Abstract
Study design
Imaging study of thoracic spine.
Objective
The purpose of this study was to investigate dynamic alignment and range of motion (ROM) at all segmental levels of thoracic spine.
Summary of background data
Thoracic spine is considered to have restricted ROM because of restriction by the rib cage. However, angular movements of thoracic spine can induce thoracic compressive myelopathy in some patients. Although few previous studies have reported segmental ROM with regard to sagittal plane, these were based on cadaver specimens. No study has reported normal functional ROM of thoracic spine.
Methods
Fifty patients with cervical or lumbar spinal disease but neither thoracic spinal disease nor compression fracture were enrolled prospectively in this study (34 males, 16 females; mean age 55.4 ± 14.7 years; range 27–81 years). After preoperative myelography, multidetector-row computed tomography scanning was performed at passive maximum flexion and extension position. Total and segmental thoracic kyphotic angles were measured and ROM calculated.
Results
Total kyphotic angle (T1/L1) was 40.2° ± 11.4° and 8.5° ± 12.8° in flexion and extension, respectively (P < 0.0001). The apex of the kyphotic angle was at T6/7 in flexion. Total ROM (T1/L1) was 31.7° ± 11.3°. Segmental ROM decreased from T1/2 to T4/5 but increased gradually from T4/5 to T12/L1. Maximum ROM was at T12/L1 (4.2° ± 2.1°) and minimum at T4/5 (0.9° ± 3.0°).
Conclusions
Thoracic spine showed ROM in sagittal plane, despite being considered a stable region. These findings offer useful information in the diagnosis and selection of surgical intervention in thoracic spinal disease.
Keywords: Range of motion, Thoracic spine, Sagittal plane, Multidetector-row CT, Dynamic alignment
Introduction
Thoracic spine is considered to have a restricted range of motion (ROM) during flexion and extension compared with that of cervical and lumbar spine; ROM of thoracic spine is restricted by the rib cage. However, little is known about angular movements of thoracic spine. Although previous studies reported ROM of 4°–12° in the sagittal plane for all thoracic segments [1–4], these were based on cadaver specimens. The proportion of surgical cases involving thoracic spine has recently increased (11.2 % of all spinal surgeries according to a large cohort study in Japan) [5]. Therefore, clarification of normal alignment and functional ROM of thoracic spine with regard to diagnosis and selection of surgical techniques is important.
It is unclear whether thoracic spine has restricted ROM. One study reported that ossification of the thoracic posterior longitudinal ligament (OPLL) occurs in association with cervical OPLL [6]. Furthermore, cases of traumatic thoracic spinal cord injury without fracture/dislocation have been reported, and in 3.1 % cases of ossification of the thoracic OPLL diagnosed in our facility, spinal cord injury without fracture/dislocation was noted [7]. Against this background, it is expected that there is some angular movements of thoracic spine as well as cervical and lumbar spine.
The aim of this study was to investigate dynamic alignment and ROM of thoracic spine at the segmental level using multidetector-row computed tomography (MDCT).
Materials and methods
Study population
A total of 50 patients (34 males, 16 females; mean age 55.4 ± 14.7 years; range 27–81 years) admitted to our hospital for cervical or lumbar spinal disease from June 2009 to May 2010 were enrolled prospectively in this study. All the patients were verified as not having thoracic disc herniation, spondylosis, OPLL, ossification of the thoracic ligamentum flavum (OLF), tumour, or spinal compression fracture using radiography, CT scanning, and magnetic resonance imaging (MRI). We defined spinal compression fracture as a reduction in vertebral height more than 15 % using spine lateral radiography. The cases in which a reduction in vertebral height was <15 % and there was no traumatic episode were included as within physiological degenerative change. After preoperative myelography for diagnosis of cervical or lumbar spinal disease, MDCT scanning at the thoracic level was performed in both maximum flexion and extension. This study was approved by the institutional review board. The aims of this study were explained to all patients before myelography and CT scanning, and all patients gave informed consent to their participation.
CT in spinal flexion and extension
In spinal flexion, triangular pillows were placed under the upper and lower back, while in extension, they were placed under the middle back and buttocks (Fig. 1a, b). CT scans were obtained (1-mm-thick axial helical) with sagittal and coronal reconstruction using a 64-line, multi-slice unit (Light Speed VCT; GE Healthcare Bio-Sciences, Piscataway, NJ, USA). It took about 5 s to perform MDCT.
Fig. 1.
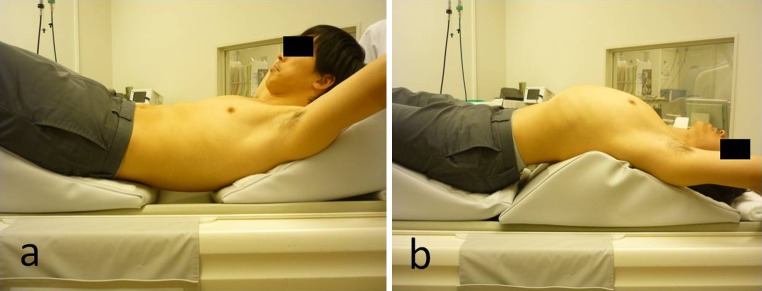
Body posture during flexion (a) and extension (b) on computed tomography. a Triangular pillows supporting the upper and lower back; b triangular pillows supporting the middle back and buttocks
Measurement and data analysis
All CT images were transferred to a microcomputer and all parameters measured using Scion imaging software (Digitalcore Co., Ltd., Onis 2.1, Tokyo, Japan). Segmental kyphotic angles (T1/T2 − T12/L1) were measured in the sagittal plane with reference to the superior edge of the vertebral body as the measuring method of Cobb’s angle (Fig. 2), and total kyphotic angle (T1/L1) was calculated as the summation of segmental kyphotic angles (T1/T2 − T12/L1). Total and segmental ROM were then calculated [ROM = (kyphotic angle at maximum flexion) − (kyphotic angle at maximum extension)]. It was the reason for measuring with reference to each superior edge instead of the inferior edge of the next vertebral body to calculate total kyphotic angle as the summation of segmental kyphotic angles. All parameters were measured once on two different days by a spinal surgeon, and average values were adopted.
Fig. 2.
CT images in the sagittal plane following myelography. a Flexion; b extension
Statistical analyses
The StatMate (ATMS Co., Ltd., Tokyo, Japan) software package was used for data analysis on a personal computer. All values are expressed as the mean ± standard deviation. Mann–Whitney U test was used to determine any significant difference in the kyphotic angle between flexion and extension. Statistical significance was set at P < 0.05.
Results
Total kyphotic angle and ROM
Total kyphotic angle (T1/L1) was 40.2° ± 11.4° [mean ± standard deviation (SD)] and 8.5° ± 12.8° in flexion and extension, respectively (P < 0.0001). Total calculated ROM (T1/L1) was 31.7° ± 11.3°.
Segmental kyphotic angle and ROM
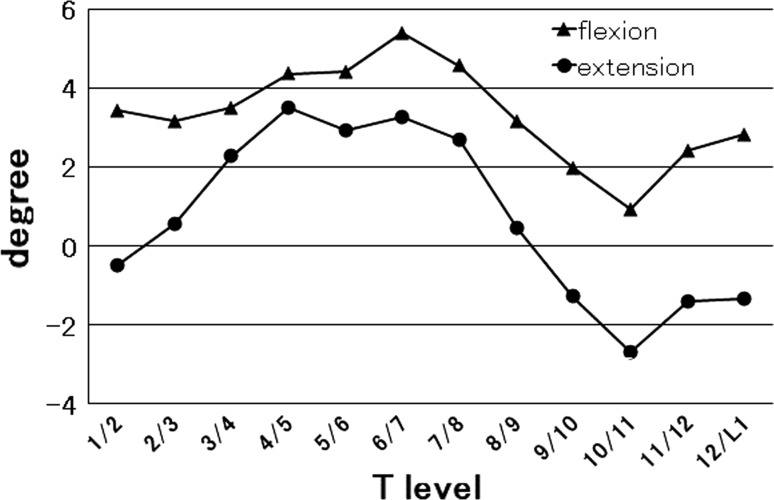
In flexion, the segmental kyphotic angle increased gradually from T1/2 (3.4° ± 4.1°) to T6/7 (5.4° ± 2.6°) but decreased from T6/7 to T10/11 (0.9° ± 2.3°). Below T10/11, the kyphotic angle increased again. The maximum and minimum kyphotic angles in flexion were at T6/7 (5.4° ± 2.6°) and T10/11 (0.9° ± 2.3°), respectively.
In extension, changes in the segmental kyphotic angle were similar to those in flexion. The maximum and minimum kyphotic angles in extension were at T4/5 (3.5° ± 3.0°) and T10/11 (2.7° ± 3.0°), respectively (Fig. 3).
Fig. 3.
The segmental kyphotic angle measured with reference to the superior edge of the vertebral body. All segmental levels except T4/5 showed significant angular movements (P < 0.05)
There were significant changes in the segmental kyphotic angle at all levels not involving T4/5 between flexion and extension. Calculated segmental ROM decreased from T1/2 (3.9° ± 2.8°) to T4/5 (0.9° ± 3.0°) but increased gradually from T4/5 to T12/L1. Maximum and minimum calculated ROM were at T12/L1 (4.2° ± 2.1°) and T4/5 (0.9° ± 3.0°), respectively (Table 1).
Table 1.
The segmental ROM calculated from the kyphotic angle at all levels for maximum flexion and extension
| T level | ROM | P (flexion–extension kyphotic angle) |
|---|---|---|
| 1/2 | 3.9 ± 2.8 | <0.0001 |
| 2/3 | 2.6 ± 3.3 | <0.001 |
| 3/4 | 1.2 ± 2.5 | <0.05 |
| 4/5 | 0.9 ± 3.0 | 0.16 |
| 5/6 | 1.5 ± 2.9 | <0.01 |
| 6/7 | 2.1 ± 2.5 | <0.001 |
| 7/8 | 1.9 ± 2.6 | <0.01 |
| 8/9 | 2.7 ± 2.6 | <0.0001 |
| 9/10 | 3.3 ± 2.5 | <0.0001 |
| 10/11 | 3.6 ± 2.2 | <0.0001 |
| 11/12 | 3.8 ± 2.5 | <0.0001 |
| 12/L1 | 4.2 ± 2.1 | <0.0001 |
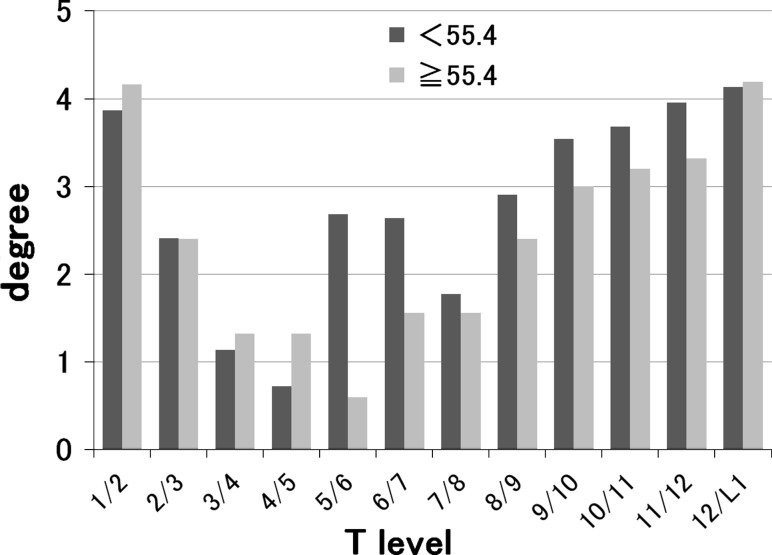
Subjects were divided into two groups by the mean age (55.4 years): in the elderly group, the segmental kyphotic angle in the lower region was more than that in the younger group (below T10/11) and the segmental ROM in the middle and lower region tended to be smaller than that in the younger group (below T5/6) (Fig. 4). Subjects were divided into a female group and a male group: in the female group, the segmental kyphotic angle in the lower region tended to be more than that in the male group and the segmental ROM in the almost all region tended to be more than that in the male group excluding T4/5 and T8/9 (Fig. 5).
Fig. 4.
Subjects were divided into two groups by the mean age (55.4 years). In the elderly group, the segmental ROM tended to be smaller in the middle and lower region (below T5/6)
Fig. 5.
Subjects were divided into a female group and a male group. In the female group, the segmental ROM tended to be more in the almost all region
Discussion
The aims of the present study were to investigate dynamic alignment and ROM at all segmental levels of thoracic spine using MDCT. We demonstrated that the total kyphotic angle (T1/L1) was 40.2° ± 11.4° (mean ± SD) and 8.5° ± 12.8° in flexion and extension, respectively (P < 0.0001). Total calculated ROM (T1/L1) was 31.7° ± 11.3°.
Thoracic spine is considered to have restricted ROM during flexion and extension compared with cervical and lumbar spine because thoracic spine is restricted by the rib cage. However, normal angular movements of thoracic spine have not been clarified as few studies have reported objective numerical results based on in vivo procedures. On the other hand, the number of patients with thoracic spinal disease requiring surgical intervention is increasing. An ageing population and the development of diagnostic imaging equipment (CT and MRI) would appear to have contributed to an increased diagnosis of thoracic spinal disease. In fact, thoracic spinal surgery accounted for 11.2 % of all spinal surgeries according to a large cohort study in Japan [5]. Spinal decompressive or fusion surgeries are widely performed for thoracic compressive myelopathy because of thoracic disc herniation, spondylosis, OPLL, OLF, and tumour. Kyphotic angle and ROM should be considered by the surgeon when preoperatively selecting the surgical procedure, extent of surgery, and fixed alignment. Postoperatively, kyphotic angle and ROM could also be important predictive factors for adjacent segmental degeneration. Therefore, we believe it is indispensable to clarify normal alignment and ROM of thoracic spine to aid in diagnosis and selection of surgical intervention.
Although the present study demonstrated that functional ROM of total thoracic spine in sagittal alignment was 31.7° ± 11.3°, we had expected this figure to be higher. CT scans were obtained with patients in the supine position, unaffected by gravity. Bible et al. [8, 9] reported the normal functional ROM of total cervical and lumbar spine as 102.1° and 81.2°, respectively, on sagittal plane as measured by electrogoniometer and torsiometer. In addition, ROM from C2 to C7 was 55.3° in sagittal plane according to the results of medical checkups on the cervical spine performed on 1,200 healthy volunteers [10]. Consequently, although ROM of thoracic spine is less than that of cervical and lumbar spine, these results led us to conclude that thoracic spine must exhibit significant angular movements in sagittal plane.
The present study demonstrated that the inflexion point of the segmental kyphotic angle was at T6/7 in flexion. In a study conducted on 100 normal, healthy volunteers, Gelb et al. [11] showed that the apex of the thoracic kyphotic curve was at the T6/7 intervertebral disc in individuals aged 40–59 years and at the T7 vertebral body in those aged over 60 years. Our findings with regard to segmental kyphotic angle concur with this report. Moreover, the present study showed that the segmental kyphotic angle increased again below T10/11 and the minimum point of segmental kyphotic angle was T10/11 in all groups. This tendency is stronger in the elderly group and the female group considering our results of age and gender; hence, it is conjectured that the degeneration of vertebral body and intervertebral disc due to ageing and bone density loss is likely to appear below T10/11 because of the stability loss by the rib cage due to transition between true rib and floating rib and the more weight bearing than the upper or middle region.
With regard to segmental ROM of thoracic spine, White et al. [1] found 4.0° of ROM for all segments from T1 to T6, increasing gradually below T7 to 12.0° at the transition between thoracic and lumbar spine. In contrast, thoracic segmental ROM in the present study was approximately 4.0° at the transition between thoracic and cervical spine and between thoracic and lumbar spine, ranging 1.0°–2.0° in the middle region. The discrepancy between these findings and the results of our study may be partly explained by the fact that our study subjects were alive, while those in the study by White et al. were only cadaveric spines. The lack of muscle constraints and rib attachments could increase ROM in the previous study. In the present study, ROM in the upper region might have been influenced by mobility of cervical spine, while ROM in the lower region could have been affected by mobility of lumbar spine, in addition to loss of stability because of the transition between true and floating ribs.
The present study had certain potential limitations, the first of these being that all subjects had been diagnosed with cervical or lumbar spinal disease. Neck, back, or lumbar pain caused by cervical and/or lumbar spinal disease can affect CT scanning images. Moreover, malalignment of the cervical or lumbar spine can have an influence on thoracic kyphotic angle and ROM. A second potential limitation was the fact that CT scanning was performed in the supine position; therefore, maximum flexion and extension could not be obtained. The subjects were not affected by gravity, and for the more obese individuals, flexion and extension were more difficult.
This study provides new and important information on dynamic alignment and ROM of thoracic spine, which is considered to be relatively stable because of its restriction by the rib cage. The key issue is that this study is the first regarding functional angular movements of thoracic spine, and we believe that it will prove useful as an index for diagnosis and selection of surgical intervention in thoracic spinal disease.
Conclusion
Thoracic spine showed ROM in sagittal plane, and a total of 31.7° ROM was measured by flexion–extension CT scanning. With regard to segmental ROM, the minimum was at T4/5. This study is the first to assess functional ROM of thoracic spine in detail and can offer useful information in the diagnosis and selection of surgical intervention in thoracic spinal disease.
Acknowledgments
No funds were received to support this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.White AA, et al. Clinical biomechanics of the Spine. 2. Philadelphia: JB Lippincott Company; 1990. pp. 103–107. [Google Scholar]
- 2.Panjabi MM, Takata K, Goel V, et al. Thoracic human vertebrae. Quantitative three-dimensional anatomy. Spine. 1991;16:888–901. doi: 10.1097/00007632-199108000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Panjabi MM, Hausfeld JN, White AA. A biomechanical study of the ligamentous stability of the thoracic spine in man. Acta Orthop Scand. 1981;52:315–326. doi: 10.3109/17453678109050109. [DOI] [PubMed] [Google Scholar]
- 4.Kothe R, Panjabi MM, Liu W. Multidirectional instability of the thoracic spine due to iatrogenic pedicle injuries during transpedicular fixation. A biomechanical investigation. Spine. 1997;22:1836–1842. doi: 10.1097/00007632-199708150-00008. [DOI] [PubMed] [Google Scholar]
- 5.Nohara Y, Taneichi H, Ueyama K, et al. Nationwide survey on complications of spine surgery in Japan. J Orthop Sci. 2004;9:424–433. doi: 10.1007/s00776-004-0802-7. [DOI] [PubMed] [Google Scholar]
- 6.Ohtsuka K, Terayama K, Yanagihara M, et al. A radiological population study on the ossification of the posterior longitudinal ligament in the spine. Arch Orthop Trauma Surg. 1987;106:89–93. doi: 10.1007/BF00435420. [DOI] [PubMed] [Google Scholar]
- 7.Ito K, Yukawa Y, Nakashima H, et al. Three cases of thoracic spinal cord injuries without fracture and dislocation. J Jpn Med Soc Spinal Cord Lesion. 2009;22:36–37. [Google Scholar]
- 8.Bible JE, Biswas D, Miller CP, et al. Normal functional range of motion of the cervical spine during 15 activities of daily living. J Spinal Disord Tech. 2010;23:15–21. doi: 10.1097/BSD.0b013e3181981632. [DOI] [PubMed] [Google Scholar]
- 9.Bible JE, Biswas D, Miller CP, et al. Normal functional range of motion of the lumbar spine during 15 activities of daily living. J Spinal Disord Tech. 2010;23:106–112. doi: 10.1097/BSD.0b013e3181981823. [DOI] [PubMed] [Google Scholar]
- 10.Yukawa Y, Kato F, Suda K, et al. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine—part I, radiographic data from over 1200 asymptomatic subjects. Eur Spine J. 2012;21:1492–1498. doi: 10.1007/s00586-012-2167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gelb DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]