Abstract
Background/Aims
This report and review of literature aimed to assess the feasibility of condylar distraction in humans and its esthetic and functional outcome.
Methods
We present a case series of eight TMJ ankylosis patients, where after a gap arthroplasty, ramus condyle unit was reconstructed using transport distraction to analyze its feasibility, esthetic and functional outcome and success.
Results
All patients had satisfactory mouth opening, and minimal pain in their follow-up period.
Conclusion
Condylar transport distraction osteogenesis holds promise for successful TMJ reconstruction and should be the method of choice as it does not involve secondary surgery or need for an alloplast.
Keywords: Transport distraction osteogenesis, Condylar distraction, Neocondyle
Introduction
Temporo-mandibular joint (TMJ) is one of the most complex synovial joints of the human body that allows both hinge and translational movements. TMJ ankylosis is a bony or fibrous union of the disk–condyle complex to the articular surface of the temporal bone leading to restriction of mandibular movements. Congenital deformities, traumatic injuries, or tumors may also require removal of deformed condyle and reconstruction to maintain the function. The goals of TMJ reconstruction include restoration of ramal height and posterior lower facial height, avoid any occlusal discrepancies or anterior open bite.
Autogenous bone grafts like costochondral, sternoclavicular are considered gold standard in TMJ reconstruction, but have their own disadvantages such as donor site morbidity, need for fixation with plates or screws, absence of cartilaginous cap, shape difference and extra growth potential. Partial and total reconstruction, using both autogenous and alloplastic materials, have been done to rehabilitate joints that are anatomically compromised, and dysfunctional.
We present a case series of eight TMJ ankylosis patients, where after a gap arthroplasty, ramus condyle unit was reconstructed using transport distraction.
Case series
Eight cases of TMJ ankylosis, in the age range of 4–17 years, who reported to our outpatient clinic with the chief complaint of restricted mouth opening and diagnosed as cases of TMJ ankylosis were included in this series (Table 1). Written informed consent was obtained from their parents or guardians. Study was ethically approved by the institutional research committee.
Table 1.
Case series.
| No. | Age (years) | Sex | Diagnosis | Space between the leading edge and articular eminence (mm) | MMOa (mm) |
Ramal length( in mm) |
Condylar positionb | GPc (mm) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-operative | Post-operative | Pre-operative | Post-operative | |||||||
| 1 | 14 | F | Right TMJ ankylosis | 12 | 3 | 38 | 50 | 58 | Adequate | 3 |
| 2 | 7 | F | Left TMJ ankylosis | 11 | 1 | 36 | 46 | 52 | Adequate | 2 |
| 3 | 8 | F | Right TMJ ankylosis | 13 | 0 | 37 | 40 | 48 | Adequate | 2 |
| 4 | 9 | M | Left TMJ ankylosis | 11 | 8 | 39 | 45 | 49 | Adequate | 3 |
| 5 | 13 | F | Right TMJ ankylosis | 14 | 0 | 42 | 52 | 56 | Adequate | 2 |
| 6 | 12 | M | Left TMJ ankylosis | 11 | 1 | 36 | 54 | 59 | Adequate | 3 |
| 7 | 7 | M | Right TMJ ankylosis | 12 | 2 | 37 | 50 | 59 | Adequate | 3 |
| 8 | 8 | F | Left TMJ ankylosis | 9 | 4 | 37 | 52 | 56 | Adequate | 1 |
Maximum mouth opening measured from maxillary incisal edge to mandibular incisal edge.
Condylar position in glenoid fossa (adequate/inadequate).
Gap between glenoid fossa and condylar head.
All patients were anesthetized under general anesthesia with nasoendotracheal blind or fibreoptic intubation. Gap arthroplasty was performed using standard Al-Kayat Bramley incision, creating a gap of about 1 cm. Temporalis fascia was used as the interpositional material (Fig. 1A). The mandibular ramus was approached through a 2 cm long incision made below the angle of the mandible (Fig. 1B). A transport disc was created at the condylar end with a partially completed L-shaped osteotomy (Fig. 1C). Length of the distractor was selected on the basis of the amount of distraction planned to reach the glenoid fossa. The distractor was placed to mark the osteotomy and screw holes were drilled. The vector was oriented in such a way that the superior fragment distracted toward the glenoid fossa (Fig. 1D). Distractor was removed for completion of the osteotomy cut, and then later re-fixed to the superior and inferior fragments at already marked position. Distraction of the fragment was carried out at the rate of 1 mm per day after a latency period of 7 days. Defect was quantified by combining vertical ramal deficiency and the surgical defect created after gap arthroplasty. This was used to assess the amount and duration of distraction. OPG after completion of distraction ensures proper condylar position in the glenoid fossa (Fig. 2A and B). Mouth opening exercises and physiotherapy were started 48 h after the operation. All patients were followed up for at least 6 months. The regenerate bone was allowed to consolidate for at least 3 months before removal of distractors. During this time, the distractor acted as an internal fixation device.
Fig. 1.
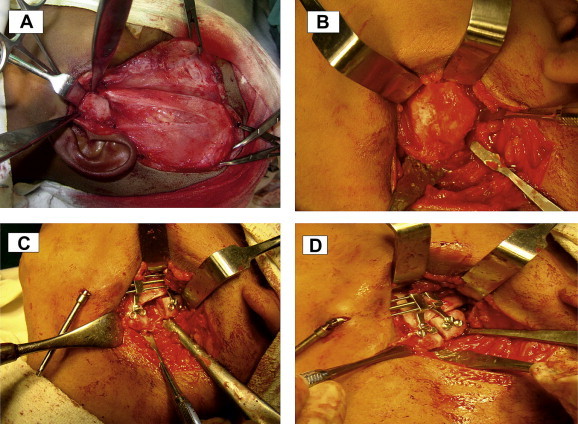
A: Gap arthroplasty was performed using standard Al-Kayat Bramley incision, creating a gap of about 1 cm. B: The mandibular ramus was approached through a 2 cm long incision made below the angle of the mandible. C: A transport disc was created at the condylar end with a partially completed L-shaped osteotomy. D: The distractor was opened and closed to its original position to check the vector and to ensure proper working.
Fig. 2.

A: Post-operative OPG showing the start of transport disc toward glenoid fossa. B: OPG after completion of distraction showing proper condylar position in the glenoid fossa. C: OPG after removal of distractor showing good bone formation.
Outcome evaluation was done by measuring maximal mouth opening, jaw movements in protrusive and lateral excursions, assessment of ramal height, posterior lower facial height, any occlusal discrepancies or anterior open bite.
Discussion
Transport distraction osteogenesis (TDO), is a slow movement of a segment of bone called the transport disc into the defect. Bone regeneration occurs at the trailing edge of the transport disc resulting in bridging the defect without the need for bone graft. Condylar distraction provides the advantage of formation of cartilaginous capsule at the end of the transport disc.1
Stucki-McCormick et al (1999)2 were the first to publish two cases of RCU reconstruction using transport distraction osteogenesis (Table 2). Their study has no long-term follow-up, but they clearly demonstrated the technique's potential. Subsequent animal studies confirmed the biological principles of regenerate bone formation at the trailing edge and fibrocartilage formation at the leading edge of the transport disc.3,6
Table 2.
Review of literature.
| Author | Model | Quantity of sample | Observations | Remarks |
|---|---|---|---|---|
| Stucki McCormick2 (1999) | Humans | Two | After distraction, bone remodeled, inducing a new cortical layer on the articular surface | A pseudodisk was generated as a result of the transport distraction |
| Hikiji et al3 (2000) | Adult rabbit | Twelve male Japanese white, 4–6 months old, weight 1.5–2.0 kg | Observed endochondral ossification within distraction gap and intramembranous ossification at upper surface of new condyle | Observed endochondral ossification occurring within the distraction gap, which was attributed to the constant application of the masticatory force |
| Zhu et al4 (2006) | Adult rhesus monkeys | Six | Bone regeneration perfect in distraction gap between the transport disc and existing mandible | A neocondyle with functional shape can be created by transport distraction osteogenesis |
| Schwartz and Relle5 (2008) | Humans | Thirteen RCU in 12 patients | Successful distraction osteogenesis in all cases. There were no complications | TDO for TMJ reconstruction shares all of the advantages of autogenous bone grafting without the disadvantages of a donor site |
| Zhu et al6 (2008) | Goats | Forty-four growing goats | Neocondyle reconstructed by means of transport distraction had potential to grow under functional stimuli of TMJ | TDO may serve as an alternative method for condylar reconstruction in growing individuals |
| Eski et al7 (2008) | Humans | Three | One of the greatest advantage of the transport distraction technique is to create a functioning joint without using interpositional material | Transport distraction of osteotomized segment creates a pseudojoint between neocondyle and glenoid fossa |
| Cheung et al8 (2009) | Adult goats | Twelve | Both transport distraction and costochondral graft established a neocondyle separating from the pseudo-disc with a joint space | TDO is an effective reconstruction method for TMJ ankylosis, matching costochondral grafting |
| Meng et al9 (2012) | Adult rabbit | Twelve | The bony transport disc gradually remodeled to a new condyle similar to the original condyle in appearance and structure. The surface of the transport disc was covered with a fibrous tissue | TDO at the condylar neck can be performed concurrently with arthroplasty of TMJ ankylosis |
Hikiji et al (2000)3 reported presence of cartilaginous cells and ossification of the cartilaginous matrix in the upper surface of transport disk. The sources of cartilaginous cells were probably derived from undifferentiated mesenchymal cells in the bone marrow and internal periosteum, which was activated by biologic signals associated with the trauma. Such a pattern of bone formation was in accordance with the osteogenetic pattern of secondary cartilage. However, considering the obvious differences in anatomy and function of the TMJ between humans and rabbits, further study was necessary.3
Zhu et al (2008) conducted an experimental investigation in 44 growing goats and suggested that a neocondyle reconstructed by means of transport distraction had the potential to grow under functional stimuli of the temporomandibular joint. They found the technique to serve as an alternative method for condylar reconstruction in growing individuals.4,6 Further animal studies conducted by Meng et al confirmed the formation of neocondyle with pseudoarthrosis, after 8 weeks of consolidation. Initially, at 4 weeks of distraction, they observed a new articulation between the glenoid fossa and transport disk. They reported that the joint space was filled with fibrous connective tissue. They noticed a densely cellular layer adjacent to the upper surface of the transport disk. The neocondyle got covered with a cap of fibrous tissue at 8 weeks. Remodeling activity was evident in the fibrous bone interface areas. Clusters of cartilaginous cells were scattered, and few cartilage were observed. In addition, the subchondral bone in the upper surface of the transport disk exhibited apparent remodeling, flattening, and sclerosis, similar to the developed pseudoarthrosis.9
Costochondral graft was compared with condylar transport distraction for reconstruction of temporomandibular joint in goats and it was found to be an effective reconstruction method for TMJ ankylosis, matching the gold standard of costochondral graft.8 Zheng et al. conducted bilateral condylectomies with disc preservation in 12 adult goats. Transport distraction of the Ramus condyle unit was performed on one side and costochondral graft on the other side. They concluded that there was no difference between both of the reconstructive techniques.10
Schwartz (2009) demonstrated the surgical technique for reconstruction of ramus condyle unit in an elucidative manner, with possible incisions, osteotomy techniques and direction of vector for distractor movements after their clinical study of thirteen TMJ reconstructions. They observed successful distraction in all cases, with no complications and development of solid regenerate bone and good articulation.5 Transport distraction of osteotomized segment creates a pseudojoint between neocondyle and glenoid fossa.7 In our series of eight TMJ ankylosis cases, we too achieved successful results in all of them. It is important to have a proper osteotomy cut, correct vector for distraction, and rounding of the superior portion of the transport disc to ensure proper reconstruction.
Conclusion
Condylar transport distraction osteogenesis holds promise for successful TMJ reconstruction and should be the method of choice as it does not involve secondary surgery or need for an alloplast.
Conflicts of interest
All authors have none to declare.
References
- 1.Constantino P.D., Friedman C.D., Shindo M.L., Houston G., Sr Sisson GA. Experimental mandibular regrowth by distraction osteogenesis: long-term results. Arch Otolaryngol Head Neck Surg. 1993;119:511–516. doi: 10.1001/archotol.1993.01880170035007. [DOI] [PubMed] [Google Scholar]
- 2.Stucki-McCormick S.U. Reconstruction of the mandibular condyle using transport distraction osteogenesis. J Craniofac Surg. 1997;8:48–52. doi: 10.1097/00001665-199701000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Hikiji H., Takato T., Matsumoto S., Mori Y. Experimental study of reconstruction of the temporomandibular joint using a bone transport technique. J Oral Maxillofac Surg. 2000;58:1270–1276. doi: 10.1053/joms.2000.16628. [DOI] [PubMed] [Google Scholar]
- 4.Zhu S.S., Hu J., Li J., Ying B. Reconstruction of mandibular condyle by transport distraction osteogenesis: experimental study in rhesus monkey. J Oral Maxillofac Surg. 2006;64:1487–1492. doi: 10.1016/j.joms.2006.03.037. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz H.C., Relle R.J. Distraction osteogenesis for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2008;66:718–723. doi: 10.1016/j.joms.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 6.Zhu S.S., Hu J., Ying B.B., Li J.H. Growth of the mandible after condylar reconstruction using transport distraction osteogenesis: an experimental investigation in goats. Plast Reconstr Surg. 2008;121(5):1760–1767. doi: 10.1097/PRS.0b013e31816b78dd. [DOI] [PubMed] [Google Scholar]
- 7.Eski M., Deveci M., Zor F., Sengezer M. Treatment of temporomandibular joint ankylosis and facial asymmetry with bidirectional transport distraction osteogenesis technique. J Craniofac Surg. 2008;19(3):732–739. doi: 10.1097/SCS.0b013e31816b6bf0. [DOI] [PubMed] [Google Scholar]
- 8.Cheung L.K., Zheng L.W., Shi X.J. Transport distraction versus costochondral graft for reconstruction of temporomandibular joint ankylosis: which is better? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:32–40. doi: 10.1016/j.tripleo.2009.02.030. [DOI] [PubMed] [Google Scholar]
- 9.Meng Q., Yang X., Long X., Li J., Cai H. Correction of rabbit model with mandibular ramus shortening by distraction osteogenesis at condylar neck. J Oral Maxillofac Surg. 2012;70(4):931–940. doi: 10.1016/j.joms.2011.02.099. [DOI] [PubMed] [Google Scholar]
- 10.Zwahlen R.A., Cheung Lim Kwong. Comparison of distraction osteogenesis versus costochondral graft in reconstruction of temporomandibular joint condylectomy with disc preservation. J Oral Maxillofac Surg. 2011;69:409–417. doi: 10.1016/j.joms.2010.05.032. [DOI] [PubMed] [Google Scholar]


