Abstract
Background
Effects of beta-blockers on the prognosis of the heart failure patients with preserved ejection fraction (HFpEF) remain controversial. The aim of this meta-analysis was to determine the impact of beta-blockers on mortality and hospitalization in the patients with HFpEF.
Methods
A search of MEDLINE, EMBASE, and the Cochrane Library databases from 2005 to June 2013 was conducted. Clinical studies reporting outcomes of mortality and/or hospitalization for patients with HFpEF (EF ≥ 40%), being assigned to beta-blockers treatment and non-beta-blockers control group were included.
Results
A total of 12 clinical studies (2 randomized controlled trials and 10 observational studies) involving 21,206 HFpEF patients were included for this meta-analysis. The pooled analysis demonstrated that beta-blocker exposure was associated with a 9% reduction in relative risk for all-cause mortality in patients with HFpEF (95% CI: 0.87 – 0.95; P < 0.001). Whereas, the all-cause hospitalization, HF hospitalization and composite outcomes (mortality and hospitalization) were not affected by this treatment (P = 0.26, P = 0.97, and P = 0.88 respectively).
Conclusions
The beta-blockers treatment for the patients with HFpEF was associated with a lower risk of all-cause mortality, but not with a lower risk of hospitalization. These finding were mainly obtained from observational studies, and further investigations are needed to make an assertion.
Introduction
Epidemiological data reveals that approximately 50% of chronic heart failure (HF) patients have normal or only mildly impaired left ventricular ejection fraction (EF), which is referred to as the HF with preserved EF (HFpEF) patients [1]. As the life expectancy increases and the population ages, the prevalence of HFpEF continues to increase [2]. More importantly, the prognosis of HFpEF patients remains poor, which is similar to that of HF patients with reduced ejection fraction (HFrEF) [3]. Thus, HFpEF is a growing major problem in public health in the world. However, efficacious therapies on HFpEF have not been well established.
Beta-blockers are a kind of drugs that inhibit sympathetic nervous system activity. It has been shown that patients with HFrEF receive significant benefits from the treatment [4], [5]. In contrast, the benefits of beta-blockers on mortality and hospitalization in patients with HFpEF have not been confirmed [6]. Currently, there is no consensus on the effect of beta-blockers in HFpEF. For instances, some observational studies demonstrated the beta-blockers treatment decreased the risks of all-cause mortality in the HFpEF patients [7]–[9], while the reduction was not observed in the sub-analysis of SENIORS trial [10] and J-DHF trial [11]. However, a small observational study has suggested that the prescription of beta-blockers increases the risk for hospitalization in the HFpEF patients [12]. Although a previous meta-analysis addressed the effects of pharmacotherapies (including beta-blockers) in the HFpEF patients [13], they used the threshold of an EF ≥ 35% as the diagnosis of the HFpEF patients, which is usually not considered “preserved.” In addition, several studies have been published since the previous meta-analysis was performed.
Given the limited evidence and uncertain effects of beta-blockers in the patients with HFpEF, this meta-analysis summarized the current data from randomized controlled trials (RCTs) and observational studies (OSs) to determine the impact of the beta-blockers treatment on mortality and hospitalization in the patients with HFpEF (an EF ≥ 40%).
Methods
This meta-analysis was performed and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [14] and the reporting Meta-Analyses of Observational Studies in Epidemiology (MOOSE) [15].
Literature search
We conducted MEDLINE, EMBASE, and the Cochrane Library databases searches for the published clinical studies from 2005 through June 2013 using the following search terms: 1) heart failure with preserved ejection fraction or heart failure with normal ejection fraction or diastolic heart failure, 2) beta-blockers. Our literature search was limited to studies involving human subjects and those published in English. We manually searched the references that were cited in other relevant publications.
Inclusion criteria
Inclusion criteria were: (1) assessment of the effectiveness of beta-blockers in the patients with HFpEF which had an EF ≥ 40%, (2) randomized controlled trials or nonrandomized controlled studies that provide information on the mortality and/or hospitalization, (3) studies that had a non-beta-blockers control group, (4) the duration of follow-up was at least 6 months.
Data extraction
Information about the study and patient characteristics, methodological quality, intervention strategies, and clinical outcomes was systematically extracted separately by two reviewers. Disagreements were resolved by consensus.
Methodological Quality
The quality of random control trial included was assessed by the Jadad quality scale [16]. The quality of the observational studies was evaluated by Newcastle-Ottawa Scale tool (available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp).
Statistical Analysis
The relative risks (RRs) and 95% CI were used as the common measure across the studies. The hazard ratios (HRs) were considered equivalent to RRs [17]–[19]. If the effect estimates were not available in the studies included, the RRs were calculated by using the following formula: RR = Probability of events given treatment/Probability of events given no-treatment. If the studies provided the adjusted estimations, they were directly used in the meta-analysis. Statistical heterogeneity was tested by the Cochran Q statistic and reported as I2-value for every outcome [20]. The RRs were pooled using the fixed-effect models (Mantel-Haenszel method) in the absence of heterogeneity among studies (I2-value less than 50%). In the presence of heterogeneity, the RRs were pooled using a random-effects model (DerSimonian and Laird method) [21]. The publication bias was assessed by Begg’s test [22]. A significance level of alpha = 0.05 was used.
A sensitivity analysis was conducted by removing one study from the total studies in each round and evaluating the influence of each single study on the primary meta-analysis result. The outcomes of all-cause mortality according to the selected study characteristics were assessed by subgroup analysis. All analyses were performed by statistical program Stata (version 11.2, Stata Corp, College Station, Texas) and R software (version. 3.0.1, available at: http://www.r-project.org/).
Results
Search results
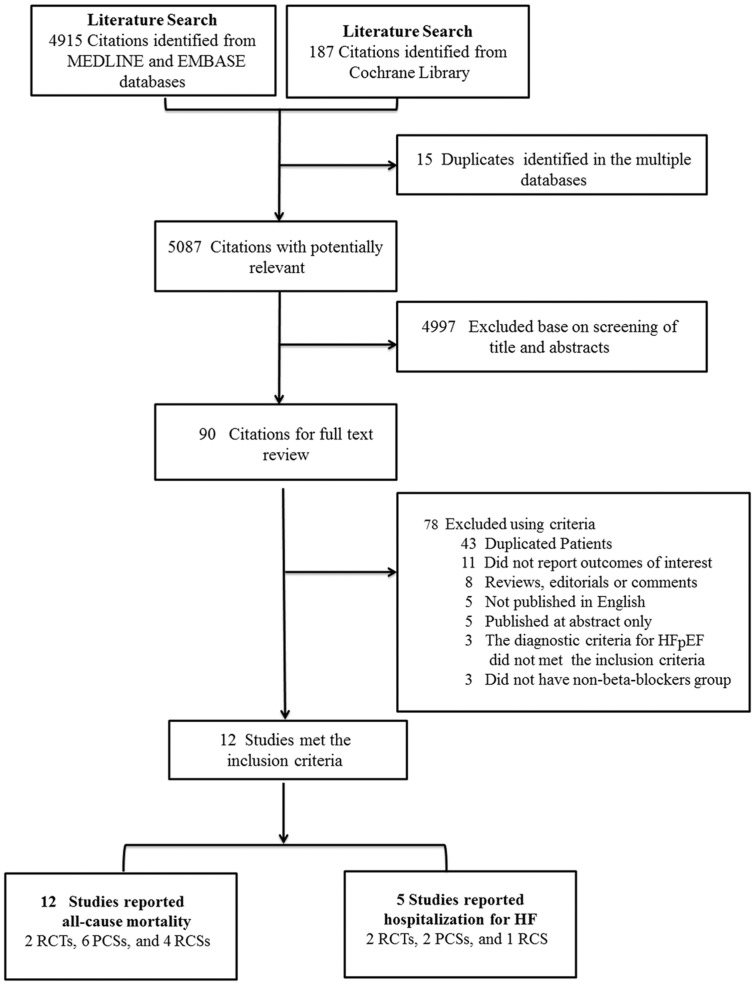
Figure 1 displays the flow diagram of study selection. Our initial search yielded 4,915 citations from MEDLINE and EMBASE databases, and 187 citations from Cochrane Library. After screening the titles and abstracts of all studies identified by the search strategy, 90 potentially relevant articles were further screened for the eligibility. Finally, 2 randomized control trials [10], [11] and 10 observational studies [7]–[9], [12], [23]–[28] were included.
Figure 1. Flowchart of study search and selection in this meta-analysis.
PCSs, prospective cohort studies; RCSs, retrospective cohort studies; RCTs, randomized controlled trials;
Characteristics and quality of study included
The characteristics of the studies included are presented in Table 1. Of the 12 studies included, 2 studies were randomize-controlled design [10], [11] (one from the sub-analysis), 6 studies were prospective cohort design [7], [12], [23]–[26], and 4 studies were retrospective design [8], [9], [27], [28]. The definition of HFpEF differed across the included studies, with an EF ≥ 40% in 5 studies and EF ≥ 50% in 7 studies. 4 studies included the elderly HFpEF patients only.
Table 1. Studies characteristics of the included studies.
| Study | Year | Study design | Definition of HFPEF (LVEF) | Entry age (years) | Sample size | Beta-blockers group (N) | Non-beta-blocker group (N) | Mean follow-up (years) | Outcomes | estimate effect | Adjusted |
| SENIORS [10] | 2009 | RCT | > 40% | >70 | 643 | 320 | 323 | 1.75 | All-cause mortality and HF hospitalization | HR | Yes |
| J-DHF [11] | 2013 | RCT | > 40% | > 20 | 245 | 120 | 125 | 3.2 | Mortality and hospitalization for HF | RR | Yes |
| Fukuta H [23] | 2005 | PCS | ≥ 50% | NA | 137 | 68 | 69 | 1.75 | Death | RR | Yes |
| Chan, J. D [24] | 2005 | PCS | ≥ 40% | > 65 | 342 | NA | NA | 2.3 | All-cause mortality | HR | Yes |
| Grigorian SL [25] | 2005 | PCS | > 50% | NA | 416 | 98 | 318 | 4.57 | Death | HR | Yes |
| OPTIMIZE-HF [26] | 2009 | PCS | > 40% | NA | 4153 | 1621 | 2532 | 1 | Mortality or readmission | HR | Yes |
| Farasat SM [12] | 2009 | PCS | ≥ 50% | > 18 | 66 | 43 | 23 | 0.5 | All-cause mortality and HF hospitalization | RR | No |
| Dobre D [7] | 2010 | PCS | ≥ 40% | > 30 | 443 | 227 | 216 | 2.08 | All-cause death | HR | Yes |
| Tehrani F [27] | 2008 | RCS | ≥ 50% | > 80 | 142 | 51 | 91 | 5 | Death | RR | No |
| R Shah [8] | 2008 | RCS | > 50% | > 65 | 13533 | 4562 | 8971 | 3 | Death | RR | Yes |
| NevzorovRV [28] | 2012 | RCS | ≥ 50% | > 18 | 345 | 154 | 191 | 2 | Mortality | HR | Yes |
| El-Refai M [9] | 2013 | RCS | ≥ 50% | > 18 | 741 | 570 | 171 | 2.1 | Death or hospitalization | HR | Yes |
HR: Hazard ratio; PCS: prospective cohort study; RCS: retrospective cohort study; RCT: randomized controlled trial; RR: relative risk; NA: not available.
Among a total of 21,206 patients, 7,834 patients were in the beta-blockers group and 13,030 patients in the control group (Note: Chan’s study did not provide the exact data of the two groups). There were only 5 studies that provided the data regarding hospitalization [9]–[12], [26]. The mean follow-up period, ranging from 0.5 to 4.57 years, was similar between the beta-blockers and the non-beta-blockers group. The effect estimations of hazard ratios (HRs) were provided in 7 studies and RRs in 5 studies, which were adjusted for the baseline characteristics.
Of the two RCTs included, the Jadad score was 4 in the SENIORS trials and 2 in the J-DHF trials. The quality of the included OSs assessed by Newcastle-Ottawa Scale tool was displayed in Table S1 (median score, 7; range, 5 to 8).
Patient characteristics
Patient characteristics of the studies included are presented in Table 2. The mean age of the patients with HFpEF was 77.7 years. Among them, 59.8% were female with the mean LVEF of 55.8%. Ischemic etiology was the primary cause for HF in 48.3% of the patients. The prevalence of hypertension, diabetes mellitus, atrial fibrillation and chronic obstructive pulmonary disease (COPD) was 70.7, 37.0%, 35.5% and 37.8%, respectively. Baseline medication included ACEI/ARB in 50.3% of the patients, diuretics in 75.6%, nitrates in 37.3%, and digoxin in 22.3%.
Table 2. Patients characteristics of the included studies.
| Study | SENIORS[10]† | J-DHF[11] | FukutaH[23] | Chan, J. D[24]‡ | Grigoria SL[25] | OPTIMIZE-HF[26] | FarasatSM[12] | Dobre D[7] | Tehrani F[27] | R Shah[8] | Nevzorov R[28] | El-Refai M[9] |
| Year | 2009 | 2013 | 2005 | 2005 | 2006 | 2009 | 2009 | 2007 | 2008 | 2008 | 2012 | 2013 |
| Mean age, years * | 76(5) | 72(11) | 65(14) | 80(5) | 73(10) | 81 | 71(13) | 78(10) | 87(5) | 80 | 77(11) | 71(12) |
| Type of beta-blockers | Nebivolol | Carvedilol | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Dose of beta-blockers | Starting with 1.25mg/d to 10mg/d | 7.5 mg/d | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Female,% | 49.9 | 42 | 57 | 50.3 | 51 | 31.6 | 8.2 | 55.5 | 69 | 70 | 58.8 | 60.6 |
| LVEF,% | 49(10) | 63(11) | 62(7) | NA | >50 | NA | NA | ≥40 | 60(10) | NA | NA | 57 (5) |
| History of MI,% | 34.4 | NA | NA | 60.5 | NA | NA | NA | 36.1 | 44 | 21 | 13.3 | NA |
| Ischemic etiology, % | 76.9 | 14.7 | 58 | 84.7 | 41.1 | NA | 48.5 | NA | 44 | 48 | 51.3 | 25.5 |
| Hypertension,% | 77.7 | 80.4 | 80 | 63.7 | 60.8 | NA | 89.4 | 49.4 | 75 | 71 | 69.8 | 73.4 |
| Diabetes mellitus,% | 24.3 | 3.6 | 23 | 16.8 | 26.9 | 36.6 | 54.5 | 28.7 | 26 | 39 | 40 | 46.4 |
| Atrial fibrillation (%) | 36.6 | 40.8 | NA | 23.6 | NA | 35.2 | NA | 44.5 | NA | NA | 44.9 | 29.8 |
| COPD (%) | NA | NA | NA | 14.7 | NA | 28.2 | NA | 28.4 | NA | 33 | NA | 39 |
| Anemia (%) | NA | NA | NA | NA | 37.8 | 19.7 | NA | 54.4 | 54 | NA | 32.5 | NA |
| Medication | ||||||||||||
| Statin | 13.3 | NA | NA | 12.7 | NA | 28 | NA | NA | 22 | 17 | 23.7 | NA |
| ACEI/ ARB, % | 91.5 | 23.3 | 55 | 44.5 | 50.5 | 58.2 | NA | 77.4 | 47 | 47 | 46.96 | 26 |
| Aspirin,% | NA | 20.4 | NA | 65.8 | 28.1 | 48.9 | NA | NA | NA | 41 | 36.8 | NA |
| Diuretics,% | 83.1 | 60 | 50 | 52.9 | 66.1 | 80.4 | NA | 88 | 62 | NA | 48.13 | NA |
| CCB,% | NA | NA | 27 | 27.4 | 31 | NA | NA | 15.3 | 33 | NA | 25.2 | NA |
| Nitrates,% | NA | NA | NA | 45.9 | 36.8 | NA | NA | 46.5 | 20 | NA | 24.7 | NA |
| Digoxin,% | NA | 20.4 | NA | 36.3 | 22.1 | 21.9 | NA | 22.1 | 30 | NA | 11.6 | NA |
| Mineralocorticoid receptor blockers,% | 5.6 | 23.3 | NA | NA | NA | 8.0 | 6.1 | 40.6 | NA | NA | 20.0 | NA |
*The values were given as mean (standard deviation), †the values were presented as the patients with an EF ≥ 35% among the participants who used the beta-blockers treatment, ‡the values were presented as the participants who used the beta-blockers treatment. ACEI: angiotensin-converting enzyme inhibitor; ARBs: angiotensin-receptor blockers; CCB: calcium channel blockers; COPD: chronic obstructive pulmonary disease; LVEF: left ventricular ejection fraction; MI: myocardial infarction; NA: not available.
Effect of beta-blockers on all-cause mortality
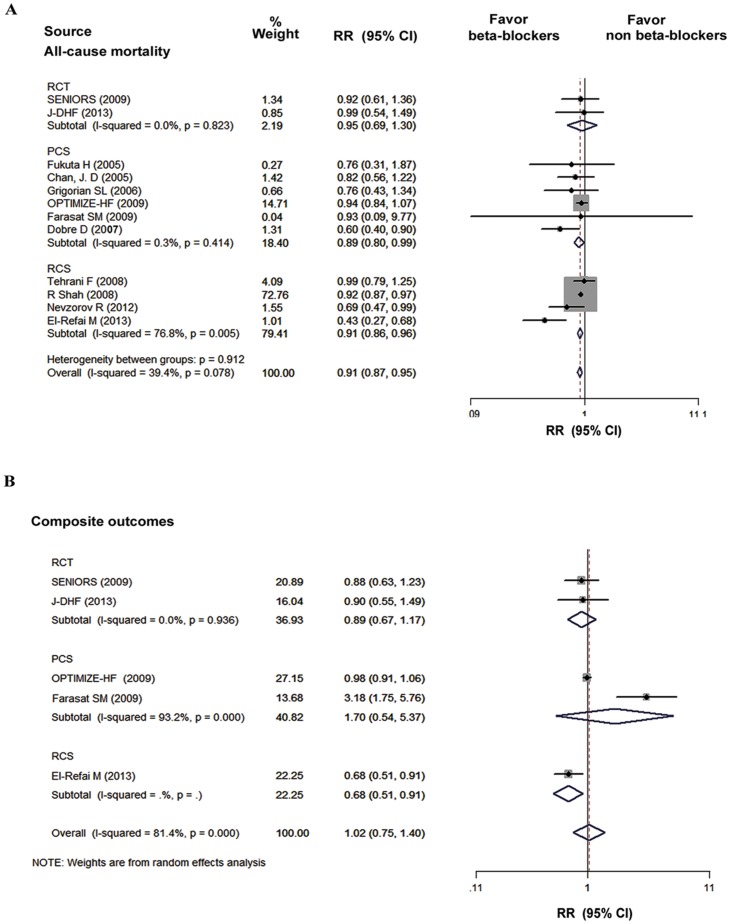
Figure 2 displays the results of the pooled analyses of all studies that reported the outcomes of all-cause mortality and composite outcomes. Of the 12 studies that reported the mortality and hospitalization, only 4 studies showed that beta-blocker treatment was associated with a significantly lower risk of all-cause mortality in HFpEF patients. There was a 5% decrease in risk of all-cause mortality from the RCT (I2 = 0%, RR, 0.95; 95% CI, 0.69 to 1.30; P = 0.73), a 11% reduction from the prospective cohort studies (I2 = 0.3%, RR, 0.89; 95% CI, 0.80 to 0.99; P < 0.05), and a 22% reduction from the data of retrospective cohort studies (I2 = 76.8%, RR, 0.91; 95% CI, 0.86 to 0.96; P < 0.05). Overall, the treatment with beta-blockers was associated with a significant reduction in the risk for the mortality compared with the non-beta-blockers group (I2 = 39.4%, RR, 0.91; 95% CI, 0.87 to 0.95; P < 0.05). However, the composite outcomes of mortality and hospitalization was not affected by the beta-blockers treatment (I2 = 81.4%, RR, 1.02; 95% CI, 0.75 to 1.40; P = 0.88). No evidence for publication bias was found using Begg’s test for the studies that reported all-cause mortality (P = 0.19) and composite outcomes (P = 0.46), and the Begg’s funnel plots were displayed in Figure S1 and Figure S2, respectively.
Figure 2. The pooled analyses of all-cause mortality and composites outcomes in beta-blockers group versus non-beta-blockers group.
CI, confidence interval; PCS, prospective cohort study; RCS, retrospective cohort study; RCTs, randomized controlled trials; RR, relative risk.
Effect of beta-blockers on hospitalization
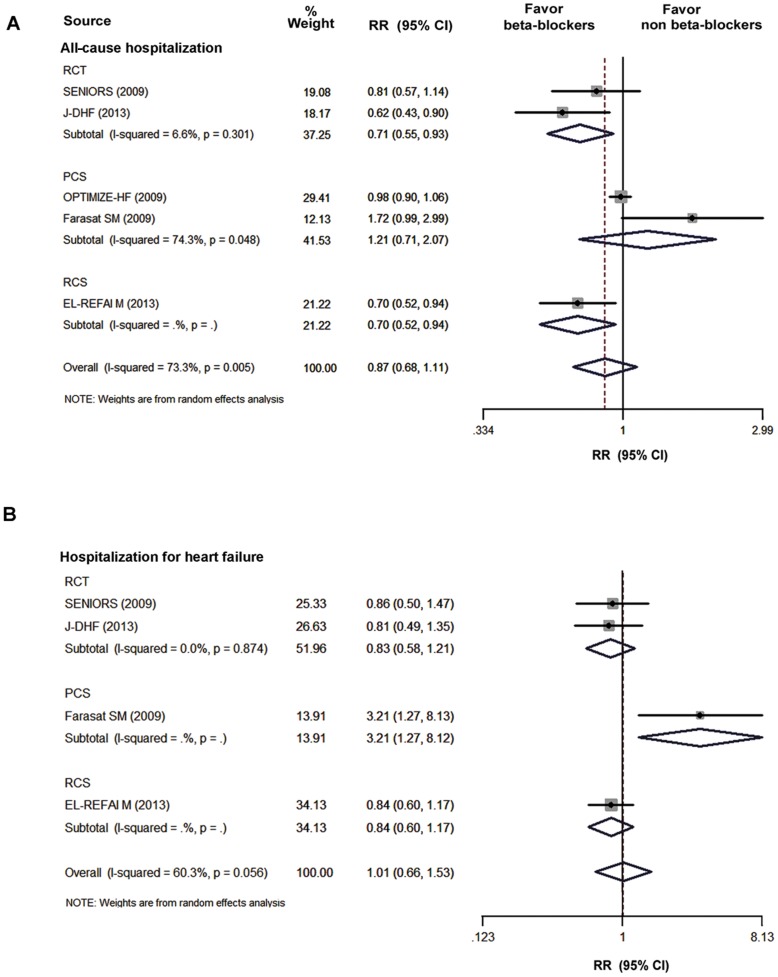
Figure 3 shows the pooled analyses of the included studies that reported the outcomes of hospitalization. Five studies provided the data of all-cause hospitalization. The pooled analysis showed that the beta-blockers treatment did not improve the risk for all-cause hospitalization (I2 = 73.3%, RR, 0.87; 95% CI, 0.68 to 1.11; P = 0.26, Figure 3A) in HFpEF. Similarly, the pooled overall RRs of HF hospitalization did not demonstrate a significant benefit of the beta-blocker treatment (I2 = 60.3%, RR, 1.01; 95% CI, 0.66 to 1.53; P = 0.97; Figure 3B). No evidence for the publication bias was found using the Begg’s test for studies reporting all-cause hospitalization (P = 0.81) and HF hospitalization (P = 0.09), and the Begg’s funnel plots were displayed in Figure S3 and Figure S4, respectively.
Figure 3. The pooled analysis of hospitalization in beta-blockers group versus non-beta-blockers group.
A: All-cause hospitalization; B: HF hospitalization CI, confidence interval; PCS, prospective cohort study; RCS, retrospective cohort study; RCTs, randomized controlled trials; RR, relative risk.
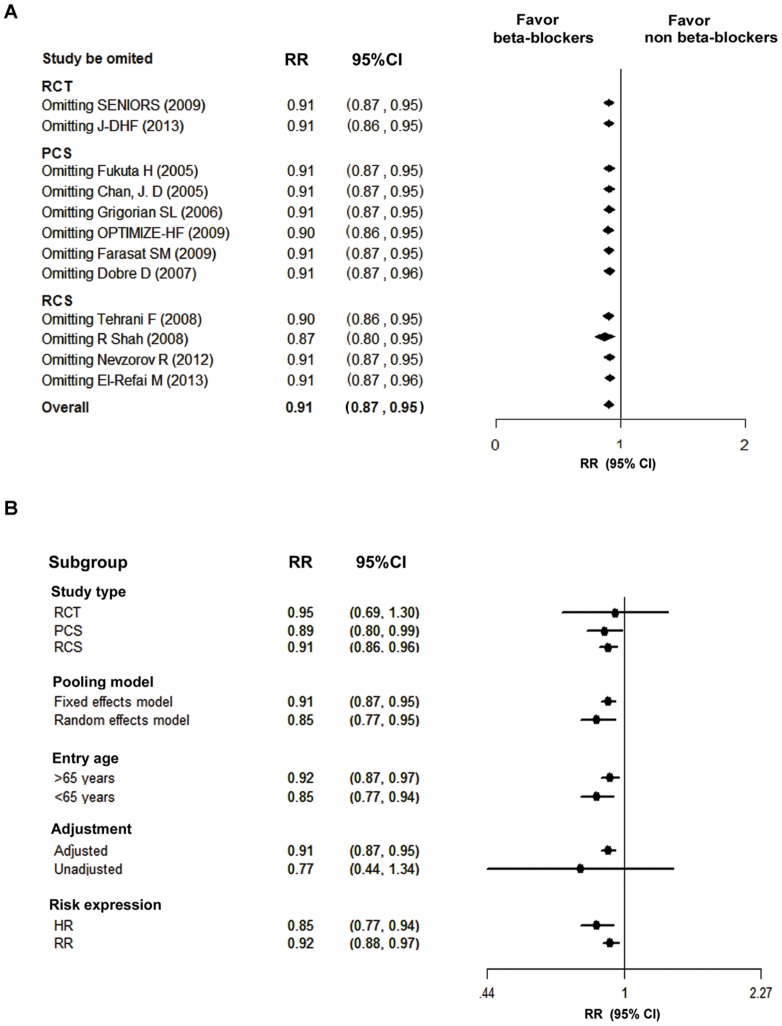
Sensitivity Analyses
We performed leave-one-out sensitivity analysis on all-cause mortality by omitting one study at a time, and found that none of the individual study significantly influenced the pooled estimate of all-cause mortality (Figure 4A). In addition, we conducted subgroup analyses and the results were displayed in Figure 4B. When the pooled analysis of all-cause mortality was performed using random-effect model, a similar result was observed (Figure 4B). A protective effect of beta-blockers was observed when the pooled analysis was limited to those studies that only included elderly patients. However, when the effect estimates were limited to the unadjusted subgroups (those studies performed multivariate analysis to obtain RRs), the pooled analysis did not show a significant effect on all-cause mortality in the patients with HFpEF.
Figure 4. Sensitivity analyses.
A: Leave-one-out analysis; B: Subgroup analyses. The adjusted subgroup was those studies that performed multivariate analysis to obtain Relative Risks, and the provided RRs were directly used for pooling analysis. The unadjusted subgroup group was those studies without performing multivariate analysis, and the RRs were calculated by using the primary data. CI, confidence interval; HR, hazard ratio; LVEF, left ventricular ejection fraction; PCS, prospective cohort study; RCS, retrospective cohort study; RCT, randomized controlled trial; RR, relative risk.
Discussion
In contrast to the well-reported benefits of the beta-blockers treatment for patients with HFrEF, the effect of beta-blockers exposure in HFpEF remains uncertain. In this meta-analysis involving 21,206 patients, the effect of beta-blockers on the HFpEF with an EF ≥ 40% was firstly evaluated. We found that beta-blocker treatment was associated with a statistically significant reduction in all-cause mortality. However, the prescription of beta-blockers did not significantly improve the hospitalization (all-cause or HF related) or composite outcomes of mortality and hospitalization in HFpEF patients.
It should be emphasized that this meta-analysis was challenged by the differential criteria of the EF cut-off value (range from 35% to 55%) used in the clinical studies investigating HFpEF. In the earlier clinical studies, the cut-off value of EF > 35% was used as the definition of HFpEF [29], [30], while this cut-off value was relatively low and generally not considered “preserved”. In recent years, both the threshold of EF ≥ 50% and EF ≥ 40% were identified as the diagnostic criteria for HFpEF in clinical studies [9], [11]. The heart failure patients with an EF 40% to 50% who had mild systolic dysfunction were characteristically and prognostically similar to those with an EF ≥ 50% [31]. More importantly, recent ACCF/AHA guidelines recognized that the range of 40% to 50% was defined as borderline and intermediate criteria of patients with HFpEF [32]. We, therefore, chose an EF value ≥ 40% as a definition for HFpEF patients in this meta-analysis. To our knowledge, this is the first meta-analysis to evaluate the effect of beta-blockers in HFpEF patients with an EF ≥ 40%.
This meta-analysis reveals that beta-blockers exert a significantly protective effect on all-cause mortality reduction in HFpEF patients. The mortality benefit associated with beta-blockers in this analysis was largely driven by the results of Shah R et al [8]. However, the protective effect still remained after removing this study using the sensitivity analysis. Furthermore, both fixed and random effects models in the pooled analysis shows the significantly similar benefit of the beta-blockers treatment. In addition, this protective effect was noted as well when the pooled analysis was limited to the studies that only included elderly patients. Accordingly, the conclusion that the treatment of beta-blockers reduces all-cause mortality in patients with HFpEF (EF≥40%) is fairly reliable.
The mechanism of the beta-blockers treatment that exerts benefits on all-cause mortality in patients with HFpEF has not been precisely clarified. It might be mainly due to the anti-hypertensive effect, the arrhythmic-risk reduction, and the myocardial perfusion improvement. Previous studies have found that hypertension is the most important cause of HFpEF [33]. Therefore, beta-blockers, as effective anti-hypertension drugs, could exert anti-hypertensive effect and improve the survival of the patients with HFpEF. Additionally, the patients with HFpEF usually have a history of ischemic heart diseases and atrial fibrillation [32]. HFpEF in this condition may benefit from the beta-blockers treatment via controlling ventricular rate, improving myocardial metabolism and ventricular remodeling, and reducing arrhythmic-risk and acute coronary events. The ESC guidelines mentioned that an adequate treatment of hypertension, myocardial ischemia and tachycardia should be recommended to the patients with HFpEF [34].
It is interesting that the protective effect of beta-blockers on HFpEF regarding all-cause mortality is significant, but all-cause (or HF related) hospitalization is not. The lack of the reduction in hospitalization in this meta-analysis is probably due to the following reasons. First, the patients with HFpEF were elderly and typically characterized by multiple non-cardiac or/and cardiac comorbidities. Previous studies demonstrated that the incidence of non-cardiac related hospitalization in HFpEF was much higher, while the incidence of HF hospitalization in HFpEF was lower compared to HFrEF [34]. The comorbidity of diabetes mellitus or COPD might affect the effect of non-selective beta-blockers. These drugs could increase insulin resistance or cause bronchial constrictions. It is possible that the patients with HFpEF hospitalization for diabetes mellitus and/or COPD may not benefit from the beta-blocker treatment. Thus, the higher hospitalization remains. Second, there is very limited data regarding the hospitalization available to produce a meaningful finding. With the clinical studies increase, a significant outcome regarding the hospitalization, in particular HF-related hospitalization, will be reported. In the future, more randomized clinical trials are necessary to explore whether the beta-blockers treatment could improve hospitalization in patients with HFpEF.
Although this meta-analysis demonstrated a significant benefit of beta-blockers on all-cause mortality in HFpEF, the recommendations for this treatment in clinical practice should be cautious. This benefit is mainly derived from the observational studies and only 9% risk reduction was observed. More large-scale RCTs in HFpEF are required to assure the protective effect of beta-blockers. Fortunately, a large-scale clinical trial (β-PRESERVE study) aiming at the role of β-blockers (metoprolol) in HFpEF is on the way now [35].
Study limitations
There are several limitations in our meta-analysis. First, the publication bias may only occur for published articles in English. Second, the available RCTs were underpowered to provide conclusive findings about the effects of beta-blockers on HFpEF due to small sample sizes. Third, the outcomes regarding exercise tolerance, diastolic function and quality of life were not assessed in this meta-analysis. As we know, it is also important to clarify the effect of beta-blockers on the outcomes of symptoms and functional status. However, the available data is too limited to perform a powerful meta-analysis. Furthermore, the application of meta-analytic methods to the observational studies in this meta-analysis may produce inherent biases, including the observational design that has lost the randomization and made the calculation of a single summary effect estimate potentially misleading. However, the credibility could be greatly improved as we performed and reported this meta-analysis according to the reporting Meta-Analyses of Observational Studies in Epidemiology (MOOSE). Finally, there are only two studies (SENIORS and J-DHF trials) in this meta-analysis that provided the specific doses and types of the beta-blockers administrated We could not assess whether the doses and types of beta-blockers affect the effects of beta-blockers on HFpEF.
Conclusions
This meta-analysis demonstrated that the beta-blockers treatment reduced all-cause mortality in HFpEF patients with EF ≥ 40%, while it did not affect hospitalization. Beta-blockers may be an efficacious therapeutic option for the patients with HFpEF, and further large scale RCTs are urgently required to assert this issue.
Supporting Information
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting all-cause mortality. RR, relative risk; and SE standard error.
(TIF)
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting composite outcome. RR, relative risk; and SE standard error.
(TIF)
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting all-cause hospitalization. RR, relative risk; and SE standard error.
(TIF)
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting heart failure hospitalization. RR, relative risk; and SE standard error.
(TIF)
The Quality of Observational Studies Assessed by Newcastle–Ottawa Scale.
(DOCX)
PRISMA Checklist.
(DOC)
This supplementary material included: 1_Primary data (XLSX); 2_Data for Figure 2A(dta); 3_Data for Figure 2Bb (dta); 4_Data for Figure 3A(dta); 5_Data for Figure 3B(R); 6_Data for Figure 4A(dta); 7_Data for Figure 4B(dta); 8_Command for each figure.
(RAR)
Acknowledgments
The authors are grateful to Prof. John Fu from the College for Public Health and Social Justice, Saint Louis University, and Prof. Yulin Liao from Department of Cardiology, Nanfang Hospital, Southern Medical University for their language editing and valuable comments.
Funding Statement
This work was supported by grants from National Basic Research Program of China (973 Program) (No. 2013CB733804), National Natural Science Foundation of China (No. 81227801 and No. 81271640), and the Team Program of Natural Science Foundation of Guangdong Province, China (S2011030003134) to Jianping Bin. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Lam CS, Donal E, Kraigher-Krainer E, Vasan RS (2011) Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail 13: 18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Masoudi FA, Havranek EP, Smith G, Fish RH, Steiner JF, et al. (2003) Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol 41: 217–223. [DOI] [PubMed] [Google Scholar]
- 3. Smith GL, Masoudi FA, Vaccarino V, Radford MJ, Krumholz HM (2003) Outcomes in heart failure patients with preserved ejection fraction: mortality, readmission, and functional decline. J Am Coll Cardiol 41: 1510–1518. [DOI] [PubMed] [Google Scholar]
- 4. Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, et al. (2001) Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 344: 1651–1658. [DOI] [PubMed] [Google Scholar]
- 5. Krum H, Roecker EB, Mohacsi P, Rouleau JL, Tendera M, et al. (2003) Effects of initiating carvedilol in patients with severe chronic heart failure: results from the COPERNICUS Study. JAMA 289: 712–718. [DOI] [PubMed] [Google Scholar]
- 6. Paulus WJ, van Ballegoij JJ (2010) Treatment of heart failure with normal ejection fraction: an inconvenient truth!. J Am Coll Cardiol 55: 526–537. [DOI] [PubMed] [Google Scholar]
- 7. Dobre D, van Veldhuisen DJ, DeJongste MJ, Lucas C, Cleuren G, et al. (2007) Prescription of beta-blockers in patients with advanced heart failure and preserved left ventricular ejection fraction. Clinical implications and survival. Eur J Heart Fail 9: 280–286. [DOI] [PubMed] [Google Scholar]
- 8. Shah R, Wang Y, Foody JM (2008) Effect of statins, angiotensin-converting enzyme inhibitors, and beta blockers on survival in patients >or = 65 years of age with heart failure and preserved left ventricular systolic function. Am J Cardiol 101: 217–222. [DOI] [PubMed] [Google Scholar]
- 9. El-Refai M, Peterson EL, Wells K, Swadia T, Sabbah HN, et al. (2013) Comparison of Beta-blocker effectiveness in heart failure patients with preserved ejection fraction versus those with reduced ejection fraction. J Card Fail 19: 73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van Veldhuisen DJ, Cohen-Solal A, Bohm M, Anker SD, Babalis D, et al. (2009) Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). J Am Coll Cardiol 53: 2150–2158. [DOI] [PubMed] [Google Scholar]
- 11. Yamamoto K, Origasa H, Hori M (2013) Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study ( J-DHF ). Eur J Heart Fail 15: 110–118. [DOI] [PubMed] [Google Scholar]
- 12. Farasat SM, Bolger DT, Shetty V, Menachery EP, Gerstenblith G, et al. (2010) Effect of Beta-blocker therapy on rehospitalization rates in women versus men with heart failure and preserved ejection fraction. Am J Cardiol 105: 229–234. [DOI] [PubMed] [Google Scholar]
- 13. Holland DJ, Kumbhani DJ, Ahmed SH, Marwick TH (2011) Effects of treatment on exercise tolerance, cardiac function, and mortality in heart failure with preserved ejection fraction. A meta-analysis. J Am Coll Cardiol 57: 1676–1686. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151: 264–269, W64. [DOI] [PubMed]
- 15. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- 16. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1–12. [DOI] [PubMed] [Google Scholar]
- 17. Spruance SL, Reid JE, Grace M, Samore M (2004) Hazard ratio in clinical trials. Antimicrob Agents Chemother 48: 2787–2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J (2007) Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 298: 2654–2664. [DOI] [PubMed] [Google Scholar]
- 19. Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB (2011) Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA 306: 1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 21. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 22. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–1101. [PubMed] [Google Scholar]
- 23. Fukuta H, Sane DC, Brucks S, Little WC (2005) Statin therapy may be associated with lower mortality in patients with diastolic heart failure: a preliminary report. Circulation 112: 357–363. [DOI] [PubMed] [Google Scholar]
- 24. Chan JD, Rea TD, Smith NL, Siscovick D, Heckbert SR, et al. (2005) Association of beta-blocker use with mortality among patients with congestive heart failure in the Cardiovascular Health Study (CHS). Am Heart J 150: 464–470. [DOI] [PubMed] [Google Scholar]
- 25. Grigorian SL, Roman AV, Ramos PM, Veloso PR, Bandin DM, et al. (2006) Angiotensin-converting enzyme inhibitors prescription is associated with longer survival among patients hospitalized for congestive heart failure who have preserved systolic function: a long-term follow-up study. J Card Fail 12: 128–133. [DOI] [PubMed] [Google Scholar]
- 26. Hernandez AF, Hammill BG, O'Connor CM, Schulman KA, Curtis LH, et al. (2009) Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) Registry. J Am Coll Cardiol 53: 184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tehrani F, Phan A, Chien CV, Morrissey RP, Rafique AM, et al. (2009) Value of medical therapy in patients >80 years of age with heart failure and preserved ejection fraction. Am J Cardiol 103: 829–833. [DOI] [PubMed] [Google Scholar]
- 28. Nevzorov R, Porath A, Henkin Y, Kobal SL, Jotkowitz A, et al. (2012) Effect of beta blocker therapy on survival of patients with heart failure and preserved systolic function following hospitalization with acute decompensated heart failure. European Journal of Internal Medicine 23: 374–378. [DOI] [PubMed] [Google Scholar]
- 29. Carson P, Johnson G, Fletcher R, Cohn J (1996) Mild systolic dysfunction in heart failure (left ventricular ejection fraction >35%): baseline characteristics, prognosis and response to therapy in the Vasodilator in Heart Failure Trials (V-HeFT). J Am Coll Cardiol 27: 642–649. [DOI] [PubMed] [Google Scholar]
- 30. Ghio S, Magrini G, Serio A, Klersy C, Fucili A, et al. (2006) Effects of nebivolol in elderly heart failure patients with or without systolic left ventricular dysfunction: results of the SENIORS echocardiographic substudy. Eur Heart J 27: 562–568. [DOI] [PubMed] [Google Scholar]
- 31. Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, et al. (2007) Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol 50: 768–777. [DOI] [PubMed] [Google Scholar]
- 32.Yancy CW, Jessup M, Bozkurt B, Masoudi FA, Butler J, et al.. (2013) 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. [DOI] [PubMed]
- 33. Nohria A, Tsang SW, Fang JC, Lewis EF, Jarcho JA, et al. (2003) Clinical assessment identifies hemodynamic profiles that predict outcomes in patients admitted with heart failure. J Am Coll Cardiol 41: 1797–1804. [DOI] [PubMed] [Google Scholar]
- 34. Ather S, Chan W, Bozkurt B, Aguilar D, Ramasubbu K, et al. (2012) Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol 59: 998–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhou J, Shi H, Zhang J, Lu Y, Fu M, et al. (2010) Rationale and design of the beta-blocker in heart failure with normal left ventricular ejection fraction (beta-PRESERVE) study. Eur J Heart Fail 12: 181–185. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting all-cause mortality. RR, relative risk; and SE standard error.
(TIF)
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting composite outcome. RR, relative risk; and SE standard error.
(TIF)
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting all-cause hospitalization. RR, relative risk; and SE standard error.
(TIF)
Begg’s Funnel Plots with Pseudo 95% Confidence Limits for studies reporting heart failure hospitalization. RR, relative risk; and SE standard error.
(TIF)
The Quality of Observational Studies Assessed by Newcastle–Ottawa Scale.
(DOCX)
PRISMA Checklist.
(DOC)
This supplementary material included: 1_Primary data (XLSX); 2_Data for Figure 2A(dta); 3_Data for Figure 2Bb (dta); 4_Data for Figure 3A(dta); 5_Data for Figure 3B(R); 6_Data for Figure 4A(dta); 7_Data for Figure 4B(dta); 8_Command for each figure.
(RAR)