Abstract
Problem considered
This clinical report describes the prosthodontic treatment of an 18-year-old female diagnosed with amelogenesis imperfecta.
Materials and method
The specific objectives of the treatment were to restore esthetics and masticatory function. Metal-ceramic fixed partial dentures were fabricated at the existing vertical dimension of occlusion utilizing the PMS occlusal scheme.
Results
Clinical examination of the patient 12 months after treatment revealed no evidence of disease or degeneration of the restored teeth.
Conclusion
The patient's esthetic and functional expectations were satisfied.
Keywords: Amelogenesis imperfecta, Hypoplasia, Hypocalcification, Hypomaturation, Full mouth rehabilitation
Introduction
Amelogenesis imperfecta is an inherited disorder associated with defective ameloblasts. It is reported to have an incidence of one person in every 16,000.1 Amelogenesis imperfecta (AI) was first described in 1890, but not until 1938 did Finn classify it as a separate entity from dentinogenesis imperfecta.2 Defects in enamel formation fall in three categories, each of which develops by a different mode of inheritance. The characteristics of the first group, termed enamel hypoplasia, include an imperfectly formed matrix, deficiencies in the quantity of enamel formed, and irregular deposition of enamel. Enamel hypoplasia seems to be inherited by sex linked incomplete dominant genes. Individuals in the second group, termed enamel hypocalcification, have a normal matrix that is not fully calcified, resulting in easily abraded enamel (unlike enamel hypoplasia). Enamel hypocalcification is inherited in an autosomally dominant manner. The third group comprises of hypomaturation, in which the final stages of the mineralization process are abnormal. The hypomaturation forms differ from hypocalcification in that the enamel is harder, with a mottled opaque white to yellow-brown or red-brown color, and tends to chip from the underlying dentin rather than wear away.3–8
Fourteen subtypes of AI have been identified based on the pattern of inheritance, histological evaluation, radiographic and clinical appearance. Clinical presentation alone is not adequate to differentiate many subtypes. It has been established that a structurally abnormal gene mapped to loci on the short and long arms of the X chromosornc causes X-linked amelogenesis irnperfecta. Autosomal dominant amelogenesis imperfecta has been localized to chromosome 4q.2
According to Seow, the primary clinical problems of AI are esthetics, dental sensitivity, and loss of occlusal vertical dimension.3 The treatment plan for patients with AI is related to many factors including the age of the patient, the socioeconomic status of the patient, the type and severity of disorder, and the intraoral situation at the time the treatment plan is developed. This clinical report describes the treatment of an 18-year-female with amelogenesis imperfecta in which metal ceramic full veneer crowns in the anterior teeth and metal-ceramic crowns with metal occlusal surfaces in the posterior teeth were fabricated.3,9
Clinical report
An 18 year old female previously diagnosed with hypomaturation type AI presented for prosthodontic treatment. Her primary concerns included dissatisfaction with the size, shape, and shade of her teeth, poor masticatory efficiency and mild sensitivity of the teeth. The patient stated that her primary teeth were also discolored and did not report any parafunctional habits. A detailed medical, dental, and social history did not reveal any contraindications to dental therapy. The family history revealed that the patient's parents were not affected by AI, though her brother was affected. Dental treatment in the form of posterior restorative composite on the premolars and molars had been previously provided, aimed at “holding” the dentition stable until a more planned approach to reconstruction was possible. On examination, the patient's anterior and posterior teeth were discolored, stained, pitted and hypoplastic. The oral hygiene was fair with no loss of vertical dimension. The periodontal condition was satisfactory and no teeth were carious. The maxillary and mandibular teeth were well aligned with mild crowding of the mandibular anterior teeth. Overjet was recorded as 2 mm and overbite as 1 mm (Fig. 1a and b).
Fig. 1.

a and b: Teeth in open mouth and centric occlusion (vertical dimension is satisfactory).
The treatment plan was developed with the following aims: to improve esthetics, restore masticatory function and reduce reported sensitivity. Fabrication of metal-ceramic crowns with metal occlusal surfaces for all posterior teeth (considering the financial limitations of the patient) and full veneer metal ceramic crowns for all anterior teeth was planned.4 The patient was informed of the diagnosis and treatment plan and her consent recorded. Following dental prophylaxis and oral hygiene instructions, the patient was placed on a 0.12% chlorohexidine gluconate (Periogard Oral Rinse; Colgate Oral Pharmaceuticals, Canton, Mass. USA) oral rinse, twice daily. Diagnostic casts were made, followed by face-bow and centric, protrusive and lateral records. Casts were mounted in centric relation record on a semi-adjustable articulator. The patient had canine-protected occlusion. It was determined that the patient had 3–4 mm of interocclusal distance; therefore, the patient's existing vertical dimension was not altered.5
Maxillary and mandibular anterior teeth were prepared conventionally for full metal-ceramic restorations and the posterior teeth were prepared for partial veneer crowns in several appointments. Semi- solid food was prescribed till all the teeth had been reduced and temporaries provided. Laboratory-processed polymethyl methacrylate provisional restorations were fabricated at the existing occlusal vertical dimension by the indirect technique, from the pre-operative wax-up on the programmed semi-adjustable articulator and cemented with zinc-oxide non-eugenol cement (IRM, Dentsply International Inc. USA). Several adjustment appointments were made in order to fine tune the provisionals for esthetics and function. The procedure took about 4 weeks.
Irreversible hydrocolloid impressions with the cemented provisional restorations were obtained and poured in Type III dental stone. A custom incisal guide table was fabricated in acrylic resin (Pattern Resin LS; GC America) as per Dawson's description of the Pankey-Mann-Schuyler scheme from the existing anterior guidance. Definitive impressions of the prepared maxillary and mandibular anterior teeth were obtained using vinyl polysiloxane impression material (Aquasil, Dentsply Inc.). Working casts were generated in Type IV die stone and mounted onto the articulator using interocclusal records. Shade selection was done with the patient's consent in conformation with her complexion. The six maxillary anterior and mandibular full veneer ceramo-metal crowns were fabricated (Ceramco3, Dentsply, USA) in accordance with the customized incisal guide table taking guidance from the cast of the temporary restorations and addition silicone putty incisal indices of the refined provisionals. Definitive restorations were adjusted for optimal contacts, contours, esthetics, guidance & occlusion and luted.
After establishing the anterior guidance, all the posterior teeth were prepared. A Broderick Plane Analyser was not required as the existing vertical dimension, occlusal plane and scheme were utilized. Impressions were made with vinyl polysiloxane material (Aquasil, Dentsply International, USA) and poured in Type IV die stone (Kalabhai). Separable dies were prepared and the casts articulated by means of a centric relation record and a remount jig. A coping trial and occlusal adjustments prior to glazing enabled fine occlusal refinement. The patient's natural occlusal scheme (canine-protected occlusion) and anterior guidance were preserved in the definitive restorations. The individual crowns were cemented with glass ionomer cement (Ketac-Cem Maxicap; 3M ESPE, St. Paul, Minn.) (Fig. 2a–c).
Fig. 2.
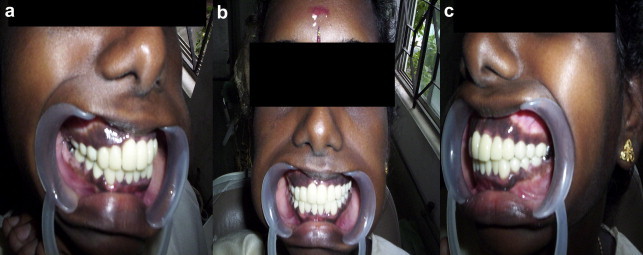
a, b, c. Post rehabilitation right lateral, frontal and left lateral views.
Discussion
Management of amelogenesis imperfecta in the young adult using fixed prosthodontics is not a novel approach. If such teeth are not rehabilitated, apart from poor aesthetics, tooth chipping & fracture, pain, compromised dental form & function and periodontal, occlusal & TMJ derangements are likely hazards. The fixed prosthodontic treatment selected in the present case, though invasive, was financially more viable. Laminates would have been the most conservative, esthetic and attractive option but high cost precluded their use. Also, precise laboratory support required for their fabrication is a limitation. Durability of laminates is often affected by chipping and open margins. For similar reasons, all porcelain crowns were not given. An advantage of full veneer porcelain fused to metal crowns is the strengthening effect they provide to weak hypoplastic teeth. As the patient had a wide smile exposing almost all teeth, metal crowns were not given on the posteriors, which would have been an even more economical option. We gave easily cleansable supra-gingival margins on the posterior teeth and sub gingival margins on the anteriors. A limitation of this approach was that the esthetics was below par at the finish lines because of the umbrella effect.6
Often, in the hypoplastic pattern of amelogenesis irnperfecta, the unaltered dentition looks remarkably like teeth already prepared for crowns. Radiographically, only a thin outline of enamel is seen covering the dentin and the enamel is one fourth to one eighth of the normal thickness.7 For this patient and subtype of amelogenesis imperfecta, alterations to normal margin design or cement choice were not necessary because of the limited change in the quality of the enamel.2 Alterations in technique depend specifically on the clinical condition of the tooth i.e. whether it is pitted, smooth, rough, hard, soft, or totally lacking enamel). Here, the enamel was hard and smooth. In the more severe pattern of hypoplastic amelogenesis imperfecta, the enamel may be of such poor quality, that margins are preferentially placed on cementum.3 The anterior metal ceramic crowns and posterior metal-ceramic crowns with metal occlusal surfaces were satisfactory both esthetically and functionally at the end of one year of clinical service. Compliance, regular recall appointments and scrupulous oral hygiene measures are paramount in full mouth rehabilitation cases, because of the large number of restorations in the mouth.
Conclusion
This clinical report described the oral rehabilitation of a young adult female patient affected by hypomaturation type of amelogenesis imperfecta. Although several treatment options were presented as part of the optimum treatment plan to achieve the best result, the patient declined these optionsdue to significant financial constraints. Metal-ceramic crowns with metal occlusal surfaces were placed on the posterior teeth and full metal ceramic crowns were placed on the maxillary and mandibular anterior teeth to improve the occlusion and esthetics.
Conflicts of interest
All authors have none to declare.
References
- 1.Weinmann J.P., Svoboda J.F., Woods R.W. Hereditary disturbances of enamel formation and calcification. J Am Dent Assoc. 1945;32:397–418. [Google Scholar]
- 2.Witkop C.J. Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: problems in classification. JOP. 1988;17:547–553. doi: 10.1111/j.1600-0714.1988.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 3.Seow W.K. Clinical diagnosis and management strategies of amelogenesis imperfecta variants. Pediatr Dent. 1993;15:384–393. [PubMed] [Google Scholar]
- 4.Mink J.R., Okeson J.P. Fixed prosthodontics for the young adolescent. In: Goldman H.M., editor. vol. VI. Mosby; St. Louis: 1977. pp. 493–503. (Current Therapy in Dentistry). [Google Scholar]
- 5.Coley-Smith A., Brown C.J. Case report: radical management of an adolescent with amelogenesis imperfecta. Dent Update. 1996;23:434–435. [PubMed] [Google Scholar]
- 6.Goodacre C.J., Guillermo B., Rungcharassaeng, Kan J.Y.K. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–132. doi: 10.1016/S0022-3913(03)00212-9. [DOI] [PubMed] [Google Scholar]
- 7.Winter G.B., Brook A.H. Enamel hypoplasia and anomalies of the enamel. Dent Clin North Am. 1975;19:3–24. [PubMed] [Google Scholar]
- 8.Haug R.H., Ferguson F.S. X-linked recessive hypomaturation amelogenesis imperfecta: report of case. J Am Dent Assoc. 1981;102:865–867. doi: 10.14219/jada.archive.1981.0203. [DOI] [PubMed] [Google Scholar]
- 9.Sengün A., Özer F. Restoring function and esthetics in a patient with amelogenesis imperfecta: a case report. Quintessence Int. 2002;33:199–204. [PubMed] [Google Scholar]


