Abstract
Objective
This study was initiated to investigate if spousal concordance in metabolic syndrome (MS) components exist in Japan.
Methods
In all, 756 couples (mean age: 48.9 and 47.3 years for husbands and wives, respectively) were identified. Each subject was classified as an MS, MS reserves (MSRES) or no risk of MS (NonMS) case after Japanese Ministry of Health, Labour and Welfare (JMHLW) criteria. Criteria of the National Cholesterol Education Program and of the Joint Interim Statement were also applied.
Results
With Japanese Ministry of Health, Labor and Welfare (JMHLW) criteria, MS, MSRES and NonMS cases accounted for 11.9, 14.7 and 73.4 % in husbands and 1.6, 3.7 and 94.7 % in wives. Waist circumference (WC), body mass index (BMI), systolic blood pressure (SBP) and hemoglobin A1c (HbA1c) showed significant correlation (p < 0.01). Correlation was also significant (p < 0.05) for mean blood pressure (MBP) and fasting plasma glucose (FPG). When adjusted for age, correlations were significant only for WC, BMI and HbA1c. Furthermore, none of the correlation coefficients were greater than 0.2. Logistic regression analyses did not suggest significant mutual influence in MS status between the couples.
Conclusions
Spousal concordance in MS components was detected for WC, BMI, SBP, MBP, FPG and HbA1c, but the correlation was generally weak and modest in Japanese couples.
Keywords: Husband, Metabolic syndrome, Spousal concordance, Wife
Introduction
Based on the concept that metabolic syndrome (MS) is a common etiology of various age-related and lifestyle-related diseases such as hypertension, and dysfunction in glucose and lipid metabolism [1–4], Japanese Ministry of Health, Labour and Welfare (JMHLW) launched an anti-metabolic syndrome campaign in 2007 [5].
In practice, the Ministry [5–7] stipulates that health insurance organizations carry out a designated health examination (i.e., health examination designed for early detection of MS) followed by designated health guidance (as a tool of intervention), not only to the employees as the insured (at the ages of 40 years and above), but also to their family members, especially housewives. However, the prevalence rates of the examination were not high, being at the level of 43.2 % for those at 40–74 years (48.5 and 38.1 % for men and women, respectively) [8].
Rather exceptionally, examination data for wives in addition to data for husbands have been accumulating in Kyoto Industrial Health Association, probably as a reflection of continuous efforts since 1975 to encourage housewives to have health examinations annually [9]. The encouragement is based on the understanding that the health of a wife is an important basis for the health of all family members, including her husband, who is the employee and the insured [9].
Taking advantage of the compilation of data on MS for both husbands and wives, the present study was initiated to investigate if concordance in MS components would be detected between couples, and such being the case, the power of the correlation.
Spousal concordance or within-pair correlation in health issues such as MS and its components has been discussed in recent years in various populations (e.g., Canadians [10], Chinese [11], Koreans [12, 13] and Swedes [14]). However, this issue has been seldom discussed in Japan, possibly because data paired for husbands and wives are generally not available.
Subjects and methods
Subjects studied
The study was conducted in the fiscal years 2010–2012 in a large electronics device-manufacturing plant with nearly 1,800 male employees. The working men (all full-time regular employees) had the designated health examination [5–7] in the Kyoto Industrial Health Association. Subjects were selected by ages of 40–65 years. The men to women ratios (100:30–40) of subjects who had health examination in Kyoto Industrial Health Association have been reported annually [15]. As most of female examinees were house-wives of male examinees, it was possible to estimate from the men to women ratio that about 30–40 % of their wives had the designated health examination (as employees’ family members), also in the Kyoto Industrial Health Association.
Taking advantage of the data on the health insurance certificates, a man and a woman were considered to be a couple when they had the same insurance code and identification number. In practice, 756 couples were identified after exclusion of 91 cases with incomplete health examination data (e.g., either fasting plasma glucose [FPG] or Hemoglobin A1c [HbA1c] data were missing). It should be noted that the Japanese Ministry of Health, Labor and Welfare (JMHLW)'s MS criteria [6, 7] will be satisfied by either FPG or HbA1c (priority given to FPG) and do not request both parameters.
Ethical issues
Each participant agreed to join this study and permitted in written form the use of information on their health insurance certificates for identification of the couple (as detailed above). The study protocol was approved by the Ethics Committee of Kyoto Industrial Health Association.
Classification of subjects in terms of metabolic syndrome (MS)
Each individual was classified into three groups of those with MS (the MS), the MS reserves, or those with MS risks (the MSRES) and those with no current MS risk (the NonMS), after the examination system defined by JMHLW [6, 7] as summarized in Table 1.
Table 1.
Comparison of metabolic syndrome definition by the Japanese Ministry of Health, Labor and Welfare (JMHWL), National Cholesterol Education Program (NCEP) and Joint Interim Statement (JIS)
| Item | Unit | JMHLWa | NCEPb | JISc |
|---|---|---|---|---|
| Step-wise approach | Two steps | Single step | Single step | |
| The 1st stepd | ||||
| Waist circumference (WC) | cm | ≥85 for men, ≥90 for women | ||
| Body mass index (BMI) | kg/m2 | BMI ≥ 25 when WC is <85 for men and <90 for women | ||
| The 2nd step | ||||
| Waist circumference for Asians [16] | ≥90 for men, ≥80 for women |
≥90 for men, ≥80 for women |
||
| Blood pressure (BP) | ||||
| Systolic/diastolic | mm Hg | ≥130/≥ 85 | ≥130/≥ 85 | ≥130/≥ 85 |
| Triglyceride (TG) | mg/100 ml serum | ≥150e | ≥150 | ≥150 |
| HDL-cholesterol (HDL-C) | mg/100 ml serum | <40e | <40 for men, <50 for women |
<40 for men, <50 for women |
| Fasting plasma glucose (FPG) | mg/100 ml plasma | ≥110f | ≥110 | ≥100 |
| MS classificationg | 2+/3h for MS, 1/3 for MSRES, 0/3 for NonMS |
3+/5 for MS, 2−/5 for NonMS |
3+/5 for MS, 2−/5 for NonMS |
|
Subjects under medication for hyperlipidemia, hyperglycemia or hypertension are taken as if they meet the corresponding criteria
aReference [6]
bReference [2]
cReference [17]
dWaist circumference of ≥ 85 cm for men and ≥ 90 cm for women is an essential criterion
eEither triglyceride or HDL-cholesterol
fHbA1c ≥ 6.0 % (National Glycohemoglobin Standardization Program) in case FPG is not available [7]
g+ or − means ‘and more’ or ‘and less’, respectively, e.g., 2+ indicates two or more
hThree items in the 2nd step
In some cases, the subjects were also classified after the National Cholesterol Education Program (NCEP) criteria [2] (as modified for Asians [16]) and the Joint Interim Statement (JIS) criteria [17]. The waist circumference (WC) criterion is set at ≥ 102 cm for men and ≥ 88 cm for women in the original NCEP criteria and left unspecified in the JIS setting, so that WC can be set subject to the population to be applied. In the present analysis, however, the criteria of ≥ 90 cm for men and ≥ 80 cm for women, suggested for Asians in general [16], were employed in application of the JIS criteria for closer comparison with the results in other reports on East Asian populations.
Statistical evaluation
With regard to clinical parameters, a normal distribution was assumed for all except triglyceride (TG), for which a log-normal distribution was considered. Paired t test, McNemar’s test, analysis of variance (followed by ad hoc test after Scheffe) and logistic regression analyses were employed as necessary. Correlation analysis was conducted between husbands and wives for MS components and related items with and without adjustment for husband–wife mean ages. SPSS (version 20) was used as the statistical software.
With respect to the evaluation of correlation coefficients (r), it is known that t = r × [(n − 2)/(1 − r2)]1/2, where t = 2.576 and 1.980 for p = 0.01 and 0.05, respectively, when n (the number of cases) is large. In the present study with n = 756 as stated above, the equation gives r = 0.093 and 0.071 for p = 0.01 and 0.05, respectively.
Results
Demographic data for the population studied
The basic demographic data of the husbands and wives are summarized in Table 2. The arithmetic means (AM) of ages were 48.9 years for husbands and 47.3 years for wives: the mean difference in age was 1.6 years, and a close correlation was detected between the ages of husbands and the ages of wives (r = 0.98, p < 0.01). A majority of wives were non-drinkers (60.4 %) and non-smokers (96.6 %), whereas husbands showed lower non-drinking (26.1 %) and non-smoking rates (68.9 %). With regard to waist circumference (WC), the average (range in parenthesis) was 82.9 cm (63.0–119.0 cm) for husbands and 77.2 cm (61.0–117.5 cm) for wives.
Table 2.
Basic demographic parameters of the population studied
| Unit | Husbands | Wives | p for differencea | |||
|---|---|---|---|---|---|---|
| AM | ASD | AM | ASD | |||
| Age | Years | 48.9 | 7.0 | 47.3 | 7.1 | ** |
| Difference in age | Years | 1.6 | 2.8 | 1.6 | 2.8 | |
| Waist circumference (WC) | cm | 82.9 | 8.2 | 77.2 | 8.4 | ** |
| Body mass index (BMI) | kg/m2 | 23.3 | 3.1 | 21.3 | 2.9 | ** |
| Non-drinking rateb | % | 26.1 | 60.4 | ** | ||
| Non-smoking ratec | % | 68.9 | 96.6 | ** | ||
Data for 756 couples
AM Arithmetic mean, ASD Arithmetic standard deviation
a p by paired t test for age, waist circumference and BMI, and by McNemar’s test for drinking and smoking habits; ** for p < 0.01
bRate for those who never or seldom drink (n = 197 for husbands and 457 for wives)
cRate for those who are not current smokers (n = 521 for husbands and 730 for wives)
Distribution of MS, MSRES and NonMS cases by gender and by couple
When individuals were classified in terms of MS using JMHLW criteria [6, 7], it became clear that about 12 % of the husbands had MS, whereas the prevalence of MS was as low as 1.6 % for wives (Table 3). As a result, the couples in which both husbands and wives were in the MS group counted for only two cases or 0.3 % of the 756 couples examined. The number of cases in which both husbands and wives were in the group of MS or MSRES (i.e., both having the MS risk as either MS or MSRES) was 15 (2.0 %; the number at the cross of the MS + MSRES line and the MS + MSRES column in the section for JMHLW in Table 3).
Table 3.
Numbers of MS, RES and NonMS cases as classified by the criteria of the Japanese Ministry of Health, Labor and Welfare (JMHWL), National Cholesterol Education Program (NCEP) and Joint Interim Statement (JIS)
| Wives | Husbands | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| JMHLW | NCEP | JIS | ||||||||||
| MS | MSRES | MS + MSRES | NonMS | Total | MS | NonMS | Total | MS | NonMS | Total | ||
| MS | Number | 2 | 2 | 4 | 8 | 12 | 5 | 19 | 24 | 7 | 21 | 28 |
| % | 0.3 | 0.3 | 0.5 | 1.1 | 1.6 | 0.7 | 2.5 | 3.2 | 0.9 | 2.8 | 3.7 | |
| MSRES | Number | 6 | 5 | 11 | 17 | 28 | ||||||
| % | 0.8 | 0.7 | 1.5 | 2.2 | 3.7 | |||||||
| MS + MSRES | Number | 8 | 7 | 15 | 25 | 40 | ||||||
| % | 1.1 | 0.9 | 2.0 | 3.3 | 5.4 | |||||||
| NonMS | Number | 82 | 104 | 186 | 530 | 716 | 77 | 655 | 732 | 98 | 630 | 728 |
| % | 10.8 | 13.8 | 24.6 | 70.1 | 94.7 | 10.2 | 86.6 | 96.8 | 13.0 | 83.3 | 96.4 | |
| Total | Number | 90 | 111 | 201 | 555 | 756 | 82 | 674 | 756 | 105 | 651 | 756 |
| % | 11.9 | 14.7 | 26.6 | 73.4 | 100.0 | 10.8 | 89.2 | 100.0 | 13.8 | 86.1 | 100.0 | |
In further trials, two other criteria systems (Table 1) of the NCEP [2] and JIS [17] were applied (see right half of Table 3). It should be noted that, different from the JMHLW system, these criteria classified subjects into dichotomous groups of MS and NonMS, with no MSRES group (Table 1). The JIS system allocated more husbands (see corresponding columns in Table 3; 13.8 %), and both the NCEP and JIS systems allocated more wives (corresponding lines; 3.2 and 3.7 %, respectively) into MS groups than the JMHLW system (i.e., 11.9 and 1.6 % for husbands and wives). As a result, the rate for the couples (in which both husbands and wives were in the MS group) also increased; to 0.7 % in the NCEP system and to 0.9 % in the JIS system (Table 3).
Significant difference in clinical parameters among the MS and MSRES groups as compared with the NonMS group
After classification into the MS, MSRES and NonMS groups using the JMHLW system, the distributions of the clinical parameters in the three groups were compared. The results are presented in terms of AM and arithmetic standard deviation (ASD) in Table 4, together with statistical significance of the difference among the groups. TG was distributed log-normally, and geometric mean (GM) and geometric standard deviation (GSD) were given in place of AM and ASD in Table 4. The statistical evaluation was conducted after logarithmic conversion.
Table 4.
Comparison of clinical parameters in the three groups by genders
| Parameter (unit) | The couples | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Husbands | Wives | |||||||||||||||||||
| MS | MSRES | NonMS | p fora | MS | MSRES | NonMS | p fora | |||||||||||||
| AM | ASD | AM | ASD | AM | ASD | ANOVA | A | B | C | AM | ASD | AM | ASD | AM | ASD | ANOVA | A | B | C | |
| Number of cases | 90 | 111 | 555 | 12 | 28 | 716 | ||||||||||||||
| WC (cm) | 93.9 | 7.1 | 91.6 | 5.8 | 79.4 | 5.6 | ** | * | ** | ** | 94.8 | 9.4 | 94.1 | 5.9 | 76.2 | 7.4 | ** | ns | ** | ** |
| BMI (kg/m2) | 27.0 | 3.0 | 26.1 | 2.7 | 22.1 | 2.2 | ** | * | ** | ** | 28.7 | 3.6 | 26.4 | 2.5 | 21.0 | 2.5 | ** | * | ** | ** |
| SBP (mm Hg) | 134.7 | 14.2 | 127.3 | 15.5 | 120.2 | 12.7 | ** | ** | ** | ** | 122.6 | 10.9 | 124.6 | 14.8 | 111.5 | 13.7 | ** | ns | ** | ** |
| DBP (mm Hg) | 87.3 | 8.9 | 82.8 | 9.5 | 76.5 | 9.1 | ** | ** | ** | ** | 80.1 | 6.9 | 76.8 | 8.0 | 68.2 | 9.7 | ** | ns | ** | ** |
| MBP (mm Hg) | 103.1 | 8.6 | 97.6 | 10.7 | 91.1 | 9.4 | ** | ** | ** | ** | 94.3 | 6.2 | 92.7 | 8.8 | 82.6 | 10.4 | ** | ns | ** | ** |
| TGb (mg/100 ml) | 167.5 | 1.77 | 125.5 | 1.71 | 84.2 | 1.66 | ** | ** | ** | ** | 145.2 | 1.64 | 103.0 | 1.70 | 63.2 | 1.51 | ** | ns | ** | ** |
| HDL-C (mg/100 ml) | 54.1 | 14 | 57.8 | 14 | 66.5 | 16.8 | ** | ns | ** | ** | 61.5 | 13.8 | 69.2 | 18.2 | 79.1 | 16.6 | ** | ns | ** | ** |
| FPG (mg/100 ml) | 127.4 | 51.0 | 96.3 | 21.9 | 93.8 | 15.7 | ** | ** | ** | ns | 94.2 | 17.5 | 91.4 | 12.8 | 85.7 | 7.2 | ** | ns | ** | ** |
| HbA1c (%) | 5.9 | 1.3 | 5.2 | 0.7 | 5.1 | 0.5 | ** | ** | ** | ns | 5.3 | 0.5 | 5.2 | 0.5 | 5.0 | 0.3 | ** | ns | ** | ** |
In total, 756 couples were analyzed
AM, Arithmetic mean; ASD, Arithmetic standard deviation; WC, waist circumference; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; MBP, mean blood pressure [MBP = (SBP + 2 × DBP)/3]; TG, triglyceride; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c
aANOVA: p after one-way analysis of variance; A: p for difference between the MS and the MSRES; B: p for difference between the MS and the Non-MS; C: p for difference between the MSRES and NonMS.
**, * and ns for p < 0.01, p < 0.05 and p ≥ 0.05
bGM and GSD are shown in place of AM and ASD. Comparisons were made after logarithmic conversion
The comparison in husbands showed that, in almost all parameters, AM values (GM in case of TG) for MS and MSRES groups were significantly (p < 0.01 or p < 0.05) higher (lower in case of HDL-cholesterol) than corresponding values for the NonMS group. The trends were also similar for wives, although the differences of the MS group from the MSRES group were statistically insignificant (Table 4).
Correlation of MS components and other related parameters between husbands and wives
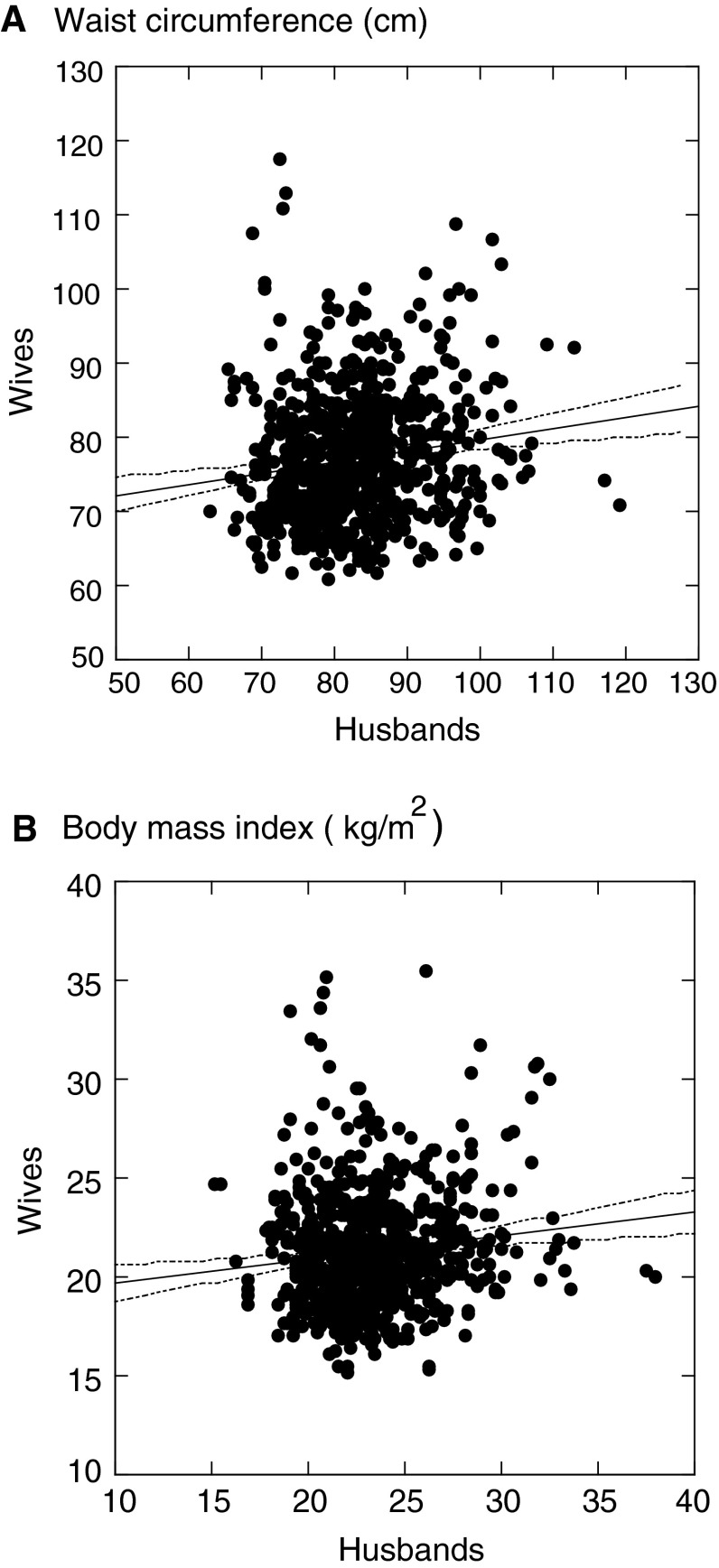
To examine possible spousal concordance in MS components and MS evaluation, simple correlation analyses were conducted, taking the values for husbands and wives as independent and dependent variables. The results are summarized in the middle of Table 5. Significant correlations (p < 0.01) were detected in WC, body mass index (BMI), systolic blood pressure (SBP) and HbA1c (p < 0.01). Mean blood pressure (MBP) and fasting plasma glucose (FPG) also showed significant correlations (p < 0.05). Wide 95 % confidence intervals suggested large variations around the regression lines. Cases of WC and BMI are shown in Fig. 1 for visual understanding of the correlations and large variations. Rather unexpectedly, MS (as scored) did not show significant correlation between spouses (r = 0.056, p > 0.05; see the bottom line in Table 5).
Table 5.
Correlation in MS components and other clinical parameters between 756 couples
| Item (unit) | Correlation coefficient | Partial correlation coefficient | |||
|---|---|---|---|---|---|
| 95 % confidence interval | p a | p a | |||
| Waist circumference (cm) | 0.146 | 0.076 to 0.215 | ** | 0.114 | ** |
| BMI (kg/m2) | 0.128 | 0.058 to 0.198 | ** | 0.128 | ** |
| SBP (mmHg) | 0.084 | 0.013 to 0.155 | ** | 0.008 | ns |
| DBP (mmHg) | 0.064 | −0.008 to 0.134 | ns | 0.029 | ns |
| MBP (mmHg) | 0.080 | 0.008 to 0.150 | * | 0.020 | ns |
| TGb (mg/100 ml) | 0.052 | −0.020 to 0.123 | ns | 0.041 | ns |
| HDL-C (mg/100 ml) | −0.039 | −0.110 to 0.033 | ns | −0.040 | ns |
| FPG (mg/100 ml) | 0.092 | 0.021 to 0.162 | * | 0.031 | ns |
| HbA1c (%) | 0.152 | 0.081 to 0.221 | ** | 0.096 | ** |
| MS-RES-NonMS scorec | 0.056 | −0.016 to 0.127 | ns | 0.033 | ns |
In total, 756 couples were subjected to analyses. For abbreviations, see Table 4. The intercepts (α) and slopes (β) are in the regression equation of Y = α + βX, where X and Y are the values for husbands and wives, respectively. Partial correlation coefficients are for correlation between husbands and wives, taking three variables of the item for husbands, that for the wives and the average ages of each husband and wife pair
a p for correlation coefficients or partial correlation coefficients.
**, * and ns stand for p < 0.01 (r > 0.093), p < 0.05 (r > 0.071) and p ≥ 0.05, respectively. For basis of evaluation of p values, see “Statistical evaluation” in the “Subjects and methods” section
bAfter logarithmic conversion
cMS, RES and NonMS are given scores of 3, 2 and 1, respectively
Fig. 1.
Correlation between husbands and wives on a waist circumference, and b body mass index. Each dot represents one pair of a husband and his wife. The line in the middle is a calculated regression line and dotted lines on both sides show the 95 % ranges. The regression line for a is Y = 647 + 0.15X [where X and Y are waist circumference (in cm) for husbands and wives, respectively] (r = 0.146, p < 0.01) and the line for b is Y = 18.5 + 0.12X [where X and Y are body mass index (in kg/m2) for husbands and wives, respectively] (r = 0.128, p < 0.01)
It should be noted that r values were generally small (i.e., < 0.2). Statistical significance despite these small r values may be due to the large number of cases (n = 756), as described in details in the “Statistical evaluation” section in the “Subjects and methods”.
Further correlation analyses with adjustment for age were conducted taking three variables [i.e., each MS component (and related item) for husbands, that for wives, and the mean age of a husband and his wife]. The husband–wife partial correlation coefficients are shown in the right most column in Table 5. Different from corresponding correlation coefficients (in the middle of Table 5), the partial correlation coefficients were no longer significant for SBP, MBP and FPG, although the coefficients remained significant for WC, BMI and HbA1c. Simple regression analyses with age (separately for husbands and for wives) showed that a close correlation existed for SBP, MBP and FPG with age (p < 0.01 for all of three items both in husbands and wives). There was a close and significant correlation between the ages of couples (r = 0.979; p < 0.01). Therefore, it appeared prudent to consider that, as these three items (i.e., SBP, MBP and FPG) correlated with age in both husbands and wives, apparent correlation was consequently observed.
Possible elevation in MS risk of husbands in association with MS of wives, and reverse cases
To examine possible increase in MS risk in association with an MS spouse, logistic regression analyses were conducted in which MS status of husbands was taken as the dependent variable and their ages and the MS status of wives (as scored) were taken as independent variables; i.e., the MS status of wives were given scores of 3, 2, and 1 for MS, MSRES, and NonMS when the JMHLW criteria was applied, and scores of 2 and 1 for MS and NonMS for the other two criteria. The analyses were also repeated with the MS status of husbands. The results are summarized in Table 6. The odds ratios were all greater than 1, and application of NCEP and JIS criteria tended to give greater odds ratios (1.52–1.62) than application of JMHLW criteria (1.10–1.26). Nevertheless, the 95 % lower limits of confidence intervals were all smaller than 1.0. Correspondingly, p values were > 0.1 in all cases. The observation suggested that the MS status of husbands was not significantly influenced by the MS status of their wives, and the reverse was also the case.
Table 6.
Logistic regression analyses for possible effects of MS status of spouses
| Criteria | Dependent variable | Independent variables | Odds ratio | 95 % confidence interval | |
|---|---|---|---|---|---|
| Age | MS status | ||||
| JMHLW | MS of husbandsa | Age of husbands | MS of wivesb | 1.22 | 0.75 to 1.98 |
| Ibid. | MS risk of husbandsc | Age of husbands | MS risk of wivesb | 1.23 | 0.68 to 2.24 |
| Ibid. | MS of wivesa | Age of wives | MS of husbandsb | 1.26 | 0.84 to 1.91 |
| Ibid. | MS risk of wivesc | Age of wives | MS risk of husbandsb | 1.10 | 0.51 to 2.35 |
| NCEP | MS of husbandsa | Age of husbands | MS of wivesb | 1.57 | 0.56 to 4.43 |
| Ibid. | MS of wivesa | Age of wives | MS of husbandsb | 1.62 | 0.57 to 4.58 |
| JIS | MS of husbandsa | Age of husbands | MS of wivesb | 1.54 | 0.62 to 3.80 |
| Ibid. | MS of wivesa | Age of wives | MS of husbandsb | 1.52 | 0.61 to 3.76 |
p values were > 0.1 in all cases
JMHLW for reference [6], NCEP for reference [2] and JIS for reference [17]
MS, metabolic syndrome group; MSRES, MS reserve group; Non-MS, non-metabolic syndrome group
aYes for the MS group, and no for the MSRES and NonMS groups
bMS, MSRES and NonMS cases are scored as 1, 2 and 3
cYes for the MS and MSRES groups, and no for the NonMS group
Discussion
The present study revealed a statistically significant, yet weak and modest, husband–wife correlation in several MS components. Familial aggregation of MS has been a focus of studies in various populations [10–14, 18–28]. The subjects studied in families included parents (i.e., couples), children and relatives. Among the study subjects, spousal concordance in MS-related items [10–14, 18, 23, 25, 26] is of particular interest, and BMI has been the item most commonly studied. Thus, Katzmarzyk et al. [10], Wu et al. [11] and Jacobson et al. [14] observed correlation coefficients of 0.14 for 1,341 couples in Canada, 0.11 for 431 Chinese couples, and 0.18 for 8,663 couples in Sweden, respectively. Lee et al. [18] observed that BMI showed the highest spousal correlation (0.34) among 303 couples in Korea, followed by SBP (0.18) and HDL-C (0.17). Jee et al. [12], however, obtained a substantially low correlation coefficient of 0.06 (followed by 0.06 for DBP and 0.05 for SBP) for 2,269 couples also in Korea. In a nationwide survey on 3,141 couples in the same country, Kim et al. [13] observed a high (≥ 0.10) correlation coefficient for glycosylated hemoglobin (0.55), SBP (0.24), DBP (0.14) and HDL-C (0.10). Significant correlations for SBP (r = 0.084) and HbA1c (r = 0.152) observed in the present study are in agreement with findings by Kim et al. [13], but the correlation coefficients are substantially smaller in the present study (Table 5).
Di Castelnuovo et al. [26] made a systematic review followed by meta-analysis, and concluded that the study revealed a statistically significant positive spousal concordance for various factors including diastolic blood pressure (DBP), blood glucose and WC, and that BMI and smoking were the two most strongly correlated factors between couples. In general, however, the strength appeared to be quite modest across the components studied [26]. The observations in the present study—that several MS components showed significant correlation between husbands and wives (Table 5) and that the power was nevertheless modest and weak—are in general agreement with the conclusions of Di Castelnuovo et al. [26]. In addition, relatively close correlation for BMI are common to both Di Castelnuovo et al. [26] and the present study.
MS prevalence in the present study population was 10.6 % for men and 0.9 % for women, and that for MS + MSRES was 26.4 % for men and 5.4 % for women (Table 3), when the JMHLW criteria were applied. The prevalence is apparently lower than the values reported by others. For example, the prevalence of MS + MSRES was 26.4 % for men and women combined among 6 million 40–74 year-old examinees, according to national data compilation by JMHLW [8]. In the studies conducted by nongovernmental research groups, Arai et al. [29] reported an MS prevalence of 12.1 % for men and 1.7 % for women in a field survey with 1,917 and 1,347 women using the JMHLW criteria. With the same criteria, Miyatake et al. [30] observed an even higher prevalence of 26.8 % for 1,245 men and 3.6 % for 1,932 women, and Li et al. [31] also using the JMHLW criteria reported a higher prevalence of 22 % for men and 17 % for women in a rural area. The ages of the populations were various depending on the studies, but they were mostly at middle ages.
In other surveys in East Asia in which NCEP criteria were used, Oh et al. [32] in Korea observed an MS prevalence of 29.0 % for men and 16.8 % for women, and Kim et al. [13] reported an MS prevalence of 25.7 % for men and 25.9 % for women. According to Kim et al. [23], the prevalence was 24.6 % for men and 28.1 % for women. Xu et al. [33] found that 28.4 and 18.7 % of women surveyed in Shanghai, China, met the NCEP criteria for MS. When evaluated with the NCEP criteria, the MS prevalence was 10.8 and 3.2 % for men and women, respectively, in the present study (Table 3).
Factors to induce concordance of MS between couples have been discussed by several authors [10, 13, 24, 26], and include both nutritional intake and physical loads in daily life. With regard to the nutritional intake of the present study population, the general expectation would be that the couples share similar dietary habits. Nevertheless, the plant studied offers canteen service so that husbands may take lunch there on workdays, the lunch being different from that their wives make at home. As for physical load, husbands will spend energy not only on work, but on commuting between their homes and the plant; this is also different from that of the daily life of wives. These factors in daily life may reduce the extent of concordance in MS in the present study.
There are several limitations in the present study. First of all, the population studied was full-time male employees in a large company and their wives, and the conclusion drawn may not be applicable to workers and their families in general. The number of cases studied, 756 couples, may not be large enough. Furthermore, the MS prevalence was low, particularly among wives in the present study population as discussed above. Whereas the low MS prevalence is apparently good for health of the participating population, it was inevitable to use MS + MSRES data (rather than MS data) to obtain sufficient numbers of cases in making statistical evaluations, especially when statistical analyses were applied.
Overall conclusions are therefore that weak and modest correlations are detectable between spouses for several MS components, including WC, BMI and HbA1c, in these couples in Japan. However, because the available number of cases is limited, the present results should be taken as preliminary, and the conclusion may need to be confirmed by studies with larger numbers of couples.
Acknowledgments
The authors are grateful to the administration and the staff of Kyoto Industrial Health Association, Kyoto, Japan, for their interest in and support of this study. Thanks are also due to the enterprise, its employees and their wives for their generosity to allow us to analyze their health examination results. The contribution of Prof. K. Murata, Department of Environmental Health Sciences, Akita University Graduate School of Medicine, Akita 010-8543, Japan, in the discussion on the statistical evaluation of study results is gratefully acknowledged.
Conflict of interest
None declared.
List of abbreviations
- AM
Arithmetic mean
- ANOVA
Analysis of variance
- ASD
Arithmetic standard deviation
- BMI
Body mass index
- DBP
Diastolic blood pressure
- FPG
Fasting plasma glucose
- GM
Geometric mean
- GSD
Geometric standard deviation
- HbA1c
Hemoglobin A1c
- HDL-C
High density lipoprotein cholesterol
- IU
International unit
- JIS
Joint Interim Statement
- JMHLW
Japanese Ministry of Health, Labor and Welfare
- MBP
Mean blood pressure
- MS
Metabolic syndrome (or cases with metabolic syndrome)
- MSRES
MS reserve
- NCEP
National Cholesterol Education Program
- NonMS
Those with no current risk of metabolic syndrome
- R2
Coefficient of determination
- SBP
Systolic blood pressure
- TG
Triglyceride
- WC
Waist circumference
References
- 1.Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 2.Expert Panel on Detection Evaluation, and treatment of high blood cholesterol in adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP adult treatment panel III) J Am Med Assoc. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 3.Examination Committee of Criteria for Metabolic Syndrome in Japan Definition and diagnosis criteria for metabolic syndrome. J Jpn Soc Intern Med. 2005;94:794–809. doi: 10.2169/naika.94.794. [DOI] [Google Scholar]
- 4.International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. http://www.idf.org/webdata//docs/met-def-update2006.pdf (2005).
- 5.Japanese Ministry of Health, Labour and Welfare. Ordinance No. 96 on the amendment of health examination system (in Japanese) (2007).
- 6.Japanese Ministry of Health, Labour and Welfare. Standard programs for designated health examination and health guidance, p. 25, 45 (in Japanese) (2007).
- 7.Japanese Ministry of Health, Labour and Welfare. Note on HbA1c values as a criterion for diagnosis of metabolic syndrome, etc., 13 November 2012 (in Japanese).
- 8.Japanese Ministry of Health, Labour and Welfare. Prevalence rates of designated health examination and health guidance in 2020 (in Japanese). http://www.mhlw.go.jp/stf/houdou/2r9852000002qxla-att/2r9852000002qxmr.pdf (2013). Accessed 29 May 2013.
- 9.Kyoto Industrial Health Association. Book in celebration of the 70th anniversary of Kyoto Industrial Health Association, Kyoto, Japan, p. 19 (2011) (in Japanese).
- 10.Katzmarzyk PT, Hebebrand J, Bouchard C. Sousal resemblance in the Canadian population: implications for the obesity epidemic. Int J Obes Relat Metab Disord. 2002;26:241–246. doi: 10.1038/sj.ijo.0801870. [DOI] [PubMed] [Google Scholar]
- 11.Wu D-M, Hong Y, Sun C-A, Sung P-K, Rao DC, Chu N-F. Familial resemblance of adiposity-related parameters: results from a health check-up population in Taiwan. Eur J Epidemiol. 2003;18:221–226. doi: 10.1023/A:1023337917377. [DOI] [PubMed] [Google Scholar]
- 12.Jee SH, Suh I, Won SY, Kim M. Familial correlation and heritability for cardiovascular risk factors. Yonsei Med J. 2002;43:160–164. doi: 10.3349/ymj.2002.43.2.160. [DOI] [PubMed] [Google Scholar]
- 13.Kim HC, Kang DR, Choi KS, Nam CM, Thomas GN, Suh I. Spousal concordance of metabolic syndrome in 3141 Korean couples: a nationwide survey. Ann Epidemiol. 2006;16:292–298. doi: 10.1016/j.annepidem.2005.07.052. [DOI] [PubMed] [Google Scholar]
- 14.Jacobson P, Torgerson JS, Sjöström L, Bouchard C. Spouse resemblance in body mass index: effects on adult obesity prevalence in the offspring generation. Am J Epidemiol. 2007;165:101–108. doi: 10.1093/aje/kwj342. [DOI] [PubMed] [Google Scholar]
- 15.Kyoto Industrial Health Association. The 59th annual report. Kyoto Industrial Health Association, Kyoto, Japan, p. 52 (2012) (in Japanese).
- 16.The Asia–Pacific perspective. Sydney: International Association for the Study of Obesity Task Force; 2000. pp. 15–21. [Google Scholar]
- 17.Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 18.Lee KE, Klein BEK, Klein R. Familial aggregation of components of the multiple metabolic syndrome in the Framingham heart and offspring cohort: genetic analysis workshop problem I. http://biomedcentral.com/1471-2156/4/s1/1594. Accessed 28 March 2013. [DOI] [PMC free article] [PubMed]
- 19.Millen BE, Pencina MJ, Kimokoti RW, Zhu L, Meigs JB, Ordovas JM, et al. Nutritional risk and the metabolic syndrome in women: opportunities for preventive intervention from the Framingham Nutrition Study. Am J Clin Nutr. 2006;84:434–441. doi: 10.1093/ajcn/84.1.434. [DOI] [PubMed] [Google Scholar]
- 20.Park HS, Park JY, Cho S-I. Familial aggregation of the metabolic syndrome in Korean families with adolescents. Atherosclerosis. 2006;186:215–221. doi: 10.1016/j.atherosclerosis.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 21.Chien KL, Hsu HC, Chen WJ, Chen MF, Su TC, Lee YT. Familial aggregation of metabolic syndrome among the Chinese: report from the Chin-Shan community family study. Diabetes Res Clin Pract. 2007;76:418–424. doi: 10.1016/j.diabres.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 22.Chiu Y-H, Lin W-Y, Wang P-E, Chen Y-D, Wang T–T, Warick J, et al. Population-based family case–control proband study on familial aggregation of metabolic syndrome: finding from Taiwanese people involved in Keelung community-based integrated screening (KCIS no. 5) Diabetes Res Clin Pract. 2007;75:348–356. doi: 10.1016/j.diabres.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 23.Kim HM, Kim DJ, Jung IH, Park C, Park J. Prevalence of the metabolic syndrome among Korean adults using the new International Diabetes Federation definition of the new abdominal obesity criteria for the Korean people. Diabetes Res Clin Pract. 2007;77:99–106. doi: 10.1016/j.diabres.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Monden C. Partners in health? Exploring resemblance in health between partners in married and cohabiting couples. Sociol Health Illn. 2007;29:391–411. doi: 10.1111/j.1467-9566.2007.01003.x. [DOI] [PubMed] [Google Scholar]
- 25.Feng Y, Zang T, Xu X, Xu X. Familial aggregation of metabolic syndrome and its components in a large Chinese population. Obesity. 2008;16:125–129. doi: 10.1038/oby.2007.22. [DOI] [PubMed] [Google Scholar]
- 26.Di Castelnuovo A, Quacquaruccio G, Donati MB, de Gaetano G, Lacoviello L. Spousal concordance for major coronary risk factors: a systematic review and meta-analysis. Am J Epidemiol. 2009;169:1–8. doi: 10.1093/aje/kwn234. [DOI] [PubMed] [Google Scholar]
- 27.Matsuo T, Kim MK, Murotake Y, Numao S, Kim MJ, Ohkubo H, et al. Indirect lifestyle intervention through wives improves metabolic syndrome components in men. Int J Obs. 2010;34:136–145. doi: 10.1038/ijo.2009.226. [DOI] [PubMed] [Google Scholar]
- 28.Kanzaki N, Kimura H. Relation between health checkup results and stages of behavior change and lifestyle: a comparison between workers in their 30s and 40s. Jpn J Rural Med. 2012;61:55–66. [Google Scholar]
- 29.Arai H, Yamamoto A, Matsuzawa Y, Saito Y, Yamada N, Oikawa S, et al. Prevalence of metabolic syndrome in the general Japanese population in 2000. J Atherosol Thromb. 2006;13:202–208. doi: 10.5551/jat.13.202. [DOI] [PubMed] [Google Scholar]
- 30.Miyatake N, Wada J, Kawasaki Y, Nishii K, Makino H, Numata T. Relationship between metabolic syndrome and cigarette smoking in the Japanese population. Intern Med. 2006. doi:10.2169/internalmedicine.45.1850. [DOI] [PubMed]
- 31.Li L, Wang L, Yamasaki M, Iwamoto M, Ikenishi R, Yoneyama T, et al. Prevalence of metabolic syndrome in rural community as defined by the Japanese Association of Internal Medicine and Ministry of Health, Labor and Welfare. Jpn J Rural Med. 2008;56:703–713. [Google Scholar]
- 32.Oh J-Y, Sung Y-A, Hong YS, Barrett-Connor E. Prevalence and factor analysis of metabolic syndrome in an urban Korean population. Diabetes Care. 2004;27:2027–2032. doi: 10.2337/diacare.27.8.2027. [DOI] [PubMed] [Google Scholar]
- 33.Xu W-h, Ruan X-n, Fu X-j, Zhu Q-l, Zhang H, Bai Y, et al. Relevance of the metabolic syndrome in Pudong New Area of Shanghai using three proposed definitions among Chinese adults. BMC Public Health. 2010;10:246–256. doi: 10.1186/1471-2458-10-246. [DOI] [PMC free article] [PubMed] [Google Scholar]