Abstract
Background
The assessment of needs for cancer care is a critical step in providing high quality care and achieving cancer patients' and families' satisfaction. Instruments can be used to assess needs and guide cancer care planning. This study discusses the importance of the needs assessment, relationships between needs, satisfaction and quality of life; and reviews the assessment instruments of needs experienced by cancer patients and their families.
Methods
A systematic search was conducted in MEDLINE and CANCERLIT data bases. Instruments were evaluated based on their conceptual and measurement models as well as their demonstrated reliability and validity. The authors also sought information pertaining to instruments' burden of administration and responsiveness. Measures compromised by a lack of published psychometric description were not included.
Results
This search identified 17 patient needs assessment instruments and seven family needs assessment instruments. The development and psychometric proprieties of most of these instruments were well documented. However, data on their responsiveness and burden of administration were scarce.
Conclusions
Each selected instrument meets some but not all of our criteria for validity, reliability, responsiveness and burden. It is questionable whether any instrument can be developed meeting all the requirements. However, there is still a need to continue researching and developing needs assessment instruments leading to effective intervention and improving quality of cancer care.
Review
Introduction
Health care, including cancer care, is in the midst of a revolution driven by strong forces of cost containment and competition.[1] While economic pressures may be new to health care in general and cancer care in particular, they are common in highly competitive industries where price reductions regularly occur simultaneously with performance improvements. Cancer care providers will be expected to both improve performance and reduce costs; not as a one-time event but as a way of life. However, these improvements are unlikely to occur without a much better understanding of patient and family needs and the factors that influence them. Once those needs are fully understood, interventions can be designed that will improve adherence and reduce waste and rework.
These pressures to contain costs occur at the same time that consumers are taking a more active role in their care.[2] Such trends are manifested in the growth of not only alternative and complimentary care, but also in the growth of e-health. Cancer patients and their families are searching for alternatives, in part because the health field does not fully understand and respond to their needs. The experience of patients with advanced cancer, and of their families, illustrate the implications of not designing delivery systems around a clear understanding of patient and family needs.
In Approaching Death, the Institute of Medicine[3] identified key patient needs such as fears of abandonment and protracted death, and need for reliable, respectful care and advance care planning that promotes "norms of decency." Yet too many people suffer unnecessary pain and distress and there are major impediments to good end of life care.[4,5] In fact, a large study[6] of seriously ill hospitalized patients documented substantial shortcomings in communication, treatment, and characteristics of death. The Institute of Medicine report also identified the lack of scientific knowledge and data on patient and family needs, especially the paucity of longitudinal data [3]. Inadequate understanding of needs among diverse populations has also been identified as a major problem[3].
Needs assessments are required to guide care planning, in part because many caregivers and patients do not communicate concerns to their clinicians.[7-11] When they do share needs, they often omit important psychosocial concerns.[12,13] Several factors contribute to this breakdown. Many patients and caregivers believe that pain, grief, anger, and suffering are inevitable with cancer. Others believe that clinicians do not want to address such issues, as evidenced by the absence of clinician inquiry or concern required to develop a meaningful dialog [14-19]. As a result of inadequate understanding of patient and family needs, both healthcare costs and unnecessary suffering increase.[20-22] Substantial evidence points especially to the damaging effects of inadequately meeting information and support needs [19,23-25]. For instance, if clinicians are unaware that a caregiver feels unprepared to clean and drug a patient's wound, then adequate training may not be provided; infections may then develop that increase suffering and costs. The research conducted so far also fails to describe how patient and caregiver information and support needs change with key events such as learning that treatment is no longer working [26-29].
Many obstacles exist to assessing patient or caregiver needs including: lack of clarity on best practices in initially identifying needs; determining possible levels of performance on each need; measuring the importance of needs and employing needs assessment data in design; and improvement and evaluation efforts. We will first examine how needs assessment relates to satisfaction and quality of life, and point out the complex relationships among needs themselves. Next we will review existing cancer needs assessments and comment on their strengths and weaknesses. Then we will make recommendations for future research in this field. Because we believe cancer is a family disease with ramifications far beyond the patient, we propose that needs assessment should focus on both patients and family caregivers. We will examine needs assessment instruments that address both patients and families.
Relationships among and between needs, satisfaction and quality of life
In developing needs assessments, it is important to understand how needs relate to each other, as well as how those interrelationships affect satisfaction and quality of life. This section will examine those relationships and how they are influenced by various applications such as programs to improve cancer care.
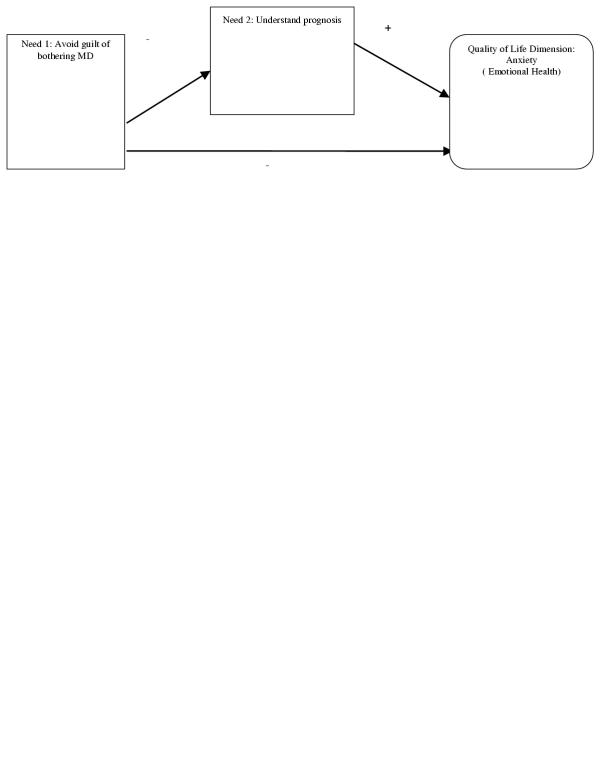
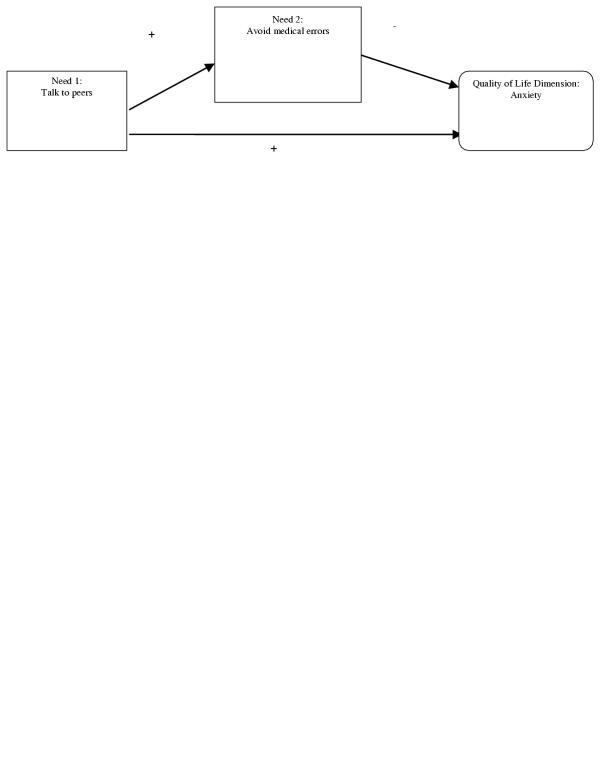
Some needs are more proximally related to quality of life (or satisfaction) than others. Figure 1 portrays one such relationship. Here, a patient's need to understand prognosis may raise anxiety (a key aspect of emotional health status), thus having a direct effect on quality of life. Another need, that of avoiding the guilt of bothering a busy MD, may have a small but direct effect on quality of life, because the guilt may raise anxiety. However, that need to avoid guilt may have a much stronger influence on the ability to meet a more proximal need (the ability to obtain a clear understanding of prognosis). The end result is that not bothering the MD (in order to avoid guilt), despite the need to understand one's prognosis, may further raise patient anxiety and substantially impact quality of life.
Figure 1.
Possible proximal relationship between needs and quality of life
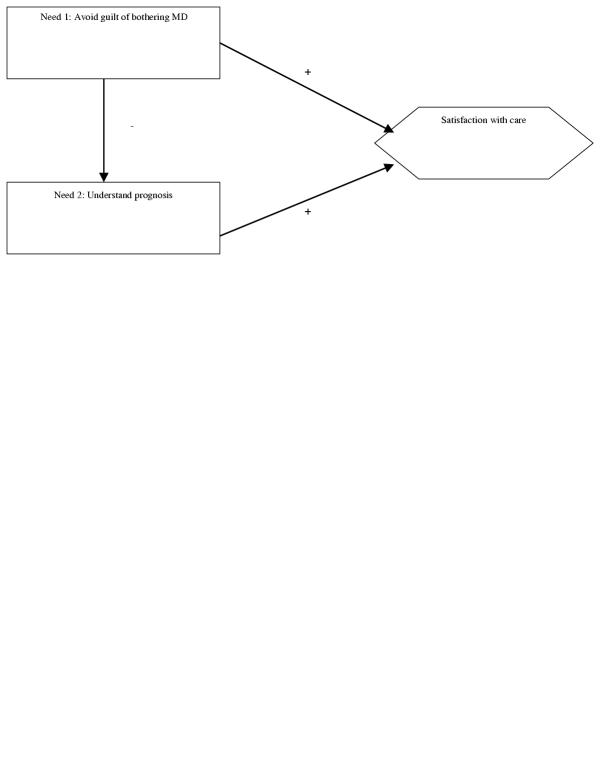
The relationship between two needs (e.g. avoiding guilt and understanding prognosis) may be different when it comes to satisfaction. Both of the needs shown in Figure 1 (if not met) work to reduce quality of life, but one may offset the other when it comes to satisfaction. Figure 2 provides an example where lack of a clear understanding of prognosis could reduce satisfaction with care. But the guilt associated with bothering a busy MD may counteract that dissatisfaction with care, if patients put the blame on themselves (rather than on the MD) for being poorly informed. Furthermore, the direct effect of guilt on satisfaction may be stronger than the indirect effect, whereas the indirect effect may be stronger in relationship to quality of life.
Figure 2.
Possible relationship between needs and satisfaction
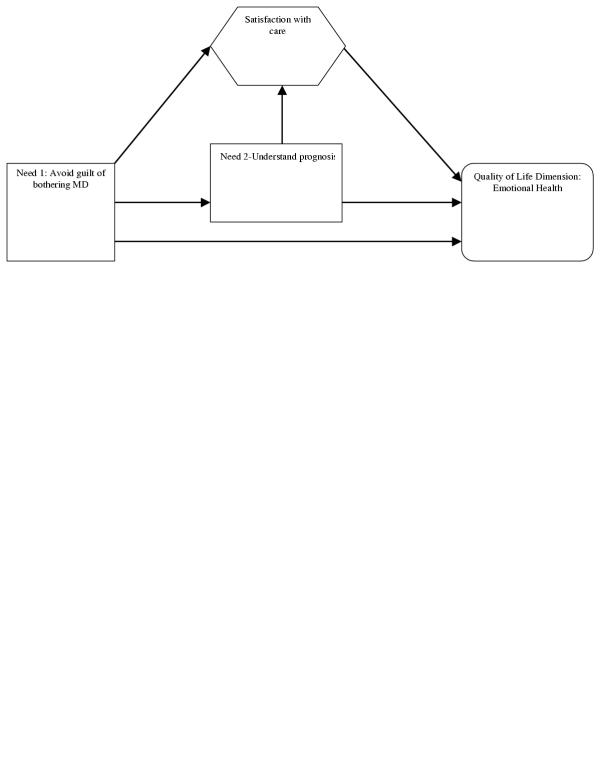
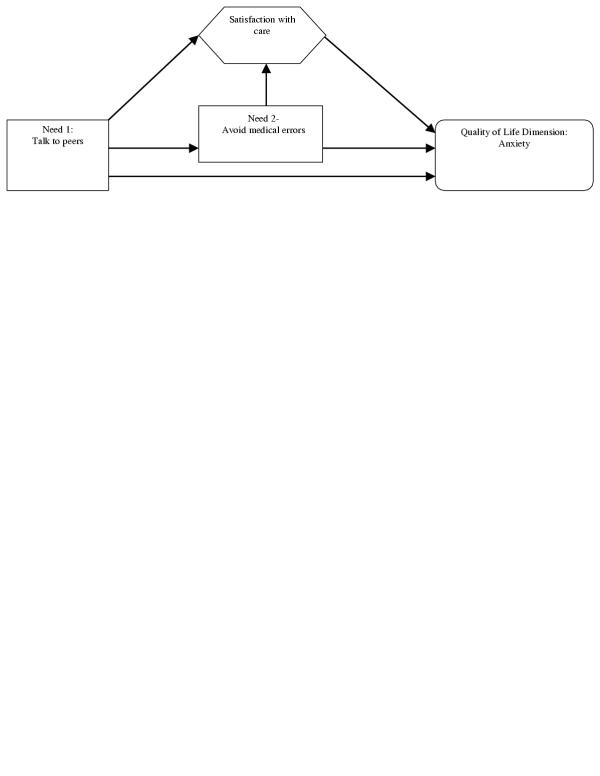
Putting these relationships together (as shown in Figure 3) leads to a more complex model than the one initially proposed, but one that offers much more insight into how to best intervene to improve quality of life. Depending on the proximity and the strength of these relationships, one might conclude that obtaining an honest and understandable prognosis is more important to improving quality of life than bothering an physician. If a means other than interaction with physician were available (possibly through selective use of information technology), one would not need to worry about training patients in the appropriateness and methods of assertiveness in order to feel less guilt.
Figure 3.
Possible relationship between needs, satisfaction and quality of life
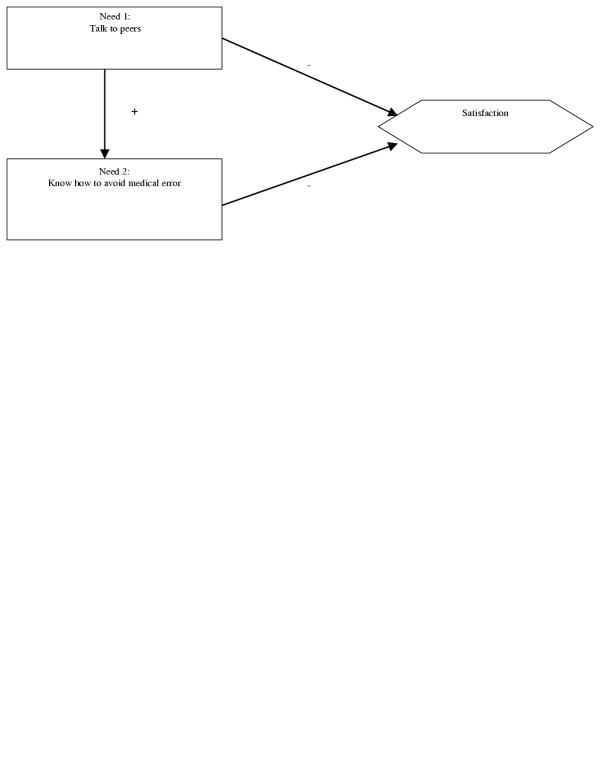
Another example is the relationship between the need to talk to patients who have already completed treatment, the need to avoid medication errors such as infections, and the relationship between those needs and the quality of life dimension of functional well-being. Talking to peers may elicit information on how to avoid medication errors, as well as provide a small calming effect. However, knowing how to avoid errors may increase anxiety.
When it comes to satisfaction with care, a different relationship might exist. We know that informed patients tend to have high expectations and thus may be less satisfied with care. Hence talking to peers and knowing how to avoid medical error may both have a negative effect on satisfaction as Figure 5 would suggest.
Figure 5.
Relationship with satisfaction
Figure 4.
Possible relationship between needs and quality of life
And putting these two relationships together leads to a much better understanding of quality of life. If a way to help patients avoid medical errors will be provided, the discussion with patients might even further lessen anxiety.
This suggests that measuring the importance of needs may require: (1) measuring both the direct importance to quality of life (or satisfaction), as well as (2) the importance of one need in meeting another need. And one cannot estimate the importance of these second order effects without understanding the relationships exemplified in Figure 3, a task the authors have never seen carried out in a needs assessment.
Thus the relationships between needs, as well as among needs and satisfaction and quality of life, should be better understood if we hope to improve care and quality of life. This understanding is important for designing and conducting needs assessments. If a needs assessment prioritizes which needs should be addressed, and if that assessment is done without recognizing relationships among needs, the results can be used in potentially damaging ways. For example, a program that might be established to connect patients could increase a patient's perceived need to prevent medical errors, and thus increase anxiety, unless an initiative to prevent medical errors is also put in place. Hence, these unintended consequences should be considered. Simple mechanisms can be developed to ensure that these relationships are identified. For instance, one might place the needs on 3 × 5 cards, and sort the cards so that cards are placed together if meeting one need will have a great effect (positive or negative) on meeting another. If such a relationship is formed, one might flag analysis such that if one need is addressed, the effect on another need should be considered.
Methods
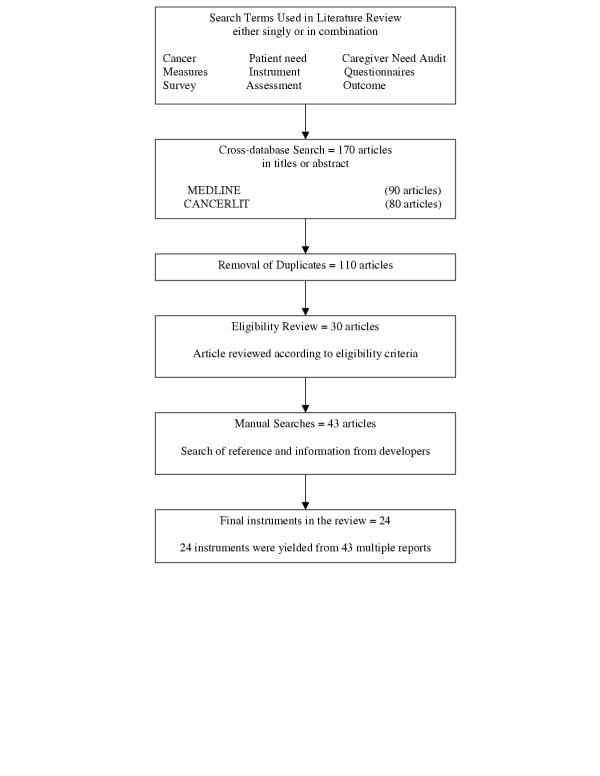
A systematic search was conducted in MEDLINE (1966–Aug2002) and CANCERLIT(1975–Aug2002) to identify needs assessment instruments used to guide cancer care program design and intervention research. The search terms used, either singly or in combination, were 'cancer', 'patient need', 'caregiver need', 'audit measures', 'instrument', 'questionnaires', 'survey', 'assessment' and 'outcome' that appear in the title/abstract. The articles from these searches were further selected using the following inclusion criteria: empirical studies; studies with cancer in adult patients; studies about patients/caregivers experienced needs/problems for care.
The search produced 170 articles. Manual searches of the bibliographies of searched articles and reviews in the field were also conducted. Each instrument's developer was also contacted to verify the psychometric evaluation information we found in the literature. Excluded from our analyses were instruments that : 1) did not document how they were developed or tested,[30,31] 2) did not measure importance or satisfaction[32] and 3) did measure satisfaction with specific health providers[33,34]. We included both instruments that studied satisfaction of a broad set of needs derived from a health status perspective, and instruments that studied one class of needs only, e.g., needs for information or for one type of cancer. Figure 7 illustrates our selection process.
Figure 7.
Search and selection process
A total of 24 instruments were selected with 43 articles which present the relevant information for evaluation. The final instruments included in the study were the Cancer Rehabilitation Evaluation System (CARES);[35-38] the Cancer Rehabilitation Evaluation System-Short form (CARES-SF)[39]; the Cancer Patient Need Survey (CPNS)[40,41]; the Cancer Patient Need Questionnaire (CPNQ)[42,43]; the Supportive Care Need Survey (SCNS)[44]; the Home Care Study-Patient Form (HCS-PF)[45]; the Needs Evaluation Questionnaire (NEQ)[46]; the Patient Needs Assessment Tool (PNAT)[47]; the Derdiarian Informational Needs Assessment (DINA)[48]; the Patient Informational Needs Questionnaire (PINQ)[49]; the Prostate Cancer Needs Assessment (PCNA)[50]; the Psychosocial Needs Inventory (PNI)[51]; the Toronto Informational Needs Questionnaire-Breast Cancer (TINQ-BC)[52,53]; the Information Needs Measure (INM)[54]; the Support Team Assessment Schedule (STAS)[55-58]; Palliative Care Assessment (PACA)[59]; the Needs Near The End-of-Life Care Screening Tool (NEST)[60,61]; the Family Inventory of Need (FIN)[62]; the Family Inventory of Need-Husband (FIN-H)[63,64]; the FAMCARE scale[65]; the Home Caregiver Need Survey (HCNS)[40,66-68]; the Home Care Study-Caretaker Form (HCS-SF)[45]; the Need Satisfaction Scale (NSS) [69]and the Information and Support Needs Questionnaire (ISNQ)[70,71].
Psychometric evaluation criteria
We described each instrument in terms of the following criteria.
Purpose and administration
We identified the instrument's original intended use(s) and application and the administration method, either self-reported or professionally-interviewed.
Items and domains
Numbers of items and domain structure of the instrument were reported.
Question format
The instrument's response format was reported.
Conceptual and measurement model
A search was conducted for the theoretical framework for the concepts the instrument is intended to measure and the relationship between those concepts. Information on conceptual and empirical support of scale structure, distinctiveness of multiple scales, and variability of the scale were obtained.
Validity
Content validity
Content validity was evaluated by investigating methods used to develop the instrument content and the empirical validation of the instrument in order to establish the appropriateness of instrument's intended use.
Construct calidity
Construct validity was studied to support the proposed interpretation of scores on the instrument based on theoretical implications associated with the constructs.
Reliability
Internal consistency
Internal consistency was examined to understand whether the items correlate with each other within the instrument. The estimates should be reported on both the total score and subscale scores when it is appropriate.
Reproducibility
Test-retest reproducibility
Test-retest reproducibility of the self-administered instrument was studied to assess whether the instrument produces stable scores over time. The time interval between administrations and the rationale that changes should be minimal were also searched.
Inter-rater reproducibility
For professionally-reported instruments, inter-rater reproducibility was searched to assess whether the instrument produces similar results across different interviewers.
Responsiveness
The instrument's ability to detect change was assessed. Longitudinal data was particularly searched.
Burden
Respondent burden
We looked for average time required to complete the instrument and assumed reading level. We also paid attention on the degree of missing data; the refusal rates and the refusal reasons.
Administrative burden
For professionally-administered instruments, we searched for the average time required and level of training needed for an interviewer to administer the instrument.
Results
Table 1 [see Additional file: 1] summaries the evaluation of these selected instruments.
Conceptual and measurement model
Seven instruments were developed with conceptual models. The dimensions of five instruments were examined by factor analysis. However, the instruments, which have both conceptual model definition and measurement evaluation, are the FIN and the NEST. The measurement invariance of the NEST was indicated by the multi-sample confirmatory factor analysis across socio-demographic strata. Furthermore, the uni-dimensionality of the NEST-SF was evaluated by the partial credit model, an approach in the Item Response Theory (IRT). It was the only instrument in our review using this relatively new measurement technique.
Validity
A wide variety of approaches were taken to examine instrument validity. The following paragraphs describe the various methods.
Content validity
In most case, panels of professionals were used to derive or review items. Literature review was most commonly used to generate instrument content (14 instruments). Eleven instruments used qualitative analysis of statements by patients/caregivers to generate items. The PCNA is an example of using such procedures. Other instruments selecting items from existing instruments were also observed (three instruments). Pre-testing of the items was conducted for eight instruments.
Construct validity
In our review, construct validity was mostly assessed by the relationship between the instrument under development and a measure of another concept to which it is supposedly theoretically related (12 out of 24). In general, good construct validity was shown. Another four instruments were examined for their discriminant validity, and one with poor discriminant validity was found.
Reliability
Internal consistency
The internal consistency of 20 out of 24 instruments in our review was assessed by the Cronbach alpha. The criterion level for coefficient alpha with a new scale has been suggested to be at about .70 or above[72]. Sixteen instruments had shown good internal consistency ranging from 0.7 to 0.95, except for some of the subscales.
Reproducibility
Test-Retest reproducibility
Nine of 24 instruments examined stability over time using an appropriate time interval between tests. The test-retest agreement of CARE, CARE-SF and DINA achieved above 80%. Good intercorrelation was indicated for CPNQ, NEQ, PCNA, PCNA, FAMCARE and FIN-H.
Inter-rater reproducibility
We examined only three professionally-administered instruments: the PNAT, STAS and PACA. Each of these three instruments demonstrated internal agreement between different raters. The domain inter-rater reliability of the PNAT ranges from 0.73–0.87 by Friedman test. The inter-rater agreement of the STAT also achieved .9 for each domain except predictability. The 0.4 and above Kappa estimates for the PACA domains also indicated a good inter-rater reproducibility.
Responsiveness
Instrument responsiveness was not commonly evaluated in our review. CARES-SF detected patients' change over time. The responsiveness of the DINA was examined by comparing a control group and experimental group. Both STAS and PACA were able to detect the intervention effects. The PINQ and the HCNS were able to detect expected changes in needs of patients and caregivers over time.
Burden
Respondent burden
The average completion time needed was reported for 16 instruments in our review, ranging from a few minutes to 43 minutes. The reading level was examined only for the CPNQ, the SCNS and the PCNA. Non-completion rate of those reported ranged from 11%–35%. Several investigators further explored the reasons and the pattern of non-completion. For example, the investigators of the PINQ found that some of the refusal reasons are "not wanting to be reminded of their illness, feel too old", etc. The investigators of the PNI revealed that men were less likely to participate in the research.
Administrative burden
Out of the three professionally-administered instruments included in our review, the PNAT is the only instrument which had demonstrated its low training requirement for professionals to complete in an experimental design study.
Discussion
In our review for cancer needs assessment instruments, 17 questionnaires were found for patients' needs and seven questionnaires were found for their families. Most instruments employ a self-reported format. Self-administered questionnaires are relatively inexpensive and require much less time than interviews.[73] Advocates for interviews or semi-structured interviews by professionals argued that such approaches might be employed in a clinical setting and reduce missing data. Future research might help us understand the circumstances under which specific administration formats should be used.
There is great variation in domains and numbers of item across instruments. Domains developed by different researchers often have very different organizing structures. Most of the instruments have their items distributed over several domains and similar domain names were found across instruments. Table 2 [see Additional file: 1] lists different domain names found in the review, with corresponding numbers of items in the instruments. However, domains with similar names sometimes contain items that are conceptually and operationally quite different. This may be due to different viewpoints from which the instruments were developed. However, the field would benefit if a common set of domain terms could be adopted to form the core of the needs assessments, and if items could be placed uniformly within domains.
The Likert-type scale is widely applied in our review to measure importance and satisfaction of needs. Some instruments have additional questions to check the presence of, or desire for, help with the need. However, instruments using Likert-type scales may produce "ceiling-effects," in which the majority of needs are rated as very or somewhat important. This low variability among highly-rated needs results in low separation of the needs, and provides no guidance on where scarce resources should be concentrated. The developers of the INM applied the Thurstone scale to overcome this "ceiling-effect." However, this type of scale's greatest disadvantage is that the participant either agrees or disagrees with a given item, and is not able to indicate more subtle responses that lie between two extremes.[74] New measurement strategies, not just scaling methods, need to be investigated, to have a structure for presenting questions to respondents and a corresponding method of analyzing the data in needs assessment context. This will allow scarce resources to be focused.
Conceptual and measurement models of the instruments were not often defined in our review. While many instruments spoke of semi-structured interviews as a way to identify items, this very general term actually provides little information about what was found and how. Ideally, conceptual theory and empirical study should support the measurement structure. We are pleased to see that the factor structure of the PINQ was examined separately for two disease groups and tested again in another longitudinal study. This was a good demonstration of a measurement model evaluation providing statistical evidence of factorial validity across groups. Item Response Theory (IRT) was used to assess the unidimensionality of the NEST-SF. There is a growing body of literature to advocate the potential advantages of using IRT in health outcome assessment. Future research examining the IRT application in needs assessment context is indicated.
Building assessment upon a strong conceptual theory is important; however, we have not seen a conceptual theory that adequately addressed the relationship among needs as specified in the first part of this paper. Such research is needed to understand the relationships among and between needs, satisfaction and quality of life.
One of our primary concerns, however, is lack of evidence that the instruments are sensitive to change. Only six instruments in our review had been tested over time for their responsiveness to change. For example, the DINA was evaluated by comparing an experimental group that was expected to change, with a control group that was expected to remain stable. However, effect size estimation, a useful expression of the change scores, was not reported in these studies. To understand how needs change over time as well as how effective the care intervention is, it is critical to more fully address responsiveness of the instruments.
The reading level of the instruments was not commonly examined, nor were the reasons for missing data and non-completion rates. Such information could yield important insights about the acceptability of the instruments. For instance, five of the respondents who withdrew from participation in the FIN-H study reported that they didn't feel comfortable talking about their feelings. Developers need to anticipate the possibility of emotional or physical strain that the instrument may place on the respondents.
The delivery mechanism may influence the completion rate as well. Mailing may take more time and increase the possibility of forgetting to respond. Telephone and in-clinic surveys can produce a higher response rate[75] but also increase expense[76]. It has been shown that computer-assisted administration of a survey is acceptable to cancer patients who are receiving treatments.[77,78] We believe computer-assisted interactive needs assessment programs can potentially decrease expense and time of collecting needed information, improve ease of use, and possibly yield immediate tailored feedback. It can be conducted as a routine part of the intervention over the disease course. We would urge an investigation of the feasibility of computer-assisted needs assessment.
Of particular note are the few instruments designed to assess the needs of cancer patients/families during the "prevention," "survivorship" and "bereavement" stages. It is valuable to know the needs of people at risk of cancer who are undergoing prevention. However, there is little understanding of the needs of those with a family history of cancer. The ISNQ, the only instrument we found pertaining to a cancer prevention stage, is a good demonstration of an instrument assessing needs of women who have primary relatives with breast cancer.
No instruments targeting the survivorship and bereavement stages were found in our review. Cancer survivors should still receive support according to their needs; thus, more work should be undertaken for cancer survivorship needs assessment. Also, research focusing on caregivers/families who lost a loved one with cancer has not been fully explored. In particular, longitudinal studies conducted from the pre-bereavement to the post-bereavement period are rare. The grief experiences and needs of cancer families should receive monitoring and intervention over the disease course of their loved one, until a period of time after the death. Bereavement instrument research should also incorporate the special needs of younger women and men whose loved one died from cancer.
Needs assessment offers a rich opportunity to more fully understand the experiences of patients and their families. It is a crucial step in prioritizing the allocation of resources to improve quality of care. In our review, each selected instrument meets some but not all of our criteria for validity, reliability, responsiveness and burden. It is questionable whether any instrument can be developed meeting all the requirements as a ideal tool. However, we believe an ideal needs assessment tool would be one that opens the communication channel between patients/families and the professionals. In an era of limited resources, needs assessment should yield information that directs professionals on where and how to prioritize and focus improvement efforts.- At the same time, needs assessment should give patients and families a chance to identify and express the issues they want recognized and addressed by professionals.
Figure 6.
Relationship of needs to satisfaction and quality of life
Supplementary Material
Contributor Information
Kuang-Yi Wen, Email: kuangyi@chsra.wisc.edu.
David H Gustafson, Email: dhgustaf@facstaff.wisc.edu.
References
- Berwick D. The total customer relationship in health care: broadening the bandwidth. The Joint Commission Journal On Quality Improvement. 1997;23:245–250. doi: 10.1016/s1070-3241(16)30314-5. [DOI] [PubMed] [Google Scholar]
- Ross C, Steward C, Sinacore JM. The importance of patient preferences in the measurement of health care satisfaction. Medical Care. 1993;31:1138–1149. doi: 10.1097/00005650-199312000-00006. [DOI] [PubMed] [Google Scholar]
- Medicine of Institute. In: Approaching death: Improving care at the end of life. Field M and Cassel C, editor. Washington, D.C.; 1997. [PubMed] [Google Scholar]
- Bretsher M, Rummons R, Sloan J, Kaur J,, Bartlett A, Borkenhagen L, Loprinzi C. Quality of life in hospice patients. Psychosomatics. 1999;40:309–313. doi: 10.1016/S0033-3182(99)71224-7. [DOI] [PubMed] [Google Scholar]
- Silveira M, EiPiero A, Gerrity M, Geudtner C. Patients knowledge of options at the end of life. Journal of the American Medical Association. 2000;284:2483–2488. doi: 10.1001/jama.284.19.2483. [DOI] [PubMed] [Google Scholar]
- Investigators SUPPORT. A controlled trial to improve care for seriously ill hospitalized patients: The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) Journal of the American Medical Association. 1995;274:1591–1598. doi: 10.1001/jama.274.20.1591. [DOI] [PubMed] [Google Scholar]
- Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. Journal of the American Medical Association. 1997;277:678–682. doi: 10.1001/jama.277.8.678. [DOI] [PubMed] [Google Scholar]
- Guadagnoli E, Ward P. Patient participation in decision-making. Social Science and Medicine. 1998;47:329–339. doi: 10.1016/S0277-9536(98)00059-8. [DOI] [PubMed] [Google Scholar]
- Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. American Journal of Preventive Medicine. 1999;17:285–294. doi: 10.1016/S0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Social Science and Medicine. 1999;49:651–661. doi: 10.1016/S0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- Maguire P. Improving communication with cancer patients. European Journal of Cancer. 1999;35:1415–1422. doi: 10.1016/S0959-8049(99)00178-1. [DOI] [PubMed] [Google Scholar]
- Cull A, Stewart M, Altman D. Assessment of and intervention for psychosocial problems in routine oncology practice. British Journal of Cancer. 1995;72:229–235. doi: 10.1038/bjc.1995.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osoba D. Rationale for the timing of health-related quality-of-life-assessments in oncological palliative therapy. Cancer Treat Rev. 1996;22 Suppl A:69–73. doi: 10.1016/s0305-7372(96)90066-3. [DOI] [PubMed] [Google Scholar]
- Ford S, Fallowfield L, Lewis S. Doctor-patient interactions in oncology. Social Science and Medicine. 1996;42:1511–1519. doi: 10.1016/0277-9536(95)00265-0. [DOI] [PubMed] [Google Scholar]
- Marvel MK, Epstein RM, Flowers K, Beckman HB. Soliciting the patient's agenda: have we improved? Journal of the American Medical Association. 1999;281:283–287. doi: 10.1001/jama.281.3.283. [DOI] [PubMed] [Google Scholar]
- Holland JC, Almanza J. Giving bad news: is there a kinder, gentler way? Cancer. 1999;86:738–740. doi: 10.1002/(SICI)1097-0142(19990901)86:5<738::AID-CNCR2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Kim MK, Alvi A. Breaking the bad news of cancer: the patient's perspective. Laryngoscope. 1999;109:1064–1067. doi: 10.1097/00005537-199907000-00010. [DOI] [PubMed] [Google Scholar]
- Sabo D. Men, death anxiety and denial. In: Clark D, Fritz J and Rieder P, editor. Clinical Sociological Perspectives of Illness and Loss. Philadelphia, Charles Press; 1990. pp. 71–84. [Google Scholar]
- Schulz R, Beach S. Caregiving as a risk factor for mortality. Journal of the American Medical Association. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Cegala DJ. A study of doctors' and patients' communication during a primary care consultation: Implications for communication training. Journal of Health Communication. 1997;2:169–194. doi: 10.1080/108107397127743. [DOI] [PubMed] [Google Scholar]
- Northouse L. Social support in patients and husbands adjustment to breast cancer. Nursing Research. 1988;37:91–95. [PubMed] [Google Scholar]
- Northouse P, Northouse L. Communication and cancer: Issues confronting patients, health professionals and caregivers. Journal of Psychosocial Oncology. 1987;5:17–46. [Google Scholar]
- Peters-Golden H. Varied perceptions of social support in the illness experience. Social Science Medicine. 1982;16:463–491. doi: 10.1016/0277-9536(82)90057-0. [DOI] [PubMed] [Google Scholar]
- Northouse L, Peters-Golden H. Cancer and the family: Strategies to assist spouses. Seminars in Oncology Nursing. 1993;9:74–82. doi: 10.1016/s0749-2081(05)80102-0. [DOI] [PubMed] [Google Scholar]
- Vitaliano P. Psychological and physical concomitants of caregiving; introduction to special issue. Annals of behavioral medicine. 1997;19:75–77. doi: 10.1007/BF02883322. [DOI] [PubMed] [Google Scholar]
- Northouse L. A longitudinal study of the adjustment of patients and husbands to breast cancer. Oncol Nurs Forum. 1989;16:511–516. [PubMed] [Google Scholar]
- Ell K, Nishimoto R, Mantell J. Longitudinal analysis of psychological adaptation among family members of patients with cancer. Journal of psychosomatic research. 1988;32:429–438. doi: 10.1016/0022-3999(88)90026-8. [DOI] [PubMed] [Google Scholar]
- Wilson S, Morse JM. Living with a wife undergoing chemotherapy. Image J Nurs Sch. 1991;23:78–84. doi: 10.1111/j.1547-5069.1991.tb00647.x. [DOI] [PubMed] [Google Scholar]
- Wilkerson S. Factors which influence how nurses communicate with cancer patients. Journal of Advance Nursing. 1991;16:677–688. doi: 10.1111/j.1365-2648.1991.tb01726.x. [DOI] [PubMed] [Google Scholar]
- Grobe ME, Ahmann DL, Ilstrup DM. Needs assessment for advance cancer patients and their families. Oncol Nurs Forum. 1982;9:26–30. [PubMed] [Google Scholar]
- Longman AJ, Atwood JR, Sherman JB, Benedict J, Shang TC. Care needs of home-based cancer patients and their caregivers. Cancer Nursing. 1992;15:182–190. [PubMed] [Google Scholar]
- Bruera E, Kehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. Journal of Palliative Care. 1991;7:6–9. [PubMed] [Google Scholar]
- Davis SW, Quinn S, Fox L, MacElwee N, Engstrom PF. Satisfaction among cancer outpatients. Progress in clinical and biological research. 1988;278:227–232. [PubMed] [Google Scholar]
- Thomas S, Glynne JR, Chait I. Is it worth the wait? A survey of patients' satisfaction with an oncology outpatient clinic. European journal of cancer care. 1997;6:50–58. doi: 10.1111/j.1365-2354.1997.tb00269.x. [DOI] [PubMed] [Google Scholar]
- Schag CC, Heinrich RL, Ganz PA. Cancer Inventory of Problem Situations: An instrument for assessing cancer patients' rehabilitation needs. Journal of Psychosocial Oncology. 1983;1:11–24. [Google Scholar]
- Meyerowitz BE, Heinrich RL, Schag CC, Burish TG, Bradley L. Coping with chronic illness: research and applications. A competency-based approach to coping with cancer. New York, Academic Press; 1983. pp. 137–158. [Google Scholar]
- Ganz PA, Rofessart J, Polinsky ML, Schag CC, Heinrich RL. A comprehensive approach to the assessment of cancer patients' rehabilitation needs: the Cancer Inventory of Problem Situations and a companion interview. Journal of psychosocial Oncology. 1986;4:27–42. [Google Scholar]
- Ganz PA, Shag CC, Polinsky ML, Heinrich RL, Flack VF. Rehabilitation needs and breast cancer: the first month after primary therapy. Breast Cancer Research and Treatment. 1987;10:243–253. doi: 10.1007/BF01805761. [DOI] [PubMed] [Google Scholar]
- Schag CC, Ganz PA, Heinrich RL. Cancer Rehabilitation Evaluation System-Short Form (CARES-SF). A cancer specific rehabilitation and quality of life instrument. Cancer. 1991;15:1406–1413. doi: 10.1002/1097-0142(19910915)68:6<1406::aid-cncr2820680638>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Wingate AL, Lackey NR. A description of the needs of noninstitutionalized cancer patients and their primary care givers. Cancer Nursing. 1989;12:216–225. [PubMed] [Google Scholar]
- Gates MF, Lackey NR, White MR. Needs of Hospice and clinic patients with cancer. Cancer Practice. 1995;3:226–232. [PubMed] [Google Scholar]
- Foot G, Sanson-Fisher R. Measuring the unmet needs of people living with cancer. Cancer Forum. 1995;19:131–135. [Google Scholar]
- Girgis A, Boyes A, Sanson-Fisher RW, Burrows S. Perceived needs of women diagnosed with breast cancer: rural versus urban location. Australian and New Zealand journal of Public Health. 2000;24:166–173. doi: 10.1111/j.1467-842x.2000.tb00137.x. [DOI] [PubMed] [Google Scholar]
- Bonevski B,, Sanson-Fisher R,, Girgis A,, Burton L,, Cook P,, Boyes A. Evaluation of an instrument to assess the needs of patients with cancer. Cancer. 2000;88:217–225. doi: 10.1002/(SICI)1097-0142(20000101)88:1<217::AID-CNCR29>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- McCusker J. Development of scales to measure satisfaction and preferences regarding long-term and terminal care. Medical Care. 1984;22:476–493. doi: 10.1097/00005650-198405000-00011. [DOI] [PubMed] [Google Scholar]
- Tamburini M, Gangeri L, Brunelli C, Beltrami P, Boeri C, C. Borreanim, Fusco Karmann M, Greco G, Miccinesi L, Trimigno Murru & P. Assessment of hospitalized cancer patients' needs by the Needs Evaluation Questionnaire. Annals of Oncology. 2000;11:31–37. doi: 10.1023/A:1008396930832. [DOI] [PubMed] [Google Scholar]
- Coyle N, Goldstein L, Passik S, Fishman B, Portenoy R. Development and validation of a patient needs assessment tool (PNAT) for oncology clinicians. Cancer Nursing. 1996;19:81–92. doi: 10.1097/00002820-199604000-00001. [DOI] [PubMed] [Google Scholar]
- Derdiarian AK. Informational needs of recently diagnosed cancer patients. Nurs Res. 1986;35:276–281. [PubMed] [Google Scholar]
- Mesters I, Borne van den B, Boer MD, Pruyn J. Measuring information needs among cancer patients. Patient Education and Counseling. 2001;43:253–262. doi: 10.1016/S0738-3991(00)00166-X. [DOI] [PubMed] [Google Scholar]
- Boberg EW, Gustafson DH, Hawkins RP, Offord KP, Koch C, Wen K, Kreutz K, Salner A. Assessing the unmet information, support and care delivery needs of men with prostate cancer. Patient Education and Counseling. 2003;49:233–242. doi: 10.1016/S0738-3991(02)00183-0. [DOI] [PubMed] [Google Scholar]
- Thomas C, Morris SM, McIllmurray MB, Soothill K, Francis B, Harman JC. The psychosocial needs of cancer patients and their main carers. Lancaster University, Institute for Health Research; 2001. [Google Scholar]
- Galloway S, Graydon J, Harrison D, Evans-Boyden B, Palmer-Wickham S, Burlein-Hall S, Rich-van der Bij L, West P, Blair A. Informational needs of women with a recent diagnosis of breast cancer: development and initial testing of a tool. Journal of Advanced Nursing. 1997;25:1175–1183. doi: 10.1046/j.1365-2648.1997.19970251175.x. [DOI] [PubMed] [Google Scholar]
- Templeton H, Dphil CM. Adaptation of an instrument to measure the informational needs of men with prostate cancer. Journal of Advance Nursing. 2001;35:357–364. doi: 10.1046/j.1365-2648.2001.01883.x. [DOI] [PubMed] [Google Scholar]
- Denger LF, Davison BJ, Sloan JA, Mueller B. Development of a scale to measure information needs in cancer care. Journal of Nursing Measurement. 1998;6:137–153. doi: 10.1046/j.1365-2834.1998.00060.x. [DOI] [PubMed] [Google Scholar]
- McCarthy M, Higginson I. Clinical audit by a palliative care team. Palliative Medicine. 1991;5:215–221. [Google Scholar]
- Higginson IL, Wade A, McCarthy M. A comparison of four outcome measures of terminal care. In: Gilmore A and Gilmore S, editor. A safer death. London, Plenum Press; 1988. pp. 205–211. [Google Scholar]
- Higginson IJ, McCarthy M. Validity of the support team assessment schedule: do staffs' ratings reflect those made by patients or their families? Palliat Med. 1993;8:219–228. doi: 10.1177/026921639300700309. [DOI] [PubMed] [Google Scholar]
- Higginson IJ, Wade AM, McCarthy M. Effectiveness of two palliative support teams. Journal of Public Health Medicine. 1992;14:50–56. [PubMed] [Google Scholar]
- Ellershaw JE, Peat SJ, Boys LC. Assessing the effectiveness of a hospital palliative care team. Palliative Medicine. 1995;9:145–152. doi: 10.1177/026921639500900205. [DOI] [PubMed] [Google Scholar]
- Emanuel LL, Alpert HR, Baldwin DC, Emanuel EJ. What terminally ill patients care about: toward a validated construct of patients' perspectives. Journal of Palliative Medicine. 2000;3:419–431. doi: 10.1089/jpm.2000.3.4.419. [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Emanuel LL. The promise of a good death. Lancet. 1998;351 Suppl 2:S21–S29. doi: 10.1016/s0140-6736(98)90329-4. [DOI] [PubMed] [Google Scholar]
- Kristjanson LJ, Atwood J, L.F. Denger. Validity and Reliability of the Family Inventory of Needs (FIN): Measuring the Care Needs of Families of Advanced Cancer Patients. Journal of Nursing Measurement. 1995;3:109–126. [PubMed] [Google Scholar]
- Kilpatrick MG, Kristjanson LJ, Tataryn D. Measuring the information needs of husbands of women with breast cancer: validity and reliability of the Family of Inventory of Needs--Husbands. Oncol Nurs Forum. 1998;25:1347–1351. [PubMed] [Google Scholar]
- Kilpatrick MG, Kristjanson LJ, Tataryn DJ, Fraser VH. Information needs of husbands of women with breast cancer. Oncology Nursing Forum. 1998;25:1565–1601. [PubMed] [Google Scholar]
- Kristjanson LJ. Validity and reliability testing of the FAMCARE scale: Measure Family Satisfaction with Advance Cancer Care. Social Science Medicine. 1993;36:693–701. doi: 10.1016/0277-9536(93)90066-D. [DOI] [PubMed] [Google Scholar]
- Wingate AL, Lackey NR. A description of the needs of noninstitutionalized cancer patients and their primary caregivers. Cancer Nursing. 1989;12:216–225. [PubMed] [Google Scholar]
- Hileman JW, Lackey NR. Self-identified needs of patients with cancer at home and their home caregivers: a descriptive study. Oncology Nursing Forum. 1990;17:907–913. [PubMed] [Google Scholar]
- Hileman JW, Lackey NR, Hassanein RS. Identifying the needs of home caregivers of patients with cancer. Oncol Nurs Forum. 1992;19:771–777. [PubMed] [Google Scholar]
- Harrington V, Lackey NR, Gates MF. Needs of caregivers of clinic and hospice cancer patients. Cancer Nursing. 1996;19:118–125. doi: 10.1097/00002820-199604000-00006. [DOI] [PubMed] [Google Scholar]
- Dawson NJ. Need satisfaction in terminal care setting. Social Science Medicine. 1991;32:83–87. doi: 10.1016/0277-9536(91)90131-U. [DOI] [PubMed] [Google Scholar]
- Chalmers K, Thomson K. Coming to terms with the risk of breast cancer: perceptions of women with primary relatives with breast cancer. Qualitative Health Research. 1996;6:256–282. [Google Scholar]
- Chalmers KI, Luker KA, Leinster SJ, Elis I, Booth K. Information and support needs of women with primary relatives with breast cancer: development of the Information and Support Needs Questionnaire. Journal of Advance Nursing. 2001;35:497–507. doi: 10.1046/j.1365-2648.2001.01866.x. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–333. [Google Scholar]
- Evan NJ. Needs assessment methodology: a comparison of results. Journal of College Student Personnel. 1985;26:107–114. [Google Scholar]
- Title CR, Hill RJ. Attitude measurement and prediction of behavioral: An evaluation of conditions and measurement techniques. Sociometry. 1967;30:199–213. [PubMed] [Google Scholar]
- Harris LE, Weinberger M, Tierney WM. Assessing inner-city patients' hospital experiences: a controlled trial of telephone interviews versus mailed surveys. Medical Care. 1997;35:70–76. doi: 10.1097/00005650-199701000-00006. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Kosinski M, Ware JE Jr. Comparison of the costs and quality of norms for the SF-36 health survey collected by mail versus telephone interview: results from a national survey. Medical Care. 1994;32:551–567. doi: 10.1097/00005650-199406000-00002. [DOI] [PubMed] [Google Scholar]
- Degner LF, Davison BJ, Sloan JA, Mueller B. Development of a scale to measure information needs in cancer care. Journal of Nursing Measurement. 1998;6:137–153. doi: 10.1046/j.1365-2834.1998.00060.x. [DOI] [PubMed] [Google Scholar]
- Newell S, Sanson-Fisher RW, Stewart J. Are touchscreen computer surveys acceptable to medical oncology patients? Journal of Psychosocial Oncology. 1997;15:37–46. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.