Abstract
Objective
Universal mental health screening in pediatric primary care is recommended, but studies report slow uptake and low rates of patient follow-through after referral to specialized services. This review examined possible explanations related to the process of screening, focusing on how parents and youth are engaged and how providers evaluate and use screening results.
Method
Narrative synthesis following a systematic review of three databases (plus follow-up of citations, expert recommendations, and checks for multiple publications about the same study). Searching identified 1,188 titles; 186 full-text papers were reviewed. Two authors extracted data from 45 papers meeting inclusion criteria.
Results
Published studies report few details about how mental health screens were administered including how clinicians explain their purpose or confidentiality, or whether help was provided for language, literacy, or disability problems. Though not addressed directly in the studies reviewed, uptake and detection rates appeared to vary with means of administration. Screening framed as universal, confidential, and intended to optimize attention to patient concerns increased acceptability. Studies said little about how providers were taught to explore screen results. Screening increased referrals, but many still followed negative screens, in some cases because of parent concerns apparently not reflected by screen results but possibly stemming from screen-prompted discussions.
Conclusions
Little research has addressed the process of engaging patients in mental health screening in pediatric primary care or how clinicians can best use screening results. The literature does offer suggestions for better clinical practice and research that may lead to improvements in uptake and outcome.
Keywords: mental health, patient engagement, pediatrics, primary care, screening
Introduction
Much evidence points to a gap between the prevalence of child and adolescent mental health problems and the amount and timeliness of treatment received.1, 2 Universal screening in pediatric primary care has been proposed as a way to detect and systematically address mental health care needs. Screening and initial treatment of mental health problems are recommended by the American Academy of Pediatrics’ Task Force on Mental Health, and the US Preventive Services Task Force recommends screening for adolescent depression.3, 4 The 2010 Patient Protection and Affordable Care Act mandates that commercial health plans offer depression screening,5 while Medicaid’s Early and Periodic, Screening, Diagnosis, and Testing (EPSDT) requires mental health assessment of all covered children.6 However, to date, screening remains far from universal,7–9 and mental health service follow-up rates after a positive result are reported to be low.10–12 While there are many potential explanations for these disappointing results, including difficulty coordinating with other screening initiatives,13 the mechanics of and compensation for administration,14, 15 and limited availability of follow-up treatment,15–18 other explanations, may involve how screening has been implemented.
One set of potential difficulties with implementation centers on how screens are presented to youth and families. Universal mental health screening addresses conditions that are particularly stigmatized and subject to cultural variation in symptomatology, threshold for treatment, and even legitimacy as diagnostic entities.19 The appropriateness of mental health screening in general medical settings may not be universally accepted by patients or even providers. In mental health screening, respondents must actively collaborate to disclose potentially sensitive information,20 and must decide whether what they are experiencing matches the questions and response categories on the screener.21, 22 Ultimately, respondents can credibly assert the existence of a problem even if the screen does not detect it, or vice versa.
A second set of potential difficulties relates to the way initial screening results are used by front-line clinicians. Screening programs choose their initial tests and cut-points to balance the risk of missing cases with the burden (on both clinicians and patients) of subsequent assessments needed to confirm a diagnosis.23 Programs normally include plans for these subsequent assessments and figure them into the effort needed for implementation.24, 25 While many brief instruments have been validated for detecting child mental health conditions,26–30 their psychometric properties make them unsuitable for use as universal screens without a deliberate follow-up step. For example, the Pediatric Symptom Checklist (PSC), the Strengths and Difficulties Questionnaire (SDQ), and the Patient Health Questionnaire (PHQ) have positive predictive values of 50% or less at the prevalence rates found in well-child visits.31–34 The PSC and SDQ have negative predictive values of about 90% at well-child visit prevalence rates, so even negative results may need at least brief validation of a child’s low-risk status. In addition, broad-band instruments such as the PSC and SDQ yield only a risk of having some disorder, requiring additional steps to refine a working diagnosis before a treatment plan can be developed. The PSC and SDQ have subscales that point toward a particular group of problems, but these distinctions may not be reliable across populations.30, 35
The purpose of this paper is to review available information about how families and youth are currently engaged in mental health screening programs in primary care, and how providers evaluate and use the information collected from screens. Improving the fit between screening practices and the nature of mental health screening could be one path toward improving mental health screening outcomes.
Method
Search Strategy
PubMed, PsycInfo, and EMBASE were searched for studies of universal mental health screening in pediatric primary care in developed countries. A research librarian and an expert in systematic reviews were consulted on database selection and search term development. Terms were identified using each database’s controlled vocabulary and other key words within 4 domains: mental health, children, primary care, and screening. Three authors (K.F., L.W., R.Z.) came to consensus on the final terms for each database. Searches combined these terms using “AND” logic. In addition to the database searches, studies were identified through reviewing citations of key papers. No restrictions were placed on start date; the end date for inclusion was through May 2012. Once a final set of papers had been selected, an additional hand search was made for papers related to the same studies that might contain additional information on the screens or their use.36
Study Selection and Data Abstraction
Three authors (K.F., L.W., R.Z.) developed selection criteria with a broad view of primary care that also included studies of school-based services and low-acuity services within pediatric emergency departments. A key criterion was that screening was administered systematically to patients attending primary care visits. Psychometric validation studies and epidemiological studies were excluded. Studies of attitudes toward screening were included as long as the participants had actually experienced screening and were not responding to hypothetical scenarios. Studies were excluded if they did not involve children or youth or examined only screening for substance abuse or developmental delay. No exclusions were made based on research design or language. One author (R.Z.) reviewed all titles and abstracts generated through the formal database searches according to these criteria. She then retrieved the full text for the selected papers and formally coded each article for inclusion in the review. In unclear cases, 2 or more authors reviewed the paper and reached consensus on whether to include it.
Data abstraction followed PRISMA guidelines.37 The extraction tool addressed the 2 main potential problems with screening implementation discussed above. To gather information about approaches to engaging patients in the screening process, including addressing concerns about stigma, descriptions were noted of by whom and how screens were presented to families, if and how issues of confidentiality were discussed, and the type of assistance offered while completing the screener. To gather information about plans for second stage evaluation of screening results, descriptions were noted of how clinicians were taught or supported in scoring instruments, interpreting results, and using results in clinical decision making. Within these 2 major areas, sub-areas emerged during analysis. When present, data on how the factors studied related to rates of participation in screening or to visit process or outcome were also extracted. Each paper was initially abstracted by a single author and then checked by a second author. When a single study was represented by multiple papers, we merged information from the different papers unless it was explicitly stated that methods differed across the elements of interest. No attempt was made to rate the strength of study methods. The heterogeneity of study designs and measures precluded a formal meta-analysis. The results presented here represent a narrative synthesis of the extracted data. The online supplement to this paper includes a sample search strategy from one of the databases (Pubmed) (Supplement 1, available online), detailed tables (Tables S1 and S2, available online) summarizing abstracted data, and the PRISMA checklist of the search process (Table S3, available online).
Results
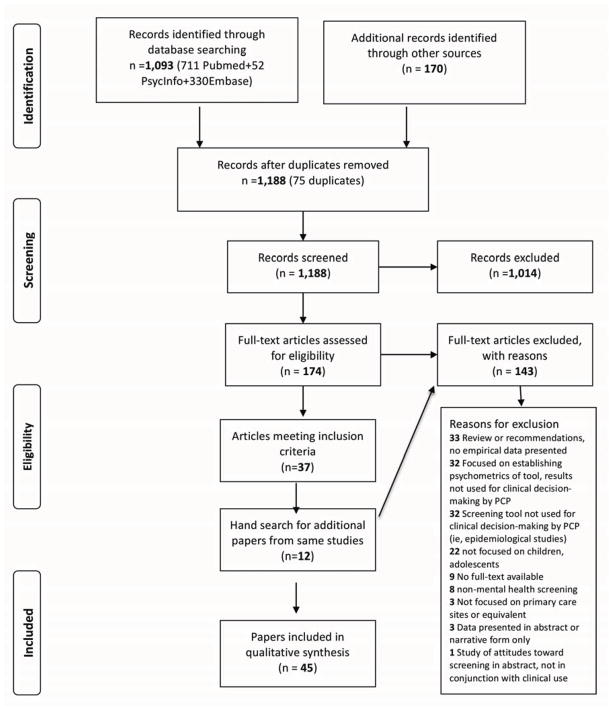
Initial searches produced 1,263 titles of possible relevance (Figure 1). Of these, we screened the 1,188 unique titles and abstracts. Review of these titles and abstracts, plus searches for papers possibly related to those found to be in range, resulted in a preliminary review of 186 full-text articles. The final narrative synthesis included 45 papers describing 38 studies. The most common reasons for exclusion after full-text review were that the paper was a review article without original data (n=33) or an epidemiologic (n=32) or psychometric (n=29) study without information about clinical use. The 38 studies synthesized spanned nearly 4 decades from 1976 to 2012, though 31 studies (35 papers) were published between 2002 and 2012. Twenty-five took place in primary care settings, 6 in emergency departments, and 1 entirely and another partly in school-based sites. One study was conducted among children in foster care, and 2 others among children receiving a variety of ambulatory services. One study was a survey of parents who had used primary care services for children with mental health problems, and another compiled state data on primary care mental health screening.9, 38 Of the 36 studies that described a single screening program, 11 involved only screens completed by parents, while 22 included screening completed by youth themselves and 3 by either parents or youth depending on age.
Figure 1.
Literature search flow diagram.
Most (n=21) of the studies were observational, examining either systematic or convenience samples of patients who underwent screening. Nine conducted pre–post comparisons of screening trials or programs.39–47 Two studies compared different timing of feedback of screening results to providers,10, 48 and one compared screening to providers asking the same questions as part of the visit.49 One study was part of a randomized trial of depression treatment, but all study participants were similarly screened.50 Only one study randomized parents to complete a screen versus usual care.51 Table 1 presents a summary of the settings and instruments used, with additional details about the populations and data elements extracted presented in Tables S1 and S2, available online.
Table 1.
Summary of Included Papers and Studies
| Study | Paper citation(s) | Setting | Instrument | Respondent | Framing to patient | Youth confidentiality | Accommodation | Scoring | Second stage evaluation |
|---|---|---|---|---|---|---|---|---|---|
| 1. | Applegate 200339 | PC | PSC | Parent only | Not stated | Parent only | Not stated | PCP with training | PCP decides |
| 2. | Asarnow 200550; Asarnow 200976; Wells 201277 | PC | Items from CIDI and CES-D | Youth | “Interested in how youth feeling” | Self-administered; no further detail | English only | Study staff | PCP supported by care manager |
| 3. | Ballard 201263; Horowitz 201066 | ED | SIQ | Youth | Not stated | Self-administered; answers shared if concern for safety | English only | Not stated | On-site MH staff evaluate positives |
| 4. | Berger-Jenkins 201240 | PC | Initial question for “concerns” then PSC | Parent | Not stated | Parent only | English and Spanish | Nurse | PCP decides; brief training |
| 5. | Briggs 201258 | PC | ASQ-SE | Parent | Letter given to parent | Parent only | English and Spanish, can ask for help | Psychologist | On-site psychologist evaluates positives |
| 6. | Chisolm 200852 | PC | Health eTouch | Youth | Not stated | Tablet with safeguards; told clinician will see results | Not stated; literacy a problem | Automatic | Referral information for + items; automatic email to suicide team |
| 7. | Chisolm 200910 | PC | Health eTouch | Youth | Not stated | Same as Study 6 | Not stated | Automatic | Same as Study 6 |
| 8. | Stevens 200848 | PC | Health eTouch | Youth | Not stated | Same as Study 6 | Not stated | Automatic | Same as Study 6 |
| 9. | Gardner 201053 | PC | Health eTouch | Youth | Not stated | Same as Study 6 | Not stated | Automatic | PCP option to discuss with on-site SW |
| 10. | Diamond 201072 | PC | BHS | Youth | Not stated | Not stated | Not stated | Automatic | PCP decides |
| 11. | Fein 201059 | ED | BHS | Youth | Pamphlet and slide show explain purpose | Introduction explains limits of confidentiality | English only but could be audio-assisted | Automatic | “Routine care” with consult available |
| 12. | Pailler 200945, 60 | ED | BHS | Youth | Same as study 11 | Same as study 11 | Same as study 11 | Automatic | Same as study 11 |
| 13. | Gall 200054 | School HC | PSC with additional questions | Youth | Not stated | Not stated | Not stated | Not stated | Refer positive screens |
| 14. | Garrison 199265 | PC | Custom survey | Parent only | Not stated; asked if willing to share with PCP | Parent only | English and Spanish | PCP | PCP decides |
| 15. | Gruttadero 201138 | PC | N/A | N/A | Parents feel giving screen positive frame | N/A | N/A | N/A | N/A |
| 16. | Hacker 200611 | PC | PSC | Parent or youth | Not stated | Youth do in waiting area | Multiple languages | PCP scores | PCPs told to refer + or parent concern |
| 17. | Hacker 200912 | PC | PSC | Parent or youth | Not stated | Same as Study 16 | Multiple languages | PCP scores | Same as Study 16 |
| 18. | Hartung 201055 | PC | Primary Care MH Screener | Parent | Not stated | Parent only | Parent only | Not scored; item by item review | Training on symptom clusters, follow-up probes |
| 19. | Hayutin (2009)51 | PC and GI clinic | PSC | Parent | Parents given handout about interpretation | Parent only | Not stated | Some parents self-scored | PCP got 5-minute training on interpreting results |
| 20. | Horwitz 200857 | PC | CHADIS system | Parent | Not stated | Parent only | Not stated | Automatic | Guidance for + items; PCP’s had 30-min training |
| 21. | Husky 201156 | PC | DPS-8 | Youth | Not stated | Disclosure if danger | Not stated | Automatic | PCP decides |
| 22. | Jee 201141 | PC for foster care | SDQ | Youth and foster parents | Not stated | Not stated | English only | Not scored till after visit | Provider reviews items, on-site SW can help |
| 23. | Jellinek 199978; Wasserman 199979; Kelleher 199780 | PC | PSC | Parents | Not stated | Parent only | Not stated | Not stated | PCPs not given results |
| 24. | John 200761 | Outpatient pediatric clinics | Short Mood and Feeling Questionnaire | Youth | Not stated | Not stated | Not stated | Automatic | Prompts for counseling |
| 25. | King 200967 | ED | Multiple | Youth | Not stated | Notify parent if “high risk” | English only | Research staff | Not stated |
| 26. | King 201268 | ED | Multiple | Youth | Not stated | Some youth told staff member will review results | English only, reading level <6.1 | Research staff | Not stated |
| 27. | Kuhlthau 20119 | Multiple (claims data) | Multiple | Parent or youth | Not known | Not known | Not known | Not known | Not known |
| 28. | Metz 197662 | PC | Multiphasic visit | Parent | Not known | Parent only | Not known; administered by staff | Clinical staff | PCP given detailed summary after visit |
| 29. | Murphy 199642; Pagano 199671 | School clinics and PC | PSC with function questions | Parent | Voluntary, reason explained | Parent only | Initially none, then given orally in English or Spanish | Not stated | PCP could refer regardless of score |
| 30. | Navon 200134 | PC | PSC | Parent | Desire to include emotions and behavior, voluntary | Parent only | Bilingual research assistant | Research staff | PCP decides, could bring to MDT |
| 31. | Olson 200543 | PC | Health Teen Screener | Youth | Not stated | Tablet with safeguards | Not stated | Automatic | 2-hr training in interviewing and motivation |
| 32. | Olson 200944 | PC | Health Teen Screener | Youth | Not stated | Tablet with safeguards | Not stated | Automatic | Areas of teen readiness to change highlighted |
| 33. | Schubiner 199449 | PC | Safe Times Questionnaire | Youth | Learning how adolescents are interviewed | Not stated | Not stated | PCP scores | Training in interviewing, risk categories, psychometrics of screen |
| 34. | Smith 199064 | PC | STAI, CDI | Youth | Mood questionnaire for all new patients | Not stated | Not stated | Not stated | Received results after initial assessment |
| 35. | Williams 201169 | ED | DPS | Youth | Short orientation to computer | Headphones and audio-assisted | Audio-assisted, English only | Automatic | Managed by onsite SW |
| 36. | Wintersteen 201046 | PC | Custom survey, two stage, in EMR template | Youth | Part of psychosocial part of visit | Not stated | Not stated | Not applicable | 90-min training on response to suicidality; on-site SW for help |
| 37. | Zuckerbrot 20068 | PC | Columbia Depression Screen and option to use DISC module | Youth | Not stated | Confidential place to complete | Not stated (front desk staff assisted sometimes) | Part automatic, part PCP | Some PCP training and list of referral resources |
| 38. | Rausch 201247 | PC | Columbia Depression Scale | Youth | Not stated | Not stated | English and Spanish instruments | PCP scored | “Brief introduction” to adolescent depression” and scoring guide; refer positives |
Note: CDI = Children’s Depression Inventory; CES-D = Center for Epidemiologic Studies Depression Scale; DPS = Diagnostic Predictive Scales; ED = Emergency Department; EMR = electronic medical record; MH=Mental Health; PC = Primary Care; PCP = Primary Care Provider; PSC = Pediatric Symptom Checklist; SDQ = Strengths and Difficulties Questionnaire; STAI = State-Trait Anxiety Inventory.
A. Engaging Parents and Youth in the Screening Process
Who Presents Screening to Parents and Youth?
Different types of staff were used to introduce and administer mental health screening, but no consensus emerged on who is best suited for this role. There was no evidence that parents or youth were given a choice about who would administer the screening tool. Among studies that did not employ temporary research assistants for the task (n=21), 13 reported screens being introduced by administrative staff (e.g., “front desk personnel”) prior to visits.8, 10–12, 40, 44, 48, 52–57 Seven reported that screens were given to families by nurses or specially trained aides.41, 47, 58–62 One study incorporated screening questions into the prompts given to primary care providers by an electronic medical record system.46 Only one study, in an emergency department, asked families who they thought should best introduce mental health screening to eligible patients. In that study, respondents felt that screens should be introduced by clinicians, and only after there had been time to build a level of rapport suited to a sensitive topic.45 In another emergency department study, most youth said they were comfortable with being asked by a nurse about suicidality.63
Explaining the Purpose and Processes of Screening
Little is described about how the purpose or processes of mental health screening are explained to parents or youth. Examples from the studies include having an appointment clerk tell parents that “optional mental health screening” is available at no cost,56 having a staff member say that clinicians are interested in how youth are feeling,50 and saying that a “mood questionnaire” is being given to all new patients.64 One study told parents the clinic was “including questions about children’s emotion and behavior as part of their pediatric visit.”34 In another, a nurse asked parents to complete the socioemotional scales of the Ages and Stages Questionnaire for their child and presented them with a letter (in English or Spanish) explaining its purpose (the contents of the letter are not described in the published report).58 The most elaborate framing was described in a study conducted in an emergency department.60 A “slide show” introduced screening using “adolescents’ own words about how a depressed teenager might feel.” The slides also described what would happen if a screen were scored positive.
No studies compared the success of different means of explanation; however, parent and youth willingness to be screened varied among studies that presented screening as optional or universal. A study that invited families to complete screening materials online prior to visits reported that only 9% did so.57 In a study where registration staff asked parents if they would be interested in screening, only about 45% accepted.56 In an emergency department study, nurses or technicians, “at any time during the adolescent patient’s assessment,” used a laminated pamphlet to describe the purpose of screening and ask for the adolescent’s participation; 65% agreed to be screened.59 In contrast, systematically presenting screening to patients or families as a routine part of health maintenance visits resulted in a higher rate of completion (85–95%).11, 41, 54, 64, 65 Youth in one emergency study said they preferred universal screening to avoid the feeling of being “targeted” as having a mental health problem. 45
Statements About Confidentiality
Most studies (n=18 of 27) in which youth were given screens did not state how confidentiality was explained. Those that did used varying language. Two studies of suicide screening in an emergency department told teens that clinicians and parents would be informed of results that indicated a concern for safety.66, 67 Two studies of more comprehensive screening, one in an outpatient setting and one in an emergency department, told teens that their results would remain confidential unless there was evidence of danger to self or others, abuse, or significant functional impairment.56, 60 In 4 studies, youth were told explicitly that their health care provider would see the results.10, 48, 52, 53 One study said only that they had explained the “standard limits of confidentiality.”59
There was evidence that youth valued knowing whether their responses would be confidential. One study of a computerized, broad-band primary care mental health screener for youth 11–20 found that a belief that data would remain private and be used only for health care was positively correlated with satisfaction with use of the screen.52 In Pailler et al.’s emergency department study, youth also said they wanted to know about the extent of confidentiality around their results.45 Another study found that youth completing a screen on a handheld device preferred it to paper because they believed it was more likely to preserve the confidentiality of their responses.44 One study suggested that some youth might change their answers to screens based on who would talk with them about results.68 Youth from low-income families, when told a research staff member would meet with them to review results, reported, on average, lower scores on a suicide risk instrument than did those who were told they would not have the review. Higher-income youth did not demonstrate this difference, and it is not clear if the same effect would be seen if the review had involved a nurse, doctor, or social worker.
Privacy for Youth During Administration
Providing privacy during the completion of a screen is another aspect of assuring confidentiality and increasing disclosure. Most studies involving youth did not discuss privacy, and one suggested it could be difficult to assure, at least in an emergency department. In that study, parents gave consent for only 60% of eligible youth to be screened. The second most common reason for parents declining consent was unwillingness to leave the room while the youth completed the screen.66 Another emergency department study used computer-assisted administration with headphones, offering the possibility of private responses even though others might be present.60, 69 Three primary care studies offered youth a “confidential space” to complete the screen.8, 56, 64 Some studies using computerized screens noted the advantage that responses could no longer be seen once they were entered.43, 70
Assistance With Completion
Little is known about the best strategies for conducting screening in primary care when families come from varying cultural, language, or literacy backgrounds. Eight of the studies reviewed excluded families that did not speak English;41, 50, 59, 63, 64, 67–69 many others (n=20) did not state the language in which screening was administered. Only 3 studies reported that parents or youth were able to ask for assistance when completing screens,34, 42, 58 and one computer-administered screen had an option that allowed the respondent to listen to the questions as they were presented.59, 60
Two studies provided insight into the impact of helping families who have problems with language or literacy. One, which used the PSC with Latino families, found a high rate of incomplete forms when the instrument was self-administered.42, 71 After a switch to oral administration, completion rates improved, and the proportion “positive” increased among parents of children over five (it stayed the same for younger children). The study was not able to determine what about oral administration had been helpful; the authors speculated that overcoming inability to read the written form, greater confidence in disclosing the information verbally, or the ability of the person administering the screen to explain unfamiliar terms, may have contributed. In another study with a high (70%) completion rate and a culturally heterogeneous population (screening forms in 6 languages), language and literacy issues were thought to be among the reasons why some forms were not completed.12
Attitudes Toward Screening and Screening Uptake
In addition to valuing statements about universal and confidential processes, as noted above, studies found that youth and parents value screening as a means to improve treatment. In one study, youth rated screening more highly if they believed that it would help them communicate with their provider and receive better care.52 Other reasons for endorsing screening included the hope for better linkage to services63 and increasing the likelihood of having one’s concerns addressed during the visit.44 In a survey of parents of children with mental health problems, screening was seen by the parents as an opportunity for doctors to signal that mental health problems beyond common concerns such as attention-deficit/hyperactivity disorder (ADHD) were appropriate for discussion in primary care.38
B. Evaluation and Use of Screening Results
Scoring Screening Instruments
Only 6studies stated or implied that providers were taught how to score the screens used,8, 11, 12, 39, 47, 49 and only 1 stated explicitly that providers were taught that a screen could have variable and low predictive values depending on the cut-point used.8 In 20, screens were scored by a computer, research assistant, or co-located mental health provider.10, 34, 40, 43–45, 48, 50–53, 56–59, 62, 67–69, 72. One study had providers review the screen during the visit but not score it formally until afterwards.41 Another suggested that providers not score the screen at any time, but rather should follow up on individual positive items and assess for functional impairment before considering a referral.55 Several studies did not describe how screens were scored.
Exploring Initial Screening Results With Families
The studies reviewed provide little guidance on how providers should explain and confirm screening results with families. Only 2 studies said explicitly that providers were trained either to ask follow-up questions about specific positive answers55 or to validate the results through further questioning.8 Some appeared to assume that clinicians would be recommending further care for those with positive screen results. 34, 42, 47, 53, 54 One explicitly said that children who scored positive (on the PSC) should be referred to a co-located social worker unless they were already receiving mental health care.11 Though some providers received a degree of training on diagnosis and management of the conditions targeted in the screens8, 46, 49, 57 or had some degree of access to a mental health consultant,11, 41, 53, 58, 59 others received only brief instruction,47 in one case as little as a few minutes.51 Other providers were simply instructed to follow “routine practice” or use results in whatever way they felt was clinically indicated 39, 40, 59, 60, 62 or as an “adjunct to their clinical judgment.”34 One study provided more general training in motivational interviewing, patient-centered counseling, and developing action plans regarding issues that might come up as a result of screening.43 Three computerized screening systems provided prompts or referral resources keyed to particular positive answers, but except in one case57 there did not appear to be training provided on use of the prompts.10, 48, 52, 53, 61
Screening Follow-Up
Reported referral rates provide some clues to how providers use screening results to make clinical decisions. Whether parents were also asked more generally about mental health concerns influenced the relationship of screening results to follow-up plans. In one study, the overall referral rate for children who were PSC positive was 75% versus 5% for children who were negative. However, among children whose parents said they had mental health concerns about their child, referral rates for PSC-positive and negative children were very similar (94% and 72%, respectively).11 In a study of adolescents that used a different outcome measure,10 16% of those with positive screens had at least one mental health visit in the follow-up observation period, compared to 5% of those who screened negative. However, the relationship of receiving follow-up services to a positive screen was seen for depression and suicidal thoughts, but not for substance problems. This study also involved a comparison of youth whose providers received screening results at the time of the visit or after a delay. Receipt of results at the time of the visit led to increased provider rates of recognition of youth mental health problems48 but not to subsequent differences in service use. Thus, it was not clear if the difference in utilization related to increased provider referrals or to screened youth being motivated to seek mental health services. Even youth who screened negative had more utilization than youth who had not been screened (though the comparison group was not randomized).
Four studies, when viewed together, could suggest that more elaborate screens offering diagnostic support may allow providers to be more discerning about follow-up processes compared to brief screens that yield only an overall risk status. Three studies using the brief PSC reported that about 70% or more of those with a positive result received a referral.11, 42, 54 In contrast, in a study using the Depressive Psychopathology Scale (DPS-8; an 84-item computerized instrument covering suicide, social phobia, panic attacks, generalized anxiety, obsessive-compulsive disorder, depression, and substance abuse),56 45% of those positive received a referral. Three of these studies (two PSC and the DPS-8 study) were carried out in settings with integrated or co-located behavioral health services, although they differed in the age range of the children/youth involved and in whether parents were asked if they had concerns.
Two studies found that although positive screens greatly increased the likelihood of referral, a large proportion of the mental health referrals made from primary care ultimately were for children who had screened negative. In Hacker et al.’s study using the PSC,11 61% of mental health referrals were for children with negative screens. In the study with youth using the DPS-8,56 11 (46%) of the total 24 with mental health follow-up plans were screen negative. Screening may thus prompt parents or youth to provide information during the visit even if they did not reveal it in their responses to the screen itself. In 2 studies using computerized screens with summary reports, screened youth reported that the process had reduced the chance that one of their concerns would not be discussed.43, 44 Screening may also prompt providers to ask additional questions (beyond those on the screen) even when they are not explicitly trained to do so. Some providers reported that screening had helped them better plan visits and focus on topics that were most relevant to patients.43, 44, 72 In a study that made audio recordings of visits before and after screening was introduced, screening increased the number of discussions of behavioral issues, and this was not related to the screening score.39 One study randomized providers to use the PSC scored by either parents or by a staff assistant.51 After the visit, parents reported on the extent to which PSC items had been discussed with their child’s doctor. Screening (compared to a nonscreened control group) increased discussions regardless of who scored the PSC, but staff scoring increased the extent to which providers raised topics rather than parents. Parent scoring did not impact the extent to which parents initiated discussions, but it was positively correlated with their satisfaction that PSC-related issues had been sufficiently discussed.
Discussion
For mental health screening to succeed, respondents must be willing to divulge potentially sensitive information and agree to its meaning and validity. This review found that current use in primary care, at least as reflected in the contents of published reports, places little emphasis on steps that would make this possible. Published reports give little explanation of how the purpose of screening is explained or what youth are told about who will have access to the information. Assistance with completion or accommodation for language differences, hearing or vision impairment, or limited literacy is not usually described, and there are only inconsistent reports of attention to privacy during the screening process. However, though systematic comparison among studies is not possible, there is some evidence that attention to these factors influences attitudes toward screening and rates of uptake.
The literature also provides little insight into how clinicians evaluate initial screening results and use them to make clinical decisions. While some programs paired screening with training or facilitated access to consultation and evaluation, the plans described for many assumed either that clinicians already knew what to do with the information or that all patients who screened positive should be referred for evaluation or treatment from a specialist. Only 2 papers said explicitly that the psychometrics of the screens they used had been explained to providers and that providers were trained either to ask follow-up questions or in some way validate the screen results.8, 55 In the absence of skills to interpret results, and especially when using instruments that do not explicitly help differentiate among possible mental health problems, busy clinicians may opt to refer all positive screens (or cases with parental concerns). Such a policy could overwhelm limited mental health resources with large numbers of appointments, many of which might not be kept. In fact, one study noted that the cut-point on its depression screen had to be adjusted upward because primary care and behavioral health providers could not handle the volume of cases being identified.48 One of the reviewed papers—perhaps because it was evaluating a new instrument—provides a possible model for what providers should know if they are to use existing screening tools. Hartung et al.55 trained providers how to decide when follow-up questions were warranted, suggested general probes to get further information, and underscored that assessing impairment was a necessary step before considering a referral.
Other guidance can be drawn from the studies about possible ways to address problems with engagement. The few studies that asked found that both patients and providers found screening useful as a way to more efficiently and acceptably initiate discussions of mental health problems and be responsive to patient concerns.38, 43, 44, 72 The studies reviewed suggest that families and youth are likely to feel positively about screening that is framed as universal, intended to optimize attention to their concerns, and designed to address common but sensitive issues in a thoughtful and confidential manner. As has been found in other settings, computerized screening was well accepted and may prove to be an effective way of efficiently administering screens that offer more decision support, overcome literacy barriers, and create a greater sense of confidentiality.73, 74 Studies of general medical care have also found that youth asked to disclose sensitive concerns are responsive to assurances about confidentiality.75 These considerations apply not just to screening but also to engaging parents, children, and youth in any service to which they are subsequently referred.38,45 Mental health problems can be chronic or recur across the lifespan, and negative experiences may make an individual reluctant to seek services when they are needed at a time in the future.
All of our observations regarding the relationship of engagement and evaluation to screening uptake or follow-up are best taken as jumping off points for further study; we did not conduct a formal meta-analysis, and none of the studies reviewed were designed to explore these issues. The scanty information provided in most studies about engagement and evaluation steps does not necessarily mean that they were neglected by investigators, but could reflect a form of publication bias. Investigators or editors may see these details as unrelated to outcomes and thus less important to report than other study details. In addition, the inclusion of studies from school and low-acuity emergency settings goes beyond the usual definition of primary care, though it reflects the ways in which many children and youth receive general medical services. The strongest conclusion that can be drawn from this review is that the existing literature on pediatric mental health screening processes for patient engagement and provider use is very limited. Key issues such as how to present screeners in ways that are not potentially damaging to therapeutic relationships (intrusive, culturally inappropriate, not confidential, etc.), or how to help providers make valid use of screening results, have not received systematic study.
The large number of screen-negative children referred in some studies poses an important question for planning follow-up services. We do not know if these referrals represent false negative results (which could be caused by failure to disclose information on the screen itself, a misadjustment of the cut-off point, or the overall process prompting disclosure of concerns not covered on the screen), or, less optimistically, an oversensitization to mental health concerns prompted by using the screen. New research on mental health screening in primary care should at the very least provide details about how screening is framed to patients and how providers are taught to use results; ideally it should study variations in these aspects of the process within the context of a clear vision of the clinical goals desired.
Supplementary Material
Clinical Guidance.
The literature suggests that screening can have a positive effect on parent, youth, and primary care provider willingness to discuss mental health issues.
There is a suggestion in published studies that parents and youth favor screening that is framed as universal, confidential, and designed to improve communication with their primary care provider, but there remain many questions about screening can best be presented in primary care settings.
Screening may have unpredictable and potentially undesired impact for patients and systems in the absence of support for clinical decision making, first-line treatment, and linkage to specialty care. Factors that promote effective screening—attention to informing patients about clinical goals, using accessible terms, and discussing confidentiality—are also important aspects of any care that is subsequently offered.
Mental health professionals working with primary care providers may want to inquire about the extent to which their colleagues have been trained to interpret screening results. If asked for informal or formal consultation based on screening findings (positive or negative), it could be important to ask how the screen was administered, what other information has been gathered, and how the combined information has led to a desire for consultation or referral.
Acknowledgments
This work was supported by the National Institute of Mental Health (NIMH) grant P20 MH 086048.
The authors gratefully acknowledge the guidance of Andrea Villanti, Ph.D., and Donna Hesson, M.L.S., of the Johns Hopkins School of Public Health for guidance with systematic literature review methods.
Footnotes
Supplemental material cited in this article is available online.
Disclosure: Drs. Wissow, Brown, Fothergill, Gadomski, Hacker, and Salmon, and Ms. Zelkowitz report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Lawrence S. Wissow, Johns Hopkins School of Public Health
Dr. Jonathan Brown, Johns Hopkins School of Public Health
Dr. Kate E. Fothergill, Johns Hopkins School of Public Health
Dr. Anne Gadomski, Bassett Research Institute
Dr. Karen Hacker, Cambridge Health Alliance
Dr. Peter Salmon, University of Liverpool
Ms. Rachel Zelkowitz, Johns Hopkins School of Public Health
References
- 1.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. Am J Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- 2.Kramer T, Garralda ME. Psychiatric disorders in adolescents in primary care. Br J Psychiatry. 1998;173:508–513. doi: 10.1192/bjp.173.6.508. [DOI] [PubMed] [Google Scholar]
- 3.Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health. Policy statement - the future of pediatrics: Mental health competencies for pediatric primary care. Pediatr. 2009;124:410–421. doi: 10.1542/peds.2009-1061. [DOI] [PubMed] [Google Scholar]
- 4.US Preventive Services Task Force. Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force Recommendation Statement. Pediatr. 2009;123:1223–1228. doi: 10.1542/peds.2008-2381. [DOI] [PubMed] [Google Scholar]
- 5.Preventive regulations, 2010 Patient Protection and Affordable Care Act. [Accessed December 24, 2012];Public Law 111 – 148. ( http://www.gpo.gov/fdsys/pkg/PLAW-111publ148)
- 6.Semansky R, Koyanagi C, Vandivort-Warren R. Behavioral health screening policies in Medicaid programs nationwide. Psych Services. 2003;54:736–739. doi: 10.1176/appi.ps.54.5.736. [DOI] [PubMed] [Google Scholar]
- 7.Olson AL, Kemper KJ, Kelleher KJ, Hammond CS, Zuckerman BS, Dietrich AJ. Primary care pediatricians’ roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110:1169–1176. doi: 10.1542/peds.110.6.1169. [DOI] [PubMed] [Google Scholar]
- 8.Zuckerbrot RA, Maxon L, Pagar D, Davies M, Fisher PW, Shaffer D. Adolescent depression screening in primary care: feasibility and acceptability. Pediatrics. 2007;119:101–108. doi: 10.1542/peds.2005-2965. [DOI] [PubMed] [Google Scholar]
- 9.Kuhlthau K, Jellinek M, White G, VanCleave J, Simons J, Murphy M. Increases in behavioral health screening in pediatric care for Massachusetts Medicaid patients. Arch Ped Adoles Med. 2011;165:660–664. doi: 10.1001/archpediatrics.2011.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chisolm D, Klima J, Gardner W, Kelleher K. Adolescent behavioral risk screening and use of health services. Admin Policy Mental Health. 2009;36(6):374–380. doi: 10.1007/s10488-009-0245-8. [DOI] [PubMed] [Google Scholar]
- 11.Hacker K, Myagmarjav E, Harris V, Suglia S, Weidner D, Link D. Mental health screening in pediatric practice: Factors related to positive screens and the contribution of parental/personal concern. Pediatr. 2006;126(5):1896–1906. doi: 10.1542/peds.2006-0026. [DOI] [PubMed] [Google Scholar]
- 12.Hacker KA, Williams S, Myagmarjav E, Cabral H, Murphy M. Persistence and change in pediatric symptom checklist scores over 10 to 18 months. Acad Pediatr. 2009;9:270–277. doi: 10.1016/j.acap.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Norlin C, Crawford M, Bell C, Sheng X, Stein M. Delivery of well-child care: A look inside the door. Academ Ped. 2011;11:18–26. doi: 10.1016/j.acap.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Earls MF, Hay SS. Setting the stage for success: Implementation of developmental and behavioral screening and surveillance in primary care practice -- the North Carolina Assuring Better Child Health and Development (ABCD) project. Pediatr. 2006;118:e183. doi: 10.1542/peds.2006-0475. [DOI] [PubMed] [Google Scholar]
- 15.Weitzman C, Leventhal JM. Screening for behavioral health problems in primary care. Curr Opin Ped. 2006;18:641–648. doi: 10.1097/MOP.0b013e3280108292. [DOI] [PubMed] [Google Scholar]
- 16.Brent DA. Screens and doors: The management of adolescent depression in primary care. Arch Pediatr Adolesc Med. 2006;160:755–756. doi: 10.1001/archpedi.160.7.755. [DOI] [PubMed] [Google Scholar]
- 17.Richardson LP, Lewis CW, Casey-Goldstein M, McCauley E, Katon W. Pediatric primary care providers and adolescent depression: A qualitative study of barriers to treatment and the effect of the black box warning. J Adolesc Health. 2007;40:433–439. doi: 10.1016/j.jadohealth.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Sanci L, Lewis D, Patton G. Detecting emotional disorders in young people in primary care. Curr Opin Psych. 2010;23:318–323. doi: 10.1097/yco.0b013e32833aac38. [DOI] [PubMed] [Google Scholar]
- 19.Canino G, Alegria M. Psychiatric diagnosis - is it universal or relative to culture? J Child Psychol Psychiatry. 2008;49:237–250. doi: 10.1111/j.1469-7610.2007.01854.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maynard DW, Freese J, Schaeffer NC. Requests, blocking moves, and rational (inter)action in survey introductions. Am Sociol Rev. 2010;75:791–798. doi: 10.1177/0003122410379582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warnecke RB, Johnson TP, Chavez N, et al. Improving question wording in surveys of culturally diverse populations. Ann Epidemiol. 1997;7:334–342. doi: 10.1016/s1047-2797(97)00030-6. [DOI] [PubMed] [Google Scholar]
- 22.Bradburn NM, Rips LJ, Shevell SK. Answering autobiographical questions: The impact of memory and inference on surveys. Science. 1987;236:157–161. doi: 10.1126/science.3563494. [DOI] [PubMed] [Google Scholar]
- 23.Gordis L. Epidemiology. Philadelphia: Saunders; 2004. [Google Scholar]
- 24.Klabunde CN, Lanier D, Breslau ES, et al. Improving colorectal cancer screening in primary care practice: Innovative strategies and future directions. J Gen Intern Med. 2007;22(8):1195–1205. doi: 10.1007/s11606-007-0231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 26.Williams SB, O’Connor E, Eder M, Whitlock E. Screening for child and adolescent depression in primary care settings: A systematic review for the US Preventive Services Task Force. U.S. Preventive Services Task Force Evidence Syntheses; 2009. formerly Systematic Evidence Reviews. Report No.: 09-05130-EF-1. [PubMed] [Google Scholar]
- 27.Carter AS, Briggs-Gowan MJ, Davis NO. Assessment of young children’s social-emotional development and psychopathology: Recent advances and recommendations for practice. J Child Psychol Psychiatry. 2004;45:109–134. doi: 10.1046/j.0021-9630.2003.00316.x. [DOI] [PubMed] [Google Scholar]
- 28.Gilbody S, House A, Sheldon T. Screening and case finding instruments for depression (review) Cochrane Database Syst Rev. 2005 Oct 19;(4):CD002792. doi: 10.1002/14651858.CD002792.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilbody S, Sheldon T, House A. Screening and case-finding instruments for depression: A meta-analysis. CMAJ. 2008;178:997–1003. doi: 10.1503/cmaj.070281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simonian SJ. Screening and identification in pediatric primary care. Behav Modif. 2006;30:114–131. doi: 10.1177/0145445505283311. [DOI] [PubMed] [Google Scholar]
- 31.Richardson LP, McCauley E, Grossman DC, et al. Evaluation of the patient health questionnaire-9 item for detecting major depression among adolescents. Pediatr. 2010;126:1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gardner W, Klima J, Chisolm D, et al. Screening, triage, and referral of patients who report suicidal thought during a primary care visit. Pediatrics. 2010;125:945–952. doi: 10.1542/peds.2009-1964. [DOI] [PubMed] [Google Scholar]
- 33.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 34.Navon M, Nelson D, Pagano M, Murphy M. Use of the pediatric symptom checklist in strategies to improve behavioral health care. Psych Services. 2001;52:800–804. doi: 10.1176/appi.ps.52.6.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kostanecka A, Power T, Clarke A, Watkins M, Hausman CL, Blum NJ. Behavioral health screening in urban primary care settings: Construct validity of the PSC-17. J of Dev Behav Ped. 2008;29:124–128. doi: 10.1097/DBP.0b013e31816a0d9e. [DOI] [PubMed] [Google Scholar]
- 36.Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: Audit of primary sources. BMJ. 2005;331:1064–1065. doi: 10.1136/bmj.38636.593461.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gruttadaro D, Markey D. The family experience with primary care physicians and staff: A report by the National Alliance on Mental Illness. Arlington, VA: National Alliance on Mental Illness; May, 2011. [Google Scholar]
- 39.Applegate H, Kelley ML, Applegate BW, Jayasinghe IK, Venters CL. Clinical case study: Pediatric residents’ discussions of and interventions for children’s behavioral and emotional problems. J Pediatr Psychol. 2003;28:315–321. doi: 10.1093/jpepsy/jsg021. [DOI] [PubMed] [Google Scholar]
- 40.Berger-Jenkins E, McCord M, Gallagher T, Olfson M. Effect of routine mental health screening in a low-resource pediatric primary care population. Clin Pediatr. 2012;51:359–365. doi: 10.1177/0009922811427582. [DOI] [PubMed] [Google Scholar]
- 41.Jee SH, Halterman JS, Szilagyi M, Conn A, Alpert-Gillis L, Szilagyi PG. Use of a brief standardized screening instrument in a primary care setting to enhance detection of social-emotional problems among youth in foster care. Acad Pediatr. 2011;11:409–413. doi: 10.1016/j.acap.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 42.Murphy JM, Ichinose C, Hicks RC, et al. Utility of the pediatric symptom checklist as a psychosocial screen to meet the federal Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) standards: A pilot study. J Pediatr. 1996;129:864–869. doi: 10.1016/s0022-3476(96)70030-6. [DOI] [PubMed] [Google Scholar]
- 43.Olson AL, Gaffney CA, Hedberg VA, et al. The healthy teen project: Tools to enhance adolescent health counseling. Ann Fam Med. 2005;3 (Suppl 2):S63–S65. doi: 10.1370/afm.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Olson AL, Gaffney CA, Hedberg VA, Gladstone GR. Use of inexpensive technology to enhance adolescent health screening and counseling. Arch Pediatr Adolesc Med. 2009;163:172–177. doi: 10.1001/archpediatrics.2008.533. [DOI] [PubMed] [Google Scholar]
- 45.Pailler ME, Cronholm PF, Barg FK, Wintersteen MB, Diamond GS, Fein JA. Patients’ and caregivers’ beliefs about depression screening and referral in the emergency department. Pediatr Emerg Care. 2009;25:721–727. doi: 10.1097/PEC.0b013e3181bec8f2. [DOI] [PubMed] [Google Scholar]
- 46.Wintersteen MB. Standardized screening for suicidal adolescents in primary care. Pediatrics. 2010;125:938–944. doi: 10.1542/peds.2009-2458. [DOI] [PubMed] [Google Scholar]
- 47.Rausch J, Hametz P, Zuckerbrot R, Rausch W, Soren K. Screening for depression in urban Latino adolescents. Clin Pediatr (Phila) 2012;51:964–971. doi: 10.1177/0009922812441665. [DOI] [PubMed] [Google Scholar]
- 48.Stevens J, Kelleher KJ, Gardner W, et al. Trial of computerized screening for adolescent behavioral concerns. Pediatrics. 2008;121:1099–1105. doi: 10.1542/peds.2007-1878. [DOI] [PubMed] [Google Scholar]
- 49.Schubiner H, Tzelepis A, Wright K, Podany E. The clinical utility of the safe times questionnaire. J Adolesc Health. 1994;15:374–382. doi: 10.1016/1054-139x(94)90260-7. [DOI] [PubMed] [Google Scholar]
- 50.Asarnow JR, Jaycox LH, Duan N, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: A randomized controlled trial. JAMA. 2005;293:311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]
- 51.Hayutin LG, Reed-Knight B, Blount RL, Lewis J, McCormick ML. Increasing parent-pediatrician communication about children’s psychosocial problems. J Pediatr Psychol. 2009;34:1155–1164. doi: 10.1093/jpepsy/jsp012. [DOI] [PubMed] [Google Scholar]
- 52.Chisolm DJ, Gardner W, Julian T, Kelleher KJ. Adolescent satisfaction with computer-assisted behavioural risk screening in primary care. Child and Adolescent Mental Health. 2008;13:163–168. doi: 10.1111/j.1475-3588.2007.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gardner W, Klima J, Chisolm D, et al. Screening, triage, and referral of patients who report suicidal thought during a primary care visit. Pediatrics. 2010;125:945–952. doi: 10.1542/peds.2009-1964. [DOI] [PubMed] [Google Scholar]
- 54.Gall G, Pagano ME, Desmond MS, Perrin JM, Murphy JM. Utility of psychosocial screening at a school-based health center. J Sch Health. 2000;70:292–298. doi: 10.1111/j.1746-1561.2000.tb07254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hartung CM, Lefler EK. Preliminary examination of a new mental health screener in a pediatric sample. Jrnl Ped Health Care. 2010;24:168–175. doi: 10.1016/j.pedhc.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 56.Husky M, Miller K, McGuire L, Flynn L, Olfson M. Mental health screening of adolescents in pediatric practice. Jrnl of Beh Health Studies and Research. 2011;38:159–169. doi: 10.1007/s11414-009-9207-x. [DOI] [PubMed] [Google Scholar]
- 57.Horwitz SM, Hoagwood KE, Garner A, et al. No technological innovation is a panacea: A case series in quality improvement for primary care mental health services. Clin Pediatr (Phila) 2008;47:685–692. doi: 10.1177/0009922808315215. [DOI] [PubMed] [Google Scholar]
- 58.Briggs RD, Stettler EM, Silver EJ, et al. Social-emotional screening for infants and toddlers in primary care. Pediatrics. 2012;129:e377. doi: 10.1542/peds.2010-2211. [DOI] [PubMed] [Google Scholar]
- 59.Fein JA, Pailler ME, Barg FK, et al. Feasibility and effects of a web-based adolescent psychiatric assessment administered by clinical staff in the pediatric emergency department. Arch Pediatr Adolesc Med. 2010;164:1112–1117. doi: 10.1001/archpediatrics.2010.213. [DOI] [PubMed] [Google Scholar]
- 60.Pailler ME, Fein JA. Computerized behavioral health screening in the emergency department. Pediatr Ann. 2009;38:156–160. doi: 10.3928/00904481-20090301-08. [DOI] [PubMed] [Google Scholar]
- 61.John R, Buschman P, Chaszar M, Honig J, Mendonca E, Bakken S. Development and evaluation of a PDA-based decision support system for pediatric depression screening. Stud Health Technol Inform. 2007;129(Pt 2):1382–1386. [PubMed] [Google Scholar]
- 62.Metz JR, Allen CM, Barr G, Shinefield H. A pediatric screening examination for psychosocial problems. Pediatrics. 1976;58:595–606. [PubMed] [Google Scholar]
- 63.Ballard ED, Bosk A, Snyder D, et al. Patients’ opinions about suicide screening in a pediatric emergency department. Pediatr Emerg Care. 2012;28:34–38. doi: 10.1097/PEC.0b013e31823f2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Smith MS, Mitchell J, McCauley EA, Calderon R. Screening for anxiety and depression in an adolescent clinic. Pediatrics. 1990;85:262–266. [PubMed] [Google Scholar]
- 65.Garrison WT, Bailey EN, Garb J, Ecker B, Spencer P, Sigelman D. Interactions between parents and pediatric primary care physicians about children’s mental health. Hosp Community Psychiatry. 1992;43:489–493. doi: 10.1176/ps.43.5.489. [DOI] [PubMed] [Google Scholar]
- 66.Horowitz L, Ballard E, Teach S, et al. Feasibility of screening patients with nonpsychiatric complaints for suicide risk in a pediatric emergency department: A good time to talk? Pediatric Emergency Care. 2010;26:787–792. doi: 10.1097/PEC.0b013e3181fa8568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.King CA, O’Mara RM, Hayward CN, Cunningham RM. Adolescent suicide risk screening in the emergency department. Acad Emerg Med. 2009;16:1234–1241. doi: 10.1111/j.1553-2712.2009.00500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.King CA, Hill RM, Wynne HA, Cunningham RM. Adolescent suicide risk screening: The effect of communication about type of follow-up on adolescents’ screening responses. J Clin Child Adolesc Psychol. 2012;41:508–515. doi: 10.1080/15374416.2012.680188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Williams JR, Ho ML, Grupp-Phelan J. The acceptability of mental health screening in a pediatric emergency department. Pediatr Emerg Care. 2011;27:611–615. doi: 10.1097/PEC.0b013e318222554e. [DOI] [PubMed] [Google Scholar]
- 70.Julian TW, Kelleher K, Julian DA, Chisolm D. Using technology to enhance prevention services for children in primary care. J Prim Prev. 2007;28:155–165. doi: 10.1007/s10935-007-0086-8. [DOI] [PubMed] [Google Scholar]
- 71.Pagano M, Murphy JM, Pedersen M, et al. Screening for psychosocial problems in 4–5-year-olds during routine EPSDT examinations: Validity and reliability in a Mexican-American sample. Clin Pediatr (Phila) 1996;35:139–146. doi: 10.1177/000992289603500305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Diamond G, Levy S, Bevans K, et al. Development, validation, and utility of internet-based, behavioral health screen for adolescents. Pediatrics. 2010;126:e163. doi: 10.1542/peds.2009-3272. [DOI] [PubMed] [Google Scholar]
- 73.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 74.Newman JC, Des Jarlais DC, Turner CF, Gribble J, Cooley P, Paone D. The differential effects of face-to-face and computer interview modes. Am J Public Health. 2002;92:294–297. doi: 10.2105/ajph.92.2.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ford CA, Millstein SG, Halpern-Felsher BL, Irwin CE., Jr Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care. A randomized controlled trial. JAMA. 1997;278:1029–1034. [PubMed] [Google Scholar]
- 76.Asarnow JR, Jaycox LH, Tang L, et al. Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. Am J Psychiatry. 2009;166(9):1002–1010. doi: 10.1176/appi.ajp.2009.08121909. [DOI] [PubMed] [Google Scholar]
- 77.Wells KB, Tang L, Carlson GA, Asarnow JR. Treatment of youth depression in primary care under usual practice conditions: Observational findings from youth partners in care. J Child Adolesc Psychopharmacol. 2012;22:80–90. doi: 10.1089/cap.2011.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jellinek MS, Murphy JM, Little M, Pagano ME, Comer DM, Kelleher KJ. Use of the pediatric symptom checklist to screen for psychosocial problems in pediatric primary care: A national feasibility study. Arch Pediatr Adolesc Med. 1999;153:254–260. doi: 10.1001/archpedi.153.3.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wasserman RC, Kelleher KJ, Bocian A, et al. Identification of attentional and hyperactivity problems in primary care: A report from pediatric research in office settings and the ambulatory sentinel practice network. Pediatrics. 1999;103:e38. doi: 10.1542/peds.103.3.e38. [DOI] [PubMed] [Google Scholar]
- 80.Kelleher KJ, Childs GE, Wasserman RC, McInerny TK, Nutting PA, Gardner WP. Insurance status and recognition of psychosocial problems. A report from the pediatric research in office settings and the ambulatory sentinel practice networks. Arch Pediatr Adolesc Med. 1997;151:1109–1115. doi: 10.1001/archpedi.1997.02170480039006. [DOI] [PubMed] [Google Scholar]
- 81.Stevens J, Klima J, Chisolm D, Kelleher KJ. A trial of telephone services to increase adolescent utilization of health care for psychosocial problems. J Adolesc Health. 2009;45:564–570. doi: 10.1016/j.jadohealth.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 82.Stevens J, McGeehan J, Kelleher KJ. Readiness to change in adolescents screening positive for substance use in urban primary care clinics. J Child Adolesc Subst Abuse. 2010;19:99–107. doi: 10.1080/10678281003634876. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.