Abstract
Purpose
To identify changes in cervical alignment parameters following surgical correction of thoracolumbar deformity and then assess the preoperative parameters which induce changes in cervical alignment following corrective thoracolumbar deformity surgery.
Methods
A retrospective study of 49 patients treated for thoracolumbar deformity with preoperative planning of an acceptably aligned coronal and sagittal plane in each case. We compared cervical spine parameters in two distinct low [preoperative C7 sagittal vertical axis (SVA) ≤6 cm] and high (preoperative C7 SVA ≥9 cm) C7 SVA groups. Multilinear regression analysis was performed and revealed the relationship between postoperative cervical lordosis and preoperative spinopelvic parameters and surgical plans.
Results
In the lower C7 SVA group, cervical lordosis was significantly increased after thoracic/lumbar deformity correction (p < 0.01). In contrast, the high C7 SVA group showed decreased cervical lordosis postoperatively (p < 0.01). Multilinear regression analysis demonstrated the preoperative parameters (preoperative C2–7 angle, T1 slope, surgical plan for PT and C7 SVA), which determine the postoperative cervical lordosis.
Conclusion
In spinal deformity procedures, preoperative spinal alignment parameters, and surgical plans could affect postoperative cervical spine alignment.
Keywords: Spinal deformity surgery, Cervical spine lordosis, Global sagittal balance
Introduction
The reciprocal curves of cervical lordosis, thoracic kyphosis, and lumbar lordosis allow for maintenance of horizontal gaze and minimization of energy expenditure in the normal state. There is increasing recognition of the complex global interactions among these sagittal curves, the pelvis, and compensatory mechanisms that attempt to maintain global sagittal spinopelvic alignment [1–4].
Compromise of sagittal alignment, as can occur in adult spinal deformity, is associated with increased pain and disability [5]. Pedicle subtraction osteotomy (PSO) is a recognized surgical procedure for sagittal alignment restoration [3, 6]. Although the PSO procedure produces a focal increase in lordosis, it has been shown to result in significant reciprocal changes, even outside of the instrumented regions of the thoracolumbar spine [7]. Klineberg et al. reported that a thoracic osteotomy with limited fusion produced spontaneous reciprocal decrease in lordosis of the unfused lumbar spine. They also reported that a lumbar osteotomy with limited fusion resulted in a spontaneous increase in the kyphosis of unfused thoracic segments. These reciprocal changes may negatively impact the global spinopelvic alignment and may increase the risks of junctional degeneration [8].
Our objectives in the present study were twofold. First, we sought to assess changes in cervical alignment parameters following surgical correction of thoracolumbar deformity and to assess whether these changes are impacted by the presence or absence of significant preoperative positive sagittal malalignment. Second, we aimed to identify the preoperative parameters which induce these changes in cervical alignment following corrective thoracolumbar deformity surgery.
Materials and methods
Patient population
Consecutive adult patients with thoracolumbar spinal deformity who were surgically treated by the senior author (CPA) between April 2009 and April 2011 were identified based on surgical records. Inclusion criteria for the present study included: age ≥21 years, surgically treated for spinal deformity with more than five levels of instrumented fusion, availability of pre- and postoperative full-length anteroposterior (AP) and lateral standing X-rays that included visualization from C1 through S1, and visualization of the femoral heads. Patients with ankylosing spondylitis or spinal deformity due to neuromuscular conditions, tumor, or infection were excluded from the analysis. Clinical, surgical, and radiographic records were analyzed. This study was approved by the Institutional Review Board of the University of California, San Francisco.
Radiological measurements
Full-length standing AP and lateral radiographs were obtained in a standardized upright position, with arms forward horizontally and folded. Radiographic measurements were obtained in accordance with standard techniques on standing radiographs [9]. The occiput to C2 angle (Occ–C2) was measured from the line between the anterior arch of C1 and the inferior end of the occiput to the line along the inferior margin of the C2 body. The C1–C2 angle (C1–2) was measured from the line between the anterior arch of C1 and the posterior arch of C2 to the line along the inferior margin of the C2 body. The C2–C7 angle (C2–7) was measured between the line along the posterior body of C2 to the line along the posterior body of C7. The T1 slope was measured between the line along the superior endplate of T1 and a horizontal reference line.
Thoracic kyphosis (T5–12) was defined by the Cobb angle between the cranial endplate of T5 and the caudal endplate of T12. Thoracolumbar kyphosis (T10–L2) was defined by the angle between the cranial endplate of T10 and the caudal endplate of L2. Lumbar lordosis (L1–5) was defined by the angle between the cranial endplate of L1 and the S1. The C7 sagittal vertical axis (C7 SVA) and the C2 SVA were defined by the horizontal distance from the superior posterior end of the upper sacral endplate to the C7 or C2 plumblines, respectively.
Pelvic tilt (PT) was defined by the angle between the line connecting the midpoint of the S1-endplate to the axis of the femoral heads and the vertical plane. Sacral slope (SS) was defined as the angle between the horizontal and sacral endplates. Pelvic incidence (PI) was defined as the angle perpendicular to the sacral endplate at its midpoint and the line connecting this point to axes of the femoral heads.
Study design and statistical analyses
The data were analyzed using SPSS software (SPSS, Chicago, Illinois). Patients were categorized based on preoperative C7 SVA (sagittal vertical axis) into one of three groups: low C7 SVA (C7 SVA ≤6 cm), intermediate C7 SVA (C7 SVA between 6 and 9 cm), and the high C7 SVA group (C7 SVA ≥9 cm). The mean values, standard errors, and ranges of the measured radiographic parameters were determined for each group and differences in the mean measurements within and between groups were assessed using t tests and ANOVA. Chi-square test was performed to analyze the parametric variables. Statistical analyses were two sided, and p < 0.05 was considered to be statistically significant.
The relationship between preoperative radiographic parameters and cervical lordosis was defined using forward stepwise multivariate linear regression analysis. This included an initial correlation analysis to identify the relationships between preoperative global sagittal spinopelvic parameters. Patients from all three SVA groups (low, intermediate, and high) were used for multivariate analysis. For each case, the surgical plan was presumed to include achievement of an ideal C7 SVA (0 mm) and an ideal PT (≤25°) following deformity correction [3, 9, 10]. Based on the amount of correction necessary to achieve these ideals, two parameters were defined: “C7 SVA plan” (preoperative C7 SVA −0 mm) and the “PT plan” (preoperative PT −25°). Patients with coronal imbalance and scoliosis with or without sagittal deformity were also included with the goal of a neutral coronal alignment (coronal offset <5 cm).
Results
Study population demographics for the 49 patients included are summarized in Table 1. The uppermost instrumented spinal level was between T3 and T12 (most common level was T10), and the lowest instrumentation level was at L5 or at the pelvis in all cases (39 cases included pelvic instrumentation). Patients were categorized into low (n = 21), intermediate (n = 7), or high (n = 21) preoperative C7 SVA (Table 1). There were no significant differences in the demographic parameters listed in Table 1. Compared with the intermediate and high preoperative SVA groups, the number of patients with a preoperative diagnosis of scoliosis was significantly higher in the low C7 SVA group. PSO was the most common procedure in the high C7 SVA group, and facetectomy was the most common type of osteotomy in the low C7 SVA group. The mean amount of correction of C7 SVA was significantly higher in the high preoperative C7 SVA group compared with the low preoperative C7 SVA group. The mean interval between surgery and acquisition of intermediate follow-up standing full-length postoperative X-rays was 178 days.
Table 1.
Demographics and clinical details of this study
| Low C7 SVA (≤6 cm, n = 21) | Intermediate C7 SVA (6 cm < SVA <9 cm, n = 7) | High C7 SVA (≥9 cm, n = 21) | Total patients (n = 49) | |
|---|---|---|---|---|
| Age (years, mean ± SD) | 64.5 ± 10.196 | 61 ± 15.143 | 67.7 ± 9.844 | 65.2 ± 10.86 |
| Sex (n, M:F) | 5:16 | 3:4 | 4:17 | 12:36 |
| Radiologic follow-up periods (days, mean ± SD) | 136 ± 103.19 | 146 ± 72.4 | 235.1 ± 246.6 | 178 ± 184.51 |
| Revision surgery (n) | 8 | 5 | 11 | 24 |
| Preoperative diagnosis | ||||
| Kyphosis | 0 | 1 | 5 | 6 |
| Kyphoscoliosis | 3 | 0 | 5 | 8 |
| Scoliosis | 10 | 1 | 0 | 11** |
| Flat back | 8 | 5 | 7 | 20 |
| Proximal junctional kyphosis | 0 | 0 | 4 | 4 |
| Osteotomy | ||||
| PSO | 3 | 4 | 18 | 25** |
| SPO | 6 | 1 | 1 | 8 |
| VCR | 0 | 1 | 2 | 3 |
| Facetectomy | 12 | 1 | 2 | 15** |
| Interbody fusion | 11 | 6 | 14 | 31 |
| Correction | ||||
| PT (º, mean ± SE) | 2.67 ± 1.57 | 7.43 ± 4.67 | 7.48 ± 2.43 | 5.40 ± 1.39 |
| C7 SVA (mm, mean ± SE) | 13.80 ± 7.17 | 34.42 ± 28.23 | 99.38 ± 11.65 | 53.42 ± 9.03** |
Forty-nine patients were enrolled. Patients whose C7 SVA was 6–9 cm (n = 7) were included in the intermediate C7 SVA group
SVA Sagittal vertical axis, PSO pedicle subtraction osteotomy, SPO Smith–Peterson osteotomy, VCR vertebral column resection, PT pelvic tilt
** Statistical differences among groups were found in the preoperative diagnosis of scoliosis, the types of osteotomy, and amount of C7 SVA correction (p < 0.01)
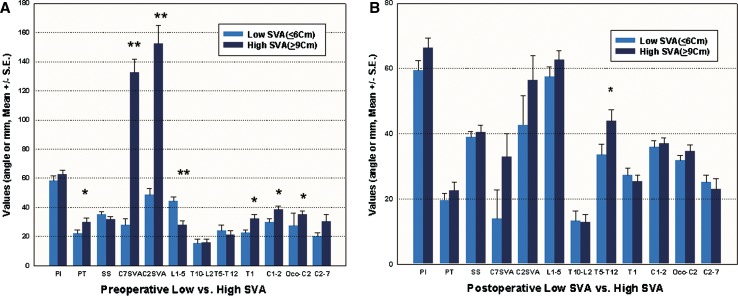
Compared with the low C7 SVA group, the high C7 SVA group had significantly higher preoperative PT (22.3° ± 2.2° vs. 30.0° ± 2.6°; p < 0.05), T1 slope (22.9° ± 1.8° vs. 32.2° ± 3.0°; p < 0.05), C1–2 angle (30.5° ± 2.1° vs. 38.6° ± 1.8°; p < 0.05), and Occ–C2 (27.2° ± 1.9° vs. 35.0° ± 2.5°; p < 0.05) (Fig. 1a).The low C7 SVA group had significantly greater lumbar lordosis (44.3° ± 2.8°) compared with the high C7 SVA group (28.1° ± 2.6°; p < 0.01). In contrast, on postoperative imaging, the differences in radiographic measurements only included higher thoracic kyphosis (44.0° ± 3.3° vs. 33.5° ± 3.4°; p < 0.05) in the high C7 SVA group (Fig. 1b).
Fig. 1.
Comparison of preoperative and postoperative sagittal radiographic measurements. a The high C7 SVA group demonstrates higher PT, L1–5, T1, C1–2, and Occ–C2. b The high C7 SVA group, compared to the low C7 SVA group, has higher PT and T5–T12. (*p < 0.05, **p < 0.01). PI pelvic incidence, PT pelvic tilt, SS sacral slope, SVA sagittal vertical axis
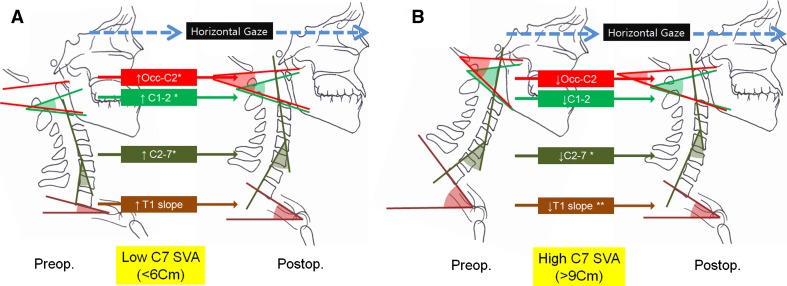
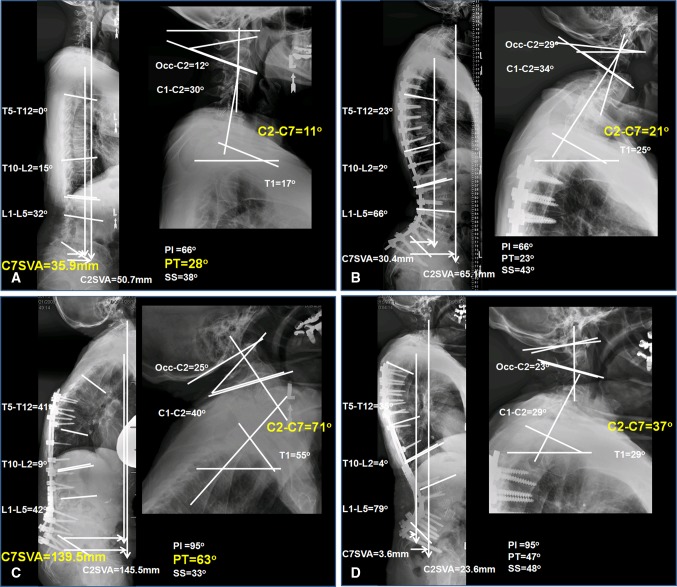
The postoperative changes in cervical spine alignment that occurred in the low and high C7 SVA groups are illustrated in Fig. 2. In the low C7 SVA group, parameters reflective of cervical lordosis tended to increase after thoracolumbar deformity correction (Occ–C2, p = 0.034; C1–2, p = 0.001; C2–7 angles p = 0.025; T1, p = 0.13). In contrast, in the high C7 SVA group, parameters reflective of cervical lordosis tended to decrease after thoracolumbar deformity correction (Occ–C2, p = 0.86; C1–2, p = 0.38; C2–7, p = 0.025; T1, p = 0.007). Specific case examples that illustrate the observed reciprocal changes in cervical lordosis in both the low C7 SVA and high C7 SVA groups are shown in Fig. 3.
Fig. 2.
a Reciprocal changes in cervical spine alignment of flattened spinal curve with low C7 SVA (<6 cm). Cervical lordosis parameters increased after thoracolumbar correction deformity surgery. Occ–C2 angle*(preop 31.8 ± 1.5° vs. postop 35.0 ± 2.5°), C1–C2 anlge*(preop 36.0 ± 1.8° vs. 38.6 ± 1.8°), C2–C7 angle*(preop 25.1 ± 2.2° vs. postop 30.5 ± 4.5°) and T1 slope (preop 27.3 ± 2.3° vs. postop 32.2 ± 3.0°) increase postoperatively. b High C7 SVA patient group (mean C7 SVA = 132.4 mm) patients depicting higher cervical lordosis parameters preoperatively (left). These cervical lordosis parameters decrease after thoracolumbar correction deformity surgery (right). Occ–C2 angle (Preop 35.0 ± 2.5° vs. postop 34.6 ± 2.0°), C1–C2 angle (preop 38.6 ± 1.8° vs. 36.9 ± 1.8°), C2–C7 angle*(preop 30.5 ± 4.5° vs. postop 23.0 ± 3.1°), and T1 slope**(preop 32.2 ± 3.0° vs. postop 25.5 ± 1.8°) decrease postoperatively (*p < 0.05, **p < 0.01)
Fig. 3.
Case illustrations. Low C7 SVA. a Sagittal preoperative radiographs (left full-length spine lateral radiograph, right cervical spine lateral radiograph) of a patient presenting a low C7 SVA (C7 SVA = 35.9 mm). b Sagittal postoperative radiograph of the same patient after thoracolumbar deformity surgery. Angles reflecting cervical lordosis (Occ–C2, C1–2, C2–7, and T1) are increased postoperatively. High C7 SVA. c Sagittal preoperative radiographs (left whole spine lateral, right cervical spine lateral) of a patient presenting a high C7 SVA (C7 SVA = 139.5 mm). d Sagittal postoperative radiograph of the same patient after pedicle subtraction osteotomy. Angles reflecting cervical lordosis (Occ–C2, C1–2, C2–7 and T1) are decreased postoperatively. PI pelvic incidence, PT pelvic tilt, SS sacral slope, SVA sagittal vertical axis
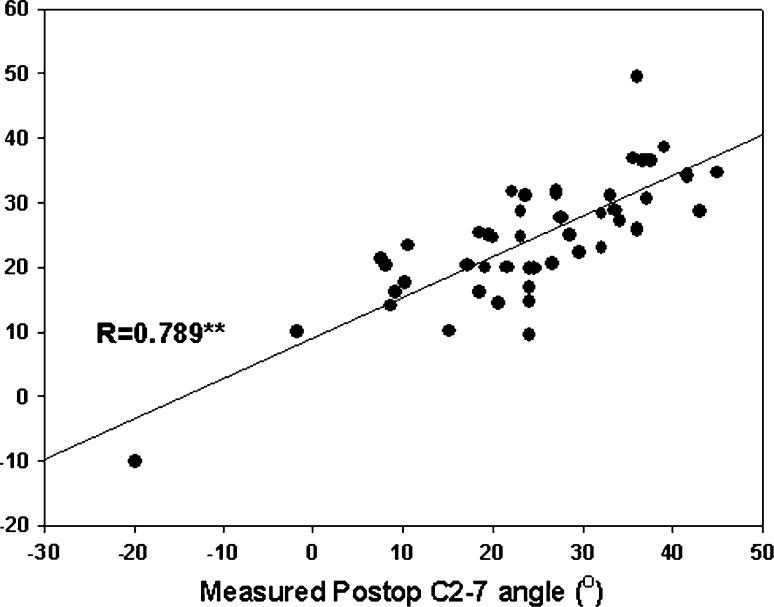
The correlation matrix among all of the assessed radiographic parameters is shown in Table 2. We found significantly high correlations (R > 0.7) between C1–2 and Occ–C2 (0.81), C7 SVA and C2 SVA (0.96), as well as PI and PT (0.76). Therefore, we removed Occ–C2, C2 SVA, and PI parameters from the multilinear regression analysis, to avoid multicollinearity with C1–2, C7 SVA, and PT, respectively. A multilinear regression model was then established (Table 3). Postoperative cervical lordosis (C2–7) had a linear correlation (R = 0.81, adjusted R2 = 0.62) with the equation composed of the variables preoperative C2–7, PT plan (amount of PT change needed to reach 25°), C7 SVA plan (amount of C7 SVA change needed to reach 0 mm), and T1 slope. The coefficients were based on preoperative deviation from ideal spinal pelvic alignment 0 mm SVA and 25° PT with the assumption that this was the correction goal involved in operative planning.
Table 2.
Matrix of correlations among the main spinal and pelvic parameters
| PI | PT | SS | C7 SVA | C2 SVA | T1 | C1–2 | Occ–C2 | C2–7 | L1–5 | T10–L2 | T5–T12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PI | 1 | |||||||||||
| PT | 0.76** | 1 | ||||||||||
| SS | 0.56** | –0.11 | 1 | |||||||||
| C7 SVA | 0.20 | 0.31* | –0.10 | 1 | ||||||||
| C2 SVA | 0.20 | 0.29* | –0.08 | 0.96** | 1 | |||||||
| T1 | –0.03 | 0.14 | –0.25 | 0.38** | 0.43** | 1 | ||||||
| C1–2 | 0.03 | 0.22 | –0.24 | 0.36* | 0.37** | 0.20 | 1 | |||||
| Occ–C2 | –0.04 | 0.11 | –0.21 | 0.40** | 0.46** | 0.07 | 0.81** | 1 | ||||
| C2–7 | 0.05 | 0.14 | –0.10 | 0.21 | 0.13 | 0.59** | 0.18 | –0.06 | 1 | |||
| L1–5 | 0.18 | –0.18 | 0.49** | –0.50** | –0.43** | –0.02 | –0.20 | –0.29* | 0.16 | 1 | ||
| T10–L2 | –0.11 | 0.11 | –0.34* | –0.12 | –0.06 | 0.01 | 0.09 | 0.08 | –0.02 | 0.02 | 1 | |
| T5–T12 | –0.09 | 0.01 | –0.19 | –0.15 | –0.11 | 0.42** | 0.06 | –0.06 | 0.39** | 0.47** | 0.41** | 1 |
P pelvic incidence, PT pelvic tilt, SS sacral slope, SVA sagittal vertical axis
* p < 0.05
** p < 0.01
Table 3.
Multiple linear regression model shows correlations between the postoperative cervical lordosis and preoperative spinopelvic parameters and surgical planning
| A. Correlation and prediction rates to the multilinear regression model | |||
|---|---|---|---|
| r | r 2 | Adjusted r 2 | Std. error of the estimate |
| 0.808 (d) | 0.653 | 0.619 | 7.61677 |
| B. Statistically significant intercept and coefficients of the multilinear regression equation for the postoperative cervical lordosis | |||||
|---|---|---|---|---|---|
| Model | Unstandardized coefficients | Standardized coefficients | t | Sig | |
| B | SE | β | B | SE | |
| (Constant) | 11.851 | 3.012 | 3.935 | 0.000 | |
| Preop C2 to7 angle | 0.440 | 0.085 | 0.598 | 5.194 | 0.000 |
| Preop PT plan | –0.290 | 0.107 | –0.266 | –2.720 | 0.010 |
| Preop C7 SVA plan | –0.072 | 0.023 | –0.336 | –3.208 | 0.003 |
| Preop T1 angle | 0.260 | 0.124 | 0.257 | 2.100 | 0.042 |
Discussion
Thoracolumbar deformity surgery for correction of scoliosis and sagittal malalignment is an important option for symptomatic patients who fail to respond to nonoperative measures. However, only a few recent studies have begun to define the reciprocal changes in the cervical spine, and no study to date has clearly assessed their impact on clinical outcome after thoracolumbar deformity surgery [3–5, 11, 12]. Alteration of normal cervical lordosis has been associated with symptomatic pain and accelerated disc degeneration [13]. Therefore, understanding the compensatory behavior of the mobile cervical spine in thoracolumbar deformity patients may be important with respect to the prevention of secondary cervical spine disorders.
In this study, we identified the reciprocal changes of cervical spine alignment after thoracolumbar deformity surgery and which were induced by preoperative parameters. Specifically, patients with low preoperative SVA demonstrated significant increase in cervical lordosis following deformity correction surgery, while patients having high preoperative SVA demonstrated significant decrease in cervical lordosis following surgery. In addition, we provide a quantitative means of explaining the postoperative changes in cervical alignment that accompany correction of thoracolumbar deformity based on preoperative radiographic parameters, as an aid to surgical planning.
The importance of sagittal spinopelvic alignment of the spine in adult deformity patients has been well recognized [1, 14, 15]. Sagittal malalignment after lumbar spine surgery is a major source of pain and disability. Positive sagittal malalignment was identified as the radiographic parameter most highly correlated with adverse health status outcomes [5]. However, the influence of global sagittal alignment on cervical alignment and neck pain is not fully understood. Knott et al. demonstrated that the T1 slope was the radiographic parameter that had the strongest correlation with SVA [16]. They reported that when the T1 slope was higher than 25° all patients had at least 10 cm of positive sagittal malalignment (C2 SVA). They also showed that patients with negative sagittal alignment had mostly low T1 slopes, usually <13°. Similarly, in the present study we observed different cervical spine alignments between low and high sagittal alignment groups. In the low C7 SVA group (≤6 cm), the preoperative cervical spine had hypolordotic curvatures (low T1 slope and C2–7, C1–2, and Occ–C2 angles), in comparison with the high C7 SVA group (≥9 cm). Collectively, these data suggest that cervical alignment is affected by thoracic regional alignment as well as global sagittal alignment.
The present study, in combination with prior studies, strongly suggests that changes in C7 SVA induce changes in the T1 slope, which in turn may serve as a driving force for inducing reciprocal alterations in cervical spine alignment. Knott et al. have shown a significant correlation between global sagittal alignment and T1 slope, and Smith et al. have shown that the changes in T1 slope that accompany thoracolumbar deformity correction significantly correlate with the compensatory changes in cervical lordosis [16, 17]. In the present study, we further implicate the T1 slope in helping to set the cervical lordosis, since the only preoperative radiographic parameters incorporated into the best-fit linear regression model to predict postoperative cervical lordosis included cervical lordosis, PT, C7 SVA, and T1 slope.
A reciprocal relationship exists between lumbar lordosis and thoracic kyphosis. Therefore, the sagittal thoracic compensatory curve and pelvic retroversion can normalize after restoration of lumbar lordosis [4, 6, 11, 12, 18, 19]. In a previous study of AIS patients, there was a tendency to have more cervical kyphosis in thoracic hypokyphosis patients preoperatively [2, 20–22]. These preoperative kyphotic cervical spines were able to gain more lordosis after restoration of thoracic kyphosis in the scoliosis correction. However, another report argued that, due to the inherent rigidity of the cervical spine, the strong preoperative inverse correlation between cervical and thoracic kyphosis was lost after instrumentation [20]. In the present study, we postulated that restoration of global and regional sagittal alignment could induce reciprocal changes in cervical spine alignment. In Fig. 3, we illustrate that the patient with low C7 SVA has increased cervical lordosis, and the patient with high C7 CVA has decreased cervical lordosis after corrective thoracolumbar deformity surgery. These findings imply that postoperative cervical spine alignment may depend on changes in regional anatomic curvatures (thoracic or lumbar) and sagittal alignment and the observed cervical changes differ depending on the preoperative sagittal alignment.
Although identification of preoperative parameters which may be important in determining postoperative alignment within the given correction strategy paradigms have been studied [4], changes in cervical alignment after surgery are not as clearly understood. We performed a regression analysis to better understand the changes in cervical alignment that accompany thoracolumbar spinal deformity correction. The variables which affect postoperative cervical lordosis were preoperative cervical alignment (C2–7 and T1 slope) and planning for correcting thoracolumbar deformity (PT plan and C7 SVA plan).
Conclusion
Thoracolumbar deformity patients frequently have abnormal curvature of the cervical spine. However, the role of thoracolumbar deformity correction on cervical spine alignment is not entirely understood. This study provides evidence that cervical lordosis has reciprocal changes obligatory for global spine balance. Preoperative parameters in regional spine alignment (C2–7 and T1 angles) and surgical plans based on common correction goals (PT and C7 SVA) could affect postoperative cervical spine sagittal alignment. Therefore, when patients undergo corrective thoracolumbar deformity surgery, significant postoperative reciprocal changes in cervical alignment may occur. These changes are affected by preoperative alignment and correction strategies for the deformity in the sagittal plane. General predictions for postoperative cervical alignment can be made based upon the formulas presented in this work (Fig. 4).
Fig. 4.
Graphical representation of the relationship between predicted and true postoperative values of cervical lordosis (n = 49)
Acknowledgments
This work was supported by National Research Foundation of Korea Grant funded by the Korean Government (2011-0011066).
Conflict of interest
The authors have no personal financial or institutional interest in any of the drugs, materials, or devices described in this article.
References
- 1.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupere G, Pelissier J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hilibrand AS, Tannenbaum DA, Graziano GP, Loder RT, Hensinger RN. The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J Pediatr Orthop. 1995;15:627–632. doi: 10.1097/01241398-199509000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Lafage V, Schwab F, Vira S, Hart R, Burton D, Smith JS, Boachie-Adjei O, Shelokov A, Hostin R, Shaffrey CI, Gupta M, Akbarnia BA, Bess S, Farcy JP. Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction? J Neurosurg Spine. 2011;14:184–191. doi: 10.3171/2010.9.SPINE10129. [DOI] [PubMed] [Google Scholar]
- 4.Lafage V, Schwab F, Vira S, Patel A, Ungar B, Farcy JP. Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine (Phila Pa 1976) 2011;36:1037–1045. doi: 10.1097/BRS.0b013e3181eb9469. [DOI] [PubMed] [Google Scholar]
- 5.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 6.Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine (Phila Pa 1976) 2002;27:612–618. doi: 10.1097/00007632-200203150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Klineberg E, Schwab F, Ames C, Hostin R, Bess S, Smith JS, Gupta MC, Boachie O, Hart RA, Akbarnia BA, Burton DC, Lafage V. Acute reciprocal changes distant from the site of spinal osteotomies affect global postoperative alignment. Adv Orthop. 2011 doi: 10.4061/2011/415946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Virginie L, Christopher A, Frank S, Eric K, Behrooz A, Justin S, Oheneba BA, Douglas B, Robert H, Richard H, Christopher S, Kirkham W, Shay BISSG Changes in thoracic kyphosis negatively impact sagittal alignment following lumbar pedicle subtraction osteotomy: A comprehensive radiographic Analysis. Spine (Phila Pa 1976). doi: 10.1097/BRS.0b013e318225b926
- 9.Schwab F, Lafage V, Patel A, Farcy JP, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 10.Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2009;34:785–791. doi: 10.1097/BRS.0b013e31819d0c86. [DOI] [PubMed] [Google Scholar]
- 11.Blondel B, Lafage V, Schwab F, Farcy JP, Bollini G, Jouve JL. Reciprocal sagittal alignment changes after posterior fusion in the setting of adolescent idiopathic scoliosis. Eur Spine J. 2012;21:1964–1971. doi: 10.1007/s00586-012-2399-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilharreborde B, Vidal C, Skalli W, Mazda K. Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur Spine J. 2013;22:330–337. doi: 10.1007/s00586-012-2493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miyazaki M, Hymanson HJ, Morishita Y, He W, Zhang H, Wu G, Kong MH, Tsumura H, Wang JC. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine (Phila Pa 1976) 2008;33:E870–E876. doi: 10.1097/BRS.0b013e3181839733. [DOI] [PubMed] [Google Scholar]
- 14.Etame AB, Than KD, Wang AC, La Marca F, Park P. Surgical management of symptomatic cervical or cervicothoracic kyphosis due to ankylosing spondylitis. Spine (Phila Pa 1976) 2008;33:E559–E564. doi: 10.1097/BRS.0b013e31817c6c64. [DOI] [PubMed] [Google Scholar]
- 15.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine (Phila Pa 1976) 2000;25:575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 16.Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10:994–998. doi: 10.1016/j.spinee.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 17.Smith JS, Shaffrey CI, Lafage V, Blondel B, Schwab F, Hostin R, Hart R, O’Shaughnessy B, Bess S, Hu SS, Deviren V, Ames CP. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine. 2012 doi: 10.3171/2012.6.SPINE1250. [DOI] [PubMed] [Google Scholar]
- 18.Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 2002;27:59–64. doi: 10.1097/00007632-200201010-00014. [DOI] [PubMed] [Google Scholar]
- 19.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine (Phila Pa 1976) 2006;31:2343–2352. doi: 10.1097/01.brs.0000238970.67552.f5. [DOI] [PubMed] [Google Scholar]
- 20.Canavese F, Turcot K, De Rosa V, de Coulon G, Kaelin A. Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Eur Spine J. 2011;20:1141–1148. doi: 10.1007/s00586-011-1837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruickshank JL, Koike M, Dickson RA. Curve patterns in idiopathic scoliosis. A clinical and radiographic study. J Bone Joint Surg Br. 1989;71:259–263. doi: 10.1302/0301-620X.71B2.2925744. [DOI] [PubMed] [Google Scholar]
- 22.Hwang SW, Samdani AF, Tantorski M, Cahill P, Nydick J, Fine A, Betz RR. Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine. 2011 doi: 10.3171/2011.6.SPINE1012. [DOI] [PubMed] [Google Scholar]