Abstract
Background
Among patients with diseases such as HIV, cancer and mental illness, perceived stigma is common and is linked to quality of life (QOL), depression and healthcare seeking behavior. Our clinical experience suggests that stigma is also an important problem among patients with cirrhosis, but no formal studies exist on the topic.
Aims
We aimed to determine the prevalence and consequences of stigma in patients with cirrhosis.
Methods
A survey was developed and mailed to 300 patients with cirrhosis from a variety of etiologies. Among the 149 respondents, stigma was measured using a composite of previously validated scales. Correlates of stigma were measured using an a priori theoretical construct, in order to investigate hypothesized consequences such as impaired social support, depression, and reduction in healthcare seeking behavior.
Results
89% of respondents chose “agree” or “strongly agree” for at least one of the 18 stigma-related questions, indicating they felt stigmatized in at least one aspect of their lives. Patient factors associated with more perceived stigma on multivariable linear regression included younger age (p=0.008), and hepatitis C (p=0.001) or alcohol (p=0.01) as the etiology of liver disease. Patients with higher levels of perceived stigma had less social support (r2=0.898, p<0.001), were less likely to seek medical care (r2=0.108, p<0.001), suffered from more depression (r2=0.17, p<0.001) and had worse QOL (r2=0.175, p<0.001).
Conclusions
Perceived stigma is common among patients with cirrhosis, and is associated with adverse attitudes and behaviors such as decreased healthcare seeking behavior. Healthcare providers need to be aware of these perceptions and their potential impact on patients’ interaction with the medical system.
Keywords: social support, health behavior, stigma, cirrhosis, quality of life
Introduction
The prevalence of cirrhosis is thought to be increasing, related to the aging hepatitis C cohort and rise in fatty liver disease [1]. Liver transplantation is not the solution for everyone, and since the majority of patients live more than a decade after diagnosis[2], cirrhosis should be viewed as a chronic condition with a management focus on optimizing quality of life (QOL).
QOL in cirrhosis is known to be decreased compared to age matched controls [3] even when the cirrhosis is well compensated [4]. This decrement may be partially caused by factors other than the biological effects of liver disease. One such factor is “stigma” which is defined as “a mark of disgrace associated with a particular circumstance, quality, or person”[5]. In patients with hepatitis C (HCV) for example, stigma is associated with depression and anxiety [6] and, in both hepatitis B and HCV, is correlated with worse QOL [7]. In fact, just being informed of the diagnosis of HCV has been shown to worsen QOL in patients with HCV compared to those unaware of their diagnosis [8].
Little is known about stigma in other types of cirrhosis. In our clinical experience, patients who are diagnosed with cirrhosis often comment that they thought “it could only happen to alcoholics.” Qualitative data in HCV have demonstrated that the stigma of intravenous drug use carries over to all patients with HCV, regardless of method of infection [9]. We therefore hypothesize that the stigma associated with socially undesirable behaviors such as drug and alcohol abuse, also carries over to the cirrhotic population at large.
The effects of this stigma are likely to be multi-fold. Consequences of stigma have been well-studied in HIV and include an association with depression [10], relation to decreased adherence to anti-retroviral therapy [11] and correlation with decreased access to care [12]. We hypothesize that stigma exerts similar effects in the cirrhotic population.
In this study, we sought to quantify the presence of stigma among patients with cirrhosis, and to ascertain its association with social support, QOL, and interaction with the healthcare system.
Methods
Survey development
The survey was created to include four theoretical domains within stigmatization: stereotypes, discrimination, shame and social isolation. With these domains in mind, between three and six questions were selected to represent each domain from previously validated and studied surveys of stigma in various other disease states. Six questions were derived from the liver-disease QOL survey [3], four from HIV literature [12], and nine from HIV/cancer literature [13]. If necessary, the questions were altered in order to address “liver disease” as the cause of stigma. In order to address the question of alcohol specifically, we created one question: “Some people assume that because I have liver disease, I must have been a drinker”. This gave a total of 19 stigma-related questions with answer choices based on a four point Likert scale. One question, which addressed work-place discrimination, was dropped from final analysis due to low response (66% were unemployed). Additionally, the survey included the following validated items based upon our a priori hypotheses: PHQ-2 for assessment of depression [14], SF-1 for addressing perception of overall health [15], one question addressing number of disability days, MARS scale addressing medication adherence[16], five questions addressing tendency to seek medical care [17], three addressing social support [18], two direct questions regarding the effects of stigmatization, and an area for comments. Additional data was gathered from the medical record including cause of cirrhosis, gender, age, Child-Turcot-Pugh (CTP) score and duration of time with diagnosis of cirrhosis. CTP was used rather than MELD (Model for End-Stage Liver Disease) scores as it has been shown to be better correlated with QOL [19]. The full survey is available as a Supplement.
Survey Administration
For the purpose of this survey, the various causes of cirrhosis were divided into two categories. The first category included those that are traditionally perceived (justifiably nor not) to be “behavior-related” diagnoses: HCV-related and alcoholic cirrhosis. The second category included what are perceived to be “non behavior-related” diagnoses: non-alcoholic fatty liver disease, cryptogenic, autoimmune, genetic, and other. One hundred and fifty “behavior-related” and one hundred and fifty “non behavior-related” patients were randomly selected from patients enrolled into our center’s Cirrhosis Program. This clinical program prospectively enrolls all patients seen in our liver clinic, with cirrhosis diagnosed by the attending hepatologist, into a registry for chronic disease management. Inclusion criteria for the current study included age greater than or equal to 18 and attendance at a hepatology appointment in the previous year. Exclusion criteria included severe encephalopathy as determined by active confusion or asterixis documented by a hepatologist. Surveys were mailed to each selected patient and a reminder survey was sent to all original non-responders. Participants were assigned random numbers so as to assure anonymity of responses while in the mail system.
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Institutional Review Boards of the University of Michigan. Informed consent was assumed by return of survey (as explained in informational handout included with letter).
Data analysis
Reliability of the stigma scale was determined using Cronbach’s alpha, which was found to be 0.92 for the scale as a whole, implying excellent reliability[20]. Subscale reliability was 0.72 for stereotypes, 0.78 for discrimination, 0.77 for shame, and 0.86 for social isolation. Statistical analysis was performed treating all scales as continuous measures – in other words, an un-weighted average of Likert scores from all questions. This includes the stigma, medication adherence, social support, and care-seeking behavior scales. Sensitivity analysis was performed by dichotomizing responses, but this did not substantially change the results. Depression was treated as a dichotomous variable, based upon an affirmative response to either of the two questions. Pairwise correlations were performed to investigate associations hypothesized in the theoretical model shown in Figure 2. Multivariable linear regression was used to determine patient factors associated with higher degree of perceived stigma; all variables were included in the final model. Standard regression diagnostics demonstrated absence of heteroskedasticity, thus supporting use of linear models. The qualitative comments were analyzed using the methods of qualitative description. Comments were assigned codes independently by two authors (VVS, MLV) corresponding to the stigma subscales (stereotype, discrimination, shame, social isolation), or “not applicable.” Any disagreement was resolved by consensus. The data are reported as the number of comments in each category, along with representative samples.[21]
Results
Baseline Characteristics
Table 1 shows the baseline characteristics of the 149 responders to the 300 surveys sent (response rate 49.7%). The mean age of responders was 58 with 49% male and 92% white. Most patients had mild to moderate cirrhosis (58% CTP class A, 36% CTP class B). 46% of patients had “behavior-related” diagnoses (12 % alcoholic cirrhosis, 34% HCV cirrhosis) and 54% had “non behavior-related” diagnoses (28% fatty liver, 26% other). There were no statistically significant differences in these baseline characteristics between responders and non-responders (data not shown).
Table 1.
Characteristics of Study Participants
| Characteristic | N (%) |
|---|---|
| Gender | |
| Women | 76 (51) |
| Men | 73 (49) |
| Age | |
| 18–39 | 8 (5.4) |
| 40–49 | 15 (10.1) |
| 50–59 | 59 (39.6) |
| 60–69 | 42 (28.2) |
| >70 | 25 (16.8) |
| Diagnosis | |
| Alcoholic Cirrhosis | 18 (12.1) |
| Viral (HCV/HBV) Cirrhosis | 51 (34.2) |
| Fatty Liver Disease | 42 (28.2) |
| Other | 38 (25.5) |
| Race | |
| White | 141 (94.6) |
| Black | 4 (2.7) |
| Hispanic | 0 (0) |
| Other | 4 (2.7) |
| CTP Score | |
| A | 87 (58.4) |
| B | 54 (36.2) |
| C | 8 (5.4) |
HBV- hepatitis B virus, HCV – hepatitis C virus, CTP – Child-Turcotte-Pugh
Demographic characteristics of the 151 non-responders to the survey were not statistically different, with a mean age of 60, 54% male, and 84% white. Etiologies of liver disease among non-responders were alcohol (22%), hepatitis C (31%), NAFLD/cryptogenic (28%) and other (19%).
Perceived Stigma
The overwhelming majority of respondents (89%) indicated they felt stigmatized in at least one aspect of their lives by choosing “agree” or “strongly agree” for at least one of the 18 stigma-related questions. Table 2 shows the proportion of subjects responding affirmatively to each question, organized by sub-scale. After combining all 18 questions into an un-weighted average of the sum of responses on a 4-point scale, the mean stigma score was 2.04 (standard deviation 0.59, range 1–3.28). Patient factors associated with more perceived stigma on multivariable linear regression included younger age (p=0.008) and hepatitis C (p=0.001) or alcohol (p=0.01) as the etiology of liver disease, as shown in Table 2. Forty-seven subjects chose to provide comments; of these, 6 were related to stereotypes, 6 to discrimination, 2 to shame, and 7 to social isolation. The remaining comments were unrelated to stigma, and mostly focused on physical symptoms. Representative comments from each of these domains include:
Table 2.
Proportion of subjects responding “agree” or “strongly agree” to each of the 18 stigma questions, organized by sub-scales.
| Stereotypes | |
| Some people assume that because I have liver disease, I must have been a drinker. | 82% |
| Other people think I am partially to blame for my liver disease. | 72% |
| I feel like some people are concerned that my liver disease could be contagious. | 64% |
| I feel like other people think I am a bad person because I have liver disease. | 61% |
| Discrimination | |
| People with liver disease are looked down upon by society. | 70% |
| Some doctors or nurses don’t like taking care of patients with liver disease. | 63% |
| I feel I have been treated with less respect by others because of my liver disease. | 60% |
| Shame | |
| I feel like I am partially to blame for my liver disease. | 72% |
| I feel less competent that I did before I was diagnosed with liver disease. | 72% |
| Because of my liver disease, I feel flawed and incomplete. | 70% |
| Because of my liver disease, I sometimes feel useless. | 66% |
| Social Isolation | |
| I avoid telling other people about my liver disease. | 75% |
| I feel lonely more often than usual because of my liver disease. | 64% |
| I feel like I am an outsider because of my liver disease. | 64% |
| I avoid doing some things in public because of my liver disease. | 63% |
| My liver disease makes me stand out to other people. | 60% |
| Some people avoid me because of my liver disease. | 58% |
| I feel abandoned by family members because of my liver disease. | 55% |
“I got admitted…in the unit where I work…One of our pulmonary doctors went around asking my friends and other co-workers whether I drink alcohol or not. When told that I don’t and never drink, he insisted maybe I was a closet drinker. Regardless that I am diagnosed with [Auto Immune] liver disease, in his mind, I have it, therefore I am an alcoholic. I don’t know if he also thought I use street drugs.”
“Many medical personnel (Drs., nurses, nutritionists) are uninformed about liver disease that is non-alcoholic related and assume it is. I feel pain involved is undertreated and not believed by medical personnel due to thinking I already have a substance abuse problem. Why don’t they just automatically test us for drugs/ETOH then we can move on to my care and concerns. Not the concerns of ETOH.”
“I believe people and even some friends prejudge me as a drunk or a heavy drinker. When they first hear about my liver problems, you can see the prejudgment that I drink a lot and do not take care of myself. Non-verbal communication that comes over them and their facial look. First impressions are always the strongest and most difficult to overcome.”
“Before being diagnosed with Hep C, I was a productive public figure. I tried to hide my diagnosis. When my liver disease and Hep C leaked I had a hard time with the stigma. I used to work with children…I’m sure parents would be concerned if they thought their child had been exposed… I’m horribly embarrassed at having cirrhosis and always have to add to Drs. “I’m not a drinker or drug addict”… I have a few friends who have…mentioned that the liver and liver disorders reflect certain personal issues…as if I have somehow contributed to my own cirrhosis!”
“I now live in [small town] and no one really has heard about autoimmune hep[atitis] and it is making me feel really down and like an outsider.”
“I take full responsibility for causing my liver disease.”
“Due to swollen liver area some think I’m pregnant even though I’m well past the age of menopause. Can be a little embarrassing to be asked when due.”
Associations with Stigma
As shown in Figure 2, patients with higher levels of perceived stigma had less social support (r2=0.898, p<0.001) and were less likely to seek medical care (r2=0.108, p<0.001). When asked directly, 22% of patients said they avoided seeking medical care for fear of being judged. Patients with higher levels of stigma also suffered from more depression (r2=0.17, p<0.001), which was associated with worse QOL (r2=0.175, p<0.001). Stigmatized patients were less likely to be adherent with medications, though this was not statistically significant (r2=0.025, p= 0.06).
Discussion
This study found that the majority (89%) of patients with cirrhosis perceive at least some stigmatization related to their disease. Furthermore, with increasing sense of stigma there was more depression, lower social support, a decrease in QOL, and a decreased tendency to seek medical care. Thus, stigma is not only common in this population, but it may have deleterious consequences.
These findings are consistent with previous research in other disease states, specifically HIV and HCV, which have shown that in those diseases stigma has a broad range of downstream affects. Further supporting evidence comes from the Liver-Disease QOL scale, which found that stigma predicted 8.8% of variance of overall perceived health in subgroup analysis [3]. Based on HCV research, we hypothesized that there would be some stigmatization carried over into the cirrhotic population at large. However, we found an even higher degree of stigma than may be accounted for just by overlap with HCV. For example, 22% of our patients stated they avoided seeking medical care for fear of being judged, a number even higher than the 9% who felt stigmatized by their doctors in HCV literature [22].
Even among physicians, cirrhosis is considered an “un-prestigious” disease ranking third lowest of all diseases in one survey, even less prestigious than depression, schizophrenia and AIDS [23]. High levels of stigmatization may be in part due to the common misconception that all patients with cirrhosis must have a history of substance abuse. In our survey, 59.9% of patients said they had been assumed to be alcoholics due to their cirrhosis despite only 12.1% having a diagnosis of alcoholic cirrhosis. In fact, this question was the most-likely question to be answered affirmative out of all of the stigma-related questions, even by those patients who were considered to have a “non-behavior related” diagnosis (52.5% answering affirmatively). Alcoholism is known to be one of the most severely stigmatized diseases, even more so than psychiatric illnesses, a result thought to be secondary to societal blaming of patients for their disease and the continued perception that alcoholism is self-caused, not a mental or medical illness [24]. This relationship to alcoholism is consistent with our finding that a very high degree of variance in social support is accounted for by stigma (89.8%) as alcoholism is known to cause alienation and result in subsequent low social support [25].
One surprising finding was that younger patients experience more stigma despite adjustment for confounders; we had frankly hypothesized the opposite. Possible reasons for this finding include higher overall emotional distress from experiencing illness at a young age, or possibly generational differences in expectations regarding doctor-patient communication and health care delivery.
Limitations of this study include those common to most surveys, including nonresponse bias and measurement error. We used previously validated stigma questions where possible in order to minimize use of leading questions and improve validity of questions. The response rate was comparable to other mailed surveys [11]. By pre-dividing our list into separate categories, we were able to capture inherent differences between groups with and without a predominance of substance abuse history, which we feel is a strength of this study. We were also limited in our ability to collect data by desire to keep the survey concise and minimize response burden. It is important to emphasize that this was a cross-sectional study, and while stigma is correlated with domains such as healthcare seeking behavior, these associations are not necessarily causative. Further studies using a longitudinal design are warranted, and should include a larger sample size to permit investigation of relationships between these domains using pathway analysis or structural equation modeling. Finally, this was a single-center study of a demographically homogenous sample, and we did not assess the extent to which patients experience stigma through their contact with our center versus other medical centers. Future studies might investigate whether patients receiving care at high volume liver centers experience less stigmatization than those receiving care at low volume centers.
In conclusion, our study shows that cirrhosis is a highly stigmatized disease, and this stigma may lead to adverse health behaviors. Healthcare providers need to be aware of these perceptions and their potential impact on patients’ interaction with the medical system, and should consider specifically addressing stigma when discussing the disease and treatment course. We speculate that these findings might also reflect a bias against liver disease among the general public, which could affect research funding and support for public programs. The American Association for the Study of Liver Diseases and the American Liver Foundation might consider public advertising campaigns aimed at mitigating negative perceptions of liver disease. In addition, future research could lead to interventions aimed at preventing negative effects of stigma in this population.
Figure 1. Conceptual Model of Stigma.
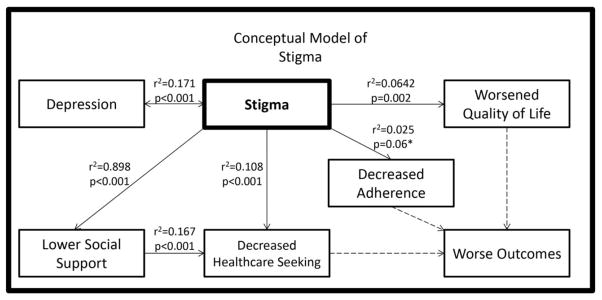
Correlations between Stigma and the various subgroups of the survey (solid arrows) as well as their hypothesized relation with outcomes (dashed arrows). The p-value associated with adherence (ns) is not statistically significant.
Table 3.
Patient characteristics associated with more perceived stigma in multivariable analysis
| Coefficient | P-value | |
|---|---|---|
| Age (per year) | −.012 | 0.008 |
| Male gender | −.106 | 0.33 |
| CTP score | .024 | 0.78 |
| Months since diagnosis | .0005 | 0.68 |
| White race (vs all others) | .146 | 0.42 |
| Hepatitis C (vs Other etiology) | .447 | 0.001 |
| Alcohol (vs Other etiology) | .465 | 0.01 |
CTP – Child-Turcotte-Pugh. Coefficient should be interpreted as increase in stigma score (range 1–4). P<0.05 was the threshold used for statistical significance.
Acknowledgments
we would like to thank Natalie Fisher and Selwan Edward, MD, for their assistance with survey administration.
Financial support: This work was supported in part by K23DK085204 from the National Institutes of Health (MLV).
References
- 1.Davis GL, Alter MJ, El-Serag H, Poynard T, Jennings LW. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology. 2010;138:513–521. 521 e511–516. doi: 10.1053/j.gastro.2009.09.067. [DOI] [PubMed] [Google Scholar]; Davis GL, Roberts WL. The healthcare burden imposed by liver disease in aging Baby Boomers. Curr Gastroenterol Rep. 2010;12:1–6. doi: 10.1007/s11894-009-0087-2. [DOI] [PubMed] [Google Scholar]
- 2.Gines P, Quintero E, Arroyo V, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7:122–128. doi: 10.1002/hep.1840070124. [DOI] [PubMed] [Google Scholar]
- 3.Gralnek IM, Hays RD, Kilbourne A, et al. Development and evaluation of the Liver Disease Quality of Life instrument in persons with advanced, chronic liver disease--the LDQOL 1. 0. Am J Gastroenterol. 2000;95:3552–3565. doi: 10.1111/j.1572-0241.2000.03375.x. [DOI] [PubMed] [Google Scholar]
- 4.Spiegel BM, Younossi ZM, Hays RD, Revicki D, Robbins S, Kanwal F. Impact of hepatitis C on health related quality of life: a systematic review and quantitative assessment. Hepatology (Baltimore, Md ) 2005;41:790–800. doi: 10.1002/hep.20659. [DOI] [PubMed] [Google Scholar]
- 5.Oxford Dictionaries. City: Oxford University Press; Apr, 2010. Stigma. [Google Scholar]
- 6.Golden J, Conroy RM, O’Dwyer AM, Golden D, Hardouin JB. Illness-related stigma, mood and adjustment to illness in persons with hepatitis C. Social science & medicine (1982) 2006;63:3188–3198. doi: 10.1016/j.socscimed.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Drazic YN, Caltabiano ML. Chronic hepatitis B and C: Exploring perceived stigma, disease information, and health-related quality of life. Nursing & health sciences. 2012 doi: 10.1111/nhs.12009. [DOI] [PubMed] [Google Scholar]
- 8.Rodger AJ, Jolley D, Thompson SC, Lanigan A, Crofts N. The impact of diagnosis of hepatitis C virus on quality of life. Hepatology (Baltimore, Md ) 1999;30:1299–1301. doi: 10.1002/hep.510300504. [DOI] [PubMed] [Google Scholar]
- 9.Butt G, Paterson BL, McGuinness LK. Living with the stigma of hepatitis C. Western journal of nursing research. 2008;30:204–221. doi: 10.1177/0193945907302771. discussion 222–233. [DOI] [PubMed] [Google Scholar]
- 10.Grov C, Golub SA, Parsons JT, Brennan M, Karpiak SE. Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS care. 2010;22:630–639. doi: 10.1080/09540120903280901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peretti-Watel P, Spire B, Pierret J, Lert F, Obadia Y. Management of HIV-related stigma and adherence to HAART: evidence from a large representative sample of outpatients attending French hospitals (ANRS-EN12-VESPA 2003) AIDS care. 2006;18:254–261. doi: 10.1080/09540120500456193. [DOI] [PubMed] [Google Scholar]
- 12.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. Journal of general internal medicine. 2009;24:1101–1108. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of health and social behavior. 2000;41:50–67. [PubMed] [Google Scholar]
- 14.Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) Journal of psychosomatic research. 2005;58:163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE., Jr Scales for measuring general health perceptions. Health services research. 1976;11:396–415. [PMC free article] [PubMed] [Google Scholar]
- 16.Ediger JP, Walker JR, Graff L, et al. Predictors of medication adherence in inflammatory bowel disease. Am J Gastroenterol. 2007;102:1417–1426. doi: 10.1111/j.1572-0241.2007.01212.x. [DOI] [PubMed] [Google Scholar]
- 17.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA : the journal of the American Medical Association. 1995;274:305–311. [PubMed] [Google Scholar]
- 18.Norbeck JS, Lindsey AM, Carrieri VL. Further development of the Norbeck Social Support Questionnaire: normative data and validity testing. Nursing research. 1983;32:4–9. [PubMed] [Google Scholar]
- 19.Kanwal F, Hays RD, Kilbourne AM, Dulai GS, Gralnek IM. Are physician-derived disease severity indices associated with health-related quality of life in patients with end-stage liver disease? The American journal of gastroenterology. 2004;99:1726–1732. doi: 10.1111/j.1572-0241.2004.30300.x. [DOI] [PubMed] [Google Scholar]
- 20.Cronbach LJ. A case study of the split-half reliability coefficient. Journal of education & psychology. 1946;37:473–480. doi: 10.1037/h0054328. [DOI] [PubMed] [Google Scholar]
- 21.Neergaard MA, Olesen F, Andersen RS, Sondergaard J. Qualitative description - the poor cousin of health research? BMC medical research methodology. 2009;9:52. doi: 10.1186/1471-2288-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zickmund S, Hillis SL, Barnett MJ, Ippolito L, LaBrecque DR. Hepatitis C virus-infected patients report communication problems with physicians. Hepatology (Baltimore, Md ) 2004;39:999–1007. doi: 10.1002/hep.20132. [DOI] [PubMed] [Google Scholar]
- 23.Album D, Westin S. Do diseases have a prestige hierarchy? A survey among physicians and medical students. Social science & medicine (1982) 2008;66:182–188. doi: 10.1016/j.socscimed.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol and alcoholism (Oxford, Oxfordshire) 2011;46:105–112. doi: 10.1093/alcalc/agq089. [DOI] [PubMed] [Google Scholar]
- 25.Room R. Stigma, social inequality and alcohol and drug use. Drug and alcohol review. 2005;24:143–155. doi: 10.1080/09595230500102434. [DOI] [PubMed] [Google Scholar]


