Abstract
This paper addresses behavioral and social research priorities for prevention and treatment of HIV-1 infection. The approach used to define these priorities is based on three premises: (1) Behavioral interventions for prevention and treatment are necessary but not sufficient for producing reductions in transmission or advances in treatment; the same is true of biomedical interventions; by themselves they cannot maximally impact the health of communities. (2) Combination prevention and treatment strategies should include optimal combinations of behavioral and biomedical strategies, but also must include the varieties of the behaviors of individuals, communities, and systems needed to ensure effective treatment and prevention; and (3) It is no longer useful, given scientific advances in understanding how treatment contributes to prevention, to discuss prevention without incorporating treatment and vice versa. This re-definition of behavioral approaches in combination prevention and treatment provides a new paradigm for defining behavioral research in HIV-1 disease. No longer is it sufficient to focus on single behavior (e.g., high-risk sexual behavior, adherence to anti-retroviral medications) of individuals in a vertical way. Rather, the behavioral agenda needs to expand to encompass traditional investigations of single behaviors, but also needs to include the behavior of many actors and systems which are essential in facilitating reductions in transmission and improvements in treatment outcomes. In addition, there is the need for expanded implementation research agenda to encompass the study of methods to achieve high coverage, acceptability and effectiveness of available menu of interventions.
Keywords: HIV prevention, behavior, combination prevention strategies
Clinical trials demonstrating the efficacy of the use of anti-retroviral medications for prevention (e.g., chemoprophylaxis, prevention of mother-to-child transmission), improved treatment for HIV-1 infected individuals, and reducing transmission to others rightfully attract the admiration of those in treatment and prevention science and bring hope to those working in the field and to patients with the disease. But while those advances make important contributions to the scientific literature and attract excitement from the public at large, implementing them in ways that affect widespread benefit are considerably more complicated (1).
Some have expressed concern that these important advances in treatment and prevention of HIV-1, especially those based in the use of anti-retroviral therapy, have greatly reduced or even completely eliminated the need for behavioral or social strategies in HIV-1 prevention (2). After years of HIV-1 prevention clinical trials—using a variety of strategies including treatment of sexually transmitted infections including HSV-2 and behavioral counseling—success in preventing transmission of HIV-1 was achieved through male circumcision (3,4,5) and the use of anti-retroviral therapies for chemoprophylaxis (6) as well as to prevent transmission from individuals infected with HIV-1 to uninfected individuals in discordant couples (7,8), including prevention of transmission from mothers infected with HIV-1 to their infants during pregnancy and breastfeeding periods (9). Prior research has demonstrated the prevention potential of treating individuals for substance abuse, and providing clean needles and syringes to those continuing to use them (11,12).
We and others have advanced the position that behavioral and social strategies are necessary, but not sufficient, for preventing and treating HIV-1 disease (13). All of the evidence points to the importance of behavioral and social strategies to reduce HIV-1 transmission and to treat those with the disease. Examples abound with adherence to HIV-1 medications being one of the greatest barriers to efficacy when anti-retroviral medications are used for chemoprophylaxis (whether in pill or gel form—6) and prevention of mother-to-child transmission programs dependent upon individual and systems variables (9). The same is true for those infected with HIV-1; the “cascade of treatment” typically shows that 20-30% of these infected individuals in most jurisdictions in the United States know that they are infected with HIV-1 and are in treatment effective enough to reduce viral load to undetectable (13)
Our first premise is that biomedical, like behavioral interventions, are necessary but not sufficient for prevention and treatment of HIV-1. Biomedical interventions are similar to behavioral strategies: the biomedical strategies cannot work nor will they have widespread effectiveness if the conditions for their use are not optimized and if individuals fail to use them in ways that are necessary to ensure that they work and achieve their intended effect.
A New Framework for Combination Prevention and Treatment
Our analysis of combination prevention and treatment is based on a second premise, specifically expanding the understanding of “combination prevention and treatment” and of “behavior.” “Combination prevention and treatment” most frequently is used to define the optimal ways of combining biomedical and behavioral (and sometimes social and structural) and biomedical interventions to prevent or treat disease (12). We incorporate these elements into our definition of combination prevention and treatment, but also expand the concept to address the varieties of behaviors—on the part of individuals as well as larger systems—needed to ensure effective treatment and prevention. “Behavior” refers to the actions of the individual, as well as to the behavior of systems (e.g., family or health care systems), of those working in those systems, and of entire communities (1). Often when “behavior” is discussed, the emphasis is placed on strategies directed to the individual that aim, for example, to help that person get tested, adhere to treatment or prevention regimens, and/or reduce risk behavior. Undoubtedly, such strategies can play a role in the overall promotion of prevention and treatment. But strategies focused only on the individual are time- and labor-intensive, while having an effect on reported risk behaviors, have had limited efficacy on HIV acquisition and may have limited reach and therefore limited efficacy in the community-at-large (14).
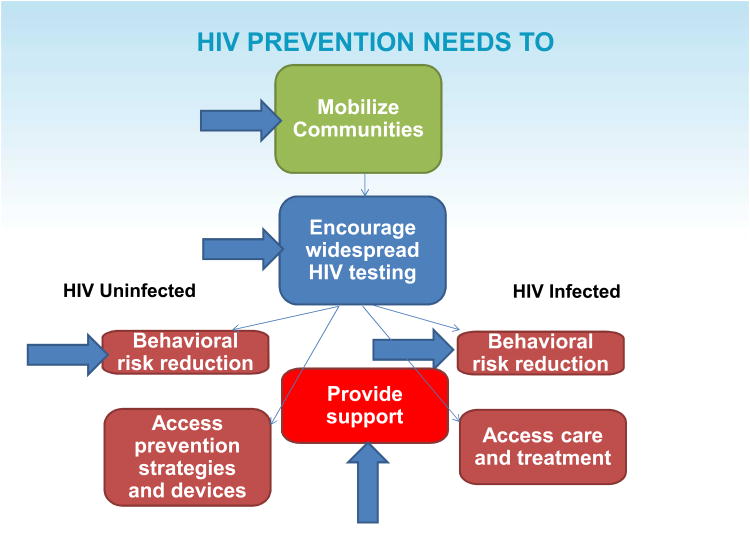
The model of HIV-1 prevention and treatment presented in Figure 1 demonstrates this broadened use of “behavior.” Community awareness and mobilization are essential for ensuring that the services are designed to appeal to the needs of the population and that the individuals for whom the services are designed know about them and are motivated to use them. Following mobilization, HIV diagnosis is essential so that infected and uninfected individuals can receive appropriate services. The next phase involves appropriate triage so that those who do not have HIV-1 infection can be counseled in how to avoid it, and so that they can access specialized services (e.g., male circumcision, drug or mental health treatment, chemoprophylaxis, if available). Those who are infected also need to be counseled in how to avoid spreading HIV-1 to others, how to access specialized treatments if necessary (e.g, drug or mental health treatment), and the importance of and linkage to care for their HIV disease not only for their own health benefits but also for the public health (7,8). Adherence is essential for both uninfected and infected individuals, and community support may be essential for adherence at levels needed to ensure that the prevention and treatment strategies can work (1,6).
Figure 1.
What is needed to successfully confront the HIV epidemic?
An effective HIV-1 prevention and treatment service system in the low, middle, and high income countries needs to incorporate all of the elements necessary for successful deployment of prevention activities and efficacious management of HIV-1 disease. A comprehensive system must include useful prevention activities, early identification of HIV-1 infected individuals in need of care, linkage to care, appropriate initial and continued counseling and other forms of support for continued risk reduction and management of HIV-1 disease, assessment if HIV-1 disease stage, treatment with anti-retroviral medications for those who qualify, monitoring while on treatment to ensure efficacy, adherence support, and provision of sexual and reproductive health services (1). All of this would ideally be structured in ways that make access easily available and affordable and that do not require extensive travel, lengthy wait times, loss of income to the individuals being served, and that is done in ways that respect and recognize the dignity of the patients.
Table 1 lists the full range of activities needed to implement this complex agenda. Easy to access services has become the priority for many HIV-1 prevention and treatment systems as the goal is not only to increase the number of persons on treatment, but also to maintain them in prevention and treatment services.
Table 1. Essential Elements of Community-wide Implementation of HIV-1 Prevention and Treatment Programs.
| Easily Accessible Services |
|
| Effective Management |
|
| Community-wide Support Systems |
|
| Adequate Prevention Programs |
|
| Early Identification of HIV-1 Infected Individuals |
|
| Appropriate Initial and Continued Counseling |
|
| Linkage to and Maintenance in Care |
| Maintaining Treatment and Prevention Standard of Care |
|
| Sexual and Reproductive Health Services |
Effective management of prevention and treatment services involves skills and behaviors that have been little studied or addressed in the HIV-1 prevention or treatment literature. The focus of behavioral research has been on the outcome: do individuals engage in behaviors to reduce the chances of acquiring or spreading HIV or optimizing treatment. This narrow perspective has led to studies—most often using strategies targeted at the individual—to reduce certain behaviors (e.g., high-risk sexual behavior) or increase others (e.g., adherence to medications). The expanded paradigm presented here retains that focus, as ultimately it is the behavior of individuals that has a large influence on disease outcomes. But the expanded paradigm also widens that focus to recognize that those specific outcomes are influenced strongly by the behavior of systems (e.g,. systems of prevention and care that facilitate easy access for consumers), other individuals (e.g., health care providers), services offered (e.g., all of the tools in the “prevention tool box,” strategies for diagnosing HIV-1 infection and linking individuals to care, strategies for maintaining standards of prevention and care) (1).
There is increasing recognition that the behavior of managers and management systems are essential for effective application of behavioral and biomedical prevention and treatment strategies (15). If those in charge do not appreciate the importance of how to manage personnel in a transparent and fair manner, then those personnel will be disenchanted and unmotivated and that attitude will undoubtedly affect their interactions with patients. If resources are not well utilized and essential supplies not well managed, then interruptions in service are inevitable, thereby affecting the health of clientele but also causing people to lose faith in the health system. Patients will receive less than adequate service if front-line health care providers are not skilled—both medically and interpersonally.
There has been recognition of the increasing importance of community-wide support systems to motivate testing, address educational barriers, and support behavioral risk reduction and adherence needs of community members (16). A variety of evidence-based strategies have been identified to maximize testing coverage as well as diagnosis and linkage to care of persons infected with HIV-1 and considerable emphasis has been placed on effective initial and ongoing counseling.
Linkage to and maintenance in care remain a work in progress, most often using community health workers to walk individuals through systems and follow up with them when the fail to return. No doubt, other health system “behaviors” such as easy access and culturally appropriate care are essential as well. Monitoring and maintaining quality of services, especially in low and middle income countries remains a challenge, especially with turnover of staff and difficult working conditions. Maintaining high quality of services remains a challenge, especially as the goal is to expand availability of new biomedical technologies and to continue efforts at task shifting and task sharing, so that diverse types of providers can prescribe and monitor the use of anti-retroviral therapies and other efficacious interventions.
Research Priorities
The approach to “behavior” presented in Figure 1 and developed in Table 1 changes the research agenda from a focus on specific behaviors (e.g., reductions in sexual risk behaviors; adherence to antiretroviral medications) to a focus on the broader “Essential Elements of Community-Wide Implementation of HIV-1 Prevention and Treatment Programs.” Examples of a broadened research agenda that is inclusive of implementation research questions are presented in Table 2. This expanded paradigm, and the research examples derived from it and presented in Table 2, hopefully will provide a stimulus to broaden thinking about the kinds of questions asked in research, and the kinds of programmatic interventions developed, to maximize at the individual and societal level the benefits that advances in prevention and treatment science have delivered to us thus far. A planned study, HPTN 071 (PopART) aims to take a borad approach to the challenge of preventing HIV transmission at community level. In the latter study, interventions to be studied include community mobilization, house-to-house HIV testing, use of community health workers to promote linkage and adherence, combined with use of treatment as prevention and referral for male circumcision, promotion of prevention of mother to child transmission and widescale provision of condoms.
Table 2. Behavioral Research Priorities to Address Essential Elements of Community-wide Implementation of HIV-1 Prevention and Treatment Programs.
| Access to Services |
|---|
| Example research priority: Constrained resources may not make it possible to address all issues that provide easy access to services. Which variables (e.g., proximity, waiting times, cost) are most influential in promoting access to and satisfaction with prevention and treatment services? |
| Effective Management |
| Example research priority: Which management skills are essential for ensuring effective prevention and treatment services? How are these best taught and maintained? How can quality of management be monitored and maintained? |
| Community-wide Support Systems |
| Example research priority: What configurations of community support systems maximize testing, reduce risk behaviors, and maintain adherence? |
| Adequate Prevention Programs |
| Example research priority: What strategies can be used to motivate policy makers and program planners to make full use of the prevention tool box? |
| Early Identification of HIV-1 Infected Individuals |
| Example research priority: What testing strategies are the most cost-effective for identifying HIV-1 infected individuals and ensuring their entry into and maintenance in care? What enhances linkage to care? |
| Appropriate and Continued Counseling |
| Example research priority: What counseling strategies most cost-effectively reduce risk and maintain adherence? |
| Maintaining Prevention and Treatment Standard of Care |
| Example research priority: How can health care providers, especially with task shifting, establish and maintain prevention and treatment standard of care. |
Conclusions
There is no question that biomedical advances in HIV prevention and care are transformative and life-saving. We now have tools that we did not have only a few years ago. But these technologies can have little effect if they are not used the way that they need to be in order to make a real difference in confronting the epidemic. In this way, efficacy and effectiveness all come back to behavior—of individuals and of systems. Simply put, these advances will have little benefit without individual behavior and an understanding and reformation of systems responsible for attracting people to services and keeping them there for the longterm.
These optimal packages will cost money, and those funds are difficult to find in these tight economic times. But there is also no doubt that the strategies proven so efficacious in clinical trials will fail to have impact on epidemics in communities, regions, or countries unless the complexity of their implementation is addressed. Vermund and Hayes (17) put it eloquently: “Yet as we have more tools for HIV prevention, ‘HIV fatigue’ in donor nations combined with concern from economic downturns form 2008 onwards may result in HIV programs. Past experience suggests, however, that failures in HIV prevention or early treatment will simply cost society more in the long run, given the high direct costs of illness and indirect costs of disability, suffering and death.”
Prevention and treatment programs that incorporate the complexity of “behaviors” necessary for success are a good investment. They will promote health and productivity among individuals and protect society from further disease.
Acknowledgments
Funding support provided by the HIV Prevention Trials Network through the following award: UM1 AI068619
Footnotes
Conflicts: The author has grants/grants pending with the NIH and has been reimbursed for travel by the NIH.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Munderi P, Grosskurth H, Droti B, et al. What are the essential components of HIV treatment and care services in low and middle-income countries: an overview of settings and levels of the health system? AIDS. 2012;(2):S97–S103. doi: 10.1097/QAD.0b013e32835bdde6. [DOI] [PubMed] [Google Scholar]
- 2.Sullivan PS, Carballo-Dieguez A, Coates TJ, et al. Success and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380:388–399. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sawires S, Dworkin S, Fiamma A, et al. Male circumcision and HIV/AIDS: opportunities and challenges. Lancet. 2007;369:708–718. doi: 10.1016/S0140-6736(07)60323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilliam FD, Brooks RA, Leibowitz AA, et al. Framing male circumcision to promote its adoption in different settings. AIDS and Behavior. 2010;14:1207–1211. doi: 10.1007/s10461-009-9656-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baeten JM, Celum C, Coates TJ. Male circumcision and HIV risk and benefits for women. Lancet. 2009;374:182–184. doi: 10.1016/S0140-6736(09)61311-8. [DOI] [PubMed] [Google Scholar]
- 6.Baeten JM, Grant R. Use of antiretrovirals for HIV prevention: what we do and what we don't know. Curr HIV/AIDS Rep. doi: 10.1007/s11904-013-0157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donnell D, Baeten JM, Kiarie J, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort study. Lancet. 2010;375:2092–1098. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Audureau E, Kahn JG, Besson MH, et al. Scaling up prevention of mother-to-child HIV transmission programs in sub-Saharan African countries: a multilevel assessment of site-program-, and country-level determinants of performance. BMC Pub Health. 2013;13:286–296. doi: 10.1186/1471-2458-13-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kresina TF, Lubran R, Clark HW, et al. Substance abuse treatment, HIV/AIDS and the continuum of response for people who inject drugs. Adv Prev Med. 2012:541489. doi: 10.1155/2012/874615. Epub 2012 Nov 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kresina TF, Bruce RD, Mulkevy KP. Evidence-based prevention interventions for people who use illicit drugs. Adv Prev Med. 2013;2013:360957. doi: 10.1155/2013/360957. Epub 2013 March 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coates TJ, Richter L, Caceres C. Behavioural strategies for HIV prevention: How to make them work better. Lancet. 2008:36–51. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dombrowsky JC, Kitahata MM, van Rompanaey SE, et al. High levels of antiretroviral use and viral suppression among persons in HIV care in the United States, 2010. J Acquir Immune Defic Syndr. 2013 Apr 8; doi: 10.1097/QAI.0b013e3182945bc7. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Auerbach J, Coates TJ. HIV prevention research: accomplishments and challenges for the third decade of AIDS. Am J Pub Health. 2000;90:1–4. doi: 10.2105/ajph.90.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szekeres G, Ehrhardt E, Coates TJ. Developing and supporting leadership for HIV/AIDS. AIDS. 2008;(2):S19–S26. doi: 10.1097/01.aids.0000327433.90419.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rachlis B, Sodhi S, Burciul B, et al. A taxonomy for community-based care programs focused on HIV/AIDS prevention, treatment, and care in resource-poor settings. Glob Health Action. 2013;6:1–21. doi: 10.3402/gha.v6i0.20548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vermund S, Hayes RJ. Combination prevention: new hope for stopping the epidemic. Curr HIV/AIDS Rep. 2013 doi: 10.1007/s11904-013-0155-y. Epub ahead of print March 1, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]