Abstract
Context:
Hyponatremia is a common electrolyte disturbance in critically ill hence understanding its implications is important.
Aims:
This study was carried out to ascertain frequency, predisposing conditions and outcome in critically ill patients with hyponatremia on intensive care unit (ICU) admission.
Settings and Design:
This was an observational, prospective study of a series of ICU patients during a 12-month period.
Materials and Methods:
The patients were divided into two groups: Hyponatremic (serum sodium < 135 mmol/L) and Eunatremic groups (135-145 mmol/L). Clinical examination included volume status and drug history, biochemistries, clinical diagnosis and cause of hyponatremia.
Statistical Analysis Used:
Fisher's exact test, unpaired t-tests Wilcoxon ranksum tests, profile-likelihood method, log-rank test and Kaplan—Meier curves were used. P < 0.05 were considered to be statistically significant.
Results:
In the hyponatremic group, the frequency of hyponatremia on ICU admission was 34.3%, most were euvolumic, 58.96%. Females comprised of 36.5%. The mean age was 60.4 ± 17.2. The Syndrome of inappropriate Antidiuretic Hormone (SIADH) criteria was met in ninety-one patients (36.25%), peumonia being the leading cause of SIADH. Patients with severe sepsis, elective surgery patients, renal failure and heart failure, cirrhosis of liver and subarachnoid hemorrhage were other more likely etiologic causes (P < 0.05). The hyponatremic group spent a longer time in the ICU (P = 0.02), had longer mechanical ventilator days (P < 0.05) and had an increased mortality rate (P = 0.01).
Conclusions:
Hyponatremia present on admission to the ICU is independent risk factors for poor prognosis.
Keywords: Critically ill, epidemiology, hyponatremia
Introduction
Hyponatremia is a common electrolyte disturbance occurring in critically ill patients.[1] Symptoms range from nausea and malaise, with mild reduction in the serum sodium, to lethargy, decreased level of consciousness, headache, seizures and coma.
Hyponatremia can be classified on the basis of serum osmolality, volume status and urinary sodium into hypertonic, isotonic and hypotonic types. Hypotonic hyponatremia is further classified into hypervolemic, euvolemic and hypovolemic as follows:[2]
Hypovolemic hyponatremia: Decreased total body sodium and decreased total body water. The sodium deficit exceeding water deficit
Euvolemic hyponatremia: Normal body sodium with increase in total body water
Hypervolemic hyponatremia: Increase in total body sodium with greater increase in total body water.
The treatment of hyponatremia depends on the duration of hyponatremia and volume status of the patients. There is serious neurologic sequel if hyponatremia is inappropriately treated. Limited data is available on whether the presence of hyponatremia on intensive care unit (ICU) admission is independently associated with excess mortality. This study was done to ascertain the frequency, aetiology and outcome in critically ill patients admitted to the ICU with hyponatremia.
Materials and Methods
This was an observational, prospective study of a series of ICU patients during a 12-month period. Hyponatremia was defined as a serum sodium level less than 135 mmol/L. Patients with hyperlipedemias, paraprotenemias (Pseudohyponatremia) and those receiving mannitol, radiographic contrast agents, or having hyperglycemia (translocational hyponatremia) and patients with hypernatremia were excluded. The patients were divided into two groups: Hyponatremic (serum sodium level less than 135 mmol/L) and normal serum sodium (135-145 mmol/L) groups. Hyponatremic patients were further divided into three groups as per volume status as discussed above. History and clinical examination was recorded in all the patients at the time of ICU admission. Detailed drug history was recorded; especially the use of thiazides diuretics and selective serotonin reuptake inhibitors (SSRIs) and clinical evaluation of volume status was done. Parameters for patients including presence of acute renal failure, need for mechanical ventilator and ventilator days, duration of ICU and hospital stay (days) were recorded as observational data and other variables useful to calculate Acute Physiology and Chronic Health Evaluation II (APACHE II) and the sequential organ failure assessment scores were also recorded.[3]
Laboratory data included values for complete blood count, fasting blood glucose, serum potassium (K), serum urea, serum creatinine, serum uric acid, liver function tests, lipid profile, morning serum cortisol, thyroid function tests. Urine sodium, urine osmolality, serum osmolality, serum sodium were analyzed directly with an iron specific electrode (Cobas b 121 POC system blood gas analyzer and patients were diagnosed to have Syndrome of inappropriate Antidiuretic Hormone (SIADH) if they met its criteria as proposed by Bartter and Schwartz in 1967.[4]
Statistical analysis
Statistical analysis used: Fisher's exact test, unpaired t-tests Wilcoxon ranksum tests, Mantel-cox test, profile-likelihood method, log-rank test, Pearson's test and Kaplan-Meier curves were used. All P values were 2-tailed and P < 0.05 were considered to be statically significant.
Results
A total of 730 patients were studied, out of which 27 patients were excluded due to presence of hypernatremia (serum sodium > 145 mmol/L), one patient had paraprotenemia and another with hypertrig lyceredemia were excluded. The base line characteristic of study patients is given in Table 1. Of the remaining 699 patients most had normal serum sodium (448, 66.9%). The frequency of hyponatremia on ICU admission was 34.3% of all ICU admissions incidence rate ratio, 1.61; 95% confidence interval [CI], 1.15-2.25, P < 0.01. Females comprised of 56.5% of hyponatremic patients and 39.9% of normal serum sodium group. Patients who were taken up for elective surgery were more likely to have hyponatremia than emergency surgery patients (P < 0.01). The mean age of patients with hyponatremia was 60.4 ± 17.2. The hyponatremic group had significantly higher APACHE II score when compared to those of the normal serum sodium group (P < 0.01). 91 patients (36.25%) of the hyponatremic group met the criteria for a diagnosis of SIADH. The largest group of hyponatremic patients were euvolumic; 148 (58.96%) followed by hypervolumic; 66 (26.29%) and hypovolumic; 37 (14.74%). Etiologic factors causing hyponatremia is given in Figure 1 and Table 2.
Table 1.
Baseline characteristics of the patients*
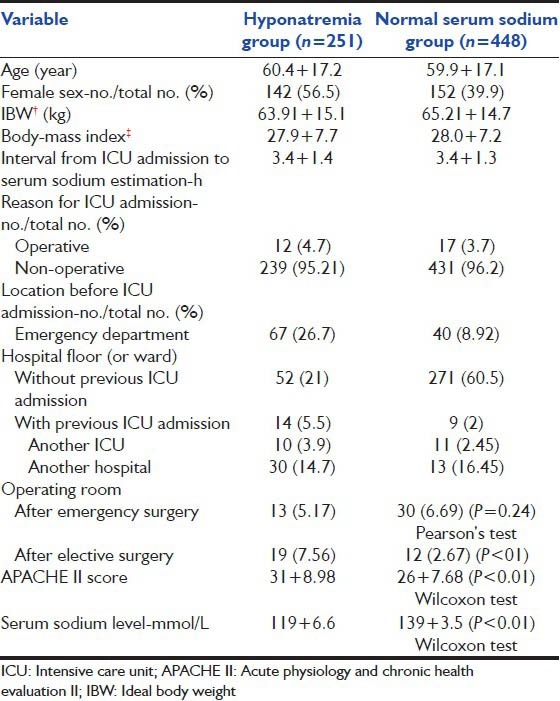
Figure 1.
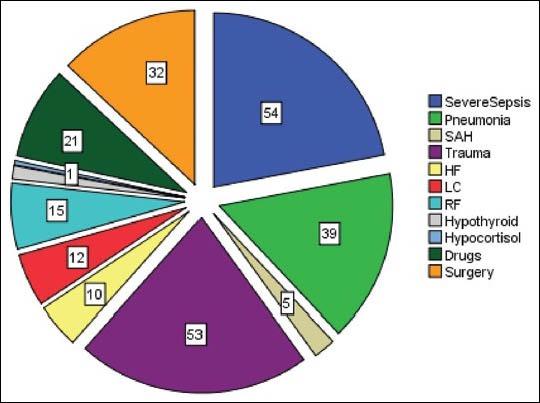
Etiologic factors associated with hyponatremia. SAH = Subarac hnoid haemorrhage, HF = Heart failure, LC = Liver cirrhosis, RF = Renal failure
Table 2.
Etiologic factors associated with hyponatremia
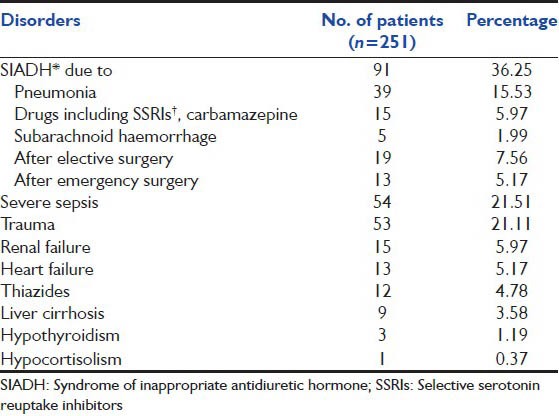
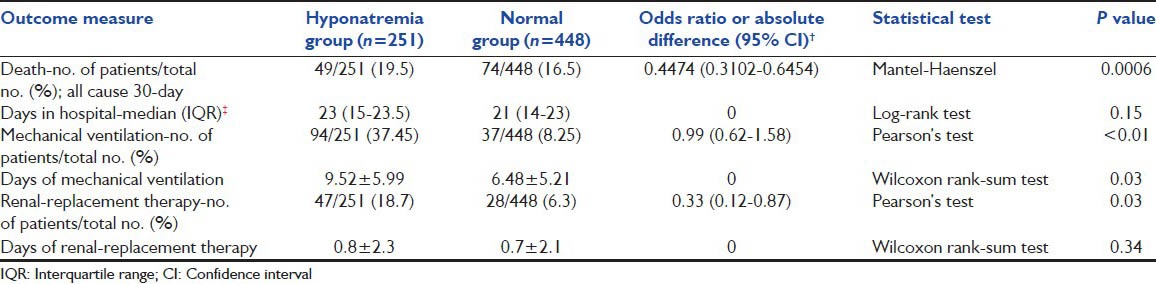
SIADH was the most common cause of hypontremia and pneumonia was the most common cause leading to SIADH. Severe sepsis (sepsis plus at least one acute organ dysfunction secondary to documented or suspected infection)[5] [Figure 1] and trauma were the next leading causes of hyponatremia [Table 3]. Describes the outcome of hyponatremia of all volume status in critically ill patients. Patients with hyponatremia spent a longer time in the ICU (P = 0.02), had longer mechanical ventilator days mean 9.52 ± 5.99 versus 6.48 ± 5.21 (P = 0.03) [Table 3] and had an increased mortality rate [Graph 1] (hazard ratio = 2.23; 95% CI of ratio = 1.323-3.773, P = 0.01), than patients in the normal serum sodium group.
Table 3.
Outcomes and adverse events*
Graph 1.
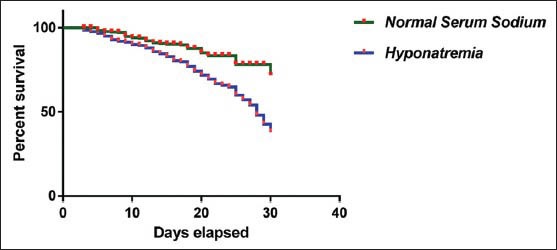
The time from inclusion to death in the two groups. Comparison of survival curves log-rank (Mantel-Cox) test; P < 0.0001
Discussion
In our study, the frequency of hyponatremia on ICU admission was 34.3% of all ICU admissions the incidence rate ratio, 1.61; 95% CI, 1.15-2.25, P 0< 0.01 and correlates well with recent studies which have reported hyponatremia to occur in about 30-40% of ICU patients as observed by DeVita et al.[1]
Females comprised of 56.5% of hyponatremic patients and 39.9% of normal serum sodium group. The risk of developing hyponatremia and its complications is higher in women and children compared with men, because of differences in respect of muscle mass and hormonal and anatomical factors.[6]
Like our study Bennani et al. in a study on hyponatremia in ICU found that euvolumic hyponatremia was the most common (50.6%) type of hyponatremia.[7]
In our study, SIADH is the most common cause of hyponatremia. In a study by Berghmans et al. also found that SIADH is the most frequent cause of hyponatremia.[8] Coussement et al. also found SIADH as a common and potentially lethal complication in critically ill patients.[9]
In our study severe sepsis is the second most common etiology for hyponatremia. Hannon and Boston observed that hyponatraemia associated with sepsis is known to have an increased morbidity and mortality. The cause of this phenomenon is unknown, but may be related to dilution of the extracellular space with retained exogenous fluid.[10]
Pneumonia is known to be associated with hyponatremia at the time of admission and it is associated with more severe illness, increased risk of mortality and prolonged hospital stays as reported by Nair et al.[11] In our study, pneumonia at the time of ICU admission, was the most common cause leading to SIADH [Table 2].
In the present study, patients who were taken up for elective surgery were more likely to have hyponatremia than emergency surgery patients. Like our study Leung et al. found that pereoperative hyponatremia association was particularly marked in patients undergoing nonemergency surgery adjusted odds ratio (aOR), 1.59; 95% CI, 1.50-1.69; P < 0.001 and patients with hyponatremia had a higher risk of 30-day mortality and this finding was consistent in all the subgroups. Furthermore, hyponatremia was associated with a greater risk of perioperative major coronary events (1.8% vs. 0.7%; aOR, 1.21; 95% CI, 1.14-1.29), wound infections and pneumonia and prolonged median lengths of stay by approximately 1 day.[12]
Bissram et al. found that symptomatic hyponatraemia was associated with volume depletion (32.6%), congestive heart failure (HF) (26%), SIADH (26%), thiazide diuretic use (26%) and selective serotonin re-uptake inhibitor use (26%). In 21.7% of cases, the cause was multifactorial (congestive HF, SIADH or medication use with volume depletion).[13]
In our study, hyponatremic patients had longer ICU stay, had longer ventilator days [Table 3] and had an increased mortality [Graph 1]. Shakhe et al. also found an increased mortality and ICU length of stay and increased ventilator days among hyponatremic patients admitted to ICU.[14]
In a large a retrospective study in 77 medical, surgical and mixed ICUs in Austria, with a database of 151,486 adults admitted consecutively over a period of 10 years Funk et al. demonstrated that all types and grades of dysnatremia were associated with increased mortality.[15]
However, taking into account all comorbidities and relative severity of illness mortality comparison would require a large scale regression analysis and subgroup analysis as per volume status for a definitive comment on prognosis.[16]
Conclusion
Hyponatremia is a frequent finding in the critically ill; most of these patients are euvolumic. SIADH is the most common cause of hyponatremia in critically ill. Pneumonia being the leading cause of SIADH. Severe sepsis, trauma, surgery (elective more than emergency), thiazides and other drugs (SSRIs and Carbamazapine), renal failure, HF, liver cirrhosis, subarachnoid haemorrhage, hypothyroidism and hypocortisolism are other etiologic factors for hyponatremia (P < 0.05). Hyponatremic patients had longer ICU stay and longer mechanical ventilation days and higher mortality. Patients with hyponatremia had a higher APACHE II score and higher mortality rate than those with normal serum sodium; however, because the former are more severely ill, no causality is apparent or suggested.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.DeVita MV, Gardenswartz MH, Konecky A, Zabetakis PM. Incidence and etiology of hyponatremia in an intensive care unit. Clin Nephrol. 1990;34:163–6. [PubMed] [Google Scholar]
- 2.Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581–9. doi: 10.1056/NEJM200005253422107. [DOI] [PubMed] [Google Scholar]
- 3.Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–800. doi: 10.1097/00003246-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Bartter FC, Schwartz WB. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med. 1967;42:790–806. doi: 10.1016/0002-9343(67)90096-4. [DOI] [PubMed] [Google Scholar]
- 5.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644–55. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 6.Moritz ML, Ayus JC. Dysnatremias in the critical care setting. Contrib Nephrol. 2004;144:132–57. doi: 10.1159/000078883. Ayus JC, Arieff AI. Brain damage and postoperative hyponatremia: The role of gender. Neurology 1996;46:323-8. [DOI] [PubMed] [Google Scholar]
- 7.Bennani SL, Abouqal R, Zeggwagh AA, Madani N, Abidi K, Zekraoui A, et al. Incidence, causes and prognostic factors of hyponatremia in intensive care. Rev Med Interne. 2003;24:224–9. doi: 10.1016/s0248-8663(02)00811-1. [DOI] [PubMed] [Google Scholar]
- 8.Berghmans T, Paesmans M, Body JJ. A prospective study on hyponatraemia in medical cancer patients: Epidemiology, aetiology and differential diagnosis. Support Care Cancer. 2000;8:192–7. doi: 10.1007/s005200050284. [DOI] [PubMed] [Google Scholar]
- 9.Coussement J, Danguy C, Zouaoui-Boudjeltia K, Defrance P, Bankir L, Biston P, et al. Treatment of the syndrome of inappropriate secretion of antidiuretic hormone with urea in critically ill patients. Am J Nephrol. 2012;35:265–70. doi: 10.1159/000336716. [DOI] [PubMed] [Google Scholar]
- 10.Hannon RJ, Boston VE. Hyponatraemia and intracellular water in sepsis: An experimental comparison of the effect of fluid replacement with either 0.9% saline or 5% dextrose. J Pediatr Surg. 1990;25:422–5. doi: 10.1016/0022-3468(90)90385-m. [DOI] [PubMed] [Google Scholar]
- 11.Nair V, Niederman MS, Masani N, Fishbane S. Hyponatremia in community-acquired pneumonia. Am J Nephrol. 2007;27:184–90. doi: 10.1159/000100866. [DOI] [PubMed] [Google Scholar]
- 12.Leung AA, McAlister FA, Rogers SO, Jr, Pazo V, Wright A, Bates DW. Preoperative hyponatremia and perioperative complications. Arch Intern Med. 2012;172:1474–81. doi: 10.1001/archinternmed.2012.3992. [DOI] [PubMed] [Google Scholar]
- 13.Bissram M, Scott FD, Liu L, Rosner MH. Risk factors for symptomatic hyponatraemia: The role of pre-existing asymptomatic hyponatraemia. Intern Med J. 2007;37:149–55. doi: 10.1111/j.1445-5994.2006.01294.x. [DOI] [PubMed] [Google Scholar]
- 14.Shakhe J, Gandhi N, Raghuraman G. Impact of hyponatraemia in critically ill patients. Endocr Abstr. 2013;10:31–55. [Google Scholar]
- 15.Funk GC, Lindner G, Druml W, Metnitz B, Schwarz C, Bauer P, et al. Incidence and prognosis of dysnatremias present on ICU admission. Intensive Care Med. 2010;36:304–11. doi: 10.1007/s00134-009-1692-0. [DOI] [PubMed] [Google Scholar]
- 16.Pai MP, Paloucek FP. The origin of the “ideal” body weight equations. Ann Pharmacother. 2000;34:1066–9. doi: 10.1345/aph.19381. [DOI] [PubMed] [Google Scholar]


