Abstract
Background: Sildenafil citrate may increase endometrial thickness and affect the outcome of frozen-thawed embryo transfer cycles.
Objective: The aim of this study was to estimate the effect of sildenafil citrate on ultrasonographic endometrial thickness and pattern and to investigate the estrogen level on the day of progesterone administration, the implantation rate and chemical pregnancy rate in frozen embryo transfer cycles.
Materials and Methods: This randomized controlled trial was conducted on 80 patients who had an antecedent of poor endometrial response and frozen embryos. 40 patients were given estradiol by a step up method with menstruation to prepare the endometrium, and the other 40 were given sildenafil citrate tablets (50 mg) daily in addition to the above treatment protocol from the first day of the cycle until the day progesterone was started. This was discontinued 48-72 hours prior to the embryo transfer.
Results: The endometrial thickness was significantly higher in the sildenafil citrate group (p<0.0001), the triple line patterns of the endometrium were significantly higher in the sildenafil citrate group (p<0.0001), while the intermediate patterns of the endometrium were not significantly different in the two groups. The echogen patterns of the endometrium were significantly higher in control group (p<0.0001). Finally, implantation rate and the chemical pregnancy rates were higher in the sildenafil citrate group but not significantly.
Conclusion: As our study shows, the oral use of sildenafil citrate is a good way to improve the endometrial receptivity. We recommend the routine use of oral sildenafil citrate in patients with a previous failure of assisted reproduction technology cycles due to poor endometrial thickness.
Key Words: Sildenafil citrate, Endometrial thickness, Embryo transfer
Introduction
Despite the improvement in ovarian stimulation protocols and subsequent access to a number of dominant follicles, mature oocytes, and embryos for transfer, in vitro fertilization (IVF) has successfully reached a plateau. Therefore, more attention should be focused on implantation and endometrial receptivity. Implantation remains a major limiting step of assisted reproductive technology (ART) and uterine receptivity is essential for successful implantation in all species (1).
Successful implantation requires good embryo quality, appropriately timed and arranged endometrial receptivity, and efficient crosstalk between the embryo and the receptive endometrium. It is thought that the impairment of any one of these factors or biological processes may result in implantation failure (2).
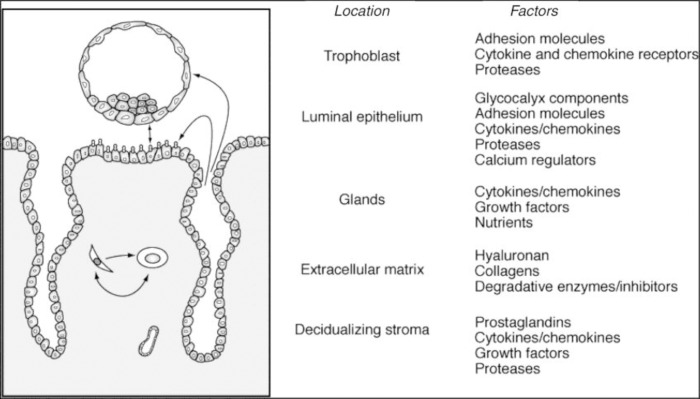
The endometrium is normally a non-receptive environment for an embryo, except during the window. Implantation window is a period during which the endometrium is optimally receptive to implanting blastocyst within the cycle days 20 and 24. It is characterized by a refractory endometrial status (3). Endometrial receptivity during the implantation window depends on the following factors (4-13).
Morphological Markers
Endometrial thickness
Endometrial echogenic pattern
Endometrial and sub endometrial blood flows
During implantation window, the endometrial epithelium encompasses four cell types: microvilli-rich cells, pinopode cells, vesiculated cells, and ciliated cells (14).
Biochemical Markers
Endometrial adhesion molecules
Endometrial anti-adhesion molecules
Endometrial cytokines
Growth factors
Endometrial immune markers
Endometrial Glycodelin
Insulin like growth factor (IGF)
Leukemia inhibitory factor (LIF).
The process of embryo implantation is described as having three phases
Apposition: “unstable adhesion” of the transferred embryo to the surface of the uterine lining.
Attachment (adhesion): “stable adhesion,” believed to involve signaling back and forth between the embryo and the lining.
Penetration (invasion): invasion of the trophectoderm cells from the embryo through the surface of the lining deeper the stroma of the uterine lining, forming a vascular connection to the mother (15).
In any of these stages, a number of the above factors are effective. There are 14 treatment options for improving the implantation:
(a) blastocyst transfer, (b) assisted hatching, (c) co-culture, (d) preimplantation genetic screening, (e) hysteroscopy, (f) sildenafil citrate, (g) salpingectomy for tubal disease, (h) oocyte donation, (i) transfer of six or more embryos, (j) intratubal embryo transfer, (k) natural-cycle IVF, (l) antiphospholipid antibodies (APA) testing and treatment, (m) allogenic lymphocyte therapy, and (n) IV immunoglobin therapy (15).
In this article, we have focused on endometrial thinning as a cause of implantation failure, and discuss its causes and treatment methods.
Causes of thin endometrium
Permanent damage to the basal endometrium.
Endometrial resistance to estrogen.
Reduced blood flow.
Over-exposure to testosterone.
Estrogen induced endometrial proliferation is in large part dependent upon blood flow to the basal endometrium (16).
Nitric oxide (NO) leads to relaxation of vascular smooth muscles through a cyclic guanyl monophosphate (cGMP) mediated pathway. Nitric oxide synthase isoforms have been identified in the vascular muscles of both human endometrium and myometrium. Phosphodiesterase (PDE) is a family of isoenzymes that hydrolyze cyclic nucleotides, such as cGMP. The inhibitors of specific Phosphodiesterase (PDE) subtypes have been identified with an ability to augment the effects of cyclic nucleotides on target tissues as the endometrium (16) .
Sildenafil citrate is a potent and selective inhibitor of cGMP specific phosphodiesterase type 5 (PDE5) that prevents the breakdown of cGMP and potentiates the effect of nitric oxide on vascular smooth muscles (17). Sildenafil citrate could lead to an improvement in uterine blood flow and, in conjunction with estrogen, led to the estrogen-induced proliferation of the endometrial lining (16).
Sildenafil citrate enhances uterine blood flow and increases endometrial thickening (18). The achieved implantation depends on the blastocyst’s ability to infiltrate the endometrium and develop a sustaining blood supply, which requires the following genes to produce the necessary proteins for digesting the endometrial cellular matrix, to regulate cell growth, and to induce angiogenesis:
a) Tumor suppressor factor (p53).
b) Plasminogen activator inhibitor 1 (PAI-1).
c) Vascularendothelial growth factor (VEGF) (15, 18, 19).
Sildenafil citrate was enhanced markedly in p53 and stimulated angiogenic responses with increased VEGF (20, 21). The aim of this study was to estimate the effect of sildenafil citrate on ultrasonographic endometrial thickness and pattern and to investigate the estrogen level on the day of progesterone administration, the implantation rate and chemical pregnancy rate in frozen embryo transfer cycles.
Materials and methods
Subjects
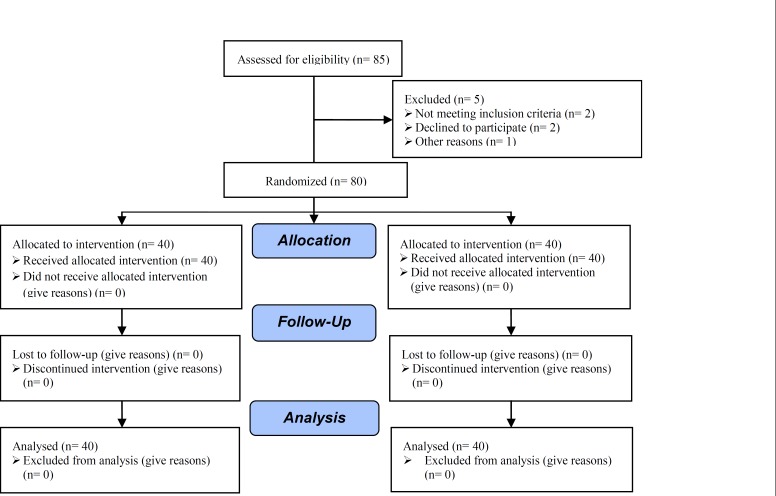
The study was a randomized clinical controlled trial, conducted in the Research and Clinical Center for Infertility affiliated to Shahid Sadoughi University of Medical Sciences between 2009-2011. The project was approved by the ethical committee of the infertility department of the university and was initiated after getting written consents from the participants and the financial support from the university. A total of 80 patients with an antecedent of poor endometrial response and frozen embryos were included in this study.
The inclusion criteria required the subjects to :
be younger than 40 years.
have high-quality frozen embryos.
The exclusion criteria included:
a history of endocrine diseases.
a history of hysteroscopic surgeries.
cardiovascular, renal and liver diseases.
hypotension (blood pressure <90/50 mmHg).
a history of stroke or myocardial infarction.
Treatment protocols
Patients who met these conditions entered the study and were divided into two groups based on randomized tables. To prepare the endometrium, one of the two groups was given estradiol by a step-up method while in menstruation. From the first to the fourth day of the menstrual cycle, 2 mg estradiol valerat tablets, from the 5th to the 8th day of the menstrual cycle, 4 mg estradiol valerat tablets, and from the 9th to the 12th day of the menstrual, 6 mg estradiol valerat tablets were given daily. The second group was given sildenafil citrate tablets (50 mg) daily in addition to the above treatment protocol from the first day of the cycle until the day of starting progesterone. It was discontinued 48-72 hours prior to the embryo transfer.
Assays
On the thirteenth day of the menstrual cycle, the endometrial thickness was estimated by transvaginal ultrasonography (arranged in a series every other day). The evaluations were performed by a single investigator. If the endometrial thickness was more than 8mm, 100 mg of progesterone was injected intramuscularly. Then estrogen and progesterone were measured in the blood samples in an hour, and, after three days, embryos were transferred.
Outcome
Administering stradiol valerat and progesterone continued until two weeks after the embryos were transferred. In case BHCG was tested and proved to be positive, estradiol valerat and progesterone were continueed until the 11th week of pregnancy. Then, four weeks after the embryo transfer, the number of gestational sacs were determined by vaginal ultrasound.
Statistical analysis
After data collection and coding, the data were entered into the computer. Using version 18 of SPSS software, Mann-Whitney test, Chi-square, and independent-samples T-test, the results were analyzed.
Results
The patients were divided into two groups based on randomized tables. The basal patients’ variables are shown in Table I. There was no significant difference between the two groups. Long cycle, estrogen, progesterone, and estrogen/ progesterone ratio on the progesterone day was significantly different in the two groups, but LH on the progesterone day was not significantly different in the two groups (Table II). Endometrial thickness was significantly higher in the sildenafil citrate group (p<0.0001).
Table I.
Characteristics of patients at the beginning of the cycle
| Variable | Control group (mean) | Sildenafil citrate group (mean) | p-value |
|---|---|---|---|
| Infertility duration (months) | 71 | 75 | 0.39 |
| Age (years) | 28 | 29 | 0.47 |
| Basal FSH ( IU/L) | 5.4 | 5.6 | 0.4 |
| Basal LH ( IU/L) | 8.765 | 8.77 | 1 |
| Basal estrogen (pg/mL) | 55.8 | 56.5 | 0.73 |
| Basal progesterone (ng/ml) | 0.66 | 0.645 | 0.7 |
| Basal FSH/LH | 0.7 | 0.72 | 0.7 |
Table II.
Effect of sildenafil citrate on long cycle, progesterone, estrogen, estrogen/ progesterone and LH on progesterone day, endometrial thickness, and implantation rate
| Variable | Control group (mean) | Sildenafil citrate group (mean) | p-value |
|---|---|---|---|
| Duration cycle ( days) | 13.375 | 12.125 | <0.0001 |
| Progesterone on progesterone day (ng/mL) | 0.88 | 1.12 | <0.0001 |
| Estrogen on progesterone day (pg/mL) | 984.5 | 643.5 | <0.0001 |
| Estrogen/ progesterone on progesterone day | 0.9 | 0.73 | <0.0001 |
| LH on progesterone day (IU/L) | 1.13 | 1.1 | 0.98 |
| Endometrial thickness (mm) | 8.0 | 9.8 | <0.0001 |
| Implantation rate (%) | 8.75 | 14.16 | 0.22 |
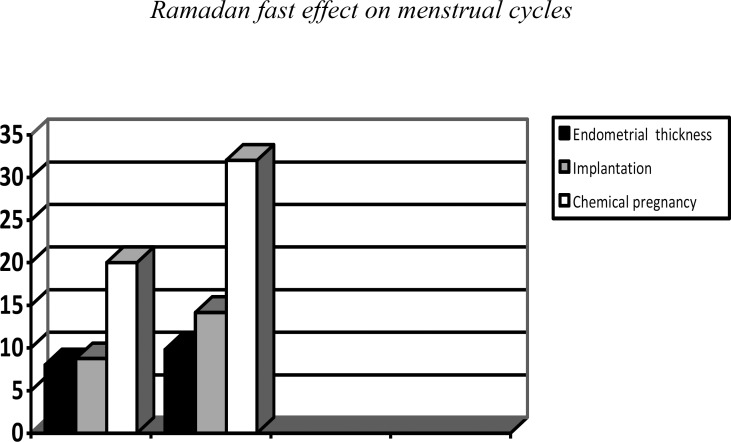
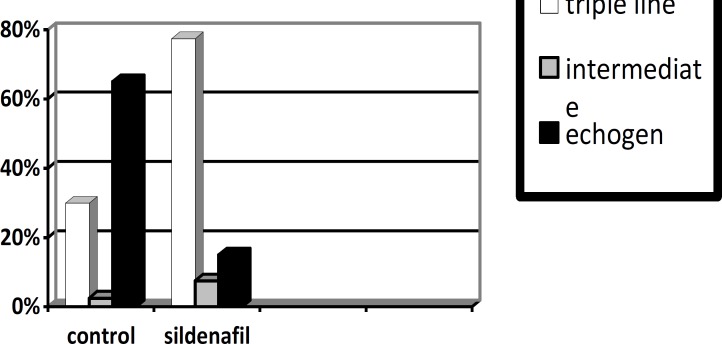
Implantation rate was higher in the sildenafil citrate group but not significantly (p=0.22). The triple line pattern of the endometrium was significantly higher in the sildenafil citrate group (p<0.0001), while the intermediate pattern of the endometrium was not significantly different in the two groups, the echogen pattern of the endometrium was significantly higher in the control group (p<0.0001) (Table III). Finally chemical pregnancy rates were higher in the sildenafil citrate group but not significantly (Figure I, II).
Table III.
Effect of FSH/LH ratio on endometrial pattern and chemical pregnancy
|
Variable
(mm) |
Control group | Sildenafil citrate group | p-value | ||
|---|---|---|---|---|---|
| + | - | + | - | ||
| Triple line | 12 (30%) | 28 (70%) | 31 (77.5%) | 9 (22.5%) | <0.0001 |
| Intermediate | 1 (2.5%) | 39 (97.5%) | 3 (7.5%) | 37 (92.5%) | 0.3 |
| Echogen | 26 (65%) | 14 (35%) | 6 (15%) | 34 (85%) | <0.0001 |
| Chemical pregnancy | 8 (20%) | 32 (80%) | 13 (32%) | 27 (68%) | 0.13 |
Figure 1.
Factors regulated during the early stages of implantation. (Diedrich et al Hum Reprod Update 2007; 13: 365-377)
Figure 2.
Comparison of endometrial thickness, implantation, and chemical pregnancy in the two groups
Figure 3.
Comparison of echogen, intermediate and triple line pattern of endometrium in the two groups
Figure 4.
Consort flow diagram
Discussion
In this study, we evaluated the effect of sildenafil citrate on the outcome of frozen-thawed embryo transfer cycles. Endometrial growth seems to be dependent on uterine artery blood flow, and the importance of endometrial development in the pregnancy outcome has been already reported (22, 23). A positive linear correlation between endometrial thickness measured on the hCG day and pregnancy rate (PR) was identified (24). A good correlation has been found between endometrial thickness and the prevalence of conception. An endometrial thickness of ≥9 mm in the late proliferative phase, as determined by vaginal ultrasound, correlates well with the chance of pregnancy after IVF, whereas a thinner endometrium is associated with poorer prognosis for success (23).
Sildenafil citrate improves the uterine artery blood flow and the sonographic endometrial thickening in patients with a prior assisted reproductive cycle failing due to poor endometrial response (16, 23, 25). Increased endometrial thickness is associated with higher pregnancy rates. However, no attainment of pregnancy was predicted by endometrial thickness alone (26). In our study, sildenafil citrate clearly increased endometrial thickness (9.8 mm vs. 8 mm), and the chemical pregnancy rates were higher in the sildenafil citrate group but not significantly.
Uterine receptivity was assessed simultaneously by measuring vasoactive cytokines possibly involved in the development of spiral arteries and assessing endometrial and uterine arterial blood flow (1). Endometrial and subendometrial blood flows measured by vaginal color Doppler ultrasound are a good predicator of pregnancy during IVF treatment (6, 27). The present results confirm and extend previous observations that the advanced hyperechogenic transformation of the endometrium is associated with poor in vitro fertilization and embryo transfer (IVF-ET) outcome (28).
In our study, sildenafil citrate increased the triple line pattern of the endometrium but decreased its echogen pattern. A combined analysis of endometrial thickness and pattern on the day of hCG administration proved to be a better predictor of the outcome of IVF/ICSI-ET and may be more helpful for patient counseling than a separate analysis (29). Elevated estrogen concentrations may increase sensitivity to progesterone action and, thus, lead to secretory advancement (30). Estrogen/progesterone ratios, which are also associated with the impairment of endometrial receptivity, are the main factors affecting receptivity (31). In this study, sildenafil citrate significantly decreased the estrogen, progesterone and estrogen/ progesterone ratio on the progesterone day.
Conclusion
In our study, it was shown that the oral use of sildenafil citrate can be a good way to improve endometrial receptivity. We recommend the routine use of oral sildenafil citrate in patients with a previous failure of assisted reproduction technology cycles due to poor endometrial thickness.
Acknowledgements
The authors are thankful to the admissions, as well as the lab and operation room team of the Research and Clinical Center for Infertility for their assistance and financial support.
Conflict of interest
There is no conflict of interest in this study.
References
- 1.Ledee N, Chaouat G, Serazin V, Lombroso R, Dubanchet S, Oger P, et al. Endometrial vascularity by three-dimensional power Doppler ultrasound and cytokines: a complementary approach to assess uterine receptivity. J Reprod Immunol. 2008;77:57–62. doi: 10.1016/j.jri.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Maruyama T. Therapeutic Strategies for Implantation Failure due to Endometrial Dysfunction. J Mammal Ova Res. 2009;26:129–133. [Google Scholar]
- 3.Bergh PA, Navot D. The impact of embryonic development and endometrial maturity on the timing of implantation. Fertil Steril. 1992;58:537–542. doi: 10.1016/s0015-0282(16)55259-5. [DOI] [PubMed] [Google Scholar]
- 4.Critchley HOD, Saunders PTK. Hormone Receptor Dynamics in a Receptive Human Endometrium. Reprod Sci. 2009;16:191–199. doi: 10.1177/1933719108331121. [DOI] [PubMed] [Google Scholar]
- 5.Dharmaraj N, Wang P, Carson DD. Cytokine and Progesterone Receptor Interplay in the Regulation of MUC1 Gene Expression. Mol Endocrinol. 2010;24:2253–2266. doi: 10.1210/me.2009-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao MZ, Zhao XM, Li WY, Liu GM, Jia XF, Zhang HQ. Assessment of Uterine Receptivity by Endometrial and Subendometrial Blood Flows Measured by Vaginal Color Doppler Ultrasound in Women Undergoing IVF Treatment. J Reprod Contracept. 2007;18:205–212. [Google Scholar]
- 7.Kim J, Fazleabas A. Uterine receptivity and implantation: The regulation and action of insulin-like growth factor binding protein-1 (IGFBP-1), HOXA10 and forkhead transcription factor-1 (FOXO-1) in the baboon endometrium. Reprod Biol Endocrinol. 2004;2:34. doi: 10.1186/1477-7827-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ding T, Song H, Wang X, Khatua A, Paria BC. Leukemia inhibitory factor ligand-receptor signaling is important for uterine receptivity and implantation in golden hamsters (Mesocricetus auratus) Reproduction. 2008;135:41–53. doi: 10.1530/REP-07-0013. [DOI] [PubMed] [Google Scholar]
- 9.Meseguer M, Aplin JD, Caballero-Campo P, O'Connor JE, Martin JC, Remohi J, et al. Human endometrial mucin MUC1 is up-regulated by progesterone and down-regulated in vitro by the human blastocyst. Biol Reprod. 2001;64:590–601. doi: 10.1095/biolreprod64.2.590. [DOI] [PubMed] [Google Scholar]
- 10.Dimitriadis E, White CA, Jones RL, Salamonsen LA. Cytokines, chemokines and growth factors in endometrium related to implantation. Hum Reprod Update. 2005;11:613–630. doi: 10.1093/humupd/dmi023. [DOI] [PubMed] [Google Scholar]
- 11.DeLoia JA, Krasnow JS, Brekosky J, Babaknia A, Julian J, Carson DD. Regional specialization of the cell membrane-associated, polymorphic mucin (MUC1) in human uterine epithelia. Hum Reprod. 1998;13:2902–2909. doi: 10.1093/humrep/13.10.2902. [DOI] [PubMed] [Google Scholar]
- 12.Kimber SJ. Leukaemia inhibitory factor in implantation and uterine biology. Reproduction. 2005;130:131–145. doi: 10.1530/rep.1.00304. [DOI] [PubMed] [Google Scholar]
- 13.Damario MA, Lesnick TG, Lessey BA, et al. Endometrial markers of uterine receptivity utilizing the donor oocyte model. Hum Reprod. 2001;16:1893–1899. doi: 10.1093/humrep/16.9.1893. [DOI] [PubMed] [Google Scholar]
- 14.Bartosch C, Lopes JM. "Human Endometrium Ultrastructure during the Implantation Window: A New Perspective of the Epithelium Cell Types.". Reprod Sci. 2011;18:525–539. doi: 10.1177/1933719110392055. [DOI] [PubMed] [Google Scholar]
- 15.Ly D, Nabil KA, Joelle S, Agarwal A. Evidence-Based Management of Infertile Couples with Repeated Implantation Failure Following IVF. Current Women’s Health Reviews. 2010;6:200–218. [Google Scholar]
- 16.Sher G, Fisch JD. Effect of vaginal sildenafil citrate on the outcome of in vitro fertilization (IVF) after multiple IVF failures attributed to poor endometrial development. Fertil Steril. 2002;78:1073–1076. doi: 10.1016/s0015-0282(02)03375-7. [DOI] [PubMed] [Google Scholar]
- 17.Sher G, Fisch JD. Vaginal sildenafil citrate (Viagra): a preliminary report of a novel method to improve uterine artery blood flow and endometrial development in patients undergoing IVF. Hum Reprod. 2000;15:806–809. doi: 10.1093/humrep/15.4.806. [DOI] [PubMed] [Google Scholar]
- 18.Richter KS, Bugge KR, Bromer JG, Levy MJ. Relationship between endometrial thickness and embryo implantation, based on 1,294 cycles of in vitro fertilization with transfer of two blastocyst-stage embryos. Fertil Steril. 2007;87:53–59. doi: 10.1016/j.fertnstert.2006.05.064. [DOI] [PubMed] [Google Scholar]
- 19.Goodman C, Jeyendran RS, Coulam CB. P53 tumor suppressor factor, plasminogen activator inhibitor, and vascular endothelial growth factor gene polymorphisms and recurrent implantation failure. Fertil Steril. 2009;92:494–498. doi: 10.1016/j.fertnstert.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 20.Di X, Gennings C, Bear H, Graham L, Sheth C, White K, Gewirtz D. Influence of the phosphodiesterase-5 inhibitor, sildenafil citrate, on sensitivity to chemotherapy in breast tumor cells. Breast Cancer Res Treat. 2007;124:349–360. doi: 10.1007/s10549-010-0765-7. [DOI] [PubMed] [Google Scholar]
- 21.Pyriochou A, Zhou Z, Koika V, Petrou C, Cordopatis P, Sessa WC, Papapetropoulos A. The phosphodiesterase 5 inhibitor sildenafil citrate stimulates angiogenesis through a protein kinase G/MAPK pathway. J Cell Physiol. 2007;211:197–204. doi: 10.1002/jcp.20929. [DOI] [PubMed] [Google Scholar]
- 22.Kelly SM, Sladkevicius P, Campbell S, Nargund G. Investigation of the infertile couple: a one-stop ultrasound-based approach. Hum Reprod. 2001;16:2481–2484. doi: 10.1093/humrep/16.12.2481. [DOI] [PubMed] [Google Scholar]
- 23.Jerzak M, Kniotek M, Mrozek J. Sildenafil citrate citrate decreased natural killer cell activity and enhanced chance of successful pregnancy in women with a history of recurrent miscarriage. Fertil Steril. 2008;90:1848–1853. doi: 10.1016/j.fertnstert.2007.08.043. [DOI] [PubMed] [Google Scholar]
- 24.Takasaki A, Tamura H, Miwa I, Taketani T, Shimamura K, Sugino N. Endometrial growth and uterine blood flow: a pilot study for improving endometrial thickness in the patients with a thin endometrium. Fertil Steril. 2010;93:1851–1858. doi: 10.1016/j.fertnstert.2008.12.062. [DOI] [PubMed] [Google Scholar]
- 25.Paulus WE, Strehler E, Zhang M, Jelinkova L, El-Danasouri I, Sterzik K. Benefit of vaginal sildenafil citrate citrate in assisted reproduction therapy. Fertil Steril. 2002;77:846–847. doi: 10.1016/s0015-0282(01)03272-1. [DOI] [PubMed] [Google Scholar]
- 26.Kovacs P, Matyas S, Boda K, Kaali SG. The effect of endometrial thickness on IVF/ICSI outcome. Hum Reprod. 2003;18:2337–2341. doi: 10.1093/humrep/deg461. [DOI] [PubMed] [Google Scholar]
- 27.Wang L, Qiao J, Li R, Zhen X, Liu Z. Role of endometrial blood flow assessment with color Doppler energy in predicting pregnancy outcome of IVF-ET cycles. Reprod Biol Endocrinol. 2010;8:1–7. doi: 10.1186/1477-7827-8-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fanchin R, Righini C, Ayoubi JM, Olivennes F, de Ziegler D, Frydman R. New look at endometrial echogenicity: objective computer-assisted measurements predict endometrial receptivity in in vitro fertilization-embryo transfer. Fertil Steril. 2000;74:274–281. doi: 10.1016/s0015-0282(00)00643-9. [DOI] [PubMed] [Google Scholar]
- 29.Chen SL, Wu FR, Luo C, Chen X, Shi XY, Zheng HY, Ni YP. Combined analysis of endometrial thickness and pattern in predicting outcome of in vitro fertilization and embryo transfer: a retrospective cohort study. Reprod Biol Endocrinol. 2010;8:30. doi: 10.1186/1477-7827-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pellicer A, Valbuena D, Cano F, Remohi J, Simon C. Lower implantation rates in high responders: evidence for an altered endocrine milieu during the preimplantation period. Fertil Steril. 1996;65:1190–1195. doi: 10.1016/s0015-0282(16)58337-x. [DOI] [PubMed] [Google Scholar]
- 31.Macklon NS, Fauser BC. Impact of ovarian hyperstimulation on the luteal phase. J Reprod Fertil. 2000;55(Suppl):101–108. [PubMed] [Google Scholar]