Abstract
Background
The Internet presents a widely accessible, 24-hour means to promote chronic disease management. The objective of this review is to identify studies that used Internet based interventions to promote lifestyle modification among adults with type 2 diabetes.
Methods
We searched PubMed using the terms: [internet, computer, phone, smartphone, mhealth, mobile health, web based, telehealth, social media, text messages] combined with [diabetes management and diabetes control] through January 2013. Studies were included if they described an Internet intervention, targeted adults with type 2 diabetes, focused on lifestyle modification, and included an evaluation component with behavioral outcomes.
Results
Of the 2803 papers identified, nine met inclusion criteria. Two studies demonstrated improvements in diet and/or physical activity and two studies demonstrated improvements in glycemic control comparing web-based intervention with control. Successful studies were theory-based, included interactive components with tracking and personalized feedback, and provided opportunities for peer support. Website utilization declined over time in all studies that reported on it. Few studies focused on high risk, underserved populations.
Conclusion
Web-based strategies provide a viable option for facilitating diabetes self-management. Future research is needed on the use of web-based interventions in underserved communities and studies examining website utilization patterns and engagement over time.
Diabetes prevalence continues to grow in the United States, affecting an estimated 8.3% of the population (25.8 million people).1 A future projection shows an estimated increase in the national prevalence of diabetes to roughly 26.5% of the population by the year 2050.2 Lifestyle modification and behavior changes are key components of diabetes management, especially type 2 diabetes.3 Numerous studies have documented the benefits lifestyle modification and disease management have on improving glycemic control and reduction of diabetes related complications.3 However translating evidence-based recommendations to practical strategies designed for real world settings has proven challenging and many individuals fail to achieve the glycemic control needed to avoid diabetes related complications.4 Clearly practical strategies suitable for widespread dissemination are needed that can reach individuals where they live, work and play in order to address the diabetes epidemic in a meaningful way.
The Internet and related mobile technologies present a widely accessible, 24-hour means to promote disease management and facilitate behavior modification.5 Implementation of web-based interventions to assist with diabetes management has exploded over the past decade.6,7 To date, the majority has focused specifically on using web-based technology to facilitate the glucose monitoring process, allowing patients to upload monitoring data so their physician can adjust the dosage of insulin or medication.6,8,9 Generally these types of intervention have shown enhanced patient-provider communication, medication adherence and ultimately an improvement in glucose control. A review of Internet diabetes programs published in 2011 identified over 137 web-based mobile applications, with most focused on insulin titration and very few focused on lifestyle modification.6 When investigators reviewed the applications for content and strategies, inclusion of behavior theory and education with tailored feedback were notably lacking. These findings were surprising given that 95% of individuals with diabetes have type 2, where disease management is heavily focused on lifestyle modification and typically includes oral agents as first line therapy.10
The primary objective of this review is to identify studies that used an Internet based interventions to promote diabetes education and lifestyle modification among adults with type 2 diabetes. In light of existing diabetes related health disparities that exist along socioeconomic and racial/ethnic lines, an important secondary objective is to assess the extent to which these interventions have tailored their interventions for diverse and/or underserved communities.
METHODS
Search strategy: We searched PubMed using the terms: [internet, computer, phone, smartphone, mhealth, mobile health, web based, telehealth, social media, OR text messages] combined with the terms [diabetes management and diabetes control] through January 2013. We supplemented this search by performing a backwards search of all of the references of articles that met inclusion criteria or were topically relevant. Only papers that measured patient outcomes and described the evaluation of the study were included.
Eligibility/exclusion criteria
To be eligible, studies had to describe an internet intervention that targeted adults with type 2 diabetes, focused on behavior change and/or lifestyle, and included an evaluation component. Studies that focused exclusively on glucose monitoring or electronic health records/web portals for uploading data were not included. Studies that included glucose monitoring or electronic health records as part of a larger intervention focused on lifestyle modification and patient education were eligible. Two authors independently reviewed each abstract of identified articles. Studies were excluded at this stage if both reviewers agreed that the eligibility criteria were clearly not met. If either reviewer could not exclude the study based on the abstract, the full article was reviewed independently by two authors.
Data abstraction
One author abstracted the data from the articles using predetermined tables. A second confirmed the accuracy of the data abstracted into evidence tables. Since selected outcomes differed markedly between studies, data were not extracted for meta-analysis. Abstraction forms included sample size, study duration, target population, behavior theory, targeted behaviors, measured outcomes, as well as intervention strategies, including peer support and/or interactive components. Interactive components were defined as features that allowed users to comment, chat, edit, or interact with the information, other users, or members of the healthcare team. Target behaviors as described from the American Association of Diabetes Educators 7 were also summarized for each study.11 These behaviors included, healthy eating, being active, monitoring, taking medication, healthy coping, reducing risks, and problem solving.
RESULTS
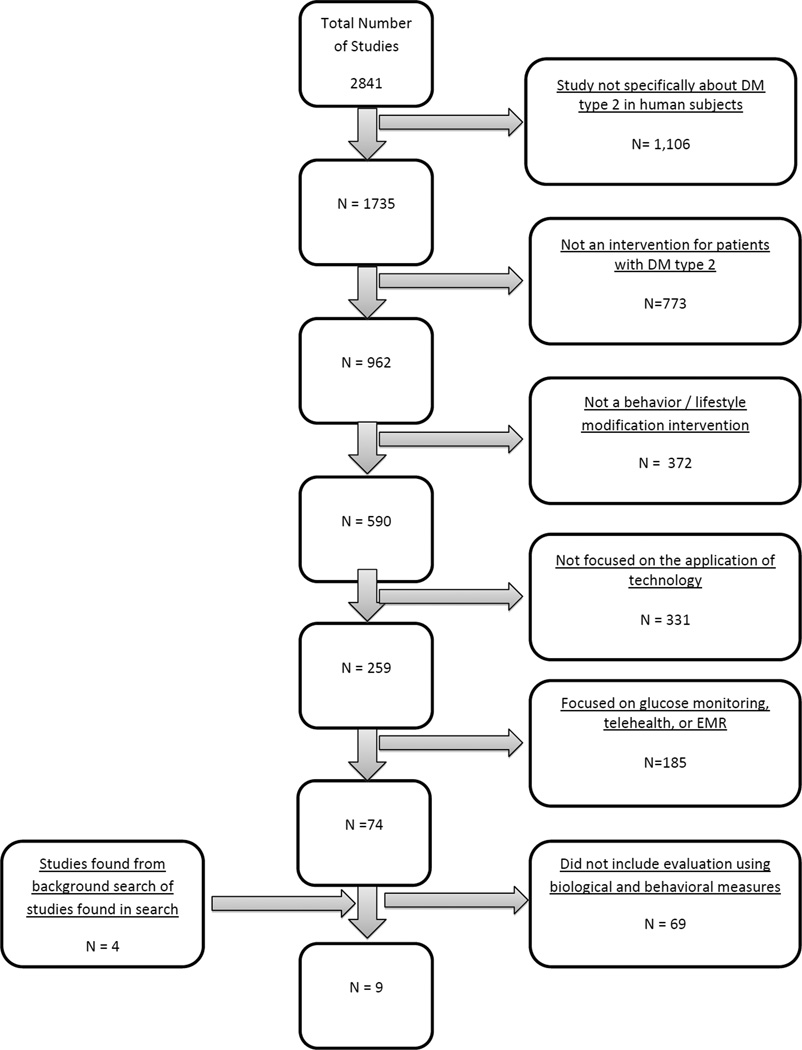
The search identified 2803 papers; nine studies (13 papers) met inclusion criteria.12–24 (Figure 1) Eight of the studies reviewed were randomized controlled trials with patients with type 2 diabetes (5 small trials < 100 participants; 3 larger trials > 300 participants) and one was quasi-experimental with a control group (n=98).21
Figure 1.
Flow diagram of search results for web-based behavioral/lifestyle modification interventions for patients living with type 2 diabetes.
Each study created a web-based intervention designed to promote diabetes education and some health behavior change; a brief description of the web-based program is provided in Table 1. The most commonly targeted behaviors included being active (8/9), healthy eating (6/9), and glucose monitoring (5/9). Just under half of programs (4/9) included a specific focus on coping skills and support; similarly 4 of 9 programs included a specific focus on medication adherence. One third of programs included a focus on problem solving (3/8) and reducing risks (3/8) such as smoking. In general, applications provided a variety of mechanisms to promote behavior modification ranging from static education to structured goal setting and progress tracking tools to platforms for social support. For example, in the Glasgow 2010 study, participants were asked to set dietary and exercise goals and track their progress using the tracking section of the website.16 In the Carter study, participants used a social networking module to discuss issues with other participants and provide support for one another.12 Six of nine programs specifically included some form of peer support or online community to engage users. These online communities could take the shape of live chats, allowing users to talk to one another instantly, as in the Glasgow 2003 study, or message boards, allowing users to post topics for everyone to discuss, as in the Liebreich study.14,19 Over half of the programs (6/9) reported using specific theory/conceptual framework to design their intervention. These included Self-efficacy/Social Cognitive Theory,14,19,20 Social Support Theory,14 Social-Ecological Framework,16 Health Belief Model24 and Transtheoretical Model.18
Table 1.
Descriptions of web-based type 2 diabetes interventions and targeted behaviors for studies meeting inclusion criteria
| Author, Year | Web-based Program Description | Peer support/ Online community |
Behavior theory | Target Behaviors* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Healthy Eating |
Being Active |
Glucose Monitoring |
Taking Medication |
Healthy Coping/ Support |
Reducing Risks/ Complications |
Problem Solving |
||||
| McKay 2001,22 Glasgow, 200314 Feil 200013 | Tailored self-management (TSM) and peer support maintenance (PS) components added to a basic internet nutrition intervention | Forums Live Chat | Self-efficacy and Social Support Theory | X | X | X | X | X | X | |
| McIlhenny 201121 | One-on-one individualized diabetes education and hands on instruction on how to access and navigate MyHERO, a web portal for evidence-based, publically available DM information | Not Mentioned | Not Mentioned | X | X | X | X | X | ||
| Noh 201023 | Web-based information system, eMOD (electronic Management of Diabetes), to provide real-time information on diabetes management including topics such as diet, dining out, hypoglycemia and stress management. | Not Mentioned | Not Mentioned | X | X | X | X | |||
| Carter 201112 | Online portal with 3 modules: self-management, health education, and social networking. Participants received laptop with wireless scale, BP cuff and glucometer and had biweekly virtual visits with nurse to review biometric data | Social Network Module | Not Mentioned | X | X | X | X | X | ||
| Lorig 201020 | Internet-based diabetes self-management program with 4 parts: The Learning Center (weekly education session content and action planning), The Discussion Center (open forum), MyTools (exercise and medication logs, meal planning etc.) and Post Office (private email). Program facilitated by peers. | Bulletin Boards, Listserve discussion group | Self-efficacy theory | X | X | X | X | X | X | |
| Glasgow 2010,16 Glasgow 2010,17 | Glasgow 201115 Program provides computer-assisted self-management, with goal setting and information modules; website includes moderated forum, graphical display of user A1C, BP and cholesterol, community resources for diabetes selfmanagement plus features to enhance engagement (quizzes, motivational quotes). Available in English and Spanish. | Moderated forum | Social-ecological framework and the “5 A’s” (assess, advise, agree, assist, and arrange) | X | X | X | X | |||
| Liebreich 200919 | Website comprises five main sections (weekly topic, education, research, fitness tips and physical activity myths) updated and archived on a weekly basis with several interactive features to engage participants (physical activity logbook, message board and personalized email) counseling from the study coordinator). | Message Boards | Social Cognitive Theory | X | ||||||
| Richardson 200724 | Web-based intervention using enhanced pedometers that upload physical activity via USB; website provides personalized information and feedback, motivational messages regarding PA, and tips about managing diabetes. | Not mentioned | Health Belief Model | X | ||||||
| Kim 200618 | Website includes general physical activity (PA) information, a PA screening instrument and assessment tool, a graded exercise test (GXT) and individualized PA description, five staged matched PA interventions, | Question and answer board | Transtheoretical Model (TTM) | X | ||||||
Target behaviors are categorized into AADE 7 Self-Care Behaviors.11
Behavioral outcomes
Nearly all of the studies measured change in physical activity (8/9). Of those, only one study reported statistically significant differences in activity levels for participants enrolled in a web-based program vs participants in the non-web-based control group.16 In intent to treat analyses, Glasgow et al (n=463) reported an increase in physical activity as measured by self-report using the Community Health Activities Model Program Questionnaire (p=0.04). Comparing a web-based program with email counseling to a control condition that provided links to publicly available web-sites, Liebreich et al. (n=49) reported an increase in total vigorous and moderate minutes of physical activity (measured by) but did not report comparison between groups.19 Kim et al found that the study’s internet intervention and print based intervention were both effective at increasing physical activity when compared to no intervention at all but did not find a significant difference between the two interventions.18 Richardson et al. compared two different styles of goal setting for physical activity, encouraging a focus on total number of steps (Lifestyle Goals) vs focusing on bouts of 10 minutes of exercise (Structured Goals) both facilitated by a web-based program.24 The investigators found both strategies to be equally effective, though individuals focused on total number of steps were more satisfied with the intervention.
Over half of the studies (5/9) measured dietary behavior. Glasgow 2010 reported significant dietary changes (eating habits, fat intake) using intent to treat analyses among individuals in the web-based intervention arm compared to participants in the non web-based intervention.16 There were no between group differences related to diet for the remaining four studies that examined diet. McKay et al. noted dietary improvements for all groups but between group differences were not significant.22
Two studies measured medication adherence, neither reported changes related to the intervention.16,21 One study noted an improvement in self-reported glucose monitoring.21
Physiologic Outcomes
Hemoglobin A1C was the most commonly measured physiologic parameter, reported in seven of nine studies. Two of those seven reported some improvement in A1C among participants in the web-based intervention arm compared to participants in the non web-based control arm.12,20 At 6 months, Lorig et al reported significant improvement in A1C in the web based treatment arm compared to the usual-care arm (p<0.05), significance decreased slightly in intent-to-treat analyses (p<0.06). Interestingly, changes in behaviors did not differ significantly between groups. In the Carter study, the web-based intervention group showed a 2.18 point decrease in HbA1c versus 0.9 in the usual care control group (p<0.05). However the study was small (n=74) with limited retention (63%) and a high baseline A1C of 8.9. Of the 4 studies that measured BMI, only one reported a significant change in weight.12 Carter et al demonstrated a BMI decrease of 11.6 points in the web-based intervention arm versus 9.6 in the control group (p<0.05), though notably both groups lost a significant amount of weight. Four of the 9 studies measured blood pressure but none demonstrated a decrease when comparing web-based intervention arm with the control. Similarly, of the 5 studies that measured participants’ lipid levels none reported a significant improvement compared with control.
Knowledge and Self-Efficacy
Two of the nine studies measured changes in diabetes knowledge. The McIlhenny study used the BASICS curriculum diabetes knowledge test. The interventional group showed a 36.7 point increase compared to the 6 point increase of the control group. However, change in knowledge did not translate into significant changes in behavior. In Carter study, the interventional group went from 50% of people scoring 80 or higher on the diabetes knowledge test to 92% compared to the control group who went from 57% scoring 80 or better to only 76%. Two studies measured self-efficacy. In the Lorig study, treatment participants had higher self-efficacy at 6 and 18 months compared to control participants. Liebreich et al. reported an improvement in behavioral capacity but not self-efficacy.
The target audience varied widely across studies. Among studies conducted in the U.S., only one focused specifically on a racial/ethnic minority population; Carter et el designed their program to be used by urban dwelling African Americans. Three of the other studies included a significant proportion of minority participants; Lorig et al. included 24% minorities, including 110 American Indians/Alaska Natives, Richardson included approximately 24% minorities and Glasgow included 36% (22% Latino and 14% African American). Other special population of interest included novice internet users,22 rural populations,21 and older adults.21,22 Two studies were conducted in South Korea; Noh et al focused on younger individuals (mean age 42) while Kim recruited a middle aged (mean age 55) clinic-based sample. With regard to Internet access, six studies required personal Internet access (two of those studies provided personal Internet access to participants), two studies did not require personal internet access and one study did not report whether or not they required personal Internet access. Of the studies that did not require personal access, one provided Internet access within the clinic and the other did not describe how participants accessed the Internet.18,21
Four of nine studies reported on website utilization of time; in all of these there was a decline. Glasgow et al. reported significant dietary changes (eating habits, fat intake) using intent to treat analyses among individuals in the web-based intervention arm compared to participants in the non web-based intervention, noting that greater Internet use was associated with greater improvements in eating patterns. Glasgow et al also noted a correlation with greater Internet use and more physical activity; Liebreich did not find a significant correlation between the Internet use and physical activity. Though Lorig et al. did not report on website utilization over time, they did note there were no significant differences in utilization patterns between racial/ethnic groups.
DISCUSSION
This review synthesized existing evidence regarding the use of Internet programs designed to promote lifestyle modification for individuals with type 2 diabetes. Of the 2803 papers identified with the included search terms, nine met inclusion criteria. Two studies demonstrated improvements in diet and/or physical activity when comparing web-based lifestyle modification program to control.16,19 Both studies were theory based, interactive, and included tracking tools with personalized feedback and opportunities for peer support. Two studies demonstrated improvements in glycemic control (as measured by A1C) using web-based intervention compared with control.12,20 One of those programs was theory-based, interactive with tracking and personalized feedback, and provided opportunities for peer support. The other program, notably the only program focused exclusively on a racial/ethnic population, was not theory-based, but did include opportunities for peer support along with a structured, nurse-led telehealth component. Few studies focused on high risk, underserved populations and more research is needed to inform internet-based strategies that seek to serve individuals for whom the digital divide persists. Similarly, more research is needed to determine which behaviors are most amenable to change through the use of internet-based strategies. This review identified studies that successfully changed dietary behaviors and physical activity; however the two studies that examined change in medication adherence were both negative.
Achieving adherence to healthy behaviors over time is one of the biggest challenges for any behavioral intervention and the same appears to be true for internet-based interventions. In past studies assessing internet strategies for diabetes, higher website utilization is associated with a reduction in glycemia as measured by Hemoglobin A1C, presumably in part through adherence to healthy behaviors.9 In the current review, all the studies that measured website utilization over time saw a decrease in program use. The impact of level of engagement with the web-based program was not consistent across programs. For example, Liebreich et al did not find website utilization to be associated with physical activity levels. On the other hand, Glasgow et al. found that greater website use was associated with dietary behaviors and physical activity levels but not with medication adherence or biologic outcomes. Further research is needed to better determine optimal utilization patterns and how those patterns vary according to the target behavior/outcome and by individual user. Assuming some optimal “dose” of interaction with web-based programs exists, maintaining participant engagement could be an important determining factor for the success of interventions aimed at promoting lifestyle modification for individuals with diabetes.
Several strategies for bolstering participant engagement with web-based interventions are described in the literature.9 One strategy is through the use of interactive modules that allow for tracking and tailored feedback. Another strategy that can increase user engagement with the intervention is through the addition of a personalized “soft touch” component from counselors or peer supporters and/or emails and telephone contacts. This provides participants with opportunities to discuss problems with others experiencing the same issues. It is significant that in the Glasgow article, the Peer Support group showed better diabetes support scale outcomes than the Tailored Self-Management alone group. This suggests further research is warranted to determine whether peer based online forums are more effective than patient –to-expert interactions in improving participant engagement as well as behavioral and biologic outcomes.
This study reveals a relative paucity of data on the use of web-based lifestyle programs for use among high risk and/or underserved populations. While several studies in included in this review targeted specific high risk and/or underserved populations, too few focused on the same priority population to draw meaningful conclusions regarding the acceptability or feasibility for those populations on the whole. Racial/ethnic minority groups in the United States are disproportionally affected by diabetes with the age-adjusted prevalence of diagnosed diabetes nearly twice as high among African Americans and Hispanics compared to whites and higher likelihood of experiences several diabetes related complications for both groups.1,25–28 Similarly, individuals of lower socioeconomic status or with low levels of education are at higher risk for diabetes and worse outcomes compared to those with higher levels of education and more resources.29 Often, it is the same groups who suffer the greatest burden of diabetes who are least likely to access the Internet.30,31 By the most recent estimates, one in five American adults does not use the internet.32 While the internet gap between minorities and whites has all but disappeared, age (being 65 or older), a lack of a high school education, and having a low household income (less than $20,000 per year) remain strong negative predictors of internet use.33 Given current socioeconomic health disparities related to type 2 diabetes, any new modality aimed at improving diabetes self-management must carefully examine its potential generalizability and reach.30
Research has shown the potential that community-based interventions hold for helping overcome health disparities in an effective and financially feasible manner.34–36 This review identified no studies describing a connection to the local community. Instead, the interventions focused on users interacting via the Internet, often creating online communities that are independent of geography. This allows the same intervention to be used in multiple geographic areas and allows more users to be able to connect to one another and members of the health worker community. However, linkages to local community resources could provide another means of increasing accountability and adherence as patients gain reinforcement from their community. Recently, we developed a website to help individuals identify and locate existing resources in their community to facilitate diabetes self-management and lifestyle modification (mydiabetesconnect.com).37 The site was developed as part of a larger city-wide diabetes management campaign, Cities for Life in Birmingham, Alabama. The site allows users to locate resources in all the major categories related to diabetes management, including diet, physical activity, diabetes education and support, and stress management. New resources can be uploaded at anytime and a star rating system allows users to assess each resource. The site also facilitates user communication with others in their community through a professionally monitored message board. Although content is specific to Birmingham, AL, the development process and site structure are readily generalizable to other communities.
Limitation
Our study has limitations. First, despite a vigorous attempt to identify relevant articles, it is possible that some were missed, or that publication bias led to underreporting of data related to our question. Second, our ability to draw strong conclusion is hampered by the heterogeneity between study interventions and measurement as well as limited number and quality of relevant studies. Despite these limitations, the review does identify several important areas in need of future research, including the use of web-based diabetes interventions in underserved communities and strategies to determine the importance of website utilization patterns and engagement over time.
Conclusion
The field of web-based interventions for lifestyle modification in patients with type 2 diabetes is new and rapidly developing. As technology continues to advance there is a need for sustained research in this field to aid in the development of more effective interventions. The studies discussed in this paper show the ability for such interventions to succeed in reaching patients and promoting appropriate lifestyle modification. Web-based strategies provide a viable option for facilitating the self-management process outside of the clinical setting.
Table 2.
Measured outcomes and results of web-based type 2 diabetes studies meeting inclusion criteria
| Author, Year | Study Design | Sample | Length of Study (Retention) |
Outcomes | Results | |||
|---|---|---|---|---|---|---|---|---|
| Behavior | Knowledge and/or Self- efficacy |
Biologic | Psycho social |
|||||
| McKay 200122, Glasgow 200314 Feil 200013 | 3-arm RCT: Basic nutrition vs TSM* vs PS** N = 320 |
Older Adults Mean age 59 Personal internet access provided | 10 mos. (82% at 1 year follow-up) | Diet, Exercise, Risk factors | A1C Lipids | Depression, Diabetes Support | Significant improvements from baseline across conditions on dietary and psychosocial outcomes, significant but modest for other behavioral outcomes and biological outcomes. No significant differences between treatment conditions on any outcomes except PS condition produced greater improvement on diabetes support. Web use declined over time |
|
| McIlhenny 201121 | Pre-post comparison with control N = 98 |
Rural living Adults Mean age 61.8 (I); 65.8 (C) Personal internet access not required |
6 mos. (54%) | Diet, Exercise, Medication adherence, Foot check | Knowledge | A1C Lipids BP | Quality of Life | Compared with control group, intervention group had larger increase in diabetes knowledge and self-reported glucose monitoring, otherwise no significant between group differences were observed. Web use declined over time. Participants reported high satisfaction with nurse educator but not internet component |
| Noh 201023 | RCT: Intervention vs. UC N = 40 |
Adults in Seoul, Korea Mean age 42.5 (I); 42.3 (C) Personal internet access required |
8 mos.(90%) | Diet, Healthy Coping/Support | A1C Lipids BMI BP | No significant between group differences were observed, though intervention group showed significant within group improvement in A1C (−1.53 +/− 1.42%; p=0.03). Frequency of access to eMOD via cell phones significantly correlated with lower A1C values; access via home computer was not correlated with A1C. Web utilization over time not reported. |
||
| Carter 201112 | RCT: Intervention vs. UC N = 74 |
Urban dwelling African Americans Mean age 52 (I); 49(C) Personal internet access provided |
9 mos. (63.5%) | Diet. Exercise. Knowledge | Knowledge | A1c Lipids BP | Intervention participants were significantly more likely to achieve the desired hemoglobin A1c target (≤7.0) and BMI(<25). Intervention participants also reported improvements in DM knowledge and adherence to diabetes management behaviors. Web utilization over time not reported. |
|
| Lorig 201020 | 3-arm RCT UC vs. Internet vs. Internet with follow-up N = 761 |
Mean age 54.3 76% white 110 American Indians/Alaska Natives Personal internet access required |
6 mos. & 18 mos. (85% & 81% at follow-up) |
Exercise | Knowledge Self-efficacy | A1C | Depression, Patient Activation | At 6 months, treatment participants had lower A1C (P <0.05) as well as improvements in patient activation (PAM) and self-efficacy (0.021 and <0.001) compared with usual-care control subjects. Health behavior changes were not significantly different between groups. In intent-to-treat analyses, PAM and self-efficacy remained significant, the P value for A1C increased to 0.060. At 18 months, change scores for self efficacy and PAM were significantly higher for treatment participants, A1C was not measured. Web utilization over time not reported. Subgroup analyses (n=45) revealed no observed differences in overall utilization between racial groups. |
| Glasgow 2010,16 Glasgow 2010,17 Glasgow 201115 | 3-arm RCT: EUC vs. CASM vs. CASM + Social Support§ N = 463 |
HMO population Mean age 58.4 21.8% Latino 14% African-American Bi-weekly internet access required |
4 mos. (82.5% at follow-up) | Diet, Exercise, Medication adherence | A1C, lipids, BMIBP | In intention to treat analyses, the intervention produced greater improvements in eating habits, fat intake, and physical activity (p<0.001, p=0.006, p=0.04). There were no between group differences in biologic outcomes at 4months. Added contact did not enhance outcomes beyond minimal contact. Greater use of the website was related to greater improvement in eating patterns and in physical activity but not with medication adherence or biological outcomes. Web use declined over time. |
||
| Liebreich, 200919 | RCT N = 49 |
Mean age: 54.1 Internet access not reported |
12 weeks (89.7%) | Exercise | Self-efficacy | BMI | Social support/coping | The intervention group demonstrated a significant improvement in total vigorous and moderate minutes of physical activity (p=0.05) with a mean difference of 47minutes (95% CI = −.37 – −102.7, p<0.052). Behavioral capacity increased significantly in the intervention group (p<0.001), self-efficacy did not. Website use decreased over time but website usage was not correlated with physical activity among intervention participants |
| Kim 200618 | 3-arm RCT: UC vs. Print-only vs. Web N=73 |
Clinic-sample in South Korea Mean Age 55.1 Personal internet access not required |
12 weeks | Exercise | Fasting Blood Sugar (mg/dl), A1C | Both the web based and printed material intervention, compared to usual care, were effective in increasing physical activity (p<.001) and decreasing fasting blood sugar (p<.01) and glycosolated hemoglobin (p<.01). Post hoc analysis for change scores indicated significant no differences between web-based and printed material interventions. Web utilization over time not reported. |
||
| Richardson 200724 | Pilot RCT: 2 goal setting approaches - Lifestyle Goals (LG) vs Structured Goals (SG) N=35 |
Mean age: 52.0 (LG); 53.0 (SG) LG: 76% white; 18% black; 6% other SG:77% white; 8% black; 15% other Personal internet access required |
6 weeks (85.7%) | Exercise | Both groups significantly increased steps, but there was no statistically significant difference between the two groups. Among study completers, steps increased by 1921 +/−2279 steps/day. Those receiving Lifestyle Goals were more satisfied with the intervention (p=0.006) and wore the pedometer more often (p<0.001). Biometrics were not measured. Web utilization over time not reported. |
|||
RCT= Randomized Control Trial; I=Intervention Arm; C=Control Arm; UC=Usual Care
Tailored Self-Management
PS=Peer Support;
EUC=Enhanced UC, CASM=Computer Assisted Self-Maintenance, CASM + Social Support=Computer Assisted Self-Maintenance and Social Support
Acknowledgements
Activities related to the conduct of this research were funded by grants from the NIDDK/UAB Diabetes Research and Training Center (P60DK079626), the American Diabetes Association (ADA 191605) and the American Academy of Family Practice with support from Sanofi.
Funding support: The project was sponsored by grants from the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, University of Alabama at Birmingham (UAB) Diabetes Research and Training Center [P60 DK079626], the American Diabetes Association [191605] (Dr. Cherrington), and the Agency for Healthcare RQ [K12 HS019465]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Diabetes Fact Sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. (Accessed at http://apps.nccd.cdc.gov/DDT_STRS2/CountyPrevalenceData.aspx?mode=DBT.)
- 2.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Vol. 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. National Diabetes Fact Sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. [Google Scholar]
- 5.Kaufman N. Internet and information technology use in treatment of diabetes. Int J Clin Pract Suppl. 2010:41–46. doi: 10.1111/j.1742-1241.2009.02277.x. [DOI] [PubMed] [Google Scholar]
- 6.Chomutare T, Fernandez-Luque L, Arsand E, Hartvigsen G. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res. 2011;13:e65. doi: 10.2196/jmir.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osborn CY, Mayberry LS, Mulvaney SA, Hess R. Patient web portals to improve diabetes outcomes: a systematic review. Current diabetes reports. 2010;10:422–435. doi: 10.1007/s11892-010-0151-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris MA, Hood KK, Mulvaney SA. Pumpers, skypers, surfers and texters: technology to improve the management of diabetes in teenagers. Diabetes Obes Metab. 2012;14:967–972. doi: 10.1111/j.1463-1326.2012.01599.x. [DOI] [PubMed] [Google Scholar]
- 9.Yu CH, Bahniwal R, Laupacis A, Leung E, Orr MS, Straus SE. Systematic review and evaluation of web-accessible tools for management of diabetes and related cardiovascular risk factors by patients and healthcare providers. J Am Med Inform Assoc. 2012;19:514–522. doi: 10.1136/amiajnl-2011-000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramadas A, Quek KF, Chan CK, Oldenburg B. Web-based interventions for the management of type 2 diabetes mellitus: a systematic review of recent evidence. Int J Med Inform. 2011;80:389–405. doi: 10.1016/j.ijmedinf.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 11.AADE7. [Accessed July 1, 2013];2013 at http://www.diabeteseducator.org/ProfessionalResources/AADE7/. [Google Scholar]
- 12.Carter EL, Nunlee-Bland G, Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspect Health Inf Manag. 2011;8:1b. [PMC free article] [PubMed] [Google Scholar]
- 13.Feil EG, Glasgow RE, Boles S, McKay HG. Who participates in Internet-based self-management programs? A study among novice computer users in a primary care setting. Diabetes Educ. 2000;26:806–811. doi: 10.1177/014572170002600509. [DOI] [PubMed] [Google Scholar]
- 14.Glasgow RE, Boles SM, McKay HG, Feil EG, Barrera M., Jr The D-Net diabetes selfmanagement program: long-term implementation, outcomes, and generalization results. Preventive medicine. 2003;36:410–419. doi: 10.1016/s0091-7435(02)00056-7. [DOI] [PubMed] [Google Scholar]
- 15.Glasgow RE, Christiansen SM, Kurz D, et al. Engagement in a diabetes self-management website: usage patterns and generalizability of program use. J Med Internet Res. 2011;13:e9. doi: 10.2196/jmir.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glasgow RE, Kurz D, King D, et al. Outcomes of minimal and moderate support versions of an internet-based diabetes self-management support program. J Gen Intern Med. 2010;25:1315–1322. doi: 10.1007/s11606-010-1480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glasgow RE, Strycker LA, Kurz D, et al. Recruitment for an internet-based diabetes self-management program: scientific and ethical implications. Ann Behav Med. 2010;40:40–48. doi: 10.1007/s12160-010-9189-1. [DOI] [PubMed] [Google Scholar]
- 18.Kim CJ, Kang DH. Utility of a Web-based intervention for individuals with type 2 diabetes: the impact on physical activity levels and glycemic control. Comput Inform Nurs. 2006;24:337–345. doi: 10.1097/00024665-200611000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Liebreich T, Plotnikoff RC, Courneya KS, Boule N. Diabetes NetPLAY: A physical activity website and linked email counselling randomized intervention for individuals with type 2 diabetes. Int J Behav Nutr Phys Act. 2009;6:18. doi: 10.1186/1479-5868-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lorig K, Ritter PL, Laurent DD, et al. Online diabetes self-management program: a randomized study. Diabetes Care. 2010;33:1275–1281. doi: 10.2337/dc09-2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McIlhenny EH, Riba J, Barbanoj MJ, Strassman R, Barker SA. Methodology for determining major constituents of ayahuasca and their metabolites in blood. Biomed Chromatogr. 2012;26:301–313. doi: 10.1002/bmc.1657. [DOI] [PubMed] [Google Scholar]
- 22.McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The diabetes network internet-based physical activity intervention: a randomized pilot study. Diabetes Care. 2001;24:1328–1334. doi: 10.2337/diacare.24.8.1328. [DOI] [PubMed] [Google Scholar]
- 23.Noh JH, Cho YJ, Nam HW, et al. Web-based comprehensive information system for self-management of diabetes mellitus. Diabetes Technol Ther. 2010;12:333–337. doi: 10.1089/dia.2009.0122. [DOI] [PubMed] [Google Scholar]
- 24.Richardson CR, Mehari KS, McIntyre LG, et al. A randomized trial comparing structured and lifestyle goals in an internet-mediated walking program for people with type 2 diabetes. Int J Behav Nutr Phys Act. 2007;4:59. doi: 10.1186/1479-5868-4-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. Jama. 2002;287:2519–2527. doi: 10.1001/jama.287.19.2519. [DOI] [PubMed] [Google Scholar]
- 26.Rucker-Whitaker C, Feinglass J, Pearce WH. Explaining racial variation in lower extremity amputation: a 5-year retrospective claims data and medical record review at an urban teaching hospital. Arch Surg. 2003;138:1347–1351. doi: 10.1001/archsurg.138.12.1347. [DOI] [PubMed] [Google Scholar]
- 27.Young BA, Maynard C, Boyko EJ. Racial differences in diabetic nephropathy, cardiovascular disease, and mortality in a national population of veterans. Diabetes Care. 2003;26:2392–2399. doi: 10.2337/diacare.26.8.2392. [DOI] [PubMed] [Google Scholar]
- 28.Young BA, Maynard C, Reiber G, Boyko EJ. Effects of ethnicity and nephropathy on lower-extremity amputation risk among diabetic veterans. Diabetes Care. 2003;26:495–501. doi: 10.2337/diacare.26.2.495. [DOI] [PubMed] [Google Scholar]
- 29.Rabi DM, Edwards AL, Southern DA, et al. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health Serv Res. 2006;6:124. doi: 10.1186/1472-6963-6-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18:318–321. doi: 10.1136/jamia.2010.006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Welch G, Shayne R. Interactive behavioral technologies and diabetes self-management support: recent research findings from clinical trials. Current diabetes reports. 2006;6:130–136. doi: 10.1007/s11892-006-0024-9. [DOI] [PubMed] [Google Scholar]
- 32.Pew Internet and American Life Project: Mobile Access 2010. [Accessed May 29,2011];2011 Jul; at http://www.pewinternet.org/Reports/2010/Mobile-Access-2010.aspx. [Google Scholar]
- 33.Pew Research Center. 2012 [Google Scholar]
- 34.Horowitz CR, Eckhardt S, Talavera S, Goytia C, Lorig K. Effectively translating diabetes prevention: a successful model in a historically underserved community. Transl Behav Med. 2011;1:443–452. doi: 10.1007/s13142-011-0067-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Plescia M, Herrick H, Chavis L. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health project. Am J Public Health. 2008;98:1678–1684. doi: 10.2105/AJPH.2007.125062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosal MC, Ockene IS, Restrepo A, et al. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos: latinos en control. Diabetes Care. 2011;34:838–844. doi: 10.2337/dc10-1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cherrington AAAA, LaCruz Debby M, Guzman Alfredo L, Cotter Alexander, Thurman Janet P, Loskutova Natalia, Fisher Edwin B. Cities for Life: Mydiabetesconnect.com: A Mixed-Methods Approach to a Community Diabetes Resource Website (published abstract) Diabetes. 2013;16 [Google Scholar]