Abstract
Introduction:
Total knee arthroplasty (TKA) is the preferred surgical treatment for end-stage osteoarthritis. However, substantial numbers of patients still experience poor outcomes. Consequently, it is important to identify which patient characteristics are predictive of outcomes in order to guide clinical decisions. Our hypothesis is that preoperative patient-reported outcome measures and radiographic measures may help to predict TKA outcomes.
Methods:
Using cohort data from the Osteoarthritis Initiative, we studied 172 patients who underwent TKA. For each patient, we compiled pre- and postoperative Western Ontario and McMaster University Arthritis Index (WOMAC) scores. Radiographs were measured for knee joint angles, femorotibial angles, anatomical lateral distal femoral angles, and anatomical medial proximal tibial angles; Kellgren and Lawrence (KL) grades were assigned to each compartment of the knee. All studied measurements were compared to WOMAC outcomes.
Results:
Preoperative WOMAC disability, pain, and total scores were positively associated with postoperative WOMAC total scores (P = .010, P = .010, and P = .009, respectively) and were associated with improvement in WOMAC total scores (P < .001, P < .001, and P < .001, respectively). For radiographic measurements, preoperative joint angles were positively associated with improvements in postoperative WOMAC total scores (P = .044). Combined KL grades (medial and lateral compartments) were negatively correlated with postoperative WOMAC disability and pain scores (P = .045 and P = .044) and were positively correlated with improvements in WOMAC total scores (P = .001).
Conclusions:
All preoperative WOMAC scores demonstrated positive associations with postoperative WOMAC scores, while among the preoperative radiographic measurements only combined KL grades and joint angles showed any correlation with postoperative WOMAC scores. Higher preoperative KL grades and joint angles were associated with better (lower) postoperative WOMAC scores, demonstrating an inverse correlation.
Keywords: primary total knee arthroplasty, outcome predictors, radiographic measures, patient-reported outcome measures, Kellgren and Lawrence grades
Introduction
Total knee arthroplasty (TKA) is an operation that has become the preferred surgical treatment for end-stage osteoarthritis (OA) of the knee. Furthermore, numerous studies have shown TKA to achieve favorable outcomes and functional gains for a great variety of patient groups.1,2 Total knee arthroplasty has been shown to be highly cost effective, with a recent estimate of an US$11 548 cost per quality-adjusted life-year gained for patients with a mean age of 68 years,3,4 and has excellent long-term success. Ranawat et al showed a 94.1% survivorship at 15 years for TKA.5 Furthermore, TKA continues to be the only intervention, with highly significant gains in quality of life for those patients with severe knee OA.6
With such high rates of efficacy and increasing demand, TKA operations have steadily grown in number to currently more than 600 000 cases per year in the United States, nearly doubling the per capita utilization of the procedure between 1991 and 2010.7,8 Likewise, the annual number of TKA operations in the United States is expected to increase to nearly 3.5 million by 2030, with a majority of these operations performed for patients less than 65 years of age.9,10 Consequently, much research has been done to better understand the patient-related factors that contribute to either favorable or poor patient-reported outcomes.
One of the more interesting findings of such recent studies is the overall effectiveness that TKA has had in patient groups that were previously suspected to be at higher risk of poor outcomes. Neither increased body mass index (BMI), increased age, nor gender has consistently proven to be associated with poor TKA outcomes.2,11,12 However, there are a substantial number of patients who have unfavorable postsurgical function.13,14 These patients may experience no improvement in symptoms after TKA and may even see a decline in overall knee function.14,15 Likewise, it has been shown that up to 20% of patients may be dissatisfied with their TKA operation.16
Although there will always be some unfavorable outcomes with any operation, there is a great interest in being able to preoperatively identify those patients who will have unsatisfactory outcomes after TKA. Many recent studies have sought to predict patient outcomes based on various preoperative patient characteristics, including radiographic findings, knee function scores, mental health, and socioeconomic status.14,17-24 Each of these variables has shown to have some predictive value but each has significant limitations. The situation is further complicated by the relatively weak association between symptoms of patients with OA and radiographic findings.24-26 Therefore, it is all the more important to determine which of these patient characteristics are comparatively most predictive of patient outcome to help develop clinical pathways to improve patient care and ultimate outcomes.
In order to better understand and delineate the compounding factors in TKA outcome, we decided to compare the predictive abilities of preoperative radiographic studies with those of patient-reported characteristics, such as the Western Ontario and McMaster Universities Arthritis Index (WOMAC), in determining TKA outcome. The purpose of our study is to simultaneously observe and compare preoperative radiological findings, patient-reported knee scores, and baseline characteristics in the context of postoperative outcomes. The study uses data from the Osteoarthritis Initiative (OAI), a National Institutes of Health multicenter cohort study of 4796 persons with or at high risk of developing knee OA.27 We hypothesize that (1) preoperative patient-reported function scores will have a greater predictive value of surgical outcome than radiological measures and (2) that general radiological measures of OA, such as Kellgren and Lawrence (KL) grades, will be better predictors of outcome than any specific joint angle measurement.
Methods
The OAI is a publicly and privately funded multicenter, prospective, longitudinal observational study of 4796 patients who have either been diagnosed with clinically significant knee OA (progression subcohort), are at high risk of developing clinically significant knee OA (incidence subcohort), or were recruited as healthy controls.27 All patients enrolled in the study were to attend a baseline visit for clinical evaluation, followed by subsequent annual visits. During each visit, clinical, radiological, and biomarker data were collected. Annual radiological data included a knee magnetic resonance imaging and a fixed flexion posteroanterior (PA) radiograph, among others. All data, including radiographic images, are publicly available on the Osteoarthritis Initiative website.28
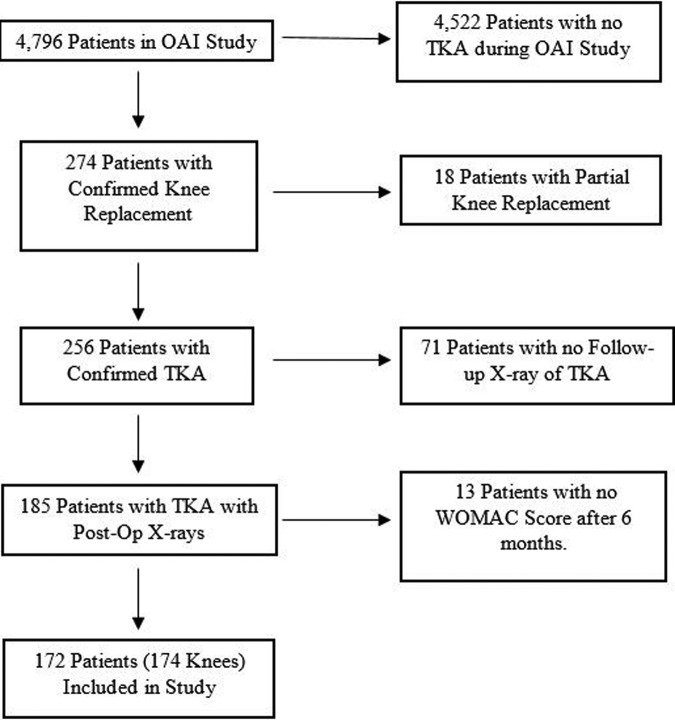
Using the data from the OAI database, our study’s inclusion criteria (Figure 1) included patients who (1) had a confirmed TKA operation (as confirmed through adjudicated medical records) during the course of the OAI study, (2) had OAI x-rays (PA) that confirmed the presence of a TKA, and (3) had at least 1 OAI study visit (baseline or annual visits) before the knee arthroplasty operation. We excluded any patients who (1) had no WOMAC score recorded beyond 6-month postsurgery or (2) had no OAI x-rays taken after the TKA operation. Using these criteria, 172 patients (comprising 174 total knee replacements) were included in our study.
Figure 1.
Study inclusions and exclusions demonstrate the criteria used to select patients from the OAI study for our study; 172 people, comprising 174 knees, were included. OAI indicates Osteoarthritis Initiative.
Pre- and postsurgical WOMAC scores were compiled for each patient included in the study. All presurgical scores were obtained from the last possible recorded scores prior to the TKA. All postsurgical scores were taken from the last OAI visit for each individual patient, such that the longest follow-up period possible between surgery and evaluations was observed for each patient. We decided to use WOMAC scores as a measure of patient-reported outcome as this has been used and validated by various investigators in the past for evaluating both patients undergoing TKA and patients with OA in general.13,17-21,28-30 Most comparisons used the WOMAC total score, the WOMAC disability (function) score, and the respective differences between preoperative and postoperative WOMAC scores, as we assessed these to be the most clinically relevant measures.
The WOMAC scores are reported such that higher WOMAC scores (0-96 scale for total) correlate with a more severe combination of OA symptoms. Changes in WOMAC scores are reported as decreases in WOMAC scores—such that a positive change in WOMAC scores represents a decrease in OA symptoms.
For each knee, the preoperative Knee injury and Osteoarthritis Outcome Score (KOOS) Quality Of Life (QOL) score from the last visit prior to TKA was compared to postoperative WOMAC scores. The KOOS QOL score is a patient-reported survey that reflects the perceived quality of life of the patient in regard to the specified knee.
Bilateral PA fixed flexion knee x-ray images were obtained during weight bearing as the patient stood in 20° to 30° of flexion (Rosenberg view), with feet internally rotated 10°. Both right and left knees were imaged together onto a 14 by 17-in film, using a focus-to-film projection of 72 in. The knees and feet were held in flexion and rotation using a plexiglass positioning frame.27 These x-rays were used to measure pre- and postsurgical joint angle (Figure 2A), anatomical femorotibial angle (Figure 2B), anatomical medial proximal tibial angle (aMPTA; Figure 2C), and anatomical lateral distal femoral angle (aLDFA; Figure 2D) on the affected knee. Preoperative Kellgren-Lawrence (KL) grades were also assigned to medial and lateral compartments of the affected knee. For parts of the analysis, the scores for the medial and lateral KL grades were summed together in order to give an overall grade of radiographic OA in the observed knee. In order to specifically observe the condition of the knees prior to surgery and the immediate physical effect of the surgery, all preoperative images were from the last possible image set for each patient, while all postoperative images were from the first image set after the TKA. All radiological measurements were made by a single musculoskeletal radiologist and were reviewed by the senior author.
Figure 2. A,.

Joint line congruency angle: the angle between the distal femur joint orientation line (line drawn between the most distal points of each femoral condyle) and proximal tibia joint orientation line (line drawn along the tibial plateaus). In this example, it measures 0.8°. B, Anatomic femorotibial angle: the angle formed by the lines that pass through the center of the diaphysis along the length of each bone. In this example, it measures 173.5°. C, Anatomic medial proximal tibial angle: the angle between the proximal tibia joint orientation line (line drawn along the tibial plateaus) and the anatomic axis of the tibia. In this example, it measures 86.9°. D, Anatomic lateral distal femoral angle: the angle between the distal femur joint orientation line (line drawn between the most distal points of each femoral condyle) and the anatomic axis of the femur. In this example, it measures 82.2°.
Statistical Analysis
Data analysis was done using IBM SPSS Statistics Version 21 (Armonk, New York). The data were initially studied using Pearson correlation studies to find significant relationships between preoperative clinical measurements and surveys and postoperative outcomes, measured using total WOMAC and WOMAC subset scores.
For each patient, preoperative joint angle, anatomical femorotibial angle, KL grade, aMPTA, and aLDFA were compared to WOMAC outcomes to determine the association between radiographic observations and outcomes. Likewise, postoperative joint angle, anatomical femorotibial angle, aMPTA, and aLDFA were compared to postoperative WOMAC scores.
For the anatomical femorotibial angle, patients were divided into 2 groups depending on whether the angle was varus (angle > 174°) or valgus (<174°). For both the varus and the valgus groups, Pearson correlations were measured when compared to postoperative WOMAC total scores. The patients were also further subdivided into groups with valgus (<173°), varus (>178°), or neutral (>173° and <178°) femorotibial angles. These groups were determined using the work of Fang et al who showed that the standard deviation of postoperative femorotibial angles for 6070 knees with TKA was 2.4° to 7.2° of valgus.31 Similar grouping was done for both aMPTA and aLDFA measurements. For aMPTA, patients with a less than 90° measurement were grouped as varus and those with above 90° were grouped as valgus. For aLDFA, patients with measurements below 82° were grouped as valgus and those with measurements above 86° were grouped as varus. Patients with aLDFA measurements of 82° to 86° were grouped as neutral. This grouping was done using the work of Ritter et al, which demonstrated significantly worse outcomes for knees with postoperative aLDFA measurements beyond 8° valgus.32 For pre- and postoperative joint angle measurements, patients were separated into groups of 4° increments for analysis—these intervals simply represented what we considered to be low, middle, and high values. One-way analysis of variance (ANOVA) was used to test for significant differences in postoperative WOMAC scores between groups.
Results
The average preoperative WOMAC total score for the studied patients was 35.0 (range: 0-73 and standard deviation: 17.6) while the average postoperative WOMAC total score was 12.6 (range: 0-51.1 and standard deviation: 13.4), signifying an average change in WOMAC score of 21.5 (P < .001, range: −28-70, and standard deviation: 19.9) and an overall improvement in osteoarthritic symptoms (Table 1). The average time between the TKA surgery and the postoperative WOMAC measurement was 3.0 years (0.5-6.1 years).
Table 1.
Baseline Characteristics.
| Male (N = 70) | Female (N = 102) | Total (172) | |
|---|---|---|---|
| Age | 68.1 (SD = 8.6) | 66.3 (SD = 8.0) | 67.0 (SD = 8.3) |
| Side | |||
| Right | 25 | 50 | 79 |
| Left | 45 | 54 | 95 |
| Race | |||
| Caucasian | 63 (92.6%) | 83 (82.2%) | 146 (84.9%) |
| African American | 5 (7.4%) | 17 (16.8%) | 22 (12.8%) |
| Asian | 0 | 1 (1.0%) | 1 (0.6%) |
| Other or N/A | 2 | 1 | 3 |
| BMI | 29.5 (SD = 3.9) | 30.7 (SD = 5.6) | 30.2 (SD = 5.0) |
| Days between OAI visit with x-ray and TKA | 225.8 (SD = 198.8) | 238.2 (SD = 194.4) | 233.2 (SD = 196.3) |
| Years between TKA and outcome measures | 2.8 (SD = 1.5) | 3.0 (SD = 1.5) | 3.0 (SD = 1.5, 0.5-6.1) |
| Preop | |||
| WOMAC total (0-96) | 29.8 (SD = 16.9) | 38.6 (SD = 17.2) | 35.0 (SD = 17.6) |
| WOMAC pain (0-20) | 6.4 (SD = 3.7) | 8.0 (SD = 4.1) | 7.3 (SD = 4.0) |
| WOMAC disability (0-68) | 20.4 (SD = 12.8) | 26.7 (SD = 12.5) | 24.1 (SD = 13.0) |
| WOMAC stiffness (0-8) | 3.1 (SD = 1.8) | 3.9 (SD = 1.6) | 3.6 (SD = 1.7) |
| Postop | |||
| WOMAC total (0-96) | 10.8 (SD = 13.2) | 13.9 (SD = 13.4) | 12.6 (SD = 13.4) |
| WOMAC pain (0-20) | 1.9 (SD = 2.6) | 2.2 (SD = 2.7) | 2.1 (SD = 2.7) |
| WOMAC disability (0-68) | 7.5 (SD = 9.6) | 9.9 (SD = 10.1) | 8.9 (SD = 10.0) |
| WOMAC stiffness (0-8) | 1.4 (SD = 1.4) | 1.8 (SD = 1.5) | 1.6 (SD = 1.5) |
| Gain/lossa | |||
| WOMAC total | 19.0 (SD = 18.7) | 24.7 (SD = 20.3) | 22.4 (SD = 19.9) |
| WOMAC pain | 4.5 (SD = 3.8) | 5.8 (SD = 4.8) | 5.3 (SD = 4.4) |
| WOMAC disability | 12.9 (SD = 14.3) | 16.7 (SD = 14.7) | 15.2 (SD = 14.7) |
Abbreviations: BMI, body mass index; SD, standard deviation; N/A, not applicable; OAI, Osteoarthritis Initiative; preop; preoperative; postop; postoperative; TKA, total knee arthroplasty; WOMAC, Western Ontario and McMaster Universities Arthritis Index. aChange in WOMAC Total or WOMAC Disability is presented as a decrease in WOMAC score - i.e. a positive change would represent an overall decrease in score.
Preoperative Patient-Reported Measures
Among the patient-reported outcome measures (PROMs) used (Table 2), preoperative WOMAC disability, pain, and total scores were significantly associated with postoperative WOMAC total scores (r = .196, P = .010; r = .195, P = .010; and r = .198, P = .009, respectively). Preoperative WOMAC disability, pain, and total scores were all strongly correlated with an overall change in WOMAC total (r = .738, P < .001; r = .634, P < .001; and r = .749, P < .001, respectively), meaning that a higher preoperative WOMAC total score correlated with a greater decrease in WOMAC total.
Table 2.
Associations Between Preoperative Patient Factors and Postoperative WOMAC Scores.
| Postop WOMAC Total | Postop WOMAC Disability | Postop WOMAC Pain | Changes in WOMAC Totala | Change in WOMAC Disabilitya | |
|---|---|---|---|---|---|
| Preop WOMAC total | |||||
| Pearson | .198b | .197b | .165b | .749b | .733b |
| P value | .009 | .009 | .030 | <.001 | <.001 |
| Preop WOMAC disability | |||||
| Pearson | .196b | .197b | .152b | .738b | .746b |
| P value | .010 | .009 | .045 | <.001 | <.001 |
| Preop WOMAC pain | |||||
| Pearson | .195b | .189b | .192b | .634b | .559b |
| P value | .010 | .013 | .011 | <.001 | <.001 |
| Preop age | |||||
| Pearson | .051 | .043 | .044 | −.103 | −.096 |
| P value | .505 | .573 | .565 | .175 | .207 |
| Preop BMI | |||||
| Pearson | .122 | .128 | .056 | .080 | .089 |
| P value | .110 | .092 | .464 | .294 | .245 |
Abbreviations: BMI, body mass index; preop; preoperative; postop; postoperative; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
a Change in WOMAC total or WOMAC disability is presented as a decrease in WOMAC score, that is, a positive change would represent an overall decrease in score. b p < 0.05
The preoperative KOOS QOL measure was negatively correlated with changes in WOMAC total (r = −.484 and P < .001) and WOMAC disability (r = −.481 and P < .001). Neither age nor BMI at time of operation showed any correlation with WOMAC outcome scores.
Association Analysis of Radiographic Measurements
The preoperative femorotibial angle was not significantly associated with postoperative WOMAC total scores in patients with a varus or valgus femorotibial measurement (Tables 3 and 4). Neither the preoperative aLDFA nor the preoperative aMPTA was associated with postoperative WOMAC total or change in WOMAC score. The preoperative joint angle was positively associated with a change in WOMAC total scores (r = .153 and P = .044).
Table 3.
Pearson Correlations Between Radiographic Measures and Postoperative WOMAC Scores.
| Postoperative Measures in Index Knee | ||||
|---|---|---|---|---|
| Number of Patients | Number of Cases | WOMAC Total | Change in WOMAC Total | |
| Preoperative measures | ||||
| Medial KL grade | 174 | Pearson r | −.115 | .090 |
| P value | .131 | .238 | ||
| Lateral KL grade | 174 | Pearson r | −.039 | .181a |
| P value | .661 | .017 | ||
| Combined KL grade | 174 | Pearson r | −.146 | .254a |
| P value | .055 | .001 | ||
| Femorotibial angle (varus patients) | 118 | Pearson r | −.057 | −.002 |
| P value | .538 | .984 | ||
| Femorotibial angle (valgus patients) | 56 | Pearson r | −.059 | .098 |
| P value | .666 | .473 | ||
| Joint angle | 174 | Pearson r | −.113 | .153a |
| P value | .138 | .044 | ||
| aLDFA (varus patients) | 72 | Pearson r | .055 | −.061 |
| P value | .645 | .608 | ||
| aLDFA (valgus patients) | 42 | Pearson r | −.168 | .001 |
| P value | .288 | .994 | ||
| aMPTA (varus patients) | 118 | Pearson r | −.101 | .157 |
| P value | .275 | .090 | ||
| aMPTA (valgus patients) | 56 | Pearson r | −.002 | −.106 |
| P value | .990 | .436 | ||
Abbreviations: aLDFA, anatomical lateral distal femoral angle; aMPTA, anatomical medial proximal tibial angle; KL, Kellgren and Lawrence; WOMAC, Western Ontario and McMaster Universities Arthritis Index. a p < 0.05
Table 4.
Pearson Correlations Between Postoperative Radiographic Measures and Postoperative WOMAC Scores.
| Number of Patients | Number of Cases | WOMAC Total | Decrease in WOMAC Total | |
|---|---|---|---|---|
| Postoperative measures | ||||
| Femorotibial angle (varus patients) | 76 | Pearson r | .106 | −.130 |
| P value | .360 | .263 | ||
| Femorotibial angle (valgus patients) | 98 | Pearson r | .052 | .010 |
| P value | .610 | .922 | ||
| Joint angle | 174 | Pearson r | −.106 | .096 |
| P value | .163 | .207 | ||
| aLDFA (varus patients) | 124 | Pearson r | −.008 | .020 |
| P value | .930 | .822 | ||
| aLDFA (valgus patients) | 18 | Pearson r | −.229 | −.053 |
| P value | .361 | .834 | ||
| aMPTA (varus patients) | 32 | Pearson r | .111 | .143 |
| P value | .547 | .434 | ||
| aMPTA (valgus patients) | 142 | Pearson r | .115 | −.078 |
| P value | .172 | .355 | ||
Abbreviations: aLDFA, anatomical lateral distal femoral angle; aMPTA, anatomical medial proximal tibial angle; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
There were no significant associations between postoperative WOMAC scores and the postoperative joint angle, aLDFA, or aMPTA. The postoperative femorotibial angles of patients with varus or valgus measurements had no significant association with postoperative WOMAC total or change in WOMAC scores (Table 4).
Subgroup Analysis of Radiographic Measures
For patients grouped into 4° intervals of preoperative joint angle (Table 5), there was a significant difference in WOMAC total scores between the groups (F = 7.276 and P = .001), with a post hoc Tukey test showing that patients who had 4° to 8° of preoperative joint angle had significantly lower postoperative WOMAC scores (better outcomes) than patients with 0° to 4° of preoperative joint angle (P = .001). There was no significant difference between patients with 8° to 12° of preoperative joint angle and the other groups with lesser angles. There was a significant difference in change in WOMAC total scores between subgroups of preoperative joint angle as well (F = 4.395 and P = .014). A post-hoc Tukey test showed that patients with 4° to 8° of preoperative joint angle had significantly greater change in WOMAC scores (greater improvement) than patients with 0° to 4° of preoperative joint angle (P = .01), while patients with 8° to 12° of pre-operative joint angle were not significantly different from the other groups. The ANOVA testing of groups’ postoperative WOMAC scores, when grouped by preoperative aMPTA, aLDFA, or femorotibial angle, showed no significant differences between groups. Average postoperative WOMAC total and change in WOMAC scores for each subgroup of each radiographic measurement are reported in Table 5.
Table 5.
Preoperative Subgroups of Radiographic Measures.
| Number of Cases | Average WOMAC Total | Average Change in WOMAC Total | |
|---|---|---|---|
| Femorotibial angle | |||
| <173 (valgus) | 47 | 14.90 | 19.36 |
| 173-178 (neutral) | 52 | 12.05 | 24.24 |
| >178 (varus) | 75 | 11.64 | 22.83 |
| ANOVA F score (P value) | 0.919 (.401) | 0.782 (.459) | |
| aMPTA | |||
| <90 (varus) | 118 | 12.17 | 23.09 |
| >90 (valgus) | 56 | 13.63 | 20.67 |
| Student t test (P value) | .505 | .524 | |
| aLDFA | |||
| <82 (valgus) | 15 | 17.45 | 19.71 |
| 82-86 (neutral) | 87 | 13.04 | 19.59 |
| >86 (varus) | 72 | 11.16 | 26.14 |
| ANOVA F score (P value) | 1.433 (.241) | 2.298 (.104) | |
| Joint angle | |||
| 0-4 | 63 | 16.92 | 16.58 |
| 4-8 | 100 | 9.41a (P = .001) | 25.90a (P = .010) |
| 8-12 | 11 | 17.53 | 22.46 |
| ANOVA F score (P value) | 7.276 (.001) | 4.395 (.014) | |
| KL grade (medial + lateral) | |||
| Grade 4 or less | 20 | 16.71 | 11.34 |
| Grade 5 | 61 | 13.78 | 19.93 |
| Grade 6 | 74 | 11.46 | 25.06b (P = .028) |
| Grade 7 or greater | 19 | 9.29 | 30.83b (P = .011) |
| ANOVA F score (P value) | 1.343 (.262) | 4.159 (.007) | |
Abbreviations: aLDFA, anatomical lateral distal femoral angle; aMPTA, anatomical medial proximal tibial angle; ANOVA, analysis of variance; KL, Kellgren and Lawrence; WOMAC, Western Ontario and McMaster Universities Arthritis Index. aThe group of knees with 4-8-degrees of joint angle was significantly different compared to the group with 0-4-degrees of joint angle with respect to WOMAC Total (p = .001) and Change in WOMAC Total (p = .010) bgroups of knees with KL grades of 6 or 'grade 7 or greater' had significantly greater changes in WOMAC Total compared to the group of knees with KL grades of '4 or less.
For postoperative radiographic measurements (Table 6), the 1-way ANOVA test demonstrated no significant difference in postoperative WOMAC scores between subgroups of postoperative femorotibial angle, aLDFA, or aMPTA. All patients had between 0° and 4° of postoperative joint angle so no further analysis was done using this data.
Table 6.
Postoperative Subgroups of Radiographic Measures.
| Number of Cases | Average WOMAC Total | Average Change in WOMAC Total | |
|---|---|---|---|
| Femorotibial angle | |||
| <173 (valgus) | 78 | 13.36 | 22.69 |
| 173-178 (neutral) | 82 | 11.84 | 22.04 |
| >178 (varus) | 14 | 13.31 | 21.84 |
| ANOVA F score (P value) | 0.270 (P = .764) | 0.025 (P = .975) | |
| aMPTA | |||
| <90 (varus) | 32 | 12.36 | 22.18 |
| >90 (valgus) | 142 | 12.70 | 22.34 |
| Student t test (P value) | .896 | .967 | |
| aLDFA | |||
| <82 (valgus) | 4 | 16.58 | 30.15 |
| 82-86 (neutral) | 46 | 8.90 | 26.04 |
| >86 (varus) | 124 | 13.90 | 20.68 |
| ANOVA F score (P value) | 2.537 (P = .082) | 1.540 (P = .217) | |
Abbreviations: aLDFA, anatomical lateral distal femoral angle; aMPTA, anatomical medial proximal tibial angle; ANOVA, analysis of variance; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
For patients separated into varus and valgus groups of preoperative femorotibial angle, we found no significant difference in postoperative WOMAC total or change in WOMAC total scores between groups. Similar results were seen with preoperative aMPTA varus and valgus grouping. One-way ANOVA testing did not show any significant difference in postoperative WOMAC total or change in WOMAC scores between aLDFA varus, neutral, or valgus groups.
Preoperative KL Grades
The medial KL grade by itself was not significantly associated with postoperative WOMAC scores although the lateral KL grade was positively associated with decreases in WOMAC total score, meaning that more severe OA in the lateral compartment (as determined by the KL grading scale) was associated with larger changes (or “gains”) for the patient (Table 3). The combined KL grade (formed by simple addition of the medial and lateral KL grade for the operated knee) was not significantly correlated with WOMAC total (r = −.146 and P = .055; Table 3) but was significantly associated with WOMAC disability (r = −.152 and P = .045), and pain (r = −.153 and P = .044). The combined KL grade was also more strongly associated with decreases in WOMAC total (r = .254 and P = .001; Table 3) and disability (r = .256 and P = .001). These findings show that higher combined KL grades were associated with lower (less symptomatic) postoperative WOMAC scores and larger changes (greater improvement) in WOMAC score.
After grouping patients by their combined preoperative KL grade, 1-way ANOVA testing showed a significant difference in overall change in WOMAC total scores between groups (F = 4.159 and P = .007). A post hoc Tukey test demonstrated that groups of patients with KL grade 6 or grade 7+ had significantly better improvement in WOMAC total scores when compared to patients with a KL grade 4 or less (P = .028 and P = .011, respectively).
Discussion
Addressing our first hypothesis, we found that preoperative WOMAC scores (especially the WOMAC total, WOMAC pain, or WOMAC disability scores) had a stronger correlation with postoperative WOMAC scores than any of the observed preoperative radiographic measures. Although some of the preoperative radiographic measures (ie, combined KL grades and joint angles) demonstrated a correlation with postoperative WOMAC scores, the strength of these relationships was substantially less than those seen with preoperative WOMAC scores and were limited to subsets of postoperative WOMAC disability and WOMAC pain (for KL grades) and changes in WOMAC total (KL grades and joint angles). Addressing our second hypothesis, of the preoperative radiographic measurements in our study, we found only KL grades and joint angles to show any correlation with subsets of postoperative WOMAC scores. Therefore, we conclude that these 2 preoperative radiographic measurements show the greatest correlation with postoperative outcomes among the common radiographic measures in our study although neither radiographic measurement was significantly correlated with absolute WOMAC total scores. Consequently, our hypothesis that radiographic measures, which directly measure osteoarthritic lesions, such as KL grades, would be most predictive of postoperative outcomes was supported by our findings, with the exception of preoperative joint angles.
As expected, most patients in our study had an overall positive outcome after TKA surgery (average decrease in WOMAC total score was 21.5 points). We also confirmed the results of several previous studies that found preoperative PROMs to be positively associated with postoperative PROMs.14,19,20,22 The observed relationship between pre- and postoperative PROMs described in this study may be a result of the continuous presence of detrimental factors, such as severe OA in other joints, other lower limb joint pain, and so on.
Slightly less intuitively understood are our results that show a strong association between preoperative WOMAC scores and greater decreases in WOMAC total and disability scores following TKA. Similar results were described by Fortin et al where the decrease between preoperative and postoperative WOMAC scores at 6 months showed a positive correlation with preoperative WOMAC scores.20 As Fortin and colleagues suggested, these results seem to imply that the patients with worst PROMs have the most function to gain from TKA, since they have such poor pain control and function to begin with. This is not to say that these patients have better absolute outcomes since preoperative WOMAC totals are positively correlated with postoperative WOMAC totals but instead that these patients see the biggest change, or gain, in function. Consequently, these results allow for better clinical judgment in interpreting the worse outcomes associated with poor preoperative PROMs—while a patient with poor preoperative function may never reach the same absolute postoperative “score” as a patient with a higher preoperative function, they may likely experience greater relative gains that may translate to higher relative patient satisfaction and so should not necessarily be deterred from pursuing TKA surgery.
Radiological measurements showed interesting results in terms of their relation to the postoperative WOMAC scores. Larger preoperative joint angles were correlated with higher decreases in WOMAC total, again likely reflecting the possibility for larger improvements that patients with more severe knee OA (or more deformed knee joints) have. When grouped by preoperative joint angle, the patients with 4° to 8° of preoperative joint angle had the lowest postoperative WOMAC total scores (representing the best outcomes). The group of patients with only 0° to 4° of joint angle had the highest postoperative WOMAC scores (representing the worst outcomes). This finding suggests a relationship between preoperative joint angle and postoperative PROMs such that patients with joint angles in the 4° to 8° range typically have better TKA outcomes than patients with joint angles closer to 0. Furthermore, such a finding seems to suggest that patients with greater preoperative joint angles tend to have better TKA outcomes in general. However, the lack of significant differences between the 4° and 8° joint angle group and the 8° to 12° joint angle group suggests that this relationship may be nonlinear.
None of the postoperative radiographic measurements showed any association with the postoperative WOMAC measured outcomes. This may be due to the relatively small variation in postoperative radiographic measures seen between patients following TKA operations. For instance, the largest joint angle measured postoperatively was 2.1°, demonstrating a small range and far less variation. In contrast to our findings, Fang et al showed that patients with postoperative femorotibial angles greater than 7.2° of valgus or less than 2.4° of valgus had significantly worse outcomes than those in between these angles (neutral).31 Likewise, Ritter et al showed that patients with less than 90° of postoperative aMPTA or greater than 8° valgus of postoperative aLDFA had significantly worse outcomes than patients with more neutral aMPTA and aLDFA measurements.32 However, both of these studies observed more than 6 000 knees, lending far more power to the analysis. Consequently, the lack of significance in our study regarding these measurements may simply indicate the smaller study sample.
One of the more interesting results of our study was the association between preoperative KL grades and the postoperative WOMAC scores. When using medial or lateral compartment KL grades individually for each patient, only the lateral KL grade was shown to correlate with positive changes in WOMAC total scores. Just as with preoperative PROMs, this could be the result of simply more function to gain for patients with more severe knee OA initially, especially since lateral compartment involvement is generally related to later progression of OA.24 Furthermore, when the KL grades were combined from each compartment, the results showed significant negative correlations for WOMAC disability and pain scores as well as stronger positive associations between KL grades and overall change in WOMAC total and disability, indicating that patients with more severe preoperative radiographic OA had greater overall improvement as measured by PROMs.
Importantly, the combined KL grades demonstrated an inverse correlation with absolute postoperative WOMAC disability and pain scores, meaning that higher KL grades (representing more severe radiographic OA) were shown to be associated with lower (less symptomatic) absolute postoperative WOMAC scores. Valdez et al described similar results when they compared radiographic severity to postoperative outcome, reporting lower absolute postoperative WOMAC scores when preoperative KL grades were higher.28 Although this relationship seems to be contradictory to that observed between pre- and postoperative PROMs, the differences may, at the least, reflect the underlying, fundamental differences between radiographic measures of OA and patient-reported symptoms of OA. As Dowsey et al showed with their work comparing preoperative PROMs to radiographic measures of OA severity, there is surprisingly little association between radiographic assessments of OA and symptoms reported by the patient.24 Therefore, it seems possible that the relationship between radiographic OA severity (as determined by KL grading) and postoperative outcomes might be relatively unrelated to the relationship seen between preoperative PROMs and postoperative outcomes. Further work is needed to more fully understand this relationship.
There are some limitations to this study. First, although the sample size of 172 patients was not insufficient for testing, a larger sample size would have provided more reliable and generalizable results. Second, due to the nature of the OAI cohort data, and our wish to use the longest follow-ups possible for WOMAC measurements, the time between the TKA operation and the postoperative WOMAC score used was highly variable. We considered this variability acceptable since we were judging eventual outcomes and not specific progression; however, a more uniform follow-up time would have provided more precise results. Finally, we realize that the WOMAC score is only one means of measuring patients’ outcomes after TKA; consequently, our results are limited in scope in this regard.
In concurrence with previous works in this area, we found preoperative PROMs, especially preoperative WOMAC scores, to be positively associated with postoperative WOMAC scores. Overall, our findings indicate that preoperative PROMs are more reliably associated with postoperative PROMs than are preoperative radiographic measurements. We also demonstrated that some preoperative radiographic measures, such as KL grades or joint angles, are inversely correlated with postoperative WOMAC scores although these relationships were only found regarding postoperative WOMAC disability and WOMAC pain scores (for KL grades) and overall change in WOMAC total (for KL grades and joint angles). However, the relationship between radiographic measurements and TKA outcomes deserves further investigation.
Acknowledgments
The OAI is a public–private partnership comprised of 5 contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This article was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Footnotes
Authors’ Note: All authors contributed to the design of the study, the collection of data, the analysis and interpretation of the data, the drafting and revision of the article, and the final approval of the article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The senior author is on the editorial board for Journal of Arthroplasty, serves on the American Academy of Orthopaedic Surgeons, and is also a paid consultant of Smith and Nephew and holds stocks in Pristine. There are no other potential conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg. 2004;86(5):963–974 [DOI] [PubMed] [Google Scholar]
- 2. Santaguida PL, Hawker GA, Hudak PL, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51(6):428–436 [PMC free article] [PubMed] [Google Scholar]
- 3. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States. Arch Intern Med. 2009;169(12):1113–1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol. 2012;26(5):649–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ranawat CS, Flynn WF, Jr, Saddler S, Hansraj KK, Maynard MJ. Long-term results of the total condylar knee arthroplasty. a 15-year survivorship study. Clin Orthop Relat Res. 1993;(286):94–102 [PubMed] [Google Scholar]
- 6. Jüni P, Reichenbach S, Dieppe P. Osteoarthritis: rational approach to treating the individual. Best Pract Res Clin Rheumatol. 2006;20(4):721–740 [DOI] [PubMed] [Google Scholar]
- 7. Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991-2010. JAMA. 2012;308(12):1227–1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. FastStats Inpatient surgery. Hyattsville, MD: Centers for Disease Control National Center for Health Statistics; 2010 [Google Scholar]
- 9. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785 [DOI] [PubMed] [Google Scholar]
- 10. Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthopaed Relat Res. 2009;467(10):2606–2612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ayyar V, Burnett R, Coutts FJ, van der Linden ML, Mercer TH. The Influence of obesity on patient reported outcomes following total knee replacement. Arthritis. 2012;2012:185–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Baker P, Petheram T, Jameson S, Reed M, Gregg P, Deehan D. The association between body mass index and the outcomes of total knee arthroplasty. J Bone Joint Surg. 2012;94(16):1501–1508 [DOI] [PubMed] [Google Scholar]
- 13. Wylde V, Dieppe P, Hewlett S, Learmonth ID. Total knee replacement: Is it really an effective procedure for all? Knee. 2007;14(6):417–423 [DOI] [PubMed] [Google Scholar]
- 14. Judge A, Arden NK, Cooper C, et al. Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford). 2012;51(10):1804–1813 [DOI] [PubMed] [Google Scholar]
- 15. Kennedy LG, Newman JH, Ackroyd CE, Dieppe PA. When should we do knee replacements? Knee. 2003;10(2):161–166 [DOI] [PubMed] [Google Scholar]
- 16. Scott CE, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92(9):1253–1258 [DOI] [PubMed] [Google Scholar]
- 17. Becker R, Döring C, Denecke A, Brosz M. Expectation, satisfaction and clinical outcome of patients after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1433–1441 [DOI] [PubMed] [Google Scholar]
- 18. Colbert CJ, Song J, Dunlop D, et al. Knee confidence as it relates to physical function outcome in persons with or at high risk of knee osteoarthritis in the osteoarthritis initiative. Arthritis Rheum. 2012;64(5):1437–1446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Escobar A, Quintana JM, Bilbao A, et al. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology. 2007;46(1):112–119 [DOI] [PubMed] [Google Scholar]
- 20. Fortin PR, Clarke AE, Joseph L, et al. Outcomes of total hip and knee replacement: Preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42(8):1722–1728 [DOI] [PubMed] [Google Scholar]
- 21. Hirschmann MT, Testa E, Amsler F, Friederich NF. The unhappy total knee arthroplasty (TKA) patient: higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2405–2411 [DOI] [PubMed] [Google Scholar]
- 22. Lingard EA, Katz JN, Wright EA, Sledge CB, Kinemax Outcomes Group Predicting the outcome of total knee arthroplasty. J Bone Joint Surg. 2004;86(10):2179–2186 [DOI] [PubMed] [Google Scholar]
- 23. Lundblad H, Kreicbergs A, Söderlund V, Ulfgren AK, Stiller CO, Jansson KÅ. The value of preoperative grade of radiographic and histological changes in predicting pain relief after total knee arthroplasty for osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;9(20):1815–1821 [DOI] [PubMed] [Google Scholar]
- 24. Dowsey MM, Dieppe P, Lohmander S, Castle D, Liew D, Choong PF. The association between radiographic severity and pre-operative function in patients undergoing primary knee replacement for osteoarthritis. Knee. 2012;19(6):860–865 [DOI] [PubMed] [Google Scholar]
- 25. Barker K, Lamb SE, Toye F, Jackson S, Barrington S. Association between radiographic joint space narrowing, function, pain and muscle power in severe osteoarthritis of the knee. Clin Rehabil. 2004;18(7):793–800 [DOI] [PubMed] [Google Scholar]
- 26. Baert IA, Staes F, Truijen S, et al. Weak associations between structural changes on MRI and symptoms, function and muscle strength in relation to knee osteoarthritis [published online February 2, 2013]. Knee Surg Sports Traumatol Arthrosc. 2013 [DOI] [PubMed] [Google Scholar]
- 27. Lester G. The osteoarthritis initiative: a NIH public–private partnership. HSS J. 2012;8(1):62–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. OAIOnline [Internet]. University of California, San Francisco; 2013. http://oai.epi-ucsf.org/datarelease/default.asp Accessed November 22, 2013
- 29. Valdes AM, Doherty SA, Zhang W, Muir KR, Maciewicz RA, Doherty M. Inverse relationship between preoperative radiographic severity and postoperative pain in patients with osteoarthritis who have undergone total joint arthroplasty. Semin Arthritis Rheum. 2012;41(4):568–575 [DOI] [PubMed] [Google Scholar]
- 30. Katz JN, Mahomed NN, Baron JA, et al. Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56(2):568–574 [DOI] [PubMed] [Google Scholar]
- 31. Jones CA, Voaklander DC, Suarez-Alma ME. Determinants of function after total knee arthroplasty. Phys Ther. 2003;83(8):696–706 [PubMed] [Google Scholar]
- 32. Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 suppl):39–43 [DOI] [PubMed] [Google Scholar]
- 33. Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93(17):1588–1596 [DOI] [PubMed] [Google Scholar]