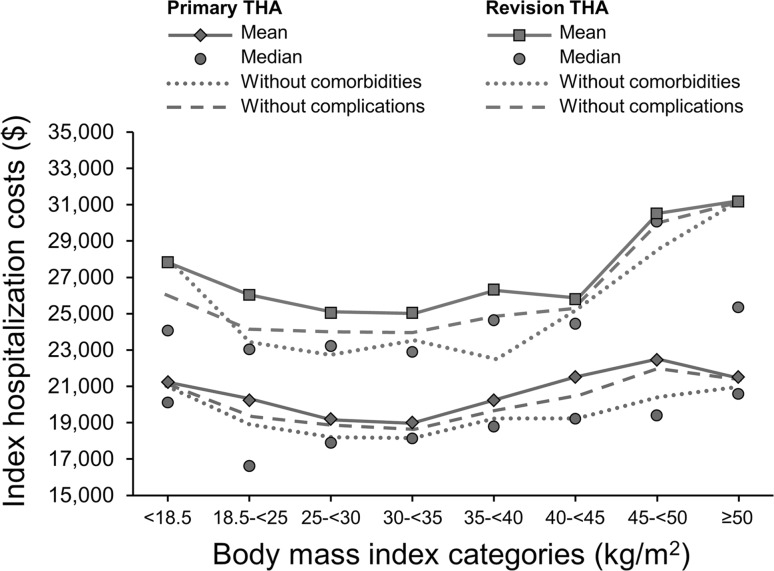
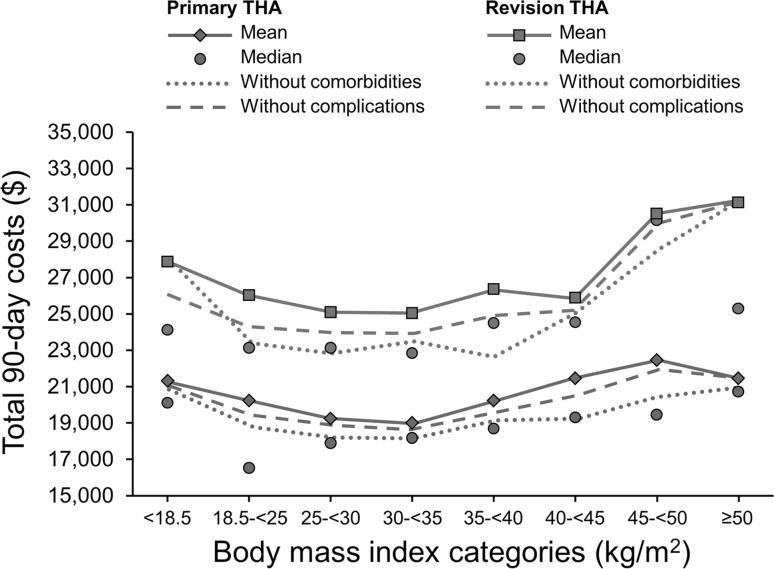
Relationship Between Obesity and Costs
Hospitalization costs (Fig. 3) and total 90-day costs (Fig. 4) followed a pattern similar to the length of stay. In the primary and revision cohorts, hospitalization costs and total 90-day costs were lowest for patients with BMI 25 to 35 kg/m2. Increasing BMI was associated with higher costs and this association persisted among patients without significant comorbidities or complications. When we examined the various cost components, the association between BMI and costs was significant for room and board costs and operating room costs.
Fig. 3.
The mean (median) hospitalization costs by BMI categories among patients undergoing THA are shown in 2010 US dollars.
Fig. 4.
The mean (median) 90-day costs by BMI categories among patients undergoing THAs are shown in 2010 US dollars.
After adjusting for age, sex, surgery type (primary versus revision), and surgical indications, every five-unit increase in BMI beyond 30 kg/m2 was associated with USD $744 and $1183 higher hospitalization and 90-day costs, respectively (Table 2). These dollar amounts corresponded to approximately 5% higher hospitalization and 90-day costs.
Table 2.
Costs associated with obesity (estimates derived from multivariate linear regression models)
| Analytical sample | Cost per five-unit increase in BMI greater than 30 kg/m2 | |||
|---|---|---|---|---|
| Hospitalization costs (USD) | 95% CI | Total 90-day costs (USD) | 95% CI | |
| All patients undergoing primary and revision THA | ||||
| Adjusted for age, sex, surgery type, surgical indication | $744 | $499–$989 | $1183 | $851–$1516 |
| Adjusted for age, sex, surgery type, surgical indication, comorbidities | $600 | $360–$841 | $1019 | $692–$1347 |
| Excluding patients with significant comorbidities* and adjusted for age, sex, surgery type, surgical indication | $657 | $381–$932 | $1053 | $747–$1359 |
| Excluding patients with complications, adjusted for age, sex, surgery type, surgical indication, comorbidities | $606 | $404–$807 | $953 | $682–$1224 |
| Patients undergoing primary THA † | ||||
| Adjusted for age, sex | $620 | $439–$801 | $906 | $628–$1184 |
| Adjusted for age, sex, comorbidities | $495 | $319–$670 | $845 | $575–$1115 |
| Excluding patients with significant comorbidities# and adjusted for age, sex | $550 | $353–$746 | $954 | $622–$1285 |
| Patients undergoing revision THA ‡ | ||||
| Adjusted for age, sex, surgical indication | $895 | $290–$1499 | $1547 | $744–$2350 |
| Adjusted for age, sex, surgical indication, comorbidities | $609 | $19–$1199 | $1170 | $383–$1957 |
| Excluding patients with significant comorbidities* and adjusted for age, sex, surgical indication | $892 | $421–$1362 | $1367 | $639–$1294 |
* Patients with selected comorbidities that are significantly associated with costs are excluded; †patients older than 25 years undergoing primary THA with degenerative arthritis and no recorded malignancies or metastases; ‡patients older than 25 years undergoing revision THA and no recorded malignancies or metastases.
This association persisted even after adjusting for comorbidities (USD $600 and $1019 hospitalization and 90-day costs, respectively), in the subset of patients without significant comorbidities ((USD $657 and $1053 hospitalization and 90-day costs, respectively), and after excluding patients with complications (USD $606 and $953 hospitalization and 90-day costs, respectively). In the primary THA cohort, the cost increase associated with five-unit increase in BMI beyond 30 kg/m2 was approximately USD $500 to $600 in hospital costs and USD $800 to $900 in 90-day costs. In the revision THA cohort, the cost increase was approximately USD $600 to $900 higher hospital costs and USD $1200 to $1500 higher 90-day costs. We also adjusted the models for length of stay (a significant predictor of costs) and the association between BMI and costs persisted. The association between BMI and costs was robust regardless of the analytical sample or adjustment for comorbidities (Table 2).
Discussion
Despite the increasing prevalence of obesity among patients undergoing THA, there are few studies examining the potential financial implications of obesity in this patient population [4, 10, 14, 19, 21, 33]. We therefore examined the association between BMI and length of stay and costs taking into account obesity-related comorbidities and short-term THA complications. We found that length of stay and costs are lowest for individuals with normal BMI or slightly overweight individuals and highest for patients at extreme ends of the BMI spectrum where every five-unit increase in BMI beyond 30 kg/m2 was associated with approximately USD $500 and $800 higher hospital costs in primary and revision THAs, respectively.
This study had some limitations. First, the time of our study is limited to the 3 months around the time of THA, and therefore, the long-term cost implications of obesity after THA are not addressed. Second, there is considerable geographic variation [40, 42] in the practice of THA and our findings may not be generalizable to THAs in other institutions or countries. Nevertheless, our study has high internal validity because all exposure and outcome data are collected uniformly for all patients and comparisons are made across BMI categories. Third, we relied on administrative data to identify comorbidities, which probably resulted in underestimation of some common comorbidities not adequately captured in administrative data. Fourth, the number of patients in the lowest BMI category was too few to draw any robust conclusions regarding the shape of the BMI-cost relationship in patients with low BMI. Finally, although we compared costs during a 3-month window, we did not separately assess the cost of postdischarge readmissions, which may be substantial [35].
Based on the findings of various large-scale studies with various indications [15, 34, 47], it is plausible to presume that obese patients undergoing THA would have longer hospital stays and higher hospital costs through increased prevalence of chronic comorbidities and complications and longer recovery. For example, a large-scale study [15] included 35,000 orthopaedic surgeries and the length of stay was 1.1 days longer for morbidly obese patients, but it has been difficult to show this association in previous THA studies [4, 10, 14, 19, 21, 33]. We believe this is a result of methodologic issues, including small sample sizes, power, measurement of obesity, and cost outcomes. Our study overcomes some of these methodologic issues. For example, three older studies included small THA cohorts, however, they raised awareness of the issue [10, 19, 33]. In contrast to a previous analysis from our institution [4], we examined BMI as a continuous variable and in eight categories, which avoided loss of information and loss of power. In addition, we identified and adjusted for comorbidities using the Elixhauser algorithm, which is more strongly associated with healthcare use and costs than the Charlson classification [8]. Two studies [14, 21] relied on administrative data from the Nationwide Inpatient Sample to address the impact of obesity on some THA outcomes, including costs. The difficulty with administrative data is underreporting of obesity, especially in the absence of incentives to do so. Comorbidities were not considered in one study, which reported USD $1500 greater charges for morbidly obese patients undergoing THA than nonobese patients [21]. The primary focus of another analysis was metabolic syndrome and the authors reported that, adjusting for hospital characteristics and comorbidities, the presence of metabolic syndrome (with obesity as one component) was associated with higher costs despite a shorter hospital stay [14]. As compared with administrative records of obesity, actual weight and BMI measures can significantly improve prediction of in-hospital complications [29]. One study [39] examining the financial impact of obesity in various surgical indications included approximately 500 patients undergoing THAs and reported that Medicare payments were 3% higher for the obese than the nonobese patients but the provider costs were 10% higher, suggesting that the increased costs associated with obesity were not accompanied by similar increases in payments. We recently conducted similar analyses in TKAs (unpublished data) and the excess costs associated with obesity seemed to be greater among patients undergoing THAs than the patients undergoing TKAs. The reasons for this are unknown but may include longer operative times owing to the more challenging anatomic condition in obese individuals undergoing THA rather than TKA. In our study, we observed a J-shaped relationship in which the length of stay and costs were lowest for patients with normal BMI or slightly overweight individuals and highest for patients at extreme ends of the BMI spectrum. Beyond 30 kg/m2, every five-unit increase in BMI was associated with approximately USD $500 higher hospital costs in primary THA and $800 higher hospital costs in revision THA. These estimates persisted in analyses that took into account obesity-related comorbidities and short-term complications, indicating that obesity has a significant impact on THA costs regardless of comorbidities and likely contributes to the growing financial burden of THA. Nevertheless, we believe that the increased costs associated with obesity may be balanced by the potential benefits of THA in obese patients.
An important finding of our study is the 12-percentage point increase in the proportion of obese patients undergoing THAs during the 8 years from 2000 to 2008. This is consistent with a previous report [11]. Fehring et al. [11] reported a 15% increase in proportion of obese patients between 1990 and 2005, reaching 40% prevalence by 2005. This is identical to our estimates. The obesity prevalence was lower in another study [14], but obesity was defined using administrative codes, which is an underestimate as a result of underreporting. For example, in our cohort, only 5% were identified as obese based on administrative codes. Together, these findings underscore the high prevalence of obesity among patients undergoing THA and the need to address the financial impact of obesity in THA, especially in an environment where cost containment is increasingly important.
We found that obesity is associated with longer hospital stays and costs in THA, even among patients without comorbid conditions or complications. The strengths of our study include the inclusion of a large, contemporary THA cohort, linkage of medical record-derived clinical data with administrative data, and the robust costing methodology. In light of this, we believe that costs are a reason to encourage weight loss in obese candidates for THA. The increasing prevalence of obesity in the THA population represents a challenge and likely contributes to the financial burden associated with THA.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Andrew JG, Palan J, Kurup HV, Gibson P, Murray DW, Beard DJ. Obesity in total hip replacement. J Bone Joint Surg Br. 2008;90:424–429. doi: 10.1302/0301-620X.90B4.20522. [DOI] [PubMed] [Google Scholar]
- 2.Apold H, Meyer HE, Espehaug B, Nordsletten L, Havelin LI, Flugsrud GB. Weight gain and the risk of total hip replacement: a population-based prospective cohort study of 265,725 individuals. Osteoarthritis Cartilage. 2011;19:809–815. doi: 10.1016/j.joca.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Arterburn DE, Maciejewski ML, Tsevat J. Impact of morbid obesity on medical expenditures in adults. Int J Obesity. 2005;29:334–339. doi: 10.1038/sj.ijo.0802896. [DOI] [PubMed] [Google Scholar]
- 4.Batsis JA, Naessens JM, Keegan MT, Wagie AE, Huddleston PM, Huddleston JM. Impact of body mass on hospital resource use in total hip arthroplasty. Public Health Nutr. 2009;12:1122–1132. doi: 10.1017/S1368980009005072. [DOI] [PubMed] [Google Scholar]
- 5.Berry DJ, Kessler M, Morrey BF. Maintaining a hip registry for 25 years: Mayo Clinic experience. Clin Orthop Relat Res. 1997;344:61–68. doi: 10.1097/00003086-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. Berenson-Eggers Type of Service (BETOS) codes. 2011. Available at: https://www.cms.gov/HCPCSReleaseCodeSets/20_BETOS.asp. Accessed September 16, 2013.
- 7.Davis AM, Wood AM, Keenan ACM, Brenkel IJ, Ballantyne JA. Does body mass index affect clinical outcome post-operatively and at five years after primary unilateral total hip replacement performed for osteoarthritis? A multivariate analysis of prospective data. J Bone Joint Surg Br. 2011;93:1178–1182. doi: 10.1302/0301-620X.93B9.26873. [DOI] [PubMed] [Google Scholar]
- 8.Dominick KL, Dudley TK, Coffman CJ, Bosworth HB. Comparison of three comorbidity measures for predicting health service use in patients with osteoarthritis. Arthritis Rheum. 2005;53:666–672. doi: 10.1002/art.21440. [DOI] [PubMed] [Google Scholar]
- 9.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Epstein AM, Read JL, Hoefer M. The relation of body-weight to length of stay and charges for hospital services for patients undergoing elective surgery: a study of two procedures. Am J Public Health. 1987;77:993–997. doi: 10.2105/AJPH.77.8.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fehring TK, Odum SM, Griffin WL, Mason JB, McCoy TH. The obesity epidemic: its effect on total joint arthroplasty. J Arthroplasty. 2007;22(6 suppl 2):71–76. doi: 10.1016/j.arth.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 13.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez Della Valle A, Chiu YL, Ma Y, Mazumdar M, Memtsoudis SG. The metabolic syndrome in patients undergoing knee and hip arthroplasty: trends and in-hospital outcomes in the United States. J Arthroplasty. 2012;27:1743–1749.e1. [DOI] [PubMed]
- 15.Hauck K, Hollingsworth B. The impact of severe obesity on hospital length of stay. Med Care. 2010;48:335–340. doi: 10.1097/MLR.0b013e3181ca3d85. [DOI] [PubMed] [Google Scholar]
- 16.Haverkamp D, Klinkenbijl MN, Somford MP, Albers GH, van der Vis HM. Obesity in total hip arthroplasty: does it really matter? A meta-analysis. Acta Orthop. 2011;82:417–422. doi: 10.3109/17453674.2011.588859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012;470:490–496. doi: 10.1007/s11999-011-1967-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson MP, Sexton SA, Yeung E, Walter WL, Walter WK, Zicat BA. The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J Bone Joint Surg Br. 2009;91:1296–1300. doi: 10.1302/0301-620X.91B10.22544. [DOI] [PubMed] [Google Scholar]
- 19.Jibodh SR, Gurkan I, Wenz JF. In-hospital outcome and resource use in hip arthroplasty: influence of body mass. Orthopedics. 2004;27:594–601. doi: 10.3928/0147-7447-20040601-16. [DOI] [PubMed] [Google Scholar]
- 20.Jones CA, Cox V, Jhangri GS, Suarez-Almazor ME. Delineating the impact of obesity and its relationship on recovery after total joint arthroplasties. Osteoarthritis Cartilage. 2012;20:511–518. doi: 10.1016/j.joca.2012.02.637. [DOI] [PubMed] [Google Scholar]
- 21.Kim SH. Morbid obesity and excessive hospital resource consumption for unilateral primary hip and knee arthroplasty. J Arthroplasty. 2010;25:1258–1266. doi: 10.1016/j.arth.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Kim Y, Morshed S, Joseph T, Bozic K, Ries MD. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin Orthop Relat Res. 2006;453:142–146. doi: 10.1097/01.blo.0000238874.09390.a1. [DOI] [PubMed] [Google Scholar]
- 23.Lowe GD, Haverkate F, Thompson SG, Turner RM, Bertina RM, Turpie AG, Mannucci PM. Prediction of deep vein thrombosis after elective hip replacement surgery by preoperative clinical and haemostatic variables: the ECAT DVT Study. European Concerted Action on Thrombosis. Thromb Haemost. 1999;81:879–886. [PubMed] [Google Scholar]
- 24.Lubbeke A, Moons KG, Garavaglia G, Hoffmeyer P. Outcomes of obese and nonobese patients undergoing revision total hip arthroplasty. Arthritis Rheum. 2008;59:738–745. doi: 10.1002/art.23562. [DOI] [PubMed] [Google Scholar]
- 25.Lubbeke A, Stern R, Garavaglia G, Zurcher L, Hoffmeyer P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007;57:327–334. doi: 10.1002/art.22542. [DOI] [PubMed] [Google Scholar]
- 26.Maradit Kremers H, Visscher SL, Moriarty JP, Reinalda MS, Kremers WK, Naessens JM, Lewallen DG. Determinants of direct medical costs in primary and revision total knee arthroplasty. Clin Orthop Relat Res. 2013;471:206–214. doi: 10.1007/s11999-012-2508-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCalden RW, Charron KD, MacDonald SJ, Bourne RB, Naudie DD. Does morbid obesity affect the outcome of total hip replacement?: an analysis of 3290 THRs. J Bone Joint Surg Br. 2011;93:321–325. doi: 10.1302/0301-620X.93B3.25876. [DOI] [PubMed] [Google Scholar]
- 28.McLaughlin JR, Lee KR. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Joint Surg Br. 2006;88:1286–1292. doi: 10.1302/0301-620X.88B10.17660. [DOI] [PubMed] [Google Scholar]
- 29.Mnatzaganian G, Ryan P, Norman PE, Davidson DC, Hiller JE. Use of routine hospital morbidity data together with weight and height of patients to predict in-hospital complications following total joint replacement. BMC Health Serv Res. 2012;12:380. doi: 10.1186/1472-6963-12-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moriarty JP, Branda ME, Olsen KD, Shah ND, Borah BJ, Wagie AE, Egginton JS, Naessens JM. The effects of incremental costs of smoking and obesity on health care costs among adults: a 7-year longitudinal study. J Occup Environ Med. 2012;54:286–291. doi: 10.1097/JOM.0b013e318246f1f4. [DOI] [PubMed] [Google Scholar]
- 31.Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20(7 suppl 3):46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 32.Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89:33–38. doi: 10.2106/JBJS.F.00163. [DOI] [PubMed] [Google Scholar]
- 33.Perka C, Labs K, Muschik M, Buttgereit F. The influence of obesity on perioperative morbidity and mortality in revision total hip arthroplasty. Arch Orthop Trauma Surg. 2000;120:267–271. doi: 10.1007/s004020050462. [DOI] [PubMed] [Google Scholar]
- 34.Quesenberry CP, Jr, Caan B, Jacobson A. Obesity, health services use, and health care costs among members of a health maintenance organization. Arch Intern Med. 1998;158:466–472. doi: 10.1001/archinte.158.5.466. [DOI] [PubMed] [Google Scholar]
- 35.Reinke CE, Kelz RR, Zubizarreta JR, Mi L, Saynisch P, Kyle FA, Even-Shoshan O, Fleisher LA, Silber JH. Obesity and readmission in elderly surgical patients. Surgery. 2012;152:355–362. doi: 10.1016/j.surg.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roder C, Bach B, Berry DJ, Eggli S, Langenhahn R, Busato A. Obesity, age, sex, diagnosis, and fixation mode differently affect early cup failure in total hip arthroplasty: a matched case-control study of 4420 patients. J Bone Joint Surg Am. 2010;92:1954–1963. doi: 10.2106/JBJS.F.01184. [DOI] [PubMed] [Google Scholar]
- 37.Sadr Azodi O, Adami J, Lindstrom D, Eriksson KO, Wladis A, Bellocco R. High body mass index is associated with increased risk of implant dislocation following primary total hip replacement: 2,106 patients followed for up to 8 years. Acta Orthop. 2008;79:141–147. doi: 10.1080/17453670710014897. [DOI] [PubMed] [Google Scholar]
- 38.Sadr Azodi O, Bellocco R, Eriksson K, Adami J. The impact of tobacco use and body mass index on the length of stay in hospital and the risk of post-operative complications among patients undergoing total hip replacement. J Bone Joint Surg Br. 2006;88:1316–1320. doi: 10.1302/0301-620X.88B10.17957. [DOI] [PubMed] [Google Scholar]
- 39.Silber JH, Rosenbaum PR, Kelz RR, Reinke CE, Neuman MD, Ross RN, Even-Shoshan O, David G, Saynisch PA, Kyle FA, Bratzler DW, Fleisher LA. Medical and financial risks associated with surgery in the elderly obese. Ann Surg. 2012;256:79–86. doi: 10.1097/SLA.0b013e31825375ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stargardt T. Health service costs in Europe: cost and reimbursement of primary hip replacement in nine countries. Health Econ. 2008;17(1 suppl):S9–S20. doi: 10.1002/hec.1328. [DOI] [PubMed] [Google Scholar]
- 41.Stevens M, Paans N, Wagenmakers R, van Beveren J, van Raay J, van der Meer K, Stewart R, Bulstra SK, Reininga IH, van den Akker-Scheek I. The influence of overweight/obesity on patient-perceived physical functioning and health-related quality of life after primary total hip arthroplasty. Obes Surg. 2012;22:523–529. doi: 10.1007/s11695-011-0483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tomek IM, Sabel AL, Froimson MI, Muschler G, Jevsevar DS, Koenig KM, Lewallen DG, Naessens JM, Savitz LA, Westrich JL, Weeks WB, Weinstein JN. A collaborative of leading health systems finds wide variations in total knee replacement delivery and takes steps to improve value. Health Aff (Millwood). 2012;31:1329–1338. doi: 10.1377/hlthaff.2011.0935. [DOI] [PubMed] [Google Scholar]
- 43.Vincent HK, Horodyski M, Gearen P, Vlasak R, Seay AN, Conrad BP, Vincent KR. Obesity and long term functional outcomes following elective total hip replacement. J Orthop Surg Res. 2012;7:16. doi: 10.1186/1749-799X-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Obesity and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 45.Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12:131–141. doi: 10.1111/j.1467-789X.2009.00712.x. [DOI] [PubMed] [Google Scholar]
- 46.Yeung E, Jackson M, Sexton S, Walter W, Zicat B, Walter W. The effect of obesity on the outcome of hip and knee arthroplasty. Int Orthop. 2011;35:929–934. doi: 10.1007/s00264-010-1051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zizza C, Herring AH, Stevens J, Popkin BM. Length of hospital stays among obese individuals. Am J Public Health. 2004;94:1587–1591. doi: 10.2105/AJPH.94.9.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]