Abstract
Host defense is a vital role played by the gastrointestinal tract. As host to an enormous and diverse microbiome, the gut has evolved an elaborate array of chemical and physicals barriers that allow the digestion and absorption of nutrients without compromising the mammalian host. The control of such barrier functions requires the integration of neural, humoral, paracrine and immune signaling, involving redundant and overlapping mechanisms to ensure, under most circumstances, the integrity of the gastrointestinal epithelial barrier. Here we focus on selected recent developments in the autonomic neural control of host defense functions used in the protection of the gut from luminal agents, and discuss how the microbiota may potentially play a role in enteric neurotransmission. Key recent findings include: the important role played by subepithelial enteric glia in modulating intestinal barrier function, identification of stress-induced mechanisms evoking barrier breakdown, neural regulation of epithelial cell proliferation, the role of afferent and efferent vagal pathways in regulating barrier function, direct evidence for bacterial communication to the enteric nervous system, and microbial sources of enteric neurotransmitters. We discuss these new and interesting developments in our understanding of the role of the autonomic nervous system in gastrointestinal host defense.
Keywords: myenteric plexus, submucosal plexus, microbiota, vagus nerve, sympathetic nerve, primary afferent nerves, microbiome, neurotransmitters
Introduction
The mammalian gastrointestinal (GI) tract is a complex organ that has evolved in a cooperative manner with a variety of prokaryotic and eukaryotic species, namely the bacteria, fungi, protozoa and archaea (previously known as archaebacteria) that comprise the microbiome of the gut (Backhed et al., 2005; Sommer and Backhed, 2013). The GI tract is in fact a host within a host. In the vertebrate host, the primary function of the GI tract is to provide the nutrients and energy required for survival and reproduction. A secondary function of the GI tract is to defend the host from potentially harmful ingested food antigens, bacteria, parasites or toxins. This defensive function of the gut extends to protect the organ itself, as well as the host, from the processes of digestion: extremes of pH, digestive enzymes, bile and other chemicals that can damage cells (Fasano and Shea-Donohue, 2005; McCole and Barrett, 2007; Turner, 2009). Digestion frequently produces unwanted antigenic peptides, which if not carefully regulated can lead to powerful immune responses that may also be deleterious to the host (Fasano, 2012; Fasano and Shea-Donohue, 2005). As a host itself, the GI tract is home to trillions of bacteria that reside throughout its length and provide the vertebrate host with specific nutritional, defensive and other symbiotic functions in return for a share of the host’s nutrients and a unique environment in which to live and reproduce (Backhed et al., 2005; Sommer and Backhed, 2013). The burden of this large number of prokaryotic species is considerable, as these commensals can quickly become pathogenic if the intestinal epithelial barrier - the single layer of cells that separate the inside of the body from the gut luminal contents - is breached or defective. It is perhaps not surprising given this introduction that the gut has evolved to be the largest immune organ of the body; where a rich network of nerves and humoral mediators regulate and control digestion, at the same time as orchestrating elaborate cellular systems of defense that work in concert with the immune system to protect the host.
In recent years, we have learned a considerable amount about how the microbiome contributes to nutritional states in mammalian hosts. Gut bacteria seem to be responsible for conditions of both under- and over-nutrition, with extreme examples ranging from kwashiorkor on one hand to obesity on the other (Ridaura et al., 2013; Smith et al., 2013; Turnbaugh et al., 2008; Turnbaugh et al., 2006). But the microbiome is also a critical factor in the development of GI inflammation (Knights et al., 2013; Natividad and Verdu, 2013; Rubino et al., 2012). This can be manifested as an idiopathic condition like inflammatory bowel disease (IBD), where in genetically susceptible individuals, an environmental trigger initiates a breakdown of innate host defenses that leads to an uncontrolled local immune response to antigens and resident commensals in the wall of the gut (Knights et al., 2013). Inflammation may also occur as a result of bacterial dysbiosis when an opportunistic pathogen like Clostridium difficile stimulates a massive local immune response and destruction of the epithelium (Peniche et al., 2013). Local control of inflammation in the gut is covered in the accompanying article by Lomax. Here we will focus on selected recent developments in the autonomic neural control of host defense functions used in the protection of the gut from luminal agents, and how the microbiota may potentially contribute to enteric neurotransmission.
Enteric Innervation
The innervation of the gut consists of both extrinsic and intrinsic components, comprising all three divisions of the autonomic nervous system (Furness, 2006; Furness, 2012). In addition, the gut receives a rich primary afferent innervation of both vagal and spinal origin (Blackshaw et al., 2007; Furness et al., 2013). Both vagal and spinal afferent terminals must extensively branch within the wall of the gut; because of the relatively low number of vagal and spinal neurons providing this innervation, for example, it has been estimated that only 1–2% of the total spinal primary afferent neurons innervate the viscera (Janig and Morrison, 1986).
For the most part, the terminals of extrinsic primary afferent, parasympathetic and sympathetic nerves extensively innervate the enteric nervous system (ENS) – the third division of the autonomic nervous system, rather than other targets in the wall of the gut. However, there are specialized sensory endings and direct innervation of the vasculature by sympathetic and primary afferent terminals (Furness, 2012; Furness et al., 2013). The ENS consists of the intrinsic primary afferent, interneurons and motor neurons that control all functions of the GI tract. These neurons are arranged in two ganglionated plexuses: the myenteric plexus that lies between the longitudinal and circular muscle layers of the muscularis externa, and the submucosal plexus the lies in the submucosa (Furness, 2006; Furness, 2012). These two neuronal plexuses are interconnected. A small population of myenteric neurons, called viscerofugal neurons, make direct connections to postganglionic sympathetic neurons in the abdominal prevertebral ganglia (Sharkey et al., 1998; Szurszewski et al., 2002). These enteric neurons form the afferent limb of local sympathetic reflexes that control motility (Lomax et al., 2010).
Enteric neurons extensively innervate all the structural and functional elements of the gut: smooth muscle, epithelium, immune elements, and vasculature. However, what is remarkable about the gut innervation is that it frequently seems to act through intermediary cell types that are interposed between nerves and target tissues. Specifically, motor activity is regulated by Interstitial cells of Cajal (Sanders et al., 2010). , which may also transduce sensory information (Powley and Phillips, 2011), and platelet-derived growth factor receptor alpha-positive cells (Baker et al., 2013; Kurahashi et al., 2011; Sanders et al., 2010). Secretion is regulated in part by enteric mast and glial cells, as well as subepithelial myofibroblasts (Bischoff, 2009; Gulbransen and Sharkey, 2012; Powell et al., 1999). The immune elements of the gut are also innervated; that is to say, nerves directly innervate lymphoid organs, such as Peyer’s patches where adapted lymphocyte responses occur, as well as diffusely distributed immune cells, such as mast cells, dendritic cells and macrophages (Chiocchetti et al., 2008; de Jonge, 2011; Matteoli et al., 2013; Nijhuis et al., 2010).
Enteric glia
Like neurons in the brain, enteric neurons are surrounded by and outnumbered by glial cells. In the GI tract there is a unique type of peripheral glial cell called enteric glia (Gulbransen and Sharkey, 2012; Neunlist et al., 2013). These cells resemble astrocytes of the brain and are found in enteric ganglia in both the myenteric and submucosal plexus and also in two extra-ganglionic sites, intramuscularly and submucosally (Gulbransen and Sharkey, 2012). Perhaps surprisingly, there is a population of cells which have the phenotypic characteristics of enteric glia that lie just beneath the epithelium (Gulbransen and Sharkey, 2012; Neunlist et al., 2013). These subepithelial enteric glia have an intimate relationship with epithelial cells, and play a role in the maintenance of barrier function. Emerging work from several groups, including our own, has recently demonstrated that protective gut functions may be orchestrated by enteric glial cell mediators or via enteric glial modulation of neurotransmission and secretion in the GI tract (Bach-Ngohou et al., 2010; MacEachern et al., 2011; Neunlist et al., 2007; Savidge et al., 2007; Van Landeghem et al., 2011). It is not easy to reconcile such physiological events in vivo, but functional parallels can been drawn to astrocytes which are known to perform protective roles in the brain (Abbott et al., 2006). Enteric glia provide trophic and cytoprotective functions towards enteric neurons (Abdo et al., 2010; Abdo et al., 2012). Recently it has become clear that they also possess receptors for many enteric neurotransmitters and are activated by synaptic transmission, e.g. by ATP release from intrinsic and extrinsic neurons following chemical or electrical stimulation (Boesmans et al., 2013; Gomes et al., 2009; Gulbransen et al., 2010; Gulbransen et al., 2012; Gulbransen and Sharkey, 2009). This positions them to “listen” to the signaling in the ENS and respond appropriately. As ATP release is common in damaged tissues, it seems feasible that glial cells are also activated by environmental cues that may emanate from tissue trauma or infection. Not only do enteric glia respond to purines like ATP, they also respond to and make cytokines, possessing, for example, interleukin (IL)-1 receptors and making IL-1, IL-6 and chemokines such as monocyte chemotactic protein 1 (Murakami et al., 2009; Ruhl et al., 2001a; Ruhl et al., 2001b; Stoffels et al., 2013). However, the precise role for glial activation within enteric ganglia remains to be determined, although early studies suggest a regulatory role of neuronal activity and protection of tissue integrity, akin to astrocytes.
Cellular and molecular mechanisms by which enteric glia protect gut integrity from acute trauma, infection, or immune insult are beginning to emerge, and several lines of evidence suggest that this regulation is likely to be multi-factorial with a variety of cell types producing a range of molecules that may induce or compromise barrier functions. For example, elevated glial-derived neurotrophic factor during inflammation could act to protect cells from apoptosis (Bassotti et al., 2006; Steinkamp et al., 2012; von Boyen et al., 2006). Enteric glia actively secrete barrier inducing epidermal and transforming growth factor-β isoforms (Neunlist et al., 2007; Van Landeghem et al., 2011), as well as reactive nitric oxide derivatives - known as S-nitrosothiols which are phylogenically old cGMP-independent signaling systems that have been shown to exert global protective functions following intestinal inflammation, infection or burn trauma (Costantini et al., 2010; Flamant et al., 2011; Savidge, 2011; Savidge et al., 2007). Nitric oxide production by enteric glia in the myenteric plexus has also demonstrated a previously unappreciated anti-secretory signal in the colon, indicating that a nicotinic-glia-nitric oxide signaling mechanism may have evolved to override excessive fluid secretion during disease states (MacEachern et al., 2011). Therefore, regulation of mucosal barrier and secretory function by its microenvironment, and in particular by neuronal-glial circuits, may confer gut protection in these disease settings and represent potentially important target cells in GI inflammatory and permeability disorders.
Host defense
Protection of the GI tract from injury is accomplished by a series of physical and chemical barriers. The gut needs to be protected from harmful agents that have been ingested, as well as from the processes of digestion and from the normal luminal contents (Fasano and Shea-Donohue, 2005; McCole and Barrett, 2007; Turner, 2009). There are specialized regional barriers at various levels of the GI tract, such as acid in the stomach, as well as some that are found throughout the length of the gut, for example, epithelial tight junctions and mucus secreted by goblet cells. Given the focus of this article, we will explore the role of the enteric innervation in the functional regulation of components of the GI epithelial barrier.
Epithelial barrier function
A single layer of epithelial cells lining the stomach and intestine is all that prevents the outside world from entering “us”, whether we are between meals or when we have eaten. These cells have a rapid rate of turnover (2–4 days) and elaborate mechanisms ensure the regular restitution of epithelial barrier breach under normal conditions. The monolayer of polarized epithelial cells that forms a continuous interface along the gut is connected through apical junctional complexes. These intercellular complexes are composed of tight junctions, adherens junctions, desmosomes and gap junctions, the latter which serve for cell-to-cell communication (Laukoetter et al., 2006; Shen et al., 2011; Turner and Turner, 2010; Turner, 2009). The protein complexes that form these junctions are regulated by many factors, for example, inflammatory mediators. The control of these protein complexes regulates epithelial permeability to molecules ranging in size from single ion permeability, regulated by claudin family members, to larger molecules regulated by zonula occludens (ZO) and occludin isoforms. Are enteric nerves involved in the control of epithelial barrier function or do they indirectly influence the permeability of the epithelium by altering the regulation of the apical junctional complex? There is increasing evidence that the answer to this question is yes, to both possibilities, but relatively few studies have directly examined this question.
Role of enteric nerves in the control of epithelial permeability
Direct evidence for the role of enteric nerves in the regulation of intestinal permeability in intact preparations under physiological conditions is quite limited. In a recent study, Overman et al. showed that the addition of the sodium channel blocker, tetrodotoxin (TTX), to preparations of the porcine ileum reduced mucosal to serosal flux of a fluorescent 4kDa macromolecular marker that passed through epithelial tight junctions (Overman et al., 2012). These data suggest that there is a tonic control of epithelial permeability by enteric nerves. However, at the same time, TTX reduced the degranulation of mucosal mast cells in these preparations, so it is not clear if the neural effect on permeability is directly or indirectly mediated. These findings are similar to that obtained by Cameron and Perdue in mouse jejunum (Cameron and Perdue, 2007). They not only showed that TTX reduced the baseline flux of horseradish peroxidase (HRP), another macromolecular permeability marker, but so did the muscarinic cholinergic antagonist atropine, suggesting a cholinergic input controls epithelial tight junctions. Consistent with this finding, the cholinergic agonist bethanechol stimulated an increase in the flux of HRP through activation of M3 receptors (Cameron and Perdue, 2007). Building on these observations, Gareau et al. demonstrated that HRP flux was greater in young rats subjected to stress (maternal separation) than in non-stressed controls (Gareau et al., 2007). This enhanced permeability was reduced to below control levels with atropine and further reduced by the nicotinic receptor antagonist hexamethonium. One interesting, but potentially complicating factor in this study, was that in the stressed animals, choline acetyltransferase (ChAT) expression was increased in the epithelium. ChAT is the rate limiting enzyme for acetylcholine (ACh) synthesis, suggesting that, at least under conditions of stress, there may be an autocrine component of cholinergic control of permeability, in addition to the neural component seen under baseline conditions (Gareau et al., 2007). The presence of an epithelial cholinergic system (muscarinic receptors and the ligand, ACh) has also been reported by others in both the small and large intestine of animals and humans (Gautron et al., 2013; Jonsson et al., 2007; Klapproth et al., 1997); in intestinal inflammation, epithelial ChAT expression was reduced (Gautron et al., 2013). In older studies, Saunders et al. also found a muscarinic cholinergic enhancement of permeability in stressed rat jejunum, but no nicotinic receptor involvement was observed in this case (Saunders et al., 1997). Further evidence for a role of cholinergic nerves in the control of permeability comes from studies that investigated bile acid induced enhancement of colonic permeability. Here, both a nicotinic and muscarinic component were identified as contributing to the serosal to luminal flux of mannitol and urea, possibly emanating from ligand activation of the recently described G-protein coupled bile acid receptor TGR5 (Cipriani et al., 2011; Fihn et al., 2003; Sun et al., 2004). The full significance of the sources of ACh and the relative role of cholinergic nerves at different levels of the gut in the control of epithelial permeability remains to be completely determined. An influence of enhanced fluid secretion hampering epithelial access of luminal macromolecular markers is also a consideration of such studies.
The role of stress and corticotrophin releasing factor
Gareau et al. and Overman et al., also explored the role of the stress hormone corticotrophin releasing factor (CRF) in the cholinergic control of permeability in the colon of rats and the ileum of pigs, respectively. Gareau et al. provided strong evidence that CRF acted via cholinergic nerves to regulate intestinal permeability (Gareau et al., 2007), which was extended by Overman et al. who showed that CRF acted via mast cells and through a TTX-sensitive, likely cholinergic, neural pathway (Overman et al., 2012). These data support previous observations that demonstrated a role for cholinergic and adrenergic nerves and mast cells in regulating CRF-induced enhanced permeability in the rat colon (Barreau et al., 2007; Santos et al., 1999). Moreover, CRF induced activation of the myenteric cholinergic neurons assessed by the neuronal activity marker Fos supports these observations (Miampamba et al., 2002; Yuan et al., 2007). That said, at least when injected intraperitoneally, CRF only seems to activate colonic myenteric, but not submucosal, neurons and not those in the small intestine or stomach (Yuan et al., 2007). Given that the physiological changes in barrier function described above were occurring in the small bowel, it remains to be determined exactly what is happening (patho)physiologically in various bowel regions in animals under conditions of stress involving the release of CRF and under baseline conditions. However, it seems fair to conclude that enteric nerves regulate epithelial barrier function either directly or indirectly, and in the case of an indirect effect, mast cell mediators may be an important source of mediators regulating tight junctions. The overall pathophysiological importance of these data relates to the control of permeability during conditions of stress; building on these data Yu et al. have recently shown that this may lead to a failure of tolerance to bacterial endotoxin and hence the development of clinical or subclinical inflammation and associated conditions of irritable bowel syndrome and inflammatory bowel disease (Yu et al., 2013).
Role of vasoactive intestinal peptide
Vasoactive intestinal peptide (VIP) is an important secretomotor transmitter extensively expressed throughout the intestinal mucosa. The secretomotor innervation is largely from submucosal neurons, but in some regions may also come as a direct projection from the myenteric plexus, for example in the stomach (Furness, 2006). Using an elegant human co-culture model, Neunlist et al. showed that electrical stimulation of submucosal neurons elicited a reduction in flux of paracellular permeability markers across a monolayer of epithelial cells (Neunlist et al., 2003). This effect was blocked by a VIP receptor antagonist and mimicked by application of VIP directly to the monolayer. The molecular mechanism of this effect was determined to be an increase in the expression of the tight junction protein ZO-1. Advancing this observation to a pathophysiological model of colitis, Conlin et al. found that VIP could prevent the increase in mannitol flux observed in animals infected with the bacterium Citrobacter rodentium (Conlin et al., 2009). In studies of isolated epithelial monolayers, infected with an analogous pathogen, VIP was found to reduce the re-distribution of tight junction proteins caused by the pathogen by preventing an increase in the myosin light chain kinase expression and the phosphorylation of myosin light chain (Conlin et al., 2009). The role of VIP (and the cholinergic agonist carbachol) has also been assessed in low birth weight neonatal piglets fed various diets (Boudry et al., 2011). Here, it reduced epithelial permeability in the jejunum but had no effect in the ileum, and its effects were not observed when animals were on a high protein diet. However, its effects were seen when they were fed an adequate protein diet or by their mothers. The significance of these differences is not clear. In contrast to these studies in which VIP reduced intestinal permeability a recent study in rat and human tissues found VIP stimulated permeability, and increased bacterial translocation (Keita et al., 2013). In rats, stress increased epithelial permeability, an effect that was largely blocked by a VIP receptor antagonist, and also the mast cell stabilizer doxantrazole. When VIP was added exogenously to ileal preparations, it also increased epithelial permeability and its effects were blocked by doxantrazole. In this study, VIP receptors were found localized on mast cells, supporting the functional observations. Similar findings were made in the human ileum, but interestingly not the human colon (Keita et al., 2013). It seems unlikely the differences between these three studies are due to species differences, but the preparations used differ considerably and this might explain the different effects. Further studies are required to ascertain the role of VIP in different regions of the gut under physiological and pathophysiological conditions.
Extrinsic autonomic control of epithelial barrier function
The extrinsic innervation of the GI tract has recently been the focus of more attention with regards to its role in the regulation of epithelial permeability. The primary observations relate to the role of vagal stimulation on enhancing barrier function in conditions where it is severely compromised, in animals with a burn injury or endotoxemia (Costantini et al., 2010; Costantini et al., 2012; Krzyzaniak et al., 2011; Zhou et al., 2013). Electrical vagal nerve stimulation prior to or up to 90 min afterwards prevented the breakdown of epithelial barrier function after a burn injury, assessed using the permeability of 4kDa labeled dextran (Costantini et al., 2010; Costantini et al., 2012; Krzyzaniak et al., 2011). This effect seems to involve the reorganization of ZO-1 expression and reduced expression of occludin, and is mimicked by the nicotinic cholinergic agonist nicotine. It may also involve enteric glial cells, since vagal nerve stimulation activated enteric glia and the protective effects of vagal nerve stimulation were mimicked by S-nitrosoglutathione, which is released by enteric glia (Costantini et al., 2010; Savidge et al., 2007). Endotoxemia also leads to a loss of barrier function and the disruption of tight junctions (Zhou et al., 2013). Carbachol, another nicotinic receptor agonist, was found to prevent the redistribution of ZO-1 and claudin-2, and reduced permeability under these conditions (Zhang and Li, 2012). Interestingly, this effect was prevented by an alpha7 nicotinic receptor antagonist, alpha-bungarotoxin. Furthermore, the effects of carbachol and the actions of the vagal stimulation were also prevented by blocking alpha7 nicotinic receptors (Zhang and Li, 2012). These results are particularly interesting in relation to the anti-inflammatory actions of vagal nerve stimulation (see Martelli et al., this volume), and likely contribute to the benefits seen in animals.
In addition to vagal nerve stimulation, epithelial barrier function of the rectum may also be enhanced by sacral nerve stimulation, and blocking sympathetic outflow to the gut by spinal epidural anesthetic also seems to enhance barrier function (Meurette et al., 2012; Schaper et al., 2013). The mediators and molecular mechanisms that cause the improved barrier function in these two models remains to be determined.
Epithelial cell proliferation
Another important feature of epithelial barrier function is the renewal of the epithelium by proliferation of stem cells. It has long been known that vagotomy alters the morphology of the gastric mucosa (Axelson et al., 1988), illustrating a role of the enteric innervation on epithelial cell proliferation, either through direct or indirect influences on the stem cell niche. Similarly, ablation of the myenteric plexus using a detergent profoundly alters the morphology of the mucosa overlying the intrinsically denervated segment (Hadzijahic et al., 1993; Holle, 1991; Holle et al., 2003). Loss of the plexus induces crypt cell proliferation dramatically altering the mucosal architecture and distribution of enteroendocrine cells (Holle et al., 2003; Zucoloto et al., 1997). The mediators of this effect remain to be determined, though VIP has been implicated in the regulation of proliferation in a cell culture model (Toumi et al., 2003). Enteric nerves are also involved in the regulation of epithelial progenitor cells in response to the enteroendocrine peptide glucagon like peptide (GLP)-2, since the proliferative response to GLP-2 are sensitive to TTX (Bjerknes and Cheng, 2001). The role of VIP in this response has recently been examined using animals lacking the VIP gene (Yusta et al., 2012). Here, it was shown that GLP-2 significantly increased crypt cell proliferation and small bowel growth to comparable levels in animals with or without the VIP gene. Thus, other enteric neurotransmitters must also be involved in regulating epithelial cell proliferation.
One recently discovered potential mediator of proliferation is serotonin (5-HT). The majority of the 5-HT in the gut is in mucosal enterochromaffin cells, but a small population of myenteric neurons also express 5-HT (Gershon, 2013). Neuronal 5-HT is synthesized by tryptophan hydroxylase (TPH)-2, whereas mucosal 5-HT is derived exclusively from TPH-1. It was observed that mucosal growth and proliferation of mucosal cells was greater in mice that lacked the serotonin transporter, SERT, or wild type mice given selective serotonin reuptake inhibitors (Gross et al., 2012). Mucosal growth was also enhanced in mice lacking TPH-1 that were given selective serotonin reuptake inhibitors, an effect that was not seen in mice lacking TPH-2, strongly suggesting that the myenteric neuronal population mediated the proliferative effect of 5-HT on the mucosa. The effect of 5-HT was mediated by 5-HT2A receptors on submucosal cholinergic neurons, which innervate the mucosal effector cells (Gross et al., 2012).
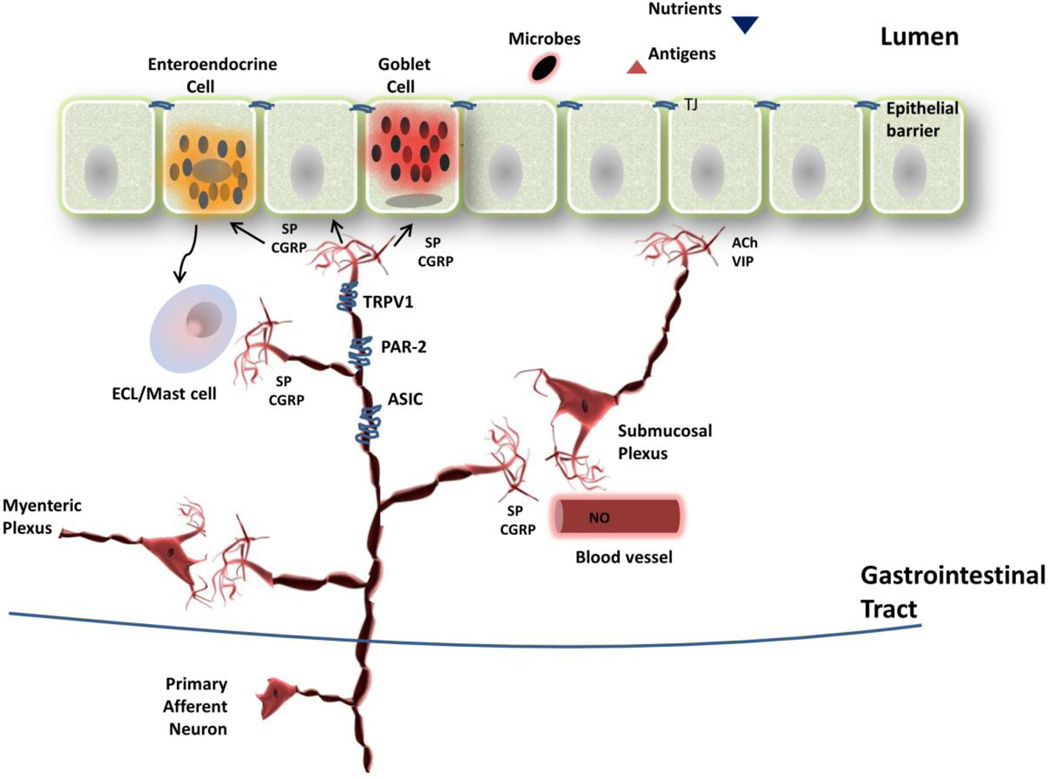
Epithelial cell proliferation may also be stimulated by activation of capsaicin-sensitive primary afferent nerves. Capsaicin, the pungent ingredient of hot peppers, activates transient receptor potential vanilloid 1 (TRPV1) receptors on spinal and vagal afferents that innervate the intestinal mucosa (Holzer, 2007). Upon activation these nerves release their transmitters, substance P and calcitonin gene-related peptide (CGRP), locally (possibly through axon reflex mechanisms) where they activate submucosal and/or myenteric neurons (Figure 1). They also initiate spinal reflexes through their terminals in the dorsal horn of the spinal cord. Local activation of capsaicin-sensitive nerves increases epithelial cell proliferation through substance P (neurokinin 1) receptors, CGRP receptors and muscarinic cholinergic receptors (Lundgren et al., 2011). It has been suggested that cholinergic nerves are activated by the primary afferent transmitters, and in turn activate the stem cell progenitors, possibly via the induction of transforming growth factor alpha (Hoffmann et al., 2002).
Figure 1.
Local effector functions of extrinsic primary afferent nerves in the gastrointestinal tract. Extrinsic primary afferent nerves stimulated directly through receptor mediated events or indirectly via luminal activation of epithelial cells or immune cells (not shown) locally release the peptides mediators substance P and CGRP to activate protective events in the gut wall. These include epithelial cell proliferation, mucus secretion, mast cell and enterochromaffin-like cell activation and/or vasodilatation, as described above. Some of these events have only been described in specific regions of the gut. ACh, acetylcholine; ASIC, acid sensing ion channel; CGRP, calcitonin gene-related peptide; ECL, enterochromaffin-like cell; NO, nitric oxide; PAR-2, protease activated receptor 2; SP, substance P; TJ, tight junction; TRPV1, transient receptor potential vanilloid 1 receptor; VIP, vasoactive intestinal peptide
Neural control of secretion
The secretion of fluid from the epithelium is an important component of barrier function (Barrett and Keely, 2000; Turner, 2009). For example, acid is secreted in the stomach for digestion, but also to sterilize food. Specialized glands in the duodenum (Brunner’s glands) are able to sustain high levels of bicarbonate secretion to protect it from gastric acid and pepsin (Moore et al., 2000). Similarly, along the intestine, bursts of secretion, regulated largely by enteric cholinergic and VIP expressing nerves, protect the mucosa from physical damage in response to mechanical stimulation and the fluid itself serves to dilute potential cytotoxins (Barrett and Keely, 2000; Chu and Schubert, 2013). We cannot review this whole subject in this short article, but have selected a recent novel observation to illustrate how luminal bacteria may interact with host defense mechanisms.
In the stomach, acid secretion is controlled by vagal cholinergic and enteric neuronal pathways (involving ACh and gastrin releasing peptide) that provide an initial cephalic phase of acid secretion to prepare the stomach for the entry of food, followed by a sustained secretion of acid for digestive and antimicrobial functions (Furness, 2006; Schubert and Shamburek, 1990). Acid stimulates blood flow required to sustain the secretion and provides a mechanism for the clearance of noxious agents. The local vasodilatation is regulated by the release of CGRP from primary afferent nerves by activation of TRPV1 receptors and by nitric oxide from the endothelium (Holzer, 2000a; Holzer, 2000b; Holzer, 2007; Schicho et al., 2003). CGRP release also serves as a negative feedback signal to inhibit acid secretion through the release of somatostatin from D cells of the gastric epithelium (Schubert and Shamburek, 1990). This elegant arrangement serves to effectively protect the gastric mucosa under physiological conditions (Figure 1). However, this protective mechanism can be manipulated under pathophysiological conditions.
Given the hostility of the gastric environment, it is challenging to imagine how even a highly evolved resident bacterium, Helicobacter pylori, could survive and colonize the stomach; they do so by using our own gastroprotective mechanisms. Zaki et al. have recently demonstrated that H. pylori activates capsaicin-sensitive primary afferents to release CGRP, which by releasing somatostatin, inhibits histamine secretion from enterochromaffin-like cells and so reduces acid secretion making it easier for the bacteria to establish themselves (Zaki et al., 2013). These findings support previous work that demonstrates enhanced expression of CGRP in the stomach (and also spinal cord) of H. pylori infected mice. Taken together, these fascinating observations illustrate how the neural regulatory systems of the host can be utilized by bacterial pathogens to overcome elements of defense and as we discuss later, how bacteria themselves may utilize neurotransmitters for direct interaction with the host.
Mucus, trefoil factors, defensins and secretory IgA
Goblet cells are distributed along the length of the gut and serve a vital role for protection of the GI tract; the mucus barrier is commonly regarded as an important physico-chemical defense (McGuckin et al., 2011). However, a diverse range of MUC protein products and trefoil factor constituents in mucin enhance barrier function and promote epithelial restitution and repair. In the small bowel, additional defense is provided by Paneth cells, which secrete antimicrobial peptides called defensins (Clevers and Bevins, 2013; Ouellette, 2011; Salzman, 2010). Finally, the gut possesses an immunological barrier accomplished by the secretion of polymeric IgA from the epithelium to the lumen (Brandtzaeg, 2013). The degree to which each of these secretory components is under neural control varies, but remarkably few studies have investigated these in a systematic manner. In all cases, cholinergic control is exercised through muscarinic receptor mechanisms, and where it has been examined, VIP also seems to be prosecretory (Castagliuolo et al., 1996; Lyte et al., 2011; Moro et al., 2001; Ogata and Podolsky, 1997; Schmidt et al., 2007). These data are consistent with the known pattern of innervation of the mucosa from submucosal neurons. The vagus plays an important role in the tonic secretion of gastric mucus (Somasundaram and Ganguly, 1987), but does not seem to have such a role in the jejunum (Greenwood and Mantle, 1992). Sympathetic mechanisms or stress increases the secretion of IgA and mucin (Castagliuolo et al., 1996; Lyte et al., 2011; Schmidt et al., 2007), although one report has found that norepinephrine inhibits the secretion of IgA (Schmidt et al., 1999).
A recent study highlights an interesting potential for mucin secretion to be controlled from the luminal aspect of the gut. Hoffman et al. investigated the distribution of 5-HT4 receptors along the GI tract and found they were present on epithelial and goblet cells (Hoffman et al., 2012). Interestingly, addition of 5-HT4 agonists to the gut lumen caused cavitation of goblet cells, an indicator of mucin secretion. These observations extend earlier work in which cholera toxin-induced mucin secretion was found to be regulated via capsaicin-sensitive nerves (Figure 1), utilizing muscarinic cholinergic and 5-HT4 receptor mechanisms (Moore et al., 1993; Moore et al., 1996). These data support the concept that local activation of mucosal nerves and enterochromaffin cells serve as important defense mechanisms in response to potentially injurious luminal factors. As we discuss the role of bacteria signaling to the gut we will expand on this concept further.
Mucosal immunity and the gut-associated lymphoid tissue (GALT)
It has long been known that the GALT and diffuse immune systems of the GI tract receive extensive innervation, leading to thorough investigations of neuroimmune function in relation to host defense (Chiocchetti et al., 2008; Crivellato et al., 2002; Crivellato et al., 1998; Felten et al., 1992; Lawson et al., 2010; Straub et al., 2006). These have recently been extensively reviewed, including articles in the current volume (Martelli et al. and Lomax) and will only be briefly touched on here. Nerves in the wall of the gut serve to both respond to threats as an alarm system, as well as to integrate host defense thereby contributing to barrier function. Much of the focus has been on the role of the extrinsic nerves of all classes. Primary afferents of vagal origin are activated by local immune and inflammatory stimuli, as well as enteroendocrine mediators, and initiate vagal reflexes including the vagal anti-inflammatory reflex (Costes et al., 2013; de Jonge, 2013; Dhawan et al., 2012)(see also Martelli et al., this volume). Spinal primary afferents are endowed with TRPV1 and protease activated receptor 2 receptors, as well as other TRP receptors allowing them to respond with the release of mediators such as substance P and CGRP that locally regulate immune function and blood flow (Holzer, 2007; Vergnolle, 2009). This gives rise to neurogenic inflammation, which is an acute, protective response to injury involving resident mast cells as well as stimulating infiltration of neutrophils and other leukocytes.
Integration of immune responses in the gut wall relies on the enteric neural regulation of immune responses. Notable are the actions of the transmitters VIP, substance P, somatostatin and neuropeptide Y (NPY), which potently activate many classes of leukocytes in the wall of the gut and regulate inflammation (Chandrasekharan et al., 2013b; Engel et al., 2011; Gross and Pothoulakis, 2007; Keita and Soderholm, 2010; Margolis and Gershon, 2009; Nijhuis et al., 2010). In addition, there are very potent immunomodulatory actions of endogenous opioids and cannabinoids, both of which are widely expressed in the GI tract and, for example, reduce intestinal inflammation (Gross and Pothoulakis, 2007; Izzo and Sharkey, 2010). However, as noted for other elements of host defense, there are few systematic studies that have examined the role of endogenously released enteric neurotransmitters of specific immune functions. Moreover, there are many examples where the neuroimmune interactions lead to maladaptive changes, so one of the big challenges that remains is to understand the regulatory functions that restore homeostasis when immune interactions lead to a breakdown in host defense. This is illustrated by a recent study that shows the interactions between tumor necrosis factor (TNF) and NPY (Chandrasekharan et al., 2013a). Using primary cultures of enteric neurons and colon explant cultures from wild type and NPY knockout mice, it was found that enteric neurons express TNF receptors (TNFR1 and R2). Primary enteric neurons from NPY knockout mice produced less TNF compared with wild type. Further, TNF activated the NPY promoter in enteric neurons through phospho-c-Jun and increased expression of NPY. However, NPY increased epithelial permeability through the pore-forming tight junctional protein claudin-2. These results help explain why NPY is pro-inflammatory in the GI tract (Chandrasekharan et al., 2008), but not why such a system would have evolved in the first place, or what prevents a modest inflammation from becoming an unregulated chronic inflammatory event leading to widespread tissue destruction.
Two other considerations merit discussion. The first is that enteric neurons express the innate immune signaling receptors, toll-like receptors (TLRs). To date, TLR2, 3, 4 and 7 have been shown to be expressed on enteric neurons (Anitha et al., 2012; Barajon et al., 2009; Brun et al., 2013; Esposito et al., 2013; Rumio et al., 2006). These are receptors for bacterial membrane glycolipids and glycoproteins (TLR2), double-stranded RNA (TLR3), bacterial lipopolysaccharide (TLR4) and single-stranded RNA (TLR7), respectively. Taken at face value, this implies bacterial and viral signaling to the ENS, but it seems likely that their role is more complex. For example, the structure of the ENS is markedly altered in mice that lack TLR2 and TLR4 (Anitha et al., 2012; Brun et al., 2013), suggesting a developmental role for this innate immune signaling system. Interestingly, wild-type mice depleted of intestinal microbiota had ENS defects similar to TLR2 knockout mice (Brun et al., 2013). The consequences of not having a fully developed ENS are striking; TLR2 knockout mice developed more severe colitis than wild-type mice. These data imply that during enteric development bacterial signaling to the ENS primes the ENS for adulthood by stimulating growth and specific neurochemical phenotypes. This is then better able to protect the adult in the face of an inflammatory stimulus. Our understanding of innate immune signaling and the ENS is very rudimentary, making further conjecture very speculative; this topic requires considerable further study.
The second are the immune interactions between enteric neurons and enteric glia. Enteric glia are able to produce and secrete immune signaling molecules such as IL-1 and IL-6 (Esposito et al., 2013; Ruhl et al., 2001a; Ruhl et al., 2001b; Stoffels et al., 2013) , as are enteric neurons (e.g., IL-8; (Tixier et al., 2005)). Again, we know little about the (patho-) physiological roles of these immune mediators, but support for a variety of functions has been provided; for example, IL-1 has neurotrophic actions (Gougeon et al., 2013), suppresses neurotransmitter release presynaptically (Xia et al., 1999), and enhances the excitatory action of bradykinin (Murakami et al., 2009). These data further support the concept of glial-neuron crosstalk as discussed above.
Bacterial signaling to the enteric nervous system
Given that resident in the lumen of the gut are hundreds of bacterial species and that many species of bacteria appear to exert physiological effects on the GI tract when administered orally, it would not be surprising to find bacterial signaling to the host involving the enteric innervation. What has been described though are some extremely interesting findings suggesting that the excitability of enteric intrinsic primary afferent neurons is regulated by the presence of a commensal microflora. McVey Neufeld et al. examined segments of the jejunum from germ-free, specific pathogen-free and germ-free mice that had been re-housed under conventional conditions, and so would have a normal bacterial flora (McVey Neufeld et al., 2013). Germ-free mice displayed less excitable intrinsic primary afferent neurons (termed AH [afterhyperpolarization] neurons (Furness et al., 1998)), with reduced resting membrane potentials and reduced input resistance compared to either of the other groups. These data support the idea that the physiological activity of the enteric nervous system is governed in part by the luminal environment of the gut. They build on other observations showing that intrinsic primary afferent excitability is influenced by luminal bacteria. For example, the probiotic bacterium Lactobacillus reuteri enhances the excitability of colonic myenteric AH neurons in the rat by reducing the activity of the calcium activated potassium channel that normally controls the magnitude of the after hyperpolarization in these neurons (Kunze et al., 2009). It is likely that there are many bacterial signaling moieties involved in this bacterial communication with enteric neurons, including histamine release or TLR activation. Mao et al. have shown direct evidence that polysaccharide A of Bacteroides fragilis is sufficient to enhance the excitability of myenteric AH cells, and when this bacterium is engineered to lack this molecule, the increased excitability seen with acute administration of this bacterium is lost (Mao et al., 2013). What remains to be determined is what the dominant signaling pathways are when hundreds of bacterial species interact and signal to the ENS, and how homeostasis and host defense are accomplished as bacterial composition is modified during the regular perturbations imposed by dietary changes, acute infections, etc.
Bacterial signaling involves not only local enteric neurons, but also the vagal and spinal innervation of the gut (Collins et al., 2012). For example, vagal afferent activity in response to normal physiological stimuli is altered by the presence of specific luminal bacteria (Perez-Burgos et al., 2013). Similarly, spinal primary afferent signaling is modulated by bacterial cell products; effects that can reduce or increase excitability depending on the bacterial species involved (Kamiya et al., 2006; Ma et al., 2009; Ochoa-Cortes et al., 2010). The implications for host defense are considerable since reflex actions that alter motor and secretory functions are under central neural control as well as local control. It remains to be determined how bacterial signaling fits into the hierarchical regulation of gut function, but moving forwards, it is apparent that luminal bacteria must be considered as essential elements in the context of enteric neural control of host defense.
Finally, an important component of luminal signaling to the epithelium is accomplished by proteases. This topic has been recently reviewed and so will only be touched on briefly here (Steck et al., 2012). Both bacteria and host cells release proteases that can activate protease activated receptors (PARs) which are not only found on epithelial cells but are also found on enteric neurons and extrinsic nerves innervating the gut. There are four PARs (PAR1, PAR2, PAR3, PAR4), all of which are G-protein coupled receptors that act as tethered ligands, activating the cell on which they are expressed (Vergnolle, 2009). They are activated by proteolytic cleavage of the N-terminus, which allows the ligand domain to bind to the receptor. PAR1, PAR2 and PAR4 activate enteric neurons, enteric glia and extrinsic primary afferents, and the responses of that occur following this activation form part of the host defense response (Buhner et al., 2012; Buresi et al., 2005; Green et al., 2000; Kugler et al., 2012; Mueller et al., 2011). Notable, as it pertains to disease, is that supernatants of biopsies taken from patients with irritable bowel syndrome (IBS) and IBD have elevated levels of protease activity which is thought to contribute to disease pathogenesis and symptom generation in these conditions (Buhner et al., 2012). The sources of protease activity (host versus bacterial) in biopsy supernatants remain to be fully determined, but could involve a multitude of signaling pathways including interferon-γ, PAR2 or TGR5 ligands.
Supernatants of colonic biopsy samples from IBS patients contain proteases that directly sensitize mouse primary afferent neurons and generate visceral and somatic hypersensitivity through the activation of PAR2 (Cenac et al., 2007; Hughes et al., 2013; Valdez-Morales et al., 2013). PAR2 activation in the GI tract also gives rise to neurogenic inflammation, through activation of primary afferent nerves and secretion, by activation of enteric neurons (Ikehara et al., 2012; Ikehara et al., 2010; Nguyen et al., 2003). Mucosal biopsy supernatants from patients with IBS also activate human enteric neurons and enteric glia (Buhner et al., 2012; Buhner et al., 2009). When these supernatants were studied on guinea pig enteric neurons, it was found that only a small proportion of myenteric neurons responded to the supernatants, whereas about half the submucosal neurons responded. PAR1 is expressed on secretomotor neurons of the submucosal plexus and agonists of this receptor inhibit fluid secretion in the mouse colon (Buresi et al., 2005). In contrast, in the mouse cecum, PAR1, but not PAR2, simulates secretion by releasing substance P (acting via neurokinin 1 receptors) and ACh (Ikehara et al., 2010). These early data are supportive of the concept of protease signaling through neural pathways to regulate host defense responses. Further work is required to dissect the contributions of bacterial and host proteases and how these circumstances, where protease activated pathways link to the other elements of host defense, contributing to the integration of mechanisms that ensure the overall maintenance of barrier function.
Microbial sources of enteric neurotransmission: new kids on the block
In a healthy individual, several complex factors determine the microbial composition of the GI tract, collectively termed as the microbiome. Host immune, genetic and environmental factors, including diet, all help to shape the gut microbiota composition. Although small intestinal microbes remain a hotly debated topic in GI disease, the vast majority of bacteria inhabit the colon where concentrations normally reach between 1011–1012 cells per gram of stool (Collins et al., 2012; Simren et al., 2013). The complexity of this “living organ” is highlighted by that fact that the microbiome is individual specific, although a recent report has proposed that the human gut microbiota is comprised of 3 general enterotypes of groups of species that contribute to a defined microbial community. An emerging consensus recognizes that such enterotype clusters may have co-evolved to play an important physiological role in human health (Simren et al., 2013).
More than 50 different bacterial phyla have now been identified, of which Firmicutes, Bacteroidetes and Actinobacteria dominate in the human colon (Backhed et al., 2005; Lozupone et al., 2012). Modern molecular-based pyrosequencing technology of ribosomal 16S RNA gene heterogeneity - which allows thousands of microbial species to be detected simultaneously in a single experiment - readily indicates that our understanding of microbial influences on human health and disease is only in its infancy since most bacteria identified still remain uncultured using traditional methods. However, such culture-based methods remain the gold standard for detection and classification of microbes. Although cultured species represent merely 20–30% of identified gut phylotypes, a distinct advantage exists using such an approach because the more abundant species often correspond to better characterized bacteria in terms of known biological function and potential health benefits. Moreover, experimental manipulation of such bacteria has recently demonstrated that they may play an important role in regulating neurotransmission in the GI tract. For example, inflammation of the GI tract is often associated with higher levels of anaerobic Clostridium, facultative Escherichia coli and streptococci, with reduced counts of histamine and GABA-producing lactobaccili and bifidobactera in stool (Hemarajata and Versalovic, 2013). In addition to its role during an immune response, histamine is an important signaling molecule in the GI system as it regulates bowel movements, intestinal permeability, and gastric acid secretion. At present, it is not clear whether such microbial dysbiosis results from altered host influences, or whether microbial-derived neurotransmitters may represent a primary cause of GI dysfunction.
Altered metabolic activity of gut microbes has been implicated in protection and regulation of the GI tract (Devkota and Chang, 2013; Geurts et al., 2013; Sommer and Backhed, 2013). Given the ability of microbes to influence intestinal permeability, activity in the ENS and the brain, it is not surprising that numerous reports have described shifting microbial taxa associated with clinical disease severity, e.g. IBD, celiac disease, Clostridium difficile infection, and post-infectious IBS (Simren et al., 2013). In many cases, clinical symptoms are alleviated by altering microbial communities using prebiotics, probiotics and antibiotics. Onset of disease symptoms of IBS after an initial episode of gastroenteritis is also supportive of a role for microbes in GI pathogenesis. Notably, following traveler’s diarrhea caused by bacterial infections by E. coli, Salmonella and Campylobacter, onset of IBS symptoms are commonly associated with severity of toxin secretion and gut pathology (Ohman and Simren, 2013). Protective mechanisms may be disrupted by modulation of a healthy gut microbiome, or metabolites such as short chain fatty acid-induced changes in luminal pH and colonic motility, elevated inflammation, and enteroendocrine cell hyperplasia that alters the balance of neuropeptide secretions (Macia et al., 2012). For example, changes in motility and secretion can drastically regulate microbiome composition by restricting nutrient delivery, and consequently altering luminal pH in healthy and diseased states (Deloose et al., 2012; Keely et al., 2012). Notably, disruption of migrating motor complexes associated with fasting that are under autonomic nervous system control, can cause a dysmotility that results in small intestinal bacterial overgrowth (Deloose et al., 2012; Lin and Pimentel, 2005). Interestingly, Ward et al. have recently shown that colonic aganglionosis of the ENS causes a profound disruption of the colonic and fecal microbiota and marked changes in the fecal metabolite profile (Ward et al., 2012). Although the exact reason why this happens was not explored, presumably the loss of motor and secretomotor control led to the compositional shift in the microbiome.
Immune activation in the gut is regulated by autonomic nervous system mediated modulation of responses to microbes or luminal antigens that breach the mucosal barrier interface (de Jonge, 2013; Keita and Soderholm, 2010). As described above, stress participates in such events by promoting bacterial translocation through enhancing mucosal permeability and local immune responses. Such a barrier dysfunction may in part result from stress-induced alteration of tight junction proteins on intestinal epithelial cells, as well as activation of mast, neuronal and glial cells in the mucosa, but also through modulation of the host microbiome (Keita and Soderholm, 2010; Neunlist et al., 2013).
Host enteroendocrine signals secreted into the lumen may also alter gut microbiome composition and function, and include catecholamines (Chen et al., 2003; Freestone et al., 2008; Green et al., 2003; Lyte et al., 2011; Pacheco and Sperandio, 2009). Several studies are strongly suggestive that the brain regulates luminal secretion of these factors (Rhee et al., 2009). For example, cold stress induces mast cell release of histamine into the small intestine in humans (Santos et al., 1998), whereas central nervous system administration of a thyrotropin releasing hormone analog – a central effector to cold stress – induces 5-HT release into the gastric lumen (Stephens, 1991; Stephens and Tache, 1989). Host factors may also influence virulence of enteric pathogens and parasites (Karavolos et al., 2013). For example, catecholamines can regulate virulence of enterohemorrhagic E. coli (Hughes et al., 2009) and Campylobacter jejuni (Cogan et al., 2007). Bacteria themselves may also contribute to this luminal signaling environment, since luminal bacteria are also able to produce norepinephrine and dopamine and these agents contribute to regulation of gut physiology (Asano et al., 2012).
Brain influences on GI function and the microbiome are also implicated via the hypothalamic pituitary adrenal axis and the autonomic nervous system, which are known regulators of gut microbiota composition by influencing mucosal-microbial crosstalk (via altered permeability, motility, secretion of fluid and neuropeptides) (Collins et al., 2012; Rhee et al., 2009). The gut microbiota may be regulated by any one of these factors; for example, microbiome colonization and diversity are regulated by psychological stressors (Bailey et al., 2004; Bangsgaard Bendtsen et al., 2012), and this can lead to the development of intestinal inflammation (Sun et al., 2013). The altered bacterial composition may subsequently influence autonomic output by changing the brain’s response to environmental and internal stimuli, leading to the potential for a maladaptive cycle that may explain, in some cases, why altering the composition of intestinal bacteria may influence psychological and even psychiatric disorders as well as intestinal disorders influenced by autonomic neural factors (Collins et al., 2012; Dinan and Cryan, 2012; Forsythe et al., 2012; O'Malley et al., 2011). Interestingly, an emerging literature now also suggests that microbiome-associated neuroactive metabolites can regulate brain development and function of the central nervous system (Collins et al., 2012; Rhee et al., 2009). Thus, both brain–gut–microbiome (top-to-bottom) and microbiome-gut-brain (bottom-to-top) signaling will likely prove to be important regulators of gut protective mechanisms in the future. With the advent of high throughput microarrays and pyrosequencing methods, new techniques are emerging for global analysis of bacterial community richness. Combining such technology with global unbiased metabolomics methods to quantify microbial-derived neurotransmitters in stool, it is now possible to start the arduous process of identifying how microbial dysbiosis is associated with gut disease and whether microbial-derived neurotransmitters contribute to altered enteric nervous system function.
Summary and Conclusions
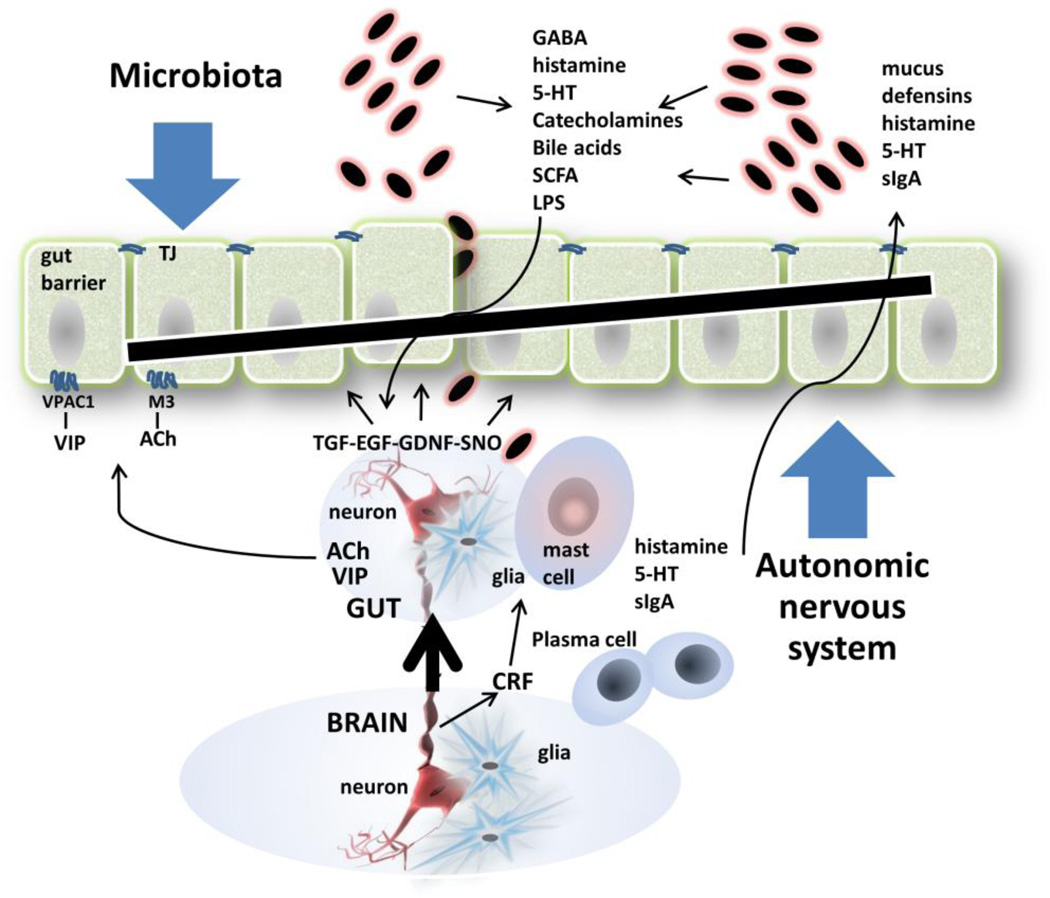
Altered enteric neurotransmission is emerging as a central feature in a range of gut diseases where protective function is compromised. Disruption of the gut protective barrier may occur at several levels, including physical breach of epithelial cell defenses by antigen, infective or commensal microorganisms, imbalance of humoral and immune mediators, or adverse stress signals elicited from the central nervous system. The GI tract is a richly innervated organ, and the autonomic nervous system orchestrates many of these protective responses - seemingly in concert with other resident cell types. Common autonomic regulatory themes play an important role in maintaining intact gut defenses, and include muscarinic cholinergic and VIP signaling pathways (Table 1). These signals are directed at a multitude of effector cells including epithelia, enteroendocrine cells, enteric glia, myofibroblasts, immune cells and luminal bacteria, initiating their own protective mechanisms. Figure 2 summarizes many of the main points outlined in this review, and highlights the emerging concept that gut bacteria may by themselves constitute a novel and dynamic effector arm of enteric neurotransmission. Further work is required to define specific mechanisms that synergize or counterbalance protective signals emanating from autonomic and central nervous systems, and to delineate such responses from neurotransmission by the gut microbiome.
Table 1.
Neurotransmitter-derived regulators of gastrointestinal host defense
| Neurotransmitter Source | Gut protective mechanism targeted |
|---|---|
| Central nervous system | |
| Vagus and sacral nerves | Gut morphology and permeability, blood flow, immunomodulation and protection from acute trauma, nicotinic neuronal and enteric glial cell activation by TRPV1, substance P, CGRP, PAR-2, S-nitrosothiols. |
| Stress response | Gut motility and permeability, pH, secretion of fluid, mucus, anti-microbial Paneth and enteroendocrine peptides, cholinergic and adrenergic neuronal activation, mast cell histamine degranulation, immunomodulation, altered microbiota composition. |
| Autonomic nervous system | Gut motility, enteric glia and myofibroblast activation, mucosal proliferation and permeability, pH, secretion of fluid, mucus, anti-microbial Paneth and enteroendocrine peptides, mast cell histamine degranulation, immunomodulation, altered microbiota composition. Regulated by cholinergic and adrenergic neuronal activation; VIP, nitric oxide, opioid and cannabinoid release, and bacterial translocation of TLR agonists. |
| Enteric glia | Enteric neuronal synaptic transmission, gut motility and proliferation, mucosal and vascular permeability, regulation of colonic secretion and immunomodulation. |
| Microbiota | Sensory and extrinsic nerve activation, gut motility, pH, mucosal permeability, secretion of fluid, mucus, anti-microbial Paneth and enteroendocrine peptides by bacteria-derived histamine, GABA, catecholamines, serotonin, TLR agonists, short chain fatty acids and bile acid TGR5 agonists. |
Figure 2.
Autonomic nervous and microbial-derived neurotransmitters regulate gut barrier integrity. A number of checks and balances operate to sense and manage luminal danger signals. Details are discussed throughout the article. Abbreviations: 5-HT, serotonin; ACh, acetylcholine; CRF, corticotrophin releasing factor; EGF, epidermal growth factor; GDNF, glial cell line-derived neurotrophic factor; LPS, lipopolysaccharide; M3, M3 muscarinic receptor; SCFA, short chain fatty acids; sIgA, secretory IgA; SNO, s-nitrosothiol; TGF, transforming growth factor; TJ, tight junction; VIP, vasoactive intestinal peptide; VPAC1, VIP and pituitary adenylate cyclase-activating peptide receptor 1.
Acknowledgements
Original research from the authors’ laboratories is supported by the Canadian Institutes of Health Research (KAS) and National Institutes of Health (NIAID AI10094001 and DK56338, TCS). KAS is the recipient a Killam Annual Professorship and is the holder of the Crohn's and Colitis Foundation of Canada Chair in Inflammatory Bowel Disease Research at the University of Calgary. TCS is the Associate Director of the Texas Children’s Microbiome Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions: KAS and TCS researched and wrote the manuscript. Both authors participated in revising the manuscript and agree to the final version.
Disclosure: The authors have no conflicts of interest to disclose.
References
- Abbott NJ, Ronnback L, Hansson E. Astrocyte-endothelial interactions at the blood-brain barrier. Nat. Rev. Neurosci. 2006;7:41–53. doi: 10.1038/nrn1824. [DOI] [PubMed] [Google Scholar]
- Abdo H, Derkinderen P, Gomes P, Chevalier J, Aubert P, Masson D, Galmiche JP, Berghe Vanden P, Neunlist M, Lardeux B. Enteric glial cells protect neurons from oxidative stress in part via reduced glutathione. FASEB J. 2010;24:1082–1094. doi: 10.1096/fj.09-139519. [DOI] [PubMed] [Google Scholar]
- Abdo H, Mahe MM, Derkinderen P, Bach-Ngohou K, Neunlist M, Lardeux B. The omega-6 fatty acid derivative 15-deoxy-Delta(1)(2),(1)(4)-prostaglandin J2 is involved in neuroprotection by enteric glial cells against oxidative stress. J. Physiol. 2012;590:2739–2750. doi: 10.1113/jphysiol.2011.222935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anitha M, Vijay-Kumar M, Sitaraman SV, Gewirtz AT, Srinivasan S. Gut microbial products regulate murine gastrointestinal motility via Toll-like receptor 4 signaling. Gastroenterology. 2012;143:1006–1016. e1004. doi: 10.1053/j.gastro.2012.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asano Y, Hiramoto T, Nishino R, Aiba Y, Kimura T, Yoshihara K, Koga Y, Sudo N. Critical role of gut microbiota in the production of biologically active, free catecholamines in the gut lumen of mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2012;303:G1288–G1295. doi: 10.1152/ajpgi.00341.2012. [DOI] [PubMed] [Google Scholar]
- Axelson J, Ekelund M, Hakanson R, Sundler F. Gastrin and the vagus interact in the trophic control of the rat oxyntic mucosa. Regul. Pept. 1988;22:237–243. doi: 10.1016/0167-0115(88)90036-5. [DOI] [PubMed] [Google Scholar]
- Bach-Ngohou K, Mahe MM, Aubert P, Abdo H, Boni S, Bourreille A, Denis MG, Lardeux B, Neunlist M, Masson D. Enteric glia modulate epithelial cell proliferation and differentiation through 15-deoxy-12,14-prostaglandin J2. J. Physiol. 2010;588:2533–2544. doi: 10.1113/jphysiol.2010.188409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005;307:1915–1920. doi: 10.1126/science.1104816. [DOI] [PubMed] [Google Scholar]
- Bailey MT, Lubach GR, Coe CL. Prenatal stress alters bacterial colonization of the gut in infant monkeys. J. Pediatr. Gastroenterol. Nutr. 2004;38:414–421. doi: 10.1097/00005176-200404000-00009. [DOI] [PubMed] [Google Scholar]
- Baker SA, Hennig GW, Salter AK, Kurahashi M, Ward SM, Sanders KM. Distribution and Ca2+ signaling in fibroblast-like (PDGFRalpha+) cells in the murine gastric fundus. J. Physiol. 2013 doi: 10.1113/jphysiol.2013.264747. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangsgaard Bendtsen KM, Krych L, Sorensen DB, Pang W, Nielsen DS, Josefsen K, Hansen LH, Sorensen SJ, Hansen AK. Gut microbiota composition is correlated to grid floor induced stress and behavior in the BALB/c mouse. PLoS One. 2012;7:e46231. doi: 10.1371/journal.pone.0046231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barajon I, Serrao G, Arnaboldi F, Opizzi E, Ripamonti G, Balsari A, Rumio C. Tolllike receptors 3, 4, and 7 are expressed in the enteric nervous system and dorsal root ganglia. J. Histochem. Cytochem. 2009;57:1013–1023. doi: 10.1369/jhc.2009.953539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreau F, Cartier C, Leveque M, Ferrier L, Moriez R, Laroute V, Rosztoczy A, Fioramonti J, Bueno L. Pathways involved in gut mucosal barrier dysfunction induced in adult rats by maternal deprivation: corticotrophin-releasing factor and nerve growth factor interplay. J. Physiol. 2007;580:347–356. doi: 10.1113/jphysiol.2006.120907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett KE, Keely SJ. Chloride secretion by the intestinal epithelium: molecular basis and regulatory aspects. Annu. Rev. Physiol. 2000;62:535–572. doi: 10.1146/annurev.physiol.62.1.535. [DOI] [PubMed] [Google Scholar]
- Bassotti G, Villanacci V, Maurer CA, Fisogni S, Fabio Di F, Cadei M, Morelli A, Panagiotis T, Cathomas G, Salerni B. The role of glial cells and apoptosis of enteric neurones in the neuropathology of intractable slow transit constipation. Gut. 2006;55:41–46. doi: 10.1136/gut.2005.073197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff SC. Physiological and pathophysiological functions of intestinal mast cells. Semin. Immunopathol. 2009;31:185–205. doi: 10.1007/s00281-009-0165-4. [DOI] [PubMed] [Google Scholar]
- Bjerknes M, Cheng H. Modulation of specific intestinal epithelial progenitors by enteric neurons. Proc. Natl. Acad Sci. U S A. 2001;98:12497–12502. doi: 10.1073/pnas.211278098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackshaw LA, Brookes SJ, Grundy D, Schemann M. Sensory transmission in the gastrointestinal tract. Neurogastroenterol .Motil. 2007;19:1–19. doi: 10.1111/j.1365-2982.2006.00871.x. [DOI] [PubMed] [Google Scholar]
- Boesmans W, Martens MA, Weltens N, Hao MM, Tack J, Cirillo C, Berghe Vanden P. Imaging neuron-glia interactions in the enteric nervous system. Front. Cell Neurosci. 2013;7:183. doi: 10.3389/fncel.2013.00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudry G, Morise A, Seve B, I LEH-L. Effect of milk formula protein content on intestinal barrier function in a porcine model of LBW neonates. Pediatr. Res. 2011;69:4–9. doi: 10.1203/PDR.0b013e3181fc9d13. [DOI] [PubMed] [Google Scholar]
- Brandtzaeg P. Gate-keeper function of the intestinal epithelium. Benef. Microbes. 2013;4:67–82. doi: 10.3920/BM2012.0024. [DOI] [PubMed] [Google Scholar]
- Brun P, Giron MC, Qesari M, Porzionato A, Caputi V, Zoppellaro C, Banzato S, Grillo AR, Spagnol L, Caro De R, Pizzuti D, Barbieri V, Rosato A, Sturniolo GC, Martines D, Zaninotto G, Palu G, Castagliuolo I. Toll-Like Receptor 2 Regulates Intestinal Inflammation by Controlling Integrity of the Enteric Nervous System. Gastroenterology. 2013 doi: 10.1053/j.gastro.2013.08.047. In press. [DOI] [PubMed] [Google Scholar]
- Buhner S, Li Q, Berger T, Vignali S, Barbara G, Giorgio De R, Stanghellini V, Schemann M. Submucous rather than myenteric neurons are activated by mucosal biopsy supernatants from irritable bowel syndrome patients. Neurogastroenterol. Motil. 2012;24:1134–e1572. doi: 10.1111/nmo.12011. [DOI] [PubMed] [Google Scholar]
- Buhner S, Li Q, Vignali S, Barbara G, Giorgio De R, Stanghellini V, Cremon C, Zeller F, Langer R, Daniel H, Michel K, Schemann M. Activation of human enteric neurons by supernatants of colonic biopsy specimens from patients with irritable bowel syndrome. Gastroenterology. 2009;137:1425–1434. doi: 10.1053/j.gastro.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Buresi MC, Vergnolle N, Sharkey KA, Keenan CM, Andrade-Gordon P, Cirino G, Cirillo D, Hollenberg MD, MacNaughton WK. Activation of proteinase-activated receptor-1 inhibits neurally evoked chloride secretion in the mouse colon in vitro. Am. J. Physiol. Gastrointest. Liver Physiol. 2005;288:G337–G345. doi: 10.1152/ajpgi.00112.2004. [DOI] [PubMed] [Google Scholar]
- Cameron HL, Perdue MH. Muscarinic acetylcholine receptor activation increases transcellular transport of macromolecules across mouse and human intestinal epithelium in vitro. Neurogastroenterol. Motil. 2007;19:47–56. doi: 10.1111/j.1365-2982.2006.00845.x. [DOI] [PubMed] [Google Scholar]
- Castagliuolo I, Lamont JT, Qiu B, Fleming SM, Bhaskar KR, Nikulasson ST, Kornetsky C, Pothoulakis C. Acute stress causes mucin release from rat colon: role of corticotropin releasing factor and mast cells. Am. J. Physiol. Gastrointest. Liver Physiol. 1996;271:G884–G892. doi: 10.1152/ajpgi.1996.271.5.G884. [DOI] [PubMed] [Google Scholar]
- Cenac N, Andrews CN, Holzhausen M, Chapman K, Cottrell G, Andrade-Gordon P, Steinhoff M, Barbara G, Beck P, Bunnett NW, Sharkey KA, Ferraz JG, Shaffer E, Vergnolle N. Role for protease activity in visceral pain in irritable bowel syndrome. J. Clin. Invest. 2007;117:636–647. doi: 10.1172/JCI29255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekharan B, Bala V, Kolachala VL, Vijay-Kumar M, Jones D, Gewirtz AT, Sitaraman SV, Srinivasan S. Targeted deletion of neuropeptide Y (NPY) modulates experimental colitis. PLoS One. 2008;3:e3304. doi: 10.1371/journal.pone.0003304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekharan B, Jeppsson S, Pienkowski S, Belsham DD, Sitaraman SV, Merlin D, Kokkotou E, Nusrat A, Tansey MG, Srinivasan S. Tumor necrosis factor-neuropeptide y cross talk regulates inflammation, epithelial barrier functions, and colonic motility. Inflamm. Bowel Dis. 2013a;19:2535–2546. doi: 10.1097/01.MIB.0000437042.59208.9f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekharan B, Nezami BG, Srinivasan S. Emerging neuropeptide targets in inflammation: NPY and VIP. Am. J. Physiol. Gastrointest. Liver Physiol. 2013b;304:G949–G957. doi: 10.1152/ajpgi.00493.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Brown DR, Xie Y, Green BT, Lyte M. Catecholamines modulate Escherichia coli O157:H7 adherence to murine cecal mucosa. Shock. 2003;20:183–188. doi: 10.1097/01.shk.0000073867.66587.e0. [DOI] [PubMed] [Google Scholar]
- Chiocchetti R, Mazzuoli G, Albanese V, Mazzoni M, Clavenzani P, Lalatta-Costerbosa G, Lucchi ML, Guardo Di G, Marruchella G, Furness JB. Anatomical evidence for ileal Peyer’s patches innervation by enteric nervous system: a potential route for prion neuroinvasion? Cell Tissue Res. 2008;332:185–194. doi: 10.1007/s00441-008-0583-y. [DOI] [PubMed] [Google Scholar]
- Chu S, Schubert ML. Gastric secretion. Curr. Opin. Gastroenterol. 2013;29:636–641. doi: 10.1097/MOG.0b013e328365efc7. [DOI] [PubMed] [Google Scholar]
- Cipriani S, Mencarelli A, Chini MG, Distrutti E, Renga B, Bifulco G, Baldelli F, Donini A, Fiorucci S. The bile acid receptor GPBAR-1 (TGR5) modulates integrity of intestinal barrier and immune response to experimental colitis. PLoS One. 2011;6:e25637. doi: 10.1371/journal.pone.0025637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clevers HC, Bevins CL. Paneth cells: maestros of the small intestinal crypts. Annu. Rev. Physiol. 2013;75:289–311. doi: 10.1146/annurev-physiol-030212-183744. [DOI] [PubMed] [Google Scholar]
- Cogan TA, Thomas AO, Rees LE, Taylor AH, Jepson MA, Williams PH, Ketley J, Humphrey TJ. Norepinephrine increases the pathogenic potential of Campylobacter jejuni. Gut. 2007;56:1060–1065. doi: 10.1136/gut.2006.114926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat. Rev. Microbiol. 2012;10:735–742. doi: 10.1038/nrmicro2876. [DOI] [PubMed] [Google Scholar]
- Conlin VS, Wu X, Nguyen C, Dai C, Vallance BA, Buchan AM, Boyer L, Jacobson K. Vasoactive intestinal peptide ameliorates intestinal barrier disruption associated with Citrobacter rodentium-induced colitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2009;297:G735–G750. doi: 10.1152/ajpgi.90551.2008. [DOI] [PubMed] [Google Scholar]
- Costantini TW, Bansal V, Krzyzaniak M, Putnam JG, Peterson CY, Loomis WH, Wolf P, Baird A, Eliceiri BP, Coimbra R. Vagal nerve stimulation protects against burn-induced intestinal injury through activation of enteric glia cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2010;299:G1308–G1318. doi: 10.1152/ajpgi.00156.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini TW, Krzyzaniak M, Cheadle GA, Putnam JG, Hageny AM, Lopez N, Eliceiri BP, Bansal V, Coimbra R. Targeting alpha-7 nicotinic acetylcholine receptor in the enteric nervous system: a cholinergic agonist prevents gut barrier failure after severe burn injury. Am. J. Pathol. 2012;181:478–486. doi: 10.1016/j.ajpath.2012.04.005. [DOI] [PubMed] [Google Scholar]
- Costes LM, Boeckxstaens GE, Jonge de WJ, Cailotto C. Neural networks in intestinal immunoregulation. Organogenesis. 2013;9 doi: 10.4161/org.25646. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crivellato E, Soldano F, Travan L. A light and electron microscopic quantitative analysis of nerve-immune cell contacts in the gut-associated lymphoid tissue of the mouse colon. J. Submicrosc. Cytol. Pathol. 2002;34:55–66. [PubMed] [Google Scholar]
- Crivellato E, Soldano F, Travan L, Fusaroli P, Mallardi F. Apposition of enteric nerve fibers to plasma cells and immunoblasts in the mouse small bowel. Neurosci. Lett. 1998;241:123–126. doi: 10.1016/s0304-3940(98)00004-4. [DOI] [PubMed] [Google Scholar]
- de Jonge WJ. Mast cells in intestinal inflammation, barrier function, and postoperative motility. J. Pediatr. Gastroenterol. Nutr. 2011;53(Suppl 2):S56–S57. [PubMed] [Google Scholar]
- de Jonge WJ. The Gut’s Little Brain in Control of Intestinal Immunity. ISRN Gastroenterol. 2013;2013:630159. doi: 10.1155/2013/630159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deloose E, Janssen P, Depoortere I, Tack J. The migrating motor complex: control mechanisms and its role in health and disease. Nat. Rev. Gastroenterol. Hepatol. 2012;9:271–285. doi: 10.1038/nrgastro.2012.57. [DOI] [PubMed] [Google Scholar]
- Devkota S, Chang EB. Nutrition, microbiomes, and intestinal inflammation. Curr. Opin. Gastroenterol. 2013;29:603–607. doi: 10.1097/MOG.0b013e328365d38f. [DOI] [PubMed] [Google Scholar]
- Dhawan S, Cailotto C, Harthoorn LF, Jonge de WJ. Cholinergic signalling in gut immunity. Life Sci. 2012;91:1038–1042. doi: 10.1016/j.lfs.2012.04.042. [DOI] [PubMed] [Google Scholar]
- Dinan TG, Cryan JF. Regulation of the stress response by the gut microbiota: implications for psychoneuroendocrinology. Psychoneuroendocrinology. 2012;37:1369–1378. doi: 10.1016/j.psyneuen.2012.03.007. [DOI] [PubMed] [Google Scholar]
- Engel MA, Becker C, Reeh PW, Neurath MF. Role of sensory neurons in colitis: increasing evidence for a neuroimmune link in the gut. Inflamm. Bowel Dis. 2011;17:1030–1033. doi: 10.1002/ibd.21422. [DOI] [PubMed] [Google Scholar]
- Esposito G, Capoccia E, Turco F, Palumbo I, Lu J, Steardo A, Cuomo R, Sarnelli G, Steardo L. Palmitoylethanolamide improves colon inflammation through an enteric glia/toll like receptor 4-dependent PPAR-alpha activation. Gut. 2013 doi: 10.1136/gutjnl-2013-305005. In press. [DOI] [PubMed] [Google Scholar]
- Fasano A. Zonulin, regulation of tight junctions, and autoimmune diseases. Ann. NY Acad. Sci. 2012;1258:25–33. doi: 10.1111/j.1749-6632.2012.06538.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasano A, Shea-Donohue T. Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nat. Clin. Pract. Gastroenterol. Hepatol. 2005;2:416–422. doi: 10.1038/ncpgasthep0259. [DOI] [PubMed] [Google Scholar]
- Felten SY, Felten DL, Bellinger DL, Olschowka JA. Noradrenergic and peptidergic innervation of lymphoid organs. Chem. Immunol. 1992;52:25–48. [PubMed] [Google Scholar]
- Fihn BM, Sjoqvist A, Jodal M. Involvement of enteric nerves in permeability changes due to deoxycholic acid in rat jejunum in vivo. Acta Physiol. Scand. 2003;178:241–250. doi: 10.1046/j.1365-201X.2003.01144.x. [DOI] [PubMed] [Google Scholar]
- Flamant M, Aubert P, Rolli-Derkinderen M, Bourreille A, Neunlist MR, Mahe MM, Meurette G, Marteyn B, Savidge T, Galmiche JP, Sansonetti PJ, Neunlist M. Enteric glia protect against Shigella flexneri invasion in intestinal epithelial cells: a role for S-nitrosoglutathione. Gut. 2011;60:473–484. doi: 10.1136/gut.2010.229237. [DOI] [PubMed] [Google Scholar]
- Forsythe P, Kunze WA, Bienenstock J. On communication between gut microbes and the brain. Curr. Opin. Gastroenterol. 2012;28:557–562. doi: 10.1097/MOG.0b013e3283572ffa. [DOI] [PubMed] [Google Scholar]
- Freestone PP, Sandrini SM, Haigh RD, Lyte M. Microbial endocrinology: how stress influences susceptibility to infection. Trends Microbiol. 2008;16:55–64. doi: 10.1016/j.tim.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Furness JB. Malden, Mass.: The enteric nervous system Blackwell Pub.; 2006. pp. xiii–274. [Google Scholar]
- Furness JB. The enteric nervous system and neurogastroenterology. Nat. Rev. Gastroenterol. Hepatol. 2012;9:286–294. doi: 10.1038/nrgastro.2012.32. [DOI] [PubMed] [Google Scholar]
- Furness JB, Kunze WA, Bertrand PP, Clerc N, Bornstein JC. Intrinsic primary afferent neurons of the intestine. Prog. Neurobiol. 1998;54:1–18. doi: 10.1016/s0301-0082(97)00051-8. [DOI] [PubMed] [Google Scholar]
- Furness JB, Rivera LR, Cho HJ, Bravo DM, Callaghan B. The gut as a sensory organ. Nat. Rev. Gastroenterol. Hepatol. 2013 doi: 10.1038/nrgastro.2013.180. In Press. [DOI] [PubMed] [Google Scholar]
- Gareau MG, Jury J, Perdue MH. Neonatal maternal separation of rat pups results in abnormal cholinergic regulation of epithelial permeability. Am. J. Physiol. Gastrointest. Liver Physiol. 2007;293:G198–G203. doi: 10.1152/ajpgi.00392.2006. [DOI] [PubMed] [Google Scholar]
- Gautron L, Rutkowski JM, Burton MD, Wei W, Wan Y, Elmquist JK. Neuronal and nonneuronal cholinergic structures in the mouse gastrointestinal tract and spleen. J. Comp. Neurol. 2013;521:3741–3767. doi: 10.1002/cne.23376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon MD. 5-Hydroxytryptamine (serotonin) in the gastrointestinal tract. Curr. Opin. Endocrinol. Diabetes Obes. 2013;20:14–21. doi: 10.1097/MED.0b013e32835bc703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geurts L, Neyrinck AM, Delzenne NM, Knauf C, Cani PD. Gut microbiota controls adipose tissue expansion, gut barrier and glucose metabolism: novel insights into molecular targets and interventions using prebiotics. Benef. Microbes. 2013 doi: 10.3920/BM2012.0065. In press. [DOI] [PubMed] [Google Scholar]
- Gomes P, Chevalier J, Boesmans W, Roosen L, Abbeel van den V, Neunlist M, Tack J, Berghe Vanden P. ATP-dependent paracrine communication between enteric neurons and glia in a primary cell culture derived from embryonic mice. Neurogastroenterol. Motil. 2009;21:870–e862. doi: 10.1111/j.1365-2982.2009.01302.x. [DOI] [PubMed] [Google Scholar]
- Gougeon PY, Lourenssen S, Han TY, Nair DG, Ropeleski MJ, Blennerhassett MG. The pro-inflammatory cytokines IL-1beta and TNFalpha are neurotrophic for enteric neurons. J. Neurosci. 2013;33:3339–3351. doi: 10.1523/JNEUROSCI.3564-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BT, Bunnett NW, Kulkarni-Narla A, Steinhoff M, Brown DR. Intestinal type 2 proteinase-activated receptors: expression in opioid-sensitive secretomotor neural circuits that mediate epithelial ion transport. J. Pharmacol. Exp. Ther. 2000;295:410–416. [PubMed] [Google Scholar]
- Green BT, Lyte M, Kulkarni-Narla A, Brown DR. Neuromodulation of enteropathogen internalization in Peyer’s patches from porcine jejunum. J. Neuroimmunol. 2003;141:74–82. doi: 10.1016/s0165-5728(03)00225-x. [DOI] [PubMed] [Google Scholar]
- Greenwood B, Mantle M. Mucin and protein release in the rabbit jejunum: effects of bethanechol and vagal nerve stimulation. Gastroenterology. 1992;103:496–505. doi: 10.1016/0016-5085(92)90839-q. [DOI] [PubMed] [Google Scholar]
- Gross ER, Gershon MD, Margolis KG, Gertsberg ZV, Li Z, Cowles RA. Neuronal serotonin regulates growth of the intestinal mucosa in mice. Gastroenterology. 2012;143:408–417. e402. doi: 10.1053/j.gastro.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross KJ, Pothoulakis C. Role of neuropeptides in inflammatory bowel disease. Inflamm. Bowel Dis. 2007;13:918–932. doi: 10.1002/ibd.20129. [DOI] [PubMed] [Google Scholar]
- Gulbransen BD, Bains JS, Sharkey KA. Enteric glia are targets of the sympathetic innervation of the myenteric plexus in the guinea pig distal colon. J. Neurosci. 2010;30:6801–6809. doi: 10.1523/JNEUROSCI.0603-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulbransen BD, Bashashati M, Hirota SA, Gui X, Roberts JA, MacDonald JA, Muruve DA, McKay DM, Beck PL, Mawe GM, Thompson RJ, Sharkey KA. Activation of neuronal P2X7 receptor-pannexin-1 mediates death of enteric neurons during colitis. Nat. Med. 2012;18:600–604. doi: 10.1038/nm.2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulbransen BD, Sharkey KA. Purinergic neuron-to-glia signaling in the enteric nervous system. Gastroenterology. 2009;136:1349–1358. doi: 10.1053/j.gastro.2008.12.058. [DOI] [PubMed] [Google Scholar]
- Gulbransen BD, Sharkey KA. Novel functional roles for enteric glia in the gastrointestinal tract. Nat. Rev. Gastroenterol. Hepatol. 2012;9:625–632. doi: 10.1038/nrgastro.2012.138. [DOI] [PubMed] [Google Scholar]
- Hadzijahic N, Renehan WE, Ma CK, Zhang X, Fogel R. Myenteric plexus destruction alters morphology of rat intestine. Gastroenterology. 1993;105:1017–1028. doi: 10.1016/0016-5085(93)90944-8. [DOI] [PubMed] [Google Scholar]
- Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Therap. Adv. Gastroenterol. 2013;6:39–51. doi: 10.1177/1756283X12459294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman JM, Tyler K, MacEachern SJ, Balemba OB, Johnson AC, Brooks EM, Zhao H, Swain GM, Moses PL, Galligan JJ, Sharkey KA, Meerveld Greenwood-Van B, Mawe GM. Activation of colonic mucosal 5-HT(4) receptors accelerates propulsive motility and inhibits visceral hypersensitivity. Gastroenterology. 2012;142:844–854. e844. doi: 10.1053/j.gastro.2011.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann P, Mazurkiewicz J, Holtmann G, Gerken G, Eysselein VE, Goebell H. Capsaicin-sensitive nerve fibres induce epithelial cell proliferation, inflammatory cell immigration and transforming growth factor-alpha expression in the rat colonic mucosa in vivo. Scand. J. Gastroenterol. 2002;37:414–422. doi: 10.1080/003655202317316042. [DOI] [PubMed] [Google Scholar]
- Holle GE. Changes in the structure and regeneration mode of the rat small intestinal mucosa following benzalkonium chloride treatment. Gastroenterology. 1991;101:1264–1273. doi: 10.1016/0016-5085(91)90076-w. [DOI] [PubMed] [Google Scholar]
- Holle GE, Dietl J, Demir I. Influence of the intramural innervation on the morphogenesis of the enteroendocrine cells and the genetic construct involved. Int. J. Mol. Med. 2003;11:275–285. doi: 10.3892/ijmm.11.3.275. [DOI] [PubMed] [Google Scholar]
- Holzer P. Gastroduodenal mucosal defense. Curr. Opin. Gastroenterol. 2000a;16:469–478. doi: 10.1097/00001574-200011000-00003. [DOI] [PubMed] [Google Scholar]
- Holzer P. Local microcirculatory reflexes and afferent signalling in response to gastric acid challenge. Gut. 2000b;47(Suppl 4):iv46–iv48. doi: 10.1136/gut.47.suppl_4.iv46. discussion iv52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzer P. Role of visceral afferent neurons in mucosal inflammation and defense. Curr. Opin. Pharmacol. 2007;7:563–569. doi: 10.1016/j.coph.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes DT, Clarke MB, Yamamoto K, Rasko DA, Sperandio V. The QseC adrenergic signaling cascade in Enterohemorrhagic E. coli (EHEC) PLoS Pathog. 2009;5:e1000553. doi: 10.1371/journal.ppat.1000553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes PA, Harrington AM, Castro J, Liebregts T, Adam B, Grasby DJ, Isaacs NJ, Maldeniya L, Martin CM, Persson J, Andrews JM, Holtmann G, Blackshaw LA, Brierley SM. Sensory neuro-immune interactions differ between Irritable Bowel Syndrome subtypes. Gut. 2013;62:1456–1465. doi: 10.1136/gutjnl-2011-301856. [DOI] [PubMed] [Google Scholar]
- Ikehara O, Hayashi H, Waguri T, Kaji I, Karaki S, Kuwahara A, Suzuki Y. Subepithelial trypsin induces enteric nerve-mediated anion secretion by activating proteinase-activated receptor 1 in the mouse cecum. J. Physiol. Sci. 2012;62:211–219. doi: 10.1007/s12576-012-0198-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikehara O, Hayashi H, Watanabe Y, Yamamoto H, Mochizuki T, Hoshino M, Suzuki Y. Proteinase-activated receptors-1 and 2 induce electrogenic Cl- secretion in the mouse cecum by distinct mechanisms. Am. J Physiol. Gastrointest. Liver Physiol. 2010;299:G115–G125. doi: 10.1152/ajpgi.00281.2009. [DOI] [PubMed] [Google Scholar]
- Izzo AA, Sharkey KA. Cannabinoids and the gut: new developments and emerging concepts. Pharmacol. Ther. 2010;126:21–38. doi: 10.1016/j.pharmthera.2009.12.005. [DOI] [PubMed] [Google Scholar]
- Janig W, Morrison JF. Functional properties of spinal visceral afferents supplying abdominal and pelvic organs, with special emphasis on visceral nociception. Prog. Brain Res. 1986;67:87–114. doi: 10.1016/s0079-6123(08)62758-2. [DOI] [PubMed] [Google Scholar]
- Jonsson M, Norrgard O, Forsgren S. Presence of a marked nonneuronal cholinergic system in human colon: study of normal colon and colon in ulcerative colitis. Inflamm. Bowel Dis. 2007;13:1347–1356. doi: 10.1002/ibd.20224. [DOI] [PubMed] [Google Scholar]
- Kamiya T, Wang L, Forsythe P, Goettsche G, Mao Y, Wang Y, Tougas G, Bienenstock J. Inhibitory effects of Lactobacillus reuteri on visceral pain induced by colorectal distension in Sprague-Dawley rats. Gut. 2006;55:191–196. doi: 10.1136/gut.2005.070987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karavolos MH, Winzer K, Williams P, Khan CM. Pathogen espionage: multiple bacterial adrenergic sensors eavesdrop on host communication systems. Mol. Microbiol. 2013;87:455–465. doi: 10.1111/mmi.12110. [DOI] [PubMed] [Google Scholar]
- Keely S, Kelly CJ, Weissmueller T, Burgess A, Wagner BD, Robertson CE, Harris JK, Colgan SP. Activated fluid transport regulates bacterial-epithelial interactions and significantly shifts the murine colonic microbiome. Gut Microbes. 2012;3:250–260. doi: 10.4161/gmic.20529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keita AV, Carlsson AH, Cigehn M, Ericson AC, McKay DM, Soderholm JD. Vasoactive intestinal polypeptide regulates barrier function via mast cells in human intestinal follicle-associated epithelium and during stress in rats. Neurogastroenterol. Motil. 2013;25:e406–e417. doi: 10.1111/nmo.12127. [DOI] [PubMed] [Google Scholar]
- Keita AV, Soderholm JD. The intestinal barrier and its regulation by neuroimmune factors. Neurogastroenterol. Motil. 2010;22:718–733. doi: 10.1111/j.1365-2982.2010.01498.x. [DOI] [PubMed] [Google Scholar]
- Klapproth H, Reinheimer T, Metzen J, Munch M, Bittinger F, Kirkpatrick CJ, Hohle KD, Schemann M, Racke K, Wessler I. Non-neuronal acetylcholine, a signalling molecule synthezised by surface cells of rat and man. Naunyn Schmiedebergs Arch. Pharmacol. 1997;355:515–523. doi: 10.1007/pl00004977. [DOI] [PubMed] [Google Scholar]
- Knights D, Lassen KG, Xavier RJ. Advances in inflammatory bowel disease pathogenesis: linking host genetics and the microbiome. Gut. 2013;62:1505–1510. doi: 10.1136/gutjnl-2012-303954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krzyzaniak M, Peterson C, Loomis W, Hageny AM, Wolf P, Reys L, Putnam J, Eliceiri B, Baird A, Bansal V, Coimbra R. Postinjury vagal nerve stimulation protects against intestinal epithelial barrier breakdown. J. Trauma. 2011;70:1168–1175. doi: 10.1097/TA.0b013e318216f754. discussion 1175–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kugler EM, Mazzuoli G, Demir IE, Ceyhan GO, Zeller F, Schemann M. Activity of protease-activated receptors in primary cultured human myenteric neurons. Front. Neurosci. 2012;6:133. doi: 10.3389/fnins.2012.00133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunze WA, Mao YK, Wang B, Huizinga JD, Ma X, Forsythe P, Bienenstock J. Lactobacillus reuteri enhances excitability of colonic AH neurons by inhibiting calcium-dependent potassium channel opening. J. Cell Mol. Med. 2009;13:2261–2270. doi: 10.1111/j.1582-4934.2009.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurahashi M, Zheng H, Dwyer L, Ward SM, Koh Don S, Sanders KM. A functional role for the ‘fibroblast-like cells’ in gastrointestinal smooth muscles. J. Physiol. 2011;589:697–710. doi: 10.1113/jphysiol.2010.201129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laukoetter MG, Bruewer M, Nusrat A. Regulation of the intestinal epithelial barrier by the apical junctional complex. Curr. Opin. Gastroenterol. 2006;22:85–89. doi: 10.1097/01.mog.0000203864.48255.4f. [DOI] [PubMed] [Google Scholar]
- Lawson VA, Furness JB, Klemm HM, Pontell L, Chan E, Hill AF, Chiocchetti R. The brain to gut pathway: a possible route of prion transmission. Gut. 2010;59:1643–1651. doi: 10.1136/gut.2010.222620. [DOI] [PubMed] [Google Scholar]
- Lin HC, Pimentel M. Bacterial concepts in irritable bowel syndrome. Rev. Gastroenterol. Disord. 2005;5(Suppl. 3):S3–S9. [PubMed] [Google Scholar]
- Lomax AE, Sharkey KA, Furness JB. The participation of the sympathetic innervation of the gastrointestinal tract in disease states. Neurogastroenterol. Motil. 2010;22:7–18. doi: 10.1111/j.1365-2982.2009.01381.x. [DOI] [PubMed] [Google Scholar]
- Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R. Diversity, stability and resilience of the human gut microbiota. Nature. 2012;489:220–230. doi: 10.1038/nature11550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundgren O, Jodal M, Jansson M, Ryberg AT, Svensson L. Intestinal epithelial stem/progenitor cells are controlled by mucosal afferent nerves. PLoS One. 2011;6:e16295. doi: 10.1371/journal.pone.0016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyte M, Vulchanova L, Brown DR. Stress at the intestinal surface: catecholamines and mucosa-bacteria interactions. Cell Tissue Res. 2011;343:23–32. doi: 10.1007/s00441-010-1050-0. [DOI] [PubMed] [Google Scholar]
- Ma X, Mao YK, Wang B, Huizinga JD, Bienenstock J, Kunze W. Lactobacillus reuteri ingestion prevents hyperexcitability of colonic DRG neurons induced by noxious stimuli. Am. J. Physiol. Gastrointest. Liver Physiol. 2009;296:G868–G875. doi: 10.1152/ajpgi.90511.2008. [DOI] [PubMed] [Google Scholar]
- MacEachern SJ, Patel BA, McKay DM, Sharkey KA. Nitric oxide regulation ofcolonic epithelial ion transport: a novel role for enteric glia in the myenteric plexus. J. Physiol. 2011;589:3333–3348. doi: 10.1113/jphysiol.2011.207902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macia L, Thorburn AN, Binge LC, Marino E, Rogers KE, Maslowski KM, Vieira AT, Kranich J, Mackay CR. Microbial influences on epithelial integrity and immune function as a basis for inflammatory diseases. Immunol. Rev. 2012;245:164–176. doi: 10.1111/j.1600-065X.2011.01080.x. [DOI] [PubMed] [Google Scholar]
- Mao YK, Kasper DL, Wang B, Forsythe P, Bienenstock J, Kunze WA. Bacteroides fragilis polysaccharide A is necessary and sufficient for acute activation of intestinal sensory neurons. Nat. Commun. 2013;4:1465. doi: 10.1038/ncomms2478. [DOI] [PubMed] [Google Scholar]
- Margolis KG, Gershon MD. Neuropeptides and inflammatory bowel disease. Curr. Opin. Gastroenterol. 2009;25:503–511. doi: 10.1097/MOG.0b013e328331b69e. [DOI] [PubMed] [Google Scholar]
- Matteoli G, Gomez-Pinilla PJ, Nemethova A, Giovangiulio Di M, Cailotto C, Bree van SH, Michel K, Tracey KJ, Schemann M, Boesmans W, Berghe Vanden P, Boeckxstaens GE. A distinct vagal anti-inflammatory pathway modulates intestinal muscularis resident macrophages independent of the spleen. Gut. 2013 doi: 10.1136/gutjnl-2013-304676. In Press. [DOI] [PubMed] [Google Scholar]
- McCole DF, Barrett KE. Varied role of the gut epithelium in mucosal homeostasis. Curr. Opin. Gastroenterol. 2007;23:647–654. doi: 10.1097/MOG.0b013e3282f0153b. [DOI] [PubMed] [Google Scholar]
- McGuckin MA, Linden SK, Sutton P, Florin TH. Mucin dynamics and enteric pathogens. Nat. Rev. Microbiol. 2011;9:265–278. doi: 10.1038/nrmicro2538. [DOI] [PubMed] [Google Scholar]
- McVey Neufeld KA, Mao YK, Bienenstock J, Foster JA, Kunze WA. The microbiome is essential for normal gut intrinsic primary afferent neuron excitability in the mouse. Neurogastroenterol. Motil. 2013;25:183–e188. doi: 10.1111/nmo.12049. [DOI] [PubMed] [Google Scholar]
- Meurette G, Blanchard C, Duchalais-Dassonneville E, Coquenlorge S, Aubert P, Wong M, Lehur PA, Neunlist M. Sacral nerve stimulation enhances epithelial barrier of the rectum: results from a porcine model. Neurogastroenterol. Motil. 2012;24:267–273. e110. doi: 10.1111/j.1365-2982.2011.01839.x. [DOI] [PubMed] [Google Scholar]
- Miampamba M, Maillot C, Million M, Tache Y. Peripheral CRF activates myenteric neurons in the proximal colon through CRF(1) receptor in conscious rats. Am. J. Physiol. Gastrointest. Liver Physiol. 2002;282:G857–G865. doi: 10.1152/ajpgi.00434.2001. [DOI] [PubMed] [Google Scholar]
- Moore BA, Kim D, Vanner S. Neural pathways regulating Brunner’s gland secretion in guinea pig duodenum in vitro. Am. J. Physiol. Gastrointest. Liver Physiol. 2000;279:G910–G917. doi: 10.1152/ajpgi.2000.279.5.G910. [DOI] [PubMed] [Google Scholar]
- Moore BA, Sharkey KA, Mantle M. Neural mediation of cholera toxin-induced mucin secretion in the rat small intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 1993;265:G1050–G1056. doi: 10.1152/ajpgi.1993.265.6.G1050. [DOI] [PubMed] [Google Scholar]
- Moore BA, Sharkey KA, Mantle M. Role of 5-HT in cholera toxin-induced mucin secretion in the rat small intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 1996;270:G1001–G1009. doi: 10.1152/ajpgi.1996.270.6.G1001. [DOI] [PubMed] [Google Scholar]
- Moro F, Levenez F, Durual S, Plaisancie P, Thim L, Giraud AS, Cuber JC. Secretion of the trefoil factor TFF3 from the isolated vascularly perfused rat colon. Regul. Pept. 2001;101:35–41. doi: 10.1016/s0167-0115(01)00257-9. [DOI] [PubMed] [Google Scholar]
- Mueller K, Michel K, Krueger D, Demir IE, Ceyhan GO, Zeller F, Kreis ME, Schemann M. Activity of protease-activated receptors in the human submucous plexus. Gastroenterology. 2011;141:2088–2097. e2081. doi: 10.1053/j.gastro.2011.08.034. [DOI] [PubMed] [Google Scholar]
- Murakami M, Ohta T, Ito S. Lipopolysaccharides enhance the action of bradykinin in enteric neurons via secretion of interleukin-1beta from enteric glial cells. J. Neurosci. Res. 2009;87:2095–2104. doi: 10.1002/jnr.22036. [DOI] [PubMed] [Google Scholar]
- Natividad JM, Verdu EF. Modulation of intestinal barrier by intestinal microbiota: pathological and therapeutic implications. Pharmacol. Res. 2013;69:42–51. doi: 10.1016/j.phrs.2012.10.007. [DOI] [PubMed] [Google Scholar]
- Neunlist M, Aubert P, Bonnaud S, Landeghem Van L, Coron E, Wedel T, Naveilhan P, Ruhl A, Lardeux B, Savidge T, Paris F, Galmiche JP. Enteric glia inhibit intestinal epithelial cell proliferation partly through a TGF-beta1-dependent pathway. Am. J. Physiol. Gastrointest. Liver Physiol. 2007;292:G231–G241. doi: 10.1152/ajpgi.00276.2005. [DOI] [PubMed] [Google Scholar]
- Neunlist M, Toumi F, Oreschkova T, Denis M, Leborgne J, Laboisse CL, Galmiche JP, Jarry A. Human ENS regulates the intestinal epithelial barrier permeability and a tight junction-associated protein ZO-1 via VIPergic pathways. Am. J. Physiol. Gastrointest. Liver Physiol. 2003;285:G1028–G1036. doi: 10.1152/ajpgi.00066.2003. [DOI] [PubMed] [Google Scholar]
- Neunlist M, Landeghem Van L, Mahe MM, Derkinderen P, Varannes des SB, Rolli-Derkinderen M. The digestive neuronal-glial-epithelial unit: a new actor in gut health and disease. Nat. Rev. Gastroenterol. Hepatol. 2013;10:90–100. doi: 10.1038/nrgastro.2012.221. [DOI] [PubMed] [Google Scholar]
- Nguyen C, Coelho AM, Grady E, Compton SJ, Wallace JL, Hollenberg MD, Cenac N, Garcia-Villar R, Bueno L, Steinhoff M, Bunnett NW, Vergnolle N. Colitis induced by proteinase-activated receptor-2 agonists is mediated by a neurogenic mechanism. Can. J. Physiol. Pharmacol. 2003;81:920–927. doi: 10.1139/y03-080. [DOI] [PubMed] [Google Scholar]
- Nijhuis LE, Olivier BJ, Jonge de WJ. Neurogenic regulation of dendritic cells in the intestine. Biochem. Pharmacol. 2010;80:2002–2008. doi: 10.1016/j.bcp.2010.06.034. [DOI] [PubMed] [Google Scholar]
- O’Malley D, Quigley EM, Dinan TG, Cryan JF. Do interactions between stress and immune responses lead to symptom exacerbations in irritable bowel syndrome? Brain Behav. Immun. 2011;25:1333–1341. doi: 10.1016/j.bbi.2011.04.009. [DOI] [PubMed] [Google Scholar]
- Ochoa-Cortes F, Ramos-Lomas T, Miranda-Morales M, Spreadbury I, Ibeakanma C, Barajas-Lopez C, Vanner S. Bacterial cell products signal to mouse colonic nociceptive dorsal root ganglia neurons. Am. J. Physiol. Gastrointest. Liver Physiol. 2010;299:G723–G732. doi: 10.1152/ajpgi.00494.2009. [DOI] [PubMed] [Google Scholar]
- Ogata H, Podolsky DK. Trefoil peptide expression and secretion is regulated by neuropeptides and acetylcholine. Am. J. Physiol. Gastrointest. Liver Physiol. 1997;273:G348–G354. doi: 10.1152/ajpgi.1997.273.2.G348. [DOI] [PubMed] [Google Scholar]
- Ohman L, Simren M. Intestinal microbiota and its role in irritable bowel syndrome (IBS) Curr. Gastroenterol. Rep. 2013;15:323. doi: 10.1007/s11894-013-0323-7. [DOI] [PubMed] [Google Scholar]
- Ouellette AJ. Paneth cell alpha-defensins in enteric innate immunity. Cell Mol. Life Sci. 2011;68:2215–2229. doi: 10.1007/s00018-011-0714-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overman EL, Rivier JE, Moeser AJ. CRF induces intestinal epithelial barrier injury via the release of mast cell proteases and TNF-alpha. PLoS One. 2012;7:e39935. doi: 10.1371/journal.pone.0039935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacheco AR, Sperandio V. Inter-kingdom signaling: chemical language between bacteria and host. Curr. Opin. Microbiol. 2009;12:192–198. doi: 10.1016/j.mib.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peniche AG, Savidge TC, Dann SM. Recent insights into Clostridium difficile pathogenesis. Curr. Opin. Infect. Dis. 2013;26:447–453. doi: 10.1097/01.qco.0000433318.82618.c6. [DOI] [PubMed] [Google Scholar]
- Perez-Burgos A, Wang B, Mao YK, Mistry B, Neufeld McVey KA, Bienenstock J, Kunze W. Psychoactive bacteria Lactobacillus rhamnosus (JB-1) elicits rapid frequency facilitation in vagal afferents. Am. J. Physiol. Gastrointest. Liver Physiol. 2013;304:G211–G220. doi: 10.1152/ajpgi.00128.2012. [DOI] [PubMed] [Google Scholar]
- Powell DW, Mifflin RC, Valentich JD, Crowe SE, Saada JI, West AB. Myofibroblasts. II. Intestinal subepithelial myofibroblasts. Am. J. Physiol. Cell Physiol. 1999;277:C183–C201. doi: 10.1152/ajpcell.1999.277.2.C183. [DOI] [PubMed] [Google Scholar]
- Powley TL, Phillips RJ. Vagal intramuscular array afferents form complexes with interstitial cells of Cajal in gastrointestinal smooth muscle: analogues of muscle spindle organs? Neuroscience. 2011;186:188–200. doi: 10.1016/j.neuroscience.2011.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat. Rev. Gastroenterol. Hepatol. 2009;6:306–314. doi: 10.1038/nrgastro.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, Griffin NW, Lombard V, Henrissat B, Bain JR, Muehlbauer MJ, Ilkayeva O, Semenkovich CF, Funai K, Hayashi DK, Lyle BJ, Martini MC, Ursell LK, Clemente JC, Treuren Van W, Walters WA, Knight R, Newgard CB, Heath AC, Gordon JI. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science. 2013;341:1241214. doi: 10.1126/science.1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubino SJ, Selvanantham T, Girardin SE, Philpott DJ. Nod-like receptors in the control of intestinal inflammation. Curr. Opin. Immunol. 2012;24:398–404. doi: 10.1016/j.coi.2012.04.010. [DOI] [PubMed] [Google Scholar]
- Ruhl A, Franzke S, Collins SM, Stremmel W. Interleukin-6 expression and regulation in rat enteric glial cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2001a;280:G1163–G1171. doi: 10.1152/ajpgi.2001.280.6.G1163. [DOI] [PubMed] [Google Scholar]
- Ruhl A, Franzke S, Stremmel W. IL-1beta and IL-10 have dual effects on enteric glial cell proliferation. Neurogastroenterol. Motil. 2001b;13:89–94. doi: 10.1046/j.1365-2982.2001.00245.x. [DOI] [PubMed] [Google Scholar]
- Rumio C, Besusso D, Arnaboldi F, Palazzo M, Selleri S, Gariboldi S, Akira S, Uematsu S, Bignami P, Ceriani V, Menard S, Balsari A. Activation of smooth muscle and myenteric plexus cells of jejunum via Toll-like receptor 4. J. Cell Physiol. 2006;208:47–54. doi: 10.1002/jcp.20632. [DOI] [PubMed] [Google Scholar]
- Salzman NH. Paneth cell defensins and the regulation of the microbiome: detente at mucosal surfaces. Gut Microbes. 2010;1:401–406. doi: 10.4161/gmic.1.6.14076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders KM, Hwang SJ, Ward SM. Neuroeffector apparatus in gastrointestinal smooth muscle organs. J. Physiol. 2010;588:4621–4639. doi: 10.1113/jphysiol.2010.196030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos J, Saperas E, Nogueiras C, Mourelle M, Antolin M, Cadahia A, Malagelada JR. Release of mast cell mediators into the jejunum by cold pain stress in humans. Gastroenterology. 1998;114:640–648. doi: 10.1016/s0016-5085(98)70577-3. [DOI] [PubMed] [Google Scholar]
- Santos J, Saunders PR, Hanssen NP, Yang PC, Yates D, Groot JA, Perdue MH. Corticotropin-releasing hormone mimics stress-induced colonic epithelial pathophysiology in the rat. Am. J Physiol. Gastrointest. Liver Physiol. 1999;277:G391–G399. doi: 10.1152/ajpgi.1999.277.2.G391. [DOI] [PubMed] [Google Scholar]
- Saunders PR, Hanssen NP, Perdue MH. Cholinergic nerves mediate stress-induced intestinal transport abnormalities in Wistar-Kyoto rats. Am. J. Physiol. Gastrointest. Liver Physiol. 1997;273:G486–490. doi: 10.1152/ajpgi.1997.273.2.G486. [DOI] [PubMed] [Google Scholar]
- Savidge TC. S-nitrosothiol signals in the enteric nervous system: lessons learnt from big brother. Front Neurosci. 2011;5:31. doi: 10.3389/fnins.2011.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savidge TC, Newman P, Pothoulakis C, Ruhl A, Neunlist M, Bourreille A, Hurst R, Sofroniew MV. Enteric glia regulate intestinal barrier function and inflammation via release of S-nitrosoglutathione. Gastroenterology. 2007;132:1344–1358. doi: 10.1053/j.gastro.2007.01.051. [DOI] [PubMed] [Google Scholar]
- Schaper J, Wagner A, Enigk F, Brell B, Mousa SA, Habazettl H, Schafer M. Regional sympathetic blockade attenuates activation of intestinal macrophages and reduces gut barrier failure. Anesthesiology. 2013;118:134–142. doi: 10.1097/ALN.0b013e3182784c93. [DOI] [PubMed] [Google Scholar]
- Schicho R, Schemann M, Pabst MA, Holzer P, Lippe IT. Capsaicin-sensitive extrinsic afferents are involved in acid-induced activation of distinct myenteric neurons in the rat stomach. Neurogastroenterol. Motil. 2003;15:33–44. doi: 10.1046/j.1365-2982.2003.00384.x. [DOI] [PubMed] [Google Scholar]
- Schmidt LD, Xie Y, Lyte M, Vulchanova L, Brown DR. Autonomic neurotransmitters modulate immunoglobulin A secretion in porcine colonic mucosa. J. Neuroimmunol. 2007;185:20–28. doi: 10.1016/j.jneuroim.2006.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt PT, Eriksen L, Loftager M, Rasmussen TN, Holst JJ. Fast acting nervous regulation of immunoglobulin A secretion from isolated perfused porcine ileum. Gut. 1999;45:679–685. doi: 10.1136/gut.45.5.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert ML, Shamburek RD. Control of acid secretion. Gastroenterol. Clin. North Am. 1990;19:1–25. [PubMed] [Google Scholar]
- Sharkey KA, Lomax AE, Bertrand PP, Furness JB. Electrophysiology, shape, and chemistry of neurons that project from guinea pig colon to inferior mesenteric ganglia. Gastroenterology. 1998;115:909–918. doi: 10.1016/s0016-5085(98)70263-x. [DOI] [PubMed] [Google Scholar]
- Shen L, Weber CR, Raleigh DR, Yu D, Turner JR. Tight junction pore and leak pathways: a dynamic duo. Annu. Rev. Physiol. 2011;73:283–309. doi: 10.1146/annurev-physiol-012110-142150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simren M, Barbara G, Flint HJ, Spiegel BM, Spiller RC, Vanner S, Verdu EF, Whorwell PJ, Zoetendal EG, Foundation Rome C. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013;62:159–176. doi: 10.1136/gutjnl-2012-302167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J, Kau AL, Rich SS, Concannon P, Mychaleckyj JC, Liu J, Houpt E, Li JV, Holmes E, Nicholson J, Knights D, Ursell LK, Knight R, Gordon JI. Gut microbiomes of Malawian twin pairs discordant for kwashiorkor. Science. 2013;339:548–554. doi: 10.1126/science.1229000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somasundaram K, Ganguly AK. The effect of subdiaphragmatic vagotomy on the gastric mucus barrier in rats. Clin. Exp. Pharmacol. Physiol. 1987;14:735–741. doi: 10.1111/j.1440-1681.1987.tb01899.x. [DOI] [PubMed] [Google Scholar]
- Sommer F, Backhed F. The gut microbiota--masters of host development and physiology. Nat. Rev. Microbiol. 2013;11:227–238. doi: 10.1038/nrmicro2974. [DOI] [PubMed] [Google Scholar]
- Steck N, Mueller K, Schemann M, Haller D. Bacterial proteases in IBD and IBS. Gut. 2012;61:1610–1618. doi: 10.1136/gutjnl-2011-300775. [DOI] [PubMed] [Google Scholar]
- Steinkamp M, Gundel H, Schulte N, Spaniol U, Pflueger C, Zizer E, Boyen von GB. GDNF protects enteric glia from apoptosis: evidence for an autocrine loop. BMC Gastroenterol. 2012;12:16. doi: 10.1186/1471-230X-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens RL., Jr. Disparate effects of intracisternal RX 77368 and ODT8-SS on gastric acid and serotonin release: role of adrenal catecholamines. Regul. Pept. 1991;36:21–28. doi: 10.1016/0167-0115(91)90192-j. [DOI] [PubMed] [Google Scholar]
- Stephens RL, Tache Y. Intracisternal injection of a TRH analogue stimulates gastric luminal serotonin release in rats. Am. J. Physiol. Gastrointest. Liver Physiol. 1989;256:G377–G383. doi: 10.1152/ajpgi.1989.256.2.G377. [DOI] [PubMed] [Google Scholar]
- Stoffels B, Hupa KJ, Snoek SA, Bree van S, Stein K, Schwandt T, Vilz TO, Lysson M, Veer CV, Hornung V, Kalff JC, Jonge de WJ, Wehner S. Post-operative Ileus Involves Interleukin-1 Receptor Signaling in Enteric Glia. Gastroenterology. 2013 doi: 10.1053/j.gastro.2013.09.030. In press. [DOI] [PubMed] [Google Scholar]
- Straub RH, Wiest R, Strauch UG, Harle P, Scholmerich J. The role of the sympathetic nervous system in intestinal inflammation. Gut. 2006;55:1640–1649. doi: 10.1136/gut.2006.091322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Fihn BM, Sjovall H, Jodal M. Enteric neurones modulate the colonic permeability response to luminal bile acids in rat colon in vivo. Gut. 2004;53:362–367. doi: 10.1136/gut.2003.015867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Zhang M, Chen CC, Gillilland M, 3rd, Sun X, El-Zaatari M, Huffnagle GB, Young VB, Zhang J, Hong SC, Chang YM, Gumucio DL, Owyang C, Kao JY. Stress-induced corticotropin-releasing hormone-mediated NLRP6 inflammasome inhibition and transmissible enteritis in mice. Gastroenterology. 2013;144:1478–1487. doi: 10.1053/j.gastro.2013.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szurszewski JH, Ermilov LG, Miller SM. Prevertebral ganglia and intestinofugal afferent neurones. Gut. 2002;51(Suppl 1):6–10. doi: 10.1136/gut.51.suppl_1.i6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tixier E, Lalanne F, Just I, Galmiche JP, Neunlist M. Human mucosa/submucosa interactions during intestinal inflammation: involvement of the enteric nervous system in interleukin-8 secretion. Cell Microbiol. 2005;7:1798–1810. doi: 10.1111/j.1462-5822.2005.00596.x. [DOI] [PubMed] [Google Scholar]
- Toumi F, Neunlist M, Cassagnau E, Parois S, Laboisse CL, Galmiche JP, Jarry A. Human submucosal neurones regulate intestinal epithelial cell proliferation: evidence from a novel co-culture model. Neurogastroenterol. Motil. 2003;15:239–242. doi: 10.1046/j.1365-2982.2003.00409.x. [DOI] [PubMed] [Google Scholar]
- Turnbaugh PJ, Backhed F, Fulton L, Gordon JI. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe. 2008;3:213–223. doi: 10.1016/j.chom.2008.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- Turner HL, Turner JR. Good fences make good neighbors: Gastrointestinal mucosal structure. Gut Microbes. 2010;1:22–29. doi: 10.4161/gmic.1.1.11427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner JR. Intestinal mucosal barrier function in health and disease. Nat. Rev. Immunol. 2009;9:799–809. doi: 10.1038/nri2653. [DOI] [PubMed] [Google Scholar]
- Valdez-Morales EE, Overington J, Guerrero-Alba R, Ochoa-Cortes F, Ibeakanma CO, Spreadbury I, Bunnett NW, Beyak M, Vanner SJ. Sensitization of Peripheral Sensory Nerves by Mediators From Colonic Biopsies of Diarrhea-Predominant Irritable Bowel Syndrome Patients: A Role for PAR2. Am. J. Gastroenterol. 2013;108:1634–1643. doi: 10.1038/ajg.2013.241. [DOI] [PubMed] [Google Scholar]
- Van Landeghem L, Chevalier J, Mahe MM, Wedel T, Urvil P, Derkinderen P, Savidge T, Neunlist M. Enteric glia promote intestinal mucosal healing via activation of focal adhesion kinase and release of proEGF. Am. J. Physiol. Gastrointest. Liver Physiol. 2011;300:G976–G987. doi: 10.1152/ajpgi.00427.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergnolle N. Protease-activated receptors as drug targets in inflammation and pain. Pharmacol. Ther. 2009;123:292–309. doi: 10.1016/j.pharmthera.2009.05.004. [DOI] [PubMed] [Google Scholar]
- von Boyen GB, Steinkamp M, Geerling I, Reinshagen M, Schafer KH, Adler G, Kirsch J. Proinflammatory cytokines induce neurotrophic factor expression in enteric glia: a key to the regulation of epithelial apoptosis in Crohn’s disease. Inflamm. Bowel Dis. 2006;12:346–354. doi: 10.1097/01.MIB.0000219350.72483.44. [DOI] [PubMed] [Google Scholar]
- Ward NL, Pieretti A, Dowd SE, Cox SB, Goldstein AM. Intestinal aganglionosis is associated with early and sustained disruption of the colonic microbiome. Neurogastroenterol. Motil. 2012;24:874–e400. doi: 10.1111/j.1365-2982.2012.01937.x. [DOI] [PubMed] [Google Scholar]
- Xia Y, Hu HZ, Liu S, Ren J, Zafirov DH, Wood JD. IL-1beta and IL-6 excite neurons and suppress nicotinic and noradrenergic neurotransmission in guinea pig enteric nervous system. J. Clin. Invest. 1999;103:1309–1316. doi: 10.1172/JCI5823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y, Liu ZQ, Liu XY, Yang L, Geng XR, Yang G, Liu ZG, Zheng PY, Yang PC. Stress-Derived Corticotropin Releasing Factor Breaches Epithelial Endotoxin Tolerance. PLoS One. 2013;8:e65760. doi: 10.1371/journal.pone.0065760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan PQ, Million M, Wu SV, Rivier J, Tache Y. Peripheral corticotropin releasing factor (CRF) and a novel CRF1 receptor agonist, stressin1-A activate CRF1 receptor expressing cholinergic and nitrergic myenteric neurons selectively in the colon of conscious rats. Neurogastroenterol. Motil. 2007;19:923–936. doi: 10.1111/j.1365-2982.2007.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusta B, Holland D, Waschek JA, Drucker DJ. Intestinotrophic glucagon-like peptide-2 (GLP-2) activates intestinal gene expression and growth factor-dependent pathways independent of the vasoactive intestinal peptide gene in mice. Endocrinology. 2012;153:2623–2632. doi: 10.1210/en.2012-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki M, Coudron PE, McCuen RW, Harrington L, Chu S, Schubert ML. H. pylori acutely inhibits gastric secretion by activating CGRP sensory neurons coupled to stimulation of somatostatin and inhibition of histamine secretion. Am. J. Physiol. Gastrointest. Liver Physiol. 2013;304:G715–G722. doi: 10.1152/ajpgi.00187.2012. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Li J. Carbachol ameliorates lipopolysaccharide-induced intestinal epithelial tight junction damage by down-regulating NF-kappabeta and myosin light-chain kinase pathways. Biochem. Biophys. Res. Commun. 2012;428:321–326. doi: 10.1016/j.bbrc.2012.10.056. [DOI] [PubMed] [Google Scholar]
- Zhou H, Liang H, Li ZF, Xiang H, Liu W, Li JG. Vagus nerve stimulation attenuates intestinal epithelial tight junctions disruption in endotoxemic mice through alpha7 nicotinic acetylcholine receptors. Shock. 2013;40:144–151. doi: 10.1097/SHK.0b013e318299e9c0. [DOI] [PubMed] [Google Scholar]
- Zucoloto S, Deus de DA, Martins AA, Muglia VF, Kajiwara JK, Garcia SB. The relationship between myenteric neuronal denervation, smooth muscle thickening and epithelial cell proliferation in the rat colon. Res. Exp. Med.(Berl) 1997;197:117–124. doi: 10.1007/s004330050061. [DOI] [PubMed] [Google Scholar]