Abstract
Background: Qi (氣 qì) refers to the vital energy of the body in Traditional Chinese medicines (TCM). Qi deficiency (氣虛 qì xū) is the most common symptom in cancer patients according to the concept of TCM. We hypothesized that cancer patients with Qi deficiency suffer from poor quality of life (QOL) and fatigue.
Method: Among the 256 registered cancer patients screened at our outpatient clinic, a total of 198 were enrolled. The inclusion criteria were (1) age between 18 and 70 years, (2) cancer diagnosis confirmed by the professional physician, (3) being Chinese, and (4) Eastern Cooperative Oncology Group (ECOG) performance status rating (PSR) ≤ 3. The major outcome is the difference in QOL score in cancer patients with and without Qi deficiency.
Results: The initial results showed statistically significant differences in WHO-QOL scores in physical, psychological, and social domains between the groups with and without Qi deficiency as well as the groups with and without cancerrelated fatigue (CRF). All patients with CRF present were also diagnosed as Qi deficient. In addition, among the patients with no CRF, 39.9% (69/173) were diagnosed as suffering from Qi deficiency, which led to poor QOL.
Conclusions: The present study showed statistically significant difference in WHO-QOL scores in physical, psychological, and social domains between the groups with and without Qi deficiency as well as the groups with and without CRF. Cancer patients diagnosed with Qi deficiency or CRF have poor QOL. The concept of Qi deficiency in TCM might be applied to cancer health care.
Keywords: Qi deficiency, Fatigue, Cancer-related Fatigue, Quality of life, Traditional Chinese Medicine
Introduction
Complementary and alternative medicines (CAMs), in particular herbal medicine and traditional Chinese medicine (TCM), are commonly used by cancer patients in Chinese-speaking population and Asian countries (Hsiao and Liu, 2010; Konkimalla and Efferth, 2008; Wu et al., 2009). TCM in combination with chemotherapy or radiotherapy can enhance the efficacy and ameliorate the side effects and complications caused by chemotherapy or radiotherapy (Chan et al., 2011; Qi et al., 2010). Syndrome differentiation of TCM plays a main role in treatment of cancer patients (Seki et al., 2005; Sun et al., 2010). The impairment of Qi (氣 qì) flow within the body is often observed in cancer patients who choose TCM as adjuvant treatment (Qi et al., 2010; Seki et al., 2005; Sun et al., 2010).
Fatigue is a common symptom or complaint among cancer patients (Wagner and Cella, 2004; Kontos and Viswanath, 2011; Stasi et al., 2003). Cancer-related fatigue (CRF) affects quality of life (QOL) including physical, mental and psychosocial aspects (Barsevick et al., 2010). Qi refers to the vital energy of the body in TCM. It maintains blood circulation, warms the body and fights diseases. Qi deficiency (氣虛 qì xū) is the most common symptom in cancer patients according to the concept of TCM. Many previous reports showed that Qi supplementation (補氣 bǔ qì) can help enhance the effects of cancer therapy (Chui et al., 2005; Li et al., 2007; Qi et al., 2010; Seki et al., 2005; Yan et al., 2008; Yan et al., 2010); and hence, the main role of TCM in cancer therapy is to balance the Qi flow in cancer patients. In addition, the QOL of cancer patients may be affected by Qi deficiency and CRF. In view of the above, we conducted this cross-sectional study to explore the relationship between Qi deficiency, CRF and QOL in cancer patients.
Materials and Methods
Study design and participants
This was a cross-sectional study conducted from January 2010 through December 2010 in Taipei City Hospital, Taiwan. Among the 256 registered cancer patients screened at our outpatient clinic, a total of 198 were enrolled. The inclusion criteria were (1) age between 18 and 70 years, (2) cancer diagnosis confirmed by the professional physician, (3) being Chinese, and (4) Eastern Cooperative Oncology Group (ECOG) performance status rating (PSR) ≤ 3. The exclusion criteria were (1) unconsciousness, (2) delirium and psychiatric, (3) complications present, and (4) any other conditions not suitable for study as evaluated by the physician-in-charge. The major outcome is the difference in QOL score in cancer patients with and without Qi deficiency. The protocol was approved by the Human Ethics Committee of our hospital. Informed consent was obtained from all the enrolled patients.
Qi deficiency
TCM practitioners make diagnosis in terms of Yin (陰 yīn), Yang (陽 yáng), Qi, Blood, and Organ (器 qì) imbalance on the basis of signs and symptoms observed by the doctors and reported by the patients. In cancer patients, Qi deficiency is the most common symptom. However, there are no existing questionnaires or diagnostic tools for Qi deficiency. Hence, we chose to use the interview approach, which is a common diagnostic method adopted by TCM practitioners. With the aim to devise a simple and efficient screening tool, nine TCM doctors with clinical experience referred to relevant references (Hu et al., 2005; WHO, 2007) and developed three yes-no questions for diagnosing Qi deficiency among cancer patients according to the concept of TCM. The questionnaire designed contained the following.
In the past week, did you often have the following symptoms?
(Often means more than 8 hour per day and more than four days per week)
-
(1)
Felt exhausted or lack of energy
-
(2)
Did not feel like talking or talked in a low and weak voice.
-
(3)
Did not feel like moving about or did not have the strength to walk.
Cancer patients responding yes to two questions or more in the interview would be classified as being Qi deficient. Validation test results showed an alpha coefficient of 0.89 and Cronbach's alpha coefficient of 0.88, indicating that the questionnaire has good reliability.
Cancer-related fatigue
Fatigue caused by cancer or cancer therapy had been proposed for recognition by the World Health Organization (WHO) and for publication in the International Statistical Classification of Diseases and Related Health problems (10th revision) (ICD-10) (Lesage and Portenoy, 2002). We adopted the criteria of cancer-related fatigue (CRF) in ICD-10, which have been validated and recommended as a diagnostic tool for CRF (Cella et al., 2001; Van Belle et al., 2005). In the ICD-10 criteria for diagnosis of CRF, fatigue is defined as present when the patient experienced six or more of the 11 symptoms listed. The 11 symptoms designed contained the following (Cella et al., 2001).
Six (or more) of the following symptoms have been present every day or nearly every day during the same 2-week period in the past month, and at least one of the symptoms is (A1) significant fatigue.
A1. Significant fatigue, diminished energy, or increased need to rest, disproportionate to any recent change in activity level
A2. Complaints of generalized weakness or limb heaviness
A3. Diminished concentration or attention
A4. Decreased motivation or interest to engage in usual activities
A5. Insomnia or hypersomnia
A6. Experience of sleep as unrefreshing or nonrestorative
A7. Perceived need to struggle to overcome inactivity
A8. Marked emotional reactivity (eg, sadness, frustration, or irritability) to feeling fatigued
A9. Difficulty completing daily tasks attributed to feeling fatigued
A10. Perceived problems with short-term memory
A11. Postexertional malaise lasting several hours
B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
C. There is evidence from the history, physical examination, or laboratory findings that the symptoms are a consequence of cancer or cancer therapy.
D. The symptoms are not primarily a consequence of comorbid psychiatric disorders such as major depression, somatization disorder, somatoform disorder, or delirium.
Quality of Life
To measure the quality of life among our subjects, we used the self-administered questionnaire of WHOQoL-BREF, Taiwan version, which was well validated with consistency coefficients ranging from 0.70 to 0.77 (Yao et al., 2002). The WHOQoL-BREF questionnaire evaluated quality of life in physical, psychological, social and environmental domains, with scores ranging from 0 to 100.
Outcome measurements
All subjects had to answer questions concerning Qi deficiency and CRF in ICD-10 posed by the attending physician during the outpatient follow-up session. They also had to complete the self-administered WHOQoL-BREF, Taiwan version under the assistance of the physician-in-charge. Standardized procedures for measurement were set up and all participating physicians received prior training before the study on how to interview the patients and assist them in completing the questionnaire. Physical measurements were made with subjects in their undergarments with a hospital gown on. Height was measured with a wall-mounted stadiometer to the nearest 0.1 cm, weight was measured on a calibrated balance beam scale to the nearest 0.1 kg, and BMI was calculated according to the formula: BMI = BW / height square (kg/m2). The major outcome is the difference in QOL score in cancer patients with and without Qi deficiency.
Statistical analysis
The data were analyzed using SPSS software (version 11.5). Student t-test was employed to examine the main outcomes, demographic data, and score of QOL. Chi- square test was used for comparison between gender (male/female) and percentage of positive response (yes%) between groups. One-way ANOVA tests were employed to examine the means among groups. All p values were two-tailed and the α level of significance was set at 0.05.
Results
Demographics and clinical features of cancer patients
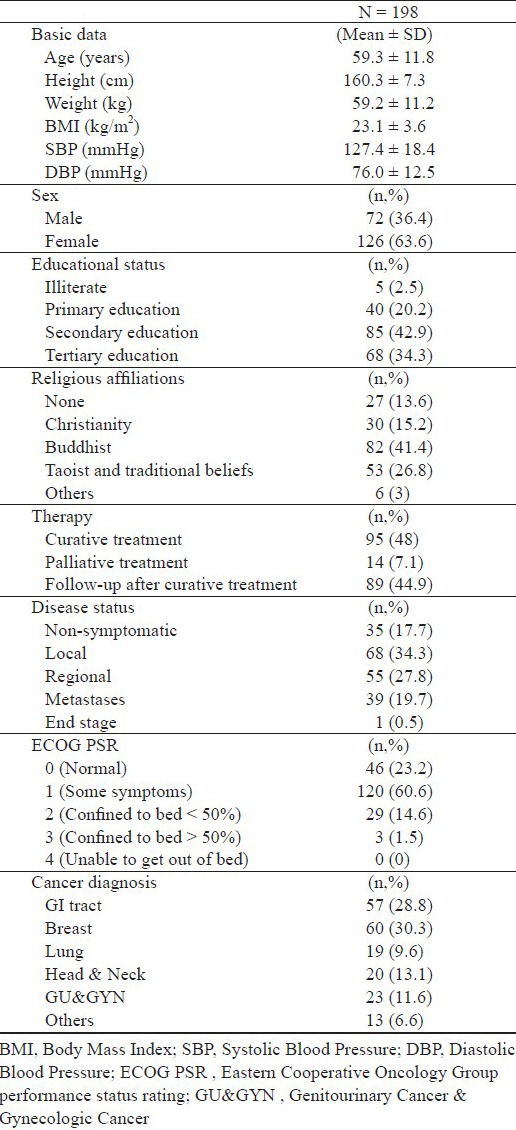
Among the 256 registered cancer patients screened at our outpatient clinic, a total of 198 fulfilled the inclusion criteria. Table 1 shows the demographic and clinical features of the study cohort. As can be seen, the means (SD) of age, BMI, and systolic/diastolic blood pressure were 59.3 (11.8) years, 23.1 (3.6) kg/m2, 127.4 (18.4)/76.0(12.5) mmHg, respectively. 48% subjects received curative treatment, 34.3% subjects had local invasive, and more than 80% subjects with ECOG <=1.
Table 1.
Demographic and clinical features of cancer patients
Quality of life in cancer patients with/without qi deficiency and with/without CRF
Table 2 displays the WHO-QOL scores among patients with/without Qi deficiency and those with/without CRF. As can be seen, there were significant differences in WHO-QOL scores in physical, psychological, and social domains.
Table 2.
Demographic characteristics and WHO-QOL scores of Cancer Patients with/without Qi Deficiency and those with/without cancer-related fatigue
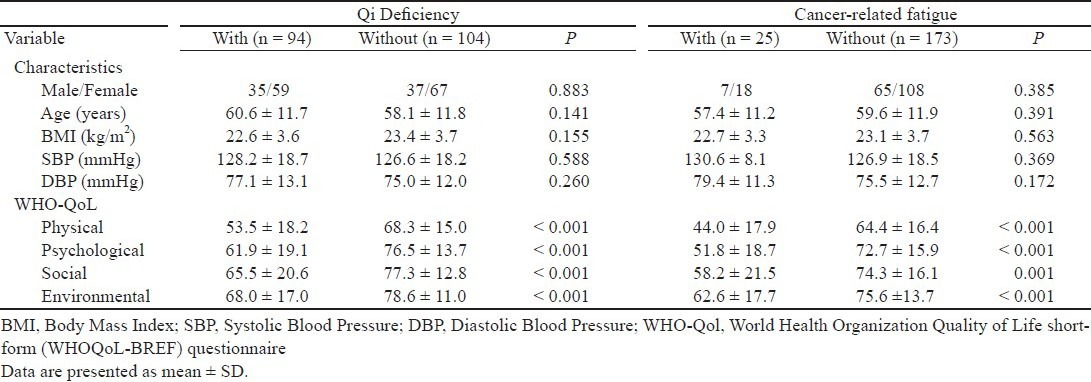
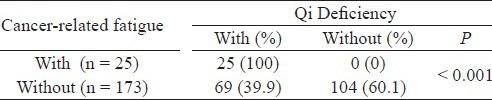
Table 3 shows the correlation between patients with/ without qi deficiency and those with/without CRF. As can be seen, the correlation is significant at p < 0.001, indicating the existence of an association between the two groups. All patients diagnosed with Qi deficiency also had CRF present. In addition, there was still 39.9% (69/173) of Qi-deficient patients in the group diagnosed with cancer having no CRF.
Table 3.
Correlations between Cancer Patients with/without Qi deficiency and those with/without cancer-related fatigue
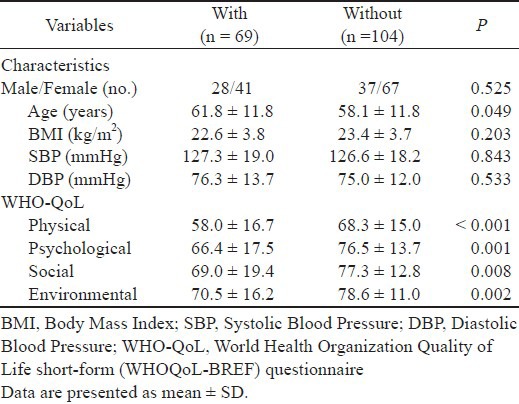
Quality of life in no-CRF cancer patients with and without Qi deficiency
Table 4 shows the demographic characteristics and WHO-QOL scores of the 173 no-CRF cancer patients with and without Qi deficiency. As can be seen, there were significant differences in WHO-QOL scores in physical, psychological, and social domains between patients with and without Qi deficiency. Qi-deficient cancer patients, even without CRF, had significantly lower WHO-QOL scores. In other words, despite of not suffering from CRF, cancer patients with Qi deficiency have poorer quality of life.
Table 4.
Demographic Characteristics and WHO-QOL scores of Nocancer-related fatigue Cancer Patients with and without Qi Deficiency Qi Deficiency
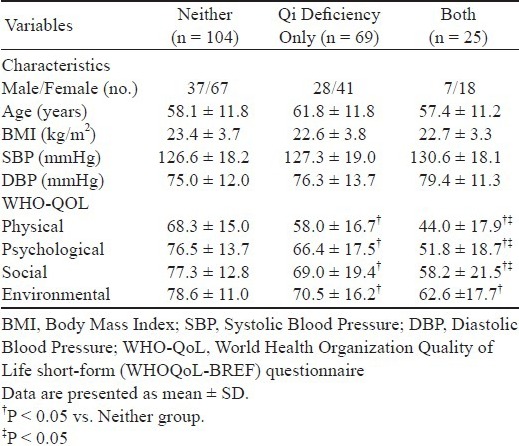
Quality of life in patients with neither Qi deficiency nor CRF, Qi deficiency only, and both
Table 5 shows the demographic characteristics and WHO-QOL scores of patients with neither Qi deficiency nor CRF, Qi deficiency only, and both. As can be seen, there were significant differences in WHO-QOL scores in physical, psychological, and social domains in all three groups of patients. Among them, cancer patients with both Qi deficiency and CRF have the lowest WHO-QOL scores, followed by those with Qi deficiency. Cancer patients with neither Qi deficiency nor CRF have the highest WHO-QOL scores.
Table 5.
Demographic characteristics and WHO-QOL scores of patients with neither Qi deficiency nor cancer-related fatigue, Qi deficiency only, and both
Discussion
CRF is the most prevalent symptom in cancer patients (Wagner and Cella, 2004). CRF is a clinical manifestation, and different definition and measurement have different prevalence in many previous studies (Campos et al., 2011; de John et al., 2004; Irvine et al., 1994; Molassiotis and Chan, 2004). In this study, we adopted the ICD-10 criteria for diagnosing CRF. Cancer patients are diagnosed as suffering from CRF if they have felt lack of energy, or an increased need to rest for at least 2 weeks over the last month, and have experienced more than 5 of the 10 common clinical sensations (generalized weakness, diminished concentration, decreased motivation, insomnia, experience of sleep as un-refreshing, perceived need to struggle to overcome inactivity, marked emotional reactivity (e.g., sadness, frustration, or irritability) to feeling fatigued, difficulty completing daily tasks attributed to feeling fatigued, perceived problems with short-term memory, and post-exertional malaise lasting several hours). Using the ICD-10 CRF diagnosis criteria, Cella et al. found fatigue presented in 17% of cancer patients receiving chemotherapy or radiation therapy while Sadler et al. reported 21% of patients undergoing blood or bone marrow transplantation having fatigue (Cella et al., 2001; Sadler et al., 2002). In the present study, only 12.6% (25/198) of our subjects were diagnosed with CRF. The relatively low percentage of patients with CRF may be attributed to the majority of patients (166, 82.3%, Table 1) having mild symptoms with ECOG PSR l 1.
In TCM, Qi is the vital energy that maintains blood circulation, warms the body and fights diseases. From our clinical experiences and description in old book of Chinese medicine, severe Qi deficiency is prevalent among cancer patients during treatment or even long after treatment, thus affecting their QOL. To our knowledge, there was currently no diagnostic or screening tool for detecting Qi deficiency in cancer patients. Hence, we attempted to develop a simple tool or questionnaire for screening patients with Qi deficiency according to the concept of TCM and our clinical experiences.
In this study, 47.5% (94/198) of the subjects were diagnosed with Qi deficiency while only 12.6% (25/198) of the subjects were diagnosed with CRF. Both of these two groups had low QOL scores. In addition, all patients diagnosed with CRF had Qi deficiency while 39.9% (69/173) of patients with Qi deficiency were diagnosed as having no CFR. From the clinical perspective of health care provision, regardless of whether cancer patients had CRF, Qi deficiency or other discomfort sensations, these symptoms should be taken into consideration. The present results showed that cancer patients with CRF and Qi deficiency had low QOL scores and greater attention should be given to them by the health care team for cancer patients. As mentioned, among those not present with CRF, there was 39.9% (69/173) with Qi deficiency, who had poor QOL and needed extra clinical care. In view of this, Qi deficiency can serve alone or in addition to CRF as an indicator for care required and attention needed.
As seen in Table 5, there was a statistically significant trend of poor QOL in physical, psychological and social domains with the diagnosis among neither, only qi deficiency and both qi deficiency and CRF groups, compared to the group with neither qi deficiency nor CRF. Among them, cancer patients with both Qi deficiency and CRF have the lowest WHO-QOL scores, followed by those with Qi deficiency. Cancer patients with neither Qi deficiency nor CRF have the highest WHO-QOL scores. The initial findings suggested that Qi diagnosis method might help in examining the different levels of QOL for cancer patients. Many reports showed that improvement in Qi flow have beneficial effects on cancer patients (Chui et al., 2005; Li et al., 2007; Li et al., 2008; Qi et al., 2010; Sang et al., 2004; Seki et al., 2005; Yan et al., 2008; Yan et al., 2010) with different mechanisms involved (Greenwood, 1999; Lu and Li, 2009; Wang et al., 2010; Zhang et al., 2006). Further in vivo and in vitro studies are needed to explore this.
A limitation of this study is that only three questions were designed for diagnosing or screening Qi deficiency, which may result in false positive or overestimation. Whether more questions should be included remains inconclusive. Nevertheless, this study proves that the three questions designed have provided an easy and quick screening tool for patients having Qi deficiency with valid differentiation results.
In summary, the present study showed statistically significant difference in WHO-QOL scores in physical, psychological, and social domains between the groups with and without Qi deficiency as well as the groups with and without CRF. Cancer patients diagnosed with Qi deficiency or CRF have poor QOL. The concept of Qi deficiency in TCM might be applied to cancer health care. Related studies are worth more in-depth investigation in future.31
Acknowledgments
We thank Chun-Ying Lie, You-Lung Song, Ching- Min Luo, Yung-Jen Tsai and all colleagues in Taipei City Hospital, Taiwan for their help with this study. This research was financially supported by the Department of Health, Taipei City Government, Taiwan, under grant 991104.
References
- 1.Barsevick A., Frost M., Zwinderman A., Hall P., Halyard M. GENEQOL Consortium. I’m so tired: biological and genetic mechanisms of cancer-related fatigue. Quality of Life Research. 2010;19:1419–1427. doi: 10.1007/s11136-010-9757-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campos M.P., Hassan B.J., Riechelmann R., Del Giglio A. Cancer-related fatigue: a practical review. Annals of Oncology. 2011;22:1273–1279. doi: 10.1093/annonc/mdq458. [DOI] [PubMed] [Google Scholar]
- 3.Cella D., Davis K., Breitbart W., Curt G., Fatigue Coalition. Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. Journal of Clinical Oncology. 2001;19:3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- 4.Chan K.K., Yao T.J., Jones B., Zhao J.F., Ma F.K., Leung C.Y., Lau S.K., Yip M.W., Ngan H.Y. The use of Chinese herbal medicine to improve quality of life in women undergoing chemotherapy for ovarian cancer: adouble - blind placebo - controlled randomized trial with immunological monitoring. Annals of Oncology. 2011;22:2241–2249. doi: 10.1093/annonc/mdq749. [DOI] [PubMed] [Google Scholar]
- 5.Chui Y.Y., Donoghue J., Chenoweth L. Responses to advanced cancer: Chinese-Australians. Journal of Advanced Nursing. 2005;52:498–507. doi: 10.1111/j.1365-2648.2005.03618.x. [DOI] [PubMed] [Google Scholar]
- 6.de Jong N., Candel M.J., Schouten H.C., Abu-Saad H.H., Courtens A.M. Prevalence and course of fatigue in breast cancer patients receiving adjuvant chemotherapy. Annals of Oncology. 2004;15:896–905. doi: 10.1093/annonc/mdh229. [DOI] [PubMed] [Google Scholar]
- 7.Greenwood M. Energetics and transformation: insights on the paradoxical opportunity presented by chronic illness and pain - Part III. American Journal of Acupuncture. 1999;27:51–56. [PubMed] [Google Scholar]
- 8.Hsiao W.L., Liu L. The role of traditional Chinese herbal medicines in cancer therapy - from TCM theory to mechanistic insights. Planta Medica. 2010;76:1118–1131. doi: 10.1055/s-0030-1250186. [DOI] [PubMed] [Google Scholar]
- 9.Hu L., Lao S.X., Tang C.Z. Expression of bcl-2 oncogene in gastric precancerous lesions and its correlation with syndromes in traditional Chinese medicine. World Journal of Gastroenterology. 2005;11:3293–3296. doi: 10.3748/wjg.v11.i21.3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Irvine D., Vincent L., Graydon J.E., Bubela N., Thompson L. The prevalence and correlates of fatigue in patients receiving treatment with chemotherapy and radiotherapy. A comparison with the fatigue experienced by healthy individuals. Cancer Nursing. 1994;17:367–378. [PubMed] [Google Scholar]
- 11.Konkimalla V.B., Efferth T. Evidence-based Chinese medicine for cancer therapy. Journal of Ethnopharmacology. 2008;116:207–210. doi: 10.1016/j.jep.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Kontos E.Z., Viswanath K. Cancer-related direct-to-consumer advertising: a critical review. Nature Reviews Cancer. 2011;11:142–150. doi: 10.1038/nrc2999. [DOI] [PubMed] [Google Scholar]
- 13.Lesage P., Portenoy R.K. Management of fatigue in the cancer patient. Oncology (Williston Park) 2002;16:373–378. 381. [PubMed] [Google Scholar]
- 14.Li J., Sun G.Z., Lin H.S., Pei Y.X., Qi X., An C., Yu J., Hua B.J. The herb medicine formula “Yang Wei Kang Liu” improves the survival of late stage gastric cancer patients and induces the apoptosis of human gastric cancer cell line through Fas/Fas ligand and Bax/Bcl-2 pathways. International Immunopharmacolpgy. 2008;8:1196–1206. doi: 10.1016/j.intimp.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Li X., Shi Z.M., Feng P., Wen Z.Y., Wang X.J. Effect of Qi- protecting powder (Huqi San) on expression of c-jun, c-fos and c-myc in diethylnitrosamine-mediated hepatocarcinogenesis. World Journal of Gastroenterology. 2007;13:4192–4198. doi: 10.3748/wjg.v13.i31.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu X., Li B. Exploration of the effect and mechanism of activating blood circulation and stasis-removing therapy on tumor metastasis. Chinese Journal of Integrative Medicine. 2009;15:395–400. doi: 10.1007/s11655-009-0395-2. [DOI] [PubMed] [Google Scholar]
- 17.Molassiotis A., Chan C.W. Fatigue patterns in Chinese patients receiving radiotherapy. European Journal of Oncology Nursing. 2004;8:334–340. doi: 10.1016/j.ejon.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 18.Qi F., Li A., Inagaki Y., Gao J., Li J., Kokudo N., Li X.K., Tang W. Chinese herbal medicines as adjuvant treatment during chemo- or radio-therapy for cancer. BioScience Trends. 2010;4:297–307. [PubMed] [Google Scholar]
- 19.Sadler I.J., Jacobsen P.B., Booth-Jones M., Belanger H., Weitzner M.A., Fields K.K. Preliminary evaluation of a clinical syndrome approach to assessing cancer-related fatigue. Journal of Pain and Symptom Management. 2002;23:406–416. doi: 10.1016/s0885-3924(02)00388-3. [DOI] [PubMed] [Google Scholar]
- 20.Sang H. Clinical and experimental research into treatment of hysteromyoma with promoting qi flow and blood circulation, softening and resolving hard lump. Journal of Traditional Chinese Medicine. 2004;24:274–279. [PubMed] [Google Scholar]
- 21.Seki K., Chisaka M., Eriguchi M., Yanagie H., Hisa T., Osada I., Sairenji T., Otsuka K., Halberg F. An attempt to integrate Western and Chinese medicine: rationale for applying Chinese medicine as chronotherapy against cancer. Biomedicine & Pharmacotherapy. 2005;59:132–140. doi: 10.1016/s0753-3322(05)80021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stasi R., Abriani L., Beccaglia P., Terzoli E., Amadori S. Cancer-related fatigue: evolving concepts in evaluation and treatment. Cancer. 2003;98:1786–1801. doi: 10.1002/cncr.11742. [DOI] [PubMed] [Google Scholar]
- 23.Sun D.Z., Liu L., Jiao J.P., Wei P.K., Jiang L.D., Xu L. Syndrome characteristics of traditional Chinese medicine: summary of a clinical survey in 767 patients with gastric cancer. Journal of Chinese Integrative Medicine. 2010;8:332–340. doi: 10.3736/jcim20100406. [DOI] [PubMed] [Google Scholar]
- 24.Van Belle S., Paridaens R., Evers G., Kerger J., Bron D., Foubert J., Ponnet G., Vander Steichel D., Heremans C., Rosillon D. Comparison of proposed diagnostic criteria with FACT-F and VAS for cancer-related fatigue: proposal for use as a screening tool. Support Care in Cancer. 2005;13:246–254. doi: 10.1007/s00520-004-0734-y. [DOI] [PubMed] [Google Scholar]
- 25.Wagner Li, Cella D. Fatigue and cancer: causes, prevalence and treatment approaches. British Journal of Cancer. 2004;91:822–828. doi: 10.1038/sj.bjc.6602012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S., Penchala S., Prabhu S., Wang J., Huang Y. Molecular basis of traditional Chinese medicine in cancer chemoprevention. Current Drug Discovery Technologies. 2010;7:67–75. doi: 10.2174/157016310791162794. [DOI] [PubMed] [Google Scholar]
- 27.WHO Library Cataloging in Publication Data; World Health Organization 2007. WHO International Standard terminologies on traditional medicine in the Western Pacific region. [Google Scholar]
- 28.Wu P., Dugoua J.J., Eyawo O., Mills E.J. Traditional Chinese Medicines in the treatment of hepatocellular cancers: a systematic review and meta-analysis. Journal of Experimental & Clinical Cancer Research. 2009;28:112. doi: 10.1186/1756-9966-28-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yan X., Shen H., Jiang H., Hu D., Zhang C., Wang J., Wu X. External Qi of Yan Xin Qigong induces apoptosis and inhibits migration and invasion of estrogen-independent breast cancer cells through suppression of Akt/NF-kB signaling. Cellular Physiology and Biochemistry. 2010;25:263–270. doi: 10.1159/000276560. [DOI] [PubMed] [Google Scholar]
- 30.Yan X., Shen H., Jiang H., Zhang C., Hu D., Wang J., Wu X. External Qi of Yan Xin Qigong induces G2/M arrest and apoptosis of androgen-independent prostate cancer cells by inhibiting Akt and NF-kappa B pathways. Molecular and Cellular Biochemistry. 2008;310:227–234. doi: 10.1007/s11010-007-9684-2. [DOI] [PubMed] [Google Scholar]
- 31.Yao G., Chung C.W., Yu C.F., Wang J.D. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. Journal of the Formosan Medical Association. 2002;101:342–351. [PubMed] [Google Scholar]
- 32.Zhang T., Ma S.L., Xie G.R., Deng Q.H., Tang Z.Z., Pan X.C., Zhang M., Xu S. Clinical research on nourishing yin and unblocking meridians recipe combined with opioid analgesics in cancer pain management. Chinese Journal of Integrative Medicine. 2006;12:180–184. doi: 10.1007/BF02836518. [DOI] [PubMed] [Google Scholar]


