Abstract
AIM: To estimate an effect size for the transversus abdominis plane (TAP) infiltration on quality of recovery in patients undergoing laparoscopic gastric band surgery.
METHODS: The pilot study was a randomized, double blinded, placebo controlled trial. Patients undergoing laparoscopic gastric band surgery were randomized to receive a bilateral TAP infiltration with 20 mL of 0.5% ropivacaine or saline. The evaluated outcomes included quality of recovery-40 (QoR-40) at 24 h, postoperative opioid consumption and pain. Data was examined using the Mann-Whitney U test.
RESULTS: Nineteen subjects were recruited. There was a positive trend favoring the TAP infiltration group in global QoR-40 scores at 24 h after surgery, median [interquartile range (IQR)] of 175.5 (170-189) compared to 170 (160-175) in the control group (P = 0.06). There also a positive trend toward a lower cumulative opioid consumption in the TAP infiltration group, median (IQR) of 7.5 (2.5-11.5) mg iv morphine equivalents compared to 13 (7-21.5) in the control group (P = 0.07). Correlation analysis (Spearman’s Rho) demonstrated an inverse relationship between 24 h cumulative opioid consumption and global QoR-40 scores, -0.49 (P = 0.03).
CONCLUSION: The use of multimodal analgesic techniques to reduce opioid related side effects is particularly desirable in morbidly obese patients undergoing gastric reduction surgery. The TAP infiltration seems to have a clinically important effect in reducing postoperative opioid consumption and improve quality of recovery after laparoscopic gastric band surgery in morbid obese patients. Future studies to confirm the beneficial effects of the TAP infiltration in these patients are warranted.
Keywords: Transversus abdominis plane, Infiltration, Gastric band, Pain, Recovery
Core tip: In this current randomized, double blinded, placebo controlled pilot study we estimated the effect of a transversus abdominis plane block on postoperative quality of recovery in morbidly obese patients undergoing laparoscopic gastric band surgery. Postoperative opioid consumption was inversely correlated to quality of recovery in this surgical population. The transversus abdominis plane block seems to be an effective strategy to improve quality of recovery in those patients.
INTRODUCTION
Pain after surgery is undertreated and fails to be managed optimally despite compelling data regarding the consequence of poorly managed analgesia[1-3]. In addition to patient suffering, postoperative pain can also affect quality of recovery after surgical procedures[4-6]. It is likely, therefore, that strategies that improve postoperative pain can also ameliorate postsurgical recovery[7-9]. The improvement of postsurgical recovery is particularly important for patients having ambulatory surgery, since those patients do not benefit from structured hospital support for recover after surgery[10-12].
Laparoscopic gastric band surgery can be performed in the outpatient setting when optimal postsurgical pain control is achived[13]. Interventions to minimize pain and reduce opioid consumption in those patients are particularly desirable in order to avoid opioids related side effect such as nausea and vomiting[14,15]. The transversus abdominis plane (TAP) Infiltration has been used to minimize pain in a diverse range of surgical procedures but its effect on obese patients undergoing laparoscopic gastric band surgery has it to be investigated[16-19]. More importantly, it is currently unknown if the analgesic benefits of the TAP infiltration can translate to a better recovery for patients undergoing laparoscopic gastric band procedures.
The main objective of the current pilot study was to estimate an effect size for TAP analgesia on postsurgical quality of recovery in patients having laparoscopic gastric band surgery. We hypothesized that patients receiving a TAP infiltration with ropivacaine would have a better quality of postsurgical recovery than patients having a TAP infiltration with saline. We also sought to estimate an effect of the TAP infiltration on postoperative analgesia.
MATERIALS AND METHODS
This pilot study was a prospective, randomized, double-blinded placebo controlled trial. Clinical trial registration for this study can be found at ClinicalTrial.gov (http://www.clinicaltrials.gov); registration identified: NCT01075087. Eligible subjects were patients undergoing laparoscopic gastric band surgery to reduce morbid obesity. Patients with a history of allergy to local anesthetics, chronic use of an opioid analgesic, corticosteroid and/or pregnant subjects were not enrolled. Reason for exclusion from the study following study drug administration was conversion from a laparoscopic to an open incision or patient request. Subjects were randomized using a computer generated table of random numbers into two groups to receive 20 mL of a bilateral ultrasound guided TAP infiltration using: saline or ropivacaine 0.5% (Naropin, APP Pharmaceuticals, Schaumburg, IL, United States). Group assignments were sealed in sequentially numbered opaque envelopes that were opened by a research nurse not involved with the patient care or data collection after the subject provided written informed consent. The same nurse prepared syringes labeled with study drug to blind subjects enrolled in the study, anesthesia providers and investigators collecting the data.
After anesthesia induction a bilateral TAP infiltration was performed in all subjects using ultrasound guidance with a portable ultrasound device (SonoSite, Bothell, WA, United States) and a linear 6-13 Mega Hertz ultrasound transducer. The technique used to performed the TAP infiltrations was the posterior approach as previously described by Hebbard et al[20]. Once the external oblique abdominal, the internal oblique abdominal and the transversus abdominal muscles were visualized using the ultrasound probe at the level of the anterior axillary line between the 12th rib and the iliac crest, the puncture area was prepared in a sterile manner. The injection of the study drug was performed using a 21 gauge 90 mm StimuQuik needle (Arrow International, Reading, PA, United States) by a single investigator with extensive experience in performing the TAP block (Gildasio S De Oliveira Jr). Once the tip of the needle was placed in the space between the internal oblique abdominal muscle and the transversus abdominal muscle, and after negative aspiration of blood, 20 mL of the study drug was administered and distribution of the solution in the TAP was confirmed using ultrasonography observation. A contralateral infiltration was performed in the same fashion.
All subjects were premedicated with 0.04 mg/kg iv midazolam. Propofol 1-2 mg/kg was administered for anesthesia induction, a remifentanil 0.05 mcg/kg per minute iv infusion was begun and succinylcholine 1-2 mg/kg was administered to induce muscle paralysis. All the medications in the study protocol were dosed based on the dosing body weight [ideal body weight (IBW) + [0.4 × (actual body weight - IBW)][21]. Tracheal intubation was initially attempted by an anesthesia resident physician or a certified registered nurse anesthetist under supervision of an attending anesthesiologist. Anesthesia maintenance was achieved using remifentanil, titrated to maintain the mean arterial pressure within 20% of baseline, desflurane titrated to a bispectral index (Aspect Medical System Inc., Norwood, MA, United States) between 40 and 60 and rocuronium. At the end of the procedure at removal of the laparoscopic instruments the remifentanil infusion was discontinued and the subjects received intravenous ketorolac 30 mg and ondansetron 4 mg. The laparoscopic insufflation pressure was kept at 15 mmHg for the procedure. Five trocars were used for the surgery (two below the xyphoid, one in the right upper quadrant, one in the left upper quadrant and the last one on the left anterior axillary line below the costal margin).
In the post anesthesia care unit (PACU) subjects were asked to rate their pain at rest upon arrival and at regular (30 min) intervals on a 0-10 pain numeric rating scale (NRS), where 0 means no pain and 10 is the worst pain imaginable. The area under the NRS pain scale vs time curve was calculated using the trapezoidal method as an indicator of pain burden during early recovery (Graph Pad Prism ver 5.03, Graph Pad Software, Inc., La Jola, CA, United States). Hydromorphone 0.4 mg iv was administered every 5 min to maintain a NRS pain score less than 4 out of 10. In cases of postoperative nausea or vomiting, subjects received 10 mg iv metoclopramide. When subjects were able to tolerate oral medications, a combination of hydrocodone 10 mg plus acetaminophen 325 mg were used for pain greater than 4 of 10. Postoperative opioid consumption (24 h) was converted to equivalent dose of oral morphine[22].
Subjects were followed up at 24 h after the procedure by an investigator unaware of group allocation and were questioned regarding analgesic consumption, pain score and the QoR-40 questionnaire was administered[23]. The questionnaire consists of 40 questions that examine 5 domains of patient recovery using a 5 point Likert scale: none of the time, some of the time, usually, most of the time and all of the time. The five domains include physical comfort, pain, physical independence, psychological support and emotional state. Individualized items of the questionnaire have been previously presented by our group[24]. Other perioperative data collected included subject’s age, height, weight, American Society of Anesthesiologist physical status, surgical duration, intraoperative remifentanil use, total intravenous fluids and total amount of hydromorphone in PACU and time to hospital discharge.
Ethics
This work has been carried out in accordance with the declaration of Helsinki (2000) of the World Medical Association. Study approval was obtained from the Northwestern University Institutional Review Board (STU00023482), and written informed consent was obtained from all the study participants.
Statistical analysis
A sample size of 23 subjects per group was estimated to achieve 80% power to detect a 10 point difference in the aggregated QoR-40 score for the 2 study groups to be compared assuming an overall standard deviation of 12 points similar what was observed in a previous investigation[25]. To account for drop-outs 50 subjects were planned to be recruited and randomized. However, due to changes in the case profiles in our hospital (increased number of gastric sleeve surgery and decreased number of laparoscopic gastric band surgery, nineteen patients were recruited). The sample size calculation was made using PASS version 8.0.15 release date January 14, 2010 (NCSS, LLC, Kaysville, UT).
The Shapiro-Wilk and Kolmogorov-Smirnov tests were used to test the hypothesis of normal distribution. Normally distributed interval data are reported as mean (SD) and were evaluated with Student’s t test for equal variances. Non-normally distributed interval and ordinal data are reported as median [range or interquartile range (IQR)] and compared among groups using the Mann-Whitney U test. A correlation analysis (Spearman’s Rho) was performed to examine a relationship between opioids consumption and global quality of recovery score. All reported P values are two-tailed. To avoid the chance of a type I error, the criterion for rejection of the null hypothesis was a two-tailed P < 0.05 for comparisons.
Statistical analysis was performed using NCSS 8 8.0.15, release date 5/15/2013 (NCSS, LLC, Kaysville, UT) and R version 3.0.1, release date 5/16/2013 (The R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
The details of the conduct of the study are shown in Figure 1. Nineteen subjects were randomized and nineteen completed the study. Patients were enrolled consecutively from 3/2010 through 7/2012. Patients’ baseline characteristics and surgical factors were not different between groups (Table 1).
Figure 1.
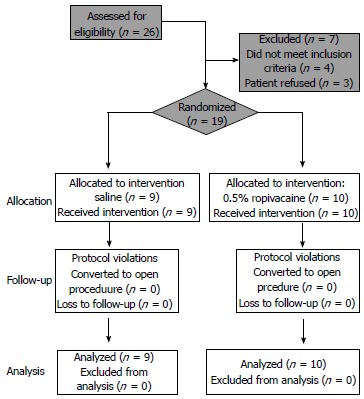
Flow chart describing subjects allocation.
Table 1.
Baseline patient and surgical characteristics
| TAP infiltration (n = 10) | Saline (n = 9) | P value | |
| Age (yr) | 47 (39-53) | 50 (36-54) | 0.90 |
| Gender | 1.00 | ||
| Male | 2 | 2 | |
| Female | 8 | 7 | |
| BMI (kg/m2) | 44.2 (39.0-45.7) | 40.1(38.5-44.3) | 0.46 |
| ASA class | 0.37 | ||
| II | 3 | 5 | |
| III | 7 | 4 | |
| Surgical duration (min) | 76.5 (51-106) | 92 (61-120) | 0.53 |
| Remifentanil (mcg) | 620 (500-750) | 850 (600-1100) | 0.23 |
| Intravenous fluids (mL) | 1050 (585-1600) | 1300 (1200-1500) | 0.43 |
Data are expressed as median [interquartile range (IQR)]. TAP: Transversus abdominis plane; ASA: American society of anesthesiologists; BMI: Body mass index.
There was a positive trend favoring the TAP infiltration group in global QoR-40 scores at 24 h after surgery, median (IQR) of 175.5 (170-189) compared to 170 (160-175) in the control group (P = 0.06). There was also a positive trend towards a reduction of postoperative pain in the post-anesthesia care unit for the TAP infiltration group, median (IQR) of 195 (135-300) (score × min) compared to 315 (195-420) (score × min) in the control group (P = 0.09). Other postoperative variables are presented in Table 2.
Table 2.
Postoperative data
| TAP infiltration (n = 10) | Saline (n = 9) | P value | |
| Nausea in PACU | 0.33 | ||
| Yes | 1 | 3 | |
| No | 9 | 6 | |
| Vomiting/Retching in PACU | 0.47 | ||
| Yes | 0 | 1 | |
| No | 10 | 8 | |
| Time to discharge from PACU (min) | 60 (60-75) | 75 (60-90) | 0.41 |
| Time to discharge from the hospital (h) | 32.1 (13.9-52.6) | 22.5 (19-26) | 0.47 |
TAP: Transversus abdominis plane; PACU: Post anesthesia care unit.
Another positive trend was identified toward a lower cumulative opioid consumption in the TAP infiltration group, median (IQR) of 7.5 (2.5-11.5) mg iv morphine equivalents compared to 13 (7-21.5) mg iv morphine equivalents in the control group (P = 0.07)
Correlation analysis (Spearman’s Rho) demonstrated an inverse relationship between 24 h cumulative opioid consumption and global QoR-40 scores, ρ = -0.49 (P = 0.03).
DISCUSSION
The most important finding of the current study was a probable benefit of the TAP infiltration to improve postoperative quality of recovery after laparoscopic gastric band surgery in morbidly obese patients. In addition, a similar trend toward a reduction in pain burden and opioid consumption was also detected in the TAP infiltration group compared to saline. The inverse relationship between postoperative opioid consumption and quality of recovery in the subjects in this study support our previous findings of reduced opioid use and improved postoperative recovery[16,23,25]. Our results suggest that the TAP infiltration may be a clinically significant multimodal strategy to reduce pain and improve quality of postsurgical recovery in patients undergoing laparoscopic gastric band surgery.
Our results are particularly important since the development of opioid related side effects such as vomiting in gastric reduction surgery can lead to surgical complications[26]. In addition greater opioid consumption in obese patients with obstructive sleep apnea can also result in postoperative hypoxemic events[27-29]. It remains to be determined if the opioid reduction due to the TAP infiltration can minimize opioid related side effects in morbid obese patients undergoing gastric reduction surgery.
Despite a possible benefit on postoperative analgesia, we did not observe a parallel reduction in hospital stay in our study population. Hospital stay, in the inpatient population, has been criticized as a reliable outcome due to the innumerous potential confounders that can alter that outcome[30-32]. Even established analgesic interventions, often fail to demonstrate a beneficial effect on duration of hospital stay[33,34]. Nevertheless, the optimal postoperative pain control in patients undergoing laparoscopic gastric band surgery may help the performance of this surgery as an outpatient procedure[35,36].
It is important to note that the transversus abdominis block successfully treats parietal pain but visceral pain is not treated by a TAP block. This is likely the reason why even patients in the TAP block group required the use of systemic opioids. Nevertheless, it seems that the reduction in the parietal pain is an important step to improve quality of recovery in patients undergoing laparoscopic gastric bending.
The TAP infiltration has been previously evaluated in morbidly obese patients undergoing different surgical procedures than the one presented in the current investigation. Sinha et al[37] detected a large effect on analgesic outcomes of the TAP infiltration in patients undergoing laparoscopic gastric bypass. The authors’ results were interesting since laparoscopic gastric bypass surgery requires a more extensive procedure which can result in greater visceral pain and a potential lower benefit of the TAP infiltration. In contrast, a retrospective evaluation of obese patients undergoing abdominal plastic surgery did not detect a benefit of the TAP infiltration compared to control for postoperative pain[38]. The effect of the TAP infiltration on postoperative pain outcomes in obese patients may, therefore, be dependent on the type of surgical procedure.
Our current study should only be interpreted according to its limitations. We were unable to complete recruitment and we were underpowered to achieve statistically significant results in our main outcomes. Based on the differences observed in the current study, group sample sizes of 24 per group would have been needed to show a difference in opioid consumption between groups if the actual difference was 5.5 as observed in the current study. Nevertheless, we believe that our current results are clinically important and will stimulate future studies involving regional and local anesthesia techniques in the morbidly obese patient population.
In summary, we report an important beneficial clinical effect of TAP infiltration on quality of recovery in morbidly obese patients after laparoscopic gastric band surgery. It seems that the reduction in postoperative opioids by the TAP infiltration resulted in a better recovery in that patient population. Future studies are warranted to confirm the beneficial effect of the TAP infiltration on postoperative recovery and analgesia in the same patient population.
COMMENTS
Background
Opioids are commonly used to treat postoperative pain in patients undergoing laparoscopic gastric banding. The transversus abdominis plane block has been used successfully to improve recovery in other patient populations but it is unknown if it can also improve recovery for obese patients undergoing laparoscopic gastric banding.
Research frontiers
The transversus abdominis plane (TAP) block seems to improve quality of recovery in patients undergoing laparoscopic gastric banding through a reduction in the consumption of opioids.
Innovations and breakthroughs
This is the first study to demonstrate a possible benefit of the TAP block on obese patients undergoing laparoscopic gastric banding
Applications
Patients undergoing laparoscopic gastric banding may have better quality of postsurgical recovery if they receive a TAP block before the surgical procedure
Terminology
Transversus abdominis block is the application of local anesthetics in the abdominal wall using ultrasound.
Peer review
This manuscript is described as a pilot study but realistically is an underpowered study that if recruitment had been successfully would have realised significant results.
Footnotes
P- Reviewers: Dubost C, McCaulCL, Mukhtar K S- Editor: Zhai HH L- Editor: A E- Editor: Wu HL
Supported by Department of Anesthesiology, Northwestern University
References
- 1.Ohri R, Wang JC, Blaskovich PD, Pham LN, Costa DS, Nichols GA, Hildebrand WP, Scarborough NL, Herman CJ, Strichartz GR. Inhibition by local bupivacaine-releasing microspheres of acute postoperative pain from hairy skin incision. Anesth Analg. 2013;117:717–730. doi: 10.1213/ANE.0b013e3182a00851. [DOI] [PubMed] [Google Scholar]
- 2.Cohen SP, Galvagno SM, Plunkett A, Harris D, Kurihara C, Turabi A, Rehrig S, Buckenmaier CC, Chelly JE. A multicenter, randomized, controlled study evaluating preventive etanercept on postoperative pain after inguinal hernia repair. Anesth Analg. 2013;116:455–462. doi: 10.1213/ANE.0b013e318273f71c. [DOI] [PubMed] [Google Scholar]
- 3.Yuan Y, Wang JY, Yuan F, Xie KL, Yu YH, Wang GL. Glycogen synthase kinase-3β contributes to remifentanil-induced postoperative hyperalgesia via regulating N-methyl-D-aspartate receptor trafficking. Anesth Analg. 2013;116:473–481. doi: 10.1213/ANE.0b013e318274e3f1. [DOI] [PubMed] [Google Scholar]
- 4.Gornall BF, Myles PS, Smith CL, Burke JA, Leslie K, Pereira MJ, Bost JE, Kluivers KB, Nilsson UG, Tanaka Y, et al. Measurement of quality of recovery using the QoR-40: a quantitative systematic review. Br J Anaesth. 2013;111:161–169. doi: 10.1093/bja/aet014. [DOI] [PubMed] [Google Scholar]
- 5.Benn J, Arnold G, Wei I, Riley C, Aleva F. Using quality indicators in anaesthesia: feeding back data to improve care. Br J Anaesth. 2012;109:80–91. doi: 10.1093/bja/aes173. [DOI] [PubMed] [Google Scholar]
- 6.Cook TM, Coupe M, Ku T. Shaping quality: the use of performance polygons for multidimensional presentation and interpretation of qualitative performance data. Br J Anaesth. 2012;108:953–960. doi: 10.1093/bja/aes026. [DOI] [PubMed] [Google Scholar]
- 7.Gardiner S, Rudkin G, Cooter R, Field J, Bond M. Paravertebral blockade for day-case breast augmentation: a randomized clinical trial. Anesth Analg. 2012;115:1053–1059. doi: 10.1213/ANE.0b013e318264ba33. [DOI] [PubMed] [Google Scholar]
- 8.Bertoglio S, Fabiani F, Negri PD, Corcione A, Merlo DF, Cafiero F, Esposito C, Belluco C, Pertile D, Amodio R, et al. The postoperative analgesic efficacy of preperitoneal continuous wound infusion compared to epidural continuous infusion with local anesthetics after colorectal cancer surgery: a randomized controlled multicenter study. Anesth Analg. 2012;115:1442–1450. doi: 10.1213/ANE.0b013e31826b4694. [DOI] [PubMed] [Google Scholar]
- 9.De Oliveira GS, Fitzgerald P, Streicher LF, Marcus RJ, McCarthy RJ. Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg. 2012;115:262–267. doi: 10.1213/ANE.0b013e318257a380. [DOI] [PubMed] [Google Scholar]
- 10.White PF, Zhao M, Tang J, Wender RH, Yumul R, Sloninsky AV, Naruse R, Kariger R, Cunneen S. Use of a disposable acupressure device as part of a multimodal antiemetic strategy for reducing postoperative nausea and vomiting. Anesth Analg. 2012;115:31–37. doi: 10.1213/ANE.0b013e3182536f27. [DOI] [PubMed] [Google Scholar]
- 11.Joshi GP, Ankichetty SP, Gan TJ, Chung F. Society for Ambulatory Anesthesia consensus statement on preoperative selection of adult patients with obstructive sleep apnea scheduled for ambulatory surgery. Anesth Analg. 2012;115:1060–1068. doi: 10.1213/ANE.0b013e318269cfd7. [DOI] [PubMed] [Google Scholar]
- 12.White PF, White LM, Monk T, Jakobsson J, Raeder J, Mulroy MF, Bertini L, Torri G, Solca M, Pittoni G, et al. Perioperative care for the older outpatient undergoing ambulatory surgery. Anesth Analg. 2012;114:1190–1215. doi: 10.1213/ANE.0b013e31824f19b8. [DOI] [PubMed] [Google Scholar]
- 13.Robert M, Denis A, Badol-Van Straaten P, Jaisson-Hot I, Gouillat C. Prospective longitudinal assessment of change in health-related quality of life after adjustable gastric banding. Obes Surg. 2013;23:1564–1570. doi: 10.1007/s11695-013-0914-2. [DOI] [PubMed] [Google Scholar]
- 14.De Oliveira GS, Castro-Alves LJ, Ahmad S, Kendall MC, McCarthy RJ. Dexamethasone to prevent postoperative nausea and vomiting: an updated meta-analysis of randomized controlled trials. Anesth Analg. 2013;116:58–74. doi: 10.1213/ANE.0b013e31826f0a0a. [DOI] [PubMed] [Google Scholar]
- 15.De Oliveira GS, Castro-Alves LJ, Chang R, Yaghmour E, McCarthy RJ. Systemic metoclopramide to prevent postoperative nausea and vomiting: a meta-analysis without Fujii’s studies. Br J Anaesth. 2012;109:688–697. doi: 10.1093/bja/aes325. [DOI] [PubMed] [Google Scholar]
- 16.Petersen PL, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, Mitchell AU, Moeller A, Rosenberg J, Dahl JB, Mathiesen O. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg. 2012;115:527–533. doi: 10.1213/ANE.0b013e318261f16e. [DOI] [PubMed] [Google Scholar]
- 17.Freir NM, Murphy C, Mugawar M, Linnane A, Cunningham AJ. Transversus abdominis plane block for analgesia in renal transplantation: a randomized controlled trial. Anesth Analg. 2012;115:953–957. doi: 10.1213/ANE.0b013e3182642117. [DOI] [PubMed] [Google Scholar]
- 18.Abdallah FW, Halpern SH, Margarido CB. Transversus abdominis plane block for postoperative analgesia after Caesarean delivery performed under spinal anaesthesia? A systematic review and meta-analysis. Br J Anaesth. 2012;109:679–687. doi: 10.1093/bja/aes279. [DOI] [PubMed] [Google Scholar]
- 19.McDermott G, Korba E, Mata U, Jaigirdar M, Narayanan N, Boylan J, Conlon N. Should we stop doing blind transversus abdominis plane blocks? Br J Anaesth. 2012;108:499–502. doi: 10.1093/bja/aer422. [DOI] [PubMed] [Google Scholar]
- 20.Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35:616–617. [PubMed] [Google Scholar]
- 21.Carron M, Guzzinati S, Ori C. Simplified estimation of ideal and lean body weights in morbidly obese patients. Br J Anaesth. 2012;109:829–830. doi: 10.1093/bja/aes368. [DOI] [PubMed] [Google Scholar]
- 22.Macintyre PE, Ready LB. Pharmacology of opioids. In: Acute pain management-a practical guide., editor. 2nd edition. Philadelphia: WB Saunders; 2001. pp. 15–49. [Google Scholar]
- 23.De Oliveira GS, Milad MP, Fitzgerald P, Rahmani R, McCarthy RJ. Transversus abdominis plane infiltration and quality of recovery after laparoscopic hysterectomy: a randomized controlled trial. Obstet Gynecol. 2011;118:1230–1237. doi: 10.1097/AOG.0b013e318236f67f. [DOI] [PubMed] [Google Scholar]
- 24.De Oliveira GS, Ahmad S, Fitzgerald PC, Marcus RJ, Altman CS, Panjwani AS, McCarthy RJ. Dose ranging study on the effect of preoperative dexamethasone on postoperative quality of recovery and opioid consumption after ambulatory gynaecological surgery. Br J Anaesth. 2011;107:362–371. doi: 10.1093/bja/aer156. [DOI] [PubMed] [Google Scholar]
- 25.De Oliveira GS, Fitzgerald PC, Marcus RJ, Ahmad S, McCarthy RJ. A dose-ranging study of the effect of transversus abdominis block on postoperative quality of recovery and analgesia after outpatient laparoscopy. Anesth Analg. 2011;113:1218–1225. doi: 10.1213/ANE.0b013e3182303a1a. [DOI] [PubMed] [Google Scholar]
- 26.Lloret-Linares C, Lopes A, Declèves X, Serrie A, Mouly S, Bergmann JF, Perrot S. Challenges in the optimisation of post-operative pain management with opioids in obese patients: a literature review. Obes Surg. 2013;23:1458–1475. doi: 10.1007/s11695-013-0998-8. [DOI] [PubMed] [Google Scholar]
- 27.Kaw R, Chung F, Pasupuleti V, Mehta J, Gay PC, Hernandez AV. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth. 2012;109:897–906. doi: 10.1093/bja/aes308. [DOI] [PubMed] [Google Scholar]
- 28.Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108:768–775. doi: 10.1093/bja/aes022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aldenkortt M, Lysakowski C, Elia N, Brochard L, Tramèr MR. Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br J Anaesth. 2012;109:493–502. doi: 10.1093/bja/aes338. [DOI] [PubMed] [Google Scholar]
- 30.Fawcett WJ, Mythen MG, Scott MJ. Enhanced recovery: more than just reducing length of stay? Br J Anaesth. 2012;109:671–674. doi: 10.1093/bja/aes358. [DOI] [PubMed] [Google Scholar]
- 31.Wongyingsinn M, Baldini G, Stein B, Charlebois P, Liberman S, Carli F. Spinal analgesia for laparoscopic colonic resection using an enhanced recovery after surgery programme: better analgesia, but no benefits on postoperative recovery: a randomized controlled trial. Br J Anaesth. 2012;108:850–856. doi: 10.1093/bja/aes028. [DOI] [PubMed] [Google Scholar]
- 32.Grady MV, Mascha E, Sessler DI, Kurz A. The effect of perioperative intravenous lidocaine and ketamine on recovery after abdominal hysterectomy. Anesth Analg. 2012;115:1078–1084. doi: 10.1213/ANE.0b013e3182662e01. [DOI] [PubMed] [Google Scholar]
- 33.De Oliveira GS, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg. 2012;114:424–433. doi: 10.1213/ANE.0b013e3182334d68. [DOI] [PubMed] [Google Scholar]
- 34.Michelet D, Andreu-Gallien J, Bensalah T, Hilly J, Wood C, Nivoche Y, Mantz J, Dahmani S. A meta-analysis of the use of nonsteroidal antiinflammatory drugs for pediatric postoperative pain. Anesth Analg. 2012;114:393–406. doi: 10.1213/ANE.0b013e31823d0b45. [DOI] [PubMed] [Google Scholar]
- 35.Krenk L, Jennum P, Kehlet H. Sleep disturbances after fast-track hip and knee arthroplasty. Br J Anaesth. 2012;109:769–775. doi: 10.1093/bja/aes252. [DOI] [PubMed] [Google Scholar]
- 36.de Silva E, Plaat F. Postoperative analgesia - still failing to meet the standard. Anaesthesia. 2012;67:801–802. doi: 10.1111/j.1365-2044.2012.07210.x. [DOI] [PubMed] [Google Scholar]
- 37.Sinha A, Jayaraman L, Punhani D. Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg. 2013;23:548–553. doi: 10.1007/s11695-012-0819-5. [DOI] [PubMed] [Google Scholar]
- 38.Gravante G, Castrì F, Araco F, Araco A. A comparative study of the transversus abdominis plane (TAP) block efficacy on post-bariatric vs aesthetic abdominoplasty with flank liposuction. Obes Surg. 2011;21:278–282. doi: 10.1007/s11695-010-0203-2. [DOI] [PubMed] [Google Scholar]


