Abstract
BACKGROUND:
Paediatric electrocardiograms (ECGs) are ordered and interpreted by general paediatricians; however, no previous studies have evaluated the accuracy of their ECG interpretations.
OBJECTIVE:
To determine general paediatricians’ practice and opinions regarding ECG use, accuracy of their interpretation of paediatric ECGs, and the relationship between accuracy and self-perceived confidence.
METHODS:
In the present cross-sectional study, Canadian general paediatricians were asked to complete a questionnaire and interpret 18 paediatric ECGs. The questionnaire assessed characteristics of ECG use, self-perceived confidence and opinions regarding ECG use in general paediatric practice. For the ECGs provided, respondents were asked whether the ECG was normal or abnormal, what abnormality the ECG demonstrated and how confident they were in this interpretation.
RESULTS:
ECG interpretation was performed by 124 general paediatricians. General paediatricians frequently use ECGs in their practice and regard this investigation as useful in patient assessment. The mean (± SD) accuracy of identifying ECGs as normal or abnormal, and identifying the specific abnormality was 80±12% and 56±20%, respectively. The sensitivity and specificity of identifying abnormal ECGs were 80% (95% CI 78% to 82%) and 79% (95% CI 75% to 83%), respectively. Correct ECG interpretation for isolated rhythm disturbances (73%) was significantly better than for abnormalities in axis (25%), chamber hypertrophy (41%) and ECG intervals (49%) (P<0.001). Overall confidence in ECG interpretation correlated with and was the only significant predictor of interpretation accuracy (r=0.396, P<0.001).
CONCLUSION:
General paediatricians were adept at detecting abnormal ECGs, but were less able to identify the abnormalities. Further education in ECG interpretation may be important for this population.
Keywords: Clinical competence, Electrocardiography, Medical education, Paediatrics, Physicians’ practice patterns, Questionnaires
Abstract
HISTORIQUE :
Ce sont des pédiatres généralistes qui demandent et interprètent les électrocardiogrammes (ECG) en pédiatrie, mais aucune étude n’a porté sur l’exactitude de leur interprétation.
OBJECTIF :
Déterminer la pratique et les avis des pédiatres généralistes en matière d’utilisation des ECG et de l’exactitude des ECG en pédiatrie et établir le lien entre la précision et l’autoperception de la confiance.
MÉTHODOLOGIE :
Dans la présente étude transversale, les pédiatres généralistes canadiens ont été invités à remplir un questionnaire et à interpréter 18 ECG en pédiatrie. Le questionnaire visait à évaluer les caractéristiques liées à l’utilisation des ECG, l’autoperception de la confiance et les avis relatifs à l’utilisation des ECG en pédiatrie générale. Les répondants étaient invités à préciser si les ECG four-nis étaient normaux ou anormaux, les anomalies démontrées et leur confiance quant à leur interprétation.
RÉSULTATS :
Cent vingt-quatre pédiatres généralistes ont interprété les ECG. Les pédiatres généralistes utilisent souvent les ECG dans leur pratique et les considèrent comme utiles dans l’évaluation des patients. L’exactitude moyenne dans l’identification des ECG comme normaux ou anormaux et dans la détermination de l’anomalie précise correspondait à 80±12 % et à 56±20 %, respectivement. La sensibilité et la spécificité de l’identification des ECG anormaux s’établissaient à 80 % (95 % IC 78 % à 82 %) et à 79 % (95 % IC 75 % à 83 %), respectivement. La bonne interprétation des ECG révélant des troubles isolés du rythme cardiaque (73 %) était considérablement plus élevée que celle des anomalies de l’axe (25 %), de l’hypertrophie ventriculaire (41 %) et des intervalles d’ECG (49 %) (P<0,001). Dans l’ensemble, la confiance à l’égard de l’interprétation des ECG était corrélée avec l’exactitude des interprétations et en était le seul prédicteur important (r=0,396, P<0,001).
CONCLUSION :
Les pédiatres généralistes décelaient bien les ECG anormaux, mais réussissaient moins bien à déterminer les anomalies exactes. Il serait peut-être important de leur fournir un perfectionnement dans l’interprétation des ECG.
Electrocardiograms (ECGs) are an essential tool for assessing children with potential cardiovascular pathology. ECGs can suggest cardiac pathology and may be useful in the assessment of structural heart disease (1). ECGs are also important in the diagnosis of conditions predisposing children to sudden death (including arrhythmias, long QT syndrome [LQTS] and hypertrophic cardiomyopathy) and there is a growing demand for ECG screening to exclude such conditions in young athletes. While the paediatric ECG is critical for diagnosis, management and appropriate referral to paediatric cardiologists for a range of conditions, accurate interpretation is challenging and important abnormalities are often missed (2–8).
General paediatricians are often the first physicians to assess children with possible cardiac pathology. Because paediatricians order and read paediatric ECGs, it is essential that they interpret these investigations correctly. Deficiencies in ECG interpretation occur in several medical specialties (2–11). Paediatric studies have revealed deficits in ECG interpretation by paediatric residents and paediatric emergency room (PER) physicians, with accuracy rates of up to 64% to 68% and 61% to 87%, respectively (2–7). Accuracy among PER physicians decreases to 30% to 73% for the most serious ECG diagnoses including arrhythmias and LQTS (6,7). Little information regarding the accuracy of ECG interpretation by general paediatricians is available. The present study investigated general paediatricians’ practice and opinions on ECG use, as well as accuracy in paediatric ECG interpretation and its relationship with self-perceived confidence. In the present study, we use the term ‘accuracy’ to indicate the proportion of responses that were deemed to be correct.
METHODS
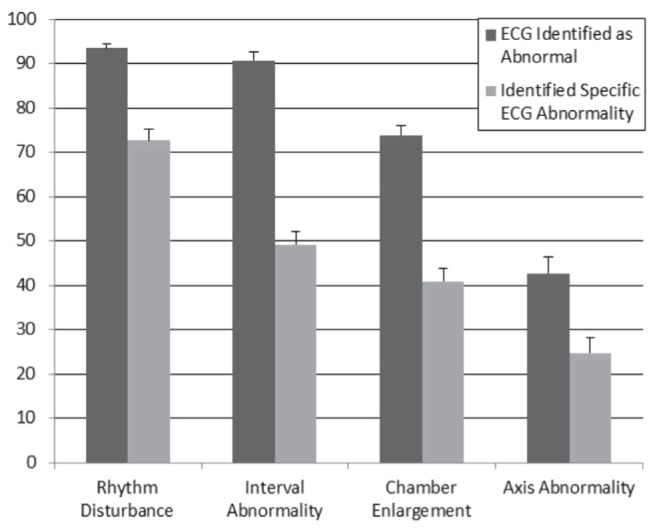
The present study aimed to include all general paediatricians practicing in Canada. The provincial Colleges of Physicians and Surgeons directories were searched to identify general paediatricians using the headings “pediatrics” or “pediatrician”. All provinces were included except Saskatchewan and Quebec because these provincial associations either did not provide online access to a physician directory or did not allow for searches according to specialty. Inclusion criteria consisted of being certified as a general paediatrician by the Royal College of Physicians and Surgeons of Canada, practicing as a general paediatrician for >50% of clinical duties and being in clinical practice within the past 12 months. Subjects were excluded if contact information was incomplete, the office address was non-Canadian or the directory identified the physician as a paediatric subspecialist. The remaining physician names were cross-linked with online physician directories provided by Canadian tertiary care paediatric hospitals to further exclude paediatric subspecialists. A total of 1230 paediatricians were identified.
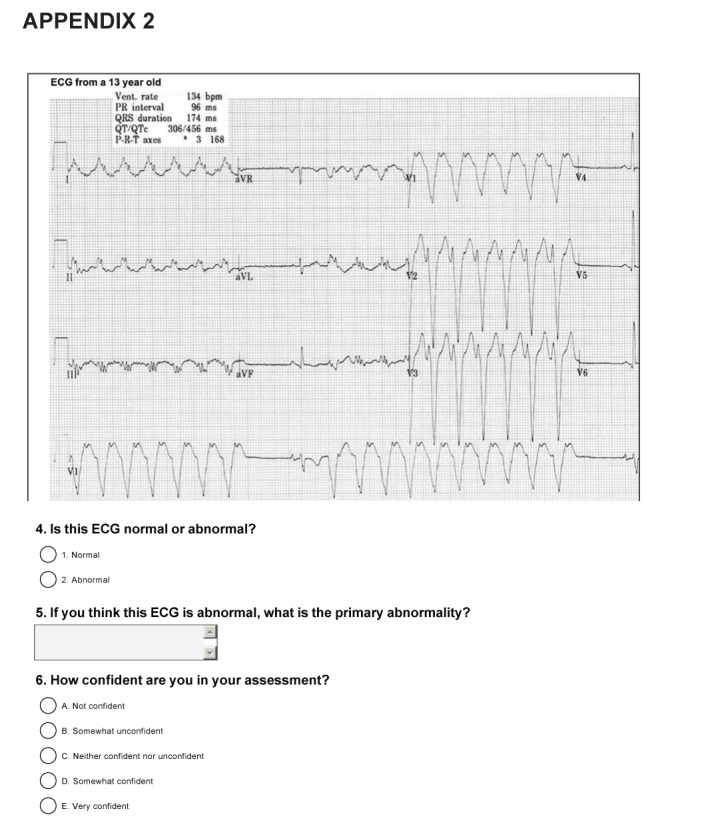
The authors developed a two-part online questionnaire (Appendixes 1 and 2). The first section of the survey assessed practice demographics, frequency of ECG use and indications for ordering an ECG. Five-point Likert scales were used to assess perceived importance of ECG interpretation skills, perceived utility of ECG use in general paediatric practice, overall self-confidence in ECG interpretation and confidence in the different aspects of ECG interpretation including rate, rhythm, axis, ECG intervals, repolarization and chamber hypertrophy.
The second part of the questionnaire included three normal and 15 pathological ECGs. Participants were asked to identify whether the ECG was normal or abnormal, to identify the specific abnormality and to rate their level of confidence in their interpretation. The abnormal ECG findings tested (Box 1) were adapted from the study by Snyder et al (5) because these abnormalities were determined by a panel of residency directors to represent the minimum proficiency that should be obtained by all general paediatric residents. One of the normal ECGs demonstrated sinus arrhythmia. ECGs were selected from the clinical practice of the study authors and were chosen to show an isolated abnormality. The ECGs were de-identified but included the patients’ age and the computer-determined readings of ventricular rate, PR interval, QRS duration, QT/corrected QT, and the P, QRS and T wave axes. To validate the ECG test, four paediatric cardiologists (including two electrophysiologists) independently interpreted the ECGs. ECGs were included if at least three of the four cardiologists agreed that the ECG demonstrated the intended abnormality. The overall agreement was 91.7%, with a kappa value of 0.83 (12). Disagreement occurred for ECGs demonstrating sinus tachycardia and right axis deviation being identified as normal, and for right ventricular hypertrophy not being identified.
Box 1: Pathological electrocardiogram diagnoses used in the questionnaire.
Sinus bradycardia
Sinus tachycardia
Right axis deviation
Left axis deviation
First degree atrioventricular block
Ventricular tachycardia
Left ventricular hypertrophy
Right ventricular hypertrophy
Biventricular hypertrophy
Supraventricular tachycardia
Long corrected QT
Right atrial enlargement
Left atrial enlargement
Pre-excitation
Complete atrioventricular block
Study participants received personalized letters outlining the inclusion criteria and providing a link to the online questionnaire. Subjects were asked to return a postage-paid card if they were ineligible for the study. Nonresponders received up to four letters sent at one-month intervals. The questionnaire was available for a total of five months and could only be completed once. Incentives to complete the study included the provision of answers to the ECG test and entry into a draw. Questionnaire answers were numerically coded for anonymity and confidentiality. The questionnaire answers were independently scored as correct or incorrect by two of the study authors (CE, CT), with a third (KW) consulted in cases of disagreement.
Data were analyzed using SPSS version 17.0 (IBM Corporation, USA). Descriptive variables were reported as relative percentages. The overall accuracy of identifying abnormal ECGs was examined, as well as the accuracy of identifying the specific pathology present. Analysis of overall accuracy was limited to respondents who interpreted >75% of the provided ECGs (n=109). Sensitivity and specificity for the identification of abnormal ECGs were calculated. Means were compared using t tests, χ2 tests and ANOVAs. Pearson’s correlations were used to assess the relationship between continuous variables and accuracy. Multivariate linear regression was performed to identify the characteristics of general paediatricians that were associated with increased ECG interpretation accuracy. Pathological ECG abnormalities were categorized into four groups: rhythm disturbances, axis abnormalities, abnormalities in ECG intervals and chamber enlargement/hypertrophy. Repeated-measures ANOVA with a Greenhouse-Geisser correction was used to determine whether differences in accuracy of ECG interpretation were present between the different ECG categories, and the calculated F statistics are reported; P<0.05 was considered to be statistically significant. Ethics approval was granted by the Human Investigations Committee of Memorial University of Newfoundland (St John’s, Newfoundland and Labrador).
RESULTS
Of the 1230 subjects approached, 278 paediatricians had an invalid address or responded that they did not meet inclusion criteria. Of the remaining 952 paediatricians, 134 (14%) completed the first section of the questionnaire and 124 (13%) completed the ECG testing. The demographic profile of respondents is presented in Table 1. At least five ECGs per month were ordered by 40% of paediatricians and 65% had all their ECGs reviewed by a paediatric cardiologist. The most common indications for ordering ECGs were investigation of murmurs (46%), syncope (19%) and palpitations (12%). ECG machines provided a computer interpretation for 87% of respondents, with 60% not relying on this interpretation and 18% relying on it at least 25% of the time. The ability to reliably interpret paediatric ECGs was viewed as somewhat to very important by 88% of respondents. ECGs were viewed by 79% of paediatricians as somewhat or very useful for evaluating potential cardiovascular conditions in children.
TABLE 1.
Respondent demographics and association with electrocardiogram (ECG) interpretation accuracy*
| Characteristic | n (%) | Per cent correct identification of ECG as normal or abnormal† | P | Per cent correct identification of ECG pathology† | P |
|---|---|---|---|---|---|
| Population of practice location | |||||
| <100,000 | 42 (31) | 84±13 | 0.018 | 65±19 | 0.002 |
| >100,000 | 92 (69) | 78±12 | 52±19 | ||
| Years in practice | |||||
| 1–5 | 44 (33) | 78±13 | 0.386 | 56±22 | 0.843 |
| 6–10 | 13 (10) | 81±15 | 54±24 | ||
| 11–15 | 29 (21) | 80±13 | 58±18 | ||
| 16–20 | 15 (11) | 80±12 | 58±16 | ||
| >20 | 33 (25) | 81±11 | 54±20 | ||
| Primary practice type | |||||
| Primary care | 29 (22) | 74±13 | 0.123 | 49±21 | 0.224 |
| Consulting paediatrics | 82 (61) | 81±13 | 59±20 | ||
| Paediatric inpatient medicine | 16 (12) | 81±11 | 60±23 | ||
| Neonatal inpatient medicine | 5 (4) | 77±9 | 54±10 | ||
| Other | 1 (1) | ‡ | ‡ | ‡ | ‡ |
| Holding an academic position | |||||
| Yes | 81 (61) | 81±13 | 0.248 | 56±21 | 0.808 |
| No | 51 (39) | 78±12 | 56±19 | ||
| Local paediatric cardiology referral centre | |||||
| Yes | 85 (63) | 77±12 | 0.016 | 53±19 | 0.056 |
| No | 49 (37) | 83±12 | 61±22 | ||
| All ECGs reviewed by cardiology | |||||
| Yes | 86 (65) | 78±12 | 0.179 | 53±20 | 0.048 |
| No | 47 (35) | 82±13 | 61±21 | ||
| Frequency of consulting cardiology for ECG interpretation | |||||
| <25% of the time | 86 (64) | 80±13 | 0.390 | 59±20 | 0.014 |
| >25% of the time | 48 (36) | 78±12 | 48±18 | ||
| ECGs ordered per month | |||||
| 0–5 | 80 (60) | 79±13 | 0.453 | 56±19 | 0.837 |
| 5–10 | 43 (32) | 81±13 | 56±23 | ||
| 10–15 | 8 (6) | 80±14 | 53±21 | ||
| 15–20 | 3 (2) | 83±6 | 63±9 | ||
| Overall confidence in ECG interpretation | |||||
| Not confident | 15 (11) | 75±9 | 0.007 | 38±17 | <0.001 |
| Somewhat unconfident | 20 (15) | 74±12 | 47±20 | ||
| Neutral | 25 (19) | 80±12 | 60±17 | ||
| Somewhat confident | 59 (44) | 80±13 | 58±20 | ||
| Confident | 14 (11) | 91±8 | 72±13 | ||
Data presented as mean ± SD unless otherwise indicated.
n and % reflect the total respondents; analysis of accuracy of ECG interpretation was limited to subjects who interpreted >75% of provided ECGs (n=109);
Analysis performed using Pearson’s correlation, t test or ANOVA;
Analysis excluded one subject in ‘other’ group
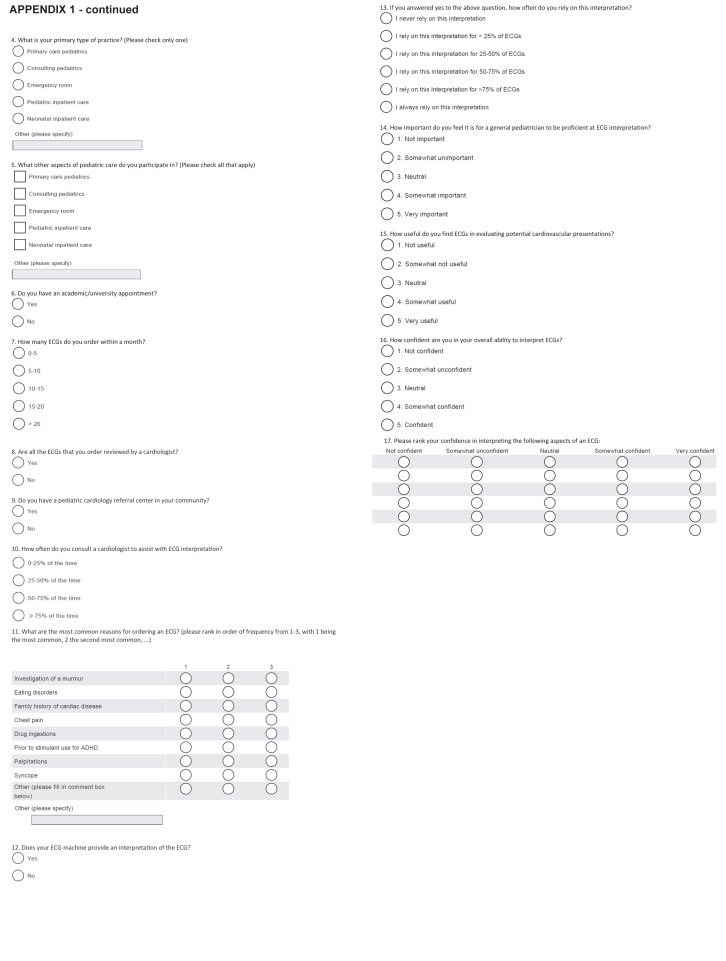
The mean (± SD) accuracy of identifying ECGs as normal or abnormal by general paediatricians was 80±12%. The sensitivity and specificity of identifying abnormal ECGs was 80% (95% CI 78% to 82%) and 79% (95% CI 75% to 83%), respectively. The frequency at which individual pathological ECGs were identified correctly as abnormal is summarized in Table 2. The mean accuracy in identifying pathological ECGs as abnormal was significantly different between the categories of ECG abnormalities (F=108.4 [1.9, 200.9]; P<0.001). As illustrated in Figure 1, ECGs were identified as abnormal more often for isolated rhythm disturbances (94±11%) or abnormal intervals (91±18%) compared with isolated chamber enlargement (74±24%; P<0.001). ECGs with isolated axis abnormalities were identified as abnormal less often (43±40%) than ECGs with abnormalities in rhythm, chamber size or ECG intervals (P<0.001).
TABLE 2.
Rate of correct electrocardiogram (ECG) identification according to abnormality
| ECG pathology | Identified as abnormal | Identified specific abnormality |
|---|---|---|
| Rhythm disturbance | ||
| Sinus bradycardia* | 95 | 82 |
| Sinus tachycardia† | 77 | 58 |
| Complete heart block | 98 | 67 |
| Ventricular tachycardia | 100 | 81 |
| Supraventricular tachycardia | 96 | 76 |
| Abnormal ECG intervals | ||
| Pre-excitation | 98 | 25 |
| Long QT syndrome | 85 | 63 |
| First-degree atrioventricular block | 90 | 58 |
| Chamber hypertrophy or enlargement | ||
| Right atrial enlargement | 76 | 48 |
| Left atrial enlargement | 61 | 39 |
| Right ventricular hypertrophy | 75 | 43 |
| Left ventricular hypertrophy | 64 | 33 |
| Biventricular hypertrophy | 93 | 37 |
| Abnormal axis | ||
| Left axis deviation | 48 | 21 |
| Right axis deviation | 39 | 28 |
Data presented as %.
ECG provided was from an eight-year-old with a heart rate of 44 beats/min;
ECG provided was from a 10-month-old with a heart rate of 194 beats/min
Figure 1).
Mean values for the per cent correct identification of pathological electrocardiograms (ECGs) by general paediatricians for ECG pathological categories. The error bars represent SEM.
The data were further analyzed to determine the ability of general paediatricians to correctly identify the specific abnormality demonstrated in each ECG (Table 2). The mean accuracy of identifying the specific ECG abnormality was 56±20%. A significant difference in the rate of identifying the ECG abnormality was found between ECG categories (F=68.4 [2.8, 297.2]; P<0.001). As demonstrated in Figure 1, the correct identification of isolated rhythm disturbances (73±26%) was significantly better than for all other ECG categories (P<0.001). Identification of isolated axis abnormalities (25±36%) was the least correctly interpreted (P<0.001) and there was no difference between chamber hypertrophy (41±29%) and ECG intervals (49±31%) (P=0.094).
The most commonly misinterpreted abnormalities were left axis deviation, right axis deviation and pre-excitation. Sinus arrhythmia was interpreted as abnormal in 32% of subjects. Supraventricular tachycardia (SVT) was interpreted as sinus tachycardia in 6% of cases and sinus tachycardia was misinterpreted as SVT in 11% of cases.
Only 55% of respondents were somewhat to very confident in their overall ECG interpretation skills. Respondents were somewhat to very confident in interpreting rate (98%), rhythm (90%), axis (67%), ECG intervals (65%), ST changes (32%) and chamber hypertrophy (44%) at varying frequencies. There was a weak positive correlation between overall confidence in ECG interpretation and accuracy in interpreting pathological ECGs as abnormal (r=0.283; P=0.003) and in correct identification of ECG abnormalities (r=0.396; P<0.001). Respondents who were confident in their interpretation were more likely to correctly interpret the specific ECG abnormality for all ECG diagnoses apart from pre-excitation, left atrial enlargement, sinus bradycardia and right axis deviation (χ2<3.4; P>0.06).
Table 1 presents the association between practice characteristics and ECG interpretation accuracy. Multivariate linear regression was performed using the factors outlined in Table 3 because these were significantly associated with accuracy in paediatric ECG interpretation (Table 1). Table 3 provides the results of the regression analysis. When controlling for other factors, the only significant predictor of correctly interpreting pathological ECGs as abnormal and of correctly identifying the specific ECG abnormality was overall confidence in ECG interpretation.
TABLE 3.
Association between per cent electrocardiogram (ECG) interpretation accuracy and other variables: Results from multiple linear regression
| Predictor variable |
Dependent variables
|
|||
|---|---|---|---|---|
|
Per cent correct identification of ECG as normal or abnormal*
|
Per cent correct identification of ECG pathology†
|
|||
| β‡ | P | β‡ | P | |
| All ECGs reviewed by cardiology | −1.5 | 0.568 | −3.0 | 0.456 |
| Local paediatric cardiology referral center | −4.0 | 0.148 | −2.1 | 0.622 |
| Consulting cardiology for ECG interpretation >25% of the time | 1.4 | 0.633 | −3.7 | 0.410 |
| Population of practice location >100,000 | −2.6 | 0.404 | −7.3 | 0.125 |
| Overall confidence in ECG interpretation | 2.7 | 0.012 | 5.7 | 0.001 |
Adjusted R2=0.085, F(5, 102)=2.990; P=0.015.
Adjusted R2=0.176, F(5, 102)=5.581; P<0.001;
estimates the increase in the dependent variable (% correct interpretation of ECGs) per unit increase in the predictor variables or in the yes versus no group for binary predictors
DISCUSSION
The majority of general paediatricians surveyed believe ECGs are useful in general paediatric practice and that ECG interpretation skills are important for general paediatricians. However, one in five abnormal ECGs were missed and one-half of the ECGs were misdiagnosed. These misdiagnoses may lead to inappropriate patient management and failure to identify patients at risk for sudden death.
Cardiac etiologies are some of the most common causes of cardiac arrest in children and young adults (13). Undiagnosed cardiovascular diseases, including hypertrophic cardiomyopathy, LQTS and coronary anomalies, may lead to sudden death in children and adolescents (14). ECGs are essential in evaluating children for propensity for sudden death, with several studies suggesting that ECGs are instrumental in screening for cardiac pathology (15–18). However, accurate interpretation of paediatric ECGs is difficult, especially for screening the general population (8,19). Increasing media attention to the occurrence and prevention of sudden death in children and young athletes will likely place increasing pressure on general paediatricians to perform and interpret screening ECGs. In addition, many cardiovascular conditions can only be identified using electrocardiography including pre-excitation, LQTS, arrhythmias and Brugada syndrome. Congenital heart disease may also be suggested by abnormalities in axis or chamber enlargement on an ECG. Therefore, it is important for paediatricians to be adept at ECG interpretation.
General paediatricians are frequently the initial physicians interpreting ECGs in children. Their ability to identify the ECG as abnormal to initiate a cardiology consultation remains vital. It is concerning that conditions with potential morbidity and mortality, including concerning arrhythmias, LQTS and ventricular hypertrophy, were misdiagnosed in 18% to 33%, 37% and 57% to 67% of cases, respectively. Paediatricians failed to identify pre-excitation in 75% of cases, which is worrying because this can predispose patients to both SVT and sudden death. More than one-third of the paediatricians surveyed do not have their ECGs routinely reviewed by a paediatric cardiologist, posing a potential for missing significant diagnoses. It is also problematic that 32% identified sinus arrhythmia as abnormal, which may result in unnecessary concern for families and inappropriate resource utilization. While routine review of ECGs by paediatric cardiology may help reduce potential missed diagnoses, it does not eliminate the need for paediatricians to identify ECG abnormalities in potentially urgent situations, such as in the setting of arrhythmias.
Several medical specialties have shown deficiencies in ECG interpretation including family, internal and emergency medicine (9,10,20–23). To our knowledge, the present study was the first to assess ECG interpretation by general paediatricians. The ECG interpretation accuracy of PER physicians ranges from 61% to 87% (3,4,6,7). Our results may not be directly comparable because these studies were performed in situ rather than as a structured questionnaire and a large proportion of the ECGs interpreted in these studies were considered to be normal. Studies of paediatric residents’ ECG interpretation using a structured questionnaire report accuracy rates ranging from 41% for junior residents to 68% for senior residents, which are comparable with our results (2,5).
Only 55% of general paediatricians were confident in their ECG interpretation skills, which is similar to results reported by Wong et al (24), who found that 49% of paediatricians in Atlantic Canada were confident in ECG interpretation. Our study demonstrated that confidence in ECG interpretation was associated with increased ECG interpretation accuracy. To our knowledge, the present study was one of the first to assess confidence in ECG interpretation and its relation to accuracy.
Our study suggests that further education in ECG interpretation may be beneficial for general paediatricians. The areas of greatest weakness in our study were axis abnormalities, chamber enlargement and abnormal ECG intervals. Although improved accuracy in all of these areas would be important, it may be most important that further education focuses on arrhythmia and abnormal interval identification because these abnormalities are associated with the greatest potential morbidity. Multiple different educational methods, including lectures, workshops, computer-assisted learning, puzzle-based learning and small group sessions, have been effective in teaching ECG interpretation in undergraduate medical education (25–29). It is unclear how education regarding ECG interpretation would be best provided to practicing physicians because research in this area is lacking.
There are limitations to our study that warrant further discussion. Although eligible participants were contacted four times, the response rate remained low. Physician response rates to mail surveys vary widely from 17% to 84% (30). Factors that may have limited our response rate were questionnaire length, requirement of respondents to access an online questionnaire and the time demands of general paediatricians. Selection bias may have occurred if the participating paediatricians were more confident or skilled in ECG interpretation, potentially making our results an inaccurate reflection of the broader population of Canadian general paediatricians. The ECGs we provided did not contain a clinical vignette, and the provision of a case scenario has been shown to change the accuracy of the ECG interpretation (31). Our study specifically examined the ECG interpretation skills of Canadian general paediatricians and may not be generalizable outside of the Canadian context. Finally, we were unable to contact all paediatricians in Canada using our methodology.
CONCLUSION
General paediatricians frequently use ECGs and regard them as useful in clinical practice. Our study suggests that the majority of general paediatricians are able to adequately identify when an ECG is abnormal. However, the accuracy of identifying the specific ECG abnormality is lower than expected. Further education for this group of physicians may be important, with particular emphasis on those diagnoses with potential for significant morbidity and mortality, along with abnormalities in axis, ECG intervals and chamber enlargement.
Appendix 1: ECG Survey
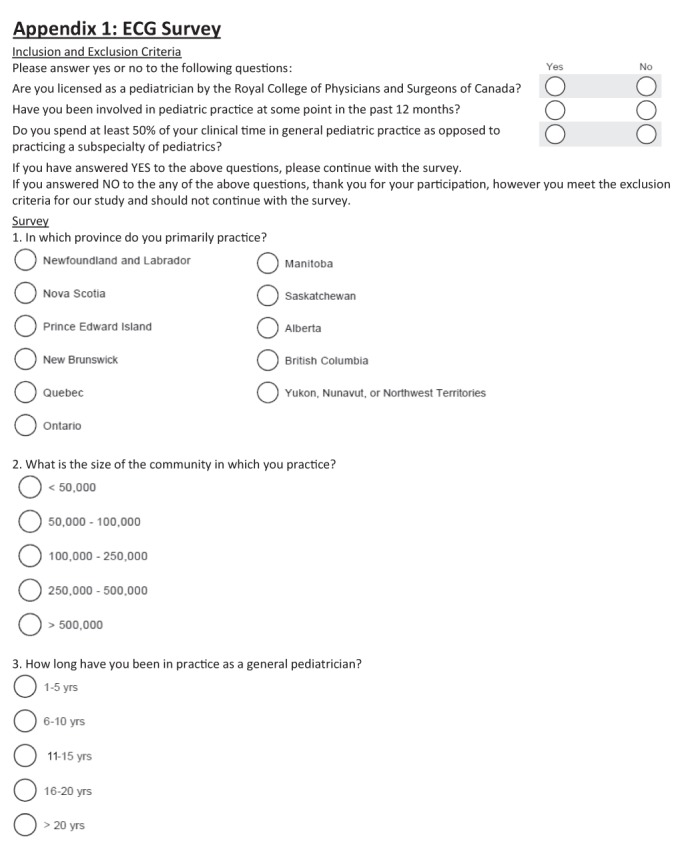
APPENDIX 2
Footnotes
DISCLOSURES: Financial support provided by the Janeway Foundation Research Fund and the Health Care Foundation (St John’s, Newfoundland). These funding agencies did not contribute to study design; data collection, analysis, or interpretation; manuscript writing; or the decision to submit the manuscript for publication. The authors have no conflicts of interest to declare. The first draft was written by Dr Carolina Escudero. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
REFERENCES
- 1.Bush DM. Evaluating cardiovascular presentations: What does an electrocardiogram have to offer? Pediatr Ann. 2005;34:858–69. doi: 10.3928/0090-4481-20051101-09. [DOI] [PubMed] [Google Scholar]
- 2.Crocetti M, Thompson R. Electrocardiogram interpretation skills in pediatric residents. Ann Pediatr Cardiol. 2010;3:3–7. doi: 10.4103/0974-2069.64356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giuffre RM, Nutting A, Cohen J, Crawford S, Johnson DW. Electrocardiogram interpretation and management in a pediatric emergency department. Pediatr Emerg Care. 2005;21:143–8. [PubMed] [Google Scholar]
- 4.Horton LA, Mosee S, Brenner J. Use of the electrocardiogram in a pediatric emergency department. Arch Pediatr Adolesc Med. 1994;148:184–8. doi: 10.1001/archpedi.1994.02170020070012. [DOI] [PubMed] [Google Scholar]
- 5.Snyder CS, Bricker JT, Fenrich AL, et al. Can pediatric residents interpret electrocardiograms? Pediatr Cardiol. 2005;26:396–9. doi: 10.1007/s00246-004-0759-5. [DOI] [PubMed] [Google Scholar]
- 6.Snyder CS, Fenrich AL, Friedman RA, Macias C, O’Reilly K, Kertesz NJ. The emergency department versus the computer: Which is the better electrocardiographer? Pediatr Cardiol. 2003;24:364–8. doi: 10.1007/s00246-002-0332-z. [DOI] [PubMed] [Google Scholar]
- 7.Wathen JE, Rewers AB, Yetman AT, Schaffer MS. Accuracy of ECG interpretation in the pediatric emergency department. Ann Emerg Med. 2005;46:507–11. doi: 10.1016/j.annemergmed.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Hill AC, Miyake CY, Grady S, Dubin AM. Accuracy of interpretation of preparticipation screening electrocardiograms. J Pediatr. 2011;159:783–8. doi: 10.1016/j.jpeds.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 9.Berger JS, Eisen L, Nozad V, et al. Competency in electrocardiogram interpretation among internal medicine and emergency medicine residents. Am J Med. 2005;118:873–80. doi: 10.1016/j.amjmed.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Boltri JM, Hash RB, Vogel RL. Are family practice residents able to interpret electrocardiograms? Adv Health Sci Educ Theory Pract. 2003;8:149–53. doi: 10.1023/a:1024943613613. [DOI] [PubMed] [Google Scholar]
- 11.Viskin S, Rosovski U, Sands AJ, et al. Inaccurate electrocardiographic interpretation of long QT: The majority of physicians cannot recognize a long QT when they see one. Heart Rhythm. 2005;2:569–74. doi: 10.1016/j.hrthm.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Randolph JJ. Online kappa calculator. < http://justus.randolph.name/kappa> (Accessed July 31, 2013).
- 13.Richman PB, Nashed AH. The etiology of cardiac arrest in children and young adults: Special considerations for ED management. Am J Emerg Med. 1999;17:264–70. doi: 10.1016/s0735-6757(99)90122-5. [DOI] [PubMed] [Google Scholar]
- 14.Mahle WT, Sable CA, Matherne PG, Gaynor JW, Gewitz MH. Key concepts in the evaluation of screening approaches for heart disease in children and adolescents: A science advisory from the American Heart Association. Circulation. 2012;125:2796–801. doi: 10.1161/CIR.0b013e3182579f25. [DOI] [PubMed] [Google Scholar]
- 15.Baggish AL, Hutter AM, Jr, Wang F, et al. Cardiovascular screening in college athletes with and without electrocardiography: A cross-sectional study. Ann Intern Med. 2010;152:269–75. doi: 10.7326/0003-4819-152-5-201003020-00004. [DOI] [PubMed] [Google Scholar]
- 16.Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296:1593–601. doi: 10.1001/jama.296.13.1593. [DOI] [PubMed] [Google Scholar]
- 17.Corrado D, Basso C, Schiavon M, Thiene G. Screening for hypertrophic cardiomyopathy in young athletes. N Eng J Med. 1998;339:364–9. doi: 10.1056/NEJM199808063390602. [DOI] [PubMed] [Google Scholar]
- 18.Wilson MG, Basavarajaiah S, Whyte GP, Cox S, Loosemore M, Sharma S. Efficacy of personal symptom and family history questionnaires when screening for inherited cardiac pathologies: the role of electrocardiography. Br J Sports Med. 2008;42:207–11. doi: 10.1136/bjsm.2007.039420. [DOI] [PubMed] [Google Scholar]
- 19.Dipchand AI, McCrindle BW, Gow RM, Freedom RM, Hamilton RM. Accuracy of surface electrocardiograms for differentiating children with hypertrophic cardiomyopathy from normal children. Am J Cardiol. 1999;83:628–30. A10. doi: 10.1016/s0002-9149(98)00933-3. [DOI] [PubMed] [Google Scholar]
- 20.de Jager J, Wallis L, Maritz D. ECG interpretation skills of South African emergency medicine residents. Int J Emerg Med. 2010;3:309–14. doi: 10.1007/s12245-010-0227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoyle RJ, Walker KJ, Thomson G, Bailey M. Accuracy of electrocardiogram interpretation improves with emergency medicine training. Emerg Med Australas. 2007;19:143–50. doi: 10.1111/j.1742-6723.2007.00946.x. [DOI] [PubMed] [Google Scholar]
- 22.Salerno SM, Alguire PC, Waxman HS. Competency in interpretation of 12-lead electrocardiograms: A summary and appraisal of published evidence. Ann Intern Med. 2003;138:751–60. doi: 10.7326/0003-4819-138-9-200305060-00013. [DOI] [PubMed] [Google Scholar]
- 23.Todd KH, Hoffman JR, Morgan MT. Effect of cardiologist ECG review on emergency department practice. Ann Emerg Med. 1996;27:16–21. doi: 10.1016/s0196-0644(96)70290-1. [DOI] [PubMed] [Google Scholar]
- 24.Wong KK, Barker AP, Warren AE. Paediatricians’ validation of learning objectives in paediatric cardiology. Paediatr Child Health. 2005;10:95–9. doi: 10.1093/pch/10.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hatala RM, Brooks LR, Norman GR. Practice makes perfect: The critical role of mixed practice in the acquisition of ECG interpretation skills. Adv Health Sci Educ Theory Pract. 2003;8:17–26. doi: 10.1023/a:1022687404380. [DOI] [PubMed] [Google Scholar]
- 26.Mahler SA, Wolcott CJ, Swoboda TK, Wang H, Arnold TC. Techniques for teaching electrocardiogram interpretation: Self-directed learning is less effective than a workshop or lecture. Med Educ. 2011;45:347–53. doi: 10.1111/j.1365-2923.2010.03891.x. [DOI] [PubMed] [Google Scholar]
- 27.Nilsson M, Bolinder G, Held C, Johansson BL, Fors U, Ostergren J. Evaluation of a web-based ECG-interpretation programme for undergraduate medical students. BMC Med Educ. 2008;8:25. doi: 10.1186/1472-6920-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raupach T, Hanneforth N, Anders S, Pukrop T, Th J ten Cate O, Harendza S. Impact of teaching and assessment format on electrocardiogram interpretation skills. Med Educ. 2010;44:731–40. doi: 10.1111/j.1365-2923.2010.03687.x. [DOI] [PubMed] [Google Scholar]
- 29.Rubinstein J, Dhoble A, Ferenchick G. Puzzle based teaching versus traditional instruction in electrocardiogram interpretation for medical students – a pilot study. BMC Med Educ. 2009;9:4. doi: 10.1186/1472-6920-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20:61–7. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 31.Hatala R, Norman GR, Brooks LR. Impact of a clinical scenario on accuracy of electrocardiogram interpretation. J Gen Intern med. 1999;14:126–9. doi: 10.1046/j.1525-1497.1999.00298.x. [DOI] [PubMed] [Google Scholar]