Abstract
Objective
There are many causes of cervical myelopathy including trauma, degenerative conditions, tumors and demyelinating disorders. However, myelopathy caused by soft disc herniation might be seen rarely than the spondylosis caused by hard disc. Here, authors retrospectively analyzed the clinical features and results of cervical myelopathy caused by soft disc herniation.
Methods
From March 2010 to December 2010, 134 patients with degenerative cervical spinal disease were treated with anterior cervical discectomy and interbody fusion. Among them, 21 patients with cervical myelopathy secondary to cervical soft disc herniation were analyzed. Their clinical features, preoperative and, postoperative clinical results were evaluated by Nurick Grade and Japanese Orthopaedic Association scale (JOA) retrospectively. Preoperative clinical features including duration of myelopathy, pain intensity and postoperative clinical results including improvement rate of myelopathy and radiculopathy were retrospectively analyzed by Nurick Grade and JOA scale. We also evaluated correlation between the duration of symptom, type of the disc herniation, pain intensity and clinical outcome.
Results
Mean age was 49.7 and male was predominant. Gait disturbance with mild to moderate pain was most common symptom in clinical features. Severe pain was shown in only 9 cases, and the other 12 cases experienced mild to moderate pain. Mean duration of myelopathy was 1.18 month. The mean JOA scores were 11.22 before surgery and 14.2 after surgery. The mean Nurick grades were 2.78 before treatment and 1.67 after treatment. Neurologic status of mild or moderate pain group on preoperative state is worse than that of severe pain group. The patients with duration of myelopathy symptom (<1 month) showed lower clinical improvement rate than the patients with myelopathy over 1 month. Patients with median type of disc herniation showed poorer neurological status than those with paramedian type of herniation in preoperative state.
Conclusion
Authors reviewed the clinical features and surgical outcome of the cervical myelopathy secondary to cervical soft disc herniation. We presumed that patients of more than one month of symptom duration, mild to moderate initial symptom would be related with better postoperative improvement rate.
Keywords: Myelopathy, Cervical herniated disc, soft disc, Surgical outcome
INTRODUCTION
Cervical myelopathy has various causes such as ossification of posterior longitudinal ligament, cervical spondylosis, and cervical disc herniation. However, most of these were more frequently found in elderly patients with spondylotic myelopathy and advanced degenerative changes in disc, facet and Luschka's joints and thickened ligamentum flavum2,24). However, soft cervical disc herniation which leads to myelopathy is less frequently seen than cervical spondylotic myelopathy. We found this disease more often in younger patients, with minimal disc degeneration, and few has been known about myelopathy caused by soft disc hernation2,15,18,19,24).
Cervical myelopathy caused by soft disc herniation might show the acute myelopathy which is rapid progression of neurologic deficit of extremities, which is so similar to the brain symptoms, we sometimes misdiagnosed this disease as disorder of brain.
Authors presented the clinical features and surgical outcome of cervical myelopathy caused by soft disc herniations and analyzed the correlation between the symptom duration, radiologic finding, pain intensity and clinical outcome, retrospectively.
MATERIALS AND METHODS
Among the total 134 patients who underwent anterior cervical discectomy and fusion for cervical disc herniation from March 2010 to December 2010, there were 32 patients having soft cervical disc herniation without any osseous disease such as ossification of posterior longitudinal ligament (OPLL). Among these 32 patients, we excluded the patients who had cervical spondylosis such as congenital stenosis and cervical spinal canal diameter less than 12 mm, we analyzed 21 patients who presented the myelopathy as initial symptom with soft disc herniation, retrospectively.
In our study, myelopathy was defined as pattern of clinical presentation, such as walking difficulty, weakness of upper limb and hand, spasticity, hyperreflexia, patchy sensory loss, and autonomous dysfunction (bladder, bowel, and sexual dysfunction) and neurologic examination which include positive Hoffman's sign, balance problem, and increased sigh of deep tendon reflex (DTR).
We retrospectively evaluated the clinical and radiographic findings and postoperative changes by using medical records, radiological findings.
Preoperative clinical features including duration of myelopathy, pain intensity and postoperative clinical results including improvement rate of myelopathy and radiculopathy were retrospectively analyzed by Nurick Grade and Japanese Orthopaedic Association scale (JOA).
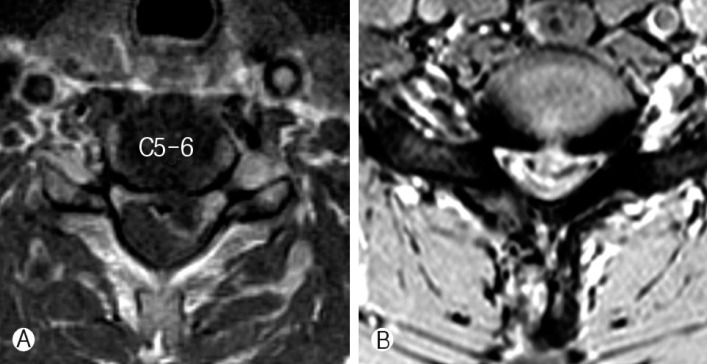
We also evaluated the locations of the disc herniation from the axial plan of preoperative cervical magnetic resonance imaging (MRI) to find out any difference according to shape of soft disc herniation. We determined central herniated disc as a median type and lateral herniated disc as a paramedian type. We also tried to evaluate the presence of signal changes of spinal cord on MRI.
We analyzed the clinical outcome and severity of myelopathy according to the intensity of initial pain, duration of myelopathy, type of disc herniation.
Intensity of pain was classified as two groups (mild to moderate, severe pain group) according to visual analogue scale.
To evaluate the correlation between the symptom duration and clinical outcome, we divide all patients into two group, group A included the patients whose symptom was continued over than 1 month, group B included the patients whose duration of symptom was lesser than 1 month.
RESULTS
General Demography and Clinical Features
Demographic data of this retrospective study was summarized on Table 1. Mean age was 49.7 years (range 22-74 years) and male outnumbered female (13:8). The most frequently involved level was C5-6 level (12 cases) and the next was C4-5 level (4 cases). Gait disturbance (15 cases) is most common clinical symptom and upper extremities weakness and bladder dysfunction were followed. All patients have pain with mild to severe degree. Among 21 patients, 9 patients (42.9%) of myelopathy showed severe pain, and 12 patients (57.1%) mild or moderate pain.
Table 1.
Clinical features of 21 patients with myelopathy caused by soft cervical disc herniation
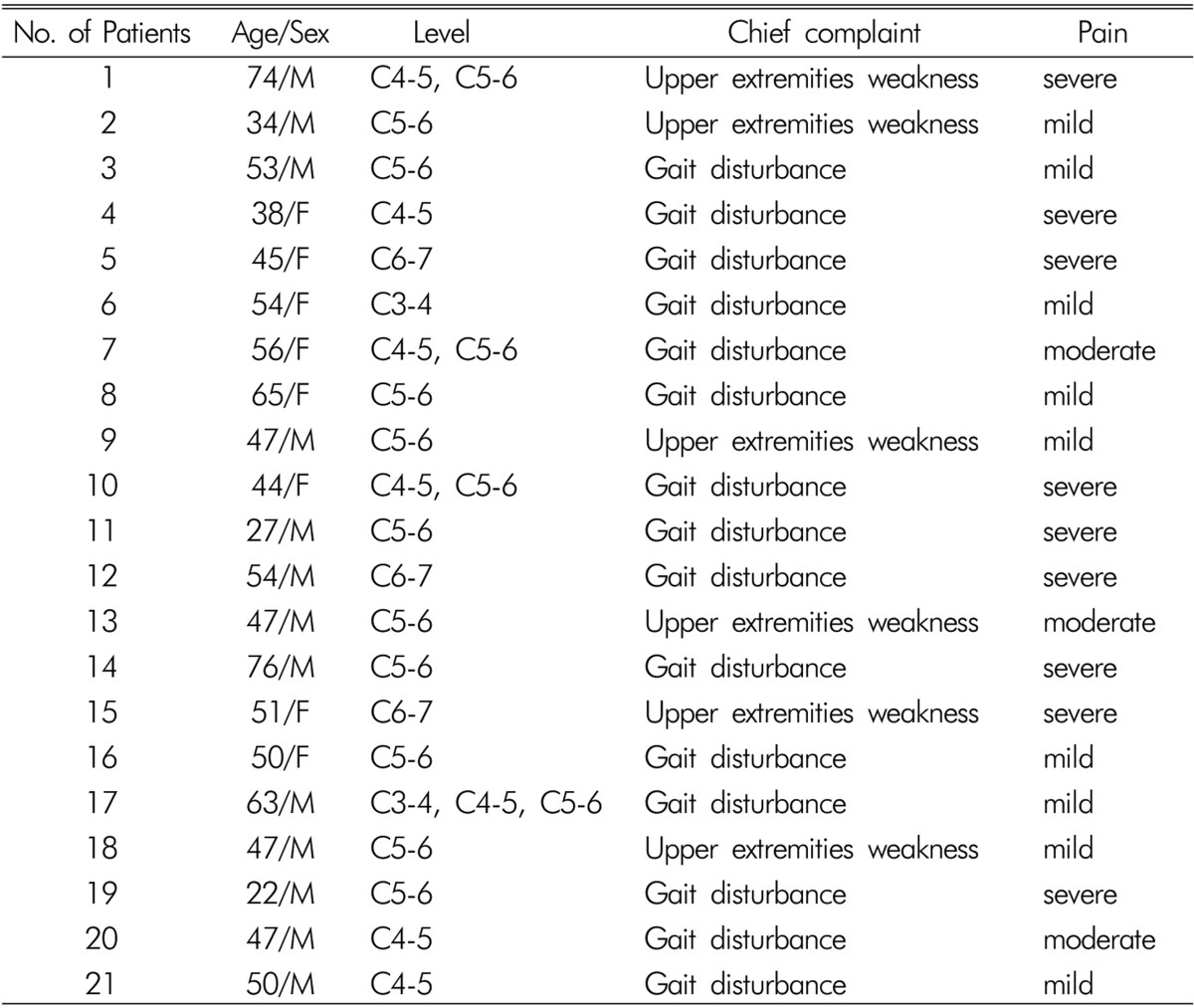
Regarding the cause of myelopathy, 17 cases (81.0%) were degenerative discogenic myelopathy and 4 cases (19%) were myelopathy secondary to minor trauma such as coughing, lifting. Mean duration of myelopathy is 1.18 months. On the basis of the MRI finding, paramedian type of disc herniation was seen in 16 cases (76.2%) and median type of disc herniation was seen in 5 cases (23.8%). Presence of spinal cord signal change on MRI (T2-weighted image) was detected in 7 cases (33.3%).
Clinical Outcomes
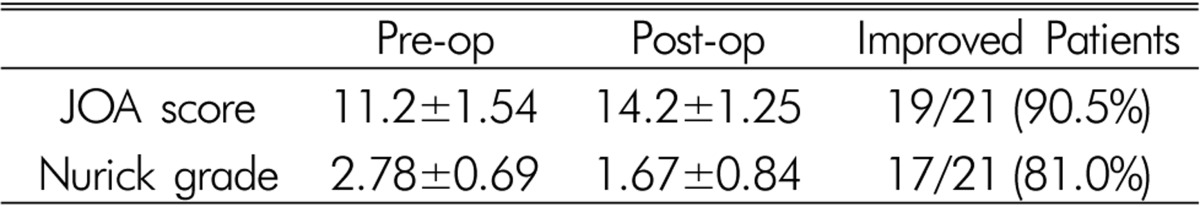
We performed anterior cervical discectomy and fusion (ACDF) in all cases. Table 2 represents change in Nurick' grade between preoperative and postoperative period. According to Nurick grade, improvement was seen in 17 patients (81.0%) of 21 patients and the other 4 patients (19.0%) showed no change after surgery. Mean pre-op Nurick grade was 2.78±0.69 and post-op grade was improved to 1.67±0.84. And according to JOA score, 19 patients (90.5%) of 21 patients showed improvement and the others (9.5%) showed no change after surgery. Mean Pre-op JOA score was 11.2±1.54 and mean post-op JOA score was improved 14.2±1.25. Overall surgical outcome of cervical myelopathy due to soft disc herniation showed relatively good outcome.
Table 2.
Postoperative changes of neurologic status (Mean±SD)
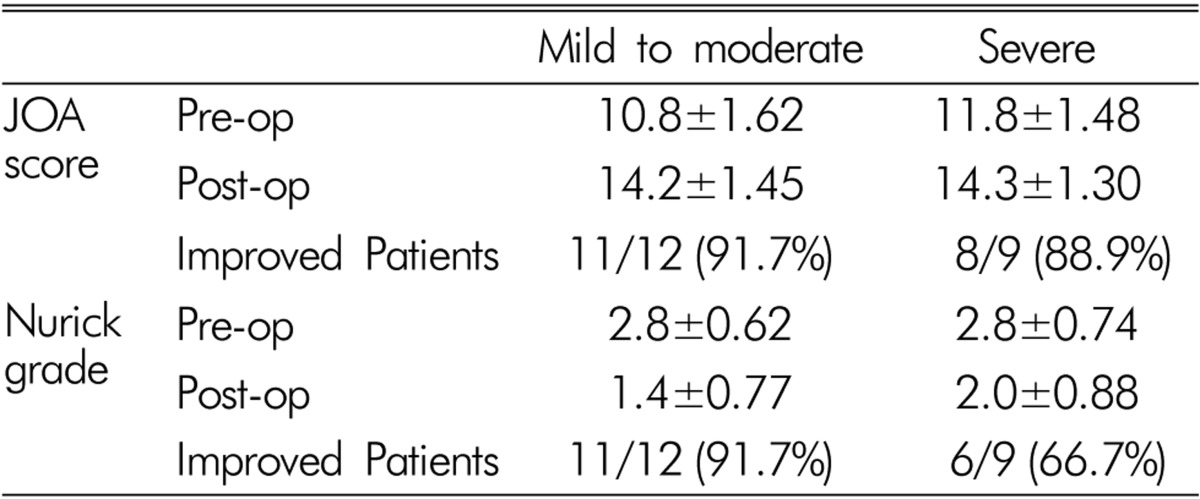
Pain Intensity and Clinical Outcomes
In comparison with severe pain group and mild to moderate pain group, mean pre-op Nurick grade of severe pain group was 2.8±0.74 and mean post-op Nurick grade was 2.0±0.88 (Table 3). Improvement was seen in 6 patients (66.7%) of 9 patients and the other 3 patients (33.3%) showed no change after surgery. Otherwise, mean pre-op Nurick grade of mild or moderate pain group was 2.8±0.62, and mean post-op Nurick grade was 1.4±0.77. Improvement was seen in 11 patients (91.7%) of 12 patients and the other 1 patients (8.3%) showed no change after surgery. According to Nurick grade, preoperative neurologic status of mild or moderate pain group was similar with severe pain group. However, improvement rate after surgery was better than severe pain group. On the basis of JOA score, mean pre-op JOA score of severe pain group was 11.8±1.48 and mean post-op JOA score was 14.3±1.30. Improvement was seen in 8 patients (88.9%) of 9 patients and the other 1 patients (11.1%) showed no change after surgery. Otherwise, mean pre-op JOA score of mild or moderate pain group was 10.8±1.62, and mean post-op JOA score was 14.2±1.45. Improvement was seen in 11 patients (91.7%) of 12 patients and the other 1 patients (8.3%) showed no change after surgery. According to JOA score, neurologic status of mild or moderate pain group on preoperative state was worse than that of severe pain group, however, improvement of JOA score after surgery was more prominent in mild to moderate pain group than in severe pain group.
Table 3.
Comparison of JOA score and Nurick grade between mild to moderate pain group and severe pain group (Mean±SD)
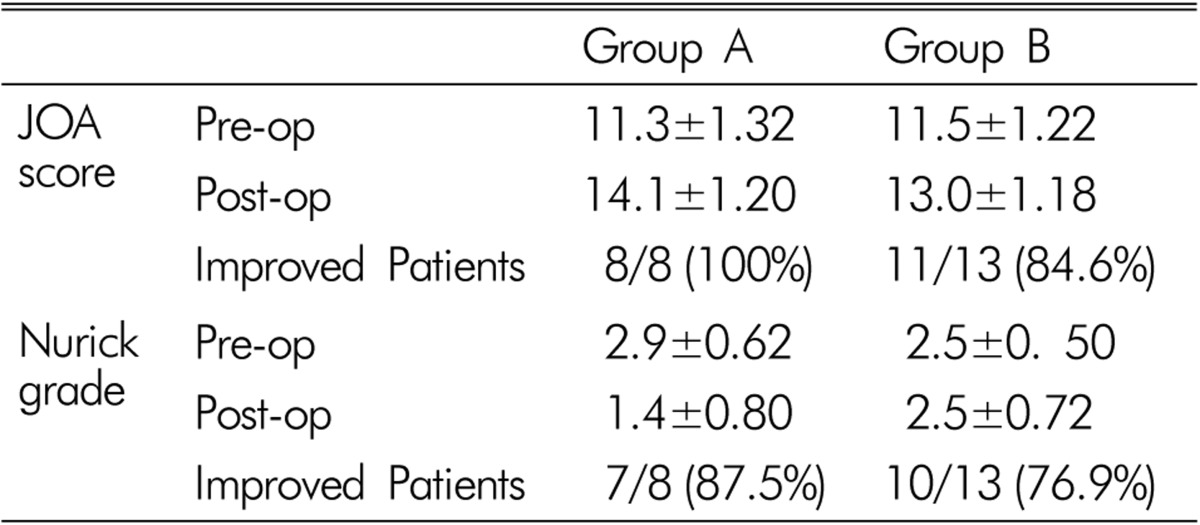
Symptom Duration and Clinical Outcome
According to JOA score, mean pre-op JOA score of group A was 11.3±1.32 and mean post-op JOA score was 14.1±1.20. Improvement was seen in all 8 patients (100%) after surgery (Table 4). Mean pre-op JOA score of group B was 11.5±1.22 and mean post-op JOA score was 13.0±1.18. Improvement was seen in 11 patients (84.6%) of 13 patients and the other 2 patients (15.4%) showed no change. According to Nurick grade, mean pre-op Nurick grade of group A was 2.9±0.62 and mean post-op grade is 1.4±0.80. Improvement was seen in 7 patients (87.5%) of 8 patients and the other 1 patients (12.5%) showed no change. Mean pre-op Nurick grade of group B was 2.5±0.50 and mean post-op grade was same with 2.5±0.72. Improvement was seen in 10 patients (76.9%) of 13 patients and the other 3 patients (23.1%) showed no change. This result showed that the patients whose symptom duration was shorter than one month showed lower clinical improvement rate than those with symptom duration of longer than one month.
Table 4.
Comparison of JOA score and Nurick grade between duration of symptom and neurologic recovery (Mean±SD)
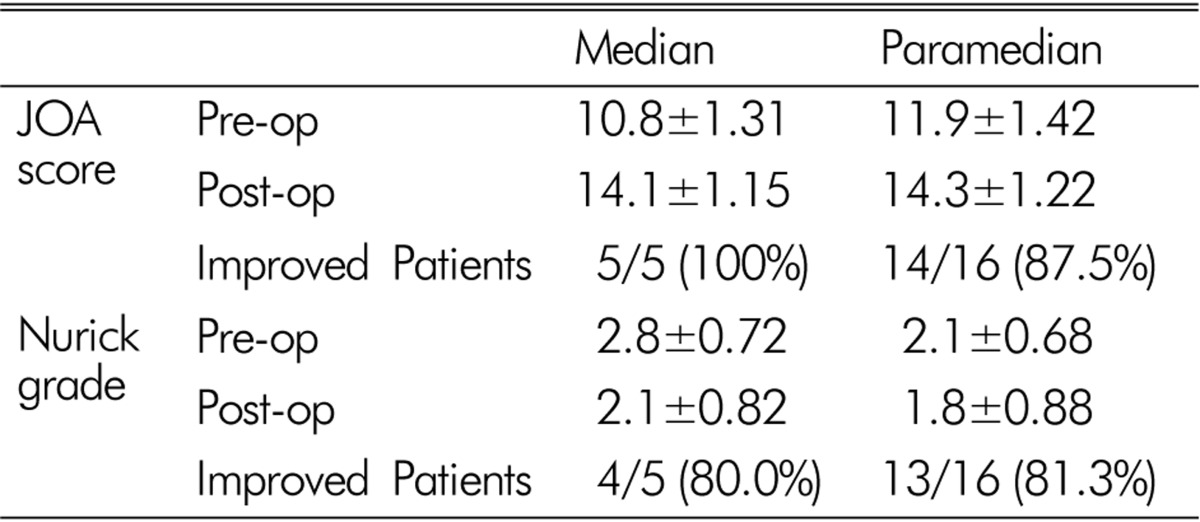
Type of Disc Herniation and Clinical Outcome
To find out the relationship between disc herniation type and outcome, we compared the median type of disc herniation with paramedian type of herniation. According to JOA score, mean pre-op JOA score of median herniation group was 10.8±1.31 and mean post-op JOA score was 14.1±1.15 (Table 5). Improvement was seen in all 5 patients (100%) after surgery. Mean pre-op JOA score of paramedian herniation group was 11.9±1.42 and mean post-op JOA score was 14.3±1.22. Improvement was seen in 14 patients (87.5%) of 16 patients and the other 2 patients (12.5%) showed no change. According to Nurick grade, mean pre-op Nurick grade of median herniation group was 2.8±0.72 and mean post-op grade was 2.1±0.82. Improvement was seen in 4 patients (80.0%) of 5 patients and the other 1 patients (20.0%) showed no change. Mean pre-op Nurick grade of paramedian herniation group is 2.1±0.68 and mean post-op grade is 1.8±0.88. Improvement was seen in 13 patients (81.3%) of 16 patients and the other 3 patients (81.3%) showed no change. Patients with median type of disc herniation showed poorer neurological status than those with paramedian type of herniation in preoperative state, however, postoperative improvement was similar between two groups.
Table 5.
Comparison of JOA score and Nurick grading between median disc herniated type and paramedian herniated type (Mean±SD)
DISCUSSION
Causes of cervical myelopathy would be numerous diseases such as cervical spondylosis, OPLL, tumor, infection(spondylitis), bony architectural abnormalities (fracture, dislocation) and soft cervical disc herniation9). And most common cause of myelopathy is cervical spondylosis in patients of more than 55 years of age8). Cervical spondylotic myelopathy (CSM) develops in almost all patients with more than 30% narrowing of the cross-sectional area of the cervical spinal canal, while some patients with severe cord compression do not have myelopathy8). The development of osteophytic spurs may lead to the narrowing of the spinal canal and potentially to mechanical compression of the neural elements. Long-standing compression of the spinal cord, in turn, can result in irreversible damage including demyelination and necrosis of the gray matter. This type of myelopathy is so called chronic myelopathy. Most of acute myelopathy is thought to result from the soft disc herniation and soft disc herniation is rarer than hard disc herniation8).
Incidence of soft cervical disc herniation associated with the cervical myelopathy has not been known exactly. In current study, soft cervical disc herniation accounts for approximately 23% of cause for cervical myelopathy.
Clinical manifestations of myelopathy are various, such as gait disturbance, spasticity, hand numbness, chest and abdominal discomfort, position and sensory disturbances, central cord syndrome, sphincter dysfunction, muscle atrophy8,11,13,14,25). It is reported that most prominent improved symptoms after surgery are spasticity and pain8). In the current study, the most common preoperative neurologic finding was gait disturbance.
In the point of radiological view, some literatures mentioned that congenitally narrow cervical canal or ligament hypertrophy which renders further compromise the spinal canal posteriorly might predispose the cervical myelopathy16). In current case, we did not evaluate the shape of spinal canal, which could be the shortage of our study. We found 7 cases (33.3%) of spinal cord signal change on MRI (T2-weighted image), however we did not evaluate these cases according to the clinical outcome. Further study of correlation between spinal cord signal changes and clinical improvement is mandatory. A few studies asserted the relation between direction of cervical disc herniation and severity of myelopathy. Lateral or posterior disc herniations are common causes of radiculopathy, whereas midline disc herniations sometimes lead to myelopathy10,16). Far lateral herniated discs are less likely produce the myelopathy, which would be related with probably due to buttressing effect by the uncinate process. In our evaluation of the direction of herniated disc, paramedian type of disc herniation showed predominant, and median type of herniation showed more severe clinical symptom initially. Many literatures asserted similar results1,5,21).
Several literatures mentioned that surgical outcomes of cervical discogenic myelopathy were better than that of spondylotic myelopathy3,6,7,17,22,23). We assumed that further prospective comparison of surgical results and outcomes between discogenic and spondylotic myelopathy would be needed. In current study, we presented the postoperative clinical improvement according to the JOA score and Nurick grade, however, we could not statistically show the improvement due to small number of our series. This would be the limitation of this study. They also asserted that the longer direct compression time of spinal cord could bring out the higher rate of irreversible injury. They presumed the pathophysiology that acute ruptured soft disc could make the sudden onset of interruption of blood supply of spinal cord might lead to the severe ischemia of the spinal cord and acute edematous cord and due to above mentioned reasons, myelopathy could be detected earlier and treated early without sequela. However, in current study, we have peculiar results that the patients with duration of symptom lesser than 1 month of myelopathy showed lower clinical improvement rate than the patients over than 1 month. We had two patients of spontaneous quadriplegia, who had complete spinal cord injury very rapidly, and remained irreversible in spite of urgent surgical decom- pression. We assumed that these severely injured patients might affect such a result of relation between symptom duration and clinical outcome. In such severely injured cases, we presumed that the vasculogenic impact might be related. Fergerson et al.12) expressed in the different point of view that acute presenting symptom might be related with vascular supply12). It has been proposed that compression by disc material to one of radicular spinal arteries at some point of its course or in the anterior spinal axis itself can produce ischemia of the spinal cord with zones of softening and necrosis, peculiar to the cervical myelopathy20). We also tried to compare the clinical outcome according to the pain intensity, which showed lessor clinical improvement rate in the severe pain intensity patients. This current result also support the vasculogenic theory of above mentioned literature. However, further comparison study according to the pain intensity especially for the group of mild pain intensity may be helpful in understanding the disease.
Bucciero et al.4) compared the recovery rate of myelopathy with that of radiculopathy after operation. Complete or most complete relief of preoperative symptomatology was observed in 95.6% of patients with radiculopathy and in 83.3% of those with myelopathy. Similar to the literature, in this study, successful relief of preoperative myelopathy was observed 90.4% in JOA score and 80.9% in Nurick grade, while radiculopathy was completely recovered.
We reported not only the clinical features of cervical myelopathy caused by soft disc herniation but also tried to analyze the clinical outcome according to clinical manifestations and radiologic findings. We assumed that patients with severe pain as initial symptom, and median type of disc herniation tended to show much more serious clinical features initially than the others. And we also presumed that mild to moderate pain as initial symptom, duration of myelopathy more than one month might be related with better clinical improvement after surgery, although number of cases was too small to have statistical analysis. Large number cases of cervical myelopathy secondary to soft disc herniation are needed to analyze the correlations between their clinical manifestations.
CONCLUSION
Authors reviewed the clinical features and surgical outcomes of the cervical myelopathy secondary to cervical soft disc herniation. In clinical features, gait problems are mostly seen without severe pain. Though their preoperative symptoms were severe, good surgical outcome can be expected. We presumed that patients of more than one month of symptom duration, mild to moderate initial symptom would be related with better postoperative improvement rate.
Fig. 1.
Type of disc herniation. (A) Paramedian type. (B) Median type.
References
- 1.Bae YJ, Lee JW, Park KS, Yeom JS, Kim KJ, Lee GY, et al. Compressive myelopathy: Magnetic resonance imaging findings simulating idiopathic acute transverse myelopathy. Skeletal Radiol. 2013;42(6):793–802. doi: 10.1007/s00256-012-1556-5. [DOI] [PubMed] [Google Scholar]
- 2.Bernhardt M, Hynes RA, Blume HW, White AA., 3rd Cervical spondylotic myelopathy. J Bone Joint Surg Am. 1993;75(1):119–128. doi: 10.2106/00004623-199301000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Boni M, Cherubino P, Denaro V, Benazzo F. Multiple subtotal somatectomy. Technique and evaluation of a series of 39 cases. Spine (Phila Pa 1976) 1984;9(4):358–362. [PubMed] [Google Scholar]
- 4.Bucciero A, Vizioli L, Cerillo A. Soft cervical disc herniation. An analysis of 187 cases. J Neurosurg Sci. 1998;42(3):125–130. [PubMed] [Google Scholar]
- 5.Chang H, Song KJ, Kim HY, Choi BW. Factors related to the development of myelopathy in patients with cervical ossification of the posterior longitudinal ligament. J Bone Joint Surg Br. 2012;94(7):946–949. doi: 10.1302/0301-620X.94B7.29018. [DOI] [PubMed] [Google Scholar]
- 6.Chiles BW, 3rd, Leonard MA, Choudhri HF, Cooper PR. Cervical spondylotic myelopathy: Patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery. 1999;44(4):762–769. doi: 10.1097/00006123-199904000-00041. discussion 769-770. [DOI] [PubMed] [Google Scholar]
- 7.Chiles BW, Leonard MA, Choudhri HF, Cooper PR. Cervical spondylotic myelopathy: Patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery. 1999;44(4):762–769. doi: 10.1097/00006123-199904000-00041. discussion 769-770. [DOI] [PubMed] [Google Scholar]
- 8.Crandall PH, Batzdorf U. Cervical spondylotic myelopathy. J Neurosurg. 1966;25(1):57–66. doi: 10.3171/jns.1966.25.1.0057. [DOI] [PubMed] [Google Scholar]
- 9.Dillin WH WR. Cervical disc disease. Spine. 1992;1:560–570. [Google Scholar]
- 10.Dubuisson A, Lenelle J, Stevenaert A. Soft cervical disc herniation: A retrospective study of 100 cases. Acta Neurochir (Wien) 1993;125(1-4):115–119. doi: 10.1007/BF01401837. [DOI] [PubMed] [Google Scholar]
- 11.Epstein JA, Marc JA, Hyman RA, Khan A, Mardayat M. Total myelography in the evaluation of lumbar discs. With the presentation of three cases of thoracic neoplasms simulating nerve root lesions. Spine (Phila Pa 1976) 1979;4(2):121–128. doi: 10.1097/00007632-197903000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Ferguson RJ, Caplan LR. Cervical spondylitic myelopathy. Neurol Clin. 1985;3(2):373–382. [PubMed] [Google Scholar]
- 13.Herkowitz HN, Kurz LT, Overholt DP. Surgical management of cervical soft disc herniation. A comparison between the anterior and posterior approach. Spine (Phila Pa 1976) 1990;15(10):1026–1030. doi: 10.1097/00007632-199015100-00009. [DOI] [PubMed] [Google Scholar]
- 14.Houser OW, Onofrio BM, Miller GM, Folger WN, Smith PL. Cervical spondylotic stenosis and myelopathy: Evaluation with computed tomographic myelography. Mayo Clin Proc. 1994;69(6):557–563. doi: 10.1016/s0025-6196(12)62248-4. [DOI] [PubMed] [Google Scholar]
- 15.Eun JP. Surgical experiences in the management of cervical spondylotic myelopathy. Korean J Spine. 2004;1(2):201–206. [Google Scholar]
- 16.Lestini WF, Wiesel SW. The pathogenesis of cervical spondylosis. Clin Orthop Relat Res. 1989;(239):69–93. [PubMed] [Google Scholar]
- 17.Lunsford LD, Bissonette DJ, Zorub DS. Anterior surgery for cervical disc disease. Part 2: Treatment of cervical spondylotic myelopathy in 32 cases. J Neurosurg. 1980;53(1):12–19. doi: 10.3171/jns.1980.53.1.0012. [DOI] [PubMed] [Google Scholar]
- 18.Mosdal C. Cervical osteochondrosis and disc herniation. Eighteen years' use of interbody fusion by cloward's technique in 755 cases. Acta Neurochir (Wien) 1984;70(3-4):207–225. doi: 10.1007/BF01406650. [DOI] [PubMed] [Google Scholar]
- 19.Murphey F, Simmons JC, Brunson B. Surgical treatment of laterally ruptured cervical disc. Review of 648 cases, 1939 to 1972. J Neurosurg. 1973;38(6):679–683. doi: 10.3171/jns.1973.38.6.0679. [DOI] [PubMed] [Google Scholar]
- 20.Rovira M, Torrent O, Ruscalleda J. Some aspects of the spinal cord circulation in cervical myelopathy. Neuroradiology. 1975;9(4):209–214. doi: 10.1007/BF00346149. [DOI] [PubMed] [Google Scholar]
- 21.Sah S, Wang L, Dahal M, Acharya P, Dwivedi R. Surgical management of cervical spondylotic myelopathy. JNMA J Nepal Med Assoc. 2012;52(188):172–177. [PubMed] [Google Scholar]
- 22.Saunders RL, Bernini PM, Shirreffs TG, Jr, Reeves AG. Central corpectomy for cervical spondylotic myelopathy: A consecutive series with long-term follow-up evaluation. J Neurosurg. 1991;74(2):163–170. doi: 10.3171/jns.1991.74.2.0163. [DOI] [PubMed] [Google Scholar]
- 23.Seifert V, Stolke D. Multisegmental cervical spondylosis: Treatment by spondylectomy, microsurgical decompression, and osteosynthesis. Neurosurgery. 1991;29(4):498–503. [PubMed] [Google Scholar]
- 24.Yamazaki S, Kokubun S, Ishii Y, Tanaka Y. Courses of cervical disc herniation causing myelopathy or radiculopathy: An analysis based on computed tomographic discograms. Spine (Phila Pa 1976) 2003;28(11):1171–1175. doi: 10.1097/01.BRS.0000067262.69584.0A. [DOI] [PubMed] [Google Scholar]
- 25.Yu YL, du Boulay GH, Stevens JM, Kendall BE. Computed tomography in cervical spondylotic myelopathy and radiculopathy: Visualisation of structures, myelographic comparison, cord measurements and clinical utility. Neuroradiology. 1986;28(3):221–236. doi: 10.1007/BF00548196. [DOI] [PubMed] [Google Scholar]