Abstract
Purpose
Although arthroplasty is an accepted option for two-level disease, there is a paucity of data regarding outcomes of two-level cervical arthroplasty. The current study was designed to determine differences between two-level cervical arthroplasty and anterior fusion.
Methods
Seventy-seven consecutive patients who underwent two-level anterior cervical operations for degenerative disc disease were divided into the arthroplasty (37 patients) and fusion (40 patients) groups. Clinical outcomes were measured by Visual Analogue Scale (VAS) of neck and arm pain, Japanese Orthopedic Association (JOA) scores, and Neck Disability Index (NDI). Every patient was evaluated by radiography and computed tomography for fusion or detection of heterotopic ossification.
Results
Thirty-seven patients (with 74 levels of Bryan discs) were compared with 40 patients who had two-level anterior fusion (mean follow-up of 39.6 ± 6.7 months). There was no difference in sex, but the mean age of the arthroplasty group was significantly younger (52.1 ± 9.1 vs. 63.0 ± 10.6 years, p < 0.001). The mean estimated blood loss was similar (p = 0.135), but the mean operation time was longer in the arthroplasty group (315.5 ± 82.0 versus 224.9 ± 61.8 min, p < 0.001). At 24 months post-operation, the arthroplasty group had increased their range of motion than pre-operation (23.5° versus 20.1°, p = 0.018). There were significant improvements in neck or arm VAS, JOA scores, and NDI in both groups. However, there were no differences in clinical outcomes or adverse events between the two groups.
Conclusions
Clinical outcomes of two-level arthroplasty and anterior cervical fusion are similar 39.6 months after surgery. Cervical arthroplasty preserves mobility at the index levels without increased adverse effects.
Keywords: Bryan disc, Cervical arthroplasty, Degenerative disc disease (DDD), Heterotopic ossification, Anterior cervical discectomy and fusion (ACDF)
Introduction
Anterior cervical discectomy and fusion (ACDF) has been the most widely accepted surgical management of degenerative disc disease (DDD) of the cervical spine [1–3]. In the past few years, the introduction of cervical arthroplasty as a treatment option has diversified the paradigm of clinical management. Arthroplastic devices have been tested for their clinical applications and have gradually gained popularity [4–9]. For one-level cervical DDD or spondylosis, several of these artificial discs have undergone large-scale, prospective, randomized, and controlled trials by the United States Food and Drug Administration Investigational Device Exemption (FDA-IDE) for comparison with ACDF [10–14]. Reports with mean follow-ups of 2–5 years have demonstrated that cervical arthroplasty is a safe and effective alternative to ACDF for one-level cervical spondylosis or DDD [10–14].
The FDA trials have also demonstrated that one-level ACDF limits approximately seven degrees in the range of motion (ROM), which can be successfully preserved by arthroplasty [10, 12–14, 16, 17]. This loss of seven degrees in ROM does not significantly affect daily activities and is seldom noticed by the patient. However, two-level ACDF inevitably limits more neck ROM and may cause noticeable hindrances to neck mobility. Thus, it is reasonable to infer that two-level arthroplasty is more advantageous than two-level ACDF in preserving neck motion [15]. Unfortunately, the aforementioned FDA-IDE trials only compared results of cervical arthroplasty to ACDF in one-level diseases. Although two-level cervical spondylosis is also commonly encountered [18], there are very few reports in the literature regarding differences between two-level cervical arthroplasty and two-level anterior cervical fusion.
The present study aimed to investigate the differences between two-level cervical arthroplasty and anterior cervical fusion. This is the first study to specifically address two-level cervical DDD treated by arthroplasty and anterior fusion.
Methods
Inclusion and exclusion criteria
Consecutive patients with two-level cervical DDD who underwent cervical arthroplasty or anterior cervical fusion between October 2006 and March 2009 in a single medical center were retrospectively reviewed. The inclusion criteria were radiculopathy and/or myelopathy caused by one- or two-level cervical DDD refractory to medical treatment for at least 8 weeks treated by cervical arthroplasty, ACDF, or anterior cervical corpectomy and fusion (ACCF), with a mean follow-up of more than 2 years. The exclusion criteria were osteoporosis, malignancy, metabolic bone disease, infection, severe systemic diseases, and patients who had a mean follow-up of less than 2 years or those lost to follow-up.
Choices of arthroplasty or fusion were based on the patients’ and surgeons’ preferences, economic considerations, segmental ossification of the posterior longitudinal ligament (OPLL), incompetent facets, or loss of pre-operative segmental mobility. The latter three conditions directly went to the fusion group.
The institutional ethics committee approved this study.
Operative techniques
Generous decompression of neural elements (i.e. resection of the bilateral uncovertebral joints, including the asymptomatic side, and the posterior longitudinal ligament) prior to artificial disc implantation or bone grafts was routinely conducted. All anterior cervical fusions, including ACDF and ACCF, were instrumented with plate and screws. The surgical techniques and management for patients with cervical arthroplasty were as described in a previously published series [7, 18].
Clinical and radiographic evaluations
All data were prospectively collected. Standard antero-posterior and lateral radiographs were taken within 5 days and approximately 3, 6, 12, and 24 months post-operatively. Lateral flexion–extension radiographs were added at each time point for arthroplasty patients but not for ACDF or ACCF patients until fusion was achieved. Clinical outcomes were assessed during the same clinical visit by two special nursing assistants, under physicians’ supervision, using the Visual Analogue Scale (VAS), Neck Disability Index (NDI), and Japanese Orthopedic Association (JOA) score. Segmental ROM at the index level was measured using the quantitative measurement analysis software, SmartIris (Taiwan Electronic Data Processing Co., Taiwan).
Radiographic interpretations, including segmental mobility and bone fusion, were made by independent radiologists and two neurosurgeons. Multi-detector computed tomography (CT) scans of the cervical spine with reconstructed images were performed on follow-up visits beyond 12 months post-surgery to confirm bone fusion.
Statistical analysis
All statistical analyses were performed using the SPSS software (SPSS Inc., Chicago, IL). Independent t-tests and paired t-tests were used for continuous variables, whereas the Fisher exact test was applied for categorical data. A p < 0.05 was considered statistically significant.
Results
Demographics
Eighty-three patients who fulfilled our inclusion criteria were enrolled at the beginning. At the end of this cohort study, a total of 77 patients (92.8 %) completed the follow-up. There were six patients (7.2 %) lost to follow-up. Seventy-seven (77) patients with two-level cervical DDD or spondylosis who underwent cervical arthroplasty or anterior cervical fusion were analyzed, including 23 (29.9 %) females and 54 (70.1 %) males. Their mean age at the time of surgery was 57.7 ± 11.3 years and their mean follow-up time was 39.6 ± 6.7 months (Table 1).
Table 1.
Clinical and demographic characteristics (n = 77)
| Characteristic | Value |
|---|---|
| Gender | |
| Male | 54 (70.1 %) |
| Female | 23 (29.9 %) |
| Age (years) | |
| Range | 24–83 |
| Mean | 57.7 ± 11.3 |
| Clinical follow-up (months) | |
| Range | 28–52 |
| Mean | 39.6 ± 6.7 |
| EBL (ml) | |
| Range | 50–800 |
| Mean | 174.4 ± 147.6 |
EBL estimated blood loss
These 77 patients were then divided into the arthroplasty group, composed of 37 patients (48.1 %) who received two-level Bryan (Medtronic Spine and Biologics, Memphis, TN) disc replacement (Fig. 1), and the fusion group, composed of 40 patients (51.9 %) who had two-level ACDF or ACCF surgery (Fig. 2). Based on the distribution of the arthroplasty or fusion levels, the C4–C5 and C5–C6 levels accounted for the most frequent levels in both groups (Table 2).
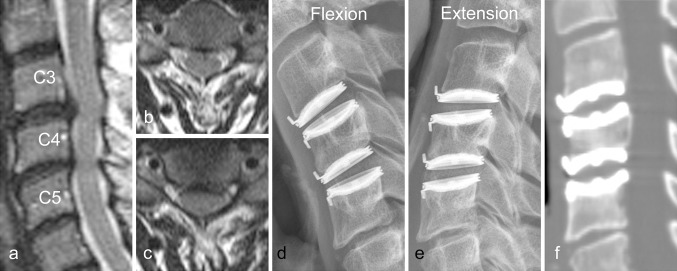
Fig. 1.
Radiographs of a 56-year-old male who underwent Bryan cervical arthroplasty at the C3, C4, and C5 levels. a–c Pre-operative magnetic resonance imaging (MRI) demonstrated a herniated intervertebral disc with root compression. d–e Dynamic lateral radiographs 24 months post-operation showed that the treated levels remained mobile. f CT scan 24 months post-operation demonstrated the negative finding of heterotopic ossification
Fig. 2.
Radiographs of an 83-year-old male who underwent anterior cervical discectomy and fusion at the C4, C5, and C6 levels. a–c Pre-operative MRI demonstrated disc herniation causing spinal stenosis. d–e Dynamic lateral radiography after 25 months revealed bony fusion without segmental mobility
Table 2.
Level distributions
| Level | No. of level (%) |
|---|---|
| Arthroplasty (n = 74) | |
| C3–4 | 3 (4.1 %) |
| C4–5 | 25 (33.8 %) |
| C5–6 | 35 (47.2 %) |
| C6–7 | 11 (14.9 %) |
| Fusion (n = 80) | |
| C2–3 | 2 (2.5 %) |
| C3–4 | 15 (18.8 %) |
| C4–5 | 24 (30.0 %) |
| C5–6 | 25 (31.3 %) |
| C6–7 | 13 (16.2 %) |
| C7–T1 | 1 (1.2 %) |
Cervical arthroplasty versus fusion in two-level diseases
Comparing the arthroplasty and fusion groups for two-level diseases (Table 3), the arthroplasty group was significantly younger (52.1 vs. 63.0 years, p < 0.001). The proportional sex composition in the two groups was also similar (75.7 versus 65.0 % males, p = 0.306). The average operation time in the arthroplasty group (315.5 min) was significantly longer than that in the fusion group (224.9 min, p < 0.001). The mean estimated blood loss (EBL) was not significantly different in both groups (198.5 ml vs. 153.3 ml, p = 0.135) and the average pre-operative ROM at the index levels was also similar (20.1° versus 19.3°, p = 0.436).
Table 3.
Comparison between the arthroplasty and fusion groups
| Variables | Total (%) | Groups | ||
|---|---|---|---|---|
| Arthroplasty | Fusion | Significant p values | ||
| No. of patients | 77 | 37 | 40 | |
| Age (years) | 52.1 ± 9.1 | 63.0 ± 10.6 | <0.001* | |
| Gender | 0.306 | |||
| Male | 28 (75.7 %) | 26 (65.0 %) | ||
| Female | 9 (24.3 %) | 14 (35.0 %) | ||
| Operation time (min) | <0.001* | |||
| Range | 180–530 | 140–375 | ||
| Mean | 315.5 ± 82.0 | 224.9 ± 61.8 | ||
| EBL (ml) | 0.135 | |||
| Range | 50–800 | 50–600 | ||
| Mean | 198.5 ± 165.4 | 153.3 ± 128.7 | ||
| Pre-op ROM (degree) | 0.436 | |||
| Range | 5.0–31.0 | 6.0–31.0 | ||
| Mean | 20.1 ± 6.3 | 19.3 ± 5.9 | ||
EBL estimated blood loss, NSAID non-steroid anti-inflammatory drug, ROM range of motion
* p < 0.05, statistically significant
The clinical outcomes measured by VAS neck, VAS arm, NDI, and JOA scores all significantly improved after surgery compared with the pre-operative scores in both the arthroplasty and fusion groups (Figs. 3, 4, 5). There were also no significant differences between the two groups at each time point of evaluation (i.e. pre-operation and at 3, 6, 12, and 24 months post-operation) (Figs. 3, 4, 5).
Fig. 3.
Comparison of the mean VAS scores for neck and arm pain in the arthroplasty (n = 37) and fusion (n = 40) groups. Error bars standard deviations (SD), asterisk significant improvement compared with pre-operative scores, brackets no significant difference between the two groups at each time point of evaluation (i.e. pre-operation and 3, 6, 12, and 24-months post-operation)
Fig. 4.
Comparison of the mean JOA scores in the arthroplasty (n = 37) and fusion (n = 40) groups. Error bars standard deviations (SD), asterisk significant improvement compared with pre-operative scores, brackets no significant difference between the two groups at each time point of evaluation (i.e. pre-operation and 3, 6, 12, and 24-months post-operation)
Fig. 5.
Comparison of the NDI scores of the arthroplasty (n = 37) and fusion (n = 40) groups. The NDI scores significantly improved after surgery compared with pre-operation scores in both groups. There were no significant differences between the two groups at each time point of evaluation (i.e. pre-operation and at 3, 6, 12, and 24-months post-operation)
The post-operative radiographic ROM measurement at the index levels was significantly different in the two groups (Table 4). In the arthroplasty group, there was a significant increase between pre- and post-operative (after 24 months) ROM (20.1° versus 23.5°, p = 0.018). In contrast, the fusion group uniformly achieved bone fusion (100 %) and demonstrated little ROM at 24 months post-operation compared with pre-operative values (1.6° versus 19.3°, p < 0.001).
Table 4.
Radiographic outcomes
| Group | ROM (degree) | ||
|---|---|---|---|
| Pre-op | 24-months | p value | |
| Arthroplasty | 20.1 ± 6.3 | 23.5 ± 7.8 | 0.018* |
| Fusion | 19.3 ± 5.9 | 1.6 ± 1.0 | <0.001* |
ROM range of motion
* p < 0.05, statistically significant
There was no secondary surgery (e.g. revision, removal, pseudo-arthrosis, conversion to fusion, or re-operation) and no other complications (e.g. instrument failure, wound infection, worsened neurologic symptoms). There also was no symptomatic adjacent segment disease (ASD) requiring further surgery. However, for the incidence of ASD, longer-term follow-up might be needed for confirmation.
Discussion
This study analyzed 77 patients with two-level cervical DDD or spondylosis who underwent surgery, with a mean follow-up of more than 3 years (range 28–52 months). Comparing the 37 patients who underwent two-level Bryan arthroplasty to the 40 patients who underwent instrumented fusion, the arthroplasty group had a mean age of 52.1 years, which was significantly younger than that of the fusion group (63.0 years, p < 0.001). The arthroplasty group had a significantly longer mean operation time (315.5 versus 224.9 min, p < 0.001). Other demographic features such as sex composition, EBL, and pre-operative ROM at the index levels were not significantly different in both groups (p = 0.306, 0.135, and 0.436, respectively). Clinical outcomes, including VAS neck, VAS arm, NDI, and JOA scores, all significantly improved after surgery compared with the pre-operative status in both groups. Moreover, there were no significant differences between the two groups at each time point of evaluation (i.e. pre-operation and at 3, 6, 12, and 24 months post-operation). The arthroplasty group had significantly increased ROM of the index levels (23.5° versus 20.1°, p = 0.018). On the other hand, there was significant limitation in the ROM post-surgery in the fusion group (1.6° versus 19.3°, p < 0.001).
The FDA-IDE trials corroborate the non-inferiority of cervical arthroplasty to ACDF in one-level diseases [10, 12–14, 16, 17]. Aside from the FDA-IDE trials, many other studies demonstrate substantially good mid-term results in one- and two-level cervical arthroplasty [7, 18, 19]. Although these reports claim similar clinical outcomes, the actual differences between one- and two-level cervical arthroplasty remain unclear. There must be care in extrapolating the success of cervical arthroplasty for one-level DDD into the two-level scenario. Theoretically, strategies for spinal motion preservation, such as arthroplasty in this case, provide less post-operative ROM limitations for multiple-level than for single-level spondylosis. It is reasonable to infer that the merit of arthroplasty, the maintenance of physiologic segmental motion, is more evident in two-level than in one-level diseases. However, some studies point to more heterotopic ossification (HO) in two-level cervical spondylosis [20, 21]. Despite little clinical significance, more HO formation in two-level arthroplasty implies an underlying discrepancy with the one-level cervical arthroplasty. Therefore, the safety and effectiveness of one-level arthroplasty cannot be simply translated into two- or multi-level diseases.
There is a paucity of evidence regarding the true biomechanical effects of two or more levels of cervical arthroplasty. One prospective randomized study claims substantial improvement in VAS and NDI for two-level Bryan cases at 2-year follow-up [22]. Several other reports have included two-level cervical arthroplasty with various case numbers and uniformly claim safety and effectiveness [18, 23]. However, most of these studies do not specifically look into the outcomes of two-level cervical arthroplasty or compare them with two-level fusion cases. A previous study suggests more HO formation and less mobile artificial discs in patients who receive two-level Bryan arthroplasty than one-level [24].
The operation time was recorded from skin incision to complete closure of the wound. We found arthroplasty to be more time-consuming because care must be taken to achieve wide decompression, fine endplate preparation, and appropriate sizing of the device, such as the carpentry of the implant could possibly affect the outcome of cervical arthroplasty.
The best candidates for cervical arthroplasty are younger patients with one-level herniated disc causing cervical radiculopathy whose facet joints are normal [7]. Compared with patients with one-level DDD, patients with two-level cervical spondylosis may have a more advanced stage of degeneration. The higher incidence of HO found in two-level cases may also imply continuous degeneration after cervical arthroplasty [21]. Therefore, the artificial discs implanted in two-level cases may be more vulnerable to adverse events related to continuous degeneration in the long run [25], while the two-level fusion constructs are usually more stable once the bone fusion is achieved. Further investigation with longer follow-up is needed to clarify the safety and efficacy of two-level cervical arthroplasty.
This study has two major limitations. First, it is a retrospective non-randomized study and the choices of cervical arthroplasty or fusion were based on patients’ and surgeons’ preferences, which indicate substantial differences (i.e. older age in the fusion group) between the two groups. A multi-center, large-scale, prospective, and randomized trial like the FDA-IDE trials for one-level diseases would be of higher scientific value. Nonetheless, this is the first study to focus specifically on two-level spondylosis and it has demonstrated similar clinical outcomes at 3 years post-operation. Despite its limitations, this report provides evidence that two-level arthroplasty is as safe and effective as anterior fusion at 3-year follow-up. Second, the relatively small sample size and mid-term follow-up time may be insufficient to detect differences in either clinical or radiographic outcomes between the two groups. It is possible that fusion-related ASD can be more prominent in the two-level than in the one-level constructs. If cervical arthroplasty has a protective effect against ASD, adopting this technology in multi-level cervical spondylosis will be more advantageous than in single-level.
The strengths of this study include the standardized outcome measurement, with a mean follow-up of over 3 years, consecutive patients, same degrees of decompression of neural elements in both groups (by the same surgeons), and a nearly one-to-one comparison between arthroplasty and fusion with focus on only two-level DDD. There is little patient selection because all patients have been followed-up under the same protocol. The lost-to-follow-up rate is approximately the same in both groups. Furthermore, a single type of arthroplasty device, Bryan disc, has been utilized, thereby reducing confounding covariates in clinical practice. Clinical outcomes are comparable with those of previously published reports, and the results may shed some light on the value of two- or multi-level cervical arthroplasty. However, further investigations are necessary to corroborate the findings here and improve the understanding of arthroplasty as a treatment for multiple-level cervical DDD.
Conclusions
Clinical outcomes of two-level cervical arthroplasty and two-level anterior cervical fusion are similar at 39.6 months after surgery. Cervical arthroplasty preserves mobility at the index levels without more adverse effects compared with anterior cervical fusion. However, larger-scale randomized trials are warranted to confirm the efficacy and safety of two-level cervical arthroplasty.
Acknowledgments
No funds were received in support of this work and no benefits in any form have been and will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study, or the findings specified in this paper.
Footnotes
L.-Y. Fay and W.-C. Huang contributed equally to this paper.
References
- 1.Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine. 2007;6(4):298–303. doi: 10.3171/spi.2007.6.4.2. [DOI] [PubMed] [Google Scholar]
- 2.Hilibrand AS, Balasubramanian K, Eichenbaum M, Thinnes JH, Daffner S, Berta S, Albert TJ, Vaccaro AR, Siegler S. The effect of anterior cervical fusion on neck motion. Spine (Phila Pa 1976) 2006;31(15):1688–1692. doi: 10.1097/01.brs.0000224165.66444.71. [DOI] [PubMed] [Google Scholar]
- 3.Matz PG, Pritchard PR, Hadley MN. Anterior cervical approach for the treatment of cervical myelopathy. Neurosurgery. 2007;60(1 Supp1 1):S64–S70. doi: 10.1227/01.NEU.0000215399.67006.05. [DOI] [PubMed] [Google Scholar]
- 4.Steinmetz MP, Patel R, Traynelis V, Resnick DK, Anderson PA. Cervical disc arthroplasty compared with fusion in a workers’ compensation population. Neurosurgery. 2008;63(4):741–747. doi: 10.1227/01.NEU.0000325495.79104.DB. [DOI] [PubMed] [Google Scholar]
- 5.Suchomel P, Jurak L, Benes V, 3rd, Brabec R, Bradac O, Elgawhary S. Clinical results and development of heterotopic ossification in total cervical disc replacement during a 4-year follow-up. Eur Spine J. 2010;19(2):307–315. doi: 10.1007/s00586-009-1259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Traynelis VC. Spinal arthroplasty. Neurosurg Focus. 2002;13(2):E10. doi: 10.3171/foc.2002.13.2.11. [DOI] [PubMed] [Google Scholar]
- 7.Wu JC, Huang WC, Tu TH, Tsai HW, Ko CC, Wu CL, Cheng H. Differences between soft-disc herniation and spondylosis in cervical arthroplasty: CT-documented heterotopic ossification with minimum 2 years of follow-up. J Neurosurg Spine. 2012;16(2):163–171. doi: 10.3171/2011.10.SPINE11497. [DOI] [PubMed] [Google Scholar]
- 8.Goffin J, van Loon J, Van Calenbergh F, Lipscomb B. A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan Cervical Disc Prosthesis. J Neurosurg Spine. 2010;12(3):261–269. doi: 10.3171/2009.9.SPINE09129. [DOI] [PubMed] [Google Scholar]
- 9.Heidecke V, Burkert W, Brucke M, Rainov NG. Intervertebral disc replacement for cervical degenerative disease–clinical results and functional outcome at two years in patients implanted with the Bryan cervical disc prosthesis. Acta Neurochir (Wien) 2008;150(5):453–459. doi: 10.1007/s00701-008-1552-7. [DOI] [PubMed] [Google Scholar]
- 10.Burkus JK, Haid RW, Traynelis VC, Mummaneni PV. Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine. 2010;13(3):308–318. doi: 10.3171/2010.3.SPINE09513. [DOI] [PubMed] [Google Scholar]
- 11.Coric D, Nunley PD, Guyer RD, Musante D, Carmody CN, Gordon CR, Lauryssen C, Ohnmeiss DD, Boltes MO. Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine. 2011;15(4):348–358. doi: 10.3171/2011.5.SPINE10769. [DOI] [PubMed] [Google Scholar]
- 12.Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007;6(3):198–209. doi: 10.3171/spi.2007.6.3.198. [DOI] [PubMed] [Google Scholar]
- 13.Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, Darden B. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9(4):275–286. doi: 10.1016/j.spinee.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Upadhyaya CD, Wu JC, Trost G, Haid RW, Traynelis VC, Tay B, Coric D, Mummaneni PV. Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine. 2012;16(3):216–228. doi: 10.3171/2011.6.SPINE10623. [DOI] [PubMed] [Google Scholar]
- 15.Kim SW, Limson MA, Kim SB, Arbatin JJ, Chang KY, Park MS, Shin JH, Ju YS. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J. 2009;18(2):218–231. doi: 10.1007/s00586-008-0854-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, Coric D, Cauthen JC, Riew DK. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 2009;34(2):101–107. doi: 10.1097/BRS.0b013e31818ee263. [DOI] [PubMed] [Google Scholar]
- 17.Sasso RC, Anderson PA, Riew KD, Heller JG. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. Orthopedics. 2011;34(11):889. doi: 10.3928/01477447-20110922-24. [DOI] [PubMed] [Google Scholar]
- 18.Tu TH, Wu JC, Huang WC, Guo WY, Wu CL, Shih YH, Cheng H. Heterotopic ossification after cervical total disc replacement: determination by CT and effects on clinical outcomes. J Neurosurg Spine. 2011;14(4):457–465. doi: 10.3171/2010.11.SPINE10444. [DOI] [PubMed] [Google Scholar]
- 19.Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J, Steib JP, Vital JM, Aubourg L, Vila T. Intermediate clinical and radiological results of cervical TDR (Mobi-C) with up to 2 years of follow-up. Eur Spine J. 2009;18(6):841–850. doi: 10.1007/s00586-009-1017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 2003;16(4):384–389. doi: 10.1097/00024720-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, Logroscino C, Pointillart V (2005) Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery 57(4):759–763; (discussion 759-763). pii:00006123-200510000-00017 [DOI] [PubMed]
- 22.Cheng L, Nie L, Zhang L, Hou Y. Fusion versus Bryan Cervical Disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop. 2009;33(5):1347–1351. doi: 10.1007/s00264-008-0655-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peng CW, Yue WM, Basit A, Guo CM, Tow BP, Chen JL, Nidu M, Yeo W, Tan SB. Intermediate results of the prestige LP cervical disc replacement: clinical and radiological analysis with minimum two-year follow-up. Spine (Phila Pa 1976) 2011;36(2):E105–E111. doi: 10.1097/BRS.0b013e3181d76f99. [DOI] [PubMed] [Google Scholar]
- 24.Wu JC, Huang WC, Tsai HW, Ko CC, Fay LY, Tu TH, Wu CL, Cheng H. Differences between one- and two-level cervical arthroplasty: more heterotopic ossification in two-level disc replacement. J Neurosurg Spine. 2012;16(6):594–600. doi: 10.3171/2012.2.SPINE111066. [DOI] [PubMed] [Google Scholar]
- 25.Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, Korge A, Mayer HM. Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 2006;31(24):2802–2806. doi: 10.1097/01.brs.0000245852.70594.d5. [DOI] [PubMed] [Google Scholar]