Abstract
BACKGROUND AND OBJECTIVES:
Although nurse home visiting has proven efficacious with small samples, scaling up to community populations with diverse families has not yet proven effective. The Durham Connects program was developed in collaboration with community leaders as a brief, universal, postnatal nurse home visiting intervention designed to screen for risk, provide brief intervention, and connect families with more intensive evidence-based services as needed. This study tested program effectiveness in reducing infant emergency medical care between birth and age 12 months.
METHODS:
All 4777 resident births in Durham, North Carolina across 18 months were randomly assigned, with even birth date families to intervention and odd birth date families to control. Intervention families were offered 3 to 7 contacts between 3 and 12 weeks after birth to assess family needs and connect parents with community resources to improve infant health and well-being. Hospital records were analyzed by using an intent-to-treat design to evaluate impact among a representative subset of 549 families.
RESULTS:
After demographic factors (ie, birth risk, Medicaid status, ethnicity, and single parenthood) were covaried, relative to control families, families assigned to intervention had 50% less total emergency medical care use (mean [M] emergency department visits and hospital overnights) (Mintervention = 0.78 and Mcontrol = 1.57; P < .001, effect size = 0.28) across the first 12 months of life.
CONCLUSIONS:
This brief, universal, postnatal nurse home visiting program improves population-level infant health care outcomes for the first 12 months of life. Nurse home visiting can be implemented universally at high fidelity with positive impacts on infant emergency health care that are similar to those of longer, more intensive home visiting programs. This approach offers a novel solution to the paradox of targeting by offering individually tailored intervention while achieving population-level impact.
Keywords: home visiting, prevention, child injuries
By providing funds for community-wide implementation of home visiting programs, the Affordable Care Act of 20101 heightened the need for rigorous evaluation of impact when programs are implemented at scale in community settings. Although some evidence supports the positive impact of nurse home visiting programs on reducing infant injuries when the program is implemented with small samples,2,3 it has been reported that community-wide implementation of the same programs reduces participation and retention rates by up to 67%,4 decreases implementation fidelity by up to 50%,5 and raises challenges in finding adequate community resources to meet every family’s identified needs.6 Distressingly, Matone et al7 found 14% more injuries for home-visited infants than matched comparison infants when an evidence-based program was scaled up in a community setting.
Problems in community-wide implementation have been overcome by the Durham Connects (DC) program,8 which was designed in collaboration with community leaders and piloted at the population level before evaluation by a randomized controlled trial (RCT). DC is a short-term, universal, inexpensive ($700 per family) postnatal nurse home visiting program designed to provide brief parenting intervention and to connect families with community resources based on individualized assessments of family needs. It does not replace the need for more intensive programs but rather serves as a universal screening and triage tool to ensure optimal matching and follow-through of families with services. Community leaders signed a memorandum of agreement to align community-based resources with birth family needs. Dodge et al8 reported a participation rate of 80% of the community population of families of newborns while maintaining 84% fidelity to the manualized DC protocol. An RCT with every birth in the Durham, North Carolina community over an 18-month period found that by age 6 months DC increases a family’s community connections, improves positive parenting behavior, and decreases emergency medical care costs by 59%. Because the program might merely defer inevitable emergency medical care and therefore have only short-lived impact, the primary goal of the current study was to evaluate impact of random assignment to DC on preventing emergency medical care (emergency department [ED] visits and hospital overnights) at infant age 12 months, well after the nurse home visitor had ended contact with the family.
The secondary goal of this study was to evaluate whether the impact of the DC program held across diverse types of families. Some home visiting programs target low-income families only,2 whereas DC targets every birthing family, raising the question of whether impact holds across income levels. Variation in impact across Medicaid and private insurance groups could influence public policy about eligibility for home visiting and private policies about whether to include home visiting in covered preventive care. We also examined whether impact varied as a function of infant medical risk, ethnicity, single-parent household status, and infant gender.
This study has been approved continuously by the Duke University Institutional Review Board since before the beginning of the study.
Methods
The Durham Connects Program
DC was piloted for 3 years, with iterative improvement before testing by an RCT. It was developed and implemented jointly by the Durham County, North Carolina Health Department and Duke University. The community wanted a program that is short-term, inexpensive, community-owned, aligned with community services, and universal, to ensure that families do not think participation stigmatizes them as “poor or risky” and to ensure buy-in from all community sectors.
DC engages every family but rapidly triages and concentrates resources to families with assessed higher needs. It is highly structured (the manual is available on request from dodge@duke.edu), consisting of 4 to 7 scripted in-person or telephone intervention contacts, beginning during a birthing hospital visit; 1 to 3 nurse home visits between 3 and 8 weeks of infant age; 1 or 2 nurse contacts with community service providers and maternal and infant health care providers; and an in-person or telephone follow-up 1 month later to reinforce community connections.
During home visits, the nurse engages the mother and father (when possible), provides brief educational interventions organized as 20 “teaching moments,” and assesses and scores health and psychosocial risk in each of 12 domains: parenting/childcare (childcare plans, parent–infant relationship, and management of infant crying), family violence/safety (material supports, family violence, past maltreatment), parent mental health/well-being (depression/anxiety, substance abuse, emotional support), and health care (parent health, infant health, and health care plan). A score of 1 (low risk) in a particular area receives no subsequent intervention. For a score of 2 (moderate risk), the nurse delivers a brief, evidence-based (when available) intervention on that particular topic over 1 to 3 sessions. For a score of 3 (high risk), the nurse uses motivational interviewing to connect the family with community resources tailored to address the particular risk (eg, short-term loans, treatment of depression or substance abuse). A score of 4 (imminent risk) receives emergency intervention. A final session 4 weeks after the nurse completes the case reinforces community connections.
Dodge et al8 reported that 80% of all families assigned to DC consented and began participation, with 86% of the consenting group completing the entire program (net completion = 69%). Of these families, 40% were European American, 37% were African American, and 23% were other or multiracial, with 26% reporting Hispanic ethnicity; 62% received Medicaid or had no health insurance, and 49% were married. Independent observer-rated adherence to the manual was 84%, and interrater agreement on scoring of risk yielded a “good agreement” κ coefficient of .69.
Participants and Evaluation Design
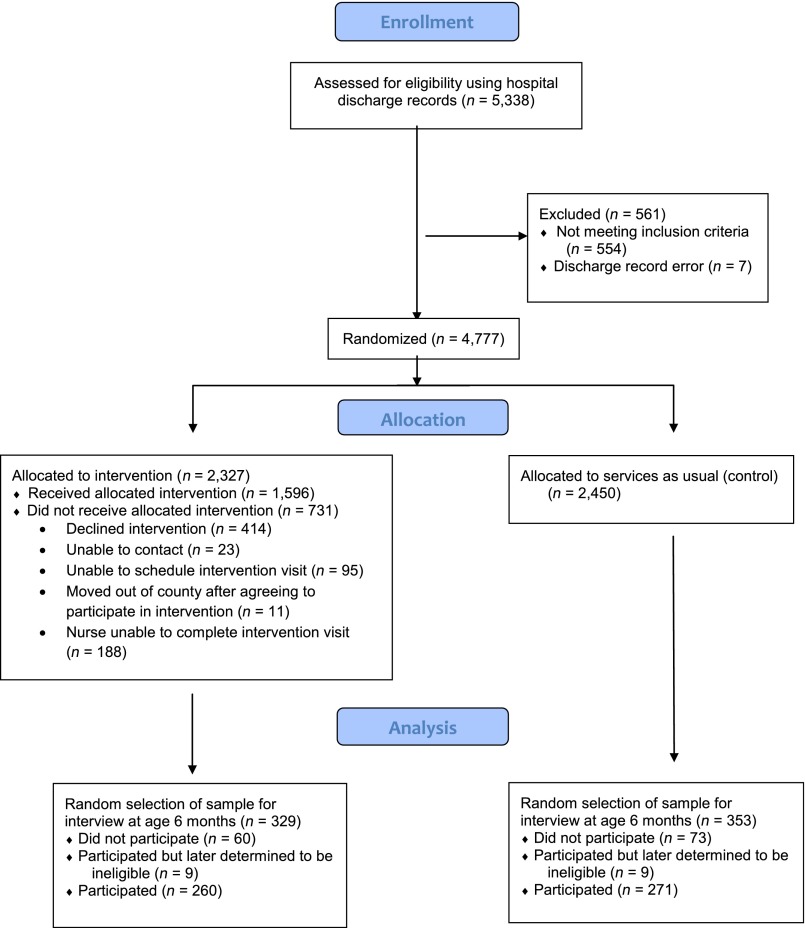
From July 1, 2009 through December 31, 2010, all 4777 residential births in Durham County, North Carolina were randomized according to infant birth date as indicated on hospital discharge records, with even birth dates (n = 2327) assigned to receive DC; odd birth dates (n = 2450) received services as usual and served as a randomized control group (Fig 1). All even birth date families were included in an intent-to-treat evaluation design.
FIGURE 1.
Consolidated Standards of Reporting Trials 2010 flow diagram of Durham Connects RCT implementation.
We selected a random, representative subsample of the 4777 families to evaluate DC impact on outcomes. Selecting a random subsample minimizes evaluation costs and is common for population-level interventions (eg, Moving to Opportunity neighborhood reassignment intervention9) as long as sufficient statistical power is retained. Using birth records, a computer algorithm randomly selected 1 birth for each day spanning the DC RCT enrollment period for participation in the impact study (n = 549 overall; n = 269 DC-eligible families; n = 280 control families). Under guidelines established by Cohen10 and using G*Power software (Heinrich-Heine-Universität, Düsseldorf, Germany),11 statistical power analyses of at least 0.80 power and a significance level of 0.05 indicated that a sample of 549 is sufficiently powered to detect hypothesized effects: an effect size of 0.21 for continuous variables and a 9% difference for dichotomous variables.
Evaluation study families were contacted at infant age 6 months and invited to participate in a research study about infant development. Nonconsenting families were replaced by a randomly selected same-ethnicity, same–birth date family. Families were recruited without consideration for DC recruitment and participation. To prevent participation and response biases, families were blinded to any relation between the study and the community DC program, and in-home interviewers were blinded to family intervention status. In total, 682 families were initially selected, and 549 (80.5%) consented. After completion of study enrollment, 18 families were determined to be ineligible because of hospital discharge record errors (eg, incorrect infant birth date); as a result, the final evaluation sample consisted of 664 families, with 531 (80.0%) consenting and participating.
Measures
Infant Emergency Medical Care
At an age 6-month interview, participants provided written consent to access administrative records from Durham County hospitals. Records were scored through age 12 months for the total number of ED visits since initial hospital discharge and the total number of hospital overnights, excluding overnights for birth-related medical care. These 2 scores were summed to create the primary outcome variable, total infant emergency medical care between birth and age 12 months. Finally, because Dodge et al8 previously reported impact on birth to age 6 months outcomes and we were interested in the preventive impact beyond age 6 months, we also computed total infant emergency medical care between 6 and 12 months of age.
Infant and Family Characteristics
Hospital discharge records provided information on baseline infant and family characteristics, including infant birth risk (scored 1 if any of the following was present and 0 otherwise: birth weight <2500 g, gestational age <37 weeks, or birth complications), health insurance at birth (scored 0 for Medicaid or uninsured and 1 for private insurance), mother race/ethnicity (0 = nonminority, 1 = minority), and infant gender (0 = male, 1 = female). We also examined mother single-parent household status (0 = 2-parent, 1 = single-parent), as reported by mothers at the age 6-month in-home interview.
Analytic Plan
Analyses were conducted by using SAS version 9.3 (SAS Institute, Inc, Cary, NC), with a 2-tailed intent-to-treat design that examined outcomes for all families regardless of intervention status or adherence. Poisson regression models were used because outcome variables were objective counts of child emergency medical care use with skewed distributions.12 Main effect models were estimated first; covariates included infant birth risk, health insurance at birth, mother’s race or ethnicity, single-parent household status, and gender. Next, moderation analyses tested whether DC intervention effects differed based on infant and family characteristics. Moderators were examined individually for each outcome; tests for significant interactions were examined, as in the work of Aiken and West.13 Intervention effect sizes for all models were calculated as (mean intervention [MI] − mean control [MC])/Average SD.
Results
Pretreatment Group Comparisons
To determine the representativeness of the evaluation subsample, we compared the 664 selected families (and, separately, the 531 participating families) with the population of birthing families on 10 preintervention variables available from hospital discharge records (Table 1). The 685 families differed significantly (P < .05) from the population on only 1 variable, infant gender (selected families were more likely to have female infants). Similarly, comparisons of the 531 participating families to the population identified only 1 significant difference (participating families were more likely to be Medicaid insured or uninsured).
TABLE 1.
Preintervention Sample Characteristics for Population and Selected Evaluation Subsample Groups
| Variable | RCT Population Versus Selected and Interviewed Evaluation Subsamples | Interviewed Intervention Versus Control Evaluation Subsamples | |||
|---|---|---|---|---|---|
| RCT Population (n = 4777) | Selected Evaluation Subsample (n = 664) | Participating Evaluation Subsample (n = 531) | Participating Intervention Subsample (n = 260) | Participating Control Subsample (n = 271) | |
| % Participation of selected | 80.0 | 81.3 | 78.8 | ||
| Infant birth risk | |||||
| % Low birth wt | 10.0 | 9.1 | 8.9 | 7.8 | 10.0 |
| % Gestation <37 wk | 8.2 | 6.7 | 6.3 | 4.7 | 7.8 |
| % Any birth complications | 7.4 | 5.8 | 6.1 | 3.9 | 8.1* |
| % Medicaid or no insurance | 60.8 | 63.1 | 65.5* | 63.3 | 67.5 |
| Mother’s age (mean, y) | 28.5 | 28.5 | 28.3 | 28.2 | 28.4 |
| Mother’s race or ethnicity | |||||
| %White, non-Hispanic | 29.7 | 29.2 | 26.6 | 28.5 | 24.7 |
| % Black | 36.7 | 38.0 | 39.4 | 36.5 | 42.1 |
| % Hispanic | 22.6 | 23.2 | 24.7 | 25.0 | 24.4 |
| % Other | 11.1 | 9.6 | 9.4 | 10.0 | 9.9 |
| % Infant female | 49.8 | 54.7** | 53.5 | 50.8 | 56.1 |
Column 2 is contrasted with column 1; column 3 is contrasted with column 1; column 5 is contrasted with column 4. *P < .05; **P < .01.
Next, we tested for bias between intervention and control families. Participation rates did not differ significantly between intervention (81%) and control (79%) families. We tested whether intervention (n = 260) and control (n = 271) groups differed on the 10 variables noted earlier plus single-parent household status and found only 1 significant difference (control condition had more infants with birth complications). Because the number of significant differences was small, we concluded that the evaluation sample was representative of the broader population and that participation was not biased between intervention and control groups. Nonetheless, gender, insurance, and birth complications were covaried in all analyses.
Impacts on Infant Emergency Medical Care
Between birth and age 12 months, families randomly assigned to DC had 50% less total infant emergency medical care than control families (MC = 1.57, MI = 0.78; P < .001, effect size = 0.28). Dodge et al8 reported 59% less emergency care between birth and 6 months of age. Current analyses indicate an additional impact on total emergency medical care between 6 and 12 months of age, with intervention families having 31% less care during this period (MC = 0.52, MI = 0.36; P < .03, effect size = 0.14).
Tests of components of birth to 12-month emergency medical care revealed that DC families had 85% fewer hospital overnights than controls (MC = 0.74, MI = 0.11; P < .001, effect size = 0.27) and 18% fewer ED visits, although this latter difference was not statistically significant (MC = 0.83, MI = 0.68; P = .223).
Impacts Across Family Subgroups
Differential impacts across types of families were tested by interaction effects between intervention and each moderator in a model that included all covariates and main effects (Tables 2 and 3). Follow-up tests of intervention effects separately for each group revealed that intervention had a significant impact on total emergency medical care for every subgroup. Significant interaction effects indicated a larger impact for 1 group and a smaller but still significant impact for the other (Table 4).
TABLE 2.
RR Estimates for Impact of Random Assignment to DC on Birth to 12-Month and 6- to 12-Month Infant Total EMC: Main Effects and Moderating Effects (n = 531)
| Variable | Birth to 12-Month Total EMC | 6- to 12-Month Total EMC | ||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| Any infant birth risk (1 = yes) | 2.97*** | 2.51–3.52 | 1.26 | 0.89–1.78 |
| Medicaid or no insurance at birth (1 = yes) | 1.99*** | 1.56–2.54 | 2.87*** | 1.88–4.40 |
| Mother minority status (1 = yes) | 0.86 | 0.68–1.09 | 0.75 | 0.51–1.11 |
| Mother single-parent status (1 = yes) | 1.69*** | 1.42–2.01 | 1.39* | 1.05–1.83 |
| Infant gender (1 = girl) | 0.52*** | 0.44–0.61 | 1.10 | 0.85–1.42 |
| Treatment (1 = DC eligible) | 0.55*** | 0.46–0.65 | 0.74* | 0.57–0.96 |
| Treatment × infant birth risk | 0.56*** | 0.37–0.84 | 0.72 | 0.32–1.59 |
| Treatment × Medicaid or no insurance | 2.26*** | 1.40–3.65 | 4.72*** | 1.88–11.88 |
| Treatment × minority status | 2.90*** | 1.78–4.75 | 4.21*** | 1.92–9.23 |
| Treatment × single-parent status | 1.24 | 0.88–1.74 | 1.89* | 1.11–3.22 |
| Treatment × infant gender | 1.53* | 1.09–2.17 | 0.67 | 0.40–1.15 |
All interaction terms were examined individually. CI, confidence interval; EMC, emergency medical care; RR, risk ratio. *P < .05; ***P < .001.
TABLE 3.
RR Estimates for Impact of Random Assignment to DC on Birth to 12-Month Infant ED Visits and Hospital Overnights: Main Effects and Moderating Effects (n = 531).
| Variable | Birth to 12-Month ED Visits | Birth to 12-Month Hospital Overnights | ||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| Any infant birth risk (1 = yes) | 1.30† | 0.99–1.69 | 9.98*** | 7.60–13.10 |
| Medicaid or no insurance at birth (1 = yes) | 4.05*** | 2.75–5.96 | 0.65* | 0.46–0.91 |
| Mother minority status (1 = yes) | 1.10 | 0.78–1.55 | 0.64** | 0.46–0.89 |
| Mother single-parent status (1 = yes) | 1.58*** | 1.28–1.95 | 2.18*** | 1.61–2.96 |
| Infant gender (1 = girl) | 0.78* | 0.64–0.95 | 0.21*** | 0.16–0.29 |
| Treatment (1 = DC eligible) | 0.88 | 0.72–1.08 | 0.15*** | 0.10–0.22 |
| Treatment × infant birth risk | 1.01 | 0.58–1.78 | 1.04 | 0.46–2.32 |
| Treatment × Medicaid or no insurance | 1.52 | 0.75–3.07 | 1.11 | 0.49–2.51 |
| Treatment × minority status | 1.92* | 1.02–3.60 | 2.02 | 0.78–5.24 |
| Treatment × single-parent status | 1.45† | 0.96–2.17 | 0.36* | 0.15–0.88 |
| Treatment × infant gender | 1.22 | 0.82–1.82 | 3.55** | 1.55–8.14 |
All interaction terms were examined individually. CI, confidence interval; RR, risk ratio. †P < .10; *P < .05; **P < .01; ***P < .001.
TABLE 4.
RR Estimates for Impact of Random Assignment to DC on Infant EMC, ED Visits, and Hospital Overnights: Post Hoc Tests of Moderation (n = 531).
| Variable | Birth to 12-Month Total EMC | 6- to 12-Month Total EMC | Birth to 12-Month ED Visits | Birth to 12-Month Hospital Overnights | ||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Treatment × birth risk | ||||||||
| No birth risks | 0.63*** | 0.52–0.77 | — | — | — | — | — | — |
| 1 or more birth risks | 0.23*** | 0.15–0.33 | — | — | — | — | — | — |
| Treatment × Medicaid or no insurance | ||||||||
| Private health insurance | 0.23*** | 0.15–0.36 | 0.20*** | 0.08–0.49 | — | — | — | — |
| Medicaid or no insurance | 0.61*** | 0.51–0.73 | 0.91 | 0.69–1.21 | — | — | — | — |
| Treatment × minority status | ||||||||
| Nonminority | 0.23*** | 0.14–0.36 | 0.23*** | 0.11–0.47 | 0.46* | 0.25–0.84 | — | — |
| Minority | 0.65*** | 0.55–0.79 | 0.96 | 0.72–1.28 | 0.96 | 0.78–1.18 | — | — |
| Treatment × single-parent status | ||||||||
| 2-parent family | — | — | 0.51** | 0.34–0.77 | — | — | 0.22*** | 0.14–0.36 |
| Single-parent family | — | — | 0.97 | 0.68–1.39 | — | — | 0.07*** | 0.03–0.14 |
| Treatment × infant gender | ||||||||
| Boys | 0.48*** | 0.38–0.59 | — | — | — | — | 0.10*** | 0.06–0.17 |
| Girls | 0.63*** | 0.48–0.82 | — | — | — | — | 0.30*** | 0.16–0.58 |
Dashes indicate moderator was not a significant overall predictor of outcome. CI, confidence interval; EMC, emergency medical care; RR, risk ratio. *P < .05; **P < .01; ***P < .001.
12-Month Total Emergency Care Outcomes
A significant interaction effect (P < .001) indicated that the observed effect size was larger for infants with 1 or more birth risks (MC = 3.64, MI = 1.13; P < .001, effect size = 0.51) but still significant for infants with no birth risks (MC = 1.11, MI = 0.71; P < .001, effect size = 0.19).
The interaction effect was significant for family health insurance (P < .001), with larger effects for families with Medicaid or no insurance (MC = 1.83, MI = 1.05; P < .001, effect size = 0.27) but still significant for privately insured families (MC = 0.84, MI = 0.30; P < .001, effect size = 0.22).
For family minority status, the interaction effect was significant (P < .001), and intervention impact was significant for both minority (MC = 1.60, MI = 0.96; P < .001, effect size = 0.23) and nonminority (MC = 1.36, MI = 0.35; P < .001, effect size = 0.36) families, with larger effects for nonminorities.
The interaction effect with gender indicated that intervention had a larger positive impact on boys (MC = 2.15, MI = 0.94; P < .001, effect size = 0.34) but still a positive impact on girls (MC = 1.05, MI = 0.61; P < .001, effect size = 0.23).
12-Month Hospital Overnights
Program impact on 12-month hospital overnights was significant for all subgroups but larger for single-parent families (MC = 0.99, MI = 0.07; P < .001, effect size = 0.34) than 2-parent families (MC = 0.53, MI = 0.13; P < .001, effect size = 0.22), and larger for boys (MC = 1.27, MC = 0.13; P < .001, effect size = 0.37) than girls (MC = 0.29, MI = 0.10; P < .001, effect size = 0.14).
12-Month ED Visits
Interaction effects indicated that program impact on the number of ED visits was significant for nonminority families (MC = 0.43, MI = 0.25; P < .02, effect size = 0.18) and in the same direction but not significant for minority families (MC = 0.93, MI = 0.84; P = .69).
6- to 12-Month Emergency Medical Care
For the limited period between 6 and 12 months of age, significant program impact on total emergency care was found for families with private health insurance (MC = 0.32, MI = 0.09; P < .001, effect size = 0.18), but it had become nonsignificant, although in the same direction, for families with Medicaid or no insurance (MC = 0.58, MI = 0.51; P = .526). Similarly, program impact was found for nonminority families (MC = 0.52, MI = 0.14; P < .001, effect size = 0.24) and in the same direction but nonsignificant for minority families (MC = 0.50, MI = 0.44; P = .78). Program impact was significant for 2-parent families (MC = 0.43, MI = 0.23; P < .002, effect size = 0.17) and in the same direction but nonsignificant for single-parent families (MC = 0.61, MI = 0.57; P = .874).
Discussion
We find that random assignment to the DC program leads to a 50% reduction in overall emergency medical care across the first 12 months of life, and this impact holds across all groups of families studied, including those with and without medical risk at birth, uninsured and insured families, ethnic minority and majority families, single-parent and 2-parent families, and families with boys and girls. Dodge et al8 showed impact of DC on reductions in emergency medical care during the first 6 months of life, including 3 to 12 weeks after birth, when intervention was ongoing. The current study shows that a preventive impact occurs during the second 6 months of life, well after the nurse home visitor had ceased all ongoing family contact. The program’s modest $700 cost per family is more than offset by savings in hospital medical care costs before the infant’s first birthday, thus making this program a worthy economic investment for a community.
The most likely mechanism through which this preventive impact occurs is through the nurse home visitor’s success in identifying individual family needs, intervening briefly to address those needs when risk was moderate, and connecting the family with targeted community resources to meet those needs for families having higher risk. In other scaling-up studies for which no positive impact was found, it might well have been that a community’s stock of resources had been depleted before all families could be served. For the current implementation, the DC program worked at the community level to align resources to serve all families with a newborn infant. Future studies will test mechanisms more directly.
Even though the DC program had a positive impact on all groups of families, some types of families experienced greater impact than others. Families with an infant born at medical risk due to low birth weight, birth complications, or early gestational age benefited more than did lower-risk families. Nurses worked to help high-risk families identify relevant community resources and become comfortable using primary pediatric care instead of emergency services. Future home visiting programs might focus on this group; however, the universal delivery of initial visits might be crucial to community support and high penetration.
Families with Medicaid or no insurance benefited more overall than did families with private insurance. However, the benefit for Medicaid families occurred primarily during the first 6 months of life, near the time when the DC nurse was in contact with families. After the intervention ended, impact on Medicaid families waned, but impact on privately insured families continued. This finding has 2 important implications for home visiting policies. First, home visiting might yield even stronger impact on Medicaid families if the program continues over time. Second, this study is the first ever to report significant savings on medical care costs for privately insured families who receive home visiting, suggesting that families and private health care insurers would benefit from adding home visiting to covered health care.
Conclusions
A brief, inexpensive postnatal nurse home visiting program can reduce hospital and emergency medical care across the first 12 months of life. This preventive impact holds for all groups of families studied, including both privately insured and Medicaid or uninsured families, suggesting the benefits of providing short-term postnatal nurse home visiting universally in a community. This program complements more intensive home visiting models by serving as a screening and triage tool that ensures optimal matching of families with long-term services only as needed. We believe that it merits support from the Maternal, Infant, and Early Childhood Home Visiting Program directly and that it will provide more efficient allocation of these funds to other programs.
Acknowledgments
The authors acknowledge the support of many Durham community leaders, program nurses, and staff members who collaborated in program implementation.
Glossary
- DC
Durham Connects
- ED
emergency department
- M
mean
- RCT
randomized controlled trial
Footnotes
Kenneth A. Dodge participated in the funding, conceptualization, design, administration, data interpretation, and manuscript drafting; W. Benjamin Goodman participated in the data collection, analysis, interpretation, administration, and manuscript drafting and is responsible for the integrity of the data and the accuracy of the data analysis; Robert A. Murphy participated in the conceptualization, design, interpretation, and manuscript revision; Karen O’Donnell participated in the conceptualization, design, clinical supervision, interpretation, and manuscript revision; Jeannine Sato participated in the program supervision and manuscript revision; and all authors approved the final manuscript as submitted.
This trial has been registered as the Durham Connects Evaluation with ClinicalTrials.gov (http://www.clinicaltrials.gov) (identifier NCT01406184).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funding was provided by The Duke Endowment and the Pew Center on the States. The views expressed are those of the author(s) and do not necessarily reflect the views of The Duke Endowment, the Pew Center on the States, or The Pew Charitable Trusts. The authors acknowledge support by NIH Grants K05DA15226, P30DA023026, and HD069981. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Patient Protection and Affordable Care Act, Pub L No. 111-148, HR 3590, 111th Cong. (2009–2010)
- 2.Olds DL, Henderson CR, Jr, Chamberlin R, Tatelbaum RT. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78(1):65–78 [PubMed] [Google Scholar]
- 3.Kitzman H, Olds DL, Henderson CR, Jr, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA. 1997;278(8):644–652 [PubMed] [Google Scholar]
- 4.Welsh BC, Sullivan CJ, Olds DL. When early crime prevention goes to scale: a new look at the evidence. Prev Sci. 2010;11(2):115–125 [DOI] [PubMed] [Google Scholar]
- 5.Daro D, McCurdy K, Falconnier L, Stojanovic D. Sustaining new parents in home visitation services: key participant and program factors. Child Abuse Negl. 2003;27(10):1101–1125 [DOI] [PubMed] [Google Scholar]
- 6.Daro D, Dodge KA. Creating community responsibility for child protection: possibilities and challenges. Future Child. 2009;19(2):67–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matone M, O’Reilly AL, Luan X, Localio AR, Rubin DM. Emergency department visits and hospitalizations for injuries among infants and children following statewide implementation of a home visitation model. Matern Child Health J. 2012;16(9):1754–1761 [DOI] [PubMed] [Google Scholar]
- 8.Dodge KA, Goodman WB, Murphy RA, O’Donnell K, Sato J, Guptill S. Implementation and randomized controlled trial evaluation of universal postnatal nurse home-visiting. Am J Public Health. 2014. In press. [DOI] [PMC free article] [PubMed]
- 9.Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes: a randomized social experiment. N Engl J Med. 2011;365(16):1509–1519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen J. Statistical Power for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988 [Google Scholar]
- 11.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160 [DOI] [PubMed] [Google Scholar]
- 12.Coxe S, West SG, Aiken LS. The analysis of count data: a gentle introduction to Poisson regression and its alternatives. J Pers Assess. 2009;91(2):121–136 [DOI] [PubMed] [Google Scholar]
- 13.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991 [Google Scholar]