Abstract
Purpose of review
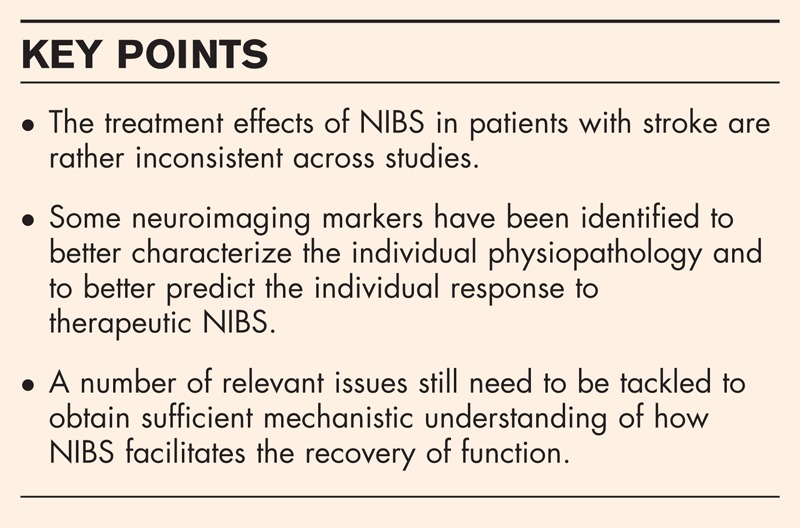
Noninvasive brain stimulation (NIBS) is increasingly used to enhance the recovery of function after stroke. The purpose of this review is to highlight and discuss some unresolved questions that need to be addressed to better understand and exploit the potential of NIBS as a therapeutic tool.
Recent findings
Recent meta-analyses showed that the treatment effects of NIBS in patients with stroke are rather inconsistent across studies and the evidence for therapeutic efficacy is still uncertain. This raises the question of how NIBS can be developed further to improve its therapeutic efficacy.
Summary
This review addressed six questions: How does NIBS facilitate the recovery of function after stroke? Which brain regions should be targeted by NIBS? Is there a particularly effective NIBS modality that should be used? Does the location of the stroke influence the therapeutic response? How often should NIBS be repeated? Is the functional state of the brain during or before NIBS relevant to therapeutic efficacy of NIBS? We argue that these questions need to be tackled to obtain sufficient mechanistic understanding of how NIBS facilitates the recovery of function. This knowledge will be critical to fully unfold the therapeutic effects of NIBS and will pave the way towards adaptive NIBS protocols, in which NIBS is tailored to the individual patient.
Keywords: brain stimulation, motor recovery, motor training
INTRODUCTION
Together with basic research in animal models, functional neuroimaging techniques have significantly advanced the understanding of neuroplastic changes following stroke. The therapeutic use of noninvasive brain stimulation (NIBS) is a prominent example for an interventional procedure that has been motivated by basic research on stroke recovery. Repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS) are the two NIBS techniques that have been predominantly tested in stroke patients. Promising results have been reported with both stimulation modalities [1,2▪], but many questions still remain to be answered. In this review, we raise some open questions regarding the therapeutic application of NIBS in poststroke patients. We focus on the use of NIBS to facilitate motor recovery, but we will also touch on the treatment of aphasia or neglect.
CAN NONINVASIVE BRAIN STIMULATION BE RECOMMENDED AS TREATMENT TO PROMOTE STROKE RECOVERY?
The overall therapeutic efficacy of rTMS in stroke patients was recently evaluated in a Cochrane review based on 19 randomized and controlled trials [3▪▪]. In a population of 73 patients, the Cochrane review found no consistent beneficial effects of ‘real rTMS’ on motor function as measured with three different scales. The authors reviewed two studies regrouping 183 patients investigating the effects of rTMS on the activities of daily living, and report a trend for an improvement after real rTMS. Only limited evidence was found for a beneficial effect of rTMS on aphasia and neglect.
Box 1.
no caption available
A recent meta-analysis focussed on the therapeutic effects of anodal tDCS in stroke including eight randomized placebo-controlled trials [4▪]. According to this meta-analysis, anodal tDCS has a beneficial effect on upper limb motor function in chronic stroke patients with arm paresis [4▪]. However, the small sample size of the published tDCS studies in stroke is a major limitation. Together, these meta-analyses show that the value of NIBS as a therapeutic intervention to promote motor stroke recovery is promising, but still needs to be confirmed in large multicentre trials with an effort of standardization of the measured outcome variables to better understand the effect of NIBS on different components of stroke recovery: from hand functions to more global scales.
HOW DOES NONINVASIVE BRAIN STIMULATION FACILITATE THE RECOVERY OF FUNCTION AFTER STROKE?
Many hypotheses have been proposed in order to explain how NIBS might produce an improvement of function in stroke patients. We will discuss local and more distributed mechanisms of action associated with NIBS effects.
Local effects: altering the functional state of the stimulated cortex
The local aftereffects of NIBS on corticomotor excitability have been extensively studied in healthy individuals. These electrophysiological studies applied single-pulse TMS of the primary motor cortex (M1) before and after NIBS and used the mean amplitude of the motor-evoked potential (MEP) as an index of corticomotor excitability. It was shown that rTMS and tDCS of the M1 can induce a bi-directional shift in corticomotor excitability depending on the stimulation parameters [5]. Here, it is important to recall that the MEP amplitude is determined by cortical and spinal excitability. The few studies that investigated the effects of rTMS or tDCS on spinal cord excitability [6–9] suggest that changes in MEP size after NIBS might at least partially be caused by a change in spinal excitability. At the cellular level, an increasing body of animal studies have consistently demonstrated a multitude of long-term effects of NIBS on gene expression, intrinsic excitability, or synaptic efficacy [5]. Therefore, it has been suggested that the bi-directional effects of NIBS over M1 on corticospinal excitability in humans might reflect long-term potentiation (LTP) and long-term depression (LTD)-like plasticity [5].
The NIBS-induced shifts in regional excitability may contribute to the therapeutic effects of NIBS in motor stroke. In healthy individuals, a slight shift in excitability might not or only moderately impact on the neural computations in the stimulated cortex. This may be different in the pathological conditions. In motor stroke, a NIBS-induced increase in corticospinal excitability might improve motor function by facilitating the volitional recruitment of corticomotor output neurons. However, the causal link between a change in excitability and functional improvement requires more detailed studies.
Distributed effects: remodelling functional network architecture
An alternative hypothesis is that NIBS induces beneficial effects by modifying the distributed activity and connectivity in functional brain systems. A popular assumption is that in motor stroke, NIBS of M1 can re-establish a functional balance between the damaged and undamaged hemisphere. The underlying hypothesis is that an abnormal increase in interhemispheric inhibition from the contralesional to the ipsilesional hemisphere contributes to motor impairment [10–12]. A functional dysbalance between homologous regions in the right and left hemisphere is also thought to contribute to poststroke aphasia, in which the temporal or frontal over-excitability in the nondamaged hemisphere is suppressed to improve naming (e.g. [13,14]) and spatial neglect [15]. The ‘interhemispheric dysbalance model’ predicts that suppressing cortical over-excitability in the contralesional hemisphere or boosting cortical excitability in the ipsilesional hemisphere will ‘release’ the ipsilesional cortex from excessive interhemispheric inhibition. This, in turn, will allow for a more effective neural processing in the lesional hemisphere and facilitate the recovery of function.
When NIBS of M1 is used to re-balance the interactions between the damaged and nondamaged hemisphere, two issues are worth considering. First, the recent studies, in which the distribution of the electrical field induced by rTMS or tDCS was modelled, raised the possibility that NIBS targeting M1 might induce effective neurostimulation in the adjacent premotor cortex as well (e.g. [16,17]). Thus, ‘focal’ NIBS over M1 might induce its effects at least partially via premotor-to-M1 connections. Second, according to the interhemispheric dysbalance model, NIBS protocols that decrease excitability in the damaged hemisphere or increase excitability in the unaffected hemisphere should have transient detrimental effects on motor function. This prediction remains to be explicitly tested in order to substantiate the validity of the interhemispheric dysbalance model.
As NIBS can induce lasting effects on the distributed activity and effective connectivity in functional brain networks [18▪], NIBS may produce its therapeutic effects by tuning the efficacy of intrahemispherical and interhemispherical interactions [19]. These lasting effects of NIBS on the distributed activity and connectivity can be captured by noninvasive brain imaging methods such as functional magnetic resonance imaging (fMRI) or electroencephalography [20,21]. Indeed, brain-imaging studies confirmed that efficient NIBS therapies in stroke patients are associated with increased task-related activity in ipsilesional brain areas and decreased activity in contralesional areas [22▪▪,23,24]. Functional brain mapping also revealed NIBS-induced changes in effective connectivity. For instance, Grefkes et al.[25] observed an improvement in the motor function of the paretic hand in motor stroke patients who received ‘inhibitory’ 1-Hz rTMS of the contralesional M1. Dynamic causal modelling of the functional MRI data [26] revealed that the individual improvement in motor function was correlated with the ability of 1-Hz rTMS to reduce effective connectivity from contralesional to ipsilesional M1 [25]. In addition, 1-Hz rTMS of contralesional M1 enhanced endogenous coupling between ipsilesional premotor areas and M1.
Together, these data suggest that the beneficial effects of NIBS involve changes in functional interactions between key network nodes in the ipsilesional and contralesional hemispheres. Interestingly, NIBS might also leave microstructural traces in the stimulated brain networks: a recent diffusion MRI study in patients with poststroke aphasia reported increases in fMRI activation after intermittent theta burst stimulation (iTBS) over the ipsilesional hemisphere [27]. These functional changes were mirrored by an increase in fractional anisotropy in the same area [27].
Bridging the neuronal and network level
A complementary account attributes the therapeutic effects of NIBS to an increase in the noise level in the stimulated neural systems evoking stochastic resonance [28,29]. Stochastic resonance refers to the phenomenon that a small increase in noise improves signal processing in nonlinear systems that deal with small signals (i.e. that work in a context of low signal-to-noise ratio). NIBS-induced stochastic resonance can explain state-dependent effects of NIBS. Stochastic resonance also constitutes an efficient means to influence endogenous neuronal oscillations, which play an essential role for the integration of information on the network level [30]. This is potentially relevant to the therapeutic use of NIBS, as NIBS may alter brain function by biasing endogenous cortical and cortico-subcortical oscillations [31,32].
WHICH BRAIN REGIONS SHOULD BE TARGETED BY NONINVASIVE BRAIN STIMULATION?
Most NIBS studies in stroke have targeted the hand area of M1 to improve motor hand function. NIBS has also been applied to M1 to relieve nonmotor symptoms such as neuropathic poststroke pain [33]. NIBS of nonmotor cortical sites has been used to improve other functions after stroke. For instance, parietal cortex stimulation has been used to treat visuo-spatial neglect [34], stimulation of the temporal regions to treat aphasia [35,36], or stimulation of the prefrontal cortex to treat poststroke depression [37].
To promote the recovery of motor function, NIBS might be used to target other brain regions than M1. Experimental work conducted in healthy individuals showed that NIBS of the dorsal premotor cortex (PMd) can induce bi-directional shifts in ipsilateral corticomotor excitability [38–40] and facilitate motor learning [41,42]. Similarly, it has been shown that NIBS of the cerebellum can influence corticomotor excitability through the cerebello-thalamo-cortical pathways [43], and the potential role of the cerebellar structures in neurorehabilitation was discussed recently [44,45]. Therefore, nonprimary motor cortex regions or the cerebellum might represent alternative targets in motor stroke [46,47]. Of note, the choice of the optimal target area might depend on the stage of recovery. Different neural targets for NIBS might be considered in the acute, subacute, and chronic state after stroke.
Most studies implicitly assume that NIBS should target a single brain area only. Yet, it might be worth considering a multisite NIBS approach in which NIBS is used to stimulate simultaneously or consecutively a set of motor regions, including the M1 or premotor, parietal and cerebellar cortex in the ipsilesional or contralesional hemisphere [48–50]. Such multisite NIBS might be more efficient than single-site NIBS. This hypothesis is at least worth testing. Along the same line, diffuse NIBS using a round transducing coil (for rTMS) or nonfocal arrangements of electrodes (for tDCS) might also be useful in poststroke patients in order to induce more widespread neuromodulation in multiple functional brain areas and systems. Such ‘diffuse’ NIBS protocols have not yet been tested and might be combined with focal or multisite NIBS.
IS THERE A PARTICULARLY EFFECTIVE NONINVASIVE BRAIN STIMULATION MODALITY THAT SHOULD BE USED?
A lot of tDCS and rTMS studies have described similar effects on brain excitability and motor outcomes, but the two modalities are not exchangeable. There are profound differences in the way tDCS and rTMS stimulate cortical neurons, in their respective spatial and temporal resolution, in the possibility to implement an effective sham condition, and the profile of side-effects. However, because of a lack of comparative studies, there is no evidence showing superior therapeutic efficacy for one modality. Even within the same NIBS modality, stimulation protocols have been rarely compared in the same group of individuals (but see [22▪▪,51]). Furthermore, a multitude of patterned or associative rTMS protocols have been introduced during the last 10 years, complementing regular rTMS at a constant frequency [5,52]. Likewise, oscillatory tDCS, transcranial alternative current stimulation, and transcranial random noise stimulation have been introduced in addition to conventional tDCS at constant current intensity [53]. At present, it is unclear whether one of these NIBS modalities will emerge as the ‘winning protocol’. As all these protocols show a substantial inter-subject variability in their neuromodulatory effects, the most pressing question is to identify the mechanisms that render the aftereffects of NIBS more stable and predictable. Solving this general question should have high priority and is at least as important as comparative studies which contrast the efficacy of the various NIBS modailities.
DOES THE LOCATION OF THE STROKE INFLUENCE THE THERAPEUTIC RESPONSE?
Clinical trials have tested the effects of NIBS in patients with cortical and subcortical strokes [54], but with a bias towards the inclusion of patients with subcortical strokes. This can be explained by the fact that cortical strokes may be less amenable to stimulation-induced gains than subcortical strokes [55–57]. Depending on the location and size of a cortical stroke, NIBS might not be efficient to improve a poststroke deficit, especially if the perilesional brain tissue does not contribute to the brain function that is impaired. Task-related fMRI might be useful to clarify whether patients with cortical stroke still can recruit perilesional brain tissue and whether the perilesional functional activation pattern can predict the individual response to NIBS.
Even if the cortical area that is targeted by NIBS is relatively far away from the site of the cortical infarction, it is likely that the electrical current will spread differently in the brain because of the expansion of the space filled with cerebrospinal fluid. In this case, it is particularly important to model the expected field distributions of the NIBS-induced tissue current in the brain and to estimate which brain regions are effectively stimulated by NIBS based on the calculated field distributions [58].
HOW OFTEN SHOULD NONINVASIVE BRAIN STIMULATION BE REPEATED?
One single session of rTMS or tDCS can induce temporary alterations in cortical excitability and sometimes a transient improvement in performance has been demonstrated [59,60▪]. However, for many simple tasks or motor functions, performance is unaltered in stroke patients [61] and healthy participants [62,63]. In contrast, repeated NIBS sessions with one or two NIBS sessions daily may prolong the aftereffects of NIBS even days after the end of the session (e.g. [64,65]). This explains why NIBS is usually given repeatedly over several days or weeks in therapeutic trials to produce cumulative therapeutic effects. However, there is little knowledge about how often the NIBS sessions should be repeated in stroke patients to obtain the best possible clinical effect. Here, it would be very helpful to establish and validate neurophysiological or neuroimaging biomarkers that indicate after how many NIBS sessions the therapeutic effect has peaked and no longer needs further enhancement.
The effects of consecutive rTMS or tDCS sessions might interact with each other. By changing the initial state of the motor cortex (using a preconditioning stimulation session), it is possible to reverse the conditioning effects of 1-Hz rTMS in healthy individuals [66]. These preconditioning effects suggest the existence of a homeostatic mechanism in the human motor cortex. In the context of repeated NIBS interventions, homeostatic metaplasticity-like effects might render the patients less sensitive to further manipulations in order to prevent destabilization of neuronal networks. In fact, it has been suggested that homeostatic-like phenomena might be one of the main factors that limit the duration or effect size of post-TMS effects (e.g. [67]). Yet, it is unknown whether homeostatic counter-regulation still applies when a night of sleep separates two consecutive NIBS sessions. It is possible that a night of sleep re-sensitizes the brain networks to NIBS. In conclusion, the relevance of homeostatic-like plasticity for producing a sustained and stable clinical response after repeated NIBS sessions needs to be systematically addressed in therapeutic settings.
IS THE BRAIN STATE DURING OR BEFORE NONINVASIVE BRAIN STIMULATION CRITICAL TO THERAPEUTIC EFFICACY?
In the recent years, it has become increasingly clear that the functional aftereffects of NIBS depend strongly on the ‘neural context’ of the stimulated brain networks at the time just before and during the administration of NIBS.
Activity-dependent noninvasive brain stimulation
If NIBS is applied in isolation (i.e., at rest), the functional state of the stimulated brain networks is ill defined and may spontaneously fluctuate rendering NIBS less efficient. Alternatively, one might couple NIBS with motor training or other neurorehabilitative interventions to boost the functional impact of NIBS to produce synergistic effects [68]. In patients with chronic stroke, a combination of NIBS and motor training may result in more enduring performance improvements and functional plasticity in the affected hemisphere compared with motor training or stimulation alone [69▪,70]. An additional advantage is that the combination of NIBS and motor learning is involving the participants more than NIBS alone (see [71] for a reference in healthy individuals).
Given the short-term homeostatic interactions described above, the relative timing between training and NIBS might also have an important impact. Motor learning and NIBS could be performed simultaneously, alternating, or sequentially, but it is currently unclear which temporal relationship between NIBS and motor learning will be most effective in a therapeutic setting. Furthermore, it is likely that some motor tasks are more suited to facilitate NIBS-induced neuromodulation than others, because the effects of NIBS on motor learning have been shown to be task dependent in healthy individuals [72]. If so, the choice of the motor training task in a combined NIBS–motor learning trial might be a critical factor for the success of the therapy.
Pharmacologically enhanced noninvasive brain stimulation
Emerging evidence suggest that pharmacological interventions targeting ion channels or modulatory transmitter systems (i.e., the dopaminergic, cholinergic, serotonergic, and noradrenergic systems) may have a potential to enhance motor recovery [73,74]. It has also been shown that the plasticity-inducing effects of NIBS can effectively be modulated by pharmacological interventions in healthy individuals [75▪]. Combining NIBS with pharmacological interventions may indeed improve our understanding of the pathophysiology of the abnormal plasticity in particular in stroke patients. The evidence supporting that the combination of pharmacotherapy and NIBS might be superior to NIBS alone is still limited. Amongst the very few published trials, Kakuda et al.[76] combined low-frequency rTMS, occupational therapy and dopamine substitution (levodopa), and found improved motor functions in the affected upper limbs. Unfortunately, the study design had no control arms in which the therapeutic effect of each intervention was tested in isolation.
CONCLUSION
We argue that the questions discussed in our review need to be tackled in future studies to gain sufficient mechanistic understanding of how NIBS facilitates the recovery of function after stroke. In tune with this view, there has recently been increased interest in the field to better characterize the individual physiopathology and to better predict the individual response to therapeutic NIBS. Several potential predictive markers have been identified, including changes in ipsilesional/contralesional M1 activity and residual perilesional activity [22▪▪], impaired connectivity between key motor regions [77], metabolic markers such as GABA levels in ipsilateral M1 [78▪▪], or asymmetry in microstructural measures based on diffusion MRI [27].
These promising lines of research need to be expanded in the future in order to pave the way towards adaptive NIBS that can be tailored to the individual patient. This might be realized through closed-loop stimulation using a brain stimulation interface (BSI). BSI could be used to track online whether NIBS evokes the intended neurobiological response. This information could then be fed back into the NIBS device to adjust the stimulation parameters in order to induce or maintain the desired functional effect. However, adaptive NIBS will require a thorough understanding of the neurobiological mechanisms that facilitate stroke recovery.
Acknowledgements
None.
Conflicts of interest
H.R.S. has received honoraria as member on a scientific advisory board (Lundbeck A/S), honoraria as handling editor of Neuroimage (Elsevier Publishers), and honoraria (Biogen Idec Denmark A/S and Genzyme A/S) as speaker and financial travel support (Magventure A/S).
H.R.S. and E.R. were supported by a Grant of Excellence sponsored by The Lundbeck Foundation Mapping, Modulation & Modeling the Control of Actions (ContAct) (R59-A5399).
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
Footnotes
Correspondence to Estelle Raffin, MSc, PhD, DRCMR, Hvidovre Hospital, Kettegåard Allé, 30, 2659 Hvidovre, Denmark. Tel: +45 38626206; e-mail: esteller@drcmr.dk
REFERENCES
- 1.Hummel F, Celnik P, Giraux P, et al. Effects of noninvasive cortical stimulation on skilled motor function in chronic stroke. Brain 2005; 128:490–499 [DOI] [PubMed] [Google Scholar]
- 2▪.Khedr EM, Shawky OA, El-Hammady DH, et al. Effect of anodal versus cathodal transcranial direct current stimulation on stroke rehabilitation: a pilot randomized controlled trial. Neurorehabil Neural Repair 2013; 27:592–601 [DOI] [PubMed] [Google Scholar]; This study compares the long-term effect of anodal tDCS over the affected hemisphere versus cathodal tDCS over the unaffected hemisphere on motor recovery in patients after subacute stroke. The authors report that both tDCS protocols enhance the effects of a traditional rehabilitation program. The effects were still present 3 months after the end of the treatment.
- 3▪▪.Hao Z, Wang D, Zeng Y, Liu M. Repetitive transcranial magnetic stimulation for improving function after stroke. Cochrane Database Syst Rev 2013; 5:CD008862. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study presents a thorough meta-analysis including all published randomized controlled trials in which the effects of rTMS therapy were compared with sham therapy or no therapy.
- 4▪.Butler AJ, Shuster M, O’Hara E, et al. A meta-analysis of the efficacy of anodal transcranial direct current stimulation for upper limb motor recovery in stroke survivors. J Hand Ther 2013; 26:162–170quiz 171 [DOI] [PubMed] [Google Scholar]; This meta-analysis summarizes the effects of anodal tDCS on motor recovery in patients with motor stroke affecting the upper limb.
- 5.Ziemann U, Paulus W, Nitsche MA, et al. Consensus: motor cortex plasticity protocols. Brain Stimul 2008; 1:164–182 [DOI] [PubMed] [Google Scholar]
- 6.Roche N, Lackmy A, Achache V, et al. Effects of anodal transcranial direct current stimulation over the leg motor area on lumbar spinal network excitability in healthy subjects. J Physiol 2011; 589:2813–2826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nitsche MA, Nitsche MS, Klein CC, et al. Level of action of cathodal DC polarisation induced inhibition of the human motor cortex. Clin Neurophysiol 2003; 114:600–604 [DOI] [PubMed] [Google Scholar]
- 8.Quartarone A, Bagnato S, Rizzo V, et al. Distinct changes in cortical and spinal excitability following high-frequency repetitive TMS to the human motor cortex. Exp Brain Res 2005; 161:114–124 [DOI] [PubMed] [Google Scholar]
- 9.Valero-Cabre A, Oliveri M, Gangitano M, Pascual-Leone A. Modulation of spinal cord excitability by subthreshold repetitive transcranial magnetic stimulation of the primary motor cortex in humans. Neuroreport 2001; 12:3845–3848 [DOI] [PubMed] [Google Scholar]
- 10.Nowak DA, Grefkes C, Ameli M, Fink GR. Interhemispheric competition after stroke: brain stimulation to enhance recovery of function of the affected hand. Neurorehabil Neural Repair 2009; 23:641–656 [DOI] [PubMed] [Google Scholar]
- 11.Murase N, Duque J, Mazzocchio R, Cohen LG. Influence of interhemispheric interactions on motor function in chronic stroke. Ann Neurol 2004; 55:400–409 [DOI] [PubMed] [Google Scholar]
- 12.Wang RY, Tseng HY, Liao KK, et al. rTMS combined with task-oriented training to improve symmetry of interhemispheric corticomotor excitability and gait performance after stroke: a randomized trial. Neurorehabil Neural Repair 2012; 26:222–230 [DOI] [PubMed] [Google Scholar]
- 13.Barwood CH, Murdoch BE, Riek S, et al. Long term language recovery subsequent to low frequency rTMS in chronic nonfluent aphasia. NeuroRehabilitation 2013; 32:915–928 [DOI] [PubMed] [Google Scholar]
- 14.Thiel A, Hartmann A, Rubi-Fessen I, et al. Effects of noninvasive brain stimulation on language networks and recovery in early poststroke aphasia. Stroke 2013; 44:2240–2246 [DOI] [PubMed] [Google Scholar]
- 15.Kim BR, Chun MH, Kim DY, Lee SJ. Effect of high- and low-frequency repetitive transcranial magnetic stimulation on visuospatial neglect in patients with acute stroke: a double-blind, sham-controlled trial. Arch Phys Med Rehabil 2013; 94:803–807 [DOI] [PubMed] [Google Scholar]
- 16.Thielscher A, Opitz A, Windhoff M. Impact of the gyral geometry on the electric field induced by transcranial magnetic stimulation. Neuroimage 2011; 54:234–243 [DOI] [PubMed] [Google Scholar]
- 17.Miranda PC, Mekonnen A, Salvador R, Ruffini G. The electric field in the cortex during transcranial current stimulation. Neuroimage 2012; 70C:48–58 [DOI] [PubMed] [Google Scholar]
- 18▪.Dayan E, Censor N, Buch ER, et al. Noninvasive brain stimulation: from physiology to network dynamics and back. Nat Neurosci 2013; 16:838–844 [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors review the key findings that contribute to our understanding of the mechanisms underlying the physiological and behavioral effects of NIBS. They emphasize the importance of combining NIBS and neuroimaging techniques to investigate brain network dynamics after NIBS.
- 19.Siebner HR, Rothwell J. Transcranial magnetic stimulation: new insights into representational cortical plasticity. Exp Brain Res 2003; 148:1–16 [DOI] [PubMed] [Google Scholar]
- 20.Siebner HR, Bergmann TO, Bestmann S, et al. Consensus paper: combining transcranial stimulation with neuroimaging. Brain Stimul 2009; 2:58–80 [DOI] [PubMed] [Google Scholar]
- 21.Thut G, Pascual-Leone A. A review of combined TMS-EEG studies to characterize lasting effects of repetitive TMS and assess their usefulness in cognitive and clinical neuroscience. Brain Topogr 2010; 22:219–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22▪▪.Stagg CJ, Bachtiar V, O'Shea J, et al. Cortical activation changes underlying stimulation-induced behavioural gains in chronic stroke. Brain 2012; 135:276–284 [DOI] [PMC free article] [PubMed] [Google Scholar]; This is an outstanding neuroimaging study on the neural effects of intermittent and excitatory theta burst stimulation in chronic stroke patients.
- 23.Salatino A, Berra E, Troni W, et al. Behavioral and neuroplastic effects of low-frequency rTMS of the unaffected hemisphere in a chronic stroke patient: a concomitant TMS and fMRI study. Neurocase 2013; [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Conchou F, Loubinoux I, Castel-Lacanal E, et al. Neural substrates of low-frequency repetitive transcranial magnetic stimulation during movement in healthy subjects and acute stroke patients. A PET study. Hum Brain Mapp 2009; 30:2542–2557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grefkes C, Nowak DA, Wang LE, et al. Modulating cortical connectivity in stroke patients by rTMS assessed with fMRI and dynamic causal modeling. Neuroimage 2010; 50:233–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friston KJ, Harrison L, Penny W. Dynamic causal modelling. Neuroimage 2003; 19:1273–1302 [DOI] [PubMed] [Google Scholar]
- 27.Allendorfer JB, Storrs JM, Szaflarski JP. Changes in white matter integrity follow excitatory rTMS treatment of poststroke aphasia. Restor Neurol Neurosci 2012; 30:103–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwarzkopf DS, Silvanto J, Rees G. Stochastic resonance effects reveal the neural mechanisms of transcranial magnetic stimulation. J Neurosci 2011; 31:3143–3147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miniussi C, Harris JA, Ruzzoli M. Modelling noninvasive brain stimulation in cognitive neuroscience. Neurosci Biobehav Rev 2013; 37:1702–1712 [DOI] [PubMed] [Google Scholar]
- 30.McDonnell MD, Ward LM. The benefits of noise in neural systems: bridging theory and experiment. Nat Rev Neurosci 2011; 12:415–426 [DOI] [PubMed] [Google Scholar]
- 31.Johnson JS, Hamidi M, Postle BR. Using EEG to explore how rTMS produces its effects on behavior. Brain Topogr 2010; 22:281–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamidi M, Slagter HA, Tononi G, Postle BR. Repetitive transcranial magnetic stimulation affects behavior by biasing endogenous cortical oscillations. Front Integr Neurosci 2009; 3:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leung A, Donohue M, Xu R, et al. rTMS for suppressing neuropathic pain: a meta-analysis. J Pain 2009; 10:1205–1216 [DOI] [PubMed] [Google Scholar]
- 34.Koch G, Bonni S, Giacobbe V, et al. Theta-burst stimulation of the left hemisphere accelerates recovery of hemispatial neglect. Neurology 2012; 78:24–30 [DOI] [PubMed] [Google Scholar]
- 35.Elsner B, Kugler J, Pohl M, Mehrholz J. Transcranial direct current stimulation (tDCS) for improving aphasia in patients after stroke. Cochrane Database Syst Rev 2013; 6:CD009760. [DOI] [PubMed] [Google Scholar]
- 36.Wong IS, Tsang HW. A review on the effectiveness of repetitive transcranial magnetic stimulation (rTMS) on poststroke aphasia. Rev Neurosci 2013; 24:105–114 [DOI] [PubMed] [Google Scholar]
- 37.Jorge RE, Robinson RG, Tateno A, et al. Repetitive transcranial magnetic stimulation as treatment of poststroke depression: a preliminary study. Biol Psychiatry 2004; 55:398–405 [DOI] [PubMed] [Google Scholar]
- 38.Baumer T, Lange R, Liepert J, et al. Repeated premotor rTMS leads to cumulative plastic changes of motor cortex excitability in humans. Neuroimage 2003; 20:550–560 [DOI] [PubMed] [Google Scholar]
- 39.Boros K, Poreisz C, Munchau A, et al. Premotor transcranial direct current stimulation (tDCS) affects primary motor excitability in humans. Eur J Neurosci 2008; 27:1292–1300 [DOI] [PubMed] [Google Scholar]
- 40.Rizzo V, Siebner HR, Modugno N, et al. Shaping the excitability of human motor cortex with premotor rTMS. J Physiol 2004; 554:483–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyd LA, Linsdell MA. Excitatory repetitive transcranial magnetic stimulation to left dorsal premotor cortex enhances motor consolidation of new skills. BMC Neurosci 2009; 10:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meehan SK, Zabukovec JR, Dao E, et al. One Hertz repetitive transcranial magnetic stimulation over dorsal premotor cortex enhances offline motor memory consolidation for sequence-specific implicit learning. Eur J Neurosci 2013; [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fierro B, Giglia G, Palermo A, et al. Modulatory effects of 1 Hz rTMS over the cerebellum on motor cortex excitability. Exp. Brain Res 2007; 176:440–447 [DOI] [PubMed] [Google Scholar]
- 44.Block HJ, Celnik P. Can cerebellar transcranial direct current stimulation become a valuable neurorehabilitation intervention? Expert Rev Neurother 2012; 12:1275–1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rosso C, Valabregue R, Attal Y, et al. Contribution of corticospinal tract and functional connectivity in hand motor impairment after stroke. PLoS One 2013; 8:e73164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lotze M, Markert J, Sauseng P, et al. The role of multiple contralesional motor areas for complex hand movements after internal capsular lesion. J Neurosci 2006; 26:6096–6102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Craciunas SC, Brooks WM, Nudo RJ, et al. Motor and premotor cortices in subcortical stroke: proton magnetic resonance spectroscopy measures and arm motor impairment. Neurorehabil Neural Repair 2013; 27:411–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arai N, Muller-Dahlhaus F, Murakami T, et al. State-dependent and timing-dependent bidirectional associative plasticity in the human SMA-M1 network. J Neurosci 2011; 31:15376–15383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Potter-Nerger M, Fischer S, Mastroeni C, et al. Inducing homeostatic-like plasticity in human motor cortex through converging corticocortical inputs. J Neurophysiol 2009; 102:3180–3190 [DOI] [PubMed] [Google Scholar]
- 50.Rizzo V, Bove M, Naro A, et al. Associative cortico-cortical plasticity may affect ipsilateral finger opposition movements. Behav Brain Res 2011; 216:433–439 [DOI] [PubMed] [Google Scholar]
- 51.Fregni F, Boggio PS, Nitsche M, et al. Anodal transcranial direct current stimulation of prefrontal cortex enhances working memory. Exp Brain Res 2005; 166:23–30 [DOI] [PubMed] [Google Scholar]
- 52.Hamada M, Terao Y, Hanajima R, et al. Bidirectional long-term motor cortical plasticity and metaplasticity induced by quadripulse transcranial magnetic stimulation. J Physiol 2008; 586:3927–3947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guleyupoglu B, Schestatsky P, Edwards D, et al. Classification of methods in transcranial Electrical Stimulation (tES) and evolving strategy from historical approaches to contemporary innovations. J Neurosci Methods 2013; 219:297–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adeyemo BO, Simis M, Macea DD, Fregni F. Systematic review of parameters of stimulation, clinical trial design characteristics, and motor outcomes in noninvasive brain stimulation in stroke. Front Psychiatry 2012; 3:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ackerley SJ, Stinear CM, Barber PA, Byblow WD. Combining theta burst stimulation with training after subcortical stroke. Stroke 2010; 41:1568–1572 [DOI] [PubMed] [Google Scholar]
- 56.Talelli P, Greenwood RJ, Rothwell JC. Exploring theta burst stimulation as an intervention to improve motor recovery in chronic stroke. Clin Neurophysiol 2007; 118:333–342 [DOI] [PubMed] [Google Scholar]
- 57.Ameli M, Grefkes C, Kemper F, et al. Differential effects of high-frequency repetitive transcranial magnetic stimulation over ipsilesional primary motor cortex in cortical and subcortical middle cerebral artery stroke. Ann Neurol 2009; 66:298–309 [DOI] [PubMed] [Google Scholar]
- 58.Wagner T, Fregni F, Eden U, et al. Transcranial magnetic stimulation and stroke: a computer-based human model study. Neuroimage 2006; 30:857–870 [DOI] [PubMed] [Google Scholar]
- 59.Mansur CG, Fregni F, Boggio PS, et al. A sham stimulation-controlled trial of rTMS of the unaffected hemisphere in stroke patients. Neurology 2005; 64:1802–1804 [DOI] [PubMed] [Google Scholar]
- 60▪.Lefebvre S, Thonnard JL, Laloux P, et al. Single session of dual-tDCS transiently improves precision grip and dexterity of the paretic hand after stroke. Neurorehabil Neural Repair 2013; [Epub ahead of print] [DOI] [PubMed] [Google Scholar]; This study suggests that one session of dual tDCS has a beneficial effect on the upper limb function of moderate to severely impaired stroke patients. This tDCS modality should be tested in longer protocols for neurorehabilitation.
- 61.Liepert J, Zittel S, Weiller C. Improvement of dexterity by single session low-frequency repetitive transcranial magnetic stimulation over the contralesional motor cortex in acute stroke: a double-blind placebo-controlled crossover trial. Restor Neurol Neurosci 2007; 25:461–465 [PubMed] [Google Scholar]
- 62.Muellbacher W, Ziemann U, Boroojerdi B, Hallett M. Effects of low-frequency transcranial magnetic stimulation on motor excitability and basic motor behavior. Clin Neurophysiol 2000; 111:1002–1007 [DOI] [PubMed] [Google Scholar]
- 63.Strens LH, Oliviero A, Bloem BR, et al. The effects of subthreshold 1 Hz repetitive TMS on cortico-cortical and interhemispheric coherence. Clin Neurophysiol 2002; 113:1279–1285 [DOI] [PubMed] [Google Scholar]
- 64.Khedr EM, Shawky OA, El-Hammady DH, et al. Effect of anodal versus cathodal transcranial direct current stimulation on stroke rehabilitation: a pilot randomized controlled trial. Neurorehabil Neural Repair 2013; 27:592–601 [DOI] [PubMed] [Google Scholar]
- 65.Boggio PS, Nunes A, Rigonatti SP, et al. Repeated sessions of noninvasive brain DC stimulation is associated with motor function improvement in stroke patients. Restor Neurol Neurosci 2007; 25:123–129 [PubMed] [Google Scholar]
- 66.Siebner HR, Lang N, Rizzo V, et al. Preconditioning of low-frequency repetitive transcranial magnetic stimulation with transcranial direct current stimulation: evidence for homeostatic plasticity in the human motor cortex. J Neurosci 2004; 24:3379–3385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thickbroom GW. Transcranial magnetic stimulation and synaptic plasticity: experimental framework and human models. Exp Brain Res 2007; 180:583–593 [DOI] [PubMed] [Google Scholar]
- 68.Cattaneo L, Sandrini M, Schwarzbach J. State-dependent TMS reveals a hierarchical representation of observed acts in the temporal, parietal, and premotor cortices. Cereb Cortex 2010; 20:2252–2258 [DOI] [PubMed] [Google Scholar]
- 69▪.Zimerman M, Heise KF, Hoppe J, et al. Modulation of training by single-session transcranial direct current stimulation to the intact motor cortex enhances motor skill acquisition of the paretic hand. Stroke 2012; 43:2185–2191 [DOI] [PMC free article] [PubMed] [Google Scholar]; In this double-blind crossover study, the authors test the effects of cathodal versus sham tDCS during a training program on 12 stroke patients. They find that tDCS facilitates the acquisition of a new motor skill and report a significant correlation between the tDCS-induced improvement during training and the tDCS-induced changes in intracortical inhibition.
- 70.Kakuda W, Abo M, Shimizu M, et al. A multicenter study on low-frequency rTMS combined with intensive occupational therapy for upper limb hemiparesis in poststroke patients. J Neuroeng Rehabil 2012; 9:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Reis J, Fritsch B. Modulation of motor performance and motor learning by transcranial direct current stimulation. Curr Opin Neurol 2011; 24:590–596 [DOI] [PubMed] [Google Scholar]
- 72.Saucedo Marquez CM, Zhang X, Swinnen SP, et al. Task-specific effect of transcranial direct current stimulation on motor learning. Front Hum Neurosci 2013; 7:333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krieger DW. Therapeutic drug approach to stimulate clinical recovery after brain injury. Front Neurol Neurosci 2013; 32:76–87 [DOI] [PubMed] [Google Scholar]
- 74.Chavez JC, Hurko O, Barone FC, Feuerstein GZ. Pharmacologic interventions for stroke: looking beyond the thrombolysis time window into the penumbra with biomarkers, not a stopwatch. Stroke 2009; 40:e558–e563 [DOI] [PubMed] [Google Scholar]
- 75▪.Nitsche MA, Muller-Dahlhaus F, Paulus W, Ziemann U. The pharmacology of neuroplasticity induced by noninvasive brain stimulation: building models for the clinical use of CNS active drugs. J Physiol 2012; 590:4641–4662 [DOI] [PMC free article] [PubMed] [Google Scholar]; This review summarizes how pharmalogical interventions modify the plasticity-inducing effects of NIBS.
- 76.Kakuda W, Abo M, Kobayashi K, et al. Combination treatment of low-frequency rTMS and occupational therapy with levodopa administration: an intensive neurorehabilitative approach for upper limb hemiparesis after stroke. Int J Neurosci 2011; 121:373–378 [DOI] [PubMed] [Google Scholar]
- 77.Grefkes C, Fink GR. Disruption of motor network connectivity poststroke and its noninvasive neuromodulation. Curr Opin Neurol 2012; 25:670–675 [DOI] [PubMed] [Google Scholar]
- 78▪▪.O'Shea J, Boudrias MH, Stagg CJ, et al. Predicting behavioural response to TDCS in chronic motor stroke. Neuroimage 2013; [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]; This study is highly relevant showing that it is possible to identify neuroimaging markers to predict the individual response to tDCS in chronic stroke patients.


