Abstract
Purpose
To evaluate the natural course of end plate marrow (Modic) changes (MC) in the cervical spine on MRI scans of patients with neck pain. A few longitudinal studies have assessed the development of MC over time in the lumbar spine but only two recent studies evaluated MC in the cervical spine in asymptomatic volunteers and those with whiplash. Thus, this study now reports on the natural course of MC in the cervical spine in symptomatic patients.
Methods
From the cervical MRI scans of 426 neck pain patients (mean age 61.2 years), 64 patients had follow-up MRI studies. The prevalence and types of MC were retrospectively assessed on the follow-up scans and compared to the original MRI findings.
Results
With an average of 2.5 years between the two MRI scans, the prevalence of MC type 1 (MC1) noted at baseline (7.4 % or 19 motion segments) slightly increased (8.2 % or 21 segments) but the prevalence of MC2 (14.5 % or 37 segments) increased considerably (22.3 % or 57 segments). In addition, 14 new MC1 segments and 8 new MC2 segments were noted. Twelve segments with MC1 at baseline converted to MC2 at follow-up. No conversion from MC2 to MC1 or reverting to a normal image was observed.
Conclusions
MC in the cervical spine are a dynamic phenomenon similar to the lumbar spine.
Keywords: Modic changes, Bone marrow, Endplate, Cervical spine, Longitudinal
Introduction
Dr. Michael Modic was the first to publish on identifying and classifying degenerative endplate and marrow changes surrounding a dehydrated intervertebral disc [1, 2]. He described three types of bone marrow changes. Modic type 1 changes (MC1) (low signal on T1-weighted sequences and high signal on T2-weighted sequences) were observed in 4 % of patients and believed to be linked to fibrovascular replacement within the subchondral bone [3]. Modic type 2 changes (MC2) (high signal on T1-weighted sequences and high- or isointense signal on T2 sequences) appear to be more common and indicate fatty replacement in the bone marrow [1, 4–6]. Type 3 changes (low signal on T1 and T2-weighted sequences) are much less frequent and correspond to subchondral sclerosis seen on plain radiographs [2]. Modic changes, particularly MC1, are believed to be associated with rapidly advancing degeneration [7]. They have been linked with low back pain (LBP) [8–14] and are less common in the asymptomatic population [6]. MC in the lumbar spine can convert from one type to another or revert back to normal [13, 15] and represent different stages of the same degenerative process [8].
Most of the literature on MC focuses on the lumbar spine, with only a couple of studies reporting on the prevalence of MC in the cervical spine [16, 17]. The inter-examiner reliability of diagnosing MC in the cervical spine has been shown to be upper moderate with almost perfect intra-examiner reliability [17]. The prevalence in patients over the age of 50 has been shown to be approximately 40 % of individuals or 14 % of the cervical motion segments evaluated [16, 17] with MC2 predominating. Although several studies dealing with the natural course of MC in the lumbar spine have been undertaken [1, 5, 7, 14, 15, 18–22], only two recent studies investigating the dynamics of MC over time for the cervical spine were found [23, 24]. However, one study only evaluated the course of MC in asymptomatic subjects and the other study had an 11-year time period between the baseline and MRI follow-up scans. Therefore, the present study aims to evaluate the course and development of MC in the cervical spine in neck pain patients and compare the findings with the studies on MC in the cervical spine mentioned above as well as correlate with similarly designed studies conducted on the lumbar region.
Materials and methods
Of the 426 patients over the age of 50 with available cervical MRI scans used in a previous study from our orthopaedic university hospital, starting from 2002, 76 of these patients had follow-up examinations (T1- and T2-weighted sagittal and axial images). Exclusion criteria, as obtained from the imaging reports or noted on the MRI, comprised recent acute vertebral fractures including Schmorl’s nodes, surgical fusions, spinal infections or tumors, inflammatory spondyloarthropathy, hemodialysis spondyloarthropathy, congenital or acquired block vertebrae, scoliosis involving a vertebral column curvature of >15° as well as patients who had undergone radiotherapy. Twelve of these 76 patients were excluded leaving 64 patients, 27 female and 37 male, with baseline and follow-up MR imaging for evaluation of the prevalence and type of MC on both imaging dates.
Imaging characteristics and classification of MC were standardized based on the literature and agreed by consensus within the two readers. Prior to study initiation, the two radiologists evaluated a sample set of images and held an in-person meeting to review and refine the standardized definitions. Because this was a retrospective study using data routinely collected, and because patients signed informed consent prior to their procedures, specific ethics approval for this study was not required according to a waiver issued by the ethics committee. Each patient was assigned a number, and data were collected for patient age, gender, presence or absence of MC, MC type and the respective segmental level. Given the fact that MC3 is usually a very rare finding, only MC1 and MC2 were considered in the present study. No mixed MC types were considered. In cases where a ‘mixed’ MC1 or MC2 was noted, the case was classified as either MC1 or MC2 based on the predominate finding. Only the motion segments C3/4, C4/5, C5/6 and C6/7 were evaluated due to the fact that MC are much less frequent in the other cervical segmental levels [16, 17]. SPSS program (Version 16.0, SPSS, Chicago, IL, USA) was used for the statistical evaluation. The prevalence rates of MC were reported in relation to the number of affected motion segments. The prevalence rates were studied in relation to MC type, gender and mean age at baseline.
Results
A total of 64 patients (256 motion segments) were considered in the final MRI comparison evaluations. The mean patient age was 61.2 years (range 50–83), the gender distribution was M:F = 37:27 or 58 % male and 42 % female patients. Out of these 64 patients, 37 or 58 % showed MC in the baseline MRI study (56 motion segments out of a possible 256 or 21.9 % of motion segments evaluated) and 46 patients or 72 % (78 motion segments out of 256 or 30.5 %) showed MC in the follow-up MRI study. This corresponded to 19 motion segments or 7.4 % with MC1 and 37 motion segments (14.5 %) with MC2 in the baseline study. At follow-up, MC were observed in 78 motion segments (30.5 %); 21 motion segments (8.2 %) had MC1 and 57 motion segments (22.3 %) demonstrated MC2 (Table 1).
Table 1.
Prevalence of Modic changes in the baseline [17] and in the follow-up MRI scans (prevalence rates are given in motion segments)
| Baseline MRI study (number of motion segments and % of total) | Follow up MRI study (number of motion segments and % of total) | |
|---|---|---|
| MC1 or 2 | 56 seg. (21.9 %) | 78 seg. (30.5 %) |
| MC1 | 19 seg. (7.4 %) | 21 seg. (8.2 %) |
| MC2 | 37 seg. (14.5 %) | 57 seg. (22.3 %) |
| No MC | 200 seg. (78.1 %) | 178 seg. (69.5 %) |
A total of 64 patients or 256 motion segments (C3/4, C4/5, C5/6 and C6/7) were considered in the evaluation. Average period between the exams for the whole study sample: 2.5 years or 925 days (7–2,920 days). Mean patients’ age: 61.2 years (50–83), M:F = 37:27
MC1 Modic changes type 1, MC2 Modic changes type 2, seg. motion segments in the cervical spine, MRI magnetic resonance imaging
New MC were detected in 22 segments (8.6 % of the total motion segments). Of these new MC, 14 or 5.5 % were MC1 and 8 were MC2 (3.1 %). The change from MC1 to MC2 occurred in 12 motion segments of the original 19 or 4.7 % (Table 2; Fig. 1). No cases of a change of MC2 to MC1 or a disappearing MC were observed.
Table 2.
Evolution of the Modic changes (MC) in the cervical spine over time
| MC natural course | No. of segments affected | Average time between the exams (range) |
|---|---|---|
| New MC1 | 14 seg. | 2.4 years or 883 days (170–2,920 days) |
| New MC2 (no MC on baseline [17]) | 8 seg. | 5.0 years or 1,853 days (850–2,920 days) |
| Change of MC1 to MC2 | 12 seg. | 3.1 years or 1,123 days (110–2,800 days) |
| Change MC2 to MC1 | None | – |
| Disappearing MC1 | None | – |
| Disappearing MC2 | None | – |
A total of 64 patients or 256 motion segments (C3/4, C4/5, C5/6 and C6/7) were considered in the evaluation. Average period between the exams for the whole study sample: 2.5 years or 925 days (7–2,920 days). Mean patients’ age: 61.2 years (50–83), M:F = 37:27
MC1 Modic Changes type 1, MC2 Modic Changes type 2, seg. motion segments in the cervical spine, MRI magnetic resonance imaging
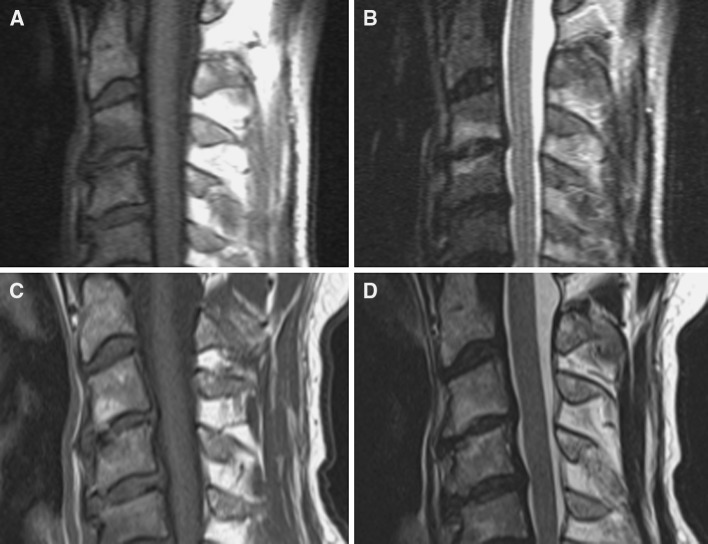
Fig. 1.
a, b Baseline MRI [17]: endplate marrow changes Modic type 1 in the motion segment C3/4 presented as low signal in T1-weighted and high signal in T2-weighted sequences. c, d Follow-up MRI of the same patient shows the evolution of Modic change type 1 to type 2 seen as high signal in both T1- and T2-weighted sequences
The average time between MR examinations in the subgroup with the new MC1 was 2.4 years. In the subgroup of new MC2 the average time between MRI was much longer with an average of 5.0 years and in the subgroup with change of MC1 to MC2 the average time between MRI examinations was 3.1 years (Table 2).
Discussion
The present study reported here is one of the first to describe the natural course and development of MC over time in the cervical spine in symptomatic patients. This occurred as the follow-up study to a larger prevalence and reliability study performed previously [17]. Between the baseline and follow-up MR imaging (mean time between the exams 2.5 years) new MC were detected in 22 motion segments (8.6 %). The most common findings observed were the increasing prevalence of MC (both types) over time, the new MC1 and evolution of MC1 to MC2. These results support those reported from several studies conducted on the lumbar spine [1, 5, 12, 14, 19, 21]. No cases were found, however, where previously observed MC in the cervical spine had disappeared or where MC2 converted to MC1 as has been reported in some previous lumbar spine follow-up studies [7, 13, 15, 18].
A previous prospective study conducted in the cervical spine [23] with 497 originally asymptomatic healthy volunteers at baseline (mean age 50.5 years) [25] and 223 at follow-up showed an increase in the prevalence of both MC types over time from 4.5 to 13.9 % of subjects. However, there was only a slight increase of MC1 over the time period (seven subjects affected at baseline and nine at follow-up) but a considerable increase of MC2 with 3 subjects affected at baseline and 18 subjects at follow-up. These developments were positively associated with age older than 40 years, male gender and pre-existing vertebral disc degeneration. A long time frame between the two MR examinations (average 11.6 years), a wider range of cervical motion segments evaluated (from C2/3 to C7/Th1, i.e. six segments per patient), the statistical evaluations being performed only with persons and not with the number of motion segments and the fact that at baseline only asymptomatic subjects were included could explain the differences in results between that study and the present study performed with actual neck pain patients. This same group of authors also published a study looking at MC in the cervical spine over a period of 11 years in patients who sustained a whiplash injury [24]. Although there were only four patients (seven motion segments) with MC at baseline, 11 years later all of these MC had disappeared and those MC that were visualized (only 17 patients) were all new. Thus the natural history of MC could not be explored in that study due to the long time interval between the MRI studies and the few subjects with Modic changes present. The authors reported no link between the MC seen on the follow-up scans and patient symptoms and no significant difference between the prevalence of MC seen in asymptomatic subjects. However, the sample size with MC was very small and not all patients in the whiplash cohort were symptomatic at follow-up. Furthermore, no categorization of the severity of the whiplash associated disorder (WAD) was reported. These authors did however find a link between MC and pre-existing posterior disc protrusion, similar to that reported in our previous study from which the baseline data for this follow-up study were taken [17]. Thus, the fact that our current study had a substantially higher proportion of patients with MC at baseline (37 patients) and follow-up (46 patients), no cases of disappearing MC, and several cases of MC1 changing to MC2 over time, contributes significant information about the likely natural history of this finding. Our study also found interesting differences in the time periods between the appearance of ‘new’ MC1 and ‘new’ MC2 as well as the time period for MC1 to change to MC2. This information was not reported in the two previous studies mentioned above and therefore adds further information on the natural history of MC in the cervical spine.
Another recent study of MRI findings in the cervical spine compared patients with lumbar disc herniation but no neck pain with asymptomatic volunteers [26]. Interestingly patients with lumbar disc herniation had a higher prevalence of disc degeneration in the cervical spine compared to the control group. However, MC were not evaluated in that study.
Little information is currently available on the clinical significance, if any, of MC in the cervical spine other than the link with disc herniation [17, 27]. Some datas are available for the lumbar spine with one study [19] in patients with LBP evaluating MC over a 14-month period in 96 patients (11 endplates, i.e. L1–S1 or 5.5 motion segments). The authors observed a progression of MC1 to MC2 in 40 % of endplates within this short period of time. In addition, the presence of MC1 at both baseline and follow-up was found to be associated with a poor clinical outcome of LBP.
A further study on the lumbar spine [15] reviewed subsequent MRI scans of 49 patients or 245 motion segments (five segmental levels per patient) with a mean age of 42.6 years and an average time of 2 years between the exams. Of the 36 motion segments with MC1 seen at baseline 13 progressed to MC2, 3 progressed to MC3 and two reverted back to normal. Of the 22 segments with MC2 at baseline, none progressed to MC3 and four reverted back to MC1. One noticeable difference between studies evaluating the course of MC over time in the lumbar spine compared to the studies in the cervical spine is that neither the previous cervical spine study [23] nor this current study found that MC in the cervical spine either disappeared or reverted to an earlier type. This may be due to the relatively small sample sizes however.
Limitations
The lack of a standardized and consistent time period between the baseline and follow-up MRI (mean time 2.5 years) likely influenced the results obtained in this study. The considerably longer average time between the baseline and the follow-up exam in the subgroup of patients with the development of new MC2 (5 years) compared to the patients with new MC1 (2.4 years) or MC1 converting to MC2 (3.1 years) suggests that new MC1 likely developed in some patients, but were not detected prior to their change into MC2 due to a longer time between the examinations. This hypothesis is supported by research on MC in the lumbar spine. MC are likely to develop over time and therefore represent different stages of a degenerative process, which is progressive. MC1 tends to precede MC2 whereas MC2 tends to be more stable [1, 8, 15, 18]. Modic et al. [1] reported that the natural course of MC1 in the lumbar spine is to convert to MC2 over a time period of 13–36 months.
In this current study, we have only considered patients over 50 years of age based on the evidence from research on the lumbar spine indicating that degenerative changes detected on imaging are more prevalent with advancing age [10, 12, 27, 28]. Therefore, it is likely that the prevalence of particularly MC1 reported here for this older population does not accurately reflect what may be found if a wider age group had been included. The prevalence of MC in the subgroup of patients from the baseline study used for the follow-up study was higher than the prevalence in the whole baseline sample (7.4 % of segments with MC1 in the subgroup and 4.3 % in the whole sample at baseline with 14.5 % of segments with MC2 in the subgroup and 10.1 % in the whole sample). Perhaps those patients who underwent a follow-up MR examination were more likely to have worse symptoms and more advanced degeneration compared to the patients who did not have a further MRI. Further studies evaluating whether or not there is a link between MC in the cervical spine and patient symptomatology are needed.
A further major limitation may be the selection bias, since out of 426 symptomatic patients from the baseline examination only 76 had a follow-up MRI examination (average 2.5 years). This small percentage of only 18 % may be because some of these patients did not seek further treatment, applied to another institution, or had symptoms that improved with treatment and thus did not require further imaging. For this part of the original sample the prevalence and course of MC could not be assessed.
Another limitation is the lack of a control group of asymptomatic subjects with which to compare the prevalence and natural history of MC. However, the purpose of this study was to follow the protocol of similar studies published on MC in the lumbar spine [14].
Conclusions
Modic changes in the cervical spine are a dynamic phenomenon similar to the lumbar spine. The appearance of new MC1 and the conversion of MC1 to MC2 over time were the most common patterns observed in those patients with MC. No cases of disappearing MC or conversion of MC2 to MC1 were observed. Follow-up studies with a larger sample of patients should be conducted to clarify whether or not the prevalence of the various MC in the cervical spine is linked with symptoms or is prognostic of treatment outcomes as is being done in the lumbar spine [9–11, 13, 27].
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. Because this was a retrospective study using data routinely collected, and because patients signed informed consent prior to their procedures, specific ethics approval for this study was not required according to a waiver issued by the ethics committee.
Conflict of interest
None.
References
- 1.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 2.Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168:177–186. doi: 10.1148/radiology.168.1.3289089. [DOI] [PubMed] [Google Scholar]
- 3.Ross JS, Modic MT. Current assessment of spinal degenerative disease with magnetic resonance imaging. Clin Orthop Relat Res. 1992;279:68–81. [PubMed] [Google Scholar]
- 4.Chung CB, Vande Berg BC, Tavernier T, Cotten A, Laredo JD, Vallee C, Malghem J. End plate marrow changes in the asymptomatic lumbosacral spine: frequency, distribution and correlation with age and degenerative changes. Skeletal Radiol. 2004;33:399–404. doi: 10.1007/s00256-004-0780-z. [DOI] [PubMed] [Google Scholar]
- 5.Mitra D, Cassar-Pullicino VN, McCall IW. Longitudinal study of vertebral type-1 end-plate changes on MR of the lumbar spine. Eur Radiol. 2004;14:1574–1581. doi: 10.1007/s00330-004-2314-4. [DOI] [PubMed] [Google Scholar]
- 6.Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]
- 7.Kerttula L, Luoma K, Vehmas T, Gronblad M, Kaapa E. Modic type I change may predict rapid progressive, deforming disc degeneration: a prospective 1-year follow-up study. Eur Spine J. 2012;21:1135–1142. doi: 10.1007/s00586-012-2147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braithwaite I, White J, Saifuddin A, Renton P, Taylor BA. Vertebral end-plate (Modic) changes on lumbar spine MRI: correlation with pain reproduction at lumbar discography. Eur Spine J. 1998;7:363–368. doi: 10.1007/s005860050091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. Eur Spine J. 2006;15:1312–1319. doi: 10.1007/s00586-006-0185-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17:1407–1422. doi: 10.1007/s00586-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahme R, Moussa R. The modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. AJNR Am J Neuroradiol. 2008;29:838–842. doi: 10.3174/ajnr.A0925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang YH, Zhao CQ, Jiang LS, Chen XD, Dai LY. Modic changes: a systematic review of the literature. Eur Spine J. 2008;17:1289–1299. doi: 10.1007/s00586-008-0758-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuisma M, Karppinen J, Niinimaki J, Ojala R, Haapea M, Heliovaara M, Korpelainen R, Taimela S, Natri A, Tervonen O. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine (Phila Pa 1976) 2007;32:1116–1122. doi: 10.1097/01.brs.0000261561.12944.ff. [DOI] [PubMed] [Google Scholar]
- 14.Jensen TS, Bendix T, Sorensen JS, Manniche C, Korsholm L, Kjaer P. Characteristics and natural course of vertebral endplate signal (Modic) changes in the Danish general population. BMC Musculoskelet Disord. 2009;10:81. doi: 10.1186/1471-2474-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutton MJ, Bayer JH, Powell JM. Modic vertebral body changes: the natural history as assessed by consecutive magnetic resonance imaging. Spine (Phila Pa 1976) 2011;36:2304–2307. doi: 10.1097/BRS.0b013e31821604b6. [DOI] [PubMed] [Google Scholar]
- 16.Peterson CK, Humphreys BK, Pringle TC. Prevalence of Modic degenerative marrow changes in the cervical spine. J Manipulative Physiol Ther. 2007;30:5–10. doi: 10.1016/j.jmpt.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Mann E, Peterson CK, Hodler J. Degenerative marrow (Modic) changes on cervical spine magnetic resonance imaging scans: prevalence, inter- and intra-examiner reliability and link to disc herniation. Spine (Phila Pa1976) 2011;36:1081–1085. doi: 10.1097/BRS.0b013e3181ef6a1e. [DOI] [PubMed] [Google Scholar]
- 18.Kuisma M, Karppinen J, Niinimaki J, Kurunlahti M, Haapea M, Vanharanta H, Tervonen O. A three-year follow-up of lumbar spine endplate (Modic) changes. Spine (Phila Pa 1976) 2006;31:1714–1718. doi: 10.1097/01.brs.0000224167.18483.14. [DOI] [PubMed] [Google Scholar]
- 19.Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Jensen TS, Manniche C. Is the development of Modic changes associated with clinical symptoms? A 14-month cohort study with MRI. Eur Spine J. 2012 doi: 10.1007/s00586-012-2309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keller A, Boyle E, Skog TA, Cassidy JD, Bautz-Holter E. Are Modic changes prognostic for recovery in a cohort of patients with non-specific low back pain? Eur Spine J. 2012;21:418–424. doi: 10.1007/s00586-011-1964-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albert HB, Manniche C. Modic changes following lumbar disc herniation. Eur Spine J. 2007;16:977–982. doi: 10.1007/s00586-007-0336-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elfering A, Semmer N, Birkhofer D, Zanetti M, Hodler J, Boos N. Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine (Phila Pa 1976) 2002;27:125–134. doi: 10.1097/00007632-200201150-00002. [DOI] [PubMed] [Google Scholar]
- 23.Matsumoto M, Okada E, Ichihara D, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Takahata T. Modic changes in the cervical spine: prospective 10-year follow-up study in asymptomatic subjects. J Bone Joint Surg Br. 2012;94:678–683. doi: 10.1302/0301-620X.94B5.28519. [DOI] [PubMed] [Google Scholar]
- 24.Matsumoto M, Ichihara D, Okada E, et al. Modic changes of the cervical spine in patients with whiplash injury: A prospective 11-year follow-up study. Injury. 2012 doi: 10.1016/j.injury.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yabe Y, Shiga H. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80:19–24. doi: 10.1302/0301-620X.80B1.7929. [DOI] [PubMed] [Google Scholar]
- 26.Okada E, Matsumoto M, Fujiwara H, Toyama Y. Disc degeneration of cervical spine on MRI in patients with lumbar disc herniation: comparison study with asymptomatic volunteers. Eur Spine J. 2011;20(4):585–591. doi: 10.1007/s00586-010-1644-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marchiori DM, Henderson CN. A cross-sectional study correlating cervical radiographic degenerative findings to pain and disability. Spine (Phila Pa 1976) 1996;21:2747–2751. doi: 10.1097/00007632-199612010-00007. [DOI] [PubMed] [Google Scholar]
- 28.Peterson C, Bolton J, Wood AR, Humphreys BK. A cross-sectional study correlating degeneration of the cervical spine with disability and pain in United kingdom patients. Spine (Phila Pa 1976) 2003;28:129–133. doi: 10.1097/00007632-200301150-00007. [DOI] [PubMed] [Google Scholar]