Abstract
Malignant melanoma is a highly metastatic cancer that bears responsibility for the majority of skin cancer-related deaths. Amidst the research efforts to better understand melanoma progression, there has been increasing evidence that hints at a role for a subpopulation of virulent cancer cells, termed malignant melanoma stem or initiating cells (MMICs), in metastasis formation. MMICs are characterized by their preferential ability to initiate and propagate tumor growth and their selective capacity for self-renewal and differentiation into less tumorigenic melanoma cells. The frequency of MMICs has been shown to correlate with poor clinical prognosis in melanoma. Additionally, MMICs are enriched among circulating tumor cells (CTCs) in the peripheral blood of cancer patients, suggesting that MMICs may be a critical player in the metastatic cascade. Although these links exist between MMICs and metastatic disease, the mechanisms by which MMICs may advance metastatic progression are only beginning to be elucidated. Recent studies have shown that MMICs express molecules critical for hematopoietic cell maintenance and trafficking, providing a possible explanation for how circulating MMICs could drive melanoma dissemination. We therefore propose that MMICs might fuel melanoma metastasis by exploiting homing mechanisms commonly utilized by hematopoietic cells. Here we review the biological properties of MMICs and the existing literature on their metastatic potential. We will discuss possible mechanisms by which MMICs might initiate metastases in the context of established knowledge of cancer stem cells (CSCs) in other cancers and of hematopoietic homing molecules, with a particular focus on selectins, integrins, chemokines, and chemokine receptors known to be expressed by melanoma cells. Biological understanding of how these molecules might be utilized by MMICs to propel the metastatic cascade could critically impact the development of more effective therapies for advanced disease.
Keywords: Melanoma, Tumor Initiating Cell, Cancer Stem Cell, ABCB5, CD271, Metastasis, Homing, Dissemination, Circulating Tumor Cell, Hematopoietic Cell Mimicry, Trafficking, Progression, Integrins, Selectins, Chemokines, Chemokine Receptors, Rolling, Adhesion
Introduction
Melanoma, a malignant tumor of the pigment-producing melanocytes, is one of the most aggressive types of skin cancer (1). Although it accounts for less than 5% of all skin cancers, melanoma is responsible for the majority of skin cancer-related deaths. It is the 5th most common cancer in men and the 6th most common in women (2). The incidence of melanoma has continued to rise in the past 30 years (2). Cutaneous melanoma is curable with surgical excision in its earliest stages, but its marked metastatic potential and its resistance to current treatments pose a therapeutic challenge to clinicians. The 5-year survival rate is only 15% for distant metastasis, improved only slightly from 12% in the past decade (3).
Due to the poor prognosis and the lack of effective therapeutic options for patients with metastases, much effort has been made to uncover the etiology and pathogenesis of melanoma. Both environmental factors and genetic susceptibility appear to play a role in disease progression (1). Risk factors for the development of melanoma include sun exposure (4), presence of atypical nevi (5, 6), skin pigmentation phenotype (7), personal (8) and family histories (7) of melanoma.
Research efforts have also yielded substantial information on the molecular pathways involved in melanoma progression. Reportedly, greater than 70% of all cutaneous melanomas have genetic alterations in CDKN2A, a locus on chromosome 9p21 encoding two tumor suppressor proteins, p16, also known as CDK4 inhibitor, and p14ARF (9). Mutations in N-RAS and BRAF, two proteins involved in the MAPK pathway that regulates transcription of genes involved in cell proliferation and survival, are found in 20% (10) and 60% (11) of melanomas, respectively. The most commonly seen BRAF mutation is a substitution of valine with glutamate (V600E). Upregulation of the PI3K pathway and subsequent inhibition of apoptosis are also seen in melanoma (12, 13).
The recent discovery of melanoma susceptibility genes has paved the way for new therapeutic strategies and led to the emergence of various small molecule inhibitors targeted against specific proteins involved in the pathogenesis of melanoma (14). A multicenter phase 3 trial suggested that the BRAF inhibitor, vemurafenib, might extend survival in patients with advanced disease harboring the V600E mutation (15). Trametinib, a small molecule inhibitor of MEK1 and MEK2, which are downstream of BRAF in the MAP kinase pathway, was shown to be comparable to vemurafenib in prolonging progression-free survival and overall survival rates in a phase 3 randomized controlled trial (16).
An alternative therapeutic approach stems from the observed phenomenon of melanoma to trigger antitumor immune responses. For instance, cytotoxic T-cells and antibodies directed against tumor-associated antigens (TAAs) have been detected in patients with melanoma (17). Some of the TAAs that are recognized by cytotoxic T-cells include tyrosinase, gp100, MART-1 (melanoma antigen recognized by T-cells), tyrosinase-related protein-1 (TRP-1) and TRP-2. Despite evidence of antitumor immunity, the overwhelming majority of melanoma patients continue to experience advancement of their disease, which suggests that melanoma cells evade immunologic clearance (18).
Accordingly, a major strategy in the efforts to develop effective melanoma therapies has been to modulate the antitumor immune response, either nonspecifically or by targeting negative regulators of the immune system, called immunologic checkpoints (19). Systemic therapies with nonspecific immune-stimulating agents such as high-dose interferon (IFN) and interleukin-2 (IL-2) have been utilized, along with the chemotherapeutic drug dacarbazine, with improvements in survival rates in some patients (15, 20–22). In an effort to take a more directed approach to boost the immune system, ipilimumab became the first FDA-approved antibody-based immune therapy for melanoma. By binding to the immunologic checkpoint CTLA-4 (cytotoxic T-lymphocyte–associated antigen 4) on tumor-reactive cytotoxic T-lymphocytes (CTLs), ipilimumab potentiates antitumor immunity and has been shown to increase survival in patients with treatment-refractory metastatic disease (23). Promising additional melanoma therapies that similarly attempt to target negative immune regulators are currently in development, including monoclonal antibodies directed against programmed death-1 (PD-1) (24–26), an inhibitory receptor on activated T-cells, and its ligand, PD-L1 (27).
Despite these numerous advances in the treatment of metastatic disease, responses to the existing immunotherapeutic agents have not been consistent, predictable or durable in many cases (19). Furthermore, resistance to therapy is a major issue, and thus, patients with advanced melanoma continue to experience marked mortality rates. Elucidating the mechanism of metastasis will be necessary to alter the disease course and improve survival in this group of patients (28). A topic of growing interest that may generate new insights into the pathogenesis of melanoma metastasis is the emerging cancer stem cell (CSC) field. CSCs are tumor subpopulations in which clinical virulence resides as a consequence of their unlimited capacity to proliferate, self-renew, and differentiate into more mature tumor populations to sustain robust tumor progression (29). CSCs, also known as tumor-initiating cells (TICs), have been identified in hematologic malignancies and numerous solid tumor entities (30), including human malignant melanoma (31–33). Importantly, CSC frequency correlates with neoplastic progression (31), metastatic potential (32, 33) and worse prognosis (33) in melanoma patients. Additionally, proof-of-principle of CSC targeting and consequent inhibition of melanoma growth has been established (31). Therefore, further study of the CSC population may provide a novel direction in the path towards enhancing our basic understanding of melanoma metastasis, yielding new insights for the development of more effective therapies for advanced disease.
In the following sections we will critically review the emerging literature on malignant melanoma initiating cells (MMICs) and their biology. We will elucidate how recently uncovered MMIC pathways may drive melanoma progression in general and, particularly, metastatic dissemination. Specifically, we will juxtapose known MMIC immunobiological functions against current understanding of homing mechanisms described for hematopoietic cells and other cancers. We propose that MMICs might highjack the leukocyte trafficking machinery to disseminate to metastatic target tissues.
Cancer Stem Cells – Defining Characteristics
The presence of phenotypic variability within malignancies has been well documented (28). Several major theories exist to explain this occurrence of tumor heterogeneity. For example, the prevailing stochastic theory proposes that all malignant cells have equal tumorigenic potential and give rise to a structurally heterogeneous tumor by acquiring various genetic alterations (34). By contrast, the CSC theory postulates that CSCs generate cancer heterogeneity via their selective ability to maintain tumor growth by generating more copies of themselves while at the same time giving rise to the heterogeneous bulk of the tumor through a process termed differentiation (29). These seemingly opposing theories are, however, not mutually exclusive, as stochastic mechanisms have been described within the CSC population, which can exhibit varying degrees of self-renewing and tumorigenic potential within any given tumor (35, 36).
The consensus definition of a CSC consists of the following three characteristics: (i) its preferential ability to initiate tumor growth, (ii) its capacity to self-renew (i.e. generate more copies of itself), and (iii) its ability to differentiate into tumor cells comprising the bulk of the tumor that have a more limited tumorigenic capacity (29, 30) (Fig. 1). Traditionally, xenotransplantation of a marker-defined subpopulation of tumor cells derived from clinical specimens into immunocompromised mice (typically non-obese diabetic (NOD) severe combined immunodeficiency (SCID) mice) at limiting dilution has been required to functionally verify these CSC-defining traits (37). Preferential tumor growth compared to marker-negative tumor bulk populations and recapitulation of the original patient tumor heterogeneity are considered evidence of CSC maintenance and differentiation (37). Serial in vivo passaging into secondary and sometimes tertiary recipient mice is thereby used to demonstrate long-term self-renewal and tumor-propagating ability (37). In vitro methodologies for the characterization of CSCs, including sphere formation assays, are only acceptable as surrogate CSC assays upon in vivo verification of CSC properties for a given population expressing the putative CSC marker being tested (37, 38). More recently, in an alternative approach, genetic lineage-tracing studies have more firmly established the existence of CSCs, by enabling side-by-side comparisons of tumor-initiating ability, self-renewal, and differentiation of genetically labeled CSCs versus tumor bulk populations (31, 39). Additionally, recent experiments utilizing lineage-tracing methods to study unperturbed tumorigenesis in murine cancer models have also confirmed long-term self-renewal and selective tumorigenic capability of CSCs in vivo in the native microenvironment of the tumor, further solidifying the CSC theory (40–42).
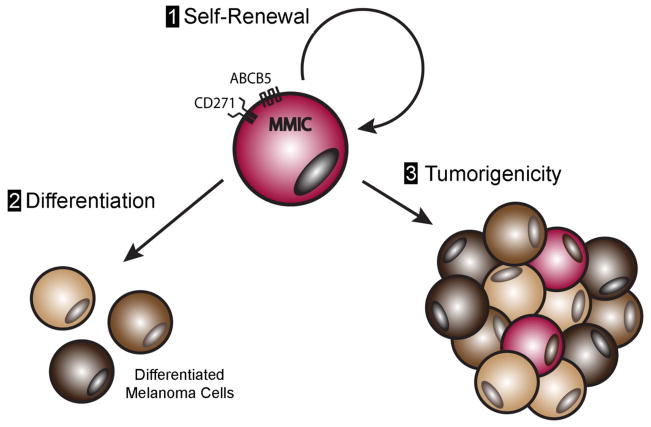
Figure 1. Defining characteristics of malignant melanoma-initiating cells (MMICs).
MMICs can be distinguished from the bulk of the melanoma cells comprising the tumor by their preferential display of three defining traits: (1) long-term self-renewal, (2) differentiation into heterogeneous tumor cells, and (3) enhanced tumorigenic growth. ATP-binding cassette member B5 (ABCB5) and nerve growth factor receptor (NGFR, also known as CD271) have been established as MMIC markers based on in vivo confirmation of these three defining characteristics.
Despite the accumulating body of evidence in support of the CSC theory, there is significant controversy surrounding certain aspects. One topic of debate arises from confusion regarding the definition of CSCs and their relationship to physiologic stem cells. It must be noted that the consensus definition of CSCs does not implicate physiologic stem cells as the origin of CSCs (37). Although cancers emerging from adult tissue stem cells undergoing malignant transformation have been observed in model organisms (43, 44), the idea that CSCs must originate from physiologic stem cells is a misconception, as committed progenitor cells have also been shown to acquire cancer stem-like properties upon malignant transformation (45). Instead, CSCs must be distinguished from the bulk population by experimental characterization of their defining functional properties.
Another point of disagreement stems from the assumption that CSCs are a constant population at the apex of a hierarchically organized tumor. Experiments have shown that malignant cells lacking self-renewal potential can undergo de-differentiation into a CSC-like phenotype depending on cues from the surrounding microenvironment (46, 47). However, physiologic cells are similarly modulated to gain stem-like properties by contextual signals from the environment. For example, progenitor, or transient amplifying (TA), cells can de-differentiate and acquire stem-like properties in physiologic tissues (48). Just as this observed phenomenon does not invalidate the hierarchical organization of physiologic tissues, the plasticity of CSCs should not undermine the CSC hypothesis, given that CSCs can be distinguished from the bulk population at any time point in a given tumor.
Some investigators, operating under the assumption that CSCs should be a rare subset mimicking the frequency of physiologic stem cells in healthy normal tissues, have presumed the high frequency of CSCs seen in certain tumors as evidence against the CSC concept (49). In fact, the proportion of CSCs may vary depending on tumor type, the stage of the tumor, and the microenvironment (50). This is in line with the increase in the number of physiologic stem cells in response to injury (51). Furthermore, differences in the experimental conditions, the model organism and the methods utilized to isolate CSCs and measure CSC frequency may also affect their quantification (33, 52, 53). Certain animal models (e.g. NOD/SCID IL-2Rγ−/− (NSG) mice) may inherently not be conducive to accurately studying CSC biology, because they cannot re-establish the original patient tumor heterogeneity (33, 54). Moreover, enzymatic digestion protocols utilized for CSC isolation were found to cleave CSC surface antigens, thereby producing false CSC marker negativity (33, 54). Therefore, CSC frequencies should be analyzed relative to the model system in which a given malignancy is studied, with special attention to the experimental methodologies used (55).
Despite these controversies, the CSC field is highly studied because of its implications for therapy. Specifically, the CSCs’ preferential ability to initiate and maintain tumorigenic growth would predict that novel therapeutic modalities targeting these aggressive cancer cell fractions, in addition to tumor bulk populations with limited proliferative ability, could result in more durable responses in cancer patients. Meanwhile, several pathways and biological mechanisms underlying CSC-driven tumor growth have been unraveled, including their preferential ability to promote tumor vascularization (56–59), survive cytotoxic therapy (60–63), persist in hostile tumor environments (64, 65), and evade antitumor immune responses (66–70). Accordingly, it stands to reason that the diverse functions of CSCs that appear to give a selective growth advantage to various malignancies, make CSCs an important focus of further studies in cancer biology. The following section will elaborate on melanoma CSCs, also known as MMICs, and their immunobiology, with a particular emphasis on their potential involvement in the metastatic cascade.
Malignant Melanoma Initiating Cells: Identifying Traits and Role in Tumorigenesis
Melanoma, with its marked resistance to conventional chemotherapy and highly aggressive behavior, has been hypothesized for some time to follow the CSC model of tumor initiation and growth (71, 72). Initial evidence supporting this hypothesis was provided when it was discovered that a subset of chemoresistant cells in melanoma cultures and in clinical melanoma biospecimens overexpressed a number of stem cell markers, including CD133 (73). Additional evidence was provided by the preferential in vitro clonogenic capacity of melanoma cells expressing CD20 (Table 1), a marker of mature B cells, as well as the in vivo preferential ability to form tumors in immunodeficient mice (74). In a separate study, CD133+ melanoma cells were shown to have an enhanced capability to initiate primary tumors in NOD/SCID mice compared to CD133− melanoma cells (75). However, the authors did not perform serial xenotransplantation experiments to confirm long-term self-renewal of CD133+ melanoma subsets (75) (Table 1). The same group also reported preferential expression of the chemoresistance determinant ABCG2 by CD133+ fractions but failed to prospectively isolate and ascribe CSC-defining traits to ABCG2-purified melanoma subpopulations (Table 1). Taken together, however, both studies suggested that melanoma did indeed comprise of functionally distinct subpopulations with varying tumorigenic capacities.
Table 1.
Confirmed and candidate MMIC markers
| MMIC marker | Function | Study | Frequency in primary melanoma | Preferential Tumor Initiation | Long- term Self- renewal | Differentiation | Assays | Animal model | Correlation with Progression |
|---|---|---|---|---|---|---|---|---|---|
| ABCB5 | Drug efflux Transporter |
Schatton et al. Nature 2008 Frank et al. Cancer Res 2011 |
1.6–20.4% |
Yes Yes |
Yes NT |
Yes NT |
Serial xenotransplantation In vivo lineage tracking ABCB5 targeting Xenotransplantation* |
NOD/SCID Nude NSG |
Yes N/A |
| NGFR (CD271) | Nerve growth factor receptor |
Boiko et al. Nature 2010 Civenni et al. Cancer Res 2011 |
2.5–41% |
Yes Yes |
Yes Yes |
Yes Yes |
Serial xenotransplantation Serial xenotransplantation Sphere formation** |
Rag2−/−γc−/− NSG NOD/SCID NSG*** |
Yes Yes |
| ALDH | Aldehyde dehydrogenase |
Boonyaratanakornkit et al. JID 2010 Prasmickaite et al. PLoS One 2010 |
2% | Yes No |
Yes NT |
Yes NT |
Serial xenotransplantation Sphere formation** Xenotransplantation* Sphere formation** |
NOD/SCID NSG NSG |
NT NT |
| CD20 | B-cell antigen | Fang et al. Cancer Res 2005 | <2% | Yes | NT | NT | Xenotransplantation* Sphere formation** |
NOD/SCID | NT |
| ABCG2 | Drug efflux transporter | Monzani et al. Eur J Cancer 2007 | NT | NT | NT | NT | NT | N/A | NT |
| CD133 | Unknown | Monzani et al. Eur J Cancer 2007 | <1% | Yes | NT | NT | Xenotransplantation* Sphere formation** |
NOD/SCID | NT |
| PD-1 (CD279) | Immune checkpoint receptor | Schatton et al. Cancer Res 2010 | 3% | Yes | NT | NT | Xenotransplantation* | NOD/SCID | NT |
| B7.2 (CD86) | Costimulatory molecule | Schatton et al. Cancer Res 2010 | 1.8% | Yes | NT | NT | Xenotransplantation* | NOD/SCID | NT |
| JARID1B | H3K4 demethylase | Roesch et al. Cell 2010 | 5–10% | No | NT | NT | Xenotransplantation* Sphere formation** |
NSG | NT |
NT: Not tested
N/A: Not applicable
Bold font: confirmed MMIC marker
Did not perform serial xenotransplantation confirming long-term self-renewal capacity
Not a stand-alone CSC-defining assay
Recapitulation of tumor heterogeneity not fully established
Concrete evidence for the existence of MMICs came with the establishment of ABCB5 as marker of TICs in melanoma (31) (Fig. 1 and Table 1). Compared to ABCB5− bulk melanoma cells, ABCB5+ fractions isolated from patient biopsies showed preferential primary and secondary tumor initiation upon serial xenotransplantation into NOD/SCID mice at limiting dilution (31). In addition, xenotransplantation of ABCB5+ cells, but not ABCB5− cells, resulted in tumors that were phenotypically representative of the original patient tumor heterogeneity, demonstrating the concurrent ability of ABCB5+ subsets to self-renew and, at the same time, differentiate to give rise to ABCB5− tumor cells (31). This result was further confirmed by lineage tracing experiments in which genetically labeled ABCB5+ and ABCB5− melanoma cells were xenotransplanted into NOD/SCID mice. Within the tumors formed, an increased frequency of labeled ABCB5+ cells was observed. Furthermore, in contrast to the ABCB5− cells that gave rise only to ABCB5− progeny, the ABCB5+ cells exhibited the exclusive ability to give rise to both ABCB5+ and ABCB5− progeny (31). Consistent with these findings, induction of terminal differentiation led to a significant downregulation of ABCB5 expression on melanoma cells in a study by Botelho et al. (76), and Oct-4-mediated dedifferentiation of melanoma cells led to increased ABCB5 expression (77). Furthermore, several recent studies showed that ABCB5 frequency correlated with in vitro clonogenic potential of melanoma cells (78–80). Moreover, ABCB5 gene amplification was found to be a predisposing factor to clinical melanoma development (81), further strengthening the support for the role of MMICs in melanoma growth. Additionally, an ABCB5 single nucleotide polymorphism, which encodes a non-synonymous ABCB5 amino acid change (K115E), correlated significantly with decreased melanoma risk in a recent study involving 585 melanoma cases and 605 age-matched controls (82). The ABCB5 K115E polymorphism was further associated with increased pigmentation and impaired ABCB5 transport function, demonstrating for the first time that functional variations in a prospective CSC gene correlate with melanomagenesis (82). ABCB5 has meanwhile also been shown to mark CSCs in other cancers besides melanoma, such as hepatocellular carcinoma (83).
Adding to the compiling evidence for the MMIC model, selective targeting and elimination of ABCB5+ cells via antibody-dependent cell-mediated cytotoxicity using an anti-ABCB5 monoclonal antibody was shown to impair tumor initiation and retard tumor growth in immunodeficient mice xenografted with human melanoma (31). These results not only unequivocally demonstrated that melanoma is a CSC-driven disease, but they also established proof-of-concept for the therapeutic utility of targeting MMICs. Similarly, therapeutic targeting of CD20, a marker previously suggested to be associated with MMICs, though not an unequivocally proven MMIC marker, resulted in inhibition of melanoma growth and recurrence in immunodeficient mouse xenografts (84). The same group reported a case of a metastatic melanoma patient whose metastatic lesions regressed after local treatment of cutaneous lesions with rituximab, a monoclonal antibody directed against CD20 (85). Moreover, in a small pilot trial, treatment with rituximab resulted in prevention of disease recurrence in 5 out of 9 metastatic melanoma patients (86). These findings, taken from studies that employ CSC-associated markers to eliminate a specific subpopulation of melanoma cells, clearly reveal the potential therapeutic relevance of targeting MMICs.
More recently, additional evidence of CSCs in melanoma was provided by the isolation of melanoma subsets expressing Nerve Growth Factor Receptor (NGFR), also known as CD271 (Table 1). Boiko et al. (32) demonstrated preferential tumor formation by CD271+ melanoma cells isolated from patient samples in serial xenotransplantation experiments using Rag−/−γc−/− mice. In addition, they achieved similar results in a more physiologic context by serial xenotransplantation of CD271+ melanoma cells or CD271− melanoma cells into human skin or bone engrafted onto Rag−/−γc−/− or NSG mice (32). Consistent with these findings, Civenni and colleagues showed that only the CD271+, but not CD271−, melanoma cells met all three criteria of the CSC definition in serial xenotransplantation assays utilizing nude and NOD/SCID mice, and NSG mice to a lesser degree; they were capable of tumor initiation, establishment of the original tumor heterogeneity, and long-term self-renewal (33). Unsurprisingly, given these results, Frank et al. found preferential coexpression of ABCB5 and CD271 on clinical melanoma specimens (57). Lastly, another molecule investigated for its potential as an MMIC marker is aldehyde dehydrogenase (ALDH), a detoxifying enzyme, the expression of which has been proposed to identify CSCs in breast (87), colon and many other cancers (88). Melanoma populations with high ALDH activity were found to be enriched with tumorigenic cells capable of prolonged self-renewal capacity in both NOD/SCID (89, 90) and NSG mice (89). However, in another study, ALDH+ melanoma cells were found to have similar tumorigenic potential compared to ALDH− cells in xenograft assays using NSG mice (91), calling into question the validity of ALDH as a universal MMIC marker (Table 1). Another marker implicated in melanoma tumorigenesis is the member of the family of jumonji/ARID1 (JARID1) histone 3 K4 demethylases, JARID1B, a protein involved in positive cell cycle control in melanoma (92). In a study by Roesch and colleagues, JARID1B marked a subpopulation of slow-cycling melanoma cells that were found to be crucial for long-term tumor growth (93). However, whether this marker coincides with MMICs was not addressed in this study (Table 1).
Some have questioned the existence of MMICs based on studies showing a generally high frequency of tumorigenic cells in melanoma and an apparent lack of association between tumorigenicity and CSC marker positivity (49, 54, 83). Quintana et al. (49) reported that an average of 1 in 4 melanoma cells isolated from patient tumors was able to form tumors in NSG mice, and therefore, interpreted that melanoma was not a cancer that followed the CSC model, based on the observed finding of low frequencies of physiologic stem cells present in the human body. In a follow-up study, the group reported no differences in tumorigenic capacity of melanoma cells in xenotransplantation assays into NSG mice when comparing ABCB5+ versus ABCB5− cell subsets and CD271+ versus CD271− subsets (54). However, these findings were called into question when Civenni et al. found that the tumor dissociation methods utilized in the studies by Quintana et al. to generate single cell suspensions from clinical melanomas cleaved off CSC markers from the cell surface (33). The resultant possible contamination with MMICs of populations thought to be negative for any CSC marker would explain the reported discrepancies in the tumorigenic potential of distinct melanoma subpopulations. Furthermore, it is crucial to note that these studies were performed in NSG mice lacking natural killer (NK) cells. Civenni et al. showed that neither marker-positive nor -negative xenotransplanted cells were able to recapitulate the original tumor heterogeneity, making NSG mice an unfit model for accurately studying the CSC-defining traits of self-renewal and differentiation (33). In addition, CSC marker-negative melanoma cells were able to initiate tumor growth in only the NSG mouse model, whereas CSC marker-positive cells were capable of tumor initiation in all immunodeficient mouse models tested (33). When scrutinized in the context of mouse models that eliminate confounding factors that may be involved in the study of CSC biology, CD271 was shown to mark a subpopulation of melanoma cells that were not only more tumorigenic than the CD271− tumor bulk, but also capable of long-term self-renewal and recapitulation of the heterogeneous composition of the original patient tumor (33).
Biological Properties of Malignant Melanoma Initiating Cells
Along with the advent of methods allowing for the identification of MMICs came the discovery of other biological capabilities specifically associated with these virulent tumor cell subsets. In other cancers, CSCs have been shown to preferentially induce neovascularization to promote tumor growth (56). There is evidence to suggest that this may also be the case in melanoma, as MMICs preferentially express vasculogenic differentiation markers, VE-cadherin and TIE-1 (31), as well as VEGFR-1 (57), and have been shown to play a crucial role in the phenomenon of “vasculogenic mimicry” (94, 95) and resultant tumor growth in a VEGFR-1-dependent manner in mouse xenografts (57). Of note, in agreement with the established association of MMICs with clinical melanoma progression (31, 33, 96), these vasculogenic differentiation markers may also be involved in promoting metastasis formation. For example, TIE-1 has been previously associated with the metastatic phenotype of melanoma cells (97), and a separate group reported TIE-1 and VE-cadherin overexpression in highly invasive melanoma cells (98). In addition, VEGFR-1 expressed by hematopoietic progenitor cells was found to be critical in the formation of pre-metastatic niches, and antibody blockade of VEGFR-1 prevented melanoma metastasis in a mouse model (99). However, the exact functional roles that these markers have in propagating melanoma metastasis remains to be elucidated. Lastly, preferential activation in MMICs of NRAS, an oncogene involved in the activation of the ERK/AKT pathway, may yet be another mechanism by which MMICs facilitate tumor initiation and growth via the involvement of RNA helicase HAGE (100).
Meanwhile, other attributes of MMICs have also been discovered that may elucidate the mechanisms underlying the enhanced capability of MMICs to persist in the human host, including their ability to evade and actively suppress the host antitumor immune response. Initial evidence pointing to the favorable immunophenotype of MMICs was provided by findings of decreased MHC class I antigen expression (66) and downregulation of various TAAs on the cell surface of MMICs vis-à-vis melanoma bulk populations (32, 66). In a subsequent study, the immune-evasive behavior of MMICs was further demonstrated when melanoma cells, induced by tumor necrosis factor alpha (TNF-α) to dedifferentiate and exhibit a stem-like phenotype, as signified by an increased expression of CD271, were less susceptible to killing by cytotoxic T lymphocytes (101). MMICs have also been found to actively modulate the antitumor immune response when compared to their bulk tumor counterparts. For example, MMICs have been shown to inhibit IL-2 production and increase production of the immunosuppressive cytokine, IL-10, leading to decreased T cell proliferation (66). Additionally, MMICs were found to preferentially express coinhibitory molecules, including PD-1 and B7.2, and induced regulatory T cells to promote immunogenic tolerance in a B7.2-dependent manner (66).
Given their expression of the drug efflux transporter, ABCB5 (31, 73, 102), MMICs have not surprisingly been implicated in drug resistance. Indeed, an increase in the frequency of ABCB5+ MMICs is found in vitro and in mouse xenografts after treatment with chemotherapeutics (103). Furthermore, tissue sampled from metastases of treated melanoma patients are enriched in ABCB5+ cells compared to pre-chemotherapy specimens (103, 104). Efflux of standard-of-care agents by ABCB5 is one proposed mechanism of MMIC chemoresistance (73, 102). Similarly, the association of treatment resistance and CSC frequency is present in many types of cancers, such as breast cancer (62, 105), glioblastoma (60, 106), hepatocellular carcinoma (83) and colorectal carcinoma (63), where ABCB5 was also determined to be a mechanism of resistance.
Melanoma Metastasis: Contribution of MMICs?
Of great clinical importance, ABCB5 frequency directly correlates with disease progression in melanoma (31). Since this initial finding, multiple studies have confirmed ABCB5 as a progression marker in clinical melanoma specimens as well as in animal models (96, 107–109). Similarly, CD271 expression was found to significantly correlate with increased metastatic burden and poor tumor-specific survival in melanoma patients (33). ABCB5 also correlates with adverse clinical outcomes and worse prognosis in other cancers (83, 110). In addition, the importance of ABCB5 in cancer progression is underlined by the finding of increased ABCB5 mutation frequency in smokers with non-small cell lung carcinoma versus non-smokers (111).
Further suggestive of a role of MMICs in disease advancement, compared to CD271− cells, patient-derived CD271+ melanoma subpopulations were shown to preferentially metastasize to the liver and lungs in a mouse xenograft model (32). Moreover, circulating tumor cells (CTCs) were found in a separate study to express elevated levels of MMIC markers (112–114). CTCs are the rare populations of malignant cells that have been found in the peripheral blood of patients with various cancers, including malignant melanoma. The presence of CTCs correlates significantly with metastatic progression in both animal models and in advanced melanoma patients (112, 114, 115). However, it remains unclear if all or only a subset of CTCs can trigger metastasis formation. Mouse xenotransplantation experiments by Ma et al. revealed that CTCs bear the ability to initiate primary tumor and metastasis formation in secondary recipients and that ABCB5+ cells were enriched within the population of melanoma CTCs (112). Furthermore, Kupas et al. showed that specifically, ABCB5+ CTCs, isolated from metastatic melanoma patients, were more tumorigenic in vivo, when compared to ABCB5− CTCs (113). In a separate study, the use of ABCB5 and CD271 in addition to melanoma differentiation antigens maximally enriched for CTCs from patient samples compared to the use of melanoma differentiation antigens alone (116). Though these previous studies are highly suggestive of a possible role of MMICs in promoting metastasis, mechanistic insights into how MMICs may fuel metastatic progression are still lacking.
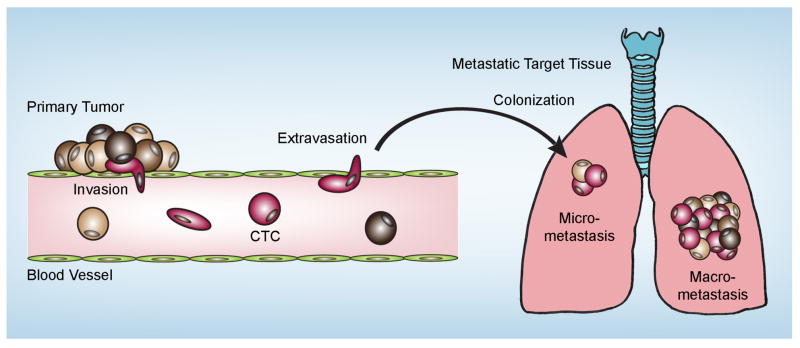
Although metastatic disease is the leading cause of cancer-related deaths (117) and a significant contributor to the high mortality rates seen in melanoma, the mechanisms involved in the complex process of metastasis development, termed the “invasion-metastasis cascade,” are still poorly understood. The “invasion-metastasis cascade” can be dissected into multiple steps (118), whereby melanoma cells (i) dissociate from the primary tumor, undergo local invasion into the dermal stroma and breach the basement membrane, (ii) intravasate into lymphatic or blood microvessels, (iii) are transported as CTCs to other organs, (iv) arrest on microvessels within the target tissue, (v) extravasate into the tissue parenchyma forming dormant micrometastases and (vi) proliferate further, forming macrometastases (119) (Fig. 2). Though conventional wisdom states that metastasis formation is an event that is triggered later in the disease process, at more advanced stages (120), recent evidence is suggestive of tumor dissemination transpiring at even the earliest of stages, perhaps occurring concomitantly with primary tumor formation (121, 122). CTC studies appear to support this newer line of thinking. For example, Reid et al. were able to detect CTCs in the blood of early stage (stage 0–II) melanoma patients (114). Because of the therapeutic and prognostic implications of detecting early metastasis, characterization of the subset of cells with metastatic capacity that allow for distant seeding in early stages of cancer has become a focus of active research.
Figure 2. Putative role of malignant melanoma-initiating cells (MMICs) in metastatic progression.
In addition to primary tumor formation, increasing evidence suggests that MMICs may play a crucial role in the “invasion-metastasis cascade.” After dissociation from the primary tumor and subsequent intravasation into the blood stream or lymphatic system, MMICs are enriched among circulating tumor cells (CTCs) and may home to distant tissues to promote metastatic seeding and also propagate macrometastasis formation. This would be consistent with the finding of increased MMIC frequencies in metastatic compared to primary melanomas.
Little is known about the role of MMICs in the metastatic process, but given their enhanced tumorigenic capacity, association with tumor progression, and enrichment in the CTC population, MMICs make an attractive candidate in the efforts to identify the cells responsible for initiating metastasis. A small number of studies in breast cancer have suggested a critical role of CSCs in metastasis formation and have actually identified the molecular networks involved in this process. In a mouse breast cancer model, in which spontaneous lung metastasis formation is seen, CSCs were revealed to play a crucial role in initiating metastatic niches via induction of periostin expression and subsequent recruitment of wnt ligands by stromal cells at metastatic loci, leading to CSC-driven metastatic expansion (123). Along the same line but utilizing breast cancer patient-derived CTCs, a recent study by Trumpp et al. showed that expression of CD44, a breast CSC marker, as well as MET and CD47 represented a subpopulation of CTCs capable of initiating metastasis in an NSG mouse model, providing a functional link between CSC phenotype and metastatic progression in the form of specific cell surface proteins expressed by CSCs (124). Furthermore, similar to the known correlation between CSC frequencies and poor clinical outcomes in other cancers (33, 83, 110), the frequency of CD44+MET+CD47+ CTCs correlated with disease stage in breast cancer patients (124). These studies in the breast cancer field, though few in number, have begun the process of dissecting the mechanism of metastasis initiation by circulating CSCs.
A major factor that drives metastasis is epithelial-to-mesenchymal transition (EMT), a process seen in normal embryogenesis and adopted by epithelial cancers to acquire a more aggressive phenotype (125). In EMT, polarized epithelial cells lose their associations to the surrounding environment and attain migratory properties of mesenchymal cells. The reversal of EMT, mesenchymal-to-epithelial transition (MET), is the acquisition of an epithelial-like phenotype, a mechanism by which neoplastic cells colonize target tissues. Both EMT and MET involve differential regulation of cell adhesion and cytoskeletal proteins. EMT is closely interrelated to the CSC model, as it may play a role in CSC-driven metastasis (55, 126). For instance, EMT-induced breast cancer cells acquire a stem-like phenotype, and breast CSCs isolated from patients have been found to express EMT-associated markers (127). There is evidence that EMT may also be an important process underlying melanoma progression. Overexpression of SLUG, a transcriptional repressor of proteins involved in cell-to-cell adhesion, was found to induce an EMT-like phenotype and promote melanoma cell migration (128). Additionally, TWIST1, a crucial transcription factor in EMT (129), was shown to be a positive regulator of melanoma invasion in vitro (130). Furthermore, elevated levels of the transcription factor SNAIL as well as fibronectin, an expression profile consistent with a mesenchymal phenotype, were associated with increased melanoma metastases in vivo (131). Because of their intrinsic plasticity, it is not unreasonable to hypothesize that EMT and MET may be utilized by MMICs to promote metastatic spread. However, despite these findings, a molecular explanation for the pro-metastatic behavior of MMICs specifically remains largely unknown, indicating the need for additional functional studies in the melanoma field using mouse models and/or manipulation of MMIC-specific molecular pathways to yield new insights into the mechanisms underlying the invasion-metastasis cascade.
Do MMICs Harness Hematopoietic Homing Molecules to Promote Metastasis?
As noted previously, nearly all patients who succumb to melanoma are killed by metastatic growths which compromise functions in vital organs, notably lymph nodes, liver, lungs and brain (132). These Stage III–IV metastases are virtually guaranteed once melanomas enter the vertical growth phase, exit the epidermis and penetrate a sufficient depth into the dermis (Breslow thickness) (133). Here, melanoma cells enter blood and lymphatic vessels and utilize such conduits to home as CTCs to distant anatomical niches permitting colony formation within favorable microenvironments. Identifying and characterizing the molecular mediators of MMIC and non-MMIC populations at each step of the “invasion-metastasis cascade” is the subject of ongoing investigation.
Given that MMICs have been previously shown to express certain proteins thought to be restricted to lymphocytes, such as the coinhibitory receptor, PD-1, the costimulatory molecule, B7.2 (66), or the B-cell antigen, CD20 (74, 84, 85), we hypothesize that MMICs capable of seeding metastases are adopting certain phenotypic aspects of circulating leukocytes, thereby harnessing their approach to home to specific target tissues. Homing is an active, multistep process that involves leukocyte-endothelial cell interactions with adhesion molecules participating in recognition, adhesion and extravasation of circulating cells into distinct sites (134). Specificity of access to and anchorage in certain extravascular spaces depends on the homing molecules utilized (135). Since cancer cell homing operationally involves steps (iii–v) of the cascade noted above, and CSCs have been shown to express CD44, a glycoprotein involved in cell adhesion and migration (136), this review will focus on the dominant surface adhesive and migratory molecules that might govern MMIC and non-MMIC homing behavior, including selectin-selectin ligands, integrins, and chemokine-chemokine receptors. By drawing parallels from current known homing mechanisms utilized by hematopoietic cells, we elaborate on potential mechanisms by which MMICs may act as drivers of metastasis.
Selectin-Selectin Ligands in Melanoma
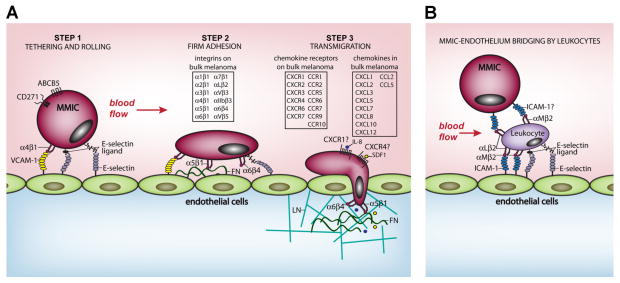
Growing evidence indicates that metastatic melanoma cells along with virtually all types of cancers may hijack and exploit at least some aspect of leukocytic selectin ligand, integrin, and/or chemokine-driven adhesive and migratory mechanisms in a process conceptually termed “leukocyte mimicry” (137, 138) (Fig. 3A). Cancer cell-leukocyte mimicry has been hypothesized to occur via genetic and epigenetic alterations in cancer cells or perhaps via direct fusion of a cancer cell with a leukocyte to form a hybrid cell, often termed the “cancer cell-leukocyte fusion theory of metastasis” (139).
Figure 3. Hypothetical model of malignant melanoma-initiating cell (MMIC) homing and extravasation into secondary tissues.
(A) Step 1: circulating MMICs co-expressing the MMIC markers ABCB5 and CD271 tether and roll in blood flow on microvascular endothelial cells of the metastatic target tissue. MMIC tethering and rolling might involve binding between constitutively active MMIC α4β1 integrin and endothelial VCAM-1 as well as potentially MMIC E-selectin glycoprotein and glycolipid ligands interacting with endothelial E-selectin. Step 2: Rolling MMICs might then transition to firm adherence upon α5β1 integrin (elevated on MMICs) engagement with its major endothelial ligand, fibronectin (FN). Step 3: MMICs might traverse endothelial cell-cell junctions via α5β1 and α6β4 (also elevated on MMICs) binding to putative surface and basement membrane integrin ligands, FN and laminin (LN), respectively. MMIC transendothelial migration might further involve IL-8 and SDF1 binding CXCR1 and CXCR4, respectively, mechanosignaling circuits identified previously in migratory melanoma cells and CSCs in other cancers. Note that several other integrins, chemokine receptors and chemokines identified previously on bulk melanoma cells or CSCs in other cancers yet heretofore not analyzed on MMICs may also contribute to MMIC rolling, firm adhesion and transmigration via activation of integrins or induction of directional movement. Also unclear is the role of β2 integrins in MMIC dissemination. Aside from the aforementioned homing molecules, additional factors may promote MMIC-driven metastasis formation. For instance, vasculogenic markers, including VEGFR-1, VE-cadherin, and TIE-1, known to be preferentially expressed by MMICs, could help foster a metastatic niche and facilitate tumor expansion in the metastatic target tissue. (B) A second possibility in melanoma extravasation involves the contribution of leukocytes, wherein neutrophils are believed to bind melanoma expressed ICAM-1 via αLβ2 and αMβ2 integrins, thereby bridging melanoma cells to the endothelial layer. The neutrophil, anchored to the endothelium via ICAM-1-β2 integrin and E-selectin-E-selectin ligand interactions, as depicted, might then help to drag the melanoma cell through the endothelial layer (not shown). Whether MMICs utilize a similar process is unclear.
Firm attachment on and movement of CTCs through vascular endothelium are key events in melanoma cell egress from the blood into target tissues. Accordingly, these steps are currently under intense scrutiny in the hope of devising potent therapies to block cancer cell extravasation. Increasing evidence has implicated a class of adhesion molecules, selectin-selectin ligands, in cancer cell homing and infiltration into distant sites (140). Selectin-selectin ligands enable leukocytes and, more recently, CTCs to sufficiently anchor to vascular endothelium, thereby overcoming hemodynamic shear forces in the bloodstream in a process termed “rolling” (137). The critical role of selectins in leukocyte homing is aptly illustrated by the genetic disorder, leukocyte adhesion deficiency II (LAD II), in which leukocyte recruitment to sites of chronic infection is impaired secondary to the inherited deficiency of specific ligands needed to recognize selectins (141). Despite their importance, selectins are perhaps the least studied class of homing molecules in cancer to date. Given that cellular rolling is often the first step in tissue colonization, preceding firm adhesion to vascular endothelium and subsequent transendothelial migration, blockade of selectin-selectin ligands represents a possible strategy for therapeutic intervention against cancer cell extravasation.
Endothelial (E)-, platelet (P)-, and leukocyte (L)-selectins comprise the selectin family and are predominantly found on endothelial cells, platelets or leukocytes, respectively. These molecules are responsible for promoting binding interactions with selectin ligands consisting of distinct types of modified sugar groups expressed on select structurally diverse proteins or lipids. E-selectin is particularly important for the capture of circulating leukocytes or CTCs expressing E-selectin ligands from the bloodstream, leading to adhesion and subsequent invasion of CTCs into the extravascular space (137). Tumor cells isolated from subjects with cancer of the colon, prostate, breast, pancreas and lung, have exhibited rolling and adhesive behavior on endothelial monolayers expressing E-selectin (140). In studies of lung cancer, a malignancy that frequently metastasizes to the liver, injection of H59 murine lung cancer cells into mice led to the induction of E-selectin expression on the hepatic sinusoidal endothelium, suggesting a critical role for E-selectin in tumor cell colonization of tissues (142). Interestingly, in this same study, B16 F1 murine melanoma cells also induced E-selectin expression on the sinusoidal endothelium (142). Consistent with these findings, cancer cell homing to tissues has been inhibited with anti-E-selectin antibodies in multiple studies performed in experimental models (137, 142–144). In addition to E-selectin, P-selectin and L-selectin have also been shown to contribute to metastatic progression (145, 146). L-selectin was found to be particularly relevant for lymphatic dissemination of tumor cells (147).
Given the experimental data implicating selectins as key players in metastasis, expression of selectin ligands on cancer cells has been a subject of great interest. Selectin ligands on leukocytes or tumor cells that are preferentially bound by selectins include sialofucosylated Lewis carbohydrates (also known as Lewis antigens), such as sialyl Lewis X (sLeX) or sialyl Lewis A (sLea), which are found at the terminus of O-linked glycans (mucins), N-linked glycans or neolactosphingolipids (137). These sialofucosylated sugar moieties act as selectin ligands only when conjugated to the correct protein or lipid. For example, the CD44 protein, which acts as a receptor for hyaluronic acid, becomes a highly potent E- and L-selectin ligand when linked to sLeX (136). sLeX and sLea are synthesized and linked to various glycoconjugates in the Golgi apparatus by the sequential action of the family of carbohydrate synthesizing enzymes called glycosyltransferases, consisting of N-acetylglucosaminyl-, galactosyl-, sialyl- and fucosyltransferases (137). Elevated expression of the selectin ligands, sLeX, diSLeX, sLea, and of glycosyltransferase regulators have been identified in clinical primary melanoma specimens, as well as metastatic cells of various cancers, and have generally been associated with poor prognosis (137, 148, 149). In melanoma specifically, the human NKI-4 melanoma cell line expressed diSLeX and sLea and also bound E-selectin (150, 151). However, it remains unclear which proteins present on melanoma cells serve as targets for sialofucosylation. Moreover, despite their observed selectin binding activity, most melanoma lines appear devoid of E-selectin ligand expression, perhaps arguing against a selectin-selectin ligand driven model of melanoma cell homing (152). This finding, or the lack thereof, could possibly be explained by the loss of selectin ligand and glycosyltransferase expression during in vitro culturing, a known consequence in prostate cancer (153). An alternative explanation could be that E-selectin ligands are not expressed by the bulk of melanoma cells, but rather by a select few, such as the MMIC subpopulation. Evidence supporting this line of reasoning comes from studies on physiologic stem cells, as well as leukemic CSCs. Specifically, vascular niche E-selectin was found to control self-renewal, dormancy and chemotherapy resistance of selectin ligand-expressing hematopoietic stem cells (154), and similarly, the perivascular niche was also found to orchestrate CSC self-renewal (155), though the mechanisms underlying this process have not yet been fully unraveled. A separate study identified P-selectin as a regulator of hematopoietic stem cell and leukemic CSC self-renewal (156). Although little is known about E-selectin ligand expression on melanoma cells as mentioned above, CD44, a bona fide marker of CSCs in several types of cancer and also present on MMICs (73), acts as a potent selectin ligand in its sialofucosylated glycoform, also known as Hematopoietic Cell E-selectin/L-selectin Ligand (HCELL) (136). HCELL was found to mediate hematopoietic stem cell homing to the bone marrow (136), inevitably raising intriguing questions regarding the relationship between selectin-selectin ligands and CSC dissemination. To our knowledge, whether CSCs express HCELL has not been determined to date, but this would certainly represent an important line of investigation, as HCELL is known to be expressed in various cancers (138). The fact that a CSC marker itself can be modified to serve as a selectin-mediated trafficking mechanism supports the possibility that MMICs may also harness selectin-selectin ligand interactions to metastasize. This possibility warrants further investigation of melanoma selectin-selectin ligand expression, as well as the enzymes responsible for the unique sugar modifications that confer binding specificity, and narrowing the search for these molecules to the MMIC compartment may greatly enhance their detection and study.
Integrins in Melanoma Stem Cell Homing
A second class of molecules evoking particular interest is the family of heterodimeric adhesion and signaling receptors called integrins, which are among the most highly versatile of known cellular receptors (157, 158). Historically, most knowledge of integrin function on cancer cells has emanated from studies of leukocytes, which have unraveled striking parallels, though also differences, between leukocyte trafficking and cancer cell homing (159, 160). The role of integrins in homing of both leukocytes and cancer cells is complicated by virtue of the large possible integrin repertoire that may exist on any given cell. For example, 18 possible integrin α subunits may pair with 8 potential β subunits to generate the 24 known integrin heterodimers in humans (161). Moreover, each heterodimer interacts with its own or overlapping set of ligands deposited on the endothelial lining of the target tissue or on other cells to mediate cell adhesion, migration, proliferation, differentiation and survival. A further complication is that each heterodimer may exist in several three-dimensional states (conformations) or glycoforms with various binding affinities due to cytokine/chemokine activation, expressed at different levels and also cluster in the plasma membrane to influence integrin binding avidity (161). As a result, the attachment and movement of melanoma cells into target tissues is almost assuredly complex, relying on a diverse interplay of integrin receptors in various states and activities, interacting with a diverse set of ligands on endothelium and within tissue.
An evaluation of integrin expression on melanoma cells may be informative in simplifying and in discerning the complex nature of integrins in both MMIC and non-MMIC homing. To date, 11 integrin heterodimers have been described on bulk primary and metastatic melanoma tissues or in cell lines in culture: α1β1, α2β1, α3β1, α4β1, α5β1, α6β1, α7β1, αVβ3, αIIbβ3, α6β4 and αVβ5 (162). Of all identified integrins above, α4β1 appears particularly significant in melanoma cell homing. For example, α4β1, which is notably absent on melanocyte tissue or cultures though present on melanoma cells (162), is a classic homing molecule on leukocytes that binds VCAM-1, an inducible integrin counterreceptor upregulated on activated endothelial cells, to promote leukocyte tethering, rolling, arrest and migration into inflamed or infected tissue (163). As a consequence, α4β1 may help melanoma cells mimic the traffic control patterns of hematopoietic cells by enabling melanoma emigration into any tissue that expresses VCAM-1 and, due to its capacity to capture cells in hemodynamic flow, circumvent the need for selectin-selectin ligand mediated cell braking or “rolling”. Moreover, α4β1 may also bind fibronectin expressed on endothelial linings (162). Strikingly, α4β1 was found to mediate melanoma cell adhesion to and extravasation through endothelial cells under static and low shear flow conditions (164, 165). Inhibition of α4β1 activity on B16 F10 cells with gambogic acid or lysophosphatidylcholine reduced colony formation and invasion in murine lung metastasis models (166, 167). Of further interest is integrin αVβ3, classically termed the “vitronectin receptor”, which may also bind fibronectin, laminin and a host of diverse endothelial, basement membrane and matrix proteins in facilitation of tumor homing (162). αVβ3 on melanoma cells has been associated with adhesion, migration, invasion, metalloprotease activity, survival and tumor angiogenesis (162). In fact, B16F0 melanoma cells cultured in a hypoxic environment, 1.5% oxygen, displayed elevated αVβ3 expression and increased adhesion to and migration on vitronectin (168). αVβ3 was elevated not only on melanoma cells but also on several different cancer types and was selectively expressed on activated tumor endothelial cells but not on resting, non-tumor endothelial cells rendering it a potentially attractive general target for anti-cancer/anti-angiogenic therapy as underscored by previous and ongoing clinical trials (169–172). Other integrins of interest in melanoma are α3β1 and α5β1, which were elevated in primary and metastatic melanoma tissue, and α1β1, α2β1 and α6β1, which were reduced in metastatic vs. primary melanoma (162). No expression of leukocyte β2 integrins has been detected on melanocytes or yet reported on unstimulated bulk melanoma cells, though interestingly, incubation of bulk melanoma cells with human umbilical vein endothelial cell (HUVEC)-conditioned media induced expression of αLβ2, leading to αLβ2-ICAM-1-dependent melanoma cell transendothelial migration (173). Nonetheless, overall absence of β2 integrins on highly metastatic melanoma cells raises important questions, given the essential role of β2 integrins in leukocyte trafficking as underscored by the inherited genetic disease LAD I. Individuals with LAD I display defects in expression and function of the β2 subunit concomitant with impaired leukocyte adhesion and migration to infected or inflamed tissue (174). One proposed scenario is that β2 integrins on leukocytes bind ICAM-1 on melanoma cells, thereby bridging the melanoma cell to endothelial surfaces to facilitate melanoma cell extravasation (164) (Fig. 3B). Indeed, ICAM-1 expression by melanoma cells has been associated with malignant potential (175). Nonetheless, expression of active β2 integrins directly on melanoma cells might necessitate pre-stimulation, as previously reported (173). Furthermore, active β2 integrins might be limited to only a minor subset of melanoma cells such as MMICs.
Another unanswered, though important question is whether MMICs express and utilize identical or unique subsets of integrins compared with their non-stem melanoma cell cohorts in completion of the homing cascade. Though comparative analyses are rare, a few studies have revealed interesting differences in integrin expression between MMIC and non-MMIC populations. For example, the α5 subunit (also known as CD49e) was preferentially expressed on ABCB5+ G3361 melanoma subpopulations compared with ABCB5− cells, and co-expression of α5 with ABCB5 was further validated in clinically derived malignant melanoma tissues (73). In contrast, no differential expression of β1 subunit (also known as CD29) was found in MMIC versus non-MMIC cohorts (73). Based on elevation of α5, the sole pairing partner of which is β1, it could be hypothesized that enhanced α5β1 heterodimer expression may result in preferential MMIC adhesion and/or migration on the major α5β1 ligand, endothelial fibronectin. In another study, microarray analysis revealed differential expression of the α6β4 integrin signaling pathway, a major laminin-binding integrin, in ABCB5-enriched melanoma subsets vis-à-vis melanoma bulk populations (176).
Given the paucity of information on integrins in MMICs, and since diverse cancers often share overlapping integrin mediators in regulation of homing, further clues to integrin-driven MMIC homing might be uncovered by studying the integrin repertoire and integrin function in CSCs of various tumor models. Of the integrin repertoire on melanoma cells, these investigations have implicated α1, α2, α4, α6, αV, β1, β3 and β5 containing integrins as markers of or mediators in CSC homing, tumorigenicity or self-renewal of diverse cancers. For example, CD133+ prostate CSC isolates from patient tissue and from peripheral blood displayed high expression of α2β1 or of α1β1, α2β1, αVβ3 and αVβ5, respectively, and exhibited α1β1-mediated cell attachment to extracellular matrix proteins and α1β1-regulated CSC differentiation (177). Additionally, prostate cancer DU-145 cells exhibiting sphere-propagating, stem-like properties were similarly enriched for α2β1 expression (178). By virtue of these findings, α2β1 has been employed more recently as a marker to segregate putative prostate CSC subsets from non-CSC populations (179, 180). In a separate study, α4 was elevated on sarcospheres of breast sarcoma cells versus adherent cell cultures, and the population of α4-high sarcospheres displayed greater cell viability, tumor-initiating ability, chemoresistance and recapitulation of tumor complexity compared with the α4 low population (181). Another prime candidate in CSC regulation is α6, which was expressed highly on the SW872-S human liposarcoma sub-cell line, displaying higher tumor initiation and self-renewal potential than α6-low expressing cells (182). Strikingly, α6 knockdown by short interfering RNA or antibody blockade inhibited liposarcoma adhesion to laminin and blocked tumor growth in vitro and in vivo (182). Moreover, α6 expression coincided with liposarcoma relapse, indicating that α6 may serve as a marker of tumor-initiating, chemoresistant subpopulations in human liposarcoma (182). In other cancers, α6 was expressed preferentially in undifferentiated fallopian tube epithelial cell subpopulations exhibiting enhanced clonal growth and self-renewal potential, which represented cell subsets prone to initiation of serous carcinoma formation (183). α6 was also found co-expressed with conventional CSC markers, enriched among tumor-initiating cell populations and/or positively correlated with tumorigenic potential of cancer cell subsets in glioblastoma, breast cancer, prostate cancer and squamous cell carcinoma (180, 184–189). Similarly, αV integrins were elevated in human prostate cancer cells with tumor- and metastasis-initiating properties (190). In fact, knockdown or pharmacologic inhibition of αV in prostate cancer cells decreased α2 expression, inhibited clonogenic and migratory potential and decreased tumorigenicity in orthotopic growth and bone metastatic preclinical models indicating a role for αV integrins in CSC-driven disease progression (191, 192). One αV integrin in particular, αVβ3, is a well-established mediator of cellular differentiation by virtue of its involvement in differentiation of the endoderm from the inner cell mass during development and induction of osteogenic differentiation of mesenchymal stem cells when in contact with its major ligand, vitronectin (193, 194). Unsurprisingly, αVβ3 and, to a lesser extent, αVβ5, induced differentiation of prostate CSCs via contact with vitronectin, while blocking αVβ3-inhibited tumor formation (195). Interestingly, the β3 subunit was elevated on tumor-initiating glioblastoma cells exhibiting enhanced migration, invasion and plasticity versus non-stem cancer cells, and invasion was blocked with anti-αVβ3 antibody (196). Finally, elevated β1 expression was detected on pancreatic CSCs and was the strongest prognostic factor in relapse and radiotherapeutic outcome for squamous cell head and neck cancer (197, 198).
In summary, several integrin subunits and their respective integrin heterodimers are expressed and/or elevated on MMICs and on various other cancer CSCs. Given that nearly all of the 11 described integrin heterodimers on bulk melanoma cells have been linked to tumor-initiating and stem-like properties of various cancers, it is plausible that each of the 11 may play some role in MMIC homing with respect to adhesion, migration or invasion, or perhaps regulate other facets of melanoma progression, including but not limited to MMIC survival and differentiation. Nonetheless, given the specific elevation of α5β1 and activation of α6β4-dependent pathways on MMICs, the abundantly described roles for α6β1 and αVβ3 in CSC functions across several cancers, and the dominant role for α4β1 in leukocyte homing concomitant with its high expression on melanoma cells, these five integrins represent particularly attractive targets for further exploration into the integrin-mediated regulation of MMIC homing and progression (Fig. 3A). Moreover, since three other integrins described on bulk melanoma cells, α1β1, α2β1, and αVβ5, have also been implicated in CSC properties of other cancers, these also warrant further investigation along with β2 integrins and their ligand ICAM-1 expressed either on melanoma or endothelial cells.
Chemokine-Chemokine Receptors in Melanoma
Chemokines and chemokine receptors are key drivers of cellular recruitment in innate and adaptive immune responses and, in accord with the hematopoietic mimicry hypothesis of cancer dissemination, have been increasingly viewed as major facilitators of cancer cell homing and metastasis (199). Since chemokine receptors belong to the superfamily of seven transmembrane-spanning G-protein coupled receptors and may transmit intracellular signals, they are known to influence expression and binding activity of classic cancer and immune cell homing molecules described above, including selectin ligands and integrins as well as an array of ancillary cytosolic regulators involved in cellular adhesion and in directional cell migration along chemokine gradients (137, 199, 200). Moreover, chemokine-chemokine receptors, which are often upregulated in various cancers, may also influence the epithelial to mesenchymal transition (EMT) involved in CSC-driven tumorigenesis, tumor survival, proliferation and resistance to anoikis, tumor neovascularization, and also help recruit into the tumor microenvironment inflammatory immune cell subsets such as tumor-associated macrophages and myeloid-derived suppressor cells believed to impact cancer progression (55, 199, 200).
To date, 19 conventional chemokine receptors and over 40 chemokines have been described in mammals and have been divided into the CXC, CC, C or CX3C families based on arrangement of cysteine residues in chemokines (199, 200). Among these, melanoma cells have been found to express chemokine receptors CXCR1–4, CXCR6, CXCR7, CCR1, CCR2, CCR5–7, CCR9 and CCR10 and to produce the chemokines CXCL1–3, CXCL5–8, CXCL10, CXCL12, CCL2 and CCL5 (201, 202). Studies suggest that some of these signaling molecules may be involved in metastasis formation in melanoma. CCR7 and CCR10 expression have been associated with lower survival, rapid melanoma progression and/or with melanoma immune evasion (201, 203). One study demonstrated that cells overexpressing CCR7 exhibited a 700-fold elevation in metastasis to the draining lymph nodes compared to vector control cells (204). In another study, CCR10-overexpressing B16 cells, when exposed to the CCR10 ligand CCL27, which is generated constitutively by keratinocytes, exhibited enhanced survival in the skin and were protected from immune related Fas-ligand mediated apoptosis (205). Strikingly, this selective survival capability evokes the immunoevasive phenotype of MMICs (discussed above), implicating chemokine-chemokine receptors as one possible mechanism utilized by MMICs to promote disease progression. Consistent with this prospect, inhibition of CXCR1 on breast CSCs using a blocking antibody or the small molecule inhibitor repertaxin selectively depleted the CSC population (206), illustrating the importance of CXCR1 expression on the CSC subset. CXCR1 may also be similarly crucial to MMIC-driven metastasis, a not unlikely possibility, considering that CXCR1 has been shown to stimulate melanoma cell chemotaxis and transendothelial migration via G-protein signaling in an IL-8-dependent manner (207). CXCR4, which happens to represent the most widely expressed molecule of its class in melanoma (202, 208), is another chemokine receptor that has been linked to CSCs. For instance, CXCR4 was detected on glioma CSCs (209), and CXCR4 signaling in pancreatic CSCs was found to be essential for tumor metastasis (210). Moreover, CXCR4 overexpression was critical for the maintenance of stemness via the STAT3 pathway in drug-resistant non-small cell lung cancer cells (211).
In melanoma in particular, CXCR4 expression was associated with clinical melanoma lung metastasis, a conclusion supported by the enhanced lung metastasis seen with ectopic overexpression of CXCR4 in B16 melanoma cells (212). Furthermore, the CXCR4 signaling axis also promoted melanoma cell growth in nutrient-deprived conditions and conferred a proliferative advantage (212), two traits reminiscent of the survival advantage and enhanced tumor-propagating ability selectively seen in MMICs. How the above described metastatic and migratory processes are influenced by chemokine-chemokine receptor engagement is not completely understood, though they may be the result of pleiotropic chemokine-related signaling acting on multiple cancer cell processes. One possible scenario is that chemokine receptor triggering controls selectin ligand and integrin activity on cancer cells in a manner analogous to the chemokine receptor-mediated control of homing receptors on leukocytes. For example, overexpression of CXCR4 or engagement by its ligand, CXCL12 (also known as SDF-1), was found to enhance adhesion of melanoma cells to the endothelium and to VCAM-1 via induction of a high affinity state of β1 integrins, similar to the CXCR4-driven induction of α4β1, α5β1 and β2 integrin activity on hematopoietic cells (213, 214).
Despite the evidence linking chemokine-chemokine receptors and metastatic disease in melanoma, a comprehensive understanding of the role of these molecules in MMIC homing is still lacking. In total, the aforementioned results support a scenario whereby various chemokine receptors, dominated especially by CXCR1 and CXCR4, along with their chemokine ligands, likely influence various aspects of MMIC homing and metastasis, either via modulation of integrin or selectin ligand activity, by directing site-specific metastasis to distinct organs, maintenance of cancer cell stemness, or through effects on survival and proliferation (Fig. 3A).
Conclusions
Metastatic melanoma remains a deadly disease despite the recent spike in drug development. With the high demand for improved insight into this malignancy that accounts for majority of the mortality rate of skin cancers, the existence of MMICs has been a subject of intense debate, especially in light of the compiling data on the presence of CSCs in various cancers. CSCs are a highly malignant subset of cells that are capable of preferential tumor initiation and propagation, long-term self-renewal and differentiation into phenotypically variable cells comprising the bulk of the tumor. There are currently numerous compelling data extrapolated from studies in animal models supporting the CSC theory in melanoma, and conflicting findings can be explained by the variations in techniques and animal models used to study MMICs.
Given their inherent virulence, the observed association between MMICs and metastatic disease is perhaps not surprising. MMICs correlate with poor prognosis and increased tumor burden in patients and are enriched among CTCs. Although such findings certainly mark MMICs as a critical participant involved in melanoma progression, there is a dearth of evidence demonstrating a direct functional link between MMICs and metastasis formation. Seeing as there are intriguing parallels between the CSC compartment and hematopoietic cells, as showcased by the reported associations between CSCs and certain hematopoietic homing molecules, leukocyte mimicry might represent an important mechanism by which MMICs seed metastasis. In particular, MMICs might exploit selectins, integrins, and/or chemokine-chemokine receptors to home to distant tissues in a manner analogous to that of leukocytes. It should be noted, however, that additional pathways and signaling molecules could be implicated in MMIC-driven metastatic progression. Among these are galectins (215, 216), which have been associated with melanoma metastasis but have not been the focus of this review.
Provided that MMICs hold a significant presence in the CTC subset, future studies on CTCs with a special focus on the MMIC compartment may yield novel mechanisms of metastasis formation. In fact, MMICs bestow the unique opportunity to perform functional assays using melanoma CTCs. One challenge that has thus far posed as a barrier to the study of melanoma CTCs is the lack of appropriate markers for the isolation of viable circulating melanoma cells. Unlike in epithelial cancers, in which a surface marker called epithelial-specific antigen (ESA, also known as EpCAM) is used to select for viable CTCs, most melanoma differentiation antigens specific to cancer cells are often heterogeneously expressed and are intracellular molecules, rendering unfeasible the isolation of these cells using methods that maintain cellular viability, such as fluorescence-activated cell sorting (FACS). In this regard, MMIC markers, such as ABCB5 and CD271, represent a unique solution to this conundrum, as they are expressed on the cell surface and, at the same time, are enriched among CTCs. The ability to isolate circulating CTCs using MMIC markers will allow for the evaluation of what are presumably the most virulent CTC subsets, but most importantly, it also immensely facilitates the much needed studies on the biology of their metastatic behavior. Such functional characterization will permit the discrimination between nontumorigenic and metastatic CTCs, enabling the generation of meaningful biomarker signatures to distinguish CTC subtypes with distinct roles in melanoma progression. The determination of these virulence-conferring markers could lead to improved melanoma staging, prognosis, and therapeutic monitoring and may expedite the development of anti-melanoma therapies specifically targeting the metastatic apparatus of the MMIC compartment responsible for neoplastic progression.
Acknowledgments
We apologize to those colleagues whose studies were not cited in this review due to space limitations. We thank Dr. George Murphy for his review of the manuscript during various stages of its evolution. Our research is supported by a Research Career Development Award from the Dermatology Foundation (to T.S.), an Innovative Research Grant from the Melanoma International Foundation (to T.S.), and an NCI SPORE in Skin Cancer Developmental Project Grant (to T.S. and S.R.B.). N.L. is the recipient of an American Skin Association Medical Student Grant.
References
- 1.Miller AJ, Mihm MC. Melanoma. New England Journal of Medicine. 2006;355(1):51–65. doi: 10.1056/NEJMra052166. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: A Cancer Journal for Clinicians. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 3.Cancer Facts & Figures 2013. American Cancer Society; Atlanta: 2013. [Google Scholar]
- 4.Gilchrest BA, Eller MS, Geller AC, Yaar M. The Pathogenesis of Melanoma Induced by Ultraviolet Radiation. New England Journal of Medicine. 1999;340(17):1341–1348. doi: 10.1056/NEJM199904293401707. [DOI] [PubMed] [Google Scholar]
- 5.Fountain JW, Bale SJ, Housman DE, Dracopoli NC. Genetics of melanoma. Cancer surveys. 1990;9(4):645–671. [PubMed] [Google Scholar]
- 6.Tucker Ma HAHEA, et al. Clinically recognized dysplastic nevi: A central risk factor for cutaneous melanoma. JAMA: The Journal of the American Medical Association. 1997;277(18):1439–1444. [PubMed] [Google Scholar]
- 7.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: III. Family history, actinic damage and phenotypic factors. European Journal of Cancer. 2005;41(14):2040–2059. doi: 10.1016/j.ejca.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 8.Rhodes Ar, WMAFTBMMCJSAJ Risk factors for cutaneous melanoma: A practical method of recognizing predisposed individuals. JAMA: The Journal of the American Medical Association. 1987;258(21):3146–3154. [PubMed] [Google Scholar]
- 9.Yang G, Rajadurai A, Tsao H. Recurrent Patterns of Dual RB and p53 Pathway Inactivation in Melanoma. J Investig Dermatol. 2005;125(6):1242–1251. doi: 10.1111/j.0022-202X.2005.23931.x. [DOI] [PubMed] [Google Scholar]
- 10.Tsao H, Goel V, Wu H, Yang G, Haluska FG. Genetic Interaction Between NRAS and BRAF Mutations and PTEN/MMAC1 Inactivation in Melanoma. J Investig Dermatol. 2004;122(2):337–341. doi: 10.1046/j.0022-202X.2004.22243.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–954. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 12.Stahl JM, Sharma A, Cheung M, et al. Deregulated Akt3 Activity Promotes Development of Malignant Melanoma. Cancer research. 2004;64(19):7002–7010. doi: 10.1158/0008-5472.CAN-04-1399. [DOI] [PubMed] [Google Scholar]
- 13.Guldberg P, thor Straten P, Birck A, Ahrenkiel V, Kirkin AF, Zeuthen J. Disruption of the MMAC1/PTEN Gene by Deletion or Mutation Is a Frequent Event in Malignant Melanoma. Cancer research. 1997;57(17):3660–3663. [PubMed] [Google Scholar]
- 14.Flaherty KT, Hodi FS, Fisher DE. From genes to drugs: targeted strategies for melanoma. Nature reviews Cancer. 2012;12(5):349–361. doi: 10.1038/nrc3218. [DOI] [PubMed] [Google Scholar]
- 15.Chapman PB, Hauschild A, Robert C, et al. Improved Survival with Vemurafenib in Melanoma with BRAF V600E Mutation. New England Journal of Medicine. 2011;364(26):2507–2516. doi: 10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flaherty KT, Robert C, Hersey P, et al. Improved Survival with MEK Inhibition in BRAF-Mutated Melanoma. New England Journal of Medicine. 2012;367(2):107–114. doi: 10.1056/NEJMoa1203421. [DOI] [PubMed] [Google Scholar]
- 17.Ferradini L, Mackensen A, Genevée C, et al. Analysis of T cell receptor variability in tumor-infiltrating lymphocytes from a human regressive melanoma. Evidence for in situ T cell clonal expansion. The Journal of Clinical Investigation. 1993;91(3):1183–1190. doi: 10.1172/JCI116278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenberg SA. Progress in human tumour immunology and immunotherapy. Nature. 2001;411(6835):380–384. doi: 10.1038/35077246. [DOI] [PubMed] [Google Scholar]
- 19.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nature reviews Cancer. 2012;12(4):252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keilholz U, Punt CJA, Gore M, et al. Dacarbazine, Cisplatin, and Interferon-Alfa-2b With or Without Interleukin-2 in Metastatic Melanoma: A Randomized Phase III Trial (18951) of the European Organisation for Research and Treatment of Cancer Melanoma Group. Journal of Clinical Oncology. 2005;23(27):6747–6755. doi: 10.1200/JCO.2005.03.202. [DOI] [PubMed] [Google Scholar]
- 21.Atkins MB, Hsu J, Lee S, et al. Phase III Trial Comparing Concurrent Biochemotherapy With Cisplatin, Vinblastine, Dacarbazine, Interleukin-2, and Interferon Alfa-2b With Cisplatin, Vinblastine, and Dacarbazine Alone in Patients With Metastatic Malignant Melanoma (E3695): A Trial Coordinated by the Eastern Cooperative Oncology Group. Journal of Clinical Oncology. 2008;26(35):5748–5754. doi: 10.1200/JCO.2008.17.5448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwartzentruber DJ, Lawson DH, Richards JM, et al. gp100 Peptide Vaccine and Interleukin-2 in Patients with Advanced Melanoma. New England Journal of Medicine. 2011;364(22):2119–2127. doi: 10.1056/NEJMoa1012863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Topalian SL, Hodi FS, Brahmer JR, et al. Safety, Activity, and Immune Correlates of Anti–PD-1 Antibody in Cancer. New England Journal of Medicine. 2012;366(26):2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369(2):122–133. doi: 10.1056/NEJMoa1302369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brahmer JR, Tykodi SS, Chow LQM, et al. Safety and Activity of Anti–PD-L1 Antibody in Patients with Advanced Cancer. New England Journal of Medicine. 2012;366(26):2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hanahan D, Weinberg Robert A. Hallmarks of Cancer: The Next Generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 29.Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414(6859):105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- 30.Schatton T, Frank NY, Frank MH. Identification and targeting of cancer stem cells. BioEssays. 2009;31(10):1038–1049. doi: 10.1002/bies.200900058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schatton T, Murphy GF, Frank NY, et al. Identification of cells initiating human melanomas. Nature. 2008;451(7176):345–349. doi: 10.1038/nature06489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boiko AD, Razorenova OV, van de Rijn M, et al. Human melanoma-initiating cells express neural crest nerve growth factor receptor CD271. Nature. 2010;466(7302):133–137. doi: 10.1038/nature09161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Civenni G, Walter A, Kobert N, et al. Human CD271-Positive Melanoma Stem Cells Associated with Metastasis Establish Tumor Heterogeneity and Long-term Growth. Cancer research. 2011;71(8):3098–3109. doi: 10.1158/0008-5472.CAN-10-3997. [DOI] [PubMed] [Google Scholar]
- 34.Michor F, Iwasa Y, Nowak MA. Dynamics of cancer progression. Nature reviews Cancer. 2004;4(3):197–205. doi: 10.1038/nrc1295. [DOI] [PubMed] [Google Scholar]
- 35.Stewart JM, Shaw PA, Gedye C, Bernardini MQ, Neel BG, Ailles LE. Phenotypic heterogeneity and instability of human ovarian tumor-initiating cells. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(16):6468–6473. doi: 10.1073/pnas.1005529108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gibbs KD, Jr, Jager A, Crespo O, et al. Decoupling of tumor-initiating activity from stable immunophenotype in HoxA9-Meis1-driven AML. Cell Stem Cell. 2012;10(2):210–217. doi: 10.1016/j.stem.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clarke MF, Dick JE, Dirks PB, et al. Cancer stem cells--perspectives on current status and future directions: AACR Workshop on cancer stem cells. Cancer research. 2006;66(19):9339–9344. doi: 10.1158/0008-5472.CAN-06-3126. [DOI] [PubMed] [Google Scholar]
- 38.Schatton T, Frank MH. The in vitro spheroid melanoma cell culture assay: cues on tumor initiation? J Invest Dermatol. 2010;130(7):1769–1771. doi: 10.1038/jid.2010.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lathia JD, Gallagher J, Myers JT, et al. Direct in vivo evidence for tumor propagation by glioblastoma cancer stem cells. PloS one. 2011;6(9):e24807. doi: 10.1371/journal.pone.0024807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen J, Li Y, Yu TS, et al. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature. 2012;488(7412):522–526. doi: 10.1038/nature11287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Driessens G, Beck B, Caauwe A, Simons BD, Blanpain C. Defining the mode of tumour growth by clonal analysis. Nature. 2012;488(7412):527–530. doi: 10.1038/nature11344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schepers AG, Snippert HJ, Stange DE, et al. Lineage Tracing Reveals Lgr5+ Stem Cell Activity in Mouse Intestinal Adenomas. Science. 2012;337(6095):730–735. doi: 10.1126/science.1224676. [DOI] [PubMed] [Google Scholar]
- 43.Barker N, Ridgway RA, van Es JH, et al. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457(7229):608–611. doi: 10.1038/nature07602. [DOI] [PubMed] [Google Scholar]
- 44.Zhu L, Gibson P, Currle DS, et al. Prominin 1 marks intestinal stem cells that are susceptible to neoplastic transformation. Nature. 2009;457(7229):603–607. doi: 10.1038/nature07589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krivtsov AV, Twomey D, Feng Z, et al. Transformation from committed progenitor to leukaemia stem cell initiated by MLL-AF9. Nature. 2006;442(7104):818–822. doi: 10.1038/nature04980. [DOI] [PubMed] [Google Scholar]
- 46.Chaffer CL, Brueckmann I, Scheel C, et al. Normal and neoplastic nonstem cells can spontaneously convert to a stem-like state. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(19):7950–7955. doi: 10.1073/pnas.1102454108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iliopoulos D, Hirsch HA, Wang G, Struhl K. Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proceedings of the National Academy of Sciences. 2011;108(4):1397–1402. doi: 10.1073/pnas.1018898108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakagawa T, Sharma M, Nabeshima Y, Braun RE, Yoshida S. Functional hierarchy and reversibility within the murine spermatogenic stem cell compartment. Science. 2010;328(5974):62–67. doi: 10.1126/science.1182868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Quintana E, Shackleton M, Sabel MS, Fullen DR, Johnson TM, Morrison SJ. Efficient tumour formation by single human melanoma cells. Nature. 2008;456(7222):593–598. doi: 10.1038/nature07567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Girouard SD, Murphy GF. Melanoma stem cells: not rare, but well done. Lab Invest. 2011;91(5):647–664. doi: 10.1038/labinvest.2011.50. [DOI] [PubMed] [Google Scholar]
- 51.Morrison SJ, Kimble J. Asymmetric and symmetric stem-cell divisions in development and cancer. Nature. 2006;441(7097):1068–1074. doi: 10.1038/nature04956. [DOI] [PubMed] [Google Scholar]
- 52.Zhang S, Balch C, Chan MW, et al. Identification and characterization of ovarian cancer-initiating cells from primary human tumors. Cancer research. 2008;68(11):4311–4320. doi: 10.1158/0008-5472.CAN-08-0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Harris MA, Yang H, Low BE, et al. Cancer stem cells are enriched in the side population cells in a mouse model of glioma. Cancer research. 2008;68(24):10051–10059. doi: 10.1158/0008-5472.CAN-08-0786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Quintana E, Shackleton M, Foster HR, et al. Phenotypic heterogeneity among tumorigenic melanoma cells from patients that is reversible and not hierarchically organized. Cancer Cell. 2010;18(5):510–523. doi: 10.1016/j.ccr.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gupta PB, Chaffer CL, Weinberg RA. Cancer stem cells: mirage or reality? Nature medicine. 2009;15(9):1010–1012. doi: 10.1038/nm0909-1010. [DOI] [PubMed] [Google Scholar]
- 56.Bao S, Wu Q, Sathornsumetee S, et al. Stem cell-like glioma cells promote tumor angiogenesis through vascular endothelial growth factor. Cancer research. 2006;66(16):7843–7848. doi: 10.1158/0008-5472.CAN-06-1010. [DOI] [PubMed] [Google Scholar]
- 57.Frank NY, Schatton T, Kim S, et al. VEGFR-1 expressed by malignant melanoma-initiating cells is required for tumor growth. Cancer research. 2011;71(4):1474–1485. doi: 10.1158/0008-5472.CAN-10-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ricci-Vitiani L, Pallini R, Biffoni M, et al. Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature. 2010;468(7325):824–828. doi: 10.1038/nature09557. [DOI] [PubMed] [Google Scholar]
- 59.Wang R, Chadalavada K, Wilshire J, et al. Glioblastoma stem-like cells give rise to tumour endothelium. Nature. 2010;468(7325):829–833. doi: 10.1038/nature09624. [DOI] [PubMed] [Google Scholar]
- 60.Bao S, Wu Q, McLendon RE, et al. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444(7120):756–760. doi: 10.1038/nature05236. [DOI] [PubMed] [Google Scholar]
- 61.Diehn M, Cho RW, Lobo NA, et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature. 2009;458(7239):780–783. doi: 10.1038/nature07733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li X, Lewis MT, Huang J, et al. Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. J Natl Cancer Inst. 2008;100(9):672–679. doi: 10.1093/jnci/djn123. [DOI] [PubMed] [Google Scholar]
- 63.Wilson BJ, Schatton T, Zhan Q, et al. ABCB5 identifies a therapy-refractory tumor cell population in colorectal cancer patients. Cancer research. 2011;71(15):5307–5316. doi: 10.1158/0008-5472.CAN-11-0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li Z, Bao S, Wu Q, et al. Hypoxia-inducible factors regulate tumorigenic capacity of glioma stem cells. Cancer Cell. 2009;15(6):501–513. doi: 10.1016/j.ccr.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vlashi E, Lagadec C, Vergnes L, et al. Metabolic state of glioma stem cells and nontumorigenic cells. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(38):16062–16067. doi: 10.1073/pnas.1106704108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schatton T, Schutte U, Frank NY, et al. Modulation of T-cell activation by malignant melanoma initiating cells. Cancer research. 2010;70(2):697–708. doi: 10.1158/0008-5472.CAN-09-1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jaiswal S, Jamieson CH, Pang WW, et al. CD47 is upregulated on circulating hematopoietic stem cells and leukemia cells to avoid phagocytosis. Cell. 2009;138(2):271–285. doi: 10.1016/j.cell.2009.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Di Tomaso T, Mazzoleni S, Wang E, et al. Immunobiological characterization of cancer stem cells isolated from glioblastoma patients. Clin Cancer Res. 2010;16(3):800–813. doi: 10.1158/1078-0432.CCR-09-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wei J, Barr J, Kong LY, et al. Glioblastoma cancer-initiating cells inhibit T-cell proliferation and effector responses by the signal transducers and activators of transcription 3 pathway. Mol Cancer Ther. 2010;9(1):67–78. doi: 10.1158/1535-7163.MCT-09-0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wei J, Barr J, Kong LY, et al. Glioma-associated cancer-initiating cells induce immunosuppression. Clin Cancer Res. 2010;16(2):461–473. doi: 10.1158/1078-0432.CCR-09-1983. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 71.Hendrix MJ, Seftor EA, Hess AR, Seftor RE. Molecular plasticity of human melanoma cells. Oncogene. 2003;22(20):3070–3075. doi: 10.1038/sj.onc.1206447. [DOI] [PubMed] [Google Scholar]
- 72.Schatton T, Frank MH. Cancer stem cells and human malignant melanoma. Pigment Cell Melanoma Res. 2008;21(1):39–55. doi: 10.1111/j.1755-148X.2007.00427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Frank NY, Margaryan A, Huang Y, et al. ABCB5-mediated doxorubicin transport and chemoresistance in human malignant melanoma. Cancer research. 2005;65(10):4320–4333. doi: 10.1158/0008-5472.CAN-04-3327. [DOI] [PubMed] [Google Scholar]
- 74.Fang D, Nguyen TK, Leishear K, et al. A tumorigenic subpopulation with stem cell properties in melanomas. Cancer research. 2005;65(20):9328–9337. doi: 10.1158/0008-5472.CAN-05-1343. [DOI] [PubMed] [Google Scholar]
- 75.Monzani E, Facchetti F, Galmozzi E, et al. Melanoma contains CD133 and ABCG2 positive cells with enhanced tumourigenic potential. Eur J Cancer. 2007;43(5):935–946. doi: 10.1016/j.ejca.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 76.Botelho MG, Wang X, Arndt-Jovin DJ, Becker D, Jovin TM. Induction of terminal differentiation in melanoma cells on downregulation of beta-amyloid precursor protein. J Invest Dermatol. 2010;130(5):1400–1410. doi: 10.1038/jid.2009.296. [DOI] [PubMed] [Google Scholar]
- 77.Kumar SM, Liu S, Lu H, et al. Acquired cancer stem cell phenotypes through Oct4-mediated dedifferentiation. Oncogene. 2012;31(47):4898–4911. doi: 10.1038/onc.2011.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Keshet GI, Goldstein I, Itzhaki O, et al. MDR1 expression identifies human melanoma stem cells. Biochem Biophys Res Commun. 2008;368(4):930–936. doi: 10.1016/j.bbrc.2008.02.022. [DOI] [PubMed] [Google Scholar]
- 79.Touil Y, Zuliani T, Wolowczuk I, et al. The PI3K/AKT signaling pathway controls the quiescence of the low-Rhodamine123-retention cell compartment enriched for melanoma stem cell activity. Stem Cells. 2012;31(4):641–651. doi: 10.1002/stem.1333. [DOI] [PubMed] [Google Scholar]
- 80.Czyz M, Koprowska K, Sztiller-Sikorska M. Parthenolide reduces the frequency of ABCB5-positive cells and clonogenic capacity of melanoma cells from anchorage independent melanospheres. Cancer Biol Ther. 2013;14(2):135–145. doi: 10.4161/cbt.22952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bertolotto C, Lesueur F, Giuliano S, et al. A SUMOylation-defective MITF germline mutation predisposes to melanoma and renal carcinoma. Nature. 2011;480(7375):94–98. doi: 10.1038/nature10539. [DOI] [PubMed] [Google Scholar]
- 82.Lin JY, Zhang M, Schatton T, et al. Genetically determined ABCB5 functionality correlates with pigmentation phenotype and melanoma risk. Biochem Biophys Res Commun. 2013;436(3):536–542. doi: 10.1016/j.bbrc.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cheung ST, Cheung PF, Cheng CK, Wong NC, Fan ST. Granulin-epithelin precursor and ATP-dependent binding cassette (ABC)B5 regulate liver cancer cell chemoresistance. Gastroenterology. 2011;140(1):344–355. doi: 10.1053/j.gastro.2010.07.049. [DOI] [PubMed] [Google Scholar]
- 84.Schmidt P, Kopecky C, Hombach A, Zigrino P, Mauch C, Abken H. Eradication of melanomas by targeted elimination of a minor subset of tumor cells. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(6):2474–2479. doi: 10.1073/pnas.1009069108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schlaak M, Schmidt P, Bangard C, Kurschat P, Mauch C, Abken H. Regression of metastatic melanoma in a patient by antibody targeting of cancer stem cells. Oncotarget. 2012;3(1):22–30. doi: 10.18632/oncotarget.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pinc A, Somasundaram R, Wagner C, et al. Targeting CD20 in melanoma patients at high risk of disease recurrence. Mol Ther. 2012;20(5):1056–1062. doi: 10.1038/mt.2012.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ginestier C, Hur MH, Charafe-Jauffret E, et al. ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell. 2007;1(5):555–567. doi: 10.1016/j.stem.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Carpentino JE, Hynes MJ, Appelman HD, et al. Aldehyde dehydrogenase-expressing colon stem cells contribute to tumorigenesis in the transition from colitis to cancer. Cancer research. 2009;69(20):8208–8215. doi: 10.1158/0008-5472.CAN-09-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Boonyaratanakornkit JB, Yue L, Strachan LR, et al. Selection of tumorigenic melanoma cells using ALDH. J Invest Dermatol. 2010;130(12):2799–2808. doi: 10.1038/jid.2010.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Luo Y, Dallaglio K, Chen Y, et al. ALDH1A isozymes are markers of human melanoma stem cells and potential therapeutic targets. Stem Cells. 2012;30(10):2100–2113. doi: 10.1002/stem.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Prasmickaite L, Engesaeter BO, Skrbo N, et al. Aldehyde dehydrogenase (ALDH) activity does not select for cells with enhanced aggressive properties in malignant melanoma. PloS one. 2010;5(5):e10731. doi: 10.1371/journal.pone.0010731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Roesch A, Becker B, Schneider-Brachert W, Hagen I, Landthaler M, Vogt T. Re-expression of the retinoblastoma-binding protein 2-homolog 1 reveals tumor-suppressive functions in highly metastatic melanoma cells. J Invest Dermatol. 2006;126(8):1850–1859. doi: 10.1038/sj.jid.5700324. [DOI] [PubMed] [Google Scholar]
- 93.Roesch A, Fukunaga-Kalabis M, Schmidt EC, et al. A temporarily distinct subpopulation of slow-cycling melanoma cells is required for continuous tumor growth. Cell. 2010;141(4):583–594. doi: 10.1016/j.cell.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Maniotis AJ, Folberg R, Hess A, et al. Vascular channel formation by human melanoma cells in vivo and in vitro: vasculogenic mimicry. The American journal of pathology. 1999;155(3):739–752. doi: 10.1016/S0002-9440(10)65173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hendrix MJ, Seftor EA, Hess AR, Seftor RE. Vasculogenic mimicry and tumour-cell plasticity: lessons from melanoma. Nature reviews Cancer. 2003;3(6):411–421. doi: 10.1038/nrc1092. [DOI] [PubMed] [Google Scholar]
- 96.Sharma BK, Manglik V, Elias EG. Immuno-expression of human melanoma stem cell markers in tissues at different stages of the disease. J Surg Res. 2010;163(1):e11–15. doi: 10.1016/j.jss.2010.03.043. [DOI] [PubMed] [Google Scholar]
- 97.Easty DJ, Herlyn M, Bennett DC. Abnormal protein tyrosine kinase gene expression during melanoma progression and metastasis. International journal of cancer Journal international du cancer. 1995;60(1):129–136. doi: 10.1002/ijc.2910600119. [DOI] [PubMed] [Google Scholar]
- 98.Hendrix MJ, Seftor EA, Meltzer PS, et al. Expression and functional significance of VE-cadherin in aggressive human melanoma cells: role in vasculogenic mimicry. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(14):8018–8023. doi: 10.1073/pnas.131209798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kaplan RN, Riba RD, Zacharoulis S, et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438(7069):820–827. doi: 10.1038/nature04186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Linley AJ, Mathieu MG, Miles AK, Rees RC, McArdle SE, Regad T. The helicase HAGE expressed by malignant melanoma-initiating cells is required for tumor cell proliferation in vivo. J Biol Chem. 2012;287(17):13633–13643. doi: 10.1074/jbc.M111.308973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Landsberg J, Kohlmeyer J, Renn M, et al. Melanomas resist T-cell therapy through inflammation-induced reversible dedifferentiation. Nature. 2012;490(7420):412–416. doi: 10.1038/nature11538. [DOI] [PubMed] [Google Scholar]
- 102.Huang Y, Anderle P, Bussey KJ, et al. Membrane transporters and channels: role of the transportome in cancer chemosensitivity and chemoresistance. Cancer research. 2004;64(12):4294–4301. doi: 10.1158/0008-5472.CAN-03-3884. [DOI] [PubMed] [Google Scholar]
- 103.Chartrain M, Riond J, Stennevin A, et al. Melanoma chemotherapy leads to the selection of ABCB5-expressing cells. PloS one. 2012;7(5):e36762. doi: 10.1371/journal.pone.0036762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sousa JF, Espreafico EM. Suppression subtractive hybridization profiles of radial growth phase and metastatic melanoma cell lines reveal novel potential targets. BMC Cancer. 2008;8:19. doi: 10.1186/1471-2407-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yang JY, Ha SA, Yang YS, Kim JW. p-Glycoprotein ABCB5 and YB-1 expression plays a role in increased heterogeneity of breast cancer cells: correlations with cell fusion and doxorubicin resistance. BMC Cancer. 2010;10:388. doi: 10.1186/1471-2407-10-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vlashi E, McBride WH, Pajonk F. Radiation responses of cancer stem cells. J Cell Biochem. 2009;108(2):339–342. doi: 10.1002/jcb.22275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Vasquez-Moctezuma I, Meraz-Rios MA, Villanueva-Lopez CG, et al. ATP-binding cassette transporter ABCB5 gene is expressed with variability in malignant melanoma. Actas Dermosifiliogr. 2010;101(4):341–348. doi: 10.1016/j.ad.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 108.Fukunaga-Kalabis M, Martinez G, Nguyen TK, et al. Tenascin-C promotes melanoma progression by maintaining the ABCB5-positive side population. Oncogene. 2010;29(46):6115–6124. doi: 10.1038/onc.2010.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Setia N, Abbas O, Sousa Y, Garb JL, Mahalingam M. Profiling of ABC transporters ABCB5, ABCF2 and nestin-positive stem cells in nevi, in situ and invasive melanoma. Mod Pathol. 2012;25(8):1169–1175. doi: 10.1038/modpathol.2012.71. [DOI] [PubMed] [Google Scholar]
- 110.Grimm M, Krimmel M, Polligkeit J, et al. ABCB5 expression and cancer stem cell hypothesis in oral squamous cell carcinoma. Eur J Cancer. 2012;48(17):3186–3197. doi: 10.1016/j.ejca.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 111.Govindan R, Ding L, Griffith M, et al. Genomic landscape of non-small cell lung cancer in smokers and never-smokers. Cell. 2012;150(6):1121–1134. doi: 10.1016/j.cell.2012.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ma J, Lin JY, Alloo A, et al. Isolation of tumorigenic circulating melanoma cells. Biochem Biophys Res Commun. 2010;402(4):711–717. doi: 10.1016/j.bbrc.2010.10.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kupas V, Weishaupt C, Siepmann D, et al. RANK is expressed in metastatic melanoma and highly upregulated on melanoma-initiating cells. J Invest Dermatol. 2011;131(4):944–955. doi: 10.1038/jid.2010.377. [DOI] [PubMed] [Google Scholar]
- 114.Reid AL, Millward M, Pearce R, et al. Markers of circulating tumour cells in the peripheral blood of patients with melanoma correlate with disease recurrence and progression. Br J Dermatol. 2013;168(1):85–92. doi: 10.1111/bjd.12057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Quintana E, Piskounova E, Shackleton M, et al. Human melanoma metastasis in NSG mice correlates with clinical outcome in patients. Sci Transl Med. 2012;4(159):159ra149. doi: 10.1126/scitranslmed.3004599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Freeman JB, Gray ES, Millward M, Pearce R, Ziman M. Evaluation of a multi-marker immunomagnetic enrichment assay for the quantification of circulating melanoma cells. J Transl Med. 2012;10:192. doi: 10.1186/1479-5876-10-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Sethi N, Kang Y. Unravelling the complexity of metastasis - molecular understanding and targeted therapies. Nature reviews Cancer. 2011;11(10):735–748. doi: 10.1038/nrc3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fidler IJ. The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nature reviews Cancer. 2003;3(6):453–458. doi: 10.1038/nrc1098. [DOI] [PubMed] [Google Scholar]
- 119.Weinberg RA. The Biology of Cancer. 2007. [Google Scholar]
- 120.Fidler IJ, Poste G. The biologic diversity of cancer metastases. Hosp Pract (Off Ed) 1982;17(7):57–64. doi: 10.1080/21548331.1982.11698073. [DOI] [PubMed] [Google Scholar]
- 121.Husemann Y, Geigl JB, Schubert F, et al. Systemic spread is an early step in breast cancer. Cancer Cell. 2008;13(1):58–68. doi: 10.1016/j.ccr.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 122.Weng D, Penzner JH, Song B, Koido S, Calderwood SK, Gong J. Metastasis is an early event in mouse mammary carcinomas and is associated with cells bearing stem cell markers. Breast Cancer Res. 2012;14(1):R18. doi: 10.1186/bcr3102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Malanchi I, Santamaria-Martinez A, Susanto E, et al. Interactions between cancer stem cells and their niche govern metastatic colonization. Nature. 2012;481(7379):85–89. doi: 10.1038/nature10694. [DOI] [PubMed] [Google Scholar]
- 124.Baccelli I, Schneeweiss A, Riethdorf S, et al. Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. Nat Biotechnol. 2013 doi: 10.1038/nbt.2576. [DOI] [PubMed] [Google Scholar]
- 125.Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nature reviews Cancer. 2002;2(6):442–454. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- 126.Sampieri K, Fodde R. Cancer stem cells and metastasis. Seminars in cancer biology. 2012;22(3):187–193. doi: 10.1016/j.semcancer.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 127.Mani SA, Guo W, Liao MJ, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133(4):704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fenouille N, Tichet M, Dufies M, et al. The epithelial-mesenchymal transition (EMT) regulatory factor SLUG (SNAI2) is a downstream target of SPARC and AKT in promoting melanoma cell invasion. PloS one. 2012;7(7):e40378. doi: 10.1371/journal.pone.0040378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yang J, Mani SA, Donaher JL, et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004;117(7):927–939. doi: 10.1016/j.cell.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 130.Weiss MB, Abel EV, Mayberry MM, Basile KJ, Berger AC, Aplin AE. TWIST1 is an ERK1/2 effector that promotes invasion and regulates MMP-1 expression in human melanoma cells. Cancer research. 2012;72(24):6382–6392. doi: 10.1158/0008-5472.CAN-12-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cheli Y, Giuliano S, Fenouille N, et al. Hypoxia and MITF control metastatic behaviour in mouse and human melanoma cells. Oncogene. 2012;31(19):2461–2470. doi: 10.1038/onc.2011.425. [DOI] [PubMed] [Google Scholar]
- 132.Tas F. Metastatic behavior in melanoma: timing, pattern, survival, and influencing factors. J Oncol. 2012:647–684. doi: 10.1155/2012/647684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Payette MJ, Katz M, 3rd, Grant-Kels JM. Melanoma prognostic factors found in the dermatopathology report. Clin Dermatol. 2009;27(1):53–74. doi: 10.1016/j.clindermatol.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 134.Springer TA. Traffic signals for lymphocyte recirculation and leukocyte emigration: the multistep paradigm. Cell. 1994;76(2):301–314. doi: 10.1016/0092-8674(94)90337-9. [DOI] [PubMed] [Google Scholar]
- 135.Butcher EC. Leukocyte-endothelial cell recognition: three (or more) steps to specificity and diversity. Cell. 1991;67(6):1033–1036. doi: 10.1016/0092-8674(91)90279-8. [DOI] [PubMed] [Google Scholar]
- 136.Sackstein R, Merzaban JS, Cain DW, et al. Ex vivo glycan engineering of CD44 programs human multipotent mesenchymal stromal cell trafficking to bone. Nature medicine. 2008;14(2):181–187. doi: 10.1038/nm1703. [DOI] [PubMed] [Google Scholar]
- 137.Barthel SR, Gavino JD, Descheny L, Dimitroff CJ. Targeting selectins and selectin ligands in inflammation and cancer. Expert Opin Ther Targets. 2007;11(11):1473–1491. doi: 10.1517/14728222.11.11.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Jacobs PP, Sackstein R. CD44 and HCELL: preventing hematogenous metastasis at step 1. FEBS Lett. 585(20):3148–3158. doi: 10.1016/j.febslet.2011.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Pawelek JM, Chakraborty AK. The cancer cell--leukocyte fusion theory of metastasis. Adv Cancer Res. 2008;101:397–444. doi: 10.1016/S0065-230X(08)00410-7. [DOI] [PubMed] [Google Scholar]
- 140.Laubli H, Borsig L. Selectins promote tumor metastasis. Seminars in cancer biology. 2010;20(3):169–177. doi: 10.1016/j.semcancer.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 141.Etzioni A, Frydman M, Pollack S, et al. Brief report: recurrent severe infections caused by a novel leukocyte adhesion deficiency. N Engl J Med. 1992;327(25):1789–1792. doi: 10.1056/NEJM199212173272505. [DOI] [PubMed] [Google Scholar]
- 142.Khatib AM, Kontogiannea M, Fallavollita L, Jamison B, Meterissian S, Brodt P. Rapid induction of cytokine and E-selectin expression in the liver in response to metastatic tumor cells. Cancer research. 1999;59(6):1356–1361. [PubMed] [Google Scholar]
- 143.Barthel SR, Wiese GK, Cho J, et al. Alpha 1,3 fucosyltransferases are master regulators of prostate cancer cell trafficking. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(46):19491–19496. doi: 10.1073/pnas.0906074106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Barthel SR, Hays DL, Yazawa EM, et al. Definition of molecular determinants of prostate cancer cell bone extravasation. Cancer research. 73(2):942–952. doi: 10.1158/0008-5472.CAN-12-3264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Borsig L, Wong R, Hynes RO, Varki NM, Varki A. Synergistic effects of L- and P-selectin in facilitating tumor metastasis can involve non-mucin ligands and implicate leukocytes as enhancers of metastasis. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(4):2193–2198. doi: 10.1073/pnas.261704098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ludwig RJ, Boehme B, Podda M, et al. Endothelial P-selectin as a target of heparin action in experimental melanoma lung metastasis. Cancer research. 2004;64(8):2743–2750. doi: 10.1158/0008-5472.can-03-1054. [DOI] [PubMed] [Google Scholar]
- 147.Qian F, Hanahan D, Weissman IL. L-selectin can facilitate metastasis to lymph nodes in a transgenic mouse model of carcinogenesis. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(7):3976–3981. doi: 10.1073/pnas.061633698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ravindranath MH, Amiri AA, Bauer PM, Kelley MC, Essner R, Morton DL. Endothelial-selectin ligands sialyl Lewis(x) and sialyl Lewis(a) are differentiation antigens immunogenic in human melanoma. Cancer. 1997;79(9):1686–1697. doi: 10.1002/(sici)1097-0142(19970501)79:9<1686::aid-cncr8>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 149.Ciolczyk-Wierzbicka D, Bodzioch M, Gil D, Zmudzinska D, Dembinska-Kiec A, Laidler P. Expression of fucosyltransferases contributes to melanoma invasive phenotype. Med Chem. 2007;3(5):418–424. doi: 10.2174/157340607781745401. [DOI] [PubMed] [Google Scholar]
- 150.Kunzendorf U, Kruger-Krasagakes S, Notter M, Hock H, Walz G, Diamantstein T. A sialyl-Le(x)-negative melanoma cell line binds to E-selectin but not to P-selectin. Cancer research. 1994;54(4):1109–1112. [PubMed] [Google Scholar]
- 151.Kaytes PS, Geng JG. P-selectin mediates adhesion of the human melanoma cell line NKI-4: identification of glycoprotein ligands. Biochemistry. 1998;37(29):10514–10521. doi: 10.1021/bi9730846. [DOI] [PubMed] [Google Scholar]
- 152.Miller N, Vile RG, Hart IR. Selectin ligands on human melanoma cells. Glycoconj J. 1996;13(1):33–43. doi: 10.1007/BF01049677. [DOI] [PubMed] [Google Scholar]
- 153.Barthel SR, Gavino JD, Wiese GK, Jaynes JM, Siddiqui J, Dimitroff CJ. Analysis of glycosyltransferase expression in metastatic prostate cancer cells capable of rolling activity on microvascular endothelial (E)-selectin. Glycobiology. 2008;18(10):806–817. doi: 10.1093/glycob/cwn070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Winkler IG, Barbier V, Nowlan B, et al. Vascular niche E-selectin regulates hematopoietic stem cell dormancy, self renewal and chemoresistance. Nature medicine. 2012;18(11):1651–1657. doi: 10.1038/nm.2969. [DOI] [PubMed] [Google Scholar]
- 155.Calabrese C, Poppleton H, Kocak M, et al. A perivascular niche for brain tumor stem cells. Cancer Cell. 2007;11(1):69–82. doi: 10.1016/j.ccr.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 156.Sullivan C, Chen Y, Shan Y, et al. Functional ramifications for the loss of P-selectin expression on hematopoietic and leukemic stem cells. PloS one. 2011;6(10):e26246. doi: 10.1371/journal.pone.0026246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110(6):673–687. doi: 10.1016/s0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 158.Danen EH, Sonnenberg A. Integrins in regulation of tissue development and function. J Pathol. 2003;201(4):632–641. doi: 10.1002/path.1472. [DOI] [PubMed] [Google Scholar]
- 159.Strell C, Entschladen F. Extravasation of leukocytes in comparison to tumor cells. Cell Commun Signal. 2008;6:10. doi: 10.1186/1478-811X-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Madsen CD, Sahai E. Cancer dissemination--lessons from leukocytes. Dev Cell. 19(1):13–26. doi: 10.1016/j.devcel.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 161.Fu G, Wang W, Luo BH. Overview: structural biology of integrins. Methods Mol Biol. 2012;757:81–99. doi: 10.1007/978-1-61779-166-6_7. [DOI] [PubMed] [Google Scholar]
- 162.Kuphal S, Bauer R, Bosserhoff AK. Integrin signaling in malignant melanoma. Cancer Metastasis Rev. 2005;24(2):195–222. doi: 10.1007/s10555-005-1572-1. [DOI] [PubMed] [Google Scholar]
- 163.Barthel SR, Johansson MW, McNamee DM, Mosher DF. Roles of integrin activation in eosinophil function and the eosinophilic inflammation of asthma. J Leukoc Biol. 2008;83(1):1–12. doi: 10.1189/jlb.0607344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Liang S, Dong C. Integrin VLA-4 enhances sialyl-Lewisx/a-negative melanoma adhesion to and extravasation through the endothelium under low flow conditions. Am J Physiol Cell Physiol. 2008;295(3):C701–707. doi: 10.1152/ajpcell.00245.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Klemke M, Weschenfelder T, Konstandin MH, Samstag Y. High affinity interaction of integrin alpha4beta1 (VLA-4) and vascular cell adhesion molecule 1 (VCAM-1) enhances migration of human melanoma cells across activated endothelial cell layers. J Cell Physiol. 2007;212(2):368–374. doi: 10.1002/jcp.21029. [DOI] [PubMed] [Google Scholar]
- 166.Jantscheff P, Schlesinger M, Fritzsche J, et al. Lysophosphatidylcholine pretreatment reduces VLA-4 and P-Selectin-mediated b16.f10 melanoma cell adhesion in vitro and inhibits metastasis-like lung invasion in vivo. Mol Cancer Ther. 10(1):186–197. doi: 10.1158/1535-7163.MCT-10-0474. [DOI] [PubMed] [Google Scholar]
- 167.Zhao J, Qi Q, Yang Y, et al. Inhibition of alpha(4) integrin mediated adhesion was involved in the reduction of B16-F10 melanoma cells lung colonization in C57BL/6 mice treated with gambogic acid. Eur J Pharmacol. 2008;589(1–3):127–131. doi: 10.1016/j.ejphar.2008.04.063. [DOI] [PubMed] [Google Scholar]
- 168.Cowden Dahl KD, Robertson SE, Weaver VM, Simon MC. Hypoxia-inducible factor regulates alphavbeta3 integrin cell surface expression. Mol Biol Cell. 2005;16(4):1901–1912. doi: 10.1091/mbc.E04-12-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Liapis H, Flath A, Kitazawa S. Integrin alpha V beta 3 expression by bone-residing breast cancer metastases. Diagn Mol Pathol. 1996;5(2):127–135. doi: 10.1097/00019606-199606000-00008. [DOI] [PubMed] [Google Scholar]
- 170.Cooper CR, Chay CH, Pienta KJ. The role of alpha(v)beta(3) in prostate cancer progression. Neoplasia. 2002;4(3):191–194. doi: 10.1038/sj.neo.7900224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Sloan EK, Pouliot N, Stanley KL, et al. Tumor-specific expression of alphavbeta3 integrin promotes spontaneous metastasis of breast cancer to bone. Breast Cancer Res. 2006;8(2):R20. doi: 10.1186/bcr1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hsu AR, Veeravagu A, Cai W, Hou LC, Tse V, Chen X. Integrin alpha v beta 3 antagonists for anti-angiogenic cancer treatment. Recent Pat Anticancer Drug Discov. 2007;2(2):143–158. doi: 10.2174/157489207780832469. [DOI] [PubMed] [Google Scholar]
- 173.Ghislin S, Obino D, Middendorp S, Boggetto N, Alcaide-Loridan C, Deshayes F. LFA-1 and ICAM-1 expression induced during melanoma-endothelial cell co-culture favors the transendothelial migration of melanoma cell lines in vitro. BMC Cancer. 12:455. doi: 10.1186/1471-2407-12-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Hanna S, Etzioni A. Leukocyte adhesion deficiencies. Ann N Y Acad Sci. 1250:50–55. doi: 10.1111/j.1749-6632.2011.06389.x. [DOI] [PubMed] [Google Scholar]
- 175.Si Z, Hersey P. Immunohistological examination of the relationship between metastatic potential and expression of adhesion molecules and ‘selectins’ on melanoma cells. Pathology. 1994;26(1):6–15. doi: 10.1080/00313029400169011. [DOI] [PubMed] [Google Scholar]
- 176.Luo Y, Ellis LZ, Dallaglio K, et al. Side population cells from human melanoma tumors reveal diverse mechanisms for chemoresistance. J Invest Dermatol. 132(10):2440–2450. doi: 10.1038/jid.2012.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rentala S, Yalavarthy PD, Mangamoori LN. Alpha1 and beta1 integrins enhance the homing and differentiation of cultured prostate cancer stem cells. Asian J Androl. 12(4):548–555. doi: 10.1038/aja.2010.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Rybak AP, He L, Kapoor A, Cutz JC, Tang D. Characterization of sphere-propagating cells with stem-like properties from DU145 prostate cancer cells. Biochim Biophys Acta. 1813(5):683–694. doi: 10.1016/j.bbamcr.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 179.Liu C, Kelnar K, Vlassov AV, Brown D, Wang J, Tang DG. Distinct microRNA expression profiles in prostate cancer stem/progenitor cells and tumor-suppressive functions of let-7. Cancer research. 72(13):3393–3404. doi: 10.1158/0008-5472.CAN-11-3864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Colombel M, Eaton CL, Hamdy F, et al. Increased expression of putative cancer stem cell markers in primary prostate cancer is associated with progression of bone metastases. Prostate. 72(7):713–720. doi: 10.1002/pros.21473. [DOI] [PubMed] [Google Scholar]
- 181.Lee KM, Han W, Kim JB, et al. The CD49d+/high subpopulation from isolated human breast sarcoma spheres possesses tumor-initiating ability. Int J Oncol. 40(3):665–672. doi: 10.3892/ijo.2011.1289. [DOI] [PubMed] [Google Scholar]
- 182.Wang L, Wang L, Gu Y, Shu Y, Shen Y, Xu Q. Integrin alpha6(high) cell population functions as an initiator in tumorigenesis and relapse of human liposarcoma. Mol Cancer Ther. 10(12):2276–2286. doi: 10.1158/1535-7163.MCT-11-0487. [DOI] [PubMed] [Google Scholar]
- 183.Paik DY, Janzen DM, Schafenacker AM, et al. Stem-like epithelial cells are concentrated in the distal end of the fallopian tube: a site for injury and serous cancer initiation. Stem Cells. 30(11):2487–2497. doi: 10.1002/stem.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Lathia JD, Gallagher J, Heddleston JM, et al. Integrin alpha 6 regulates glioblastoma stem cells. Cell Stem Cell. 6(5):421–432. doi: 10.1016/j.stem.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Alkatout I, Wiedermann M, Bauer M, Wenners A, Jonat W, Klapper W. Transcription factors associated with epithelial-mesenchymal transition and cancer stem cells in the tumor centre and margin of invasive breast cancer. Exp Mol Pathol. 94(1):168–173. doi: 10.1016/j.yexmp.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 186.Vieira AF, Ricardo S, Ablett MP, et al. P-cadherin is coexpressed with CD44 and CD49f and mediates stem cell properties in basal-like breast cancer. Stem Cells. 30(5):854–864. doi: 10.1002/stem.1075. [DOI] [PubMed] [Google Scholar]
- 187.Schober M, Fuchs E. Tumor-initiating stem cells of squamous cell carcinomas and their control by TGF-beta and integrin/focal adhesion kinase (FAK) signaling. Proceedings of the National Academy of Sciences of the United States of America. 108(26):10544–10549. doi: 10.1073/pnas.1107807108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bragado P, Estrada Y, Sosa MS, et al. Analysis of marker-defined HNSCC subpopulations reveals a dynamic regulation of tumor initiating properties. PloS one. 7(1):e29974. doi: 10.1371/journal.pone.0029974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Ali HR, Dawson SJ, Blows FM, Provenzano E, Pharoah PD, Caldas C. Cancer stem cell markers in breast cancer: pathological, clinical and prognostic significance. Breast Cancer Res. 13(6):R118. doi: 10.1186/bcr3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.van den Hoogen C, van der Horst G, Cheung H, et al. High aldehyde dehydrogenase activity identifies tumor-initiating and metastasis-initiating cells in human prostate cancer. Cancer research. 70(12):5163–5173. doi: 10.1158/0008-5472.CAN-09-3806. [DOI] [PubMed] [Google Scholar]
- 191.van den Hoogen C, van der Horst G, Cheung H, Buijs JT, Pelger RC, van der Pluijm G. Integrin alphav expression is required for the acquisition of a metastatic stem/progenitor cell phenotype in human prostate cancer. The American journal of pathology. 179(5):2559–2568. doi: 10.1016/j.ajpath.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.van der Horst G, van den Hoogen C, Buijs JT, et al. Targeting of alpha(v)-integrins in stem/progenitor cells and supportive microenvironment impairs bone metastasis in human prostate cancer. Neoplasia. 13(6):516–525. doi: 10.1593/neo.11122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Liu J, He X, Corbett SA, et al. Integrins are required for the differentiation of visceral endoderm. J Cell Sci. 2009;122(Pt 2):233–242. doi: 10.1242/jcs.037663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Salasznyk RM, Williams WA, Boskey A, Batorsky A, Plopper GE. Adhesion to Vitronectin and Collagen I Promotes Osteogenic Differentiation of Human Mesenchymal Stem Cells. J Biomed Biotechnol. 2004;2004(1):24–34. doi: 10.1155/S1110724304306017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Hurt EM, Chan K, Serrat MA, Thomas SB, Veenstra TD, Farrar WL. Identification of vitronectin as an extrinsic inducer of cancer stem cell differentiation and tumor formation. Stem Cells. 28(3):390–398. doi: 10.1002/stem.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Ruiz-Ontanon P, Orgaz JL, Aldaz B, et al. Cellular Plasticity Confers Migratory and Invasive Advantages to a Population of Glioblastoma-initiating Cells that Infiltrate Peritumoral Tissue. Stem Cells. doi: 10.1002/stem.1349. [DOI] [PubMed] [Google Scholar]
- 197.Zhu J, He J, Liu Y, Simeone DM, Lubman DM. Identification of glycoprotein markers for pancreatic cancer CD24+CD44+ stem-like cells using nano-LC-MS/MS and tissue microarray. J Proteome Res. 11(4):2272–2281. doi: 10.1021/pr201059g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Koukourakis MI, Giatromanolaki A, Tsakmaki V, Danielidis V, Sivridis E. Cancer stem cell phenotype relates to radio-chemotherapy outcome in locally advanced squamous cell head-neck cancer. Br J Cancer. 106(5):846–853. doi: 10.1038/bjc.2012.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Mukaida N, Baba T. Chemokines in tumor development and progression. Exp Cell Res. 2012;318(2):95–102. doi: 10.1016/j.yexcr.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 200.Mantovani A, Savino B, Locati M, Zammataro L, Allavena P, Bonecchi R. The chemokine system in cancer biology and therapy. Cytokine Growth Factor Rev. 2010;21(1):27–39. doi: 10.1016/j.cytogfr.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 201.Kuhnelt-Leddihn L, Muller H, Eisendle K, Zelger B, Weinlich G. Overexpression of the chemokine receptors CXCR4, CCR7, CCR9, and CCR10 in human primary cutaneous melanoma: a potential prognostic value for CCR7 and CCR10? Arch Dermatol Res. 2012;304(3):185–193. doi: 10.1007/s00403-012-1222-8. [DOI] [PubMed] [Google Scholar]
- 202.Toyozawa S, Kaminaka C, Furukawa F, Nakamura Y, Matsunaka H, Yamamoto Y. Chemokine receptor CXCR4 is a novel marker for the progression of cutaneous malignant melanomas. Acta Histochem Cytochem. 2012;45(5):293–299. doi: 10.1267/ahc.12004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Simonetti O, Goteri G, Lucarini G, et al. Potential role of CCL27 and CCR10 expression in melanoma progression and immune escape. Eur J Cancer. 2006;42(8):1181–1187. doi: 10.1016/j.ejca.2006.01.043. [DOI] [PubMed] [Google Scholar]
- 204.Wiley HE, Gonzalez EB, Maki W, Wu MT, Hwang ST. Expression of CC chemokine receptor-7 and regional lymph node metastasis of B16 murine melanoma. J Natl Cancer Inst. 2001;93(21):1638–1643. doi: 10.1093/jnci/93.21.1638. [DOI] [PubMed] [Google Scholar]
- 205.Murakami T, Cardones AR, Finkelstein SE, et al. Immune evasion by murine melanoma mediated through CC chemokine receptor-10. J Exp Med. 2003;198(9):1337–1347. doi: 10.1084/jem.20030593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ginestier C, Liu S, Diebel ME, et al. CXCR1 blockade selectively targets human breast cancer stem cells in vitro and in xenografts. J Clin Invest. 2010;120(2):485–497. doi: 10.1172/JCI39397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ramjeesingh R, Leung R, Siu CH. Interleukin-8 secreted by endothelial cells induces chemotaxis of melanoma cells through the chemokine receptor CXCR1. FASEB J. 2003;17(10):1292–1294. doi: 10.1096/fj.02-0560fje. [DOI] [PubMed] [Google Scholar]
- 208.Scala S, Giuliano P, Ascierto PA, et al. Human melanoma metastases express functional CXCR4. Clin Cancer Res. 2006;12(8):2427–2433. doi: 10.1158/1078-0432.CCR-05-1940. [DOI] [PubMed] [Google Scholar]
- 209.Hattermann K, Held-Feindt J, Lucius R, et al. The chemokine receptor CXCR7 is highly expressed in human glioma cells and mediates antiapoptotic effects. Cancer research. 2010;70(8):3299–3308. doi: 10.1158/0008-5472.CAN-09-3642. [DOI] [PubMed] [Google Scholar]
- 210.Hermann PC, Huber SL, Herrler T, et al. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1(3):313–323. doi: 10.1016/j.stem.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 211.Jung MJ, Rho JK, Kim YM, et al. Upregulation of CXCR4 is functionally crucial for maintenance of stemness in drug-resistant non-small cell lung cancer cells. Oncogene. 2013;32(2):209–221. doi: 10.1038/onc.2012.37. [DOI] [PubMed] [Google Scholar]
- 212.Murakami T, Maki W, Cardones AR, et al. Expression of CXC chemokine receptor-4 enhances the pulmonary metastatic potential of murine B16 melanoma cells. Cancer research. 2002;62(24):7328–7334. [PubMed] [Google Scholar]
- 213.Murakami T, Cardones AR, Hwang ST. Chemokine receptors and melanoma metastasis. J Dermatol Sci. 2004;36(2):71–78. doi: 10.1016/j.jdermsci.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 214.Peled A, Kollet O, Ponomaryov T, et al. The chemokine SDF-1 activates the integrins LFA-1, VLA-4, and VLA-5 on immature human CD34(+) cells: role in transendothelial/stromal migration and engraftment of NOD/SCID mice. Blood. 2000;95(11):3289–3296. [PubMed] [Google Scholar]
- 215.Braeuer RR, Shoshan E, Kamiya T, Bar-Eli M. The sweet and bitter sides of galectins in melanoma progression. Pigment Cell Melanoma Res. 2012;25(5):592–601. doi: 10.1111/j.1755-148X.2012.01026.x. [DOI] [PubMed] [Google Scholar]
- 216.Cedeno-Laurent F, Opperman MJ, Barthel SR, et al. Metabolic inhibition of galectin-1-binding carbohydrates accentuates antitumor immunity. J Invest Dermatol. 2012;132(2):410–420. doi: 10.1038/jid.2011.335. [DOI] [PMC free article] [PubMed] [Google Scholar]