Abstract
Background
Scant literature exists on STD risk specific to pregnancy and postpartum. The objective of this prospective study is to examine risk factors for incident postpartum sexually transmitted diseases (STDs) among young mothers (ages 14–25).
Methods
Pregnant women were enrolled at <24 weeks gestation (N=848). Data were collected via in-depth interviews and STD testing conducted in the second and third trimesters and at 6 and 12 months postpartum. Prevalence and incidence of STD diagnosis in pregnancy and postpartum is described. Logistic and linear regression are used to identify risk factors for postpartum infection.
Results
Forty-four percent of enrolled women never had an STD, 29% had a history of an STD prior to pregnancy, 28% got an STD during pregnancy, and 27% were diagnosed with an STD postpartum. Incidence of postpartum infection was higher for women who contracted an STD in pregnancy (43%) compared to those with a prior STD (24%) or no STD (19%). In multivariate analysis, STD in pregnancy, having less than high school education, having a new sexual partner and Black race were risk factors for incident postpartum STD.
Conclusion
Prenatal providers should be aware of the significant risk of incident infection among women diagnosed with STDs in pregnancy. Elevated postpartum incidence among those with an STD in pregnancy supports a shift towards more frequent and targeted postpartum STD screening, with implications for clinical care, future research and interventions.
Introduction
The scope and effects of sexually transmitted diseases (STDs) among reproductive-age women have substantial public health and clinical significance, including infertility, chronic pain, pelvic inflammatory disease, and increased risk for human immunodeficiency virus (HIV) acquisition (1). Young women are at elevated risk of developing STDs secondary to risky sexual behaviors (2, 3, 4). Women aged 15–24 years have the highest rates of STDs in the United States, with recent data showing rates 2–5 times higher than among the general population (3915.6 and 1513.2 per 100,000 population among females aged 15–19 years and 20–24 years, respectively) (1).
Young mothers represent a sub-population of women who are at additional risk for contracting STDs. Up to 39% of postpartum teens report an incident STD in the year following delivery, compared with annual rates of approximately 10% among non-pregnant adolescents (2, 5). Scant literature exists on STD risk specific to pregnancy and the postpartum period, and new mothers are at increased risk for contracting STDs for potentially different reasons from their non-pregnant peers (3, 6). Women who are pregnant or have recently given birth do not use condoms as consistently as non-pregnant women, with only 22% of adolescent mothers reporting condom use one year postpartum (7, 8, 9). Overall, pregnant women are five times less likely to use condoms than non-pregnant women (3). Young single women often have multiple new partners throughout pregnancy and the first year postpartum, as well as high rates of infidelity and dissolution of relationships (10). Additionally, these women experience emotional, economic and physical stress, often translating into increased rates of depression, alcohol and drug use and domestic violence, while simultaneously reducing self-efficacy and self-advocacy behaviors (4). Pregnant and postpartum women are also biologically more vulnerable given histological and cervical changes associated with pregnancy (11).
The existing literature on STD risk factors among young women has identified factors that are considered hallmarks of STD risk: young age, Black race, poverty, low levels of education, drug and alcohol use, short duration of the current relationship, interpersonal violence, poor knowledge of and commitment to condom use, low self-esteem, and depression (4, 6, 12–17). Because women are exposed to healthcare providers an average of 12 times throughout the course of prenatal care, regular communication represents a rare opportunity for education and skills building regarding STD prevention during and after pregnancy. Pregnancy is a “window of opportunity” for effective messaging regarding STD prevention at a rare time when women are regularly receiving medical care and more likely to take steps to preserve their health and well-being (2, 7). However, no studies have been conducted to determine whether the timing of previous STD infection relates to rates of incident cases in the postpartum period. The purpose of this paper is to examine whether occurrence and timing of STDs predict postpartum infection. Results may have implications for specific clinical recommendations for screening high-risk women and targeting both prenatal and postpartum interventions.
Materials and Methods
Study Participants
The data utilized in these analyses were collected as part of a larger study that examined the effects of group prenatal care of pregnancy outcomes and sexual risk from September 2001 to December 2004 (2, 18). Inclusion criteria for participation comprised women who were: (1) pregnant at <24 weeks gestational age, (2) aged 14–25 years, (3) free of severe medical problems, and (4) fluent in English or Spanish (2). Overall, 1538 women were eligible for the study and 1047 (68%) enrolled. For these analyses, all women for whom STD diagnosis data were available both during pregnancy and postpartum were included: 848 women (81% of original sample of 1047). Participants ranged in age from 14–25 years (M=19.75, SD=2.1). Seventy-seven percent of participants were Black, 14% Hispanic, 7% White, and 2% mixed or other race/ethnicity (2). Fifty-one percent had achieved a high-school level education. Sixty five percent were nulliparous.
Procedures
Baseline interviews were conducted by trained research assistants early in the second trimester, (mean=18 weeks gestation; SD=3.3). Participants completed follow-up interviews late in the third trimester (mean=35 weeks gestation; SD=3.1), at 6 months postpartum (mean=27 weeks postpartum; SD=4.5), and 12 months postpartum (mean=53 weeks postpartum; SD=5.7). Researchers assessed bacterial STD acquisition (Chlamydia and Gonorrhea) during pregnancy and the postpartum period with nucleic acid amplification tests (ligase chain reaction or strand displacement amplification; BD Diagnostic Systems, Sparks, MD).
Anyone diagnosed with an infection was referred back to their clinical sites where participants were informed of their results and treated, as per clinical protocols. Study staff followed up with a Clinic Liaison to ensure that all positive participants were treated. If a participant had yet to be treated or could not be located, study staff worked with clinic outreach workers to locate participants and get them in for treatment. This procedure led to 100% treatment rate for all STD positive participants. Clinic protocols did not require partner tests. However, partners were referred to the appropriate provider for testing and treatment (e.g., primary provider, primary care clinic, or STD clinic). Procedures were approved by human investigation committees at Yale and Emory Universities and at the study clinics.
Outcome Measures
Incident STDs
Participants were categorized as having a postpartum incident STD or having no postpartum incident STD. Postpartum incident STD was based on results of lab tests (Chlamydia and Gonorrhea) and self-report (Chlamydia, Gonorrhea, syphilis, trichomonas, genital herpes, and genital warts or HPV). Those who tested positive for Chlamydia or Gonorrhea at any point postpartum were categorized as having a postpartum STD. Patient self-report were used to supplement biological screening to reduce potential error regarding diagnoses that may have been treated during the postpartum period (19). Of the total incident STDs reported, 53.3% were Chlamydia, 12.8% were Gonorrhea, 0.3% were syphilis, 19.8% were trichomonas, 7.8% were genital herpes, and 5.8% were genital warts or HPV. Given that participants were treated for STDs during pregnancy, incident STDs reflect a new STD, new incidence from an untreated partner, or treatment failure.
STD History
Participants were categorized into one of three groups based on STD history: no STD history; STD prior to pregnancy; and incident STD in pregnancy. STD history was based on results of lab tests (Chlamydia and Gonorrhea) and self-report (Chlamydia, Gonorrhea, trichomonas, genital warts or HPV, genital herpes, or syphilis,). If an individual tested positive for Chlamydia or Gonorrhea in the second or third trimester, then they were categorized as having an STD during pregnancy. Furthermore, participants were asked at enrollment and each time point if they had been diagnosed with an STD and the approximate date of that diagnosis (19). For those with any reported STD diagnosis, dating was used to classify infection as prior to or during pregnancy. Of the total prior STDs reported, 51.2% were Chlamydia, 12.7% were Gonorrhea, 23.3% were trichomonas,7.5% were genital warts or HPV, 4.6% were genital herpes, and 0.7% were syphilis.
Established Risk Factors
Variables included in these analyses were selected based on established STD risk factors.
Sociodemographic Risk Factors
Race was measured by a categorical variable (Non-Hispanic Black, Hispanic, Non-Hispanic White and Other). Age was extracted into a dichotomous variable, mirroring the CDC categories for age of STD acquisition (1). A socioeconomic status variable was created to capture whether individuals live above or below the Federal Poverty Level, using the established cut-point of the rate for a family of 4: $21,225. Education was categorized by whether or not women had attained high school equivalency.
Behavioral Risk Factors
Condom communication was measured as an aggregate of several questions related to condom use communication and negotiation (2). Responses were coded into a binary variable which separated consistent positive responses from inconsistent or negative reports (20). Drug and alcohol use were measured as an aggregate of responses on questions that related to frequency and type of substances used during pregnancy. A binary variable was created for alcohol use alone and another for a composite of illicit drug and marijuana use, separating no from any use.
Interpersonal Risk Factors
Interpersonal violence was measured using three questions pertaining to whether or not women had been the victim of abuse by their partner(s) since their pregnancy began, using a questionnaire adapted from the Conflict Tactics Scale (21). Questions were asked at all interview points and a binary variable was created reflecting the presence or absence of interpersonal violence during the study period. Age difference between partners was measured using data on participant and partner ages at enrollment, with a 2-year age difference cut-off used because of evidence linking this to high-risk behavior (10). Women were asked at each interview whether they were in a relationship and the duration of that current relationship. These data were used to build variables measuring the duration of current relationship at postpartum follow-up.
Psychosocial Risk Factors
Self-esteem was measured using the 10-item Rosenberg scale, with responses on a four-point Likert scale (22). A cut-point was set at the median score of 34, with “high” versus “low” self-esteem capturing individual scores above or below the median. Depression was measured at 6 months postpartum using 15 of the 20 CES-D scale items (affect only, eliminating somatic symptoms associated with both depression and pregnancy), with a total score ranging from 0 to 45 (23). A score of >=16 indicates high levels of depressive symptoms (24).
Data Analytic Plan
To meet the aim of measuring STD incidence and illustrating the association between timing of previous STD and incident postpartum infection, initial analyses examined rates of postpartum STD by prior infection status: no previous STD, history of STD prior to pregnancy, and first STD in pregnancy. It was then possible to compare frequency and incidence of postpartum STD in each group. To examine the association between postpartum STDs and established risk factors, the next step was to conduct independent bivariate analyses of each variable and incident postpartum STD. To determine whether previous STD status was an independent risk factor for incident postpartum STD infection, multivariate analysis was conducted, including all variables statistically significant in bivariate analysis (p<0.05). All analyses controlled for intervention group as randomized in the parent study.
Results
STD History
The first aim was to determine whether rates of incident postpartum STDs vary among those with a history of infection, those who contracted an STD in pregnancy and those with no prior STD. At baseline, 43.5% of participants had never had an STD, while 29% of participants had a history of an STD prior to pregnancy, and 27.5% contracted their first STD in pregnancy. A total of 27.1% were diagnosed with an STD in the first 12 months postpartum. Most strikingly, 43.4% of women who were diagnosed with an STD in pregnancy also had an incident STD postpartum. Meanwhile, those who had a history of STDs pre-pregnancy or who never had an STD had postpartum rates of only 24.0% and 18.7%, respectively. Bivariate analyses showed that contracting an STD in pregnancy was associated with nearly three times the likelihood of developing an STD postpartum compared to women who did not have an STD in pregnancy (OR=2.91, 95% CI=2.11–4.03, p<.001) (Table 1).
Table 1.
Results of bivariate and multivariate analysis predicting incident STD infection within one year postpartum
| Variable | n (%) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|
| Sexually Transmitted Disease (STD) History | |||
| No history of STD | 369 (43.5%) | Referent | - |
| STD prior to pregnancy | 246 (29.0) | 0.81 (0.57–1.13) | 1.16 (0.76–1.78) |
| STD in pregnancy | 233 (27.5%) | 2.91 (2.11–4.03)** | 2.51 (1.69–3.73)** |
| African American race | 656 (77.4%) | 3.36 (2.11–5.36)** | 2.69 (1.62–4.46)** |
| Age <20 years old | 284 (33.5%) | 0.61 (0.45–0.84)** | 0.85 (0.58–1.25) |
| Living below the federal poverty level | 145 (17.1%) | 0.97 (0.65–1.44) | - |
| High-school graduate | 428 (50.5%) | 0.53 (0.39–0.72)** | 0.59 (0.41–0.86)** |
| High condom communication rating | 71 (8.4%) | 1.34 (0.76–2.35) | - |
| Drug use | 121 (14.3%) | 1.60 (1.07–2.41)* | 1.14 (0.73–1.79) |
| Alcohol use | 273 (32.2%) | 1.21 (0.86–1.69) | - |
| Interpersonal violence | 70 (8.3%) | 0.79 (0.44–1.40) | - |
| Age difference between partners of >2 years | 120 (14.2%) | 1.89 (0.79–1.82) | - |
| Relationship duration <6 mos at start of pregnancy | 646 (76.2%) | 0.60 (0.43–0.84)** | 0.92 (0.60–1.40) |
| Relationship duration <6 mos in 3rd trimester | 634 (74.8%) | 0.52 (0.37–0.72)** | 0.72 (0.47–1.09) |
| Relationship duration <6 mos at postpartum follow-up | 531 (62.6%) | 0.46 (0.34–0.62)** | 0.59 (0.42–0.85)** |
| Low self-esteem | 373 (44.0%) | 0.84 (0.62–1.15) | - |
| Depression | 173 (20.4%) | 1.59 (1.11–2.28)** | 1.41 (0.95–2.10) |
p<0.05
p<0.01
Risk Factors for Incident Postpartum STD
The second aim was to identity risk factors independently associated with incident postpartum infection (Table 1). In bivariate analyses, having an STD during pregnancy as well as Black race, age lower than 20 years, less than high school education, illicit drug use, and shorter relationship duration were associated with increased risk of incident postpartum STD (all p<0.05). In the multivariate model, women who contracted an STD in pregnancy were 2.51 times more likely to be diagnosed postpartum (OR=2.51, 95% CI=1.62–4.46, p<.001). Being Black was associated with over twice the likelihood of developing an infection postpartum (OR=2.69, 95% CI=1.62–4.46, p<.001). Having graduated high school was protective against postpartum STD infection with high school graduates approximately 40% less likely to develop an STD postpartum than non-high school graduates (OR=0.59, 95% CI=0.41–0.86, p=.006). Having a relationship of more than six months duration at postpartum follow-up was protective against STD infection during that period, with only 7.7% of women with a longer relationship developing a postpartum STD. Such women were nearly half likely to develop an STD postpartum than their counterparts in new relationships (OR=0.59, 95% CI=0.42–0.85, p=0.004). No other sociodemographic, behavioral, interpersonal, or social risk factors that we examined were significantly associated with incident postpartum STD (all p>0.05) (Table 1).
Discussion
Occurrence and timing of STD was a significant predictor of incident postpartum infection. STD infection in pregnancy was associated with increased incidence of postpartum STD, even after controlling for other established risk factors. Of those who contracted an STD in pregnancy, 43% also contracted an STD in the first year postpartum. History of STDs prior to pregnancy, meanwhile, was not linked to postpartum infection, implying the need for a paradigm shift that takes into account the timing of previous STD, rather than occurrence alone, when considering risk of postpartum STD. Short relationship duration, less than high school educational attainment, and Black race were also associated with higher incidence of postpartum STDs. In combination with STD infection in pregnancy, these risk factors could form a new classification of women at highest risk for STDs in the first year postpartum.
These results have implications for clinical care during pregnancy and in the postpartum period. Currently, nearly 95% of women in the United States receive prenatal care, but as many as 46% of women do not receive postpartum care and only 21% receive routine annual STD screening (25). These results indicate that women diagnosed with STDs in pregnancy are not receiving effective education and prevention messages, despite having regular exposure to health care providers throughout pregnancy and a potential opportunity for effective behavioral change is being squandered. Furthermore, women receive routine STD screening only once in the perinatal period – upon entry into prenatal care – but are not routinely tested in the postpartum period (25). These results suggest that women who are diagnosed with an STD during pregnancy may be particularly vulnerable to acquiring an STD postpartum. Therefore, it may be important to routinely test these women during the postpartum period to identify and treat incident STDs. Prenatal counseling should also be intensified and include reminders about safer sex postpartum while stressing the importance to condom use with new partners. Among patients with STDs during pregnancy, providers should be encouraged to engage in more meaningful dialogue and skills building to enhance reproductive health across the perinatal and postnatal periods (26).
This study has limitations that should be noted. The sample represents a group of predominantly ethnic minority women of relatively low socioeconomic status who attend urban clinics for prenatal care. To test the generalizability of these results, it is necessary to analyze data from more diverse patient populations. Additionally, several variables were dichotomized into binary categories, leaving the results at risk for misclassification bias secondary to under- or over-reporting. Furthermore, although all participants were treated for STDs during pregnancy, tests of cure were not performed because they were not mandated by clinical protocols. However, recent studies have demonstrated high cure rates for the treatments employed at the clinics [e.g., 97% for azithromycin to treat Chlamydia (27), 98.8% for Ceftriaxone to treat Gonorrhea (28)]. Therefore, cure rates among participants were likely high. Future work should include tests of cure to better approximate the extent to which postpartum STDs are due to treatment failures. Finally, although partner referrals were made for testing and treatment, partner testing and treatment were not mandated by clinic protocols and no assessments of these behaviors were obtained. Future work should measure partner testing and treatment to better approximate the extent to which postpartum STDs are due to reinfection from partners. Further, the Centers for Disease Control and Prevention report that partner services continue to be underused (29). It may be necessary to re-evaluate these clinical practices, especially in prenatal care settings, to increase the likelihood of partner testing and treatment.
Despite these limitations, there are several strengths. This study includes a large cohort of high risk young women. It replicates past findings identifying Black race, lower education, and short relationship duration as key factors related to STD risk. It further extends work on risk factors as the first study to examine how timing and occurrence of previous infection relate to rates of postpartum STDs among pregnant young women. It demonstrated that STD infection during pregnancy was associated with STD infection postpartum even after controlling for these well-established risk factors. Consequently, this work highlights women who have contracted an STD during pregnancy as a high-risk group for STD infection postpartum. This study therefore has potential impact on the design and delivery of prenatal and postpartum care.
More research is needed focusing specifically on women who contract STDs postpartum, examining their behaviors and motivations related to sexual risk behavior. The high incidence of postpartum STDs may be related to decreased worry about becoming pregnant, lack of information about risk factors, or any number of other factors. Furthermore, a qualitative assessment of the relationship between postpartum STDs and different partner types (i.e. father of baby versus new boyfriend) could promote a deeper understanding of risk. Interventions targeted at true barriers to safe sexual behaviors specific to the postpartum period have the greatest promise to reduce incident postpartum STDs.
Figure 1.
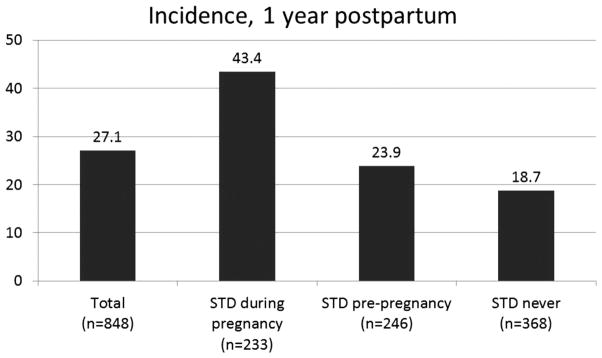
Rates of STD by History and Timing of Infection
Summary.
Young women diagnosed with STDs during pregnancy had dramatically high recurrence in the first year postpartum. Elevated postpartum incidence supports a shift towards more frequent and targeted postpartum STD screening.
Acknowledgments
Support. Primary support for this study came from the National Institute of Mental Health, (R01MH/HD61175, Ickovics PI). Additional support came from National Institute of Mental Health research grant (R01-MH074399) and training grant (T32-MH20031).
Footnotes
Conflict of Interest: The authors do not have any known conflicts of interest.
References
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2008. Atlanta, Georgia: US Dept of Health and Human Services; 2009. [Google Scholar]
- 2.Kershaw TS, Magriples U, Westdahl C, et al. Pregnancy as a window of opportunity for HIV prevention: Effects of an HIV intervention delivered within prenatal care. Am J Public Health. 2009;99(11):2079–2086. doi: 10.2105/AJPH.2008.154476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niccolai LM, Hochberg AL, Ethier K, et al. Burden of recurrent Chlamydia Trachomatis infections in young women: Further uncovering the “Hidden Epidemic”. Arch Pediatr Adolesc Med. 2007;161:246–251. doi: 10.1001/archpedi.161.3.246. [DOI] [PubMed] [Google Scholar]
- 4.Rosenberg MD, Gurvey JE, Adler N, et al. Concurrent sex partners and risk for sexually transmitted diseases among adolescents. Sex Transm Dis. 1999;26:208–212. doi: 10.1097/00007435-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Hobfoll SE, Jackson AP, Lavin J, et al. Reducing inner-city women’s AIDS risk activities: a study of single, pregnant women. Health Psychol. 1994;13:397–403. doi: 10.1037//0278-6133.13.5.397. [DOI] [PubMed] [Google Scholar]
- 6.Critchlow CW, Wolner-Hanssen P, Eschenbach DA, et al. Determinants of cervical ectopia and of cervicitis: age, oral contraception, specific cervical infection, smoking, and douching. Am J Obstet Gynecol. 1995;173:534–543. doi: 10.1016/0002-9378(95)90279-1. [DOI] [PubMed] [Google Scholar]
- 7.Ickovics JR, Niccolai LM, Lewis JB, et al. High postpartum rates of sexually transmitted infections among teens: pregnancy as a window of opportunity for prevention. Sex Transm Infect. 2003;79:469–473. doi: 10.1136/sti.79.6.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kershaw TS, Niccolai LM, Ickovics JR, et al. Short and long-term impact of adolescent pregnancy on postpartum contraceptive use: implications for prevention of repeat pregnancy. J Adolescent Health. 2003;33(5):359–368. doi: 10.1016/s1054-139x(03)00138-1. [DOI] [PubMed] [Google Scholar]
- 9.Kershaw TS, Niccolai LM, Ethier KA, et al. Perceived susceptibility to pregnancy and sexually transmitted disease among pregnant and non-pregnant adolescents. J Community Psychol. 2003;31:419–434. [Google Scholar]
- 10.Katz KS, Blake SM, Milligan RA, et al. The design, implementation and acceptability of an integrated intervention to address multiple behavioral and psychosocial risk factors among pregnant African American women. BMC Pregnancy Childbirth. 2008;8(22):25–47. doi: 10.1186/1471-2393-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reece EA, Hobbins JC, Grant NF, editors. Handbook of Clinical Obstetrics: The Fetus and Mother. 2. Hoboken NJ: Wiley-Blackwell; 2007. [Google Scholar]
- 12.Baker JG, Rosenthal SL. Psychological aspects of sexually transmitted infection acquisition in adolescent girls: a developmental perspective. J Dev Behav Pediatr. 1998;19:202–208. doi: 10.1097/00004703-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Santelli JS, Kouzis AC, Hoover DR, et al. Stage of behavior change for condom use: The influence of partner type, relationship and pregnancy factors. Fam Plann Perspect. 1996;28:101–107. [PubMed] [Google Scholar]
- 14.Paul KJ, Garcia PJ, Giesel AE, et al. Generation C: Prevalence of and risk factors for Chlamydia Trachomatis among adolescents and young women in Lima, Peru. J Midwifery Wom Heal. 2009;18:1419–1424. doi: 10.1089/jwh.2008.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deardorff J, Tschann JM, Flores E. Sexual values among Latino youth: measurement development using a culturally based approach. Cultur Divers Ethnic Minor Psychol. 2008;14(2):138–146. doi: 10.1037/1099-9809.14.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dolcini MM, Adler NE. Perceived competencies, peer group affiliation, and risk behavior among early adolescents. Health Psychol. 1994;13(6):496–506. doi: 10.1037//0278-6133.13.6.496. [DOI] [PubMed] [Google Scholar]
- 17.Ketterlinus RD, Lamb ME, Nitz KA. Adolescent nonsexual and sex-related problem behaviors: Their prevalence, consequences, and co-occurrence. In: Ketterlinus RD, Lamb ME, editors. Adolescent problem behaviors: Issues and research. Hillsdale, New Jersey: Erlbaum; 1994. pp. 17–39. [Google Scholar]
- 18.Ickovics JR, Kershaw TS, Westdalt C, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol. 2007;110(2):330–339. doi: 10.1097/01.AOG.0000275284.24298.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niccolai LM, Kershaw TS, Lewis JB, Cicchetti DV, Ethier KA, Ickovics JR. Data collection for sexually transmitted disease diagnoses: A comparison of self-report, medical record reviews, and state health department reports. Annals of Epidemiology. 2005;15:236–242. doi: 10.1016/j.annepidem.2004.07.093. [DOI] [PubMed] [Google Scholar]
- 20.Sikkema KJ, Heckman TG, Kelly JA, et al. HIV risk behaviors among women living in low-income, inner-city housing developments. Am J Public Health. 1996;86:1123–1128. doi: 10.2105/ajph.86.8_pt_1.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Straus MA. Measuring intra family conflict and violence: The Conflict Tactics Scale. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- 22.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 23.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1997;1:385–401. [Google Scholar]
- 24.Reardon DC, Cougle JR. Depression and unintended pregnancy in young women. Brit Med J. 2002;324:1097. [Google Scholar]
- 25.American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetricians and Gynecologists. 2009;114(6):1409–1420. [Google Scholar]
- 26.Centers for Disease Control and Prevention. STD’s and Pregnancy. 2011 Jul; http://www.cdc.gov/std/pregnancy/STDfact-Pregnancy.htm.
- 27.Lau C, Quershi AK. Azithromycin versus doxycycline for genital chlamydial infections. Sex Transm Dis. 2002;29(9):497–502. doi: 10.1097/00007435-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Moran JS, Handsfield HH. Neisseria gonorrhoeae. In: Yu VL, Weber R, Raoult D, editors. Antimicrobial therapy and vaccines. 2. New York: Apple Trees Productions; 2002. pp. 457–469. [Google Scholar]
- 29.Dooley SW. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR. 2008;57(RR09):1–63. [PubMed] [Google Scholar]


