Abstract
INTRODUCTION
Expenditures on material supplies and medications constitute the greatest per capita costs for surgical missions. We hypothesized that supply acquisition at nonprofit organization (NPO) costs would lead to significant cost-savings compared to supply acquisition at US academic institution costs from the provider perspective for hernia repairs and minor procedures during a surgical mission in the Dominican Republic (DR).
METHODS
Items acquired for a surgical mission were uniquely QR-coded for accurate consumption accounting. Both NPO and US academic institution unit costs were associated with each item in an electronic inventory system. Medication doses were recorded and QR-codes for consumed items were scanned into a record for each sampled procedure. Mean material costs and cost savings ± SDs were calculated in US dollars for each procedure type. Cost-minimization analyses between the NPO and the US academic institution platforms for each procedure type ensued using a two-tailed Wilcoxon matched-pairs test with α=0.05. Item utilization analyses generated lists of most frequently used materials by procedure type.
RESULTS
The mean cost savings of supply acquisition at NPO costs for each procedure type were as follows: $482.86 ± $683.79 for unilateral inguinal hernia repair (IHR, n=13); $332.46 ± $184.09 for bilateral inguinal hernia repair (BIHR, n=3); $127.26 ± $13.18 for hydrocelectomy (HC, n=9); $232.92 ± $56.49 for femoral hernia repair (FHR, n=3); $120.90 ± $30.51 for umbilical hernia repair (UHR, n=8); $36.59 ± $17.76 for minor procedures (MP, n=26); and $120.66 ± $14.61 for pediatric inguinal hernia repair (PIHR, n=7).
CONCLUSION
Supply acquisition at NPO costs leads to significant cost-savings compared to supply acquisition at US academic institution costs from the provider perspective for IHR, HC, UHR, MP, and PIHR during a surgical mission to DR. Item utilization analysis can generate minimum-necessary material lists for each procedure type to reproduce cost-savings for subsequent missions.
Keywords: global health, global disease burden, surgical mission, Dominican Republic, cost-minimization, procedural cost, material cost, item utilization, hernia repair, hydrocelectomy, excision of benign cutaneous mass, minor procedure
INTRODUCTION
An estimated 234.2 million (95% CI 187.2–281.2 million) surgeries are performed annually worldwide1. Despite the fact that 70% of the world’s population resides in developing countries, only 26% of the surgeries performed worldwide occur in these developing regions2. Although limited in the assessment of surgical disease, data do not appear to indicate that the developing world suffers a lesser burden of surgical conditions; rather, access to surgical care is limited in these regions1–3. Until developing regions of the world are able to ameliorate disparate access and sustain delivery of surgical care at the global standard for its inhabitants, humanitarian organizations will attempt to address this healthcare disparity through the implementation of surgical missions to these developing regions.
Surgical care decreases disability and premature death, and therefore plays an important role in global public health. The Disease Control Priorities Project sponsored by the World Bank roughly estimates that 11% of premature death and disability globally may be averted through the delivery of surgical services4. However, due to profound limitations in the reporting of surgical conditions, public health experts believe that the global burden of surgical disease has been grossly underestimated5–6. For these reasons, the international collaboration known as the Alliance for Surgical and Anesthesia Presence Today (ASAP TODAY; formerly known as the Global Burden of Surgical Disease Working Group) has convened since 2008 to “(1) quantitatively define global disparity in surgical care; (2) assess unmet surgical need; (3) identify priorities; (4) develop sustainable models for improved health care delivery; and (5) advocate for a presence within the global public health agenda”7. Concentrated efforts to better characterize the global epidemiology of surgical conditions ensure that surgical care will assume an increasingly greater role in global health. It is therefore imperative that sustainable models of improved surgical care delivery are developed by the global health community, and that humanitarian organizations which play a key role in the delivery of these surgical services8 contribute substantively to this effort.
Among the four types of surgical interventions with potentially significant public health impact identified by the Disease Control Priorities Project is the elective repair of simple surgical conditions such as hernias4. Umbilical, inguinal, and femoral hernias are priority 1 surgical conditions, as defined by having highly effective surgical interventions for treatment, surgical care that is cost-effective and feasible to promote globally, and large public health burdens9. With funding from the Bill and Melinda Gates Foundation, the Institute for Health Metrics and Evaluation (IHME) recently analyzed and collated data regarding global disease burden10–16. According to data for both sexes and all ages from the IHME Global Burden of Disease Study 2010, there is a disparity in the disease burden from inguinal or femoral hernia between the United States and the Dominican Republic17. Likely due to limited healthcare resources and disparate access to surgical intervention in the Dominican Republic, patients with inguinal or femoral hernias suffer greater disability and premature death in the Dominican Republic compared to the United States17. For these reasons, a surgical team from Washington University in Saint Louis organized to form Surgical Outreach for the Americas and chose to focus its humanitarian efforts on providing hernia repairs and minor procedures for the underserved patients of the Dominican Republic. Surgical Outreach for the Americas is committed to collecting and disseminating operational data to the global health community in an effort to catalyze more cost-effective and sustainable surgical care delivery for underserved patients of the developing world.
The collection and reporting of data from humanitarian organizations are critical components of developing sustainable models of care. Greater than 15% of all nonprofit organizations are involved in healthcare activities18. Of the humanitarian organizations that provide surgical care to low and middle-income countries, few of these organizations track and report their data to share valuable information with other medical mission initiatives19–33. Measurement and reporting of operational data, including supply acquisition costs, item utilization, and patient outcomes would allow other humanitarian organizations to reliably replicate and improve upon these experiences. Disseminating these metrics to the humanitarian community could reduce the time lag between the planning and the execution of medical missions, minimize waste of resources, maximize the healthcare services provided with limited budgets, and improve the quality of care delivered to the underserved patient populations. Through such information exchange, the global health community can potentially achieve cost-effective and sustainable surgical care delivery in low-resource medical environments, and serve a greater number of patients in the developing world.
According to data from 543 humanitarian organizations, the annual expenditure on short-term medical missions is conservatively estimated to be $250 million plus thousands of volunteer hours34. Among all procedural expenses, costs for material supplies and medications constitute the greatest per capita costs for surgical missions to underserved populations35. Nonprofit organizations (NPOs) that maintain repositories of healthcare materials for distribution have the potential to minimize procedural costs and increase the number of patients served during limited-budget surgical missions. Needed are data that quantify these material costs and describe the minimum necessary items to safely and effectively perform these surgical procedures at the global standard of care. Thus, the purpose of this study was to quantify the material cost-minimization resulting from NPO supply acquisition and describe the item utilization for hernia repairs and minor procedures incurred by Surgical Outreach for the Americas. We hypothesized that supply acquisition at NPO costs would lead to significant cost-savings compared to supply acquisition at United States academic institution costs from the institutional provider perspective for hernia repairs and minor procedures during a 2012 surgical mission in the Dominican Republic.
MATERIALS & METHODS
National Population and Scope of the Surgical Issue
The Dominican Republic is a Central American nation on the island of Hispaniola with an estimated population of 10,219,630 in 201336. The median age of the population is 26.5 years (age structure: 28.5% ≤ 14 years; 18.5% 15–25 years; 39.1% 25–54 years; 7% 55–64 years; 6.9% ≥ 65 years), and the average life expectancy at birth is 77.44 years36. However, only 6.2% of the $98.74 billion national gross domestic product (GDP) is spent on healthcare in the Dominican Republic, compared to 17.9% of the $15.66 trillion national GDP in the United States36. As a result, the mean per capita healthcare expenditure is $95 annually in the Dominican Republic (global rank: 71) compared to $4,271 annually in the United States (global rank: 1)37.
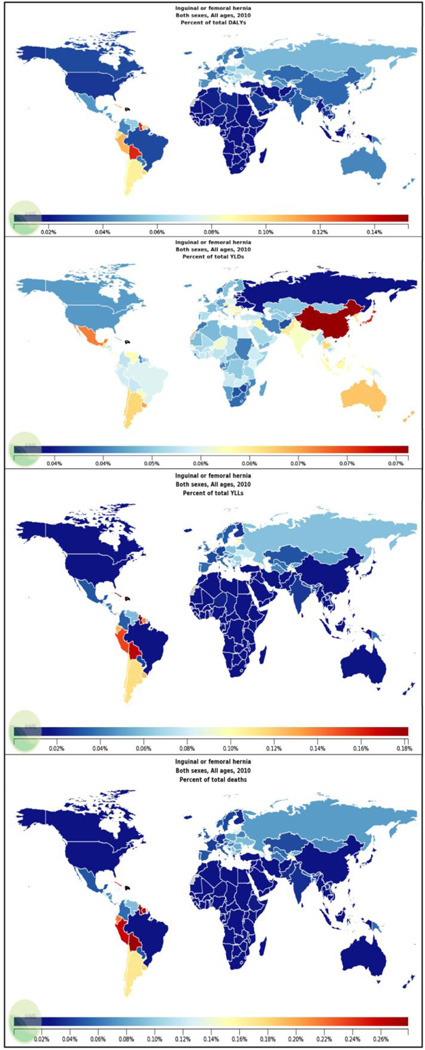
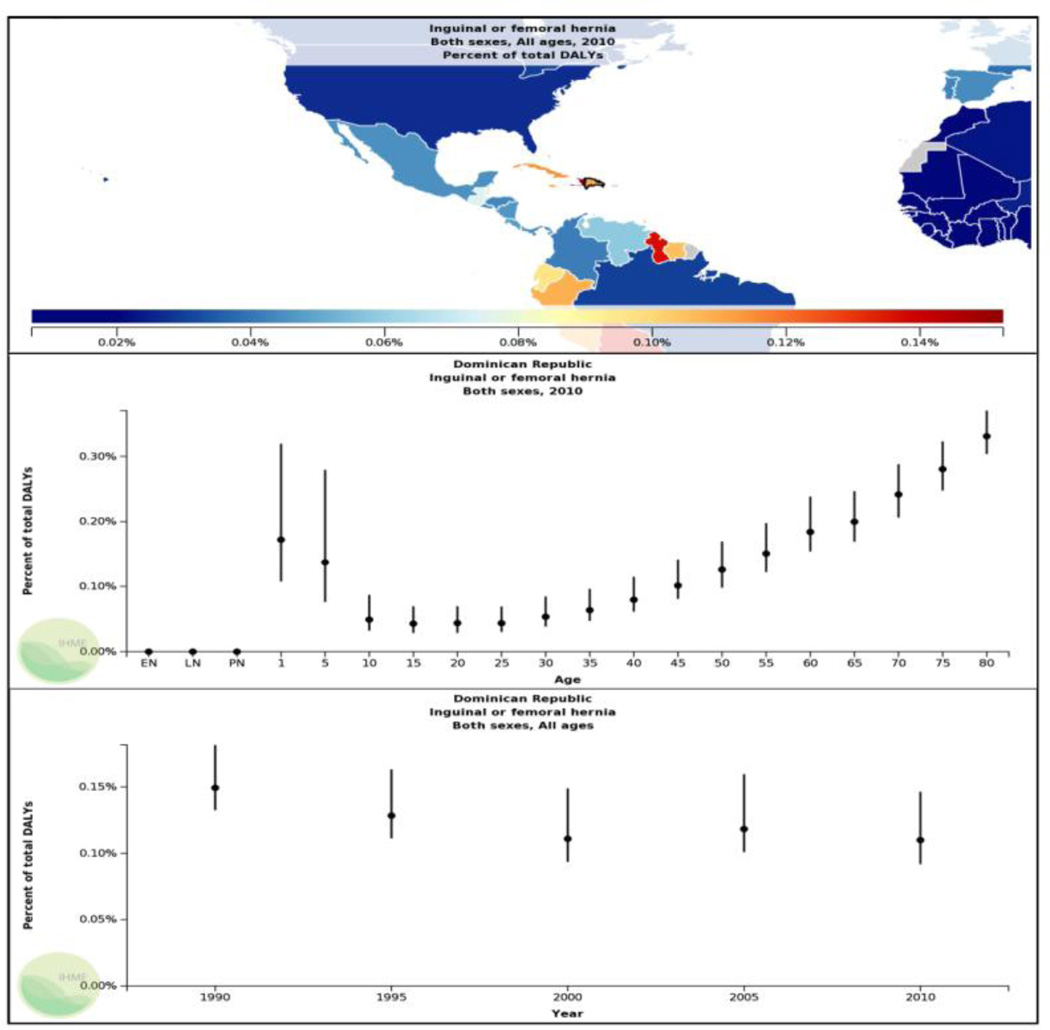
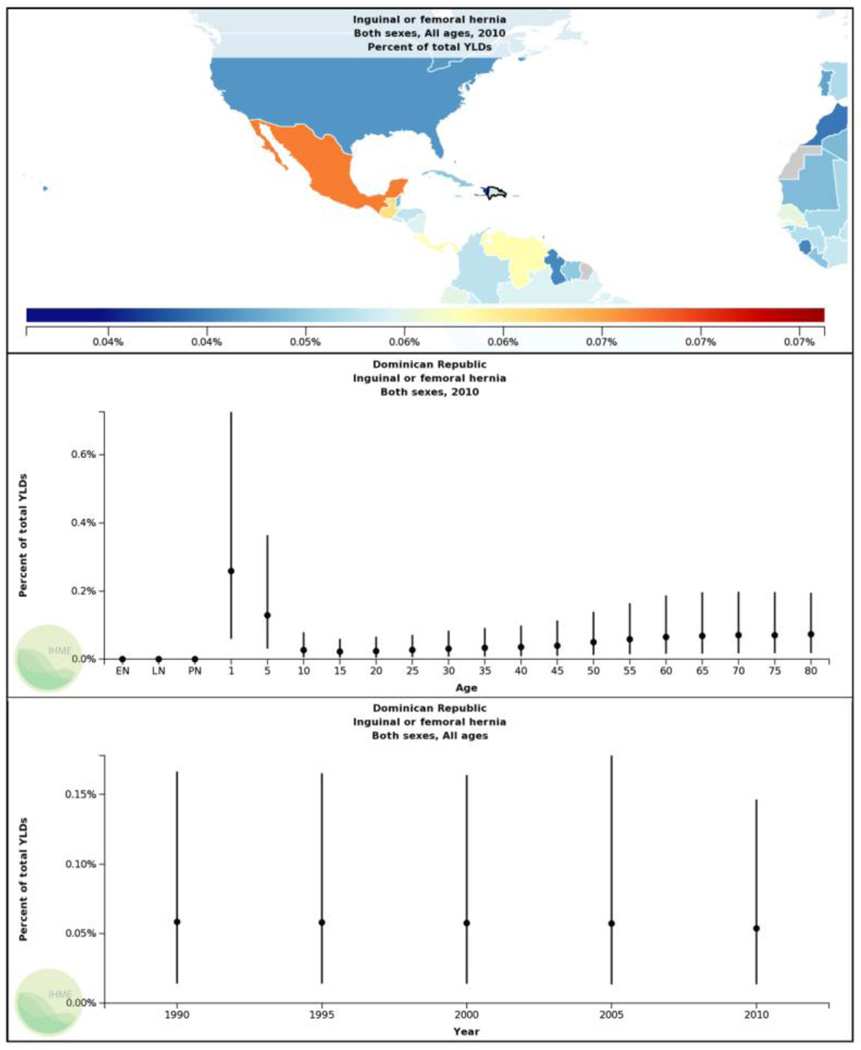
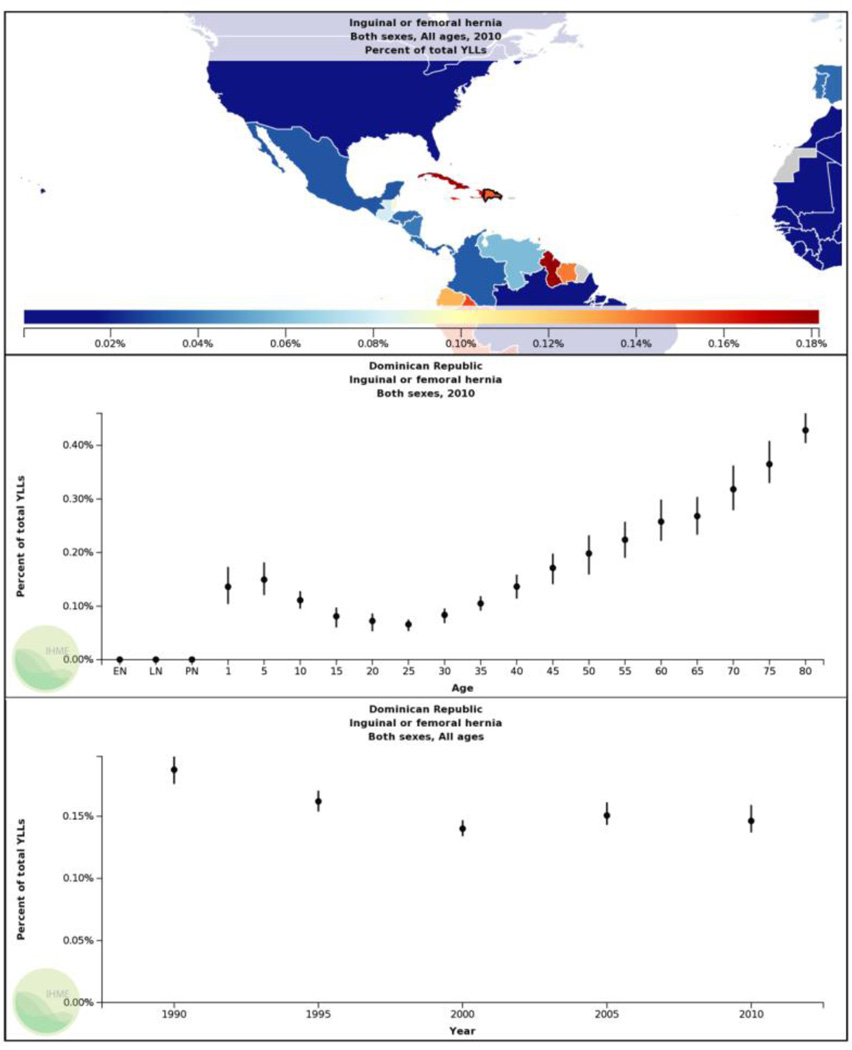
The work force in the Dominican Republic predominantly serves in service-oriented, industrial, and agricultural fields (63.1%, 22.3%, 14.6%, respectively)36. This strenuous manual labor likely contributes to the prevalence of hernias in the Dominican Republic. Given limited healthcare resources and disparate access to surgical intervention in the Dominican Republic, it is not uncommon for these hernias to go unrepaired for long periods of time, thus likely accounting for the greater disability and premature death attributable to inguinal and femoral hernias in the Dominican Republic compared to the United States. In the Dominican Republic, inguinal and femoral hernias account for 31.8 disability adjusted life years (DALYs) per 100,000 people (0.11% of total DALYs), 6.17 years lost due to disability (YLDs) per 100,000 people (0.054% of total YLDs), 25.64 years of life lost (YLLs) per 100,000 people (0.15% of total YLLs), and 1.64 deaths per 100,000 people (0.27 % of total deaths) [Figures 1–5]17. This compares less favorably to the United States where the burden of inguinal and femoral hernias is 7.23 DALYs per 100,000 people (0.027% of total DALYs), 5.58 YLDs per 100,000 people (0.046% of total YLDs), 1.65 YLLs per 100,000 people (0.011% of total YLLs), and 0.14 deaths per 100,000 people (0.016% of total deaths)17. Due to the reliance of the work force on manual labor for sustenance, the increased disability and premature death attributable to inguinal and femoral hernias in the Dominican Republic has a potentially significant negative economic impact on the population.
Figure 1.
Percent of total disability-adjusted life years (DALYs), years lost to disability (YLDs), years of life lost (YLLs), and total deaths due to inguinal or femoral hernia globally (data for both sexes and all ages from year 2010)17.
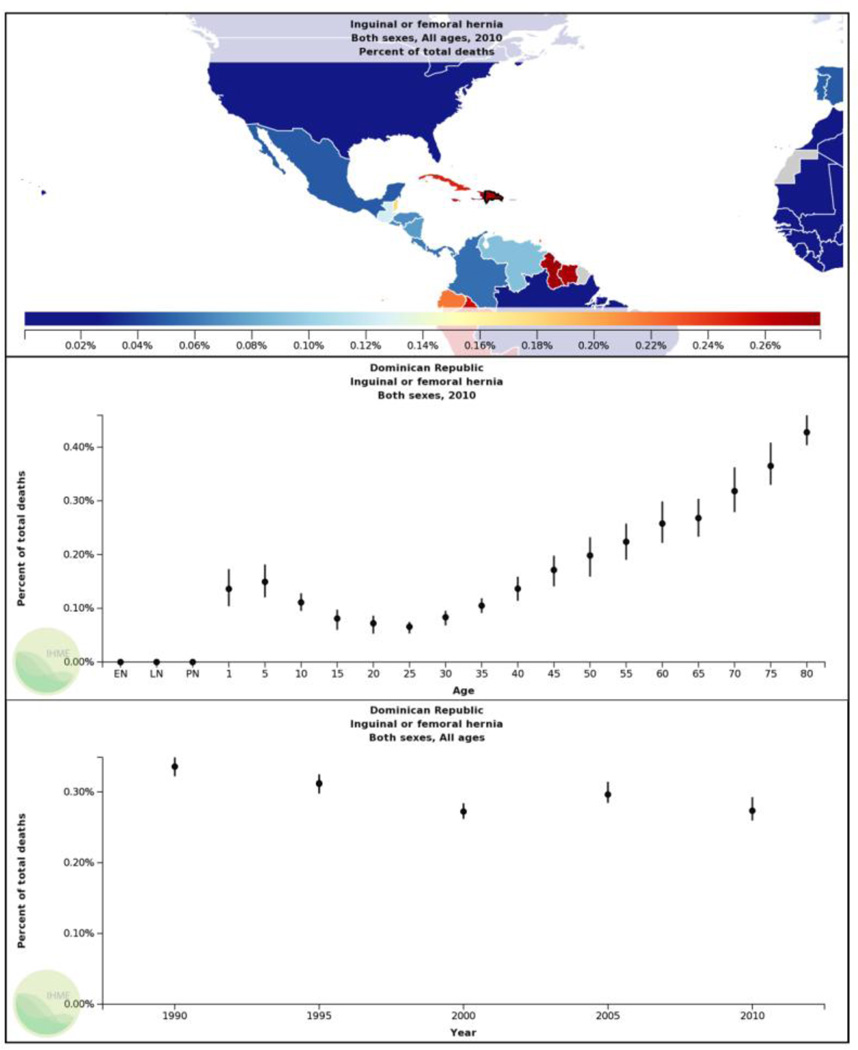
Figure 5.
Percent of total deaths due to inguinal or femoral hernia in the Dominican Republic (data for both sexes and all ages from year 2010)17. [EN= early neonatal period (0–6 days); LN= late neonatal period (7–28 days); PN= post neonatal period (29–365 days)]
Mission
The Institute for Latin American Concern (ILAC) Center in the Dominican Republic is an international collaboration established by Creighton University to provide healthcare and education to the underserved people of the Dominican Republic38. The ILAC Center is located 7.5 kilometers from Santiago, the second largest city in the Dominican Republic38. In 2004, the ILAC Center erected a level 1 outpatient surgery suite and developed a partnership with the leadership of the American Hernia Society (AHS) to provide volunteer surgical care25. Since 2009, the senior author (BDM) has contributed to this ongoing effort by conducting an annual hernia repair mission at the ILAC Center with a surgical team from Washington University in Saint Louis. In 2012, this Saint Louis-based surgical mission became formally incorporated as a non-profit humanitarian organization entitled Surgical Outreach for the Americas. From January 28th through February 4th 2012, Surgical Outreach for the Americas conducted a short-term lateral surgical mission at the outpatient ILAC Center in the Dominican Republic18. The objectives of this mission were to (1) provide basic surgical education to local students; (2) provide the underserved population with cost-effective surgical services at the global standard of care, including: inguinal, femoral, umbilical, and small ventral hernia repairs, and hydrocelectomy (priority 1 surgical conditions9), and excisions of benign cutaneous masses (priority 2 surgical condition9); and (3) measure and report operational data for the global health community.
Support and Funding
Coordination and planning began 12 months in advance of the mission by the Surgical Outreach for the Americas team leader (MMF). A $27,000 total budget was generated for the 2012 surgical mission based on prior experience and patient volume projections. Foundation grants, corporate donations, and private donations were then sought to support the mission. For the 2012 surgical mission, funding was primarily obtained through grants and monetary donations from the Foundation for Barnes-Jewish Hospital (Saint Louis, Missouri); Christian World Relief® (Richmond Heights, Missouri); and other benefactors. All members of the surgical team volunteered their time and services.
Materials Acquisition and Costs
The provider perspective was assumed for all costs. The majority of the material supplies were obtained at non-profit organization (NPO) acquisition costs from AmeriCares Foundation® (Stamford, Connecticut); Hospital Sisters Mission Outreach® (Springfield, Illinois); and MAP International® (Brunswick, Georgia). Some supplies and services were also donated by Barnes-Jewish Hospital® (Saint Louis, Missouri); FedEx® Corporation (Memphis, Tennessee); BD®, Incorporated (Franklin Lakes, New Jersey); LMA North America®, Incorporated (San Diego, California); Pall Medical Corporation® (Port Washington, New York); Trademark Medical®, Incorporated (Saint Louis, Missouri); Atrium Medical Corporation® (Hudson, New Hampshire); Bard® Davol®, Incorporated (Warwick, Rhode Island); Ethicon®, Incorporated (San Angelo, Texas); and W.L. Gore and Associates®, Incorporated (Newark, Delaware). A minimum number of supplies that were not available from nonprofit healthcare supply organizations were purchased at United States (US) academic institution acquisition costs from Cardinal Health®, Incorporated (Dublin, Ohio) and Medline Industries®, Incorporated (Mundelein, Illinois). Most material supply items procured during the 12 months of preparation before the mission were shipped by FedEx® Corporation to the ILAC Center 12 weeks prior to the mission. Transport through customs was facilitated by the ILAC Center for a brokerage fee. The remaining items and all surgical instrument packs were transported in checked luggage with the surgical team. To avoid customs regulatory issues incurred by transporting anesthetics, narcotics, and antibiotics across international borders and the cost of shipping materials of heavy weight, the following materials were purchased directly from the ILAC Center: dormicum, fentanyl, oxaforte, ceftriaxone, oxygen tanks, and normal saline bags for intravenous infusion.
Using the receipts from each purchase, the acquisition cost for one unit of each individually-packaged single-use material supply item was calculated by dividing the cost by the number of units obtained. The corresponding US academic institution acquisition costs for the same material supply items were obtained from the manufacturer sales representatives, and the unit cost was calculated in the same manner. Since most medications were purchased in large volumes to be distributed to multiple patients, medication costs were calculated by pill or by mg for liquid suspensions. Traceability Made Easy® (TME®) quick response code (QR-code) based inventory management software was purchased and downloaded to a designated laptop, and a handheld QR-code scanner with a universal serial bus (USB) adapter was rented from MASS Group®, Incorporated (Chatsworth, California). Unique QR-codes on self-adhesive labels were generated for each material supply item in our inventory for accurate accounting of consumption. For material supplies acquired during the year prior to the mission, these labels were affixed to the corresponding items prior to transport to the Dominican Republic. For residual inventory stored at the ILAC Center from prior missions by our group, these labels were affixed to the corresponding items during the 2-day preparatory period preceeding the 5 operative days of our mission. The name, unique QR-code, count, expiration date, source, NPO acquisition cost, and US academic institution cost for each item in our inventory were recorded in the TME® electronic inventory management system prior to the mission. The laptop with the TME® inventory management system and handheld QR-code scanner accompanied the surgical team to the mission.
Personnel
Based on patient volume projections, 15 experienced healthcare service volunteers were sought to fill the following roles on the Surgical Outreach for the Americas team: 1 team leader, 2 attending general surgeons, 2 general surgery residents, 3 nurse anesthetists, 2 circulating nurses, 1 emergency medicine attending, 1 medical student, 1 autoclave technician, 1 pre-operative registrar, and 1 post-operative care technician. Documentation of current passports, appropriate licensure, immunizations, international emergency healthcare coverage, emergency contact information, and security clearances were required of all volunteers 6 months in advance of the mission. Prior to travelling, volunteers were strongly encouraged to register their travel plans and review the security recommendations outlined on the United States Department of State websites39–40; and heed all recommendations regarding prophylaxis for communicable diseases endemic to the Dominican Republic on the United States Centers for Disease Control and Prevention website41. The Surgical Outreach for the Americas team was complemented by the following personnel provided by the ILAC Center in the Dominican Republic: 1 ILAC Center administrator, 2 United States Peace Corp volunteers to assist with language translation, 2 clinic coordinators, 1 post-operative care technician, 2 operating room cleaning staff members, and 1 local surgical resident. Personnel coordination was facilitated by early and frequent communication between the Surgical Outreach for the Americas team leader and the ILAC Center administrators.
Travel and Housing
Travel and housing arrangements were also coordinated between the Surgical Outreach for the Americas team leader and the ILAC Center administrators. All team members traveled together internationally on commercial airlines. As per customs regulations, each volunteer paid a $10 tourist card fee to enter the Dominican Republic. Travel between the airport and the ILAC Center was provided by a taxi service associated with the ILAC Center for a fee. In exchange for a room and board fee, the ILAC Center provided all meals and housing on a secure campus. Additional fees were paid to the ILAC Center for essential administrative support and rental of the ILAC Center outpatient operative suite.
Patient Recruitment
Cooperadores, individuals selected from the rural communities of the Dominican Republic and trained by ILAC Center healthcare workers to screen community members for health problems, played an essential role in the identification of patients with hernias, hydroceles, and benign cutaneous masses. The patients who were identified by the cooperadores were then scheduled to arrive at the ILAC Center on one of the operative days of our mission. Upon patient arrival to the ILAC Center, the patient was registered by the pre-operative registrar and issued a paper medical record. With the assistance of a translator, the emergency medicine attending and medical student then obtained basic vital signs, interviewed the patient for past medical and surgical history, conducted a physical exam, and recorded all information in the medical record. The patient was next assessed by the emergency medicine attending and the nurse anesthetists for same-day surgery eligibility. Patients who were found to be eligible for same-day surgery were then examined by the attending general surgeon and general surgery resident, and consented for the appropriate surgical procedure with the assistance of a translator. Patients presenting for excision of benign cutaneous masses were treated by the emergency medicine attending with the assistance of the medical student in a dedicated procedure room following morning clinic hours. Patients youngest in age, oldest in age, and with the greatest comorbidity burden were prioritized and scheduled to undergo their surgical procedures early in the week and early in the day.
Procedures
Surgical procedures were performed in 2 operating rooms over a 5-day period. Each operating room was equipped with an overhead light, a standard-size operating table, an intravenous pole, an anesthesia machine with a calibrated vaporizer and an oxygen tank, a cardiopulmonary monitor, a cardiac defibrillator, an anesthesia cart, an electrocautery unit, a table for surgical instruments, disposal boxes for sharps, and shelving. During the 2-day preparatory period preceeding the operative week, the operating room shelving was stocked with our material supplies and the anesthesia carts were equipped with syringes, needles, a pharmacy of medications, laryngoscopes and blades, laryngeal mask airways, endotracheal tubes, bag-valve-masks, and nasal and oral airways. Each operating room team consisted of 1 attending general surgeon, 1 general surgery resident, 1 nurse anesthetist, and 1 circulating nurse. A separate procedure room was used for excisions of benign cutaneous masses. The procedure room was equipped with an overhead light, a standard-size operating table, a table for surgical instruments, disposal boxes for sharps, and shelving equipped with our material supplies. The procedure room team consisted of 1 emergency medicine attending, 1 medical student, and 1 United States Peace Corp volunteer to assist with translation.
All surgical procedures were performed in open fashion, and at the global standard of surgical and anesthesia care. Anesthesia monitoring included continuous temperature monitoring using a cutaneous temperature strip, continuous pulse oximetry, continuous end-tidal capnography, continuous cardiac rhythm and heart rate monitoring, and intermittent sphygmomanometry. Forced air warming blankets (Bair Hugger®; Arizant Healthcare®, Incorporated; Prairie, Minnesota) were used to maintain body temperature throughout the case. A safety belt was placed over the upper legs of the patient, and padded cushions were used to support the dependent portions of the extremities. All adult surgical patients were infused with 1 liter of normal saline and all pediatric surgical patients were infused with 0.5 liter of normal saline via a peripheral intravenous (IV) drip. Within 60 minutes of the initial incision, pediatric surgical patients received 0.5 gram of IV ceftriaxone, adult surgical patients with a body mass index < 35 received 1 gram of IV ceftriaxone, and adult surgical patients with a body mass index > 35 received 2 grams of IV ceftriaxone for antibiotic prophylaxis.
All pediatric cases were performed under general anesthesia using inhaled sevoflurane, propofol (40–100 mg IV), ketorolac (10–30 mg IV), and fentanyl (25–100 µg IV). Depending on the health risks and the comfort of the patient, inguinal hernia repairs and femoral hernia repairs were performed on adults under monitored anesthesia care with local anesthesia and a regional nerve block using a 1:1 mixture of 1% lidocaine and 0.5% marcaine appropriate for the mass of the patient; or under general anesthesia using inhaled sevoflurane, propofol (100–380 mg IV), dormicum (1–2 mg IV), ketorolac (15–30 mg IV), and fentanyl (50–200 µg IV). All adult umbilical hernia repairs, small ventral hernia repairs, and hydrocelectomies were performed under general anesthesia. Phenylephrine, epinephrine, ephedrine, neostigmine, rocuronium, glycopyrrolate, metoprolol, and ondansetron were available and used as needed for general anesthesia cases. All adult excisions of benign cutaneous masses were performed under local anesthesia using a subcutaneous injection of 1% lidocaine appropriate for the mass of the patient.
Each member of the surgical team wore scrubs, a surgical cap, and a surgical mask in the operating rooms. Attending and resident surgeons scrubbed with chlorhexidine or povidone-iodine solution in the usual fashion, and wore sterile disposable gowns and sterile gloves. Operative fields were trimmed with electric clippers as necessary, prepped with chlorhexidine or povidone-iodine solution, and draped in the usual sterile fashion. The Lichtenstein tension-free repair was performed with a polypropylene mesh for all adult inguinal hernias, and the Bassini repair was performed for all pediatric inguinal hernia repairs. Either a polypropylene plug repair or a modified Lichtenstein procedure with a polypropylene mesh was performed for all femoral hernias. Hydrocelectomies were performed with eversion of the hydrocele sac by Winkelmann’s technique. Umbilical or small ventral hernia defects < 2 cm in diameter were primarily repaired, whereas umbilical or small ventral hernia defects ≥ 2 cm in diameter were repaired with preperitoneal or intraperitoneal mesh reinforcement using a mesh with an adhesion barrier and fascial closure. Benign cutaneous masses such as sebaceous cysts and lipomas were treated with simple excisions along the lines of Langer and primary closure.
All patients were recovered with cardiopulmonary monitoring in the post-operative recovery room under the supervision of a nurse anesthetist and a post-operative care technician, and discharged the same day following demonstration of the ability to tolerate clear liquids, urinate without difficulty, and ambulate independently. In a few cases in which patients underwent surgery late in the day, patients were lodged at the ILAC Center and discharged the following morning. All patients received oral medications for post-operative analgesia. All pediatric patients < 6 years of age were discharged with 120 ml of pediatric ibuprofen 100 mg/5 ml suspension or 118 ml of pediatric acetaminophen 160 mg/5 ml suspension, whereas all pediatric patients ≥ 6 years of age were discharged with 10 pills of pediatric chewable ibuprofen 100 mg dosed according to standard recommendations for postoperative analgesia over the ensuing days. Adult patients who underwent unilateral inguinal or femoral hernia repair were discharged with 8 pills of naproxen 220 mg plus 5 pills of oxaforte (codeine 50 mg/diclofenac 50 mg), whereas adult patients who underwent bilateral inguinal hernia repairs were discharged with 20 pills of ibuprofen 200 mg plus 10 pills of oxaforte dosed according to standard recommendations for postoperative analgesia over the ensuing days. Adult patients who underwent umbilical hernia repairs, small ventral hernia repairs, unilateral or bilateral hydrocelectomies, or excisions of benign cutaneous masses were discharged with 8 pills of acetaminophen 500 mg dosed according to standard recommendations for postoperative analgesia over the ensuing days.
Surgical Instruments
Instrument packs were transported by flight with the surgical team. Instrument packs for all operative procedures included: 1 #3 blade handle, 1 #7 blade handle, 4 Adson forceps with teeth, 2 Adson forceps without teeth, 2 rat tooth forceps, 4 Debakey forceps, 3 needle drivers, 1 pair of Metzenbaum scissors, 1 pair of suture scissors, 5 mosquito clamps, 2 straight clamps, 2 Kelly clamps, 1 Burlisher clamp, 1 right angle clamp, 2 Allis clamps, 1 medium-sized Weitlaner retractor, 1 Richardson retractor, 2 army-navy retractors, 1 bowl, 4 towel clamps, 4 sterile blue towels, and 10 sterile radiograph-detectable gauze sponges. Instrument packs for all small procedures included: 1 #3 blade handle, 2 Adson forceps with teeth, 1 Burlisher clamp, 1 needle driver, 1 pair of suture scissors. Large Richardson retractors and large Weitlaner retractors were also individually wrapped and sterilized in the event they were needed. Between operative cases, the autoclave technician scrubbed all surgical instruments, reassembled the instruments into operative packs, and sterilized the operative packs using the autoclave machines on the premises.
Data Collection and Statistical Analysis
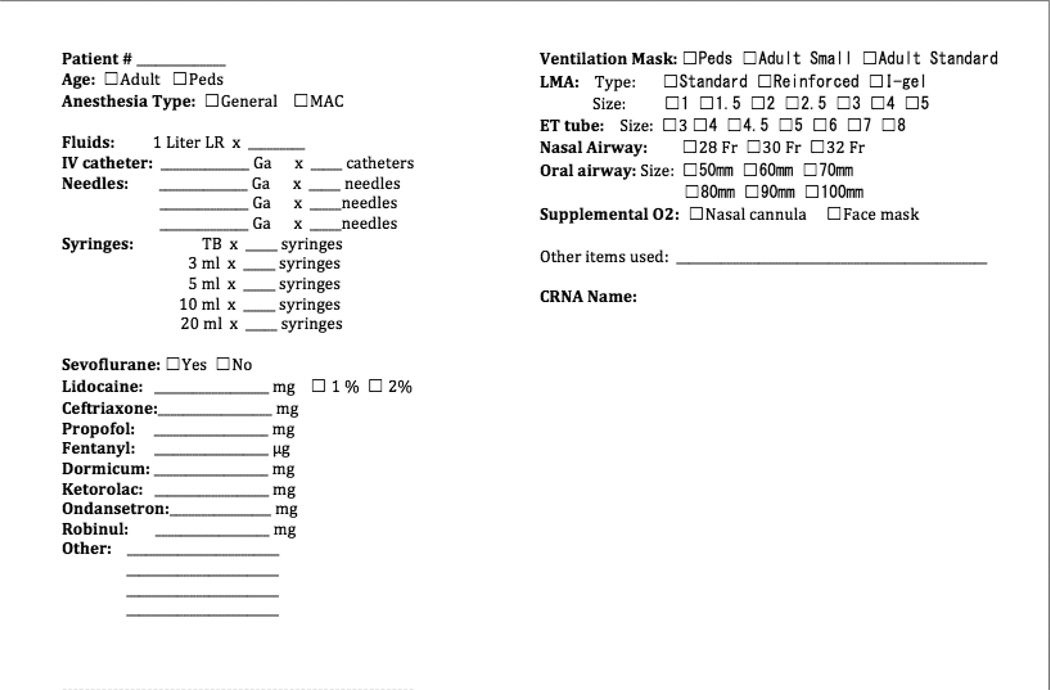
A unique QR-code with a deidentified patient number was generated for each patient, and self-adhesive labels with this unique QR-code were affixed to both the patient chart and a resealable bag attached to the chart. A convenience sampling of patients was used to measure the mean total cost of material supplies and item utilization for each procedure type. The QR-code labels affixed to the packages of each material supply item utilized during the perioperative period for a given patient were retrieved at the time of use and stored in the resealable bag attached to the chart of that patient. In addition, all administered medications and utilized anesthesia supplies were recorded intraoperatively by the nurse anesthetists using a standard form attached to each patient chart [Figure 6]. All patient charts remained in the ILAC Center. An electronic file with the deidentified patient number, pediatric or adult status, local anesthesia or general anesthesia status, medication doses administered, and operative procedure was created for each patient in the TME® electronic inventory management system. When internet access was available, all QR-codes associated with a given deidentified patient number were scanned and assigned to the corresponding electronic file using the custom TME® electronic inventory management system.
Figure 6.
Perioperative anesthesia material supply item and medication recording document.
All items in the inventory management system had previously been associated with both a NPO acquisition cost and a US academic institution acquisition cost in US dollars. TME® reports that sorted the electronic files by operative procedure were created. Under a study protocol approved by the Washington University Institutional Review Board (protocol #: 201305123) and registered with clinicaltrials.gov (study identifier: NCT01872364), the mean total cost of material supplies for each procedure type using either the NPO acquisition costs or the US academic institution acquisition costs were calculated from these reports and reported as means ± standard deviations (SD). The arithmetic difference in the total cost of material supplies between the NPO platform and the US academic institution platform was calculated for each individual procedure, and the average difference was determined by procedure type to report the mean cost savings ± SD for each procedure type. A cost-minimization analysis then ensued by statistically comparing the distribution of total costs for material supplies between the NPO platform and the US academic institution platform for each procedure type from the provider perspective. Given the limited sample size and the inherent dependence of the data, a two-tailed Wilcoxon matched-pairs test with α= 0.05 was applied to the paired distributions for total material supply costs for a given procedure. All statistical analyses were performed with Microsoft® Excel® (Redmond, Washington) and GraphPad® Prism® version 5 (La Jolla, California) software. TME® reports that sorted the electronic files by material supply item were also generated. These reports were used to perform item utilization analyses to identify the most frequently used material supply items for each procedure type. These data are reported as lists of the most consistently used materials for each procedure type, and bundles of routinely used items for all procedures, monitored anesthesia care procedures, adult general anesthesia procedures, and pediatric general anesthesia procedures.
RESULTS
Patient Characteristics
During the 2012 mission, Surgical Outreach for the Americas performed a total of 126 procedures on 106 patients over 5 operative days. The male:female ratio of these patients was 2.8:1, and the mean age of the patients was 45.6 ± 20.4 years. The case mix of the 126 procedures was as follows: 52 adult and pediatric inguinal hernia repairs, 4 adult femoral hernia repairs, 20 adult and pediatric umbilical or small ventral hernia repairs, 18 adult and pediatric hydrocelectomies, and 32 excisions of benign cutaneous masses. The general anesthesia:local or regional anesthesia ratio for all patient cases was approximately 2:1. Of the 106 patients who underwent a surgical procedure, one patient was noted to have moderate respiratory instability intraoperatively likely attributable to sequelae of liver cirrhosis. The patient was successfully stabilized and extubated postoperatively, but was transferred to a local hospital for further evaluation after postoperative recovery. No other complications occurred in the immediate postoperative period. Sampled among the 126 procedures performed were 13 unilateral inguinal hernia repairs, 3 bilateral inguinal hernia repairs, 9 hydrocelectomies, 3 femoral hernia repairs, 8 umbilical hernia repairs, and 26 excisions of benign cutaneous masses for adult patients, as well as 7 inguinal hernia repairs for pediatric patients.
Adult Unilateral Inguinal Hernia Repairs
For the convenience sample of 13 unilateral inguinal hernia repairs performed on adult patients, the mean total material supply cost using the NPO acquisition costs was $62.17 ± $0.74 for each procedure. The corresponding mean total material supply cost using the US academic institution acquisition costs was $502.79 ± $684.51 for each procedure (p=0.0002). Therefore, acquiring material supplies at the NPO acquisition costs resulted in a mean cost savings of $482.86 ± $683.79 per procedure for adult unilateral inguinal hernia repairs [Table 1].
Table 1.
Cost-minimization analysis results from acquiring material supply items at non-profit organization (NPO) acquisition costs compared to United States (US) academic institution acquisition costs for a 2012 surgical mission to the Dominican Republic
| Cost-minimization analysis results from a 2012 surgical mission to the Dominican Republic | ||||
|---|---|---|---|---|
| Procedure | Non-profit organization (NPO) material supply cost per procedure (mean US dollars ± SD) |
US academic institution material supply cost per procedure (mean US dollars ± SD) |
p-value | Mean cost-savings of material supply acquisition at NPO costs per procedure (mean US dollars ± SD) |
| Adult unilateral inguinal hernia repair | $62.17 ± $0.74 | $502.79 ± $684.51 | p=0.0002 | $482.86 ± $683.79 |
| Adult bilateral inguinal hernia repair | $51.85 ± $26.87 | $351.27 ± $184.20 | p=0.2500 | $332.46 ± $184.09 |
| Adult hydrocelectomy | $53.73 ± $23.66 | $141.68 ± $14.11 | p=0.0039 | $127.26 ± $13.18 |
| Adult femoral hernia repair | $55.47 ± $13.44 | $253.81 ± $54.32 | p=0.2500 | $232.92 ± $56.49 |
| Adult umbilical hernia repair | $47.56 ± $31.35 | $133.05 ± $31.54 | p=0.0078 | $120.90 ± $30.51 |
| Adult benign cutaneous mass excision | $4.59 ± $13.34 | $38.55 ± $19.03 | p<0.0001 | $36.59 ± $17.76 |
| Pediatric unilateral inguinal hernia repair | $23.92 ± $11.49 | $134.22 ± $16.61 | p=0.0156 | $120.66 ± $14.61 |
Adult Bilateral Inguinal Hernia Repairs
For the convenience sample of 3 bilateral inguinal hernia repairs performed on adult patients, the mean total material supply cost using the NPO acquisition costs was $51.85 ± $26.87 for each procedure. The corresponding mean total material supply cost using the US academic institution acquisition costs was $351.27 ± $184.20 for each procedure (p=0.2500). Therefore, acquiring material supplies at the NPO acquisition costs resulted in a mean cost savings of $332.46 ± $184.09 per procedure for adult bilateral inguinal hernia repairs [Table 1].
Adult Hydrocelectomies
For the convenience sample of 9 hydrocelectomies performed on adult patients, the mean total material supply cost using the NPO acquisition costs was $53.73 ± $23.66 for each procedure. The corresponding mean total material supply cost using the US academic institution acquisition costs was $141.68 ± $14.11 for each procedure (p=0.0039). Therefore, acquiring material supplies at the NPO acquisition costs resulted in a mean cost savings of $127.26 ± $13.18 per procedure for adult hydrocelectomies [Table 1].
Adult Femoral Hernia Repairs
For the convenience sample of 3 femoral hernia repairs performed on adult patients, the mean total material supply cost using the NPO acquisition costs was $55.47 ± $13.44 for each procedure. The corresponding mean total material supply cost using the US academic institution acquisition costs was $253.81 ± $54.32 for each procedure (p=0.2500). Therefore, acquiring material supplies at the NPO acquisition costs resulted in a mean cost savings of $232.92 ± $56.49 per procedure for adult femoral hernia repairs [Table 1].
Adult Umbilical Hernia Repairs
For the convenience sample of 8 umbilical hernia repairs performed on adult patients, the mean total material supply cost using the NPO acquisition costs was $47.56 ± $31.35 for each procedure. The corresponding mean total material supply cost using the US academic institution acquisition costs was $133.05 ± $31.54 for each procedure (p=0.0078). Therefore, acquiring material supplies at the NPO acquisition costs resulted in a mean cost savings of $120.90 ± $30.51 per procedure for adult umbilical hernia repairs [Table 1].
Adult Benign Cutaneous Mass Excisions
For the convenience sample of 26 benign cutaneous mass excisions performed on adult patients, the mean total material supply cost using the NPO acquisition costs was $4.59 ± $13.34 for each procedure. The corresponding mean total material supply cost using the US academic institution acquisition costs was $38.55 ± $19.03 for each procedure (p<0.0001). Therefore, acquiring material supplies at the NPO acquisition costs resulted in a mean cost savings of $36.59 ± $17.76 per procedure for adult benign cutaneous mass excisions [Table 1].
Pediatric Unilateral Inguinal Hernia Repairs
For the convenience sample of 7 unilateral inguinal hernia repairs performed on pediatric patients, the mean total material supply cost using the NPO acquisition costs was $23.92 ± $11.49 for each procedure. The corresponding mean total material supply cost using the US academic institution acquisition costs was $134.22 ± $16.61 for each procedure (p=0.0156). Therefore, acquiring material supplies at the NPO acquisition costs resulted in a mean cost savings of $120.66 ± $14.61 per procedure for pediatric unilateral inguinal hernia repairs [Table 1].
Item Utilization
Lists of the most frequently used materials were generated for each of the following procedure types: adult inguinal hernia repair [Table 2], adult femoral hernia repair [Table 3], adult umbilical hernia repair [Table 4], adult hydrocelectomy [Table 5], adult excision of benign cutaneous mass [Table 6], pediatric inguinal hernia repair [Table 7], and pediatric umbilical hernia repair [Table 8]. Bundles of routinely used items for all procedures [Table 9], adult monitored anesthesia care procedures [Table 10], adult general anesthesia procedures [Table 11], and pediatric general anesthesia procedures [Table 12] were also generated.
Table 2.
Item utilization analysis for adult inguinal hernia repair from a 2012 surgical mission to the Dominican Republic
| Most frequently used items for adult inguinal hernia repair | |
|---|---|
| Material supply item | Quantity per case |
| 18-gauge needle | 4 |
| 22-gauge needle | 1 |
| 30 ml sterile syringe | 1 |
| 10 ml sterile syringe | 2 |
| 5 ml sterile syringe | 1 |
| 3 ml sterile syringe | 3 |
| TB sterile syringe | 1 |
| electric clipper attachment | 1 |
| chlorhexidine applicator: 26 ml | 1 |
| sterile blue towels | 4 |
| latex-free laparotomy T-drape | 1 |
| #15 surgical blade | 1 |
| electrocautery scratch pad | 1 |
| electrocautery wand and holster | 1 |
| electrocautery return electrode | 1 |
| 10-pack of radiograph-detectable gauze: 4 inches × 4 inches | 1 |
| penrose drain | 1 |
| polypropylene hernia mesh with keyhole: 13.7×5.9 cm | 1 |
| 8-pack of 0 braided polyester suture: 18 inches, on a MO-6 needle | 2 |
| 2-0 vicryl suture: 27 inches, on a SH needle | 2 |
| 3-0 vicryl suture: 27 inches, on a SH needle | 2 |
| 4-0 monocryl monofilament suture: 27 inches, on a PS-1 needle | 1 |
| liquid skin adhesive (2-octyl cyanoacrylate) | 1 |
Table 3.
Item utilization analysis for adult femoral hernia repair from a 2012 surgical mission to the Dominican Republic
| Most frequently used items for adult femoral hernia repair | |
|---|---|
| Material supply item | Quantity per case |
| 18-gauge needle | 4 |
| 22-gauge needle | 2 |
| 25-gauge needle | 1 |
| 30 ml sterile syringe | 1 |
| 10 ml sterile syringe | 2 |
| 5 ml sterile syringe | 1 |
| 3 ml sterile syringe | 4 |
| electric clipper attachment | 1 |
| chlorhexidine applicator: 26 ml | 1 |
| sterile blue towels | 4 |
| latex-free laparotomy T-drape | 1 |
| #15 surgical blade | 1 |
| electrocautery scratch pad | 1 |
| electrocautery wand and holster | 1 |
| electrocautery return electrode | 1 |
| 10-pack of radiograph-detectable gauze: 4 inches × 4 inches | 1 |
| penrose drain | 1 |
| polypropylene hernia mesh: 13.7 cm × 5.9 cm or 5 cm × 15 cm | 1 |
| 8-pack of 0 braided polyester suture: 18 inches, on a Mo-6 needle | 2 |
| 3-0 vicryl suture: 27 inches, on a SH needle | 2 |
| 4-0 monocryl monofilament suture: 27 inches, on a PS-1 needle | 1 |
| liquid skin adhesive (2-octyl cyanoacrylate) | 1 |
Table 4.
Item utilization analysis for adult umbilical or small ventral hernia repair from a 2012 surgical mission to the Dominican Republic
| Most frequently used items for adult umbilical or small ventral hernia repair | |
|---|---|
| Material supply item | Quantity per case |
| 18-gauge needle | 4 |
| 22-gauge needle | 1 |
| 25-gauge needle | 1 |
| 30 ml sterile syringe | 1 |
| 10 ml sterile syringe | 2 |
| 5 ml sterile syringe | 1 |
| 3 ml sterile syringe | 4 |
| TB sterile syringe | 1 |
| electric clipper attachment | 1 |
| chlorhexidine applicator: 10.5 ml | 1 |
| sterile blue towels | 4 |
| latex-free laparotomy T-drape | 1 |
| #15 surgical blade | 1 |
| electrocautery scratch pad | 1 |
| electrocautery wand and holster | 1 |
| electrocautery return electrode | 1 |
| 10-pack of radiograph-detectable gauze: 4 inches × 4 inches | 1 |
| polypropylene mesh with bioabsorbable adhesion barrier or composite mesh with bioabsorbable adhesion barrier: medium-size | 1 |
| 8-pack of 0 braided polyester suture: 18 inches, on a Mo-6 needle | 1 |
| 3-0 vicryl suture: 27 inches, on a SH needle | 1 |
| 4-0 monocryl monofilament suture: 27 inches, on a PS-1 needle | 1 |
| liquid skin adhesive (2-octyl cyanoacrylate) | 1 |
Table 5.
Item utilization analysis for adult hydrocelectomy from a 2012 surgical mission to the Dominican Republic
| Most frequently used items for adult hydrocelectomy | |
|---|---|
| Material supply item | Quantity per case |
| 18-gauge needle | 4 |
| 22-gauge needle | 2 |
| 30 ml sterile syringe | 1 |
| 10 ml sterile syringe | 2 |
| 5 ml sterile syringe | 1 |
| 3 ml sterile syringe | 5 |
| TB sterile syringe | 1 |
| chlorhexidine applicator: 26 ml | 1 |
| sterile blue towels | 4 |
| latex-free laparotomy T-drape | 1 |
| #15 surgical blade | 1 |
| electrocautery scratch pad | 1 |
| electrocautery wand and holster | 1 |
| electrocautery return electrode | 1 |
| 10-pack of radiograph-detectable gauze: 4 inches × 4 inches | 1 |
| 2-0 vicryl suture: 27 inches, on a SH needle | 2 |
| 3-0 vicryl suture: 27 inches, on a SH needle | 1 |
| 2-0 chromic cat gut suture on a cutting needle | 1 |
| liquid skin adhesive (2-octyl cyanoacrylate) | 1 |
Table 6.
Item utilization analysis for adult excision of benign cutaneous mass from a 2012 surgical mission to the Dominican Republic
| Most frequently used items for adult excision of benign cutaneous mass | |
|---|---|
| Material supply item | Quantity per case |
| 18-gauge needle | 1 |
| 25-gauge needle | 2 |
| 10 ml sterile syringe | 1 |
| 5 ml sterile syringe | 1 |
| 3 ml sterile syringe | 2 |
| electric clipper attachment | 1 |
| chlorhexidine applicator: 10.5 ml | 1 |
| incision drape: 30 inches × 22 inches | 1 |
| mayo stand reinforced drape: 23 inches × 54 inches × 7 inches | 1 |
| #15 surgical blade | 1 |
| laceration tray | 1 |
| 5-pack of sterile lap sponges: 18 inches × 18 inches | 2 |
| 4-0 vicryl suture: 18 inches on a FS-2 needle or 27 inches on a SH needle | 1 |
| 4-0 monocryl monofilament suture: 27 inches, on a PS-2 needle | 1 |
| benzoin tincture: 0.67 ml | 1 |
| sterile adhesive strip skin closures: | 1 |
| 0.5 inches × 4 inches or 0.25 inches × 3 inches | |
| adhesive wound barrier: 4 inches × 4 inches | 1 |
Table 7.
Item utilization analysis for pediatric inguinal hernia repair from a 2012 surgical mission to the Dominican Republic
| Most frequently used items for pediatric inguinal hernia repair | |
|---|---|
| Material supply item | Quantity per case |
| 18-gauge needle | 1 |
| 22-gauge needle | 2 |
| 10 ml sterile syringe | 2 |
| 5 ml sterile syringe | 1 |
| 3 ml sterile syringe | 4 |
| electric clipper attachment | 1 |
| chlorhexidine applicator: 10.5 ml | 1 |
| sterile blue towels | 4 |
| latex-free laparotomy T-drape | 1 |
| #15 surgical blade | 1 |
| electrocautery scratch pad | 1 |
| electrocautery wand and holster | 1 |
| electrocautery return electrode | 1 |
| 10-pack of radiograph-detectable gauze: 4 inches × 4 inches | 1 |
| 8-pack of 0 braided polyester suture: 18 inches, on a MO-6 needle | 1 |
| 2-0 vicryl suture: 27 inches, on a SH needle | 1 |
| 3-0 vicryl suture: 27 inches, on a SH needle | 1 |
| 4-0 vicryl suture: 27 inches, on a SH needle | 1 |
| 4-0 monocryl monofilament suture: 27 inches, on a PS-1 needle | 1 |
| liquid skin adhesive (2-octyl cyanoacrylate) | 1 |
Table 8.
Item utilization analysis for pediatric umbilical hernia repair from a 2012 surgical mission to the Dominican Republic
| Most frequently used items for pediatric umbilical hernia repair | |
|---|---|
| Material supply item | Quantity per case |
| 18-gauge needle | 1 |
| 22-gauge needle | 2 |
| 25-gauge needle | 1 |
| 10 ml sterile syringe | 2 |
| 5 ml sterile syringe | 1 |
| 3 ml sterile syringe | 4 |
| chlorhexidine applicator: 10.5 ml | 1 |
| sterile blue towels | 4 |
| latex-free laparotomy T-drape | 1 |
| #15 surgical blade | 1 |
| electrocautery scratch pad | 1 |
| electrocautery wand and holster | 1 |
| electrocautery return electrode | 1 |
| 10-pack of radiograph-detectable gauze: 4 inches × 4 inches | 1 |
| 8-pack of 0 braided polyester suture: 18 inches, on a MO-6 needle | 1 |
| 3-0 vicryl suture: 27 inches, on a SH needle | 1 |
| 4-0 monocryl monofilament suture: 27 inches, on a PS-1 needle | 1 |
| liquid skin adhesive (2-octyl cyanoacrylate) | 1 |
Table 9.
Bundle of routinely used material supplies for all procedures from a 2012 surgical mission to the Dominican Republic
| Bundle of routinely used material supplies for all procedures | |
|---|---|
| Material supply item | Quantity per case |
| surgical cap | 1 per member of the operating room team |
| surgical face mask with eye shields | 1 per member of the operating room team |
| sterile latex-free surgical gown | 1 per member of the surgical team |
| sterile pair of latex-free surgical gloves | 2 per member of the surgical team (in appropriate sizes) |
| chlorhexidine or povidone-iodine surgical scrub brushes | 1 per member of the surgical team |
| latex-free examination gloves | 1 per member of the operating room team |
| effervescent cleaning tablet containing fast-acting protease enzymes for scrubbing surgical instruments | 1 |
| autoclave pouches or wrapping paper for surgical instrument trays | 1 (or 4 sheets if wrapping paper) |
| autoclave indicator tape | 1 |
Table 10.
Bundle of routinely used material supplies for adult monitored anesthesia care (MAC) procedures from a 2012 surgical mission to the Dominican Republic
| Bundle of routinely used material supplies for adult MAC procedures | |
|---|---|
| Material supply item | Quantity per case |
| forced air warming blankets: full body | 1 |
| pulse oximetry probe | 1 |
| electrocardiogram electrodes: standard adult-size | 4 |
| adhesive temperature monitoring strip | 1 |
| tourniquet | 1 |
| 20-gauge 1.16-inch shielded intravenous catheter | 1 |
| latex-free intravenous line set: 100 inches | 1 |
| adhesive barrier for intravenous line | 1 |
| 1 liter normal saline bag | 1 |
| oxygen face mask | 1 |
| oxygen tubing | 1 |
| nasal cannula | 1 |
| Yankauer oral suction tip | 1 |
| suction tubing | 1 |
| foam cushions for boney prominences of extremities | 4 |
| self-adhesive straps for upper extremities | 2 |
| safety belt for operating table | 1 |
Table 11.
Bundle of routinely used material supplies for adult general anesthesia procedures from a 2012 surgical mission to the Dominican Republic
| Bundle of routinely used material supplies for adult general anesthesia procedures | |
|---|---|
| Material supply item | Quantity per case |
| forced air warming blankets: full body | 1 |
| pulse oximetry probe | 1 |
| electrocardiogram electrodes: standard adult-size | 4 |
| adhesive temperature monitoring strip | 1 |
| tourniquet | 1 |
| 20-gauge 1.16-inch shielded intravenous catheter | 1 |
| latex-free intravenous line set: 100 inches | 1 |
| adhesive barrier for intravenous line | 1 |
| 1 liter normal saline bag | 1 |
| heat moisture exchanger filter with monitoring port | 1 |
| breathing circuit: adult-size | 1 |
| ventilation mask: adult small or adult standard | 1 |
| laryngeal mask airway or l-gel airway (size 3, 4, or 5) or endotracheal tube with inflatable cuff (7.0 mm, 7.5 mm, 8.0 mm, 8.5 mm, or 9.0 mm internal diameter) | 1 |
| stylet: adult-size | 1 |
| laryngoscope with lamp, blade assortment (Miller or Maclntosh: 3, 4), and batteries | 1 |
| oral airway: 80 mm, 90 mm, or 100 mm | 1 |
| nasal airway: 28 French, 30 French, or 32 French | 1 |
| bag-mask-valve system | 1 |
| Yankauer oral suction tip | 1 |
| nasal cannula | 1 |
| suction tubing | 1 |
| foam cushions for boney prominences of extremities | 4 |
| self-adhesive straps for upper extremities | 2 |
| safety belt for operating table | 1 |
Table 12.
Bundle of routinely used material supplies for pediatric general anesthesia procedures from a 2012 surgical mission to the Dominican Republic
| Bundle of routinely used material supplies for pediatric general anesthesia procedures | |
|---|---|
| Material supply item | Quantity per case |
| forced air warming blankets: full body | 1 |
| pulse oximetry probe | 1 |
| electrocardiogram electrodes: pediatric-size or pediatric defibrillator/monitoring electrodes | 4 or 2, respectively |
| adhesive temperature monitoring strip | 1 |
| tourniquet | 1 |
| 20-gauge 1.16-inch shielded intravenous catheter | 1 |
| latex-free microdrip intravenous line set: 100 inches | 1 |
| adhesive barrier for intravenous line | 1 |
| 0.5 liter normal saline bag | 1 |
| heat moisture exchanger filter with monitoring port | 1 |
| breathing circuit: pediatric-size | 1 |
| ventilation mask: pediatric small, pediatric standard, pediatric large | 1 |
| laryngeal mask airway or l-gel airway (size 1.0, 1.5, 2.0, 2.5) or endotracheal tube with inflatable cuff (4.0 mm, 4.5 mm, 5.0 mm, 5.5 mm, 6.0 mm, or 6.5 mm internal diameter) | 1 |
| stylet: pediatric-size | 1 |
| laryngoscope with lamp, blade assortment (Miller or Maclntosh: 0, 1, 2), and batteries | 1 |
| oral airway: 50 mm, 60 mm, or 70 mm | 1 |
| nasal airway: 12 French, 16 French, 20 French, or 24 French | 1 |
| bag-mask-valve system | 1 |
| nasal cannula | 1 |
| Yankauer oral suction tip | 1 |
| suction tubing | 1 |
| foam cushions for boney prominences of extremities | 4 |
| self-adhesive straps for upper extremities | 2 |
| safety belt for operating table | 1 |
DISCUSSION
Humanitarian organizations have historically played a significant role in addressing unmet surgical need in low and middle-income countries8, and this role is expected to expand in the near future. In Haiti, the nation bordering the Dominican Republic on the island of Hispaniola, foreign humanitarian organizations currently provide greater than 70% of the total healthcare delivery18. With annual expenditure on medical missions conservatively estimated to be $250 million34, global attention is being focused on the accountability of these initiatives, particularly on the efficacy and the improvement of value achieved with diminishing resources18. Recent work by Surgical Outreach for the Americas and others23–35 has demonstrated that surgical interventions can be provided at the global standard of care in a cost-minimized and sustainable manner.
Short-term missions can achieve long-term impacts on the regions served34. In one example, a pediatric craniofacial surgical mission to South Vietnam successfully lowered the age at first operation and reduced the number of adult patients with cleft lip-cleft palate over 11 years42. A strong appreciation of the healthcare environment in the region, prudent planning of the surgical care delivery, and partnership with local health providers for sustainability can enable a humanitarian organization to achieve the 5 essential elements of a mission with significant impact: (1) surgical care must be effective and safe; (2) surgical care must be widely accessible; (3) surgical care must be affordable within the local and national capacity; (4) surgical care must be appropriate for local situations; and (5) the surgical care system must be locally sustainable18,43. As humanitarian organizations begin to demonstrate their ability to deliver cost-effective care, the challenge to these organizations remains the ability to transfer knowledge and skills to the developing region to demonstrate the long-term sustainability of their efforts.
The effective building of surgical capacity in developing regions of the world requires partnerships. The foremost of these partnerships is the one developed between the humanitarian organization and local healthcare workers in the developing region for bilateral knowledge exchange and coordination of efforts. In addition to being the true fulfillment of the mission purpose, this critical partnership expands the reach and cost-effectiveness of the surgical mission far beyond that which could be reached by the humanitarian organization alone24. However, the importance of partnerships among humanitarian organizations must not be understated. Coordinated and goal-directed efforts are needed to significantly impact surgical global health. The failure to do so is wasteful, and has been deemed one of the “seven sins of humanitarian medicine” when it results from competitive humanitarianism45. By coordinating the efforts of multidisciplinary humanitarian organizations providing surgical care, such initiatives could have a synergistic effect on assessing unmet global surgical need; sustaining cost-effective surgical care delivery to meet this need; and advocating for allocation of resources, surgical services, education, and research in the developing world7,45–46.
To successfully build surgical capacity in the developing region, this transfer of knowledge must include the exchange of (1) operational data, (2) epidemiologic data, (3) outcomes and quality improvement data, and (3) surgical skill and research education. This study specifically addresses operational and basic epidemiologic data collection. Systematic data collection and reporting should be strongly encouraged among humanitarian organizations to assess regional surgical needs, to convey valuable process information to the humanitarian community and their healthcare partners in developing regions of the world, and to evaluate operational processes and outcomes for quality improvement8,44. The global health community would be well-served by the development of guidelines for recording humanitarian care, and the establishment of a central repository for such information47. According to a survey of humanitarian organizations, many organizations routinely collect such information for internal use8; however, few organizations report these data for the benefit of the global health community19–33. Disseminating these metrics to the humanitarian community could reduce the time lag between the planning and the execution of medical missions, minimize waste of resources, maximize the healthcare services provided with limited budgets, and improve the quality of care delivered to the underserved patients of the developing world.
Among all procedural expenses, expenditures on material supplies and medications constitute one of the greatest per capita costs for surgical missions35. The continuous need of healthcare missions for medical supplies and medications has historically been satisfied by the purchase of these materials at discounted rates from NPOs that maintain repositories, or the donation of these materials from healthcare institution surpluses and corporate manufacturer inventories nearing expiration. Limited budgets often prohibit purchasing materials at contracted prices from medical supply distributers. Gathering and transporting product can be extremely expensive and labor intensive; therefore, it is imperative that resources and efforts are not wasted gathering unnecessary items18. Furthermore, the increasing demand for these materials and the decreasing supply resulting from the receding economy have made it more difficult to obtain donated materials. Yet, limited resources exist to advise humanitarian organizations about the minimum necessary supplies required to successfully conduct a surgical mission21,33,48–50. In an effort to contribute evidence to this initiative, we conducted an analysis to quantify the material cost-minimization resulting from NPO supply acquisition, and an item utilization analysis to describe the minimum necessary items required to perform hernia repairs and minor procedures at the global standard of care for the underserved patients of the Dominican Republic.
The results of the cost-minimization analysis revealed that supply acquisition at NPO costs leads to significant cost-savings compared to supply acquisition at US academic institution costs from the provider perspective for unilateral inguinal hernia repairs, hydrocelectomies, umbilical hernia repairs, and excisions of benign cutaneous masses for adult patients, and unilateral inguinal hernia repairs for pediatric patients during a surgical mission in the Dominican Republic in 2012. For adult unilateral inguinal hernia repairs, Surgical Outreach for the Americas achieved a significant mean cost-savings of $482.86 ± $683.79 per procedure from material supplies by sourcing most items from NPOs ($62.17 ± 0.74 versus $502.79 ± $684.51 for NPO supply costs versus US academic institution supply costs, respectively; p=0.0002). The two items that contributed greatest to this cost-savings for adult inguinal hernia repairs were the donated mesh and the discounted prophylactic dose of intravenous antibiotics. Surgical Outreach for the Americas incurred a significant mean cost-savings of $120.90 ± $30.51 per procedure from material supplies for adult umbilical hernia repairs ($47.56 ± $31.35 versus $133.05 ± $31.54 for NPO supply costs versus US academic institution supply costs, respectively; p=0.0078). As with adult inguinal hernia repairs, the two items that contributed greatest to the cost-savings for adult umbilical hernia repairs was the donated mesh used to reinforce umbilical hernia defects ≥ 2 cm in diameter and the discounted prophylactic dose of intravenous antibiotics. A significant mean cost-savings of $36.59 ± $17.76 per procedure from material supplies was similarly achieved for adult excisions of benign cutaneous masses ($4.59 ± $13.34 versus $38.55 ± $19.03 for NPO supply costs versus US academic institution supply costs, respectively; p<0.0001). The two items that contributed greatest to the cost-savings for adult excisions of benign cutaneous masses were the discounted sterile surgical drapes and sterile surgical gloves. Surgical Outreach for the Americas incurred a significant mean cost-savings of $127.26 ± $13.18 per procedure from material supplies for adult hydrocelectomies ($53.73 ± $23.66 versus $141.68 ± $14.11 for NPO supply costs versus US academic institution supply costs, respectively; p=0.0039). Likewise, for pediatric inguinal hernia repairs, a significant mean cost-savings of $120.66 ± $14.61 per procedure from material supplies was achieved ($23.92 ± $11.49 versus $134.22 ± $16.61 for NPO supply costs versus US academic institution supply costs, respectively; p=0.0156). Note that the mean cost-savings for pediatric inguinal hernia repairs is not as great in value as that of adult unilateral inguinal hernia repairs since mesh is not used in pediatric hernia repairs and therefore its cost did not contribute to the cost-savings calculations. For both adult hydrocelectomies and pediatric inguinal hernia repairs, the three items that contributed greatest to the cost-savings were the discounted prophylactic dose of intravenous antibiotics, the discounted sterile surgical drapes, and the donated 2-octyl cyanoacrylate liquid skin adhesive.
Likely secondary to the small sample size of 3 cases for each procedure type, the mean cost-savings from material supplies for adult bilateral inguinal hernia repairs and for adult femoral hernia repairs did not achieve statistical significance. Although the mean cost-savings of $332.46 ± $184.09 per procedure for adult bilateral inguinal hernia repairs ($51.85 ± $26.87 versus $351.27 ± $184.20 for NPO supply costs versus US academic institution supply costs, respectively; p=0.2500) and $232.92 ± $ $56.49 per procedure for adult femoral hernia repairs ($55.47 ± $13.44 versus $253.81 ± $54.32 for NPO supply costs versus US academic institution supply costs, respectively; p=0.2500) were not found to be statistically significant, these cost-savings are fiscally and operationally significant to our mission. As with adult unilateral inguinal hernia repairs and adult umbilical hernia repairs, the two items that contributed greatest to the cost-savings for adult bilateral inguinal hernia repairs and adult femoral hernia repairs were the donated mesh and the discounted prophylactic dose of intravenous antibiotics. US academic institution costs exceeded NPO costs for all material supply items with the following notable exceptions: narcotics, antibiotics, and 1 liter normal saline bags for intravenous infusion. Common to each of these items was the fact that each was purchased from the ILAC Center NPO. Although the material supply cost for each of these items was greater when purchased through the ILAC Center, note that the increased material supply cost was offset by the avoidance of shipping and customs fees that would have been incurred if these items were purchased from distributers at US academic institution costs.
Limitations of this study include the limited sample size, and the focus on a single surgical mission trip from one organization. Variations in surgical procedure volume, case mix, item utilization, material costs, and cost-savings may result from different time periods, trips, sampling methods, humanitarian organizations, and host locations. For simplicity, the cost-minimization analyses in this study focused on single-use individually-packaged material supply items and medications, and did not include the cost of reusable material supply items. This focus may therefore have resulted in an underestimation of the total material supply costs and cost-savings. Nevertheless, these data provide important insights regarding cost-savings from material supply procurement through NPO repositories, and minimum necessary items to feasibly perform hernia repairs and minor procedures at the global standard of care in limited-resource settings. The savings incurred by our process of obtaining material supplies from NPO repositories translates to important health gains in terms of the greater number of patients served and the disability and mortality potentially averted. As such, these data constitute the first contribution made by Surgical Outreach for the Americas to the body of operational knowledge shared with the humanitarian community. Through such information exchange with the global health community, we hope to encourage improvements on our experience to catalyze more cost-effective and sustainable surgical care delivery in low-resource medical environments and serve a greater number of patients in the developing world.
Figure 2.
Percent of disability-adjusted life years (DALYs) due to inguinal or femoral hernia in the Dominican Republic (data for both sexes and all ages from year 2010)17. [EN= early neonatal period (0–6 days); LN= late neonatal period (7–28 days); PN= post neonatal period (29–365 days)]
Figure 3.
Percent of years lost to disability (YLDs) due to inguinal or femoral hernia in the Dominican Republic (data for both sexes and all ages from year 2010)17. [EN= early neonatal period (0–6 days); LN= late neonatal period (7–28 days); PN= post neonatal period (29–365 days)]
Figure 4.
Percent of years of life lost (YLLs) due to inguinal or femoral hernia in the Dominican Republic (data for both sexes and all ages from year 2010)17. [EN= early neonatal period (0–6 days); LN= late neonatal period (7–28 days); PN= post neonatal period (29–365 days)]
ACKNOWLEDGEMENTS
Disclaimers:
Funding for this study was provided by the Foundation for Barnes-Jewish Hospital (Saint Louis, Missouri).
JAC is supported by a KM1 Comparative Effectiveness Research (CER) Career Development Award (KM1CA156708) through the National Cancer Institute (NCI) of the National Institutes of Health (NIH); and the Washington University in Saint Louis Clinical and Translational Science Award (CTSA) program (UL1TR000448) through the National Center for Advancing Translational Sciences (NCATS) of the NIH. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NCI, the NCATS, or the NIH.
Footnotes
Presentation: These data were presented during an oral presentation at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) in Baltimore, Maryland in April of 2013.
AUTHOR CONTRIBUTIONS:
Study conception and design: Cavallo, Matthews
Acquisition of data: Cavallo, Ousley, Barrett, Baalman, Ward, Borchardt, Thomas, Perotti, Frisella
Analysis and interpretation of data: Cavallo, Matthews
Drafting of manuscript: Cavallo, Matthews
Critical revision: Cavallo, Ousley, Barrett, Baalman, Ward, Borchardt, Thomas, Perotti, Frisella, Matthews
DISCLOSURE STATEMENTS:
Dr. Cavallo has received research grant funding for unrelated studies from the National Institutes of Health, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), and the American Hernia Society in collaboration with Davol® Incorporated. Dr. Barrett has received non-financial material support for an unrelated research study from Mobisante® Incorporated. Ms. Frisella has received funding from Atrium Medical Corporation® and W. L. Gore and Associates® Incorporated for unrelated service contracts; and research grant funding from the Foundation for Barnes-Jewish Hospital for this research study. Dr. Matthews has served on advisory boards for Musculoskeletal Transplant Foundation, Covidien® Incorporated, and Synthes® Incorporated; has served as a consultant for Atrium Medical Corporation®; has received speaking fess or honoraria from Atrium Medical Corporation®, Davol® Incorporated, Ethicon® Incorporated, W.L. Gore and Associates® Incorporated; has received payments for authorship of an unrelated publication from McMahon Group® Incorporated; has received research grant funding for unrelated research studies from Covidien® Incorporated, Ethicon® Incorporated, Karl Storz Endoscopy America® Incorporated, Kensey Nash Corporation®, Musculoskeletal Transplant Foundation, Synovis Surgical Innovations®, the Society of American Gastrointestinal and Endoscopic Surgeons, and the National Institutes of Health; and has received research grant funding from the Foundation for Barnes-Jewish Hospital for this research study. Ms. Ousley, Ms. Baalman, Dr. Ward, Ms. Borchardt, Mr. Thomas, and Mr. Perotti have no conflicts of interest or financial ties to disclose.
REFERENCES
- 1.Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA. An estimation of the global volume of surgery: a modeling strategy based on available data. Lancet. 2008;372(9633):139–144. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- 2.Ozgediz D, Hsia R, Weiser T, Gosselin R, Spiegel D, Bickler S, Dunbar P, McQueen K. Population health metrics for surgery: effecive coverage of surgical services in low-income and middle-income countries. World J Surg. 2009;33(1):1–5. doi: 10.1007/s00268-008-9799-y. [DOI] [PubMed] [Google Scholar]
- 3.Taira BR, McQueen KA, Burkle FM., Jr Burden of surgical disease: does the literature reflect the scope of the international crisis? World J Surg. 2009;33(5):893–898. doi: 10.1007/s00268-009-9981-x. [DOI] [PubMed] [Google Scholar]
- 4.Debas HT, Gosselin R, McCord C, Surgery Thind A. Disease Control Priorities in Developing Countries. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease Control Priorities Project. 2nd ed. Washington, DC: International Bank for Reconstruction and Development/World Bank; 2006. pp. 1245–1260. [PubMed] [Google Scholar]
- 5.Ozgediz D, Jamison D, Cherian M, McQueen K. The burden of surgical conditions and access to surgical care in low and middle-income countries. Bull World Health Organ. 2008;86(8):646–647. doi: 10.2471/BLT.07.050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg. 2008;32(4):533–536. doi: 10.1007/s00268-008-9525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perkins RS, Casey KM, McQueen KA. Addressing the global burden of surgical disease: proceedings from the 2nd annual symposium at the American College of Surgeons. World J Surg. 2010;34(3):371–373. doi: 10.1007/s00268-009-0338-2. [DOI] [PubMed] [Google Scholar]
- 8.McQueen KA, Hyder JA, Taira BR, Semer N, Burkle FM, Jr., Casey KM. The provision of surgical care by international organizations in developing countries: a preliminary report. World J Surg. 2010;34(3):397–402. doi: 10.1007/s00268-009-0181-5. [DOI] [PubMed] [Google Scholar]
- 9.Mock C, Cherian M, Juillard C, Donkor P, Bickler S, Jamison D, McQueen K. Developing priorities for addressing surgical conditions globally: furthering the link between surgery and public health policy. World J Surg. 2010;34(3):381–385. doi: 10.1007/s00268-009-0263-4. [DOI] [PubMed] [Google Scholar]
- 10.Wang H, Dwyer-Lindgren L, Lofgren KT, Rajaratnam JK, Marcus JR, Levin-Rector A, Levitz CE, Lopez AD, Murray CJ. Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden if Disease Study 2010. Lancet. 2012;380(9859):2071–2094. doi: 10.1016/S0140-6736(12)61719-X. [DOI] [PubMed] [Google Scholar]
- 11.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA, 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, Begum N, Shah R, Karyana M, Kosen S, Farje MR, Moncada G, Dutta A, Sazawal S, Dyer A, Seiler J, Aboyans V, Baker L, Baxter A, Benjamin EJ, Bhalla K, Bin Abdulhak A, Blyth F, Bourne R, Braithwaite T, Brooks P, Brugha TS, Bryan-Hancock C, Buchbinder R, Burney P, Calabria B, Chen H, Chugh SS, Cooley R, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, Davis A, Degenhardt L, Díaz-Torné C, Dorsey ER, Driscoll T, Edmond K, Elbaz A, Ezzati M, Feigin V, Ferri CP, Flaxman AD, Flood L, Fransen M, Fuse K, Gabbe BJ, Gillum RF, Haagsma J, Harrison JE, Havmoeller R, Hay RJ, Hel-Baqui A, Hoek HW, Hoffman H, Hogeland E, Hoy D, Jarvis D, Karthikeyan G, Knowlton LM, Lathlean T, Leasher JL, Lim SS, Lipshultz SE, Lopez AD, Lozano R, Lyons R, Malekzadeh R, Marcenes W, March L, Margolis DJ, McGill N, McGrath J, Mensah GA, Meyer AC, Michaud C, Moran A, Mori R, Murdoch ME, Naldi L, Newton CR, Norman R, Omer SB, Osborne R, Pearce N, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Pourmalek F, Prince M, Rehm JT, Remuzzi G, Richardson K, Room R, Saha S, Sampson U, Sanchez-Riera L, Segui-Gomez M, Shahraz S, Shibuya K, Singh D, Sliwa K, Smith E, Soerjomataram I, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Taylor HR, Tleyjeh IM, van der Werf MJ, Watson WL, Weatherall DJ, Weintraub R, Weisskopf MG, Whiteford H, Wilkinson JD, Woolf AD, Zheng ZJ, Murray CJ, Jonas JB. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2129–2143. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD, Murray CJ. Healthy life expectancy for 187 countries, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2144–2166. doi: 10.1016/S0140-6736(12)61690-0. [DOI] [PubMed] [Google Scholar]
- 14.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gosselin R, Grainger R, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Ma J, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O'Donnell M, O'Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA, 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Years lived with disability (YLDs) for 1160 sequelae of 289 disease and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gonzalez-Medina D, Gosselin R, Grainger R, Grant B, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Laden F, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Levinson D, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mock C, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O'Donnell M, O'Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA, 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiebe N, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, AlMazroa MA, Memish ZA. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 16.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, 3rd, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Hanafiah KM, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, 3rd, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Burden of Disease Compare (GBDCompare) Tool. Seattle, Washington: Institute for Health Metrics and Evaluation (IHME; [[Accessed 11 April 2013]]. Available at: http://viz.healthmetricsandevaluation.org/gbd-compare/ [Google Scholar]
- 18.Pezzella AT. Volunteerism and humanitarian efforts in surgery. Curr Probl Surg. 2006;43(12):848–929. doi: 10.1067/j.cpsurg.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martiniuk ALC, Manouchehrian M, Negin JA, Zwi AB. Brain gains: a literature review of medical missions to low and middle-income countries. BMC Health Services Research. 2012;12:134–141. doi: 10.1186/1472-6963-12-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Negus TL, Brown CJ, Konoske P. Determining medical staffing requirements for humanitarian assistance missions. Mil Med. 2010;175(1):1–6. doi: 10.7205/milmed-d-09-00051. [DOI] [PubMed] [Google Scholar]
- 21.Hartgerink BJ, Chapman LE, Stevenson J, Donahue TF, Pagliara C. Utilization of surgical resources during the USNS COMFORT humanitarian mission to the Americas, June to October 2007. Mil Med. 2010;175(9):638–646. doi: 10.7205/milmed-d-09-00162. [DOI] [PubMed] [Google Scholar]
- 22.Yeow VK, Lee ST, Lambrecht TJ, Barnett J, Gorney M, Hardjowasito W, Lemperle G, McComb H, Natsume N, Stranc M, Wilson L. Internatinoal Task Force on Volunteer Cleft Missions. International Task Force on Volunteer Cleft Missions. J Craniofac Surg. 2002;13(1):18–25. doi: 10.1097/00001665-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Gosselin RA, Maldonado A, Elder G. Comparative cost-effectiveness analysis of two MSF surgical trauma centers. World J Surg. 2010;34(3):415–419. doi: 10.1007/s00268-009-0230-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moon W, Perry H, Baek RM. Is international volunteer surgery for cleft lip and cleft palate a cost-effective and justifiable intervention? A case study from east Asia. World J Surg. 2012;36(12):2819–2830. doi: 10.1007/s00268-012-1761-3. [DOI] [PubMed] [Google Scholar]
- 25.Turaga KK, Garg N, Coeling M, Smith K, Amirlak B, Jaszczak N, Elliott B, Manion J, Filipi C. Inguinal hernia repair in a developing country. Hernia. 2006;10(4):294–298. doi: 10.1007/s10029-006-0111-5. [DOI] [PubMed] [Google Scholar]
- 26.Shillcutt SD, Clarke MG, Kingsnorth AN. Cost-effectiveness of groin hernia surgery in the western region of Ghana. Arch Surg. 2010;145(10):954–961. doi: 10.1001/archsurg.2010.208. [DOI] [PubMed] [Google Scholar]
- 27.Walk RM, Glaser J, Marmon LM, Donahue TF, Bastien J, Safford SD. Continuing promise 2009—assessment of a recent pediatric surgical humanitarian mission. J Pediatr Surg. 2012;47(4):652–657. doi: 10.1016/j.jpedsurg.2011.09.063. [DOI] [PubMed] [Google Scholar]
- 28.Gil J, Rodriguez JM, Hernandez Q, Gil E, Balsalobre MD, Gonzalez M, Torregrosa N, Verdu T, Alcaraz M, Parrilla P. Do hernia operations in African international cooperation programmes provide good quality? World J Surg. 2012;36(12):2795–2801. doi: 10.1007/s00268-012-1768-9. [DOI] [PubMed] [Google Scholar]
- 29.Shillcutt SD, Sanders DL, Butron-Villa MT, Kingsnorth AN. Cost-effectiveness of inguinal hernia surgery in northwestern Ecuador. World J Surg. 2013;37(1):32–41. doi: 10.1007/s00268-012-1808-5. [DOI] [PubMed] [Google Scholar]
- 30.Mainthia R, Tye GW, Shapiro J, Doppenberg EMR, Ward JD. A model for neurosurgical humanitarian aid based on 12 years of medical trips to South and Central America. J Neurosurg Pediatrics. 2009;4(1):4–9. doi: 10.3171/2009.1.PEDS08193. [DOI] [PubMed] [Google Scholar]
- 31.Doman DM, Blair JA, Napierala MA, Cho MS. Do plans and execution agree in a humanitarian medical mission? J Surg Orthop Adv. 2011;20(1):67–73. [PubMed] [Google Scholar]
- 32.Chen AT, Pedtke A, Kobs JK, Edwards GS, Jr., Coughlin RR, Gosselin RA. Volunteer orthopedic surgical trips in Nicaragua: a cost-effectiveness evaluation. World J Surg. 2012;36(12):2802–2808. doi: 10.1007/s00268-012-1702-1. [DOI] [PubMed] [Google Scholar]
- 33.Ramirez-Fort MK, Lastra-Vicente R, Levitt JO, Sanchez JL, Reizner GT. Organizing a dermatology service mission. Int J Dermatol. 2013;52(3):342–349. doi: 10.1111/j.1365-4632.2012.05750.x. [DOI] [PubMed] [Google Scholar]
- 34.Maki J, Qualls M, White B, Kleefield S, Crone R. Health impact assessment and short-term medical missions: a methods study to evaluate quality of care. BMC Health Serv Res. 2008;8:121–128. doi: 10.1186/1472-6963-8-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jha P, Bangoura O, Ranson K. The cost-effectiveness of forty health interventions in Guinea. Health Policy Plan. 1998;13(3):249–262. doi: 10.1093/heapol/13.3.249. [DOI] [PubMed] [Google Scholar]
- 36.The World Factbook 2013. Washington, DC: Central Intelligence Agency; 2013. [[Accessed 14 April 2013]]. Available at: https://www.cia.gov/library/publications/the-world-factbook/geos/dr.html. [Google Scholar]
- 37.Health spending per person by country, World Bank 2002. World Development Indicators 2002. CD-ROM. Washington, DC: World Bank; 2002. [[Accessed 12 April 2013]]. Available at: http://www.NationMaster.com/graph/hea_sp_per_per-health-spending-per-person. [Google Scholar]
- 38.Institute for Latin American Concern (ILAC) Center. Omaha, Nebraska: Creighton University; 2013. [[Accessed 14 April 2013]]. Available at: http://www.creighton.edu/ministry/ilac/ilacmission/mission/index.php. [Google Scholar]
- 39.Smart traveler enrollment program (STEP) Washington, DC: Bureau of Consular Affairs, United States Department of State; 2013. [[Accessed 13 April 2013]]. Available at: https://step.state.gov/step/ [Google Scholar]
- 40.Dominican Republic: country specific information. Washington, DC: Bureau of Consular Affairs, United States Department of State; 2013. [[Accessed 13 April 2013]]. Available at: http://travel.state.gov/travel/cis_pa_tw/cis/cis_1103.html. [Google Scholar]
- 41.Health information for travelers to the Dominican Republic. Atlanta, Georgia: Centers for Disease Control and Prevention, United States Department of Health and Human Services; 2013. [[Accessed 13 April 2013]]. Available at: http://wwwnc.cdc.gov/travel/destinations/dominican-republic.htm. [Google Scholar]
- 42.Uetani M, Jimba M, Niimi T, Natsume N, Katsuki T, Xuan le TT, Wakai S. Effects of a long-term volunteer surgical program in a developing country: the case in Vietnam from 1993 to 2203. Cleft Palate Craniofac J. 2006;43(5):616–619. doi: 10.1597/05-120. [DOI] [PubMed] [Google Scholar]
- 43.Blanchard RJ, Merrell RC, Geelhoed GW, Ajayi OO, Laub DR, Eodas E. Training to serve unmet surgical needs worldwide. J Am Coll Surg. 2001;193(4):417–427. doi: 10.1016/s1072-7515(01)01037-7. [DOI] [PubMed] [Google Scholar]
- 44.Hesslein P, Cushing J. Quality Assurance; Washington, DC. Presentation at the second International Outreach Conference.2004. Mar 20, [Google Scholar]
- 45.Welling DR, Ryan JM, Burris DG, Rich NM. Seven sins of humanitarian medicine. World J Surg. 2010;34(3):466–470. doi: 10.1007/s00268-009-0373-z. [DOI] [PubMed] [Google Scholar]
- 46.Abenavoli FM. Improving humanitarian medical mission efficiacy. Plast Reconstr Surg. 2012;129(3):559e–560e. doi: 10.1097/PRS.0b013e3182419a06. [DOI] [PubMed] [Google Scholar]
- 47.Hilhorst D. Being good at doing good? Quality and accountability of humanitarian NGOs. Disasters. 2002;26(3):193–212. doi: 10.1111/1467-7717.00200. [DOI] [PubMed] [Google Scholar]
- 48.Schneider WJ, Politis GD, Gosain AK, Migliori MR, Cullington JR, Peterson EL, Corlew DS, Wexler AM, Flick R, Van Beek AL. Volunteers in plastic surgery guidelines for providing surgical care for children in the less developed world. Plast Reconstr Surg. 2011;127(6):2477–2486. doi: 10.1097/PRS.0b013e3182131d2a. [DOI] [PubMed] [Google Scholar]
- 49.Eberlin KR, Zaleski KL, Snyder D, Hamdan US. Medical Missions for Children. Quality assurance guidelines for surgical outreach programs: a 20-year experience. Cleft Palate Craniofac J. 2008;45(3):246–255. doi: 10.1597/07-094.1. [DOI] [PubMed] [Google Scholar]
- 50.Hollier LH, Sharabi SE, Koshy JC, Schafer ME, O’Young J, Flood TW. Surgical mission (not) impossible – now what? J Craniofac Surg. 2010;21(5):1488–1492. doi: 10.1097/SCS.0b013e3181edc593. [DOI] [PubMed] [Google Scholar]