Abstract
Background
This study was conducted to examine the clinical usefulness and efficacy of endoscopic curettage on benign bone tumor.
Methods
Thirty-two patients (20 men and 12 women) with benign bone tumor were included in the study. The patients were aged between five and 76 years; the mean follow-up period was 27.05 months (range, 9.6 to 39.9 months). The primary sites include simple bone cyst (9 cases), fibrous dysplasia (6 cases), enchondroma (5 cases), non-ossifying fibroma (4 cases), bone infarct (3 cases), aneurysmal bone cyst (1 case), chondroblastoma (1 case), osteoblastoma (1 case), intraosseous lipoma (1 case), and Brodie abscess (1 case). A plain radiography was performed to assess the radiological recovery. Radiological outcomes, including local recurrence and bone union, were evaluated as excellent, good, poor, and recurred.
Results
In our series, there were 27 cases (84.4%) of good or better outcomes, six cases (18.8%) of complications (4 local recurrence, 1 wound infection, and 1 pathologic fracture).
Conclusions
Our results showed that endoscopic curettage and bone graft had a lower rate of recurrence and a higher cure rate in cases of benign bone tumor. It can, therefore, be concluded that endoscopic curettage and bone graft might be good treatment modalities for benign bone tumors.
Keywords: Endoscopic curettage, Benign bone tumor
Benign bone tumor is a typical disease encountered in the field of orthopedic surgery. As one of the palliative treatments, invasive curettage of the lesion has been widely used.1) It is unavoidable, however, that palliative curettage is extremely invasive to soft tissue and the cortical bone in the lesions depending on the size of lesions. It is thus disadvantageous in that it may lead to various complications such as delayed union or bleeding, postoperative fracture due to a loss of the cortical bone and delayed wound healing and recovery at the operated sites.2-4) To reduce these undesirable side effects, Stricker5) first reported on endoscopic curettage in 1995. In 1999, Bonnel et al.6) reported that endoscopic curettage and bone graft were performed for simple bone cyst of the calcaneus. Thereafter, several authors have confirmed an excellent profile of efficacy for endoscopic curettage. In Korea, however, there is a dearth of studies evaluating the treatment. Most reports have been made regarding clinical cases (case studies). A comparative analysis of other types of bone tumor has been performed only in a limited scope.
Based on the above background, we examined the clinical usefulness of endoscopic curettage, one of the non-invasive treatment modalities, and assessed which benign bone tumors could be effectively treated with endoscopic curettage.
METHODS
Patients Selection
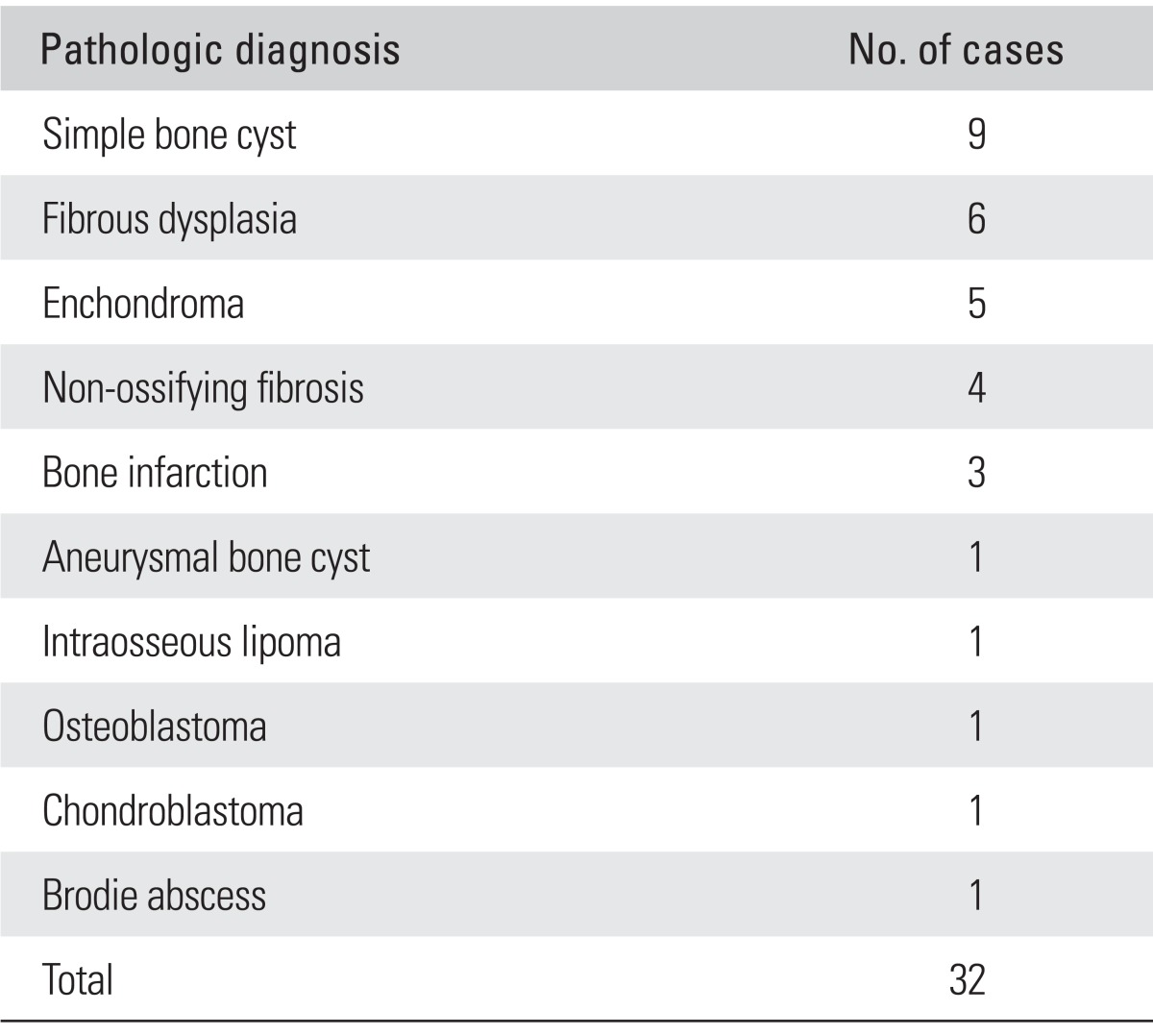
The current study included 32 patients with a diagnosis of benign bone tumor who were followed up for a mean period of 27.05 months (range, 9.6 to 39.9 months) after undergoing endoscopic curettage and bone graft at Kosin University Gospel Hospital during a period ranging from December 2007 to September 2010. The primary sites include nine cases of simple bone cyst, six cases of fibrous dysplasia, five cases of enchondroma, four cases of non-ossifying fibroma, three cases of bone infarct, one case of aneurysmal bone cyst, one case of chondroblastoma, one case of osteoblastoma, one case of intraosseous lipoma and one case of Brodie abscess (Table 1). The mean age of the study participants was 26 years (range, 5 to 76 years). Of the 32 study participations, 20 were men and 12 were women.
Table 1.
Pathologic Diagnosis
Surgical Methods
There were two surgical methods performed: endoscopic curettage and bone graft. To restore the bone defects, bone graft was performed for 30 cases. Of the 30 cases, 26 underwent allograft transplantation and four did autogenous bone graft. Of the 32 cases, 26 received an injection of platelet-rich plasma concomitantly with bone graft for the purposes of promoting the bone union.
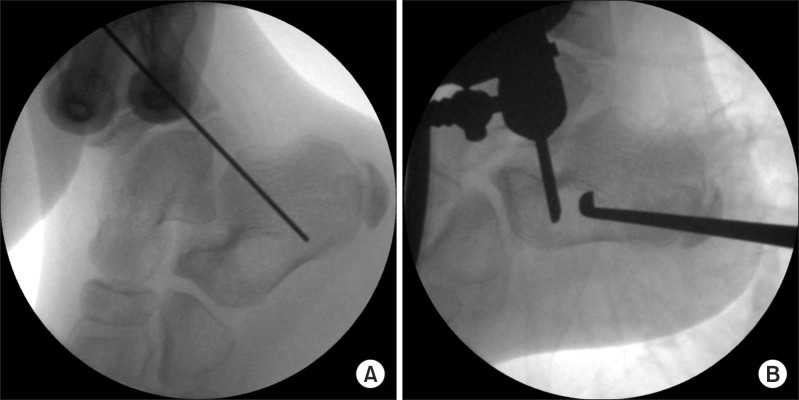
For the surgical methods, patients were placed in appropriate positions, such as a supine or lateral one, depending on the location of the bone lesions under general anesthesia or spinal one in the operation room. The margin of benign bone lesion was marked on the skin under the guidance of an X-ray amplifier. Thereafter, to ensure unnecessary damage to the normal anatomical structures, the location of a portal was determined. Through an incision, the anterior portal was created for endoscopy using a 2.0 mm K-wire. After the appropriate location of a portal was determined in other areas, the lesions were examined through the first portal. Meanwhile, a 4.0 mm 30 angled arthroscope was inserted (Fig. 1).
Fig. 1.
(A) Intraoperative radiograph of left calcaneus shows osteolytic bony leision and guide K-wire. (B) Intraoperative radiograph of left calcaneus shows curettage of simple bone cyst under endoscopic guidance.
The posterior portal was created, by which a curret, a shaver, or a bur were inserted (Fig. 2). Thus, the endosteum and bony septa of benign bone lesion were completely removed. For detection of a blind spot, the surgical procedure was performed by reversing a portal between an endoscope and a curet. If there was an insufficient visual field, the additional portals were created. The degree of curettage of the lesion was directly confirmed on gross examination based on an endoscopy, which was also confirmed using an X-ray amplifier and based on hemorragic findings. Following the curettage of benign bone lesion, the bone graft was performed using the autologous bone or bone prosthesis which were extracted from the ipsilateral ilium. To confirm the degree of bone graft, a radiogaphs or an arthroscopy were performed. Each incision site was simply sutured.
Fig. 2.

(A) Endoscopic image of simple bone cyst which is seen as a soft white tissue. (B) Endoscopic image shows curettage of simple bone cyst under endoscopic guidance. (C) Endoscopic image after thorough crettage of the tumor: only normal bone is seen in the cavity.
Evaluation Method
The timing of the determination of the bone fusion was defined as the period where the radiological changes appeared and these changes include those in the morphology of bone trabeculae between the host bone and the grafted bone and a loss of the margin. Also in the current study, at the time point where the bone marrow cavity achieved a recovery with the resorption of the grafted autologous bone and the formation of new bones, there were changes in the morphology of the bone trabeculae between the autologous bone and the host one and a loss of the margin began to occur on a plain radiography at a follow-up when there was a lack of the evidences demonstrating the recurrence of lesions or bone fracture, the time point of the autologous bone fusion was determined (Fig. 3).
Fig. 3.
Simple bone cyst of the calcaneus in a 12-year-old boy. (A) Preoperative lateral radiograph shows bone loss in calcaneus. (B) Immediate postoperative radiograph taken after curettage and defect filling with allobone graft. (C) At postoperative 4 weeks, bone graft was partially resorbed. (D) At postoperative 3 months, bony trabeculation filled the preoperative bone defect. (E) At postoperative 6 months, simple bone cyst was completely resorbed.
Postoperative outcomes were evaluated based on the radiological bone fusion. That is, postoperative outcomes were classified into four types: excellent (a complete disappearance of the bone lesion following the surgery and the total replacement of the grafted bones with new bones at a follow-up); good (the residual presence of bone lesion but the replacement of most of the grafted bones with new ones with a sufficient disappearance of bone lesion); poor (the residual presence of the bone lesion but no changing and no turning into the recurred state during the follow-up period); and recurred (the recurrence of lesions during the follow-up period). Both excellent and good cases were determined to be effective for the treatment and cure rate.
RESULTS
Radiological Outcomes
Regarding the outcomes of radiological recovery of benign bone tumor, there were 21 excellent cases (65.6%), six good cases (18.8%), one poor case (3.1%), and four recurred cases (12.5%). These results indicate that there were 27 good or better cases (84.4%).
Regarding the nine cases of simple bone cyst, there were seven excellent cases (77.8%), one good case (11.1%), and one recurred case (11.1%). Of the six total fibrous dysplasia cases, there were four excellent cases (66.7%), one good case (16.7%), and one recurred case (16.7%). Of the five total cases of enchondroma, all five were considered excellent (100%); there were no recurrences in this series. Of the four total cases of non-ossifying fibroma, two cases were considered excellent (50%); there were no recurrences in this series. Of the three cases of bone infarct, there was one excellent case (33.3%), one good case (33.3%), and one poor case (33.3%); there were no recurrences in this series. In addition, there were one case each of aneurysmal bone cyst, chondroblastoma, osteoblastoma, intraosseous lipoma and Brodie bone abscess. There was a recurrence in the aneurysmal bone cyst case and osteoblastoma case. Brodie bone abscess reflected good treatment outcomes. All other cases were found to have excellent outcomes (Tables 2 and 3).
Table 2.
Radiological Outcomes
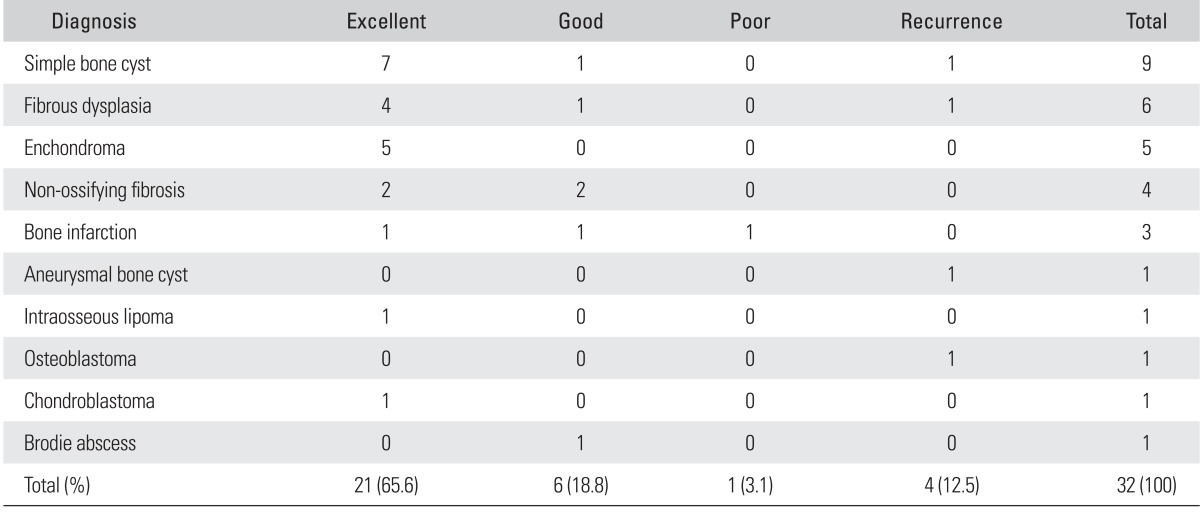
Table 3.
Summary of Study Cases
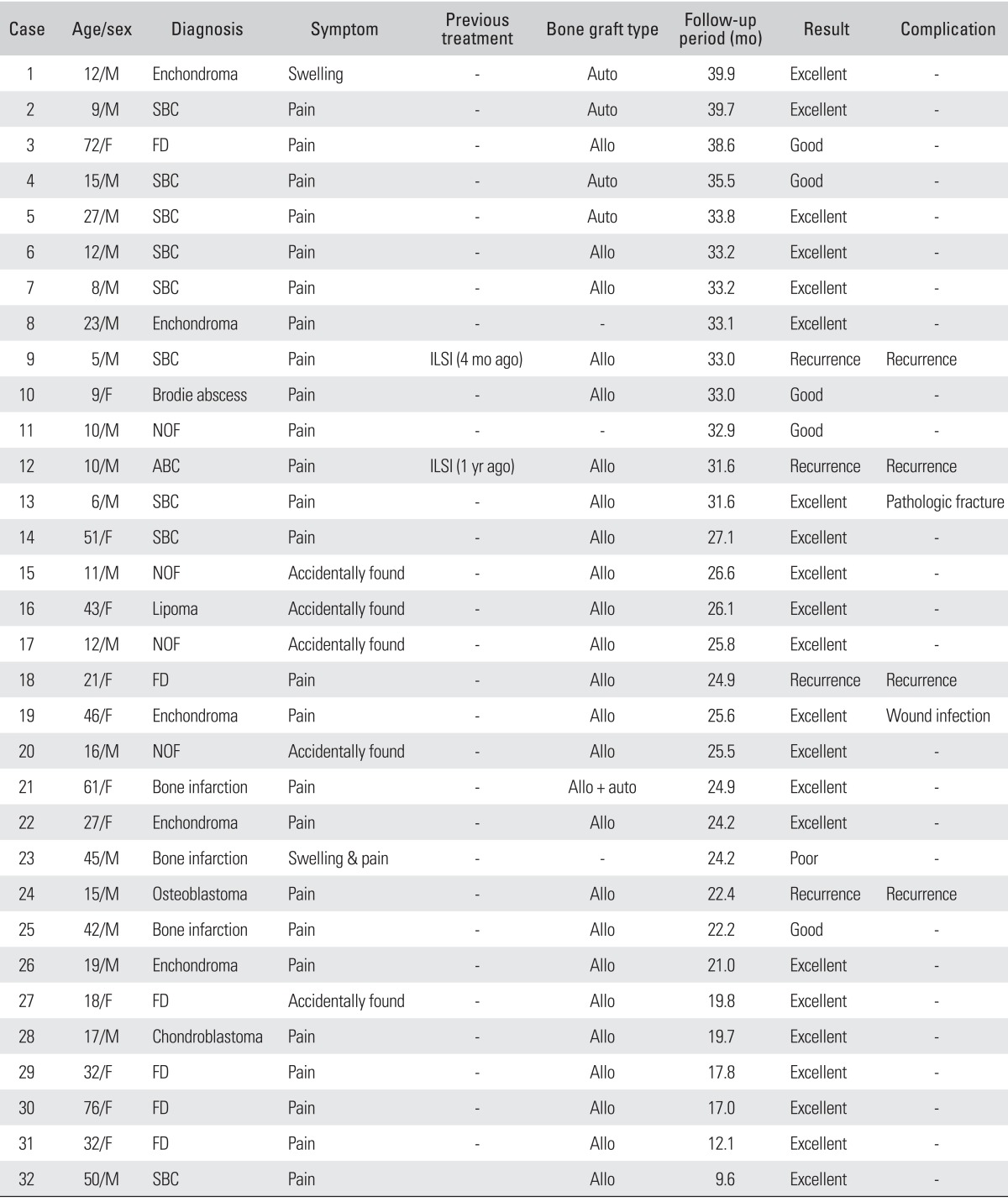
Auto: autogenous, SBC: simple bone cyst, FD: fibrous dysplasia, Allo: allogeneic, ILSI: intralesional steroid injection, NOF: non-ossifying fibrosis, ABC: aneurysmal bone cyst.
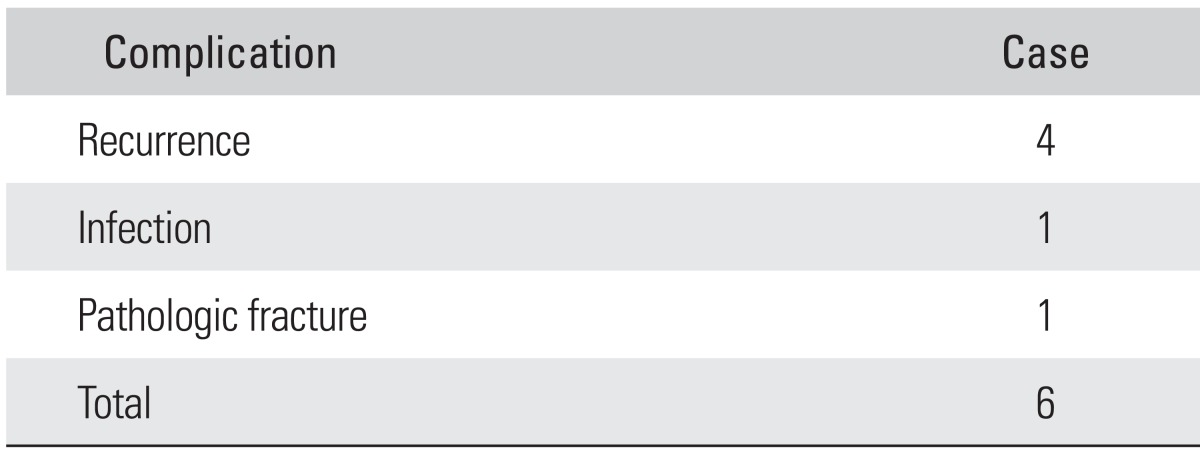
Complications
Regarding postoperative complications, there were four cases of recurrences (simple bone cyst, fibrous dysplasia, aneurysmal bone cyst, osteoblastoma), one case of pathological fracture, and one case of infections at the operated site. That is, a total of six cases of complications occurred (Table 4). The open curettage was performed for all of the recurrent cases. Pathologic fracture was non-displaced and incomplete. So conservative treatment with the casting was performed and bone union was achieved after 10 weeks. For the treatment of the portal site wound infection, antibiotics of second generation cephalosporin were used.
Table 4.
Cases with Complications
DISCUSSION
Treatments of the benign bone tumor are mainly dependent on the curettage and bone graft. It has been reported, however, that palliative curettage remains problematic in that it is possible recurrence might occur due to the residual presence of tumor tissue in the removal of the lesions.1,4) For a complete removal of the lesions, defects of the cortical bone have been inevitable. In order to resolve this, an endoscopic curettage has been reported. An endoscopic curettage is advantageous in that the treatment makes it possible not only to achieve a complete removal of the tissue of the lesion through an expanded operative field, but also minimizes damage to the adjacent soft tissue and the periosteum of cortical bone. In our series, we performed an endoscopic curettage through a minimal incision and a smaller cortical window. Thus, we minimized defects of the cortical bone, effectively removed the tissue of the lesion, and could clearly confirm where there was a residual presence of the tissue of the lesion.
In 2007, Dietz et al.7) described the advantages of an endoscopic curettage, while mentioning an endoscopic-assisted resection of enchondroma of the phalanges. According to the above authors, advantages include the following: (1) Accurate assessment was possible with the direct examination of bone marrow cavity; (2) Endoscopy is useful in making an accurate assessment of the curettage. Thus, the multiplicity, blind spot and excessive curettage could be avoided; (3) A complete removal was possible with an endoscopy. Thus, the rate of recurrence could be decreased. Also in the current study, the bone marrow cavity could be directly examined. This led to an accurate assessment of the types and status of lesion and the degree of curettage during the surgical procedure. A complete removal could therefore be confirmed on gross examination.
An endoscopic curettage requires only two smaller incision windows. It is therefore advantageous in that it needs a smaller incision site, lower levels of bleeding, and causes less damage to the bone and adjacent soft tissue compared with invasive curettage. From an aesthetic perspective, endoscopic curettage has an excellent profile of effects. Moreover, because a thinner periosteum causes minimal injury, it helps to maintain the bone's strength. It is eventually advantageous in that it achieves a prompt rehabilitation and produces an excellent profile of range of motion. In addition, it is also advantageous in that it can obtain tendoscopic images through an access to the lesions during the curettage. Any invisible parts can be examined using an angular endoscope. However, endoscopic curettage is not an easily learned technique; a learning curve is required to master the technique. In addition, there are disadvantages if the technique is suddenly converted to invasive surgical modalities; this is because: problems due to such intraoperative occurrences as the leakage of intravascular fluid and the edema of soft tissue.
Prevalence of simple bone cyst was the highest in the current study. The rate of postoperative recurrence has been reported to range from 17% to 50%,8) which is dependent on the location of lesions and the types of treatment modalities. In regard to the treatment outcomes of curettage and bone graft, the rate of healing has been reported to range from 50%9) to 88%.10) According to Jaffe and Dunham11) and Catier et al.,12) both the curettage and bone graft were effective in preventing the weakness of mechanical strength and the bone deformity during the weight-bearing phase. These authors also noted that they experienced a prompt treatment effect. According to Baek et al.,13) of the study's 36 patients who underwent curettage and bone graft including the bone marrow, 30 (83.3%) had improved or better outcomes. It has been reported, however, that both palliative curettage and bone graft are disadvantageous in that they cause iatrogenic pathological fracture, damages to the growth plate, infections, and a higher rate of recurrence of 18%-50%.14,15)
In the current study, of nine patients with benign bone cyst who underwent endoscopic curettage, one (11.1%) presented with recurrent findings. Overall, our clinical series of patients had a cure rate of 88.9%. Furthermore, the radiological bone union was also found in eight patients (88.9%) except for those who had a recurrence. In these patients, the treatment outcomes were classified as good or better.
Fibrous dysplasia is a benign bone disease that is assumed to be a developmental anomaly of the bone. Nakashima et al.16) reported eight cases of fibrous dysplasia that occurred in the femoral neck where the successful treatment outcomes were obtained using a curettage and the autologous bone graft. According to Harris et al.,17) following a comparison between nine cases for which the curettage and the autologous bone graft were performed and one case for which the internal fixation was performed following the autologous bone graft in patients with a single lesion of fibrous dysplasia, the treatment outcomes were relatively successful. Guille et al.18) reported that the successful treatment outcomes were obtained with the use of curettage and autologous bone graft in three of four patients with a single lesion occurring in the proximal femur. According to Bae et al.,19) of 23 patients who were treated with a curettage and the autologous bone graft, five had a recurrence of the lesion. While stating that these outcomes are due to an insufficient curettage, they put an emphasis of the importance of a meticulous curettage. In the current study, the surgical procedure was performed for a total of six patients, recurrence occurred in one case (16%). Assessments showed that five patients (83.3%) had improved or better outcomes.
Enchondroma is a benign tumor that accounts for 90% of total cases of bone tumors occurring in the hand. It is also a benign tumor where the soft tissue grows on the medial side of the bone.20) It is generally known that the rate of recurrence following the curettage is 2%-4.5%.21) According to Tordai et al.,22) the recurrence occurred at a rate of 2% (1/46). This author noted that recurrence occurred because of insufficient curettage. In the current study, of five total patients with enchondroma who underwent endoscopic curettage, no patients experienced had a recurrence. Postoperative radiological and clinical assessments showed that all five cases (100%) had excellent outcomes.
Non-ossifying fibroma is a tumor which is composed of fibrous connective tissue. Its histopathological characteristics are identical to those of the defects of fibrous cortical bone. Regarding the treatments for non-ossifying fibroma, many authors including Jaffe and Lichenstein23) maintained that curettage or bone resection should be performed. According to Compere and Coleman24) recommended the use of bone graft, as well as the curettage in cases of larger-sized lesion or those in which there is a concurrent presence of pathological fracture. In the current study, the endoscopic curettage and bone graft were performed for a total of four cases of non-ossifying fibroma. Of the four cases, two cases (50%) had excellent outcomes and two cases (50%) had good outcomes. That is, all cases (100%) had good or better outcomes. There were no recurrences in this series.
In the 32 cases of benign bone tumor for which the endoscopic curettage and bone graft were performed as one of the treatment modalities for benign bone tumor, radiological assessments showed a prompt recovery and a lower incidence of complications. Functional pain was also promptly resolved from postoperative month 1-2. Excluding four cases of recurrence, there were no cases where revision surgery was needed. Our clinical series of patients had relatively good treatment outcomes.
The overall recurrence rate was 12.5%. On radiological and clinical assessments, the overall recurrence rate was 84.4%. These results indicate that the recurrence rate was also in agreement with good treatment outcomes. Considering the recurrence rate and cure rate of palliative curettage, our results confirmed that endoscopic curettage and bone graft are treatment modalities that are effective for the treatment of benign bone tumor.
As benign bone tumors had good treatment outcomes. There were simple bone cyst (recurrence rate, 11.1% and cure rate, 88.9%), fibrous dysplasia (recurrence rate, 16.7% and cure rate 83.3%), enchondroma (recurrence rate, 0% and cure rate, 100%), non-ossifying fibroma (recurrence rate, 0% and cure rate, 100%).
In the current study, there were numerous limitations; it was difficult to assess the effects of surgery and to compare the treatment efficiency with conventional types of treatment modalities through multivariate analysis due to an attenuated sample size. That is, there were not larger-sized patient groups available to compare for each type of benign bone tumors. In addition, because there are no established criteria for the locations, the size and types of lesion for procedure method, it would be necessary to establish the surgical indications depending on the diagnosis and location of benign bone tumor. It is also presumed that the local recurrence due to an incomplete curettage should be resolved and further discussed.
In cases of benign bone tumor, such as simple bone cyst, fibrous dysplasia, enchondroma and non-ossifying fibroma, endoscopic curettage and bone graft had a lower rate of recurrence and a higher cure rate as compared with conventional types of treatment modalities. Of these, enchondroma had the best treatment outcomes. As the treatment methods for benign bone tumor, endoscopic curettage and bone graft might be one of the good treatment modalities.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Damien CJ, Parsons JR. Bone graft and bone graft substitutes: a review of current technology and applications. J Appl Biomater. 1991;2(3):187–208. doi: 10.1002/jab.770020307. [DOI] [PubMed] [Google Scholar]
- 2.Csizy M, Buckley RE, Fennell C. Benign calcaneal bone cyst and pathologic fracture--surgical treatment with injectable calcium-phosphate bone cement (Norian): a case report. Foot Ankle Int. 2001;22(6):507–510. doi: 10.1177/107110070102200610. [DOI] [PubMed] [Google Scholar]
- 3.Mainard D, Galois L. Treatment of a solitary calcaneal cyst with endoscopic curettage and percutaneous injection of calcium phosphate cement. J Foot Ankle Surg. 2006;45(6):436–440. doi: 10.1053/j.jfas.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Wulle C. On the treatment of enchondroma. J Hand Surg Br. 1990;15(3):320–330. doi: 10.1016/0266-7681_90_90012-s. [DOI] [PubMed] [Google Scholar]
- 5.Stricker SJ. Extraarticular endoscopic excision of femoral head chondroblastoma. J Pediatr Orthop. 1995;15(5):578–581. [PubMed] [Google Scholar]
- 6.Bonnel F, Canovas F, Faure P. Treatment of a simple bone cyst of the calcaneus by endoscopic curettage with cancellous bone injection. Acta Orthop Belg. 1999;65(4):528–531. [PubMed] [Google Scholar]
- 7.Dietz JF, Kachar SM, Nagle DJ. Endoscopically assisted excision of digital enchondroma. Arthroscopy. 2007;23(6):678.e1–678.e4. doi: 10.1016/j.arthro.2005.12.063. [DOI] [PubMed] [Google Scholar]
- 8.Rockwood CA, Wilkins KE, Beaty JH, editors. Fractures in children. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 1996. pp. 167–320. [Google Scholar]
- 9.Wilber MC, Hyatt GW. Bone cysts: results of surgical treatment in 200 cases. J Bone Joint Surg Am. 1960;42(5):879. [Google Scholar]
- 10.Spence KF, Jr, Bright RW, Fitzgerald SP, Sell KW. Solitary unicameral bone cyst: treatment with freeze-dried crushed cortical-bone allograft: a review of one hundred and forty-four cases. J Bone Joint Surg Am. 1976;58(5):636–641. [PubMed] [Google Scholar]
- 11.Jaffe KA, Dunham WK. Treatment of benign lesions of the femoral head and neck. Clin Orthop Relat Res. 1990;(257):134–137. [PubMed] [Google Scholar]
- 12.Catier P, Bracq H, Canciani JP, Allouis M, Babut JM. The treatment of upper femoral unicameral bone cysts in children by Ender's nailing technique. Rev Chir Orthop Reparatrice Appar Mot. 1981;67(2):147–149. [PubMed] [Google Scholar]
- 13.Baek SG, Oh CW, Jeon IH, Min WK, Park IH. Comparison of results by its location and treatment modality of the simple bone cyst. J Korean Musculoskelet Transplant Soc. 2006;6(2):88–97. [Google Scholar]
- 14.Yandow SM, Lundeen GA, Scott SM, Coffin C. Autogenic bone marrow injections as a treatment for simple bone cyst. J Pediatr Orthop. 1998;18(5):616–620. doi: 10.1097/00004694-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Neer CS, Francis KC, Johnston AD, Kiernan HA., Jr Current concepts on the treatment of solitary unicameral bone cyst. Clin Orthop Relat Res. 1973;(97):40–51. doi: 10.1097/00003086-197311000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Nakashima Y, Kotoura Y, Nagashima T, Yamamuro T, Hamashima Y. Monostotic fibrous dysplasia in the femoral neck: a clinicopathologic study. Clin Orthop Relat Res. 1984;(191):242–248. [PubMed] [Google Scholar]
- 17.Harris WH, Dudley HR, Jr, Barry RJ. The natural history of fibrous dysplasia: an orthopaedic, pathological, and roentgenographic study. J Bone Joint Surg Am. 1962;44(2):207–233. [PubMed] [Google Scholar]
- 18.Guille JT, Kumar SJ, MacEwen GD. Fibrous dysplasia of the proximal part of the femur: long-term results of curettage and bone-grafting and mechanical realignment. J Bone Joint Surg Am. 1998;80(5):648–658. doi: 10.2106/00004623-199805000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Bae DK, Rhee YG, Kim SK, Son YL. Clinical analysis of fibrous dysplasia. J Korean Orthop Assoc. 1992;27(5):1418–1425. [Google Scholar]
- 20.Kang ES, Roh KJ, Yoo JD. Comparative study of the simple curettage and the curettage with bonegraft in enchondroma of the hand. J Korean Orthop Assoc. 1997;32(1):156–162. [Google Scholar]
- 21.Kuur E, Hansen SL, Lindequist S. Treatment of solitary enchondromas in fingers. J Hand Surg Br. 1989;14(1):109–112. doi: 10.1016/0266-7681(89)90029-6. [DOI] [PubMed] [Google Scholar]
- 22.Tordai P, Hoglund M, Lugnegard H. Is the treatment of enchondroma in the hand by simple curettage a rewarding method? J Hand Surg Br. 1990;15(3):331–334. doi: 10.1016/0266-7681_90_90013-t. [DOI] [PubMed] [Google Scholar]
- 23.Jaffe HL, Lichtenstein L. Non-osteogenic fibroma of bone. Am J Pathol. 1942;18(2):205–221. [PMC free article] [PubMed] [Google Scholar]
- 24.Compere CL, Coleman SS. Nonosteogenic fibroma of bone. Surg Gynecol Obstet. 1957;105(5):588–598. [PubMed] [Google Scholar]