Abstract
Background
Cervical cancer disproportionately affects Latina women in the United States. This study evaluated the impact of patient navigation on cervical cancer prevention in Latinas.
Methods
Between January 2004 and April 2011, 533 Latina women with an abnormal Pap smear requiring colposcopy received patient navigation from their healthcare center in Chelsea, Massachusetts, to the Massachusetts General Hospital (MGH). The comparison group comprised 253 non-navigated Latinas from other primary care practices at MGH referred to the same MGH colposcopy clinic. Primary outcomes were the percentage of missed colposcopy appointments, time to colposcopy, and changes in the severity of cervical pathology at colposcopy over two time periods, 2004–2007 and 2008–2011.
Results
The mean age in both groups was 35 years (range 22–86). Navigated women had fewer missed colposcopy appointments over time, with the average falling from 19.8% to 15.7% (p=0.024), compared with an insignificant increase in the no-show rates from 18.6% to 20.6% (p=0.454) in the comparison group. The difference in the no-show rate trend over time between the groups was significant (p<0.001). The time to colposcopy did not change in either group, though trends over time demonstrated a shorter follow-up for navigated women (p=0.010). The grade of cervical abnormality among navigated women decreased from a numerical score of 2.03 to 1.83 (p=0.035) over the two time intervals, while the severity of pathological score in the non-navigated group did not change significantly from 1.83 to 1.92 (p=0.573) in the same interval. Comparison of trends in pathological score over time showed a decrease in the severity of cervical abnormality for navigated participants compared to the non-navigated group (p<0.001).
Conclusion
Patient navigation can prevent cervical cancer in Latina women by increasing colposcopy clinic attendance, shortening time to colposcopy, and decreasing severity of cervical abnormalities over time.
Introduction
In the United States, rates of cervical cancer morbidity and mortality have fallen dramatically since the Pap smear was developed in 1941 and cervical cancer became a preventable disease.1 However, the benefits have been unevenly distributed among racial and ethnic groups and along the spectrum of socioeconomic status.2 It is estimated that over 12,000 women will be diagnosed with and 4,220 will die from cervical cancer in 2012 in the United States.3 Latina women continue to have high rates of cervical cancer incidence and mortality compared to other groups, with an incidence rate almost twice as high and a mortality rate 1.5 times higher than non-Latina Caucasian women.4
The disproportionate disease burden among Latinas can be attributed to different factors, such as lack of awareness about prevention, language barriers, and limited access to health care.5–9 Their cervical cancer screening rates are also lower than rates among non-Latinas.10 Latinos in the US are more than twice as likely as non-Hispanic whites to live in poverty11 and studies have shown that up to 50% of low-income women do not receive the recommended follow up care after an abnormal Pap smear.12
Harold Freeman introduced the model of patient navigation to facilitate access to cancer care for minorities in 1990 and the concept has been implemented in various forms to improve prevention, diagnosis and treatment of cancer throughout the United States and around the world.13–19 Two recent studies have shown that navigation can significantly improve cervical cancer screening compliance.20,21 Other methods such as telephone counseling and educational brochures sent prior to colposcopy appointments improve patient follow up after an abnormal Pap smear.22,23 Ell et al.,24 using the Screening Adherence Follow-Up (SAFe) intervention model, improved adherence rates after an abnormal Pap smear in low-income Latina women. However, knowledge about the long-term effects of these programs on cervical cancer prevention is limited.
To improve cervical cancer prevention among Latina women, Massachusetts General Hospital (MGH) Chelsea HealthCare Center established the Cervical Health Patient Navigator Program in 2004. The program aims to reach out to Latina patients in Chelsea who need follow-up care at the MGH Colposcopy Clinic following an abnormal Pap smear.
The objective of this study was to evaluate the effects of the cervical cancer patient navigator program on colposcopy clinic attendance, colposcopy clinic follow up time, and the grade of cervical abnormality at colposcopy among Latina women in the program, and to determine the impact of an 8-year ongoing intervention on cervical cancer prevention for Latina women.
Materials and Methods
Setting
The study was conducted at the MGH Colposcopy Clinic and the MGH Chelsea HealthCare Center (MGH Chelsea), an urban community health center in Massachusetts. MGH Chelsea is the largest provider of care for the residents of Chelsea, Massachusetts, which has long been a gateway for refugees and immigrants. Latinos account for more than 62% of the population,25 over 54% speak Spanish26 and more than 24% of Chelsea residents live at or below poverty level.25 The incidence of cervical cancer in Chelsea is well above the state average (11.0 vs. 6.0 per 100,000)27 and the mortality in Chelsea is double the state average (2.5 vs. 1.2 per 100,000).28 Twenty percent of all patients seen at the MGH Colposcopy clinic are referred from MGH Chelsea and over 75% of these women are Latina.
Participants
Women were eligible for the study if they self-identified as Latina, had an abnormal Pap smear requiring colposcopy evaluation between January 1, 2004 and April 15, 2011. Eligible women who were referred for colposcopy by an MGH Chelsea provider comprised the intervention group, and eligible women referred for colposcopy from other practices within the same academic primary care network constituted the comparison group. Participants were identified from colposcopy clinic schedules and billing records.
Intervention
The Cervical Health patient navigation started in 2004. A Latina-immigrant woman and native Spanish speaker from the Chelsea community was hired and trained in patient navigation, cervical health, and cervical cancer. Patients were referred to patient navigation by the colposcopy clinic staff. Each week the staff generated a list of patients from MGH Chelsea who had missed colposcopy appointments. Over time, the lists were expanded and all Latinas from MGH Chelsea in need of colposcopy were referred for patient navigation prior to their colposcopy appointment. During the initial call, the navigator explored women's barriers to care and proposed solutions. She educated women in their own language about cervical cancer and prevention and assisted them with transportation, insurance, child care, and appointment scheduling. The most intense navigation was needed at the initial contact, often requiring several phone calls, a face-to-face meeting, or even a home visit. The navigator would accompany the most challenging patients (3–4 per month) to colposcopy appointments at MGH. The time spent with each patient varied from 1–8 hours. The navigator continued to follow the patients until they were discharged from the colposcopy clinic.
Supervision of the navigator was provided by a social worker and nurse practitioner with expertise in women's health issues. Foundation support provided $70,000 per year for the navigator salary and supervision, while $5,000 per year was available for patient expenses, educational materials, and program evaluation.
Main outcomes
The primary outcomes of this study were the percentage of missed colposcopy appointments, time to colposcopy follow-up after an abnormal Pap smear, and the grade of cervical abnormality at colposcopy. Using electronic medical records, data were collected on socio-demographic characteristics, the presence of co-morbid medical conditions (such as diabetes, end stage kidney disease, or psychiatric diagnosis), severity of Pap smear diagnosis, and pathological findings at colposcopy, time from abnormal Pap smear to colposcopy, colposcopy clinic no-show rates, total no-show rates, and whether women received follow-up care with their primary care physician or gynecologist after colposcopy.
Statistical analysis
Summary statistics were used to describe baseline characteristics of the intervention and comparison groups. Chi-square tests and Student t-tests were used to analyze categorical and continuous variables, respectively. The navigated and non-navigated groups were compared with respect to the percentage of missed colposcopy appointments, the time to colposcopy after an abnormal Pap smear, and the severity of cervical abnormality at the time of colposcopy. Grades of cervical abnormality at the time of colposcopy visit were assigned numerical values 1–5 for statistical analysis, where 1=no dysplasia/ASCUS; 2=mild dysplasia/CIN I/LGSIL; 3=moderate dysplasia/CIN II/HGSIL; 4=severe dysplasia/CIN III; and 5=carcinoma in situ.28 Difference-in-difference analysis was used to compare the trends in the primary outcomes of interest for each group over time. In order to match approximately equal numbers of comparison and navigated patients in each time period the study was divided into two 4-year periods (2004–2007 and 2008–2011). This also allowed us to evaluate the effects of improvements, such as change in leadership and expansion of the reminder calls, that were made in the program over time. Multivariate logistic regression was used to identify factors that were independently associated with colposcopy clinic attendance. Variables for which <80% of patient had data available were excluded from the analysis. Pap smear results were also assigned numerical values to facilitate analysis, where ASCUS=1, LGSIL=2, and HGSIL=3.28 All tests were two-sided and p values<0.05 were considered statistically significant.
Our analyses were performed using the Intercooled Stata statistical software package (version 11.0; StataCorp LP). Approval from the Massachusetts General Hospital Institutional Review Board was obtained prior to the initiation of the study.
Results
Of the 911 women eligible for the study, 125 (13.7%) were excluded because there was no record of an abnormal Pap smear, or because their abnormal Pap smear, colposcopy visit, or follow up procedure occurred prior to 2004. A similar percentage of eligible women were excluded from both the navigator and comparison groups. Of the 786 patients included, 533 (67.8%) were navigated participants from MGH Chelsea, and 253 (32.2%) subjects were Latina women referred for colposcopy from the other MGH primary care practices, which comprised the comparison group. Because a majority of the Latina women within the MGH primary care network receive care at MGH Chelsea, the navigated group comprised a large proportion of study participants.
Table 1 summarizes the sociodemographic characteristics of the navigated and comparison groups. While this was not a randomized study, most characteristics of the two groups were comparable. The mean age in both groups was approximately 35 years and similar percentages were single, married, separated, divorced and widowed (p=0.646). In addition, the difference in proportions of patients with significant comorbid medical diagnoses in the groups was not statistically significant (24.8% of the navigated vs. 20.6% of the comparison group, p=0.19). However, there were significant differences in the educational attainment and insurance status of the two groups. The comparison group had a higher proportion of patients with commercial (private) insurance compared with the navigated group (34% vs. 24%, p=0.006), though both groups had a similar proportion of uninsured patients (7.4% vs. 8.4%, p=0.63). Greater proportions of the comparison group had completed some college (21.1% vs. 13.2%, p=0.04) or graduated from college (21.0% vs. 6.8 %, p<0.001) compared to the navigated group. Nearly half of the navigated women (47.6%) had less than a high school education compared with only 22.8% of the comparison group (p<0.001).
Table 1.
Sociodemographic Characteristics of Navigator and Comparison Groups
| Variable | Navigator group (95% CI) | Comparison group (95% CI) | p-value |
|---|---|---|---|
| Age (mean) | 35.3 yrs (SD 9.7) | 34.6 yrs (SD 9.7) | 0.37 |
| Marital Status | 0.646 | ||
| Single | 68.4% (64.2–72.6) | 65.6% (59.2–71.70) | 0.45 |
| Married | 23.8% (19.9–27.6) | 27.3% (21.4–33.1) | 0.33 |
| Separated | 2.3% (1.0–3.7) | 2.7% (1.0–4.9) | 0.76 |
| Divorced | 5.5% (3.5–7.6) | 2.7% (1.0–4.9) | 0.10 |
| Comorbid Diagnosis | 24.8% (21.1–28.4) | 20.6% (15.6–25.5) | 0.19 |
| Education level | 0.348 | ||
| Less than high school | 47.6% (42.3–53.0) | 22.8% (15.1–30.1) | <0.001 |
| High school grad | 32.3% (27.4–37.3) | 35.1% (26.3–43.8) | 0.59 |
| Some college | 13.2% (9.6–16.8) | 21.1% (13.6–28.5) | 0.04 |
| College grad or more | 6.8% (4.1–9.4) | 21% (13.6–28.5) | <0.001 |
| Insurance status | 0.069 | ||
| Public | 68.6% (64.5–72.7) | 57.6% (51.1–64.1) | 0.004 |
| Commercial | 24.0% (20.2–27.8) | 34.0% (27.7–40.1) | 0.006 |
| No insurance | 7.4% (5.1–9.8) | 8.4% (4.8–12.1) | 0.63 |
CI, confidence interval; SD, standard deviation.
The distribution of countries of origin of the groups was similar. Fourteen Latin American countries were represented. The navigated group contained a larger proportion of patients from Honduras (21.2% vs. 6.1%, p<0.001) and the comparison group had more women from Guatemala (16.1% vs. 13.3%, p=0.05), Colombia (15.3% vs. 5.6%, p=0.002) and Mexico (11.2% vs. 3.5%, p=0.002). Differences in the fraction of patients from the other 10 countries were not statistically significant and the overall chi-square for the difference in distribution of countries of origin was not significant (0.261).
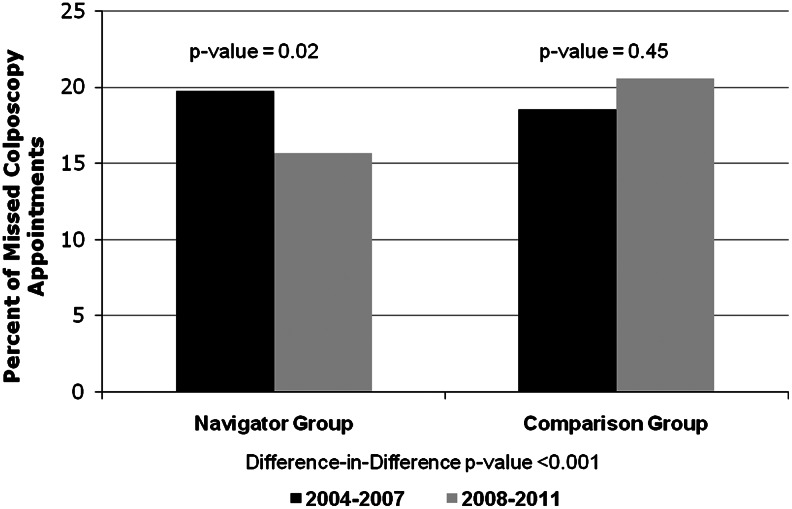
Figure 1 summarizes the analysis of the percentage of missed colposcopy clinic appointments for the navigated and comparison groups over time. In the navigated cohort, there was a significant decrease in the percentage of missed colposcopy clinic appointments between 2004 and 2007 and 2008 and 2011, with the average falling from 19.8% in the first period (95% confidence interval [CI] 17.5, 22.1) to 15.7% in the second period (95% CI 13.1, 18.4, p=0.024). The comparison group no show rate did not change significantly between the first and second study periods, slightly increasing from 18.6% (95% CI 14.8, 22.5) to 20.6% (95% CI 17.0, 24.2, p=0.454). The difference-in-difference analysis demonstrated that the trends in no show rates over the two time intervals for the navigated and non-navigated groups were significantly different (p<0.001).
FIG. 1.
Percentage of missed colposcopy appointments over time.
The time to colposcopy follow-up for navigation participants did not change significantly between the two study periods (127 days [95% CI 115, 140] to 120 days [95% CI 108, 131, p=0.393]). The time for the comparison group increased (116 days [95% CI 97, 134] to 122 days [95% CI 93, 151]) but the change was not significant (p=0.717). However, the difference-in difference analysis of the trends in the follow up time between the two groups over time revealed a significant difference favoring the navigated patients (p=0.010).
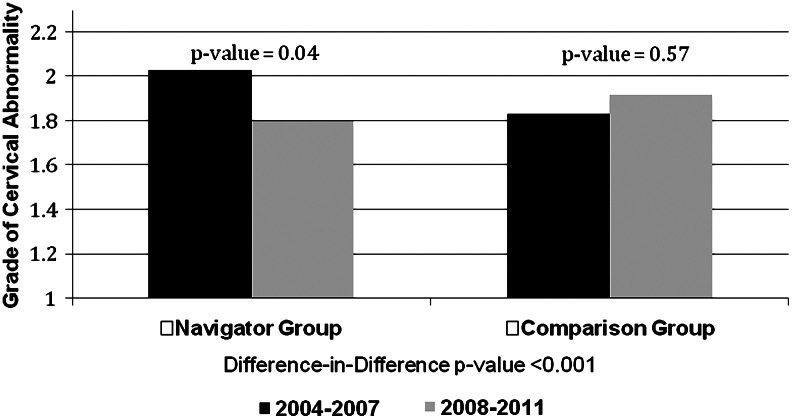
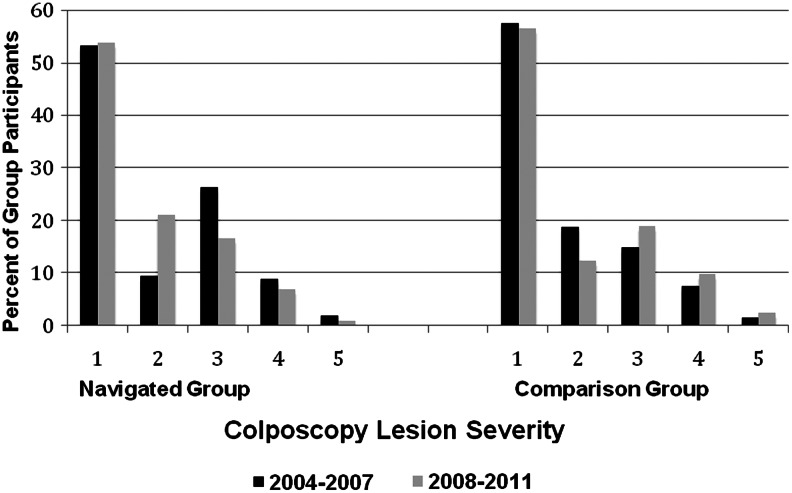
Figure 2 summarizes trends in the severity of cervical abnormalities for each group. The mean numeric value of pathologic and cytological findings at colposcopy in the navigated group significantly decreased between 2004–2007 and 2008–2011, (2.03 [95% CI 1.84, 2.22] to 1.83 [95% CI 1.69, 1.90, p=0.035]). In contrast, the average severity in the comparison group was insignificant, increasing from 1.80 (95% CI 1.66, 2.0) to 1.92 (95% CI 1.66, 2.17, p=0.573). A comparison of the data over time demonstrated a significant difference in the trends of the lesion severity of the two groups (p<0.001). The decrease in the average severity for the navigated group included a 23% decrease in the number of patients with severe dysplasia and a 47% decrease in the number of patients with carcinoma in situ. In the comparison group, the number of patients with severe dysplasia increased (30.7%), as well as the number of subjects with carcinoma in situ (66.7%) from the first to the second time period (Fig. 3).
FIG. 2.
Effect of patient navigation on severity of colposcopy diagnosis over time.
FIG. 3.
Distribution of colposcopy lesions severity over time in navigated and comparison groups.
Using linear regression analysis (Table 2) of factors influencing colposcopy clinic attendance, we found that navigation was associated with a decrease in the colposcopy no-show rate by 3% when controlling for other factors, but the effect was not statistically significant (p=0.196). Marital status and a comorbid medical condition did not significantly affect the colposcopy attendance rate. Pap smear diagnosis severity was an important factor, with higher severity associated with a decrease in the colposcopy no-show percentage by approximately 2% (p=0.039) for each level of increasing severity (mild to moderate and moderate to severe). The no-show rate also decreased by approximately 0.3% for each additional year of age (p=0.043). A record of regular screening (every 2–3 years) with Pap smears prior to the abnormal Pap smear for which they were sent to colposcopy was associated with a decrease of 19.2% (p=0.046). Insurance type was the final variable that was significantly correlated with the outcome of interest. Those covered by public (Medicaid/Medicare) insurance had a no-show rate 5% higher than those did with commercial insurance (p=0.025), and uninsured patients had an 11.7% higher no-show percentage compared with those with state insurance (p=0.002).
Table 2.
Multivariate Linear Regression Model Results for the Association Between Colposcopy Clinic No-Show Rate Percentages and Intervention Status Among All Patients
| Parameter | Regression coefficient | 95% CI | p-value |
|---|---|---|---|
| Navigator intervention | −2.97 | −7.5−1.5 | 0.196 |
| Colposcopy diagnosis severity | −2.12 | −4.6−0.35 | 0.039 |
| Age (yearly increment) | −0.28 | −0.55 to −0.01 | 0.043 |
| Marital status | |||
| Single | – | – | – |
| Married | −3.15 | −7.7−1.4 | 0.175 |
| Separated | −9.43 | −20.2−1.3 | 0.085 |
| Divorced | −2.41 | −12.6−7.8 | 0.640 |
| Widowed | 6.65 | −5.1−18.4 | 0.266 |
| Insurance status | |||
| Public insurance (Mass Health) | – | – | – |
| Commercial insurance | −5.03 | −9.4 to −0.6 | 0.025 |
| No insurance | 11.7 | 4.5−19.0 | 0.002 |
| Comorbid diagnosis | 1.19 | −4.3−6.7 | 0.673 |
| Regular cervical screening | −19.2 | −38.0 to −0.38 | 0.046 |
Discussion
This study demonstrates that a culturally tailored patient navigation program can improve cervical cancer prevention over an eight year time period among Latina women. Navigated women had better rates of colposcopy clinic attendance, shorter time to colposcopy clinic follow up, and a less severe grade of cervical abnormality at colposcopy.
Like the SAFe pilot project,24 this study shows that navigation improves adherence to colposcopy follow-up after an abnormal Pap smear in low-income Latinas. In this study, adherence improved over time, as the navigator and patients learned to work together to overcome barriers to care. In multivariate models, a number of factors were associated with decreased compliance. Colposcopy attendance was lower among women with no insurance or public insurance, consistent with previous studies.30–32 However, in the navigated patient population, 76% of whom did not have private insurance, the no-show rate over time decreased significantly compared to a stable rate in non-navigated women. The improvement in compliance over time could be a cumulative effect of the navigator's increased skill and the development of trust within the Latino community. Increased age and increased severity of diagnosis were associated with lower percentages of missed colposcopy appointments, as reported in previous studies.30,32–36
According to the 2012 American Cancer Society update on cancer statistics for Latinos, cancer was the leading cause of death in this group.37 The most clinically important potential impact of patient navigation on cervical cancer prevention was a decrease in the grade of severity in cervical pathology/cytology in the navigated group relative to the comparison group during the study period. It is possible that low-grade lesions (grade 1 and 2) could have regressed on their own.38 However, although the decrease in the average severity for the navigated group was small, it reflects a decreased percentage of higher-grade findings (3, 4, and 5) (Fig. 3). There was a substantial decrease in the percentages of navigated women with severe dysplasia and carcinoma in situ, while the comparison group had a small proportional increase of patients with these types of lesions. A change in grade leads to less invasive treatment, fewer side effects from treatment and a lower risk of developing invasive cervical cancer in the future.
The average time from an abnormal Pap smear to colposcopy for both navigated and non-navigated groups was quite long—approximately 120 days. However, the follow up period included the time required for the pathologist to read the Pap smear and for the primary care physician to receive the results and refer the patient to colposcopy—on average 6–8 weeks. To shorten the time between the Pap smear and colposcopy appointment, systems interventions are needed to provide greater efficiency in the cytological interpretation of Pap smears and in the reporting of results to primary care physicians and patients.
Strengths of the study include a large sample size and comparison of the intervention with a control group over an extended period of time. It is the first study reporting the eight-year impact of patient navigation on the degree of cervical abnormalities. Data was collected using an electronic medical record system, thereby minimizing the risk of bias created by self-reporting of colposcopy clinic attendance.
Important limitations of this study deserve comment. The findings of the study are attenuated by its retrospective design. The navigation results come from a single urban community health center affiliated with an academic medical center and may not be generalizable to other clinical settings. Because Chelsea has unique demographic characteristics within the state of Massachusetts,24 finding a suitable comparison group was challenging. As shown in the results, the MGH Chelsea study participants were different from the comparison group with respect to several important sociodemographic characteristics: the Chelsea subjects had a lower education level, a lower rate of commercial insurance, and different spectrum of countries of origin when compared to the non-navigated subjects. These differences would bias our results toward the null hypothesis, and findings may therefore underestimate the degree to which the navigator program improved follow-up. In addition, an immigrant Latina patient navigator with linguistic expertise (certified medical interpreter) living in the same community as the Latina patients, was able to effectively bridge cultural barriers between the healthcare system and the study patients. However, the methods used do not enable us to determine which specific aspects of the patient navigator program had the greatest positive impact.
Conclusion
The findings of this study support the benefit of patient navigation programs for preventing cervical cancer, specifically by assuring follow-up after an abnormal Pap smear for vulnerable populations, with the goal of reducing disparities in cancer incidence and mortality. A prospective, randomized trial of early versus delayed navigation would further strengthen the evidence of benefits of patient navigation for cervical cancer prevention in Latina women.
Acknowledgments
The authors would like to thank Diana Maldonado the cervical patient navigator and her supervisor Denise Sidorowicz, NP, for their work on the program. The authors are grateful to Steven Atlas, MD, MPH, for support and review of the manuscript. The study was funded by a grant from Proctor and Gamble to the MGH Chelsea Cervical Outreach Program. Dr. Percac-Lima was supported in part by a grant from the Agency for Healthcare Research and Quality (1R18 HS019161-01). It was presented at the New England Meeting of the Society of General Medicine in Portland, Maine on March 23, 2012 and at the Annual Meeting of the Society of General Medicine in Orlando, Florida on May 9, 2012.
Disclosure Statement
No competing financial interests exist.
References
- 1.Michalas SP. The Pap test: George N. Papanicolaou (1883–1962). A screening test for the prevention of cancer of uterine cervix. Eur J Obstet Gynecol Reprod Biol. 2000;90:135–138. doi: 10.1016/s0301-2115(00)00260-8. [DOI] [PubMed] [Google Scholar]
- 2.Downs LS. Smith JS. Scarinci I. Flowers L. Parham G. The disparity of cervical cancer in diverse populations. Gynecol Oncol. 2008;109(Suppl 2):22–30. doi: 10.1016/j.ygyno.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 3.Siegel R. Naishadham D. Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 4.Surveillance Epidemiology and End Results. Bethesda, MD: National Cancer Institute; 2012. [Jul 20;2012 ]. SEER stat fact sheets: Cancer of the cervix uteri. [Google Scholar]
- 5.Percac-Lima S. Aldrich LS. Gamba GB. Bearse AM. Atlas SJ. Barriers to follow-up of an abnormal Pap smear in Latina women referred for colposcopy. J Gen Inten Med. 2010;25:1198–1204. doi: 10.1007/s11606-010-1450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khanna N. Phillips MD. Adherence to care plan in women with abnormal Papanicolaou smears: A review of barriers and interventions. J Am Board Fam Pract. 2001;14:123–130. [PubMed] [Google Scholar]
- 7.Byrd TL. Chavez R. Wilson KM. Barriers and facilitators of cervical cancer screening among Hispanic women. Ethn Dis. 2007;17:129–134. [PubMed] [Google Scholar]
- 8.del Carmen MG. Findley M. Muzikansky A, et al. Demographic, risk factor, and knowledge differences between Latinas and non-Latinas referred to colposcopy. Gynecol Oncol. 2007;104:70–76. doi: 10.1016/j.ygyno.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Reynolds D. Cervical cancer in Hispanic/Latino women. Clin J Oncol Nurs. 2004;8:146–150. doi: 10.1188/04.CJON.146-150. [DOI] [PubMed] [Google Scholar]
- 10.National Cancer Institute. Bethesda, MD: National Institutes of Health; 2012. [Dec 1;2012 ]. Cancer trends progress report: 2011/2012 update. [Google Scholar]
- 11.Ramirez RR. de la Cruz GP. Washington, DC: U.S. Census Bureau; 2002. [Jul 20;2012 ]. Annual demographic supplement to the March 2002 current population survey from the U.S. Census Bureau. [Google Scholar]
- 12.Kaplan CP. Bastani R. Belin TR. Marcus A. Nasseri K. Hu MY. Improving follow-up after an abnormal pap smear: results from a quasi-experimental intervention study. J Women's Health Gend Based Med. 2000;9:779–790. doi: 10.1089/15246090050147754. [DOI] [PubMed] [Google Scholar]
- 13.Freeman HP. Muth BJ. Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3:19–30. [PubMed] [Google Scholar]
- 14.Freeman HP. Rodriguez RL. History and principles of patient navigation. Cancer. 2011;117(Suppl 15):3539–3542. doi: 10.1002/cncr.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Battaglia TA. Roloff K. Posner MA. Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(Suppl 2):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 16.Wells KJ. Battaglia TA. Dudley DJ, et al. Patient navigation: State of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ell K. Vourlekis B. Xie B, et al. Cancer treatment adherence among low-income women with breast or gynecologic cancer: A randomized controlled trial of patient navigation. Cancer. 2009;115:4606–4615. doi: 10.1002/cncr.24500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paskett ED. Harrop JP. Wells KJ. Patient navigation: An update on the state of the science. CA Cancer J Clin. 2011;61:237–249. doi: 10.3322/caac.20111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phillips CE. Rothstein JD. Beaver K. Sherman BJ. Freund KM. Battaglia TA. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med. 2011;26:123–129. doi: 10.1007/s11606-010-1527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clark CR. Baril N. Hall A, et al. Case management intervention in cervical cancer prevention: The Boston REACH coalition women's health demonstration project. Prog Community Health Partnersh. 2011;5:235–247. doi: 10.1353/cpr.2011.0034. [DOI] [PubMed] [Google Scholar]
- 21.Wang X. Fang C. Tan Y. Liu A. Ma GX. Evidence-based intervention to reduce access barriers to cervical cancer screening among underserved Chinese American women. J Womens Health. 2010;19:463–469. doi: 10.1089/jwh.2009.1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lerman C. Hanjani P. Caputo C, et al. Telephone counseling improves adherence to colposcopy among lower-income minority women. J Clin Oncol. 1992;10:330–333. doi: 10.1200/JCO.1992.10.2.330. [DOI] [PubMed] [Google Scholar]
- 23.Stewart DE. Buchegger PM. Lickrish GM. Sierra S. The effect of educational brochures on follow-up compliance in women with abnormal Papanicolaou smears. Obstet Gynecol. 1994;83:583–585. doi: 10.1097/00006250-199404000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Ell K. Vourlekis B. Muderspach L, et al. Abnormal cervical screen follow-up among low-income Latinas: Project SAFe. J Womens Health Gend Based Med. 2002;11:639–651. doi: 10.1089/152460902760360586. [DOI] [PubMed] [Google Scholar]
- 25.U.S. Census Bureau. Washington, DC: U.S. Census Bureau; 2010. [Jul 20;2012 ]. Chelsea (city) QuickFacts from the U.S. Census Bureau. State and county quick facts. [Google Scholar]
- 26.U.S. Census Bureau. Washington, DC: U.S. Census Bureau; 2010. [Jul 20;2012 ]. 2006–2010 American community survey from the U.S. Census Bureau. [Google Scholar]
- 27.Boston, MA: Massachusetts Department of Public Health; MassCHIP Bureau of Health Statistics and Research, Evaluation, Massachusetts Cancer Registry. 2003–2007 Incidence. [Google Scholar]
- 28.Boston, MA: Massachusetts Department of Public Health; MassCHIP, Bureau of Health Statistics, Research and Evaluation, Registry of Vital Records and Statistics. 2006–2008 Mortality. [Google Scholar]
- 29.Solomon D. Davey D. Kurman R, et al. The 2001 Bethesda system: Terminology for reporting results of cervical cytology. JAMA. 2002;287:2114–2119. doi: 10.1001/jama.287.16.2114. [DOI] [PubMed] [Google Scholar]
- 30.Peterson NB. Han J. Freund KM. Inadequate follow-up for abnormal Pap smears in an urban population. J Natl Med Assoc. 2003;95:825–832. [PMC free article] [PubMed] [Google Scholar]
- 31.Marcus AC. Crane LA. Kaplan CP, et al. Improving adherence to screening follow-up among women with abnormal Pap smears: Results from a large clinic-based trial of three intervention strategies. Med Care. 1992;30:216–230. doi: 10.1097/00005650-199203000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Eggleston KS. Coker AL. Das IP. Cordray ST. Luchok KJ. Understanding barriers for adherence to follow-up care for abnormal pap tests. J Womens Health. 2007;16:311–330. doi: 10.1089/jwh.2006.0161. [DOI] [PubMed] [Google Scholar]
- 33.Engelstad LP. Stewart S. Otero-Sabogal R. Leung MS. Davis PI. Pasick RJ. The effectiveness of a community outreach intervention to improve follow-up among underserved women at highest risk for cervical cancer. Prev Med. 2005;41:741–748. doi: 10.1016/j.ypmed.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 34.Cardin VA. Grimes RM. Jiang ZD. Pomeroy N. Harrell L. Cano P. Low-income minority women at risk for cervical cancer: A process to improve adherence to follow-up recommendations. Public Health Rep. 2001;116:608–616. doi: 10.1093/phr/116.6.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fox P. Amsberger P. Zhang X. An examination of differential follow-up rates in cervical cancer screening. J Community Health. 1997;22:199–209. doi: 10.1023/a:1025125124926. [DOI] [PubMed] [Google Scholar]
- 36.McKee MD. Schechter C. Burton W. Mulvihill M. Predictors of follow-up of atypical and ASCUS papanicolaou tests in a high-risk population. J Fam Pract. 2001;50:609. [PubMed] [Google Scholar]
- 37.Siegel R. Naishadham D. Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin. 2012;62:283–98. doi: 10.3322/caac.21153. [DOI] [PubMed] [Google Scholar]
- 38.Saslow D. Solomon D. Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Surgical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62:147–172. doi: 10.3322/caac.21139. [DOI] [PMC free article] [PubMed] [Google Scholar]