Abstract
Background:
To evaluate the correlation between the different traditional chinese medicine (TCM) deficiency syndromes, cancer related fatigue (CRF), and quality of life (QoL) in breast cancer patients.
Patients and methods:
Ninety-five breast cancer patients were categorized into different qi (氣 qì), blood (血 xuè), yin (陰 yin), and yang (陽 yáng) TCM deficiency syndrome groups (DSGs). We used the ICD-10 for diagnosing CRF. The QoL was assessed by the WHO-BREF and Short Form Health Survey (SF12) questionnaires. The major outcome was to compare the QoL scores between the different TCM DSGs. The second outcome was the intergroup analysis between the CRF and different TCM DSGs in breast cancer patients.
Results:
The patients with qi deficiency (氣虛 qì xu) had a higher correlation with CRF (p=0.001) and poorer QoL both in the WHO-BREF and SF12 survey (p<0.001), whereas the patients with yin deficiency (陰虛 yin xu) had poorer QoL in the psychological (p=0.02) and social aspects (p=0.04). The qi deficiency (氣虛 qì xu) syndrome was closely associated with yin deficiency syndrome (陰虛 yin xu). (p=0.03).
Conclusion:
Our study confirmed the concept of Qi-deficiency (氣虛 qì xu) in TCM was associated with CRF as identified in cancer care in western medicine. The breast cancer patients with qi deficiency (氣虛 qì xu) have poorer QoL. Treatment of CRF and improving QoL by supplying qi (氣 qì) may warrant further investigation.
Keywords: Traditional Chinese Medicine, Deficiency syndromes, Cancer-related Fatigue, Quality of life, Breast cancer
Introduction
TCM has been applied in cancer patient's care in recent decades. The different types of deficiency syndrome in TCM is an important concept to categorize the patients as lacking some specific element. (qi, blood, yin, yang) (氣 qì, 血 xuè, 陰 yīn, 陽 yáng). In brief, qi (氣 qì) refers to the vital energy of the body. It maintains blood circulation, warms the body, and fights diseases. The blood nourishes the body, moistens body tissues, and ensures they do not dry out. Yin (陰 yīn) and yang (陽 yáng) are complementary opposites that interact within a greater whole, as part of a dynamic system. Generally, anything that is moving, ascending, bright, progressing, hyperactive, including functional diseases of the body, pertains to yang (陽 yáng). The characteristics of stillness, descending, darkness, degeneration, hypo-activity, including organic disease, pertain to yin(陰 yīn).
Patients with any type of deficiency syndrome may also have the symptoms of weakness, low energy, anemia etc, which are roughly described as fatigue-like sensations in western medicine. Fatigue is a common and distressing problem for cancer patients (Vogelzang et al., 1997). In contrast to everyday or normal fatigue, CRF is characterized by feelings of tiredness and weakness despite adequate amounts of sleep and rest (Ahlberg et al., 2003; Portenoy and Itri, 1999). Further, QoL is a significant concern for cancer patients, and its disruption is often associated with symptoms such as fatigue, insomnia, and psychological distress (Bower et al., 2000; Portenoy, 2000). Several studies have focused on CRF and QoL in cancer patients (Gupta et al., 2007; Sadler et al., 2002), although there is limited data on the association of CRF with TCM deficiency syndrome.
Besides, we do not know the correlationship of different TCM deficiencies and QoL, and the cross talk on TCM deficiency syndrome with the fatigue so far is unclear. A previous study showed breast cancer patients are a homogenous group with a high percentage of fatigue (Mast, 1998).
Accordingly, there is a compelling need to better understand the correlation among the TCM deficiency syndromes, CRF, and QoL in breast cancer patients.
Method
Study design and subjects
The study was conducted between Mar, 2010 to Mar, 2011 in Taipei City Hospital, Taiwan. Among the 331 registered cancer patients, 95 breast cancer patients were enrolled. A trained clinical coordinator described the study and determined eligibility after patients signed in at the oncology department. Eligible patients were presented with the questionnaires at their initial visit and returned their completed questionnaires to the clinical coordinator within 24 hours. The study was approved by the Institutional Review Board at Taipei United Hospital. The eligibility criteria included (1) aged between 18 and 70 years, (2) breast cancer diagnosis confirmed by a professional physician, (3) Chinese as spoken language. Patients were excluded if with (1) unconsciousness, (2) delirium and psychiatric problems, (3) complications present, and (4) inability and unwillingness to give informed consent or were unable to understand or cooperate with the study conditions.
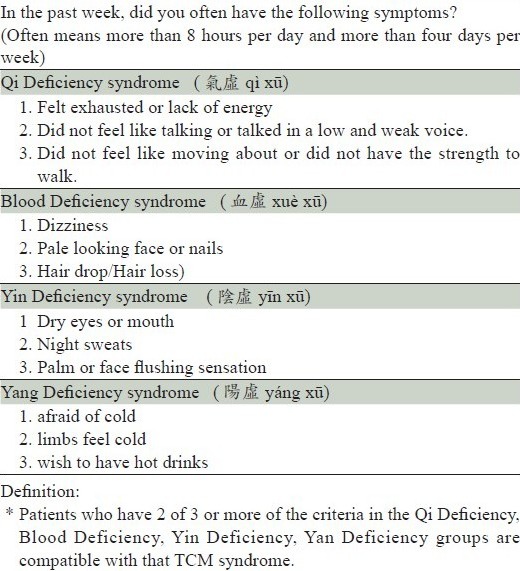
TCM DSGs defined
Deficiency syndrome is a TCM condition with weakness and lack of energy. All patients were categorized into qi (氣 qì), blood (血 xuè), yin (陰 yīn), and yang(陽 yáng) DSGs if they met the diagnosed criteria (having more than 2 out of 3 of the symptoms of the corresponding deficiency syndrome (Table 1). The validity and reliability of the diagnostic criteria were applied in our TCM study and well defined as an alpha coefficient of 0.89 and Cronbach's alpha coefficient of 0.88 through a validation test.
Table 1.
Classification Criteria for the diagnosis of TCM deficiency syndrome groups
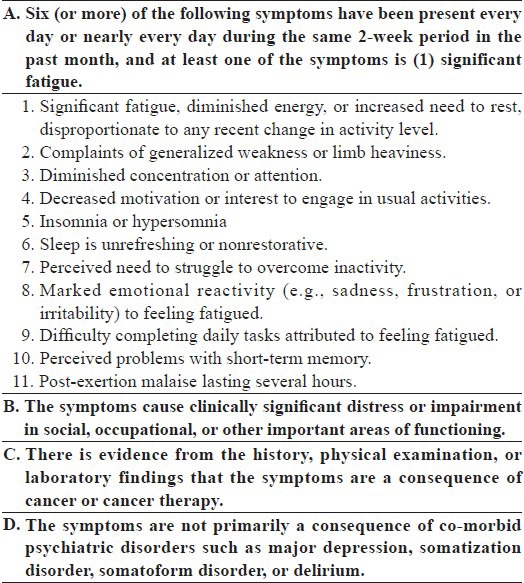
CRF defined
There are several screening instruments used in CRF survey (Alexander et al., 2009; Hann et al., 2000). The fatigue assessment in this study was performed according to the ICD-10 for CRF (Table 2) (Cella et al., 2001). It was designed to be considerably more discriminating and demanding. Six of the eleven criteria, as well as self-reported functional limitations, are prerequisites for diagnosis. Patients who reported experiencing fatigue for at least a few days each month during treatment were asked a series of questions regarding the impact of fatigue on their daily functioning, including physical, emotional, behavioral, social, occupational, and economic factors. Questions about how patients coped with fatigue during and after treatment were supplemented by questions about their current level of fatigue. This was done specifically to estimate the prevalence of CRF as defined by the proposed ICD-10 criteria (Van Belle et al., 2005).
Table 2.
Proposed ICD-10 Criteria for Cancer-Related Fatigue
QoL defined
The QoL was assessed by the WHO-BREF and SF12 questionnaires in this study. The WHOQOL-BREF instrument comprises 26 items, measuring the following broad domains: physical health, psychological health, social relationships, and environment. The SF-12 is a multipurpose short form survey with 12 questions, all selected from the SF-36 Health Survey (Ware et al., 1998). The questions were combined, scored, and weighted to create two scales that provide glimpses into mental and physical functioning and overall health-related-quality of life. The standard SF12 Health survey was weighted and summed to provide easily interpretable scales for physical and mental health.
The Physical and Mental Health Composite Scores (PCS & MCS) were then computed using the scores of twelve questions ranging from 0 to 100, where a zero score indicated the lowest level of health and 100 indicated the highest level of health (Müller-Nordhorn et al. 2001; Ware et al. 1998).
Outcome measurements
This study was designed to evaluate the correlation between TCM deficiency syndrome, CRF, and QoL in breast cancer patients. The major outcome was to compare the QoL scores between the with/without different TCM deficiency syndrome groups in breast cancer patients. The second outcome was the intergroup analysis between the CRF and different TCM DSGs and the comparison between with/without CRF in breast cancer patients.
Statistical analyses
The SPSS statistical package (version 17.0 for Windows; SPSS Inc.) was used for data entry and analysis. Demographics data was presented by descriptive statistics with mean and percentage. The outcome measures on QoL and CRF between with and without different TCM DSGs were compared using student t-test. The Chi-square test was applied to compare the fatigue of different TCM DSGs and the intergroup analysis. All p values were two tailed and the level of significance was set at 0.05.
Results
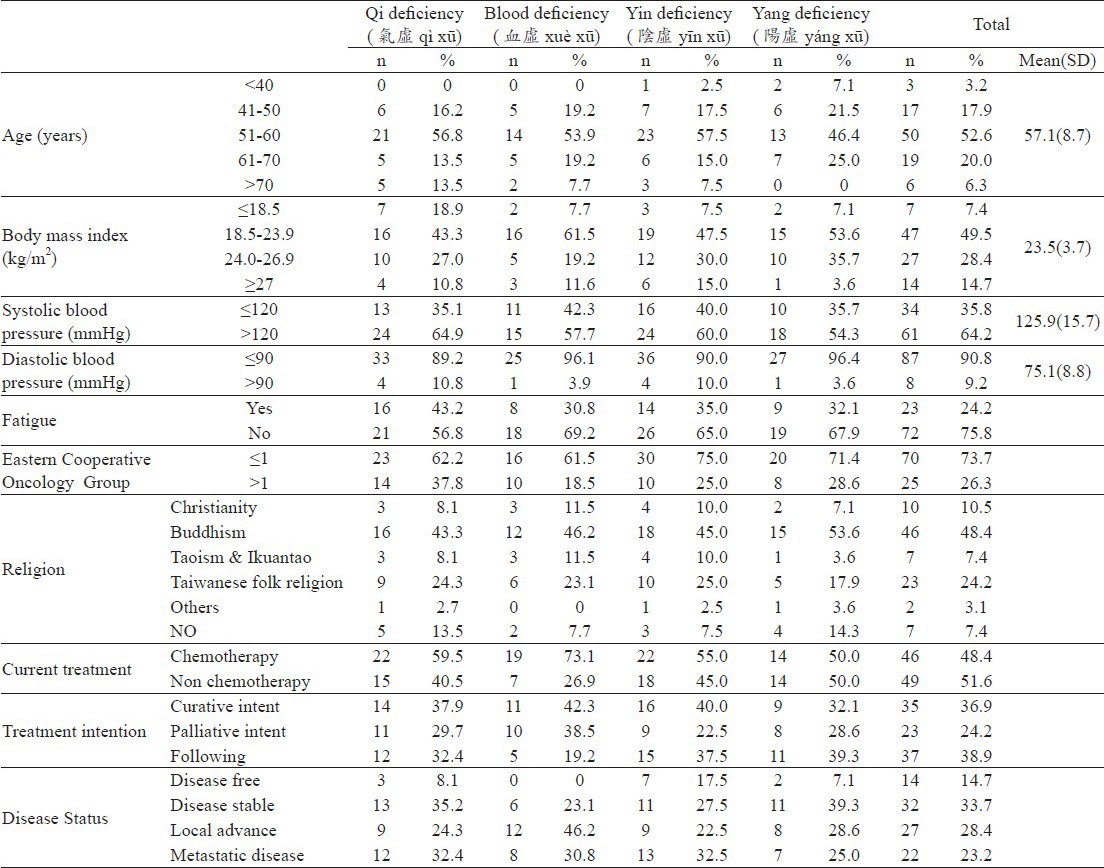
Demographics and clinical features of cancer patients
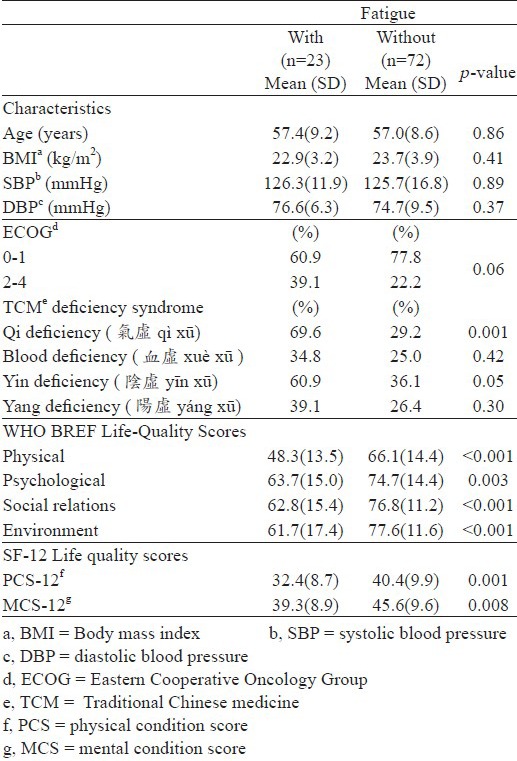
Of the total 95 breast cancer patients, the means (SD) of age, body mass index (BMI), and systolic/diastolic blood pressure were 57.1 (8.7) years, 23.5 (3.7) kg/m2, 125.9 (15.7)/75.1(8.8) mmHg, respectively. Most patients were 40-60 years old, which was compatible with the breast cancer epidemiology. Table 3 showed the baseline characteristics of the patients in different TCM DSGs. Twenty-four percent of patients were diagnosed with CRF and 43.2% of CRF had qi (氣 qì) DSG. Otherwise, 73.7% participants were showed relatively good performance (Eastern Cooperative Oncology Group, ECOG<=1); 48.4% were under chemotherapy.
Table 3.
Demographic characteristics of the participants.
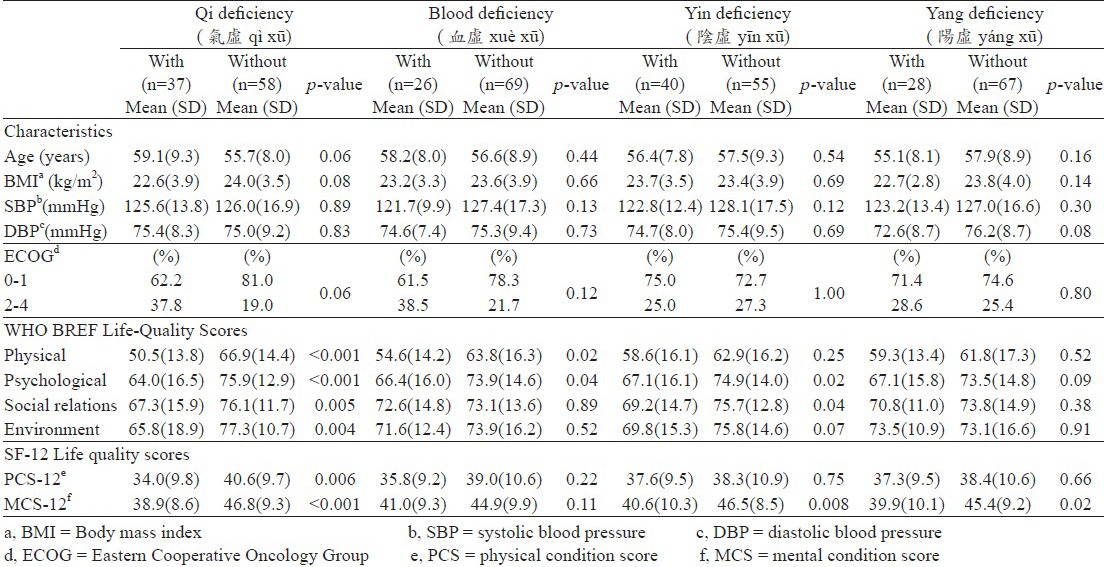
The comparison of QoL's scores between the with/without different TCM DSGs
Table 4 showed the comparison of QoL's scores for the with/without different TCM DSGs. The patients with qi deficiency (氣虛 qì xū) syndrome had lower QoL's scores in all domains of the WHO-BREF and SF12 survey. Besides, qi deficiency (氣虛 qì xū) significantly affected the QoL in the WHO-BREF physical, psychological (p<0.001), social relations (p=0.005), environment aspects (p=0.004), and mental aspect in SF12 (p<0.001). The blood deficiency (血虛 xuè xū) syndrome group had less impact on quality of life than qi deficiency (氣虛 qì xū), but significance was noted in the physical and psychological aspects (p=0.02; 0.04). Otherwise, yin deficiency (陰虛 yīn xū) was correlated with psychological (p=0.02) and social relations’ QoL domains (p=0.04) in the WHO-BREF, and also influenced the mental condition in the SF12 survey (p=0.008), whereas yang deficiency (陽虛 yang xū)was only related to Mental condition in the SF12 survey (p=0.02).
Table 4.
Comparison of QoL's scores among the with/without different TCM deficiency syndrome groups in breast cancer patients
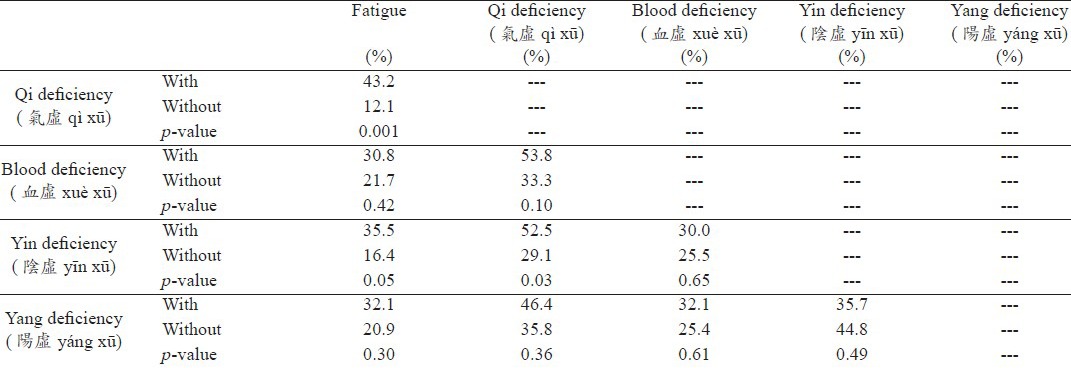
The intergroup analysis between the CRF and different TCM DSGs
Table 5 displays the intergroup analysis between the CRF and different TCM DSGs. Breast cancer patients with qi deficiency (氣虛 qì xū) had a significantly high percentage of CRF diagnosis (43.2%:12.1%; p=0.001), whereas the patients with yin deficiency (陰虛 yīn xū) also had CRF (35.5%:16.4%; p=0.05). The intergroup analysis of TCM deficiency syndrome revealed patients with qi deficiency (氣虛 qì xū) also tended to have yin deficiency (陰虛 yīn xū) (p=0.03).
Table 5.
Intergroup analysis of the CRF and different TCM deficiency syndrome groups in breast cancer patients
Comparison between with/without CRF in breast cancer patients
Table 6 compared the patients’ QoL scores and the TCM deficiency syndrome status between the with/without CRF. Patients with CRF had a higher percentage of qi deficiency (氣虛 qì xū) with great significance (69.6%; 29.2%; p=0.001). Deeper analysis also noted breast cancer patients with CRF also had poorer QoL over all domains in the WHO-BREF (physical: p<0.001; psychological: p=0.003; social: p<0.001; environment: p<0.001) and SF12 assessments. (PCS: p=0.001; MCS: p=0.008).
Table 6.
Comparison of with/without CRF in breast cancer patients
Discussion
Our initial findings that showed women with breast cancer with TCM deficiency syndrome and CRF had poor QoL scores. Among DSGs, the qi deficiency (氣虛 qì xū) group had the highest amount of CRF (43.2%:12.1%; p=0.001) and the lowest QoL's scores over the physical, psychological, social relations and environment aspects both in the WHO-BREF and SF12 surveys (Table 4). The element “Qi” (氣 qì)seems to play a critical role in the QoL of breast cancer patients. Lee et al (2005) also noted that qi (氣 qì) therapy may have beneficial psychological, physiological and immunological effects on health and help patients cope with their pain and mood disturbances (Lee et al., 2005).
The concept of TCM different deficiency syndrome has been widely applied in clinical practice in TCM for a long time. Doctors prescribe herb medication for the patients based on the type of syndrome. In our study, the analysis of the different deficiency syndromes indicated “qi” (氣 qì)is the most important element affecting the QoL in breast cancer patients, while a similar phenomenon has been noted in advanced non-small cell lung cancer (Yuan et al., 2011). Reviewing the ancient Chinese medication books, “qi” (氣 qì) is the commander of blood (血 xuè), and blood (血 xuè) is the mother of qi (氣 qì) (Tierra and Tierra, 1998). This means qi (氣 qì) attaches to the blood (血 xuè) and blood (血 xuè) supplies qi (氣 qì). This is also a manifestation of the mutual restriction of yin and yang. In TCM theory, “qi” (氣 qì) is the vital substance constituting the human body. It also refers to the physiologic functions of the organs and meridians in the human body with five functions: promoting, warming, defending, controlling and steaming. In fact, it may be difficult to find one equivalent English word that adequately describes its functions and properties. Several studies have indicated the positive effect of qi (氣 qì) therapy on symptom management and mood improvement in cancer patients (Lee et al., 2001; Lee et al., 2005), which may be compatible with our findings that qi (氣 qì)is one of the most important elements in health balance. It significantly affects QoL and is correlated with CRF. Future study on qi (氣 qì) therapy should more deeply examine the breast cancer patients.
Further, patients with qi deficiency (氣 虛 q ì xū) had a high correlation with yin deficiency (陰 虛 yīn xū) (p=0.03) in this study. Although there is a lack retrospective data on the relationships in syndrome intergroup analysis, some studies indicated yin deficiency (陰虛 yīn xū) may lead to impaired autonomic nervous system function in patients with metastatic cancer (Lin and Chen, 2010). Patients who lack the energy of qi (氣 qì) may simultaneously lack yin. (陰 yīn) Since yin in TCM represents a state of the human body lacking nutrition and fluid, yin deficiency (陰虛 yīn xū) is commonly seen in the late stage of cancer patients (Lin et al., 2008). It is no wonder that a certain percentage of patients with qi deficiency (氣虛 qì xū) also have yin deficiency (陰虛 yīn xū). We presume it may represent a more advanced disease status that is compatible with multiple elements deficiency.
Regarding CRF, patients with CRF also have a greater percentage of deficiency syndromes, especially qi deficiency (氣虛 qì xū) and yin deficiency (陰 虛 yīn xū) (Table 6). Meanwhile, much worse QoL scores were noted in patients with CRF groups over all physical, psychological, social relations, environment, and PCS-12, MCS-12 domains. Some studies have also indicated that patients with CRF have worse QoL and more cancer related symptoms that require management (Buchanan et al. 2005; Cavalli Kluthcovsky et al. 2011). Interestingly, there are some relationships between CRF and qi deficiency (氣虛 qì xū). We found 69.6% of patients with CRF have qi deficiency (氣虛 qì xū) while only 43.2% of patients with qi deficiency (氣虛 qì xū) have CRF, though both show statistical significance. This might be due to the diagnostic criteria of CRF (ICD.10), specifically excluding patients whose fatigue was considered to be caused by co-morbid psychiatric disorders, whereas qi deficiency (氣虛 qì xū) might detect the cancer related symptoms more broadly. Since there is an overlapping of the patients noted in CRF and qi deficiency (氣虛 qì xū) clinically, the patients who were diagnosed early as having qi deficiency (氣虛 qì xū) may also remind the doctor to prescribe qi (氣 qì) related therapy and support earlier.
There are still limitations to this study. First, the sample size is relatively small (n= 95), so a larger population of cancer patients will be required in a future study. Second, the treatment modalities or the patients’ disease status may display some bias on the QoL survey, and the association of these factors should be investigated in future studies.
In conclusion, patients with TCM deficiency syndromes had poorer QoL and CRF, which may need to be managed early, especially the qi deficiency (氣虛 qì xū) groups. The “qi” (氣 qì) may play an important role in the health balance of breast cancer patients. Therefore, qi (氣 qì) supply treatment may have a promising role in palliating the cancer related symptoms and improving the QoL. Qi (氣 qì) and yin (陰 yīn), are closely related to each other and need to be treated at the same time. Further research in this field would be of great help in TCM development of breast cancer patients’ care.
Acknowledgments
We thank all the patients who participated in this study and our colleagues in Taipei City Hospital, Taiwan for their help with this study. This research was financially supported by the Department of Health, Taipei City Government, Taiwan.
References
- 1.Ahlberg K., Ekman T., Gaston-Johnsson F., Mock V. Assessment and management of cancer-related fatigue in adults. Lancet. 2003;362:640–650. doi: 10.1016/S0140-6736(03)14186-4. [DOI] [PubMed] [Google Scholar]
- 2.Alexander S., Minton O., Stone P.C. Evaluation of screening instruments for cancer-related fatigue syndrome in breast cancer survivors. Journal of Clinical Oncology. 2009;27:1197–1201. doi: 10.1200/JCO.2008.19.1668. [DOI] [PubMed] [Google Scholar]
- 3.Bower J.E., Ganz P.A., Desmond K.A., Rowland J.H., Meyerowitz B.E., Belin T.R. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. Journal of Clinical Oncology. 2000;18:743–753. doi: 10.1200/JCO.2000.18.4.743. [DOI] [PubMed] [Google Scholar]
- 4.Buchanan D.R., O’Mara A.M., Kelaghan J.W., Minasian L.M. Quality-of-life assessment in the symptom management trials of the national cancer institute– supported community clinical oncology program. Journal of clinical oncology. 2005;23:591–598. doi: 10.1200/JCO.2005.12.181. [DOI] [PubMed] [Google Scholar]
- 5.Cavalli Kluthcovsky A.C., Urbanetz A.A., de Carvalho D.S., Pereira Maluf E.M., Schlickmann Sylvestre G.C., Bonatto Hatschbach S.B. Fatigue after treatment in breast cancer survivors: prevalence, determinants and impact on health- related quality of life. Supportive Care in Cancer. 2011 Oct 17; doi: 10.1007/s00520-011-1293-7. [DOI] [PubMed] [Google Scholar]
- 6.Cella D., Davis K., Breitbart W., Curt G. Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. Journal of Clinical Oncology. 2001;19:3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- 7.Gupta D., Lis C.G., Grutsch J.F. The relationship between cancer-related fatigue and patient satisfaction with quality of life in cancer. Journal of pain and symptom management. 2007;34:40–47. doi: 10.1016/j.jpainsymman.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Hann D.M., Denniston M.M., Baker F. Measurement of fatigue in cancer patients: further validation of the fatigue symptom inventory. Quality of Life Research. 2000;9:847–854. doi: 10.1023/a:1008900413113. [DOI] [PubMed] [Google Scholar]
- 9.Lee M.S., Yang K.H., Huh H.J., Kim H.W., Ryo I.T., Lee H.S. Qi therapy as an intervention to reduce chronic pain and to enhance mood in elderly subjects: a pilot study. American Journal of Chinese Medicine. 2001;29:237–245. doi: 10.1142/S0192415X01000277. [DOI] [PubMed] [Google Scholar]
- 10.Lee M.S., Yang S.H., Lee K.K., Moon S.R. Effects of Qi therapy (external Qigong) on symptoms of advanced cancer: a single case study. European Journal of Cancer Care. 2005;14:457–462. doi: 10.1111/j.1365-2354.2005.00599.x. [DOI] [PubMed] [Google Scholar]
- 11.Lin S.C., Chen M.F., Li T.C., Hsieh Y.H., Liu S.J. The distribution of Yin-Deficient symptoms and their relationship on survival rate in cancer patients with Yin-Deficiency. American Journal of Chinese Medicine. 2008;36:655–663. doi: 10.1142/S0192415X08006120. [DOI] [PubMed] [Google Scholar]
- 12.Lin S.C., Chen M.F. Increased yin-deficient symptoms and aggravated autonomic nervous system function in patients with metastatic cancer. Journal of Alternative and Complementary Medicine. 2010;16:1059–1063. doi: 10.1089/acm.2009.0487. [DOI] [PubMed] [Google Scholar]
- 13.Mast M.E. Correlates of fatigue in survivors of breast cancer. Cancer Nursing. 1998;21:136–142. doi: 10.1097/00002820-199804000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Müller-Nordhorn J., Roll S., Willich S.N. Comparison of the short form (SF) -12 health status instrument with the SF-36 in patients with coronary heart disease. Heart. 2004;90:523–527. doi: 10.1136/hrt.2003.013995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Portenoy R.K., Itri L.M. Cancer-related fatigue: guidelines for evaluation and management. Oncologist. 1999;4:1–10. [PubMed] [Google Scholar]
- 16.Portenoy R.K. Cancer-related fatigue: an immense problem. Oncologist. 2000;5:350–352. doi: 10.1634/theoncologist.5-5-350. [DOI] [PubMed] [Google Scholar]
- 17.Sadler I.J., Jacobsen P.B., Booth-Jones J.M., Belanger H., Weitzner M.A., Fields K.K. Preliminary evaluation of a clinical syndrome approach to assessing cancer- related fatigue. Journal of Pain and Symptom Management. 2002;23:406–416. doi: 10.1016/s0885-3924(02)00388-3. [DOI] [PubMed] [Google Scholar]
- 18.Tierra M., Tierra L. Diagnosis and Treatment. I. Wisconsin: Lotus Press; 1998. Chinese Traditional Herbal Medicine. [Google Scholar]
- 19.Van Belle S., Paridaens R., Evers G., Kerger J., Bron D., Foubert J., Ponnet G., Vander Steichel D, Heremans C., Rosillon D. Comparison of proposed diagnostic criteria with FACT-F and VAS for cancer- related fatigue: proposal for use as a screening tool. Supportive Care in Cancer. 2005;13:246–254. doi: 10.1007/s00520-004-0734-y. [DOI] [PubMed] [Google Scholar]
- 20.Vogelzang N.J., Breitbart W., Cella D., Curt G.A., Groopman J.E., Horning S.J., Itri L.M., Johnson D.H., Scherr S.L., Portenoy R.K. Patient caregiver, and oncologist perceptions of cancer-related fatigue: Results of a tri-part assessment survey. Seminars in Hematology. 1997;34:4–12. [PubMed] [Google Scholar]
- 21.Ware J.E., Kosinski M., Keller S.D. 3rd ed. Lincoln: Quality Metric incorporated; 1998. SF-12: how to score the SF-12 physical and mental health summary scales. [Google Scholar]
- 22.Yuan L., Zhang P.T., Yang Z.Y. Study on qi deficiency syndrome distribution and quality of life in patients with advanced non-small cell lung cancer. Chinese Journal Integrated Traditional and Western Medicine. 2011;31:880–883. [PubMed] [Google Scholar]


