Abstract
Objective
SENSE Theatre is a novel intervention program aimed at improving reciprocal social interaction in youth with autism spectrum disorder (ASD) using behavioral strategies and theatrical techniques in a peer-mediated model. Previous research using a 3-month model showed improvement in face perception, social interaction, and reductions in stress. The current study assessed a 2-week summer camp model.
Method
Typically developing peers were trained and paired with ASD youth (8–17 years). Social perception and interaction skills were measured before and after treatment using neuropsychological and parental measures. Behavioral coding by reliable, independent raters was conducted within the treatment context (theatre) and outside the setting (playground). Salivary cortisol levels to assess physiological arousal were measured across contexts (home, theatre, and playground). A pretest-posttest design for within-group comparisons was used, and pre-specified pairwise comparisons were achieved using a nonparametric Wilcoxon signed rank test.
Results
Significant differences were observed in face processing, social awareness, and social cognition (p<0.05). Duration of interaction with familiar peers increased significantly over the course of treatment (p<0.05) while engagement with novel peers outside the treatment setting remained stable. Cortisol levels rose on the first day of camp compared to home values yet declined by the end of treatment and further reduced during post-treatment play with peers.
Conclusions
Results corroborate previous findings that the peer-mediated theatre program contributes to improvement in core social deficits in ASD using a short-term, summer camp treatment model. Future studies will explore treatment length and peer familiarity to optimize and generalize gains.
Keywords: autism, social interaction, face processing, theatre, cortisol
INTRODUCTION
Autism spectrum disorder (ASD) refers to a constellation of social, language, and intellectual impairment broadly distributed over a range of functioning that historically includes autistic disorder, pervasive developmental disorder-not otherwise specified, and Asperger syndrome (APA, 2000). Impairment in reciprocal social interaction is a defining characteristic shared across the spectrum. To date, there are no efficacious pharmaceutical treatments to treat this core deficit; thus, behavioral and social skills interventions remain at the forefront (Wink, Erickson, & McDougle, 2010).
Social competence relies on awareness of the emotional and interpersonal cues of others, the ability to interpret such cues, to respond in an appropriate manner, and to be inherently motivated to engage in social interactions (Constantino, Przybeck, Friesen, & Todd, 2000; Gresham, 1986). Children with ASD lack social competence (Knott, Dunlop, & Mackay, 2006), preventing them from achieving appropriate developmental milestones and establishing interpersonal relationships, especially with peers (Krasny, Williams, Provencal, & Ozonoff, 2003). Impairment in interpersonal behavior in ASD can manifest in many ways and often includes fundamental impairment in social perception. For example, face processing is considered an important, if not necessary, component of social perception and effective social interaction. Neuropsychological studies report that individuals with ASD frequently show impairment in face processing (Adolphs, Sears, & Piven, 2001; Corbett et al., 2009; Critchley et al., 2000; Pierce, Muller, Ambrose, Allen, & Courchesne, 2001; Schultz et al., 2000). However, there is evidence that face processing can be improved through intervention (e.g., Corbett et al., 2003; Corbett et al., 2011; Faja et al., 2012; Tanaka et al., 2010).
Not surprisingly, difficulty engaging with others can contribute to increased arousal or stress in children and youth with ASD (e.g., Corbett et al., 2010; Lopata et al., 2008; Schupp, Simon, & Corbett, 2013). Level of arousal can be measured non-invasively via salivary cortisol, a stress hormone that reflects the activity of the hypothalamic pituitary adrenal (HPA) axis. In general, an increase in the level of cortisol in response to an event compared to an individual’s baseline value is suggestive of enhanced arousal, whereas a decrease is indicative of reduced stress in the given situation. In recent years, cortisol has been measured to assess changes in physiological arousal following interventions for individuals with ASD (Cashin, Browne, Bradbury, & Mulder, 2013; Corbett et al., 2011; Lopata, Volker, Putnam, Thomeer, & Nida, 2008; Viau et al., 2010).
Additionally, the context in which social interactions occur is important and may be particularly relevant in autism. For example, children with ASD who engage with peers on a playground often show significant physiological stress (Corbett, Schupp, Simon, Ryan, & Mendoza, 2010). Yet in another context, a paradigm based on social evaluative threat shown to activate the HPA axis in typically developing children, paradoxically, does not result in enhanced stress in ASD children (Corbett, Schupp, & Lanni, 2012; Jansen, Gispen-de Wied, van der Gaag, & van Engeland, 2003; Lanni, Schupp, Simon, & Corbett, 2012; Levine et al., 2012). Taken together, it appears that many children with ASD show enhanced arousal during conditions of social interaction and play; yet under performance-based conditions that include social judgment, the typical stress response is generally absent.
When considering factors of social functioning and stress in individuals with ASD, the impact of developmental factors on social behavior is critical. Many youth with ASD gain insight as they age, which includes increased awareness of their limited social competence (Knott et al., 2006). This awareness may in turn be associated with enhanced stress with unfamiliar peers (Corbett et al., 2010; Lopata et al., 2008) and increased anxiety resulting from repeated failure in social situations (Bellini, 2006).
Collectively, the previous findings emphasize the importance of considering peer influences, developmental factors, and the therapeutic context in better understanding the social challenges of youth with ASD. It is apparent that without intervention, impairment in social functioning in ASD is often intractable and lifelong. Thus, training in social skills is a critical component of intervention. While various social skills interventions for ASD exist, among the most efficacious are video modeling and peer-mediated approaches (Charlop-Christy, Le, & Freeman, 2000; Corbett, 2003; Kamps et al., 2002; Reichow & Volkmar, 2010). Video modeling, in which an individual watches skills presented on video and then imitates via active practice, can improve aspects of social functioning in children with autism (Charlop-Christy et al., 2000; Corbett, 2003; Nikopoulos & Keenan, 2007). Since the goal for socialization in children with ASD is for them to interact more appropriately with peers in natural settings, the inclusion of peer models to improve social exchanges is logical and is shown to be beneficial (Odom & Strain, 1984).
A novel approach for enhancing social competence is the use of theatre and acting techniques. Acting teaches social awareness, cognition, communication, perception, and expression; thereby, theatre may serve as a valuable tool to strengthen core socioemotional functioning in ASD. It has been shown that experience in acting leads to gains in empathy and theory of mind skills in typically developing children (Goldstein, 2011). Furthermore, theatre techniques have been used to teach empathy and social skills in medical and psychiatric training (Ballon, Kaur, Marks, & Cadenhead, 2007; Dow, Leong, Anderson, Wenzel, & Team, 2007). In fact, role-play exercise and games (H. Goldstein & Cisar, 1992) can significantly increase social skills. Thus, using theatrical approaches to target fundamental deficits in social and emotional functioning in youth with ASD holds promise. To date, the use of theatrical techniques, such as improvisational games and perspective training, have contributed to improvement in social functioning (Guli, 2004; Guli, Semrud-Clikeman, Lerner, & Britton, in press; Lerner, Mikami, & Levine, 2011).
In 2009, a theatre-based intervention research program was developed in the Social Emotional NeuroScience Endocrinology (SENSE) lab, which was subsequently named SENSE Theatre. SENSE Theatre incorporated behavioral strategies and theatrical techniques in a 10-week, peer-mediated model. In a pilot study of SENSE Theatre, neuropsychological, biological, and behavioral measures were assessed in 8 children with ASD before and after the intervention. The findings showed significant changes across several measures including improvements in face identification and theory of mind skills, as well as reductions in stress as measured by cortisol over the course of treatment (Corbett et al., 2011). The current investigation aimed to advance these findings while testing treatment dose using a 2-week summer camp model. Dose frequency (number of sessions) and duration (time period) were altered, whereas number of doses (episodes) and dose form (teaching) were similar (Warren, Fey, & Yoder, 2007). Based on the previous report (Corbett et al., 2011), it was hypothesized that children with ASD would demonstrate improvement in social interaction with peers as well as in social perception ability. Second, we hypothesized reductions in stress response over time. Other exploratory measures of home living included adaptive functioning and parental stress.
METHOD
Sixteen (16) youth attended the SENSE Theatre Summer Camp and 12 of them participated in the research, which included 9 boys and 3 girls (3 African-American, 7 Caucasian, and 2 Hispanic) between 8 and 17 years (mean age 12.17). Participants were diagnosed with autistic disorder (N=7), PDD-NOS (N=4), or Asperger syndrome (N=1) based on DSM-IV criteria (APA, 2000), confirmed by a clinical psychologist with expertise in ASD and corroborated by the Autism Diagnostic Observation Schedule-Generic (Lord, Rutter, DiLavore, & Risi, 1999). Intellectual functioning was measured with the Wechsler Abbreviated Scale of Intelligence (Wechsler, 1999) resulting in a mean IQ of 82 (74–118). Exclusion criteria included children with severe intellectual disability or frequent uncontrolled aggression. One participant failed to complete the majority of dependent measures and was dropped from the research protocol, leaving 11 in the study.
The Human Research Protection Program of Vanderbilt University approved the study. Following a thorough explanation of the research protocol, written informed consent was obtained from parents, and assent was obtained from child participants. The research component was offered for free and included two visits to Vanderbilt University for pre- and post-assessments. The visit and measurement schedule is provided in Table 1. The intervention and performances occurred at the University School of Nashville (USN), a K-12 school. The intervention, described below, also included typically developing peer actors from USN whose parents provided informed consent for them to undergo training to serve as peer models in the SENSE Theatre intervention. To promote objectivity, independent, research-reliable raters and biostatisticians completed the assessments, behavioral coding, and statistics described below.
Table 1.
Study Design
| Week | 1–2 Pre-Test |
1–2 Pre-Test |
3 Theatre |
4 Theatre |
5–6 Post-Test |
5–6 Post-Test |
|---|---|---|---|---|---|---|
| Location | Clinic | Play-ground | Theatre | Theatre | Clinic | Play-ground |
| Purpose |
1 Diagnosis 2 Baseline |
3 Peer Play Pre (P1) |
4 Interact | 4 Interact | 2 Post treatment |
3 Peer Play Post (P2) |
| Cortisol | Home (H1) Morning-2 Afternoon Evening |
Arrival 20 min 40 min 60 min |
Theatre 1 Begin and End | Theatre 2 Begin and End | Home (H2) Morning-2 Afternoon Evening |
Arrival 20 min 40 min 60 min |
Measures:
ADOS, WASI, SCQ,
NEPSY, ABAS, PSI, SRS,
Peer Interaction Paradigm Coding,
Companionship Scale
Note: H1 = Home sampling pre-test, Morning-2 = two samples, P1 = Playground 1 visit, min = minute, Begin = Beginning, H2 = Home sampling post-test, H2 = Home sampling post-test, P2 = Playground 2 visit. ADOS = Autism Diagnostic Observation Scale, WASI = Wechsler Abbreviated Scale of Intelligence, SCQ = Social Communication Questionnaire, ABAS = Adaptive Behavior Scale, Parenting Stress Index, SRS = Social Responsiveness Scale.
Diagnostic Measures
Autism Diagnostic Observation Schedule (ADOS) (Lord et al., 1999) is a semi-structured interview designed to assess behaviors indicative of autism, administered by an independent, research-reliable psychologist.
Wechsler Abbreviated Scale of Intelligence (WASI) (Wechsler, 1999) is a measure of cognitive ability that was used to obtain a quick, reasonable estimate of a child’s intellectual functioning. An estimated IQ ≥ 70 was required for participation in the study.
Social Communication Questionnaire (Rutter, Bailey, & Lord, 2003) is a screening tool for ASD. Scores of ≥ 15 are suggestive of ASD and scores of ≥ 22 are suggestive of autism.
Social Responsiveness Scale (Constantino & Gruber, 2005) is a 65-item questionnaire completed by care providers that includes characteristics of ASD. Total score as well as five treatment subscales were used in the analyses.
Neuropsychological Measures
NEPSY: Affect Recognition, Memory for Faces (Korkman, Kirk, & Kemp, 2007) was administered to assess changes in social perception. The raw total scores from the aforementioned subtests were used as dependent variables.
Parenting Stress Index (PSI) (Abidin, 2003) 3rd edition assesses the magnitude of stress as it relates to the parenting role and the parent/child dyad. The Total Score (PSI Total) and the Parent/Child Dysfunction (PSI-CD) scale were used.
Adaptive Behavior Assessment System (ABAS) (Harrison & T., 2000) assesses 10 areas of adaptive functioning. It was used to ascertain adaptive functioning in the home environment before and after intervention.
Companionship Scale (Bauminger, 2007) assesses a child’s verbal and nonverbal behavior along a 5-point Likert scale appearing from (1) 0%, (2) < 50%, (3) 50% (4) > 50% time, (5) 100% of time. The two scales that could be reliably tested during the intervention were eye contact and active involvement (amount of time the participant engages with a peer). The measure occurred during the break period of the First and Last day of camp.
Cortisol Sampling
Basal levels of salivary cortisol were collected from home by trained parents to ascertain the child’s diurnal baseline over four diurnal cycles (2 pre- and 2 post-treatment) using established methods (Corbett, Mendoza, Wegelin, Carmean, & Levine, 2008). Specifically, parents were instructed to collect the samples via passive drool 4 times per day (immediately upon waking, 30-minutes post-waking, in the afternoon, and over 2 consecutive days). All samples were obtained prior to eating or brushing teeth for the morning and evening samples, and at least 1 hour after eating for the afternoon sample. To evaluate physiological response, participants provided salivary samples at the beginning and end of the First and Last day of camp and playground visits. Once brought to the Vanderbilt University Hormone Assay Core lab, samples were centrifuged at 3000 rpm for 20 min to separate the aqueous component from mucins and other suspended particles. Salivary concentrations of cortisol were estimated in duplicate. Intra- and inter-assay coefficients of variation were 1.89 and 2.21, respectively.
The Peer Interaction (PI) Paradigm consisted of a 20-min playground interaction with two novel peers pre- and post-intervention. One peer was a confederate with the role of eliciting play during prompted time intervals. The other child was a typically developing child with no specific directions. Interactions were video recorded using four professional 70 Sony PTZ remotely operated cameras housed in glass cases and affixed to the four corners of the external fence of the 130 ft × 120 ft playground. Audio communication was obtained by Sennheiser body pack and Audio-Technica transmitters and receivers, which functioned as battery-operated microphones that were clipped to the shirt of each child. The established protocol was followed (Corbett et al., 2010); however, only Cooperative Play (participant engaged in reciprocal play with at least one child) was used for the last 5 (T4) minutes of play. Since cortisol detection in saliva has a 20-min lag time, samples were taken to correspond to specific points in time. For the current protocol, samples obtained 40 min after initiation of the play protocol corresponded to the T4 play Cooperative Play period. The Observer XT was used for the collection, analysis, and presentation of observational data (Noldus, 2008).
SENSE Theatre Camp
The SENSE Theatre program is peer-mediated, embedded in play, and performance-based. Participants with ASD were paired with typically developing actors of similar age who served as peer models and co-actors in a play. Experience working with the ASD population and severity of the participant’s symptom profile also influenced the matching of participants and peers. The SENSE Theatre approach emphasizes ten core objectives that are taught, modeled, and incorporated using direct teaching, several case examples, and ongoing supervised experience. The peers are explicitly instructed on ten core objectives that aim to improve features of autism symptomology. The core objectives and target behaviors include: (1) provide social support (build trust, reduce stress), (2) create an enjoyable environment (facilitate social play), (3) model warm social interaction (reciprocal social interaction with peers), (4) enhance motivation (increase social initiation), (5) engage in directed communication (enhance verbal to-and-fro conversation), (6) use nonverbal communication (improve eye contact, facial expressions, and gestures), (7) engage in imaginative play (develop imagination), (8) use empathic responding (develop empathy), (9) support active learning (encourage novelty and participation), and (10) advance individual learning (integrate social learning with behavior).
The daily schedule included 2 weeks of afternoon camp held Monday through Friday from 1:00 – 5:00 pm. The schedule for each day was sent to the parents of the participants in advance and was presented daily on a large white board. On the first day of camp following circle time introductions, mock auditions were held to break-the-ice and allow everyone to get to know each other. Next, participants engaged in peer-tutored theatre games (e.g., mirroring), imaginative play (e.g., pretending to be different animals), scripting (e.g., speaking lines from a scene in a play), role-playing (e.g., acting out different roles and situations with costumes), and movement with music games (e.g., freeze tag to music in slow motion). Several of these exercises ultimately blended into scenes in the play. On the second day, roles were assigned by the director, basic lines from the play were taught, and simple blocking of scenes was introduced. During the remaining days of camp (3–10), engagement in interactive theatre games faded while more time was devoted to role playing, character development, and rehearsing the play. Rehearsals included group run-through, one-on-one role-play, as well as assigned homework to develop ideas for their characters (e.g., What makes your character happy? What does he like to wear?). The second-to-last day of camp also included a technical rehearsal that involved working with lighting and set changes. The last day of camp included a dress rehearsal for invited University co-workers to allow all actors to practice before a live audience. The end of the 2-week camp culminated in participants and peers putting on two evening pubic performances of a 45-minute play that included some lyrical writing and songs.
Peer Training included 3-days of training on autism, behavioral intervention techniques, and the SENSE Theatre approach. All peers participated in training. Peers learned about the clinical presentation of ASD, which included meeting both a child and an adult with ASD. The peers learned several behavioral intervention techniques using handouts of each of the terms, carefully described definitions, and catch phrases to aid memory. The behavioral techniques were presented using live and video exemplars and included: positive reinforcement, modeling, shaping, fading, redirection, prompting, and extinction. For example, the peer observed how a child with ASD was shown the way to speak directly to another actor (modeling), was praised for his initial attempt (positive reinforcement), and received ongoing encouragement for each successive attempt (shaping), all the while reducing verbal prompts (fading). The peer-mediated intervention followed a hierarchical support model that involved initial active support with gradual fading as skills were acquired. The clinical staff to ASD child ratio was 1-to-3, and the trained peer to ASD child ratio was essentially 1-to-1. Initially, clinical staff provided more direct supervision; once peers established rapport and competence, support was faded. Typically developing peers ultimately faded their own support, allowing participants with ASD to gain greater independence.
Training Fidelity was measured by completion of an exam pertaining to knowledge of autism and behavioral methods delivered over the 3 days. The exam was administered at the beginning of the first day of training and the end of the last day of training. Initial and post-training scores were high (89% and 91%, respectively), reflecting a high degree of knowledge.
Treatment Fidelity was assessed to ensure consistent implementation of the behavioral approaches by independent raters during the 2nd and 8th days of camp. Peer fidelity was rated based on a behaviorally anchored Likert scale as follows: (1) almost none, (2) a few occasions, (3) some, (4) good demonstration of behavior, (5) optimal demonstration of the skills. Peers demonstrated an increase in strategy implementation from the beginning to the end of treatment for positive reinforcement (pre=3.40 SD=1.52, post=4.60 SD=0.55, p=0.07) and modeling (pre=2.60 SD=1.14, post=4.20 SD=0.84, p=0.05). Use of nonverbal behavior, prompting, and shaping stayed around the same mean level of 4.20, 3.75, and 3.67, respectively.
Enactment Fidelity, which is the extent to which behaviors, skills, and strategies are implemented by participants in real life settings, was used to demonstrate whether or not parents used the videos (Nigg, Allegrante, & Ory, 2002). Specifically, implementation of video modeling was documented via home logins using a unique identifier and password that allowed families to access the videos. Video modeling segments were conducted by peer actors who performed the participants’ roles and target behaviors on video. The video segments were placed on the Vanderbilt Kennedy Center website with a url that was not accessible by search engines. Participants were instructed to watch and role-play the videos 15 minutes daily to aid in the acquisition, maintenance, and generalization of skills. Each child had approximately 8–10 brief videos (lasting 30 to 120 seconds each) to watch daily over the course of the intervention. Logins and logouts served as indication of adherence to video modeling procedures. Results showed that 15 of the 16 camp participants (94%) and all research participants (12 participants) utilized the online video resources, with a mean watch time of 46.28 minutes (SD=66.51), with a large positively skewed distribution.
Statistical Analysis
This investigation used a pretest-posttest design for within-group comparisons. Salivary cortisol measurements were positive and skewed toward large values; thus, log transformation was performed to achieve approximate normality, and the transformed values were used for all cortisol analyses. Pre-specified pairwise comparisons were achieved by using a nonparametric Wilcoxon signed rank test. Because Cohen’s d was not appropriate for nonparametric analyses, instead we assessed effect sizes by calculating d statistic for pairwise comparisons (Dunlap, Cortina, Vaslow, & Burke, 1996). Statistical software R (version 2.13.0, www.r-project.org) was used for all data analysis. Reported p values were two-sided, and a p value of less than 0.05 was considered to be statistically significant.
RESULTS
Social Behavior in Setting
Based on independent raters using two measures from the Companionship Scale, the children with ASD demonstrated an increase in active involvement with peers (pre=7.85 SD=4.51; post=10.62 SD=4.35, p=.027). The finding confirms the hypothesis and supports the primary aim of the intervention – to improve social interaction. There was no significant difference in the amount of eye contact (pre=2.77 SD=1.64; post=3.00 SD=1.41, p=0.553).
Social and Affect Perception
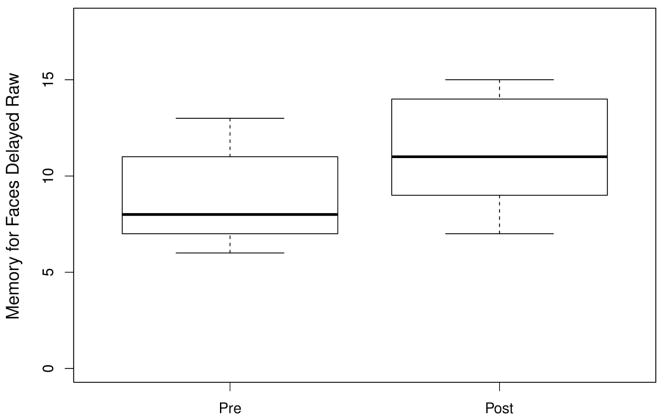
Based on neuropsychological measures, there was a significant difference between pre- and post-testing for Delayed Memory for Faces (see Figure 1 and Table 2), with a large effect size (Cohen, 1988) indicating improvement in face identification memory. There was also a significant difference between Memory for Faces Delayed, the Difference Score for Memory for Faces Immediate versus Delayed, and a trend for Immediate Memory for Faces, further supporting the improvement in the ability to identify and remember faces.
Figure 1.
Pre- post-treatment for Memory for Faces Delayed in children with ASD.
Table 2.
Social Perception and Functioning, Home Adaptive Functioning, and Parental Stress Measures
| Measure | Pre-Test Mean |
Pre-Test SD |
Post-Test Mean |
Post-Test SD |
p value | d statistic |
|---|---|---|---|---|---|---|
| Social Perception | ||||||
| Memory for Faces Immediate (MF) | 8.27 | 2.33 | 9.91 | 3.59 | 0.095 | −0.51 |
| Memory for Faces Delayed (MFD) | 8.82 | 2.52 | 11.27 | 2.9 | 0.002 | −0.89 |
| MF vs. MFD | 8.45 | 2.77 | 10.82 | 1.94 | 0.041 | −0.99 |
| Affect Recognition | 23.4 | 4.95 | 24.3 | 4.81 | 0.512 | −0.18 |
| Social Functioning* | ||||||
| SRS Awareness | 13.17 | 3.17 | 12.25 | 2.96 | 0.043 | 0.23 |
| SRS Communication | 33.67 | 5.65 | 30.42 | 6.71 | 0.068 | 0.52 |
| SRS Cognition | 19.33 | 3.7 | 14.08 | 3.5 | 0.001 | 1.46 |
| SRS Total | 100.33 | 14.82 | 89.00 | 15.6 | 0.001 | 0.74 |
| Adaptive (ABAS) | ||||||
| ABAS Communication | 50.73 | 8.96 | 59.92 | 9.01 | 0.125 | −0.28 |
| ABAS Home Living | 36.64 | 13.37 | 41.92 | 12.06 | 0.036 | −0.34 |
| ABAS Self-Care | 54.18 | 11.75 | 58.17 | 7.86 | 0.049 | −0.29 |
| ABAS Self- Direction | 39.55 | 14.81 | 43.36 | 10.31 | 0.169 | −0.22 |
| ABAS Social | 43.45 | 11.63 | 44.45 | 8.76 | 0.767 | −0.09 |
| Parent Stress (PSI) | ||||||
| PSI Total | 91.50 | 21.48 | 82.33 | 18.23 | 0.009 | 0.43 |
| Parent-Child Dysfunction | 24.83 | 6.07 | 20.83 | 4.24 | 0.006 | 0.71 |
Note: SD = Standard Deviation, SRS = Social Responsiveness Scale, (ABAS) Adaptive Behavior Assessment System, PSI = Parent Stress Inventory,
Lower scores denote improvement.
Social Functioning
Regarding other areas of social functioning, significant differences were found on the SRS Total score, Social Awareness, and Social Cognition with medium to large effect sizes, respectively (Cohen, 1988). Based on these findings, the primary hypothesis regarding improvement in social functioning was confirmed.
There were significant changes in adaptive skills; specifically, Home Living (HL) and Self-Care (SC) (see Table 2), which also were highly correlated with the child’s improvement in face memory (HL p=0.001, r=.85; SC p=0.007, r=0.76). The remaining ABAS measures did not reach statistical significance. Also, parents reported a significant decrease in total stress, including reduction related to the level of dysfunction in the parent-child relationship.
Cortisol Profile
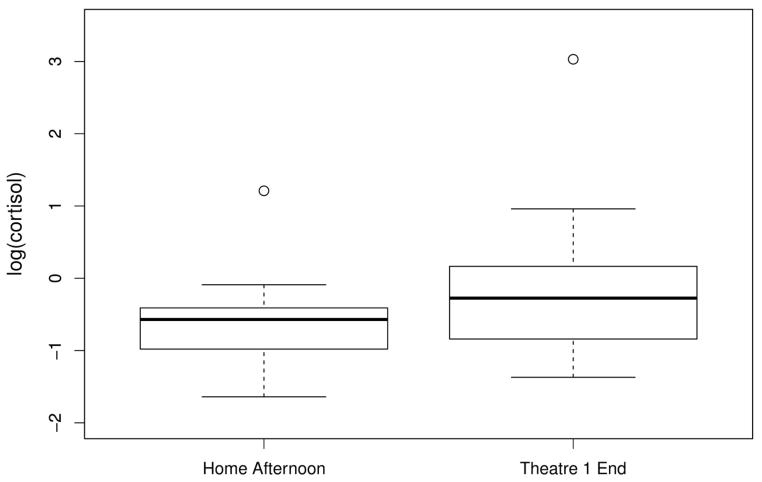
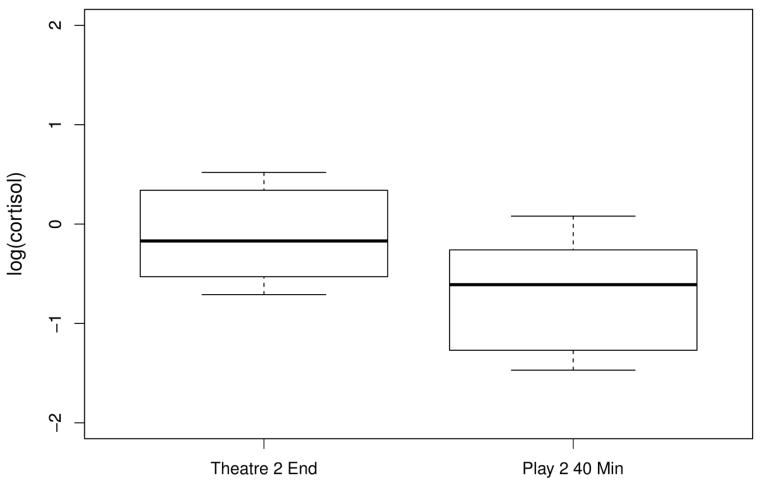
Salivary cortisol was measured to obtain: 1) home values over 2 diurnal cycles before (Home 1) and after (Home 2) the intervention; 2) response to the treatment setting at the beginning and end of the first (Theatre 1) and last (Theatre 2) day of camp, and 3) response to play outside the setting at the playground before (Play 1) and after (Play 2) camp. There were no significant differences noted for the Home values or between Home and Play 1 samples (p=>0.05). There was a significant rise of salivary cortisol on the first day of camp compared to afternoon home values p=0.02, d=−0.72 suggesting enhanced physiological arousal in the new setting (see Figure 2). Conversely, there were significant reductions in cortisol between the first day of camp (Theatre 1) and the second playground (Play 2) 40-min p=0.004, d=0.65 and 60-min cortisol values p=0.006, d=0.62. Finally, there were significant reductions from the last day of camp (Theatre 2) and the second playground 40-min p=0.01, d=1.13 and 60-min p=0.002, d=1.24 (see Figure 3) suggesting that as a group, the participants showed reduced physiological arousal upon re-exposure to the playground.
Figure 2.
Comparison between log cortisol from home and first day of theatre camp.
Figure 3.
Comparison between log cortisol from theatre end to the playground 2 visit.
Playground Interactions
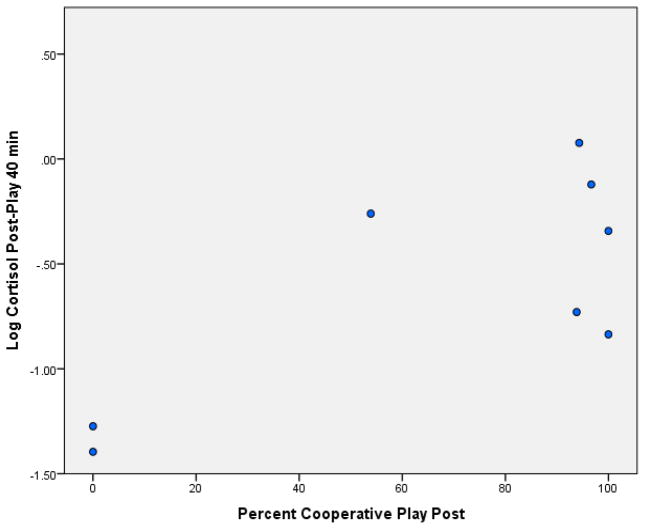
Results indicated no significant difference for Cooperative Play between T1 Pre (mean 31.79 SD=42.06) and Post (mean 41.37, SD 44.96, p=0.209) or between T4 Pre (mean 72.07, SD=34.25), and Post (56.57, SD=45.54) p=0.309. Examination of the standard deviations emphasizes the significant variability in social response across participants. To examine biobehavioral profiles, comparisons were made between engagement with peers and stress responsivity using Pearson product correlations. Explicitly, the duration of Cooperative Play for the pre-Playground (P1) and the post-playground (P2) were explored during the final 5-min time period T4 and the 40-min cortisol values. There was no significant association between T4 and amount of Cooperative Play during the P1 p=0.84, r=−0.073. However, there was a significant positive correlation between P2 Cooperative Play and 40-min cortisol p=0.034, r=0.745, indicating a strong association between social engagement and stress responsivity. The finding demonstrates a strong positive relationship between the amount of social engagement and arousal. Taken together, it appears that while the children with ASD showed a similar amount of cooperative play behavior with the new peer from the first to the second playground visit, there was less physiological arousal upon re-exposure to the playground.
DISCUSSION
A 2-week summer camp model of a theatrical intervention program was tested, which was comparable to the previous treatment (Corbett et al., 2011) in many aspects (e.g., behavioral approach, peer-mediation, theatre techniques, video modeling, afternoon delivery, and treatment dose) but with some differences (duration of training and treatment, a more homogeneous and slightly larger sample). The primary aims were to measure: 1) social perception, cognition, and amount of engagement with peers within and outside the treatment context, and 2) physiological stress in the child with ASD. Results revealed significant differences in measures of social functioning, stress responsivity, and adaptive skills.
Regarding social perception, youth with ASD showed significant improvement in face perception. Although the participants did not receive direct instruction in face processing, they improved in their ability to identify and remember facial stimuli. This finding replicates previous report (Corbett et al., 2011) of improvement on this measure of social perception following the intervention. While there are many studies showing that face processing is impaired in autism (e.g., Corbett et al., 2009; Critchley et al., 2000; Pierce et al., 2001), few studies have shown improvement in this important social skill (Corbett & Abdullah, 2005; Faja et al., 2012; Tanaka et al., 2010) especially without direct skills training. Improvements in social perception also were observed outside the treatment setting evidenced by changes in social awareness. Presumably the face-to-face contact and active practice of reciprocal social interaction with peers contributed to the improvement in perceptual skills. Even so, such exposure and practice did not extend to emotion recognition, similar to the previous study (Corbett et al., 2011). Thus, this skill may need to be trained explicitly (Corbett, 2003).
Participants also demonstrated improvement in social cognition or the ability to interpret the social meaning of engaging with others. In concert, the amount of time the participants chose to engage actively with familiar peers increased over the course of the intervention. These findings support the hypothesis and primary aim of the intervention – to enhance reciprocal social interaction with peers. Ostensibly, engaging with peers in a reciprocal, theatrical way contributes to gains in the interpretation of social cues.
Amidst significant improvement in social skills within the treatment and home setting and on neuropsychological measures, such gains did not significantly alter the amount of time participants spent with novel peers on a playground. The process of increasing socialization occurred naturally in the intervention setting over 2 weeks. However, when the participants were subsequently exposed to novel peers in a familiar setting (playground), they did not engage to a greater extent. As in the theatre experience, social engagement may need to be shaped over time allowing the child to get to know new members and settings. In other words, social familiarity must be considered in socialization, especially in autism. Some of the ASD participants expressed an interest to see and play with the peers they had previously met. There was a certain expectancy and formed association between setting and peer on the part of the children with ASD, which may have influenced the amount of social interaction.
One way to augment engagement in youth with autism may be to shape the process with both novel and familiar peers. The concentrated intervention appears helpful in improving social perception, cognitive and social interaction skills, and generalizing these gains to the home environment; however, a more extended intervention may be necessary to facilitate the transfer of skills to novel peers.
Previous research has shown that despite initial elevations in stress, as the children with ASD progress in the theatre intervention and habituate to the environment, cortisol levels decrease (Corbett et al., 2011). The current study showed a similar pattern with a rise in cortisol on the first day, which declined over time, suggesting that the children adapted to the environment. It is important to note that samples were not collected in the middle of the treatment, which would have allowed more careful characterization of the cortisol pattern over the course of treatment. Stress responsivity also was evaluated at the follow-up peer interaction playground, and participants showed even lower cortisol levels compared to the beginning and end of camp. All samples were conducted during the same time of day; thus diurnal decline is not an appropriate explanation. It is unclear if prior exposure to the playground contributed to the lower cortisol levels. To investigate further, we analyzed the relationship between the amount of social interaction on the playground and cortisol values. A strong, positive correlation existed between the amount of time engaged in cooperative play and higher cortisol levels (Figure 4). Conversely, children with low levels of cortisol were not interactive and would be aptly characterized as aloof (Wing & Gould, 1979).
Figure 4.
Correlation between log cortisol and cooperative play during post-treatment playground interaction.
Converging findings from our previous reports reveal a biobehavioral profile linking cortisol levels with social engagement in a proposed neuroendocrine spectrum model (Corbett et al., 2012). Children with ASD show a rise in cortisol during initial exposure to novel peers during the playground studies (Corbett et al., 2010; Schupp et al., 2013) and on the first day of the intervention; thus, the higher cortisol associated with more social interaction from the current study implies that increased arousal is common and may be necessary. While it is initially easy to assume that elevated cortisol is deleterious and reflects a maladaptive stress response, it may be argued that under some conditions higher cortisol may be adaptive. It is well established in experimental psychology that a moderate level of arousal is necessary for optimal performance (Yerkes & Dodson, 1908). As illustrated in the Yerkes and Dodson model, too little arousal is just as detrimental as too much arousal. Perhaps in children with ASD, a higher level of arousal or stress may be initially necessary to engage socially with novel peers. As illustrated in Figure 4, children with the highest levels of cortisol were cooperatively playing with peers, whereas those with the lowest cortisol were completely disengaged. While these ideas are intriguing, there is likely a fine line between arousal and acute stress; therefore, it is unclear what constitutes an optimal level of arousal for children with ASD. Moreover, from these data, we are unable to determine if social engagement results in an increase in cortisol, or if the rise in cortisol is necessary for children with ASD to interact with novel peers.
To ascertain the impact of the intervention on the home environment, adaptive functioning and parental stress were explored. Improvements were noted in the participants’ home living and self-care skills. These advances infer collateral improvement and generalization to the home environment. Arguably in typical development, independent self-care requires a certain level of social awareness and motivation influenced by social gains. Enhanced social awareness of peers in the theatre may result in enhanced self-awareness; thereby, self-care. This suggests that the greater awareness of social cues and frequent engagement of peers may contribute to increased awareness of self, hygiene, and related behaviors.
It is well established that parents of children with ASD experience significant stress (Hayes & Watson, 2012). Thus, parents were asked to rate their level of stress prior to (during pre-assessment within 10 days prior to camp) and following (during post-assessment within 10 days following camp) the intervention. Parents reported a sizeable reduction in overall stress as well as stress associated with their child following participation in the treatment. Reports have shown an inverse relationship between parent stress and their children’s adaptive functioning (Hall & Graff, 2011) and social relatedness (Davis & Carter, 2008). Reduction in parental stress may be related to improvement in home living, self-sufficiency, and social functioning in the child. This notion is supported by a consistent endorsement of items by parents related to an increased awareness of their child’s capabilities. While we primarily treat the child, the concomitant change in the parent’s life emphasizes that the family system can be positively impacted by gains in social functioning. Reduction in parental stress may also be impacted by the public nature of the theatrical program. At the conclusion of the intervention, the children participate in a public performance allowing their parents to observe them in a positive, supportive, and entertaining setting. The uplifting experience of witnessing their child’s success may modify their perspective and thereby dampen parental stress.
Strengths of the study include the treatment itself, which combines established behavioral techniques with novel, promising theatrical approaches that allow social skills to be practiced with peers. The design allowed comprehensive assessment of biobehavioral profiles of youth with ASD across home, clinic, treatment, and natural settings. Improvements in social perception and engagement were corroborated through the use of various instruments and methods showing moderate to strong effect sizes. Despite encouraging outcomes, limitations of the study include a rather small sample size. Testing of a comparison group would strengthen the findings. In addition, cortisol sampling throughout the intervention would have allowed more careful examination of the physiological response patterns in the participants with ASD. It is apparent that additional studies are needed to corroborate findings and to examine the importance of peer familiarity and the relationship to engagement and stress responsivity. The optimal level of arousal, duration of treatment, and the limits of generalizability are meaningful next steps.
Future studies also will help to evaluate the significant factors that contribute to the observed improvements in social functioning in the participants with ASD. Specifically, forthcoming endeavors will more adequately identify the most effective components of the intervention by comparing treatment with and without key elements in a titrated approach. It is likely that the inclusion of typically developing peers is central to the effectiveness of the intervention. The use of peer-mediation has been shown to be an effective strategy for improving a variety of skills in individuals with ASD (Odom & Strain, 1984). It is also believed that the theatrical approaches, including scripted social engagement using a play, improvisational games, and active engagement of reciprocal social behavior via performance with others, provide a novel albeit effective format for practicing social skills. Moreover, it is hypothesized that video modeling contributes to the maintenance and generalization of skills (Corbett & Abdullah, 2005). Nevertheless, it is unclear how critical the video modeling, setting, and musical components are in contributing to the observed changes in the participants with ASD.
Next steps for future development of the program fall into three primary aims related to the participant, the parent, and the peers who engage the child. While many of the participants appear to show improvements in social functioning, it is unclear if the enhanced awareness will hold up over time and to what settings it will generalize. As with many interventions for children with autism, the gains made are often context dependent in terms of individuals and setting (Belchic & Harris, 1994; Honig & McCarro, 1988). One strategy for extending the social skills to other children outside would be to introduce new peers throughout the course of treatment. For example, multiple peers could train each participant with ASD, which has been shown to enhance generalization (Pierce & Schreibman, 1997). Additionally, enhancing peer-mediated interventions in the child’s natural environment, such as school, may help to improve carry-over effects from the theatre setting to the child’s everyday world (Paul, 2008). Finally, directly teaching verbal initiation to children with ASD has been shown to enhance generalization to the school environment (Koegel, Kuriakose, Singh, & Koegel, 2012). It has been suggested that an important consideration in peer-mediated interventions is the need to consider the expectations of peers (DiSalvo & Oswald, 2002). While positive effects have been reported for peers who participate in interventions (Pierce & Schreibman, 1995), changing the negative expectations of peers in the child’s natural environment may be necessary to facilitate generalization of skills (DiSalvo & Oswald, 2002).
Whereas the reduction in stress reported by the parents following the intervention is intriguing, several unanswered questions remain. For example, do the effects hold up over time or are they an artifact of seeing their child perform on stage in a reinforcing setting? In other words, does the experience result in a shift in their perception of the child’s abilities and thereby contribute to stress reduction related to the new way of thinking about the child? Alternatively, is it a transitory state that fades with time as the child struggles to adapt to the dynamic social world? These questions can best be answered by following both parent and child over time to better understand the depth and duration of the change.
Finally, while there is evidence that the peers are positively impacted by serving as a therapeutic agent in a peer-mediated intervention (Pierce & Schreibman, 1995), we have not investigated these presumed changes in the current intervention. The fact that some peers have served in the program more than once suggests that the experience is positive and meaningful in some way. Presently, it is not known how the peers are impacted, to what extent it modifies their point of view or behavior, and the status of any changes in their own social cognition, adaptive skills, or other behaviors. Thus, the explicit examination of the peers warrants further study.
In summary, the investigation of the SENSE Theatre peer-mediated, interactive social skills program corroborates and extends previous findings (Corbett et al., 2011) showing improvement in core social deficits in ASD using a short-term, summer camp model that allows extensive practice of social interactions with peers. Concomitant gains in adaptive functioning and reductions in parental stress highlight the far-reaching implications that social impairment and thus improvement plays in the lives of children with ASD and their families.
Acknowledgments
Grant Sponsor: Martin McCoy-Jesperson Discovery Grant in Positive Psychology
Grant Sponsor: National Institute of Mental Health; Grant Number: R01 MH085717
Grant Sponsor: National Institute of Child Health and Human Development; Grant Number: P30 HD15052
Scholarships were provided by the Vanderbilt Kennedy Center, Autism Speaks Baker Summer Camp Scholarship, and donations to SENSE Theatre. We are grateful for the generous support of University School of Nashville, Emelyne M. Bingham, M.A., and Amy Weitlauf, Ph.D.
Footnotes
Disclosures: Blythe Corbett, Ph.D. is founder of SENSE Theatre 501(c)(3) but does not receive any financial compensation from the organization. Additionally, independent, research-reliable raters and biostatisticians completed the assessments, behavioral coding, and statistics.
References
- Abidin RR. The Parenting Stress Index. Lutz, FL: Psychological Assessment Resources, Inc; 2003. [Google Scholar]
- Adolphs R, Sears L, Piven J. Abnormal processing of social information from faces in autism. J Cogn Neurosci. 2001;13(2):232–240. doi: 10.1162/089892901564289. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision (DSM-IV-TR) [Google Scholar]
- Ballon JS, Kaur T, Marks II, Cadenhead KS. Social functioning in young people at risk for schizophrenia. Psychiatry Research. 2007;151(1–2):29–35. doi: 10.1016/j.psychres.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauminger N. Brief report: group social-multimodal intervention for HFASD. J Autism Dev Disord. 2007;37(8):1605–1615. doi: 10.1007/s10803-006-0246-3. [DOI] [PubMed] [Google Scholar]
- Belchic JK, Harris S. The use of multiple peer exemplars to enhance the generalization of play skills to the siblings of children with autism. Child and Family Behavior Therapy. 1994;16:1–25. [Google Scholar]
- Bellini S. The development of social anxiety in adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2006;21(3):138–145. [Google Scholar]
- Cashin A, Browne G, Bradbury J, Mulder A. The effectiveness of narrative therapy with young people with autism. J Child Adolesc Psychiatr Nurs. 2013;26(1):32–41. doi: 10.1111/jcap.12020. [DOI] [PubMed] [Google Scholar]
- Charlop-Christy MH, Le L, Freeman KA. A comparison of video modeling with in vivo modeling for teaching children with autism. J Autism Dev Disord. 2000;30(6):537–552. doi: 10.1023/a:1005635326276. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Constantino JN, Gruber CP. Social Responsiveness Scale. Los Angeles: Western Psychological Services; 2005. [Google Scholar]
- Constantino JN, Przybeck T, Friesen D, Todd RD. Reciprocal social behavior in children with and without pervasive developmental disorders. J Dev Behav Pediatr. 2000;21(1):2–11. doi: 10.1097/00004703-200002000-00002. [DOI] [PubMed] [Google Scholar]
- Corbett BA. Video Modeling: A window into the world of autism. The Behavior Analyst Today. 2003;4(3):367–377. [Google Scholar]
- Corbett BA, Abdullah M. Video Modeling: Why does it work for children with autism? Journal of Early and Intensive Behavior Intervention. 2005;2(1):2–8. [Google Scholar]
- Corbett BA, Carmean V, Ravizza S, Wendelken C, Henry ML, Carter C, Rivera SM. A functional and structural study of emotion and face processing in children with autism. Psychiatry Res. 2009;173(3):196–205. doi: 10.1016/j.pscychresns.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Gunther JR, Comins D, Price J, Ryan N, Simon D, Schupp CW, Rios T. Brief report: theatre as therapy for children with autism spectrum disorder. J Autism Dev Disord. 2011;41(4):505–511. doi: 10.1007/s10803-010-1064-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Mendoza S, Wegelin JA, Carmean V, Levine S. Variable cortisol circadian rhythms in children with autism and anticipatory stress. Journal of Psychiatry and Neuroscience. 2008;33(3):227–234. [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Schupp CW, Lanni KE. Comparing biobehavioral profiles across two social stress paradigms in children with and without autism spectrum disorders. Mol Autism. 2012;3(1):13. doi: 10.1186/2040-2392-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Schupp CW, Simon D, Ryan N, Mendoza S. Elevated cortisol during play is associated with age and social engagement in children with autism. Mol Autism. 2010;1(1):13. doi: 10.1186/2040-2392-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Critchley HD, Daly EM, Bullmore ET, Williams SC, Van Amelsvoort T, Robertson DM, Rowe A, Phillips M, McAllonan G, Howlin P, Murphy DG. The functional neuroanatomy of social behaviour: changes in cerebral blood flow when people with autistic disorder process facial expressions. Brain. 2000;123(Pt 11):2203–2212. doi: 10.1093/brain/123.11.2203. [DOI] [PubMed] [Google Scholar]
- Davis NO, Carter AS. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: associations with child characteristics. J Autism Dev Disord. 2008;38(7):1278–1291. doi: 10.1007/s10803-007-0512-z. [DOI] [PubMed] [Google Scholar]
- DiSalvo CA, Oswald DP. Peer-Mediated Interventions to increase the social interaction of children with autism: Consideration of peer expectancies. Focus on Autism and Other Developmental Disabilities. 2002;17(4):198–207. [Google Scholar]
- Dow A, Leong D, Anderson A, Wenzel R, Team VCUTM. Using Theater to Teach Clinical Empathy: A Pilot Study. Journal of General Internal Medicine. 2007;22(8):1114–1118. doi: 10.1007/s11606-007-0224-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measured designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Faja S, Webb SJ, Jones E, Merkle K, Kamara D, Bavaro J, Aylward E, Dawson G. The effects of face expertise training on the behavioral performance and brain activity of adults with high functioning autism spectrum disorders. J Autism Dev Disord. 2012;42(2):278–293. doi: 10.1007/s10803-011-1243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein H, Cisar CL. Promoting interaction during sociodramatic play: teaching scripts to typical preschoolers and classmates with disabilities. J Appl Behav Anal. 1992;25(2):265–280. doi: 10.1901/jaba.1992.25-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR. Correlations among social-cognitive skills in adolescents involved in acting or arts classes. Mind, Brain & Education. 2011;5:97–103. [Google Scholar]
- Gresham FM. Conceptual and definitional issues in the assessment of children’s social skills: Implications for classification and training. Journal of Clnical Child Psychology. 1986;15(1):3–15. [Google Scholar]
- Guli LA. Dissertation. University of Texas; Austin: 2004. The effects of creative drama based intervention for children with deficits in social perception. [Google Scholar]
- Guli LA, Semrud-Clikeman M, Lerner MD, Britton N. Social Competence Intervention Program (SCIP): A pilot study of a creative drama program for youth with social difficulties. The Arts in Psychotherapy in press. [Google Scholar]
- Hall HR, Graff JC. The relationships among adaptive behaviors of children with autism, family support, parenting stress, and coping. Issues Comprehensive PEdiatric Nursing. 2011;34(1):4–25. doi: 10.3109/01460862.2011.555270. [DOI] [PubMed] [Google Scholar]
- Harrison PLTO. Adaptive Behavior Assessment System. San Antonio, TX: Psychological Corporation; 2000. [Google Scholar]
- Hayes SA, Watson SL. The Impact of Parenting Stress: A Meta-analysis of Studies Comparing the Experience of Parenting Stress in Parents of Children With and Without Autism Spectrum Disorder. J Autism Dev Disord. 2013;43(3):629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Honig AS, McCarro PA. Prosocial behaviors of hendicapped and typical peers in an integrated preschool. Early Child Development and Care. 1988;33:113–125. [Google Scholar]
- Jansen LM, Gispen-de Wied CC, van der Gaag RJ, van Engeland H. Differentiation between autism and multiple complex developmental disorder in response to psychosocial stress. Neuropsychopharmacology. 2003;28(3):582–590. doi: 10.1038/sj.npp.1300046. [DOI] [PubMed] [Google Scholar]
- Kamps D, Royer J, Dugan E, Kravits T, Gonzalez-Lopez A, Garcia J, Carnazzo K, Morrison L, Kane LG. Peer training to facilitate social interaction for elementary students with autism and their peers. Exceptional Children. 2002;68(2):173–187. [Google Scholar]
- Knott F, Dunlop AW, Mackay T. Living with ASD: how do children and their parents assess their difficulties with social interaction and understanding? Autism. 2006;10(6):609–617. doi: 10.1177/1362361306068510. [DOI] [PubMed] [Google Scholar]
- Koegel LK, Kuriakose S, Singh AK, Koegel RL. Improving generalization of peer socialization gains in inclusive school settings using initiations training. Behav Modif. 2012;36(3):361–377. doi: 10.1177/0145445512445609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkman M, Kirk U, Kemp S. NEPSY. 2. San Antonio, TX: Harcourt Assessment; 2007. [Google Scholar]
- Krasny L, Williams BJ, Provencal S, Ozonoff S. Social skills interventions for the autism spectrum: essential ingredients and a model curriculum. Child Adolesc Psychiatr Clin N Am. 2003;12(1):107–122. doi: 10.1016/s1056-4993(02)00051-2. [DOI] [PubMed] [Google Scholar]
- Lanni KE, Schupp CW, Simon D, Corbett BA. Verbal ability, social stress, and anxiety in children with Autistic Disorder. Autism. 2012;16(2):123–138. doi: 10.1177/1362361311425916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner MD, Mikami AY, Levine K. Socio-dramatic affective-relational intervention for adolescents with asperger syndrome & high functioning autism: pilot study. Autism. 2011;15(1):21–42. doi: 10.1177/1362361309353613. [DOI] [PubMed] [Google Scholar]
- Levine TP, Sheinkopf SJ, Pescosolido M, Rodino A, Elia G, Lester B. Physiologic Arousal to Social Stress in Children with Autism Spectrum Disorders: A Pilot Study. Res Autism Spectr Disord. 2012;6(1):177–183. doi: 10.1016/j.rasd.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopata C, Volker MA, Putnam SK, Thomeer ML, Nida RE. Effect of social familiarity on salivary cortisol and self-reports of social anxiety and stress in children with high functioning autism spectrum disorders. J Autism Dev Disord. 2008;38(10):1866–1877. doi: 10.1007/s10803-008-0575-5. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S. Autism Diagnostic Observation Schedule-WPS. Los Angeles, CA: Western Psychological Services; 1999. [Google Scholar]
- Nigg CR, Allegrante JP, Ory M. Theory-comparison and multiple-behavior research: common themes advancing health behavior research. Health Educ Res. 2002;17(5):670–679. doi: 10.1093/her/17.5.670. [DOI] [PubMed] [Google Scholar]
- Nikopoulos CK, Keenan M. Using video modeling to teach complex social sequences to children with autism. J Autism Dev Disord. 2007;37(4):678–693. doi: 10.1007/s10803-006-0195-x. [DOI] [PubMed] [Google Scholar]
- Noldus . The Observer XT. Vol. 10.5. Wageningen, The Netherlands: Noldus Information Technology; 2008. [Google Scholar]
- Odom SL, Strain PS. Peer-mediated approaches to promoting children’s social interaction: a review. Am J Orthopsychiatry. 1984;54(4):544–557. doi: 10.1111/j.1939-0025.1984.tb01525.x. [DOI] [PubMed] [Google Scholar]
- Paul R. Interventions to improve communication in autism. Child Adolesc Psychiatr Clin N Am. 2008;17(4):835–856. ix–x. doi: 10.1016/j.chc.2008.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce K, Muller RA, Ambrose J, Allen G, Courchesne E. Face processing occurs outside the fusiform ‘face area’ in autism: evidence from functional MRI. Brain. 2001;124(Pt 10):2059–2073. doi: 10.1093/brain/124.10.2059. [DOI] [PubMed] [Google Scholar]
- Pierce K, Schreibman L. Increasing complex social behaviors in children with autism: Effects of peer-implemented pivotal response training. Journal of Applied Behavior Analysis. 1995;28:285–295. doi: 10.1901/jaba.1995.28-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce K, Schreibman L. Multiple peer use of pivotal response training social behaviors of classmates with autism: Results from trained and untrained peers. Journal of Applied Behavior Analysis. 1997;30:157–160. doi: 10.1901/jaba.1997.30-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichow B, Volkmar FR. Social skills interventions for individuals with autism: evaluation for evidence-based practices within a best evidence synthesis framework. J Autism Dev Disord. 2010;40(2):149–166. doi: 10.1007/s10803-009-0842-0. [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Lord C. The Social Communication Questionnaire. Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
- Schultz RT, Gauthier I, Klin A, Fulbright RK, Anderson AW, Volkmar F, Skudlarski P, Lacadie C, Cohen DJ, Gore JC. Abnormal ventral temporal cortical activity during face discrimination among individuals with autism and Asperger syndrome. Arch Gen Psychiatry. 2000;57(4):331–340. doi: 10.1001/archpsyc.57.4.331. [DOI] [PubMed] [Google Scholar]
- Schupp CW, Simon D, Corbett BA. Cortisol Responsivity Differences in Children with Autism Spectrum Disorders During Free and Cooperative Play. J Autism Dev Disord. 2013 doi: 10.1007/s10803-013-1790-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka JW, Wf, Klaiman C, Koenig K, Cockburn J, Herlihy L, Brown C, Stahl S, Kaiser MD, Schultz RT. Using computerized games to teach face recognition skills to children with autism spectrum disorder: the Let’s Face It! program. Journal of Child Psychology and Psychiatry. 2010;51(8):944–952. doi: 10.1111/j.1469-7610.2010.02258.x. [DOI] [PubMed] [Google Scholar]
- Viau R, Arsenault-Lapierre G, Fecteau S, Champagne N, Walker CD, Lupien S. Effect of service dogs on salivary cortisol secretion in autistic children. Psychoneuroendocrinology. 2010;35(8):1187–1193. doi: 10.1016/j.psyneuen.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Warren SF, Fey ME, Yoder PJ. Differential treatmet intensity research: A missing link to creating optimally effective communication interventions. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:70–77. doi: 10.1002/mrdd.20139. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- Wing L, Gould J. Severe impairments of social interaction and associated abnormalities in children: epidemiology and classification. Autism and Developmental Disorders. 1979;9(1):11–29. doi: 10.1007/BF01531288. [DOI] [PubMed] [Google Scholar]
- Wink LK, Erickson CA, McDougle CJ. Pharmacologic treatment of behavioral symptoms associated with autism and other pervasive developmental disorders. Curr Treat Options Neurol. 2010;12(6):529–538. doi: 10.1007/s11940-010-0091-8. [DOI] [PubMed] [Google Scholar]
- Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. Journal of Comparative Psychology. 1908;18:459–482. [Google Scholar]