Abstract
Aims
Nose being the primary mode of air intake in humans can be obstructed in certain conditions and mouth takes over the process of breathing. As a result, there is a reduced or complete loss of function of nose, which shows underdevelopment or stunted growth (change in form). This can lead to impaired pneumatization that can result in dimensional changes in the sinus.
Objective
To assess volume alterations in maxillary sinus as secondary and as compensatory mechanism to altered functional matrices by comparing overall maxillary sinus volume of mouth breathers with normal breathers in the age group 12–14 years and to evaluate effect of gender on maxillary sinus volume.
Material and method
Maxillary sinus volume calculated using manual segmentation method from CBCT scans of 25 normal breathers and 25 mouth breathers were compared.
Results
Mean maxillary sinus volume of mouth breathers was significantly less than normal breathers (p < 0.05).
Conclusion
Mouth breathers showed lesser maxillary sinus volume but it is still uncertain whether the reduction in the volume of maxillary sinus is because the form of the maxillary sinus is affected due to improper functioning of nasal cavity or due to the underlying pathological condition resulting in poorly growing sinus.
Keywords: Adenoids, Mouth breathing, Maxillary sinus volume, CBCT, DICOM
1. Introduction
Nasal breathing is the primary mode of air intake for humans and it plays a pivotal role in correct muscular action stimulating adequate orofacial and nasopharyngeal growth. Many studies have shown the influence of breathing pattern on craniofacial growth.1,2 Mouth breathing becomes compensatory and obligatory in the presence of any obstruction in normal breathing, which may be due to allergic rhinitis, chronic sinusitis, adenoid or tonsillar hypertrophy, nasal polyps and deviated nasal septum.3–5 As mouth becomes the primary means of breathing, there is a reduced or complete loss of function of nose, which shows underdevelopment or stunted growth (change in form).6,7
According to Moss6 “All growth changes in size, shape, and spatial position, and the maintenance of all skeletal units are always secondary to specific functional matrices.” (i.e. capsular and periosteal matrix). The capsular matrix includes oral, pharyngeal and nasal cavity. Whenever function carried out by capsular matrix is hampered the growth of skeletal units will be affected. Assuming this, the growth of the sinus should also be dependent on functions carried out by nasal capsule. When the functioning of the nasal capsule is hampered due to mouth breathing, changes in the form of maxilla and paranasal sinuses should be expected. The four sets of paranasal sinuses – maxillary, frontal, sphenoid and ethmoidal could show poor development. These paranasal sinuses show growth by pneumatization.8 In presence of stunted growth, impaired pneumatization is also a possibility which indicates the likelihood of dimensional changes in the sinuses especially maxillary sinus as it is largest of all the paranasal sinuses.
Maxillary sinus volume reaches nearly adult size between the ages of 12 and 15 years with biphasic growth spurts i.e. rapid growth during the first 3 years and then again from the age of 7–12. The growth of maxilla is also considered to be completed by 12–14 years.8 Therefore, it is decided to evaluate maxillary sinus in the age group of 12–14 years.
Evaluation of maxillary sinus can be performed using radiographs (lateral and frontal), MRI and CT scans.9–11 Lateral and frontal head films offer limited information about the maxillary sinus, with the inherent errors of a 2D representation of a 3D structure. Although MRI is most superior in soft tissue rendering, its use is limited by its cost and restricted accessibility.
CBCT represents the latest generation in medical imaging and has become a well-accepted tool for oral and maxillofacial (OMF) diagnosis and treatment planning, mainly due to its advantages in lower effective radiation dose, lower costs, easy access and shorter acquisition times.12–15 Therefore, it was decided to evaluate maxillary sinus using CBCT scans.
Males and females show variations in volume. Generally, females have larger sinuses than males from age 4–10.10,16 However, in adults, males show larger sinuses than females.14 Hence, volumetric comparison will be done males and females of mouth breathers and nasal breathers.
Some authors such as Ikeda et al,10 Cho17 have calculated the volume of maxillary sinus in patients suffering from chronic sinusitis. However, no literature, to our knowledge has described the volume alterations in maxillary sinus of mouth breathers in comparison to normal breathers and even gender comparisons have not been carried out previously.
The purpose of this study was to evaluate dimensional alterations of maxillary sinus as secondary and as compensatory mechanism to altered functional matrices and to quantify any such changes in mouth breathers in comparison to normal breathers.
2. Material and method
The control group (Group I) was formed by 25 normal breathers (age group 12–14 years) referred from other departments to the Department of Oral and Maxillofacial Surgery for CBCT scans for various other diagnostic reasons. The test group (Group II) comprised of 25 mouth breathers (age group 12–14 years) who were screened for mouth breathing from the patients visiting the OPD of the Department of Orthodontics and Dentofacial Orthopaedics. The selection of mouth breathers was done using various diagnostic tests such as water holding test, mirror condensation test and cotton wisp test. As per these tests, 51 of these patients were found to be mouth breathers and referred to the ENT (ear, nose and throat) specialist for further evaluation. From these 51 patients, the patients with acute conditions were treated and 25 patients with chronic problem were referred for CBCT by the ENT specialist. These twenty five patients (mean age 13 years 4 months) with mouth breathing due to chronic problems were selected as a test group for this study. Each group was further subdivided into subgroups as shown in Table 1.
Table 1.
Groupwise distribution of subjects.
| Group I (Normal breathers) 25 | Group II (Mouth breathers) 25 | ||
|---|---|---|---|
| Subgroup IA | Subgroup IB | Subgroup IIA | Subgroup IIB |
| 12 males | 13 females | 13 males | 12 females |
All CBCT images were acquired with a New Tom QR-DVT 9000 SCANNER (110 kV, 14 mA), installed at Department of Oral and Maxillofacial Surgery (Fig. 1). The scans were taken with patient in supine position. Table 2 shows the specifications of the CBCT scanner. The records of the scan for each patient were taken in DICOM (Digital Imaging and Communications in Medicine) image format in a compact disc for further processing. Processing of DICOM images was done using Santé Editor 3.1 software (demo version) for the purpose of calculation of maxillary sinus volume (Fig. 2).
Fig. 1.
New Tom QR-DVT 9000 Scanner.
Table 2.
New Tom 3G QR-DVT 9000.
| Manufacture | Quantitative Radiology, Verona, Italy |
| Tube voltage | 110 kV, 14 mA |
| Grey scale depth | 256 |
| Scan time | 75–77 s |
| Rotation | 360° |
| Field of view (cm) | 13 |
| Slice thickness (mm) | 0.2 Axial |
| 2 Coronal | |
| 2 Sagittal | |
| Slice number | 360 |
| Voxel size | 0.3 mm2 |
| 0.28 mm3 | |
| Scanned volume dimensions | 150 × 150 mm |
| Bits per pixel | 8 |
| Data output | DICOM |
| Patient positioning | Supine |
Fig. 2.
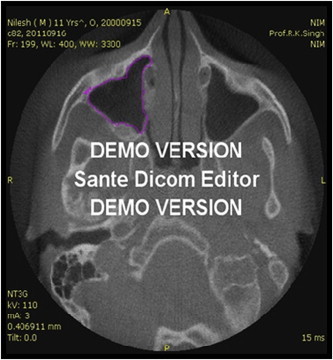
DICOM.
The DICOM files were transported from the compact disc into the computer. The axial slices were opened and the region of interest of each sample was defined by using the free hand ‘draw’ function to trace the perimeter of the radiopaque outline or the bony boundary of the right maxillary sinuses on each consecutive axial CT slice displayed on the computer monitor (Fig. 2) This was followed by calculation of area and volume of the traced region by selecting ‘selection info’ tool (Fig. 3). The volume of sinus in each slice was obtained by the software by multiplying the area (mm2) traced for maxillary sinus by the slice thickness (0.4 mm). Similarly, volume was calculated for all the slices starting from the first slice when maxillary sinus is visible to the last slice where it could be seen and was summed up to obtain the total volume of maxillary sinus of right side. Similarly, volume of left side was calculated.
Fig. 3.
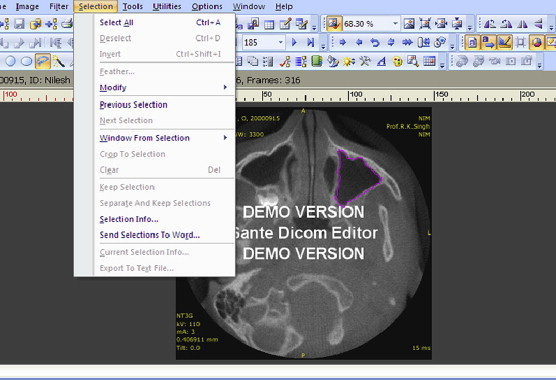
Calculation of volume using selection info tool.
3. Statistical tools employed
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) Version 15.0 statistical analysis software. Mean ± SD was calculated for maxillary sinus volume of both the sides in males and females of group I and II. Non-parametric tests i.e. Mann Whitney U test and Wilcoxon signed rank tests were used to evaluate significant difference between and amongst the mean maxillary sinus volume of two groups.
4. Observations
Table 3 shows the mean maxillary sinus volume in groups and subgroups. Table 4 shows the comparison of mean maxillary sinus volume between groups and subgroups. The results of inter and intragroup comparisons are also shown in Table 4.
Table 3.
Mean maxillary sinus volume of groups (I and II) and subgroups (IA, IB, IIA, IIB).
| Variables | Right side | Left side | Average volume |
|---|---|---|---|
| Group I | 12.916 ± 1.769 | 12.508 ± 1.509 | 12.712 ± 1.619 |
| Subgroup 1A | 12.27 ± 1.53 | 11.91 ± 1.31 | 12.09 ± 1.40 |
| Subgroup 1B | 13.62 ± 1.80 | 13.16 ± 1.48 | 13.39 ± 1.62 |
| Group II | 11.668 ± 1.593 | 11.528 ± 1.521 | 11.598 ± 1.520 |
| Subgroup IIA | 11.43 ± 1.72 | 11.33 ± 1.70 | 11.38 ± 1.67 |
| Subgroup IIB | 11.89 ± 1.50 | 11.72 ± 1.37 | 11.80 ± 1.40 |
Table 4.
Comparison of mean maxillary sinus between groups and subgroups.
| Variables | Right |
Left |
Average |
|||
|---|---|---|---|---|---|---|
| Z | P | Z | P | Z | P | |
| I & II (Overall) | 2.643 | 0.008* | 2.583 | 0.010* | 2.717 | 0.007* |
| IA & IB | 1.990 | 0.046* | 1.961 | 0.50** | 1.986 | 0.046* |
| IIA & IIB | 1.201 | 0.247** | 0.982 | 0.347** | 1.333 | 0.186** |
| IA & IIA | 1.663 | 0.098** | 1.858 | 0.068** | 1.823 | 0.068** |
| IB & IIB | 2.426 | 0.014* | 2.151 | 0.030* | 2.314 | 0.019* |
*p < 0.05 Significant, **p > 0.05 not significant.
5. Discussion
Whenever the function carried out by the nasal capsule is hampered due to mouth breathing the form of maxilla as well as maxillary sinus may be affected. In mouth breathing changes have been observed in the maxilla, hence it was anticipated that the underlying sinus may also undergo some changes. Therefore, it was decided to evaluate the effect of mouth breathing on the volume of the maxillary sinus.
The overall comparison between Group I and Group II showed (Fig. 4) that maxillary sinus volume showed a mean reduction of 1.12 cm3 in mouth breathers (Group II) that is in confirmation with Ikeda et al,10 who reported mean reduction of 1.13 cm3. Cho et al17 reported a reduction of 3.6 cm3 in the mean maxillary sinus volume in patients suffering from chronic rhinosinusitis in comparison to normal individuals. The magnitude of reduction was more, which may be due to the wide variations in age groups compared in his study (Control group, 32.69 years; chronic rhinosinusitis group 44.3 years).
Fig. 4.
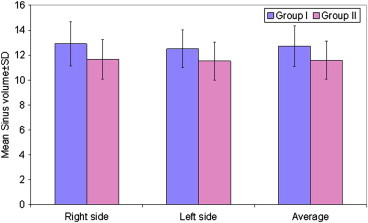
Comparison of mean sinus volume in Group I and Group II.
Contradictory to our findings, Fernandez et al11 reported that all paranasal sinuses except the sphenoidal sinus showed larger volumes in patients with sinusitis in age group of 1–20 years. In this wide range of age group maxillary sinus it shows growth and variations with pneumatization and not only by sinusitis, which could be the reason for this contradictory finding. The reduction in sinus volume may be attributed to either or both of these reasons, firstly, chronic inflammation is prone to occur in the poorly growing maxillary sinus which thickens the bony wall of the paranasal sinus, thereby causing reduction in overall volume and secondly, ethmoid infundibulum and middle meatus are narrowed by inflammation of the osteomeatal complex and by bony anatomic variations in the nasal cavity, leading to impaired pneumatization of the maxillary sinus. Both the reason seems logical but it is difficult to say whether this reduction in volume is because the form of maxillary sinus is affected due to improper functioning of nasal cavity and impaired pneumatization or due to the underlying chronic inflammation.
On comparing the volumes of right and left side, it was observed that there was no significant difference in Group I. Even Johnson18 reported that volume of maxillary sinus did not vary with side in normal subjects. However, the difference seen in Group II in the present study is similar to results shown by Fernandez11 in sinusitis group. This suggests that there was more chronic inflammatory involvement of one side of sinus in comparison to other. However, chronic inflammation is prone to occur in poorly growing sinus, hence both these factors are interrelated and it is difficult to say what the main causative factor.
Considering these findings, it can be suggested that the reduction in the sinus volume cannot completely be attributed to mouth breathing alone which results in stunted growth of nasal cavity and poor development of maxillary sinus, but also to the inflammatory status of sinus in mouth breathers.
Some authors have reported difference of the volume of the maxillary sinuses between males and females whereas others have showed no such difference. In this study, we found that mean maxillary sinus volume of females (13.39 ± 1.62 cm3) was significantly higher than males (12.09 ± 1.40 cm3) in Group I. As similar age groups were not selected in previous studies, direct comparison was not possible. But previous studies have shown that volume of maxillary sinus changes with age in males and females.10,16,18 According to Ikeda et al10 in age group of 4–9 years, females showed larger sinus whereas in age group of 10–15 years, males showed larger volumes. Karakas and Kavakli16 also found out that in age group of 5–10 years females had larger maxillary sinus volume than males and in the age group of 11–15 years, males showed an increase in the volume over females. Johnson18 stated that males had larger mean volume than females in the age group of 18–65 years.
In this study, we found that mean maxillary sinus volume of females was significantly higher than males in Group I which may be due to the fact that in the age group selected for this study, the female growth spurt must have been completed resulting in early completion of maxillary sinus growth in females. But growth was still in progress in males; hence, females had larger sinus volume than males in Group I. However, males and females of Group II did not show any significant difference in sinus volume suggesting that reduction in sinus volume is not gender dependant.
Male subjects of Group I (Subgroup IA) and Group II (Subgroup IIA) did not demonstrate significant difference in volume of maxillary sinus. Subgroup IIA had higher mean age (13 years 5 months) than Subgroup IA (12 years 4 months). This suggests that male subjects of Group II were ahead in growth as compared to males in Group I. This could be the reason for observing no significant difference in the volume for these subgroups wherein reduction in volume for Subgroup IIA was not seen which should have been observed otherwise.
Females of Group I (Subgroup IB) showed mean maxillary sinus volume significantly larger than females of Group II (Subgroup IIB). This could be attributed due to the fact that mean age of both the subgroups was comparable (Subgroup IB had mean age of 13 years 3 months and Subgroup II B had mean age of 13 years 5 months), and towards the completion of growth in females. Thus, reduction in maxillary sinus volume was observed in females in Group II, similar to the trend observed in overall comparison of Group I and Group II.
Thus, female did show larger maxillary sinus volume in normal breathers but there was no significant difference in volume observed in mouth breathers.
This study was an initial attempt to evaluate the dimensional changes in maxillary sinus of mouth breathers in comparison to normal breathers. Although, it demonstrated a conspicuous result, further longitudinal studies are necessary with larger sample sizes in order to confirm our findings.
6. Conclusion
Following were the conclusions drawn from this study:
-
1.
The volume of maxillary sinus in mouth breathers was significantly lower than normal breathers. However it remains unclear whether it is because of improper functioning of nasal cavity or due to the underlying pathological condition.
-
2.
Another finding in our study was that the maxillary sinus volume of right and left side differed significantly amongst the mouth breathers, it suggests that chronic inflammation of the sinus is more likely the cause for this. The chronic inflammation causes thickening of bony wall of the sinus, thereby reducing its volume. However, chronic inflammation is prone to occur in poorly growing sinus, hence both these factors are interrelated and it is difficult to say which the main causative factor is.
-
3.
Females and males did not show any significant differences in maxillary sinus volume in mouth breathers suggesting that reduction in sinus volume is not gender dependant.
Conflicts of interest
All authors have none to declare.
References
- 1.Bosma J.F. Maturation of function of the oral and pharyngeal region. Am J Orthod. 1963;49:94–104. [Google Scholar]
- 2.Todd T.W. Integral growth of the face. Int J Orthod. 1936;22:321–334. [Google Scholar]
- 3.Gois, Junior R., Vale Influence of nonnutritive sucking habits, breathing pattern and adenoid size on the development of malocclusion. Angle Orthod. 2008;78(4):647–658. doi: 10.2319/0003-3219(2008)078[0647:IONSHB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Neivert H. The lymphoid tissue problem in the upper respiratory tract. Am J Orthod. 1939;25(6):544–554. [Google Scholar]
- 5.Arun T., Isik F., Sayinsu K. Vertical growth changes after adenoidectomy. Angle Orthod. 2003;73:146–150. doi: 10.1043/0003-3219(2003)73<146:VGCAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Moss M.L. The primacy of functional matrices in orofacial growth. Dent Pract. 1968;19(2):65–73. [PubMed] [Google Scholar]
- 7.Farid M.M., Metwalli N. Computed tomographic evaluation of mouth breathers among paediatric patients. Dentomaxillofac Radiol. 2010;39:1–10. doi: 10.1259/dmfr/80778956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enlow D.H., Poston W.R. W B Saunders; Philadelphia: 1990. Facial Growth. [Google Scholar]
- 9.Oktay H. Study of maxillary sinus areas in different malocclusions. Am J Orthod. 1992;102:143–145. doi: 10.1016/0889-5406(92)70026-7. [DOI] [PubMed] [Google Scholar]
- 10.Ikeda A., Ikeda M., Komatsuzaki Atsushi. A CT study of the course of growth of maxillary sinus: normal subjects and subjects with chronic sinusitis. ORL. 1998;60:147–152. doi: 10.1159/000027584. [DOI] [PubMed] [Google Scholar]
- 11.Fernandez S., Escuredo A., Sanchez A., Santaolalla F. Morphometric study of the paranasal sinuses in normal and pathological conditions. Acta Otolaryngol. 2000;120:273–278. doi: 10.1080/000164800750001080. [DOI] [PubMed] [Google Scholar]
- 12.Gerson l. Computerized axial tomography: a brief survey. Bull Texas Heart Inst. 1975;4:237–239. [Google Scholar]
- 13.Martin J., How Kau C., Bahl L., Hans M. Three-dimensional cone beam computerized tomography in dentistry. Int Dentistry. 2007;9:40–49. [Google Scholar]
- 14.Martınez R.G., Swennen G.R.J. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011;76:1–11. doi: 10.1016/j.ijom.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 15.Ariji Y., Kuroki T., Moriguchi S., Ariji E., Kanda S. Age changes in the volume of the human maxillary sinus: a study using computed tomography. Dentomaxillofac Radiol. 1994;23(3):163–168. doi: 10.1259/dmfr.23.3.7835518. [DOI] [PubMed] [Google Scholar]
- 16.Karakas, Kavakli A. Morphometric examination of the paranasal sinuses and mastoid air cells using computed tomography. Ann Saudi Med. 2005;25(1):41–45. doi: 10.5144/0256-4947.2005.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho S.H., Kim T.H., Kim K.R., Lee J.M., Lee D.K., Kim J.H. Factors for maxillary sinus volume and craniofacial anatomical features in adults with chronic rhino sinusitis. Arch Otolaryngol Head Neck Surg. 2010;136(6):610–615. doi: 10.1001/archoto.2010.75. [DOI] [PubMed] [Google Scholar]
- 18.Johnson P.S., Jannert M., Strombeck A., Abul K. Computed tomography measurements of different dimensions of maxillary and frontal sinuses. BMC Med Imaging. 2011;11(8):1–7. doi: 10.1186/1471-2342-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


