Abstract
Objective
To assess the changes in the Facial Attractiveness (FA) in two groups of cleft lip and palate patients with Class III malocclusions treated using LeFort I surgery or late maxillary protraction.
Materials and Methods
Standardized pre- and post-treatment photographs were taken of 32 patients (17 corrected by orthognathic surgery and 17 by late maxillary protraction). The photographs were randomized and 42 clinicians and 121 laypeople rated them on a 10-point FA scale via a web-based survey.
Results
Clinicians’ mean FA values increased from 4.45 to 5.16 [95% CI of Mean Difference (MD), 0.59–0.82, p<0.001] in surgical cases and 4.84 to 5.30 (95% CI of MD, 0.35–0.56, p<0.001) in protraction cases. The laypeople mean FA values increased from 5.07 to 5.54 (95% CI of MD, 0.40–0.53, p<0.001) in surgical cases and 5.51 to 5.68 (95% CI of MD, 0.11–0.23, p<0.001) in protraction cases. When patients combined, laypeople rated FA 0.64 points higher (95% CI, 0.54–0.74, p<0.001) in pre-treatment and 0.38 points higher (95% CI, 0.27–0.48, p<0.05) in post-treatment relative to clinicians.
Conclusion
Both clinicians and laypeople perceived an improvement of FA after both treatments. Laypeople rated FA higher compared to clinicians.
Keywords: Facial attractiveness, Cleft lip and palate, Class III malocclusion
Introduction
Patients with cleft lip and palate have a high incidence of Class III malocclusion. These patients undergo many surgeries throughout childhood. These surgical revisions may result in increased tissue scarring and impairment (1). The resulting scar tissue can restrict the downward and forward growth of the maxilla resulting in a retruded position maxilla and a Class III malocclusion (2). As a result, standardized concepts of beauty, such as symmetry and average facial proportions (1), may not readily apply to patients with cleft lip and palate. However, the desire to improve facial aesthetics is one of the main reasons people seek treatment by an orthodontist (3–6) or oral surgeon (7–10), including patients with cleft lip and palate. The goal of orthodontic treatment includes well-aligned dental arches in an ideal occlusal relationship, as well as a balanced and proportional face that is aesthetically attractive. Successful orthodontic treatment has been deemed important for a child’s social popularity and subsequent success in future careers (11).
It is important that differences in the perception of Facial Attractiveness (FA) between clinicians and laypeople to be more thoroughly understood as facial aesthetics is an important component of the treatment-planning process (12). The lateral cephalometric norm values correlate with facial aesthetics, but cannot be the sole factor for a complete evaluation of facial attractiveness. Consequently, it is essential that orthodontists and oral surgeons understand how laypeople perceive FA and the outcome of treatment to determine which treatment option may result in better perception of facial aesthetics.
Contradictory reports exist in the literature on whether there is agreement between clinicians and the laypeople in their perception of facial aesthetics. Some studies have reported general concordance between clinicians and the public (13–15): whereas, other studies have reported the two groups perceive facial aesthetics differently (16–19). The conventional treatment of patients with cleft lip and palate for the Class III dentoskeletal malocclusion include LeFort I maxillary advancement surgery or the non-surgical orthodontic approaches, i.e., late maxillary protraction. The late maxillary protraction therapy is based on the work of Eric Liou (20), using a combination of maxillary sutural loosening (i.e., with an expander by the alternate expansion and constriction of the maxilla) and protraction (with reverse headgear) to advance the maxilla (21,22). The objectives of the study were to (I) evaluate the FA perception of clinicians and laypeople in evaluating patients with cleft Lip and palate that were treated with orthognathic-surgery (LeFort I) or late maxillary protraction, (II) to compare the perceptions of FA between clinicians and laypeople, and (III) to assess the changes of FA in both groups.
Materials and Methods
After Institute Review Board (IRB) approval of the study, the sample population was randomly selected from the list of cleft lip and palate patients who received treatment at Children’s Hospital Los Angeles (CHLA). The sample consisted of 17 orthognathic-surgery corrected patients with cleft lip and palate, and 17 late maxillary protraction corrected patients with cleft lip and palate. The Inclusion criteria for the patients were, treated patients with unilateral and bilateral cleft lip and palate with a Class III malocclusion, which were treated at CHLA. The rater population consisted of 42 clinicians and 121 laypeople. The clinician-rater group included orthodontists, pediatric dentists, general dentists, oral maxillofacial surgeons, craniofacial geneticists, craniofacial plastic surgeons, and otolaryngologists. The lay-rater group included registered nurses, anesthesia nurses, technicians, front and back office staff, and administrative staff from all departments of CHLA. The rater group was accessed via the CHLA email list-serve.
Assessment of facial attractiveness
A set of three standardized pre-treatment color photographs and a set of three standardized post-treatment color photographs were presented of each patient: full frontal, full frontal smiling, and profile view (Fig. 1). In order to eliminate identifiable information from being linked to the patient photographs, the eyes were blocked out.
Figure 1.

Set of 3 standardized photos used in the survey.
Pre- and post-treatment photographs were presented in a randomized order to the raters via an online survey. For the present study, an internet-based method (www.surveymonkey.com) was used (23). Randomization of the pre- and post-treatment photographs was performed to prevent systematic bias. The raters were asked to rate the FA of the photographs on a discrete scale between 1 (very unattractive) and 10 (very attractive) (Fig. 2). The raters were asked to take no more than 10 seconds to rate each set of photographs. The FA values were divided into 3 categories:
Figure 2.
An example of photo shown on the online survey with a discrete scale. Participants were asked to spend no more than 10 seconds and rate the patient’s facial attractiveness. Very unattractive and very attractive correspond to 1 and 10, respectively.
1-Scored <4 were considered ‘aesthetically unattractive’.
2-Scored ≥4 and <7 were considered ‘aesthetically acceptable’.
3-Scored ≥7 were considered ‘aesthetically pleasant’.
Rater reliability
In order to assess the reliability of evaluators, a Kappa analysis was performed. Cronbach’s α is a coefficient of reliability and greater than 0.95 is considered to be highly reliable. The reliability of the 42 clinicians rating 34 pre-treatment photos was 0.962 (Cronbach’s-α) and 0.974 for post-treatment photos. The reliability of 121 laypeople’s FA rating 34 pre-treatment photos were 0.983 and 0.987 for post-treatment photos. These demonstrated the raters were highly reliable.
Statistical analysis
SPSS 12.0 for Windows was used for all statistical analyses. Statistical analyses were performed on the FA ratings of clinicians and laypeople. After analyzing the distribution of the data, the FA ratings were analyzed with a multiway Analysis of Variance Repeated Measures (ANOVA) to test for differences between: clinicians vs. laypeople, surgery vs. protraction, and pre-treatment vs. post-treatment. The mean [Standard Deviation (SD)] of the pre- and post-treatment FA ratings for surgery and protraction groups as well as the 95% Confidence Intervals (CI) of differences were calculated.
Paired t-tests were performed to determine the direction of change, as a result of treatment in all patients combined, the difference between pre-treatment and post-treatment ratings (in clinicians and laypeople), and to compare the attractiveness of the initial as well as the final photographs of the cleft lip and palate patients. Then, independent t-tests were performed to evaluate clinicians vs. laypeople ratings of pre- and post-treatment photographs. The significance level was set at 0.05.
Results
According to the ANOVA tests, there were statistically significant differences in facial attractiveness ratings between the clinicians and laypeople (F=25347.874, p<0.001), between surgery and protraction (F=89.925, p<0.001), and between pre-treatment and post-treatment (F=229.352, p<0.001).
The mean (SD) pre- and post-treatment FA ratings for clinicians were 4.64 (1.54) and 5.23 (1.74), respectively. The corresponding values for laypeople were 5.29 (1.73) and 5.61 (1.83), respectively. The paired t-test indicated there were statistically significant differences in FA perception between pre-treatment photo ratings and post-treatment photo ratings (all patients combined) by clinicians (p<0.001) and laypeople (p<0.001). Clinicians rated post-treatment photographs 0.58 points higher (95% CI, 0.50–0.66) than pre-treatment photographs; laypeople rated post-treatment photographs 0.32 points higher (95% CI, 0.27–0.36) than pre-treatment photographs.
The paired t-tests also showed there were statistically significant differences in FA between pre-treatment and post-treatment photograph ratings for the surgical (p<0.001) and protraction (p<0.001) groups, according to clinicians and laypeople. Evaluation by clinicians showed the mean attractiveness value increased from 4.45 to 5.16 (mean difference= 0.71, 95% CI, 0.59–0.82) in surgical cases and 4.84 to 5.30 (mean difference=0.46, 95% CI, 0.35–0.56) in protraction cases. The mean attractiveness value increased from 5.07 to 5.54 (mean difference=0.47, 95% CI, 0.40–0.53) in surgical cases and 5.51 to 5.68 (mean difference=0.17, 95% CI, 0.11–0.23) in protraction cases for laypeople.
The Independent t-tests revealed that for the pre-treatment photographs, both rater groups (clinicians and laypeople) observed significant differences (p<0.001) in FA ratings between surgery and protraction (Table 1).
Table 1.
Facial attractiveness ratings in two treatment groups (surgery and protraction)
| Evaluator | Number of evaluations | Mean (SD) | |
|---|---|---|---|
| Clinicians Pre-Tx | Protraction | 714 | 4.84 (1.48) |
| Surgery | 714 | 4.45 (1.58) | |
| Clinicians Post-Tx | Protraction | 714 | 5.30 (1.70) |
| Surgery | 714 | 5.16 (1.77) | |
| Laypeople Pre-Tx | Protraction | 2057 | 5.51 (1.71) |
| Surgery | 2057 | 5.07 (1.73) | |
| Laypeople Post-Tx | Protraction | 2057 | 5.68 (1.79) |
| Surgery | 2057 | 5.54 (1.87) |
The independent t-test also showed there were significant differences between clinicians’ and laypeople’s ratings of patients (surgery and protraction combined), both pre-treatment (equal variances not assumed, p<0.001) and post-treatment (equal variances not assumed, p<0.001). Overall, laypeople rated 0.64 points higher (95% CI, 0.54–0.74) in the pre-treatment cases and 0.38 points higher (95% CI, 0.27–0.48) in the post-treatment cases in comparison to clinicians (Table 2).
Table 2.
Facial attractiveness ratings in clinician and laypeople
| Evaluator | Number of evaluations | Mean (SD) | |
|---|---|---|---|
| Pre-Tx | Clinicians | 1428 | 4.65 (1.54) |
| Laypeople | 4114 | 5.29 (1.74) | |
| Post-Tx | Clinicians | 1428 | 5.23 (1.74) |
| Laypeople | 4114 | 5.61 (1.83) |
Discussion
The cleft deformity often affects the facial appearance with scar tissue formation (24) and creating facial asymmetry, particularly in the nasolabial region (25). The resultant facial deformity can reinforce or induce a social stereotype in first impressions (26) and the individual’s behavior can be different when encounters those with unsightly appearances (26,27). These negative effects of facial deformity tend to increase as the patient ages (28,29). Further, alongside the functional improvement following treatment, the self-perceived improvement in facial appearance also plays a strong positive role in the quality of life and patient satisfaction (30,31). Therefore, assessment of facial aesthetics is important and various methods such as comparisons of photographs or digitally enhanced images, as well as graduated scales have been used to evaluate the facial aesthetics (27). However, there is no gold standard or standardized method, as each method has its own pros and cons (27). The Internet-based survey that was used had several advantages (23). This method increased the data collection (rater count) and rate of data accrual and analysis; the results were reproducible and logistical and monetary obstacles were eliminated. This method also enables the experimenter to sweep broad demographics.
Due to the lack of objective system to assess the facial aesthetics (32) and the subjective nature of the present study, it is difficult to eliminate biases and this could be a possible limitation of the study. Evaluators can be influenced by factors other than those, which primarily concern clinicians (i.e., hair and skin color and skin texture can influence the assessment of facial attractiveness). In this study, the standard photos taken in the CHLA were used to reduce some of these biases.
This was unfortunate, to learn that from pre- to post-treatment the mean attractiveness value for patients stayed in their same group, i.e. acceptable aesthetics. In fact, the mean scores did not move much closer towards the group of pleasant aesthetics (7 to 10). This is rather interesting in that despite the rather intense and aggressive treatment, for some reason, these patients were not altered a great deal in terms of the facial attractiveness. The present findings highlight the importance of assessing the different part of the face in terms of facial attractiveness, ie., the forehead, nose, lips, chin, and submental-cervical region (33). Ideally, assessment of FA should evaluate and score all 5 mentioned regions; however, the available FA assessment tolls either assess the face as a whole, as this study, or assesses one or a few regions, but not all of them. Previous studies on facial attractiveness are either report on self-rating of patient/parents (32,34–36) or professional assessment (32,37,38) of patients with cleft lip and palate. These studies mainly use Likert/discrete scales (36), as this study, or visual analogue scales (32,35). Orthognathic surgery and orthodontics may have improved the skeletal relationship in patients with cleft lip and palate, but they did not improve the overall facial attractiveness much. This is probably because of the status of their lips and nose that has not been affected much by orthodontics or orthognathic surgery. In particular, the preferred choice of lip fullness can vary depending on the jaw relationships (33,39). It has been noted that clinicians and laypeople preferred fuller lip positions for the more extreme retrognathic and prognathic profiles; however, they preferred more retrusive lip positions for the more average profiles (33,39). The nose has been recognized as the least aesthetic element of facial morphology (25,26, 40,41). Future studies can measure facial attractiveness based on facial proportions, scarring, skin quality, ethnicity, employ indices such as the one developed by Asher-McDade et al. (42), which is more limited to the assessment of nasolabial region, or gather information on the attractiveness of different components of the face such as forehead, nose, lips, chin, submental-cervical region, jaw relthionships, or smile dynamics (32).
One of the objectives of treatment of patients with cleft lip and palate is to improve the aesthetic appearance of the face as well as the patient’s social acceptability (25). Overall, the findings of this study showed the FA improved by both treatment modalities, as reflected in the post-treatment scores of higher than 4 in both groups. Clinicians and laypeople observed a general improvement in FA from pre- to post-treatment of all patients, regardless of surgery or protraction (Fig. 3). Furthermore, the change was greater for surgery. There are confounding factors that need to be considered, such as the initial severity of the Class III malocclusion in the patients with cleft lip and palate, and the patients’ age. Evaluation of FA in LeFort I surgery patients resulted in a greater difference between pre- and post-FA values (Fig. 4) in comparison to protraction patients. The starting values may account for the overall difference between pre- and post-treatment values. According to the raters, the starting point was lower for surgery patients, which meant the protraction patients started with faces that were more attractive. As a pre-treatment comparison of the groups was not performed in this study, an assumption that could be made from the data was that perhaps the surgery cases were more difficult cases, and the protraction cases were probably less severe cases. This may be pointing to the presence of selection bias. Future studies can compare and match the pre-treatment photographs, objectively using indices or soft-tissue analysis, to assess whether both treatments produce similar FA outcomes. However, matching the groups is difficult as there is no standardized objective system to assess all aspects of the facial aesthetics (32). Overall, the results did not state that one treatment type was preferred better to the other.
Figure 3.
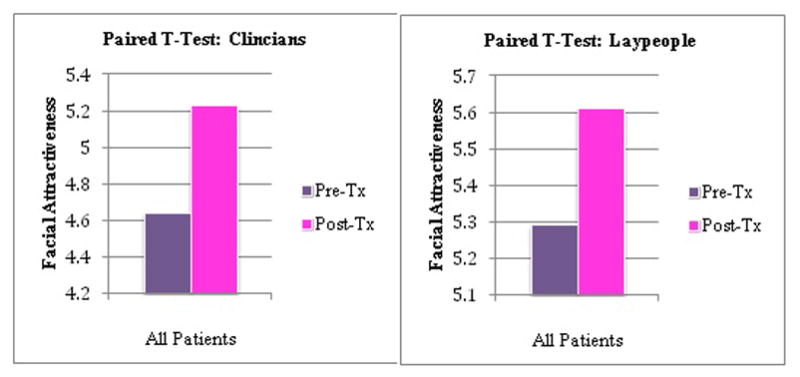
The pre- and post-treatment facial attractiveness ratings of all patients combined according to laypeople and clinicians.
Figure 4.
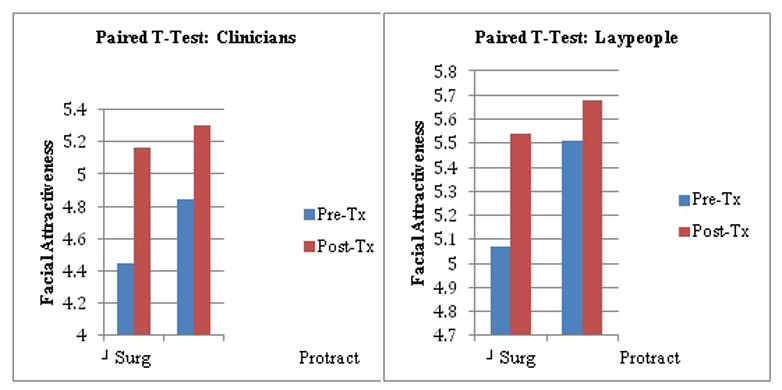
Pre- and post-treatment facial attractiveness ratings of surgery and protraction groups by laypeople and clinicians.
The results of the direct comparison of clinicians’ ratings to laypeople’s ratings indicate that laypeople generally rate FA higher than clinicians do. This is similar to the findings of studies that showed a difference between the perceived facial aesthetics of clinicians and laypeople (16–19). Clinicians are more critical in rating aesthetics and may be looking for different facial attributes, compared to laypeople (43), which are usually influenced by clinicians’ training and experience (32). Review of the literature points out that the perception of nasolabial appearance differs among professionals, lay people, and patients (19, 32). Another possible limitation of the study is that the laypeople’s sample may have some previous knowledge of the problem, and future studies can employ subjects from a wider community without this previous knowledge to comprise a more valid laypeople opinion (32). The findings of this study are important as the decision to perform cosmetic surgery to correct or enhance the patient’s face should not be based only on surgeons or professionals’ preference, but also on the patients’ and the parents’ perception of facial aesthetics.
Conclusion
Both clinicians and laypeople perceived an improvement of FA from pre-treatment to post-treatment photographs for both treatments. Laypeople in this study rated FA higher in patients with cleft lip and palate compared to clinicians.
Footnotes
Authors have no conflict of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Trotman CA, Faraway JJ, Phillips C, van Aalst J. Effects of lip revision surgery in cleft lip/palate patients. J Dent Res. 2010;89:728–32. doi: 10.1177/0022034510365485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Semb G. A study of facial growth in patients with unilateral cleft lip and palate treated by the Oslo CLP Team. Cleft Palate Craniofac J. 1991;28:1–21. doi: 10.1597/1545-1569_1991_028_0001_asofgi_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 3.Cox NH, van der Linden FP. Facial harmony. Am J Orthod. 1971;60:175–83. doi: 10.1016/0002-9416(71)90033-9. [DOI] [PubMed] [Google Scholar]
- 4.Foster EJ. Profile preferences among diversified groups. Angle Orthod. 1973;43:34–40. doi: 10.1043/0003-3219(1973)043<0034:PPADG>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Romani KL, Agahi F, Nanda R, Zernik JH. Evaluation of horizontal and vertical differences in facial profiles by orthodontists and lay people. Angle Orthod. 1993;63:175–82. doi: 10.1043/0003-3219(1993)063<0175:EOHAVD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin DC. Appearance and aesthetics in oral health. Community Dent Oral Epidemiol. 1980;8:244–56. doi: 10.1111/j.1600-0528.1980.tb01296.x. [DOI] [PubMed] [Google Scholar]
- 7.Laufer D, Glick D, Gutman D, Sharon A. Patient motivation and response to surgical correction of prognathism. Oral Surg Oral Med Oral Pathol. 1976;41:309–13. doi: 10.1016/0030-4220(76)90143-2. [DOI] [PubMed] [Google Scholar]
- 8.Jacobson A. Psychological aspects of dentofacial esthetics and orthognathic surgery. Angle Orthod. 1984;54:18–35. doi: 10.1043/0003-3219(1984)054<0018:PAODEA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Flanary CM, Barnwell GM, Jr, Alexander JM. Patient perceptions of orthognathic surgery. Am J Orthod. 1985;88:137–45. doi: 10.1016/0002-9416(85)90238-6. [DOI] [PubMed] [Google Scholar]
- 10.Mayo KH, Dryland-Vig KWL, Vig PS, Kowalski CJ. Attitude variables of dentofacial deformity patients: demographic characteristics and associations. J Oral Maxillofac Surg. 1991;49:594–602. doi: 10.1016/0278-2391(91)90341-i. [DOI] [PubMed] [Google Scholar]
- 11.Howells DJ, Shaw WC. The Validity and reliability of ratings of dental and facial attractiveness for epidemiologic use. Am J Orthod. 1985;88:402–8. doi: 10.1016/0002-9416(85)90067-3. [DOI] [PubMed] [Google Scholar]
- 12.Maple JR, Vig KW, Beck FM, Larsen PE, Shanker S. A comparison of providers’ and consumers’ perceptions of facial-profile attractiveness. Am J Orthod Dentofacial Orthop. 2005;128:690–6. doi: 10.1016/j.ajodo.2004.09.030. [DOI] [PubMed] [Google Scholar]
- 13.Eisenthal Y, Dror G, Ruppin E. Learning facial attractiveness. Neural Comput. 2006;18:119–42. doi: 10.1162/089976606774841602. [DOI] [PubMed] [Google Scholar]
- 14.Dunlevy HA, White RP, Proffit WR, Turvey TA. Professional and lay judgment of facial esthetic changes following orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1987;1:151–8. [PubMed] [Google Scholar]
- 15.Kerr WJS, O’Donnell JM. Panel perception of facial attractiveness. Br J Orthod. 1990;17:299–304. doi: 10.1179/bjo.17.4.299. [DOI] [PubMed] [Google Scholar]
- 16.Prahl-Andersen B, Boersma H, van der Linden FPGM, Moore AW. Perceptions of dentofacial morphology by lay persons, general dentists, and orthodontists. J Am Dent Assoc. 1979;98:209–12. doi: 10.14219/jada.archive.1979.0456. [DOI] [PubMed] [Google Scholar]
- 17.Cochrane SM, Cunningham SJ, Hunt NP. A comparison of the perception of facial profiles by the general public and 3 groups of clinicians. Int J Adult Orthod Orthognath Surg. 1999;14:291–5. [PubMed] [Google Scholar]
- 18.Liu Y, Korn EL, Oh HS, Pearson H, Xu TM, Baumrind S. Comparison of Chinese and US orthodontists’ evaluations of “facial attractiveness” from end-of-treatment facial photographs. Am J Orthod Dentofacial Orthop. 2009;135:621–34. doi: 10.1016/j.ajodo.2007.04.039. [DOI] [PubMed] [Google Scholar]
- 19.Mani MR, Semb G, Andlin-Sobocki A. Nasolabial appearance in adults with repaired unilateral cleft lip and palate: Relation between professional and lay rating and patients’ satisfaction. J Plast Surg Hand Surg. 2010;44:191–8. doi: 10.3109/02844311.2010.499671. [DOI] [PubMed] [Google Scholar]
- 20.Liou EJ, Tsai WC. A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J. 2005;42:121–7. doi: 10.1597/03-107.1. [DOI] [PubMed] [Google Scholar]
- 21.Yen SL. Protocols for late maxillary protraction in cleft lip and palate patients at Childrens Hospital Los Angeles. Semin Orthod. 2011;17:138–48. doi: 10.1053/j.sodo.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borzabadi-Farahani A, Lane CJ, Yen SL. Late maxillary protraction in patients with unilateral cleft lip and palate, a preliminary study. Cleft Palate-Craniofac J. 2012 doi: 10.1597/12-099. [DOI] [PubMed] [Google Scholar]
- 23.Devcic Z, Karmini K, Popenko N, Wong BJF. A web-based method for rating facial attractiveness. Laryngoscope. 2010;120:902–6. doi: 10.1002/lary.20857. [DOI] [PubMed] [Google Scholar]
- 24.Ritter K, Trotman CA, Phillips C. Validity of subjective evaluations for the assessment of lip scarring and impairment. Cleft Palate Craniofac J. 2002;39:587–96. doi: 10.1597/1545-1569_2002_039_0587_voseft_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 25.Fudalej P, Katsaros C, Bongaarts C, Dudkiewicz Z, Kuijpers-Jagtman AM. Nasolabial aesthetics in children with complete unilateral cleft lip and palate after 1-versus 3-stage treatment protocols. J Oral Maxillofac Surg. 2009;67:1661–6. doi: 10.1016/j.joms.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Nollet PJ, Kuijpers-Jagtman AM, Chatzigianni A, Semb G, Shaw WC, Bronkhorst EM, Katsaros C. Nasolabial appearance in unilateral cleft lip, alveolus and palate: a comparison with Eurocleft. J Craniomaxillofac Surg. 2007;35:278–286. doi: 10.1016/j.jcms.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Paiva TS, Andre M. Evaluating aesthetics of the nasolabial region in children with cleft lip and palate: professional analysis and patient satisfaction. Patient Prefer Adherence. 2012;6:781–7. doi: 10.2147/PPA.S36656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Richman LC. Facial and speech relationships to behavior of children with clefts across three age levels. Cleft Palate Craniofac J. 1997;34:390–5. doi: 10.1597/1545-1569_1997_034_0390_fasrtb_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 29.Richman LC, Millard T. Brief report: cleft lip and palate: longitudinal behavior and relationships of cleft conditions to behavior and achievement. J Pediatr Psychol. 1997;22:487–94. doi: 10.1093/jpepsy/22.4.487. [DOI] [PubMed] [Google Scholar]
- 30.Khattak ZG, Benington PC, Khambay BS, Green L, Walker F, Ayoub AF. An assessment of the quality of care provided to orthognathic surgery patients through a multidisciplinary clinic. J Craniomaxillofac Surg. 2012;40:243–7. doi: 10.1016/j.jcms.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Rustemeyer J, Gregersen Quality of Life in orthognathic surgery patients: postsurgical improvements in aesthetics and self-confidence. J Craniomaxillofac Surg. 2012;40:400–4. doi: 10.1016/j.jcms.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 32.Gkantidis N, Papamanou DA, Christou P, Topouzelis N. Aesthetic outcome of cleft lip and palate treatment. Perceptions of patients, families, and health professionals compared to the general public. J Craniomaxillofac Surg. 2012 doi: 10.1016/j.jcms.2012.11.034. [DOI] [PubMed] [Google Scholar]
- 33.Modarai F, Donaldson JC, Naini FB. The influence of lower lip position on the perceived attractiveness of chin prominence. Angle Orthod. 2013 doi: 10.2319/122912-974.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Broder HL, Smith FB, Strauss RP. Effects of visible and invisible orofacial defects on self-perception and adjustment across developmental eras and gender. Cleft Palate Craniofac J. 1994;31:429–436. doi: 10.1597/1545-1569_1994_031_0429_eovaio_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 35.Hunt O, Burden D, Hepper P, Stevenson M, Johnston C. Self-reports of psychosocial functioning among children and young adults with cleft lip and palate. Cleft Palate Craniofac J. 2006;43:598–605. doi: 10.1597/05-080. [DOI] [PubMed] [Google Scholar]
- 36.Noor SN, Musa S. Assessment of patients’ level of satisfaction with cleft treatment using the Cleft Evaluation Profile. Cleft Palate Craniofac J. 2007;44:292–303. doi: 10.1597/05-151. [DOI] [PubMed] [Google Scholar]
- 37.Sinko K, Jagsch R, Prechtl V, Watzinger F, Hollmann K, Baumann A. Evaluation of aesthetic, functional, and quality-of-life outcome in adult cleft lip and palate patients. Cleft Palate Craniofac J. 2005;42:355–361. doi: 10.1597/03-142.1. [DOI] [PubMed] [Google Scholar]
- 38.Russell KA, Tompson B. Correlation between facial morphology and aesthetics in patients with repaired complete unilateral cleft lip and palate. Cleft Palate Craniofac J. 2009;46:319–325. doi: 10.1597/07-143.1. [DOI] [PubMed] [Google Scholar]
- 39.Czarnecki ST, Nanda RS, Currier GF. Perceptions of a balanced facial profile. Am J Orthod Dentofacial Orthop. 1993;104:180–187. doi: 10.1016/S0889-5406(05)81008-X. [DOI] [PubMed] [Google Scholar]
- 40.Brattström V, Mølsted K, Prahl-Andersen B, Semb G, Shaw WC. The Eurocleft Study: interceanter study of treatment outcome in patients with complete cleft lip and palate. Part 2: craniofacial form and nasolabial appearance. Cleft Palate Craniofac J. 2005;42:69–77. doi: 10.1597/02-119.2.1. [DOI] [PubMed] [Google Scholar]
- 41.Offert B, Janiszewska-Olszowska J, Dudkiewicz Z, Brudnicki A, Katsaros C, Fudalej PS. Facial esthetics in children with unilateral cleft lip and palate 3 years after alveolar bonegrafting combined with rhinoplasty between 2 and 4 years of age. Orthod Craniofac Res. 2013;16:36–43. doi: 10.1111/ocr.12002. [DOI] [PubMed] [Google Scholar]
- 42.Asher-McDade C, Brattström V, Dahl E, McWilliam J, Mølsted K, Plint DA, Prahl-Andersen B, Semb G, Shaw WC, The RP. A six-center international study of treatment outcome in patients with clefts of the lip and palate: Part 4. Assessment of nasolabial appearance. Cleft Palate Craniofac J. 1992;29:409–12. doi: 10.1597/1545-1569_1992_029_0409_asciso_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 43.Papamanou DA, Gkantidis N, Topouzelis N, Christou P. Appreciation of cleft lip and palate treatment outcome by professionals and laypeople. Eur J Orthod. 2012;34:553–60. doi: 10.1093/ejo/cjr073. [DOI] [PubMed] [Google Scholar]


