Abstract
Background
ODD is considered to be a disorder of childhood, yet evidence suggests that prevalence rates of the disorder are stable into late adolescence and trajectories of symptoms persist into young adulthood. Functional outcomes associated with ODD through childhood and adolescence include conflict within families, poor peer relationships, peer rejection and academic difficulties. Little examination of functional outcomes in adulthood associated with ODD has been undertaken.
Method
Data for the present analyses come from a clinic referred sample of 177 boys aged 7 to 12 followed up annually to age 18 and again at age 24. Annual parental report of psychopathology through adolescence was used to predict self-reported functional outcomes at 24.
Results
Controlling for parent reported symptoms of ADHD, CD, depression and anxiety, ODD symptoms from childhood through adolescence predicted poorer age 24 functioning with peers, poorer romantic relationships, a poorer paternal relationship, and having nobody who would provide a recommendation for a job. CD symptoms predicted workplace problems, poor maternal relationship, lower academic attainment and violent injuries. Only parent reported ODD symptoms and child reported CD symptoms predicted a composite of poor adult outcomes.
Conclusion
ODD is a disorder that significantly interferes with functioning, particularly in social or interpersonal relationships. The persistence of impairment associated with ODD into young adulthood calls for a reconsideration of ODD as a disorder limited to childhood.
Keywords: Oppositional defiant disorder, impairment, outcomes, adulthood
Although non-compliant behavior towards parents is often the primary focus of discussions of oppositional defiant disorder (ODD), it should not be surprising to observe that youth with ODD experience difficulties beyond conflicted parent-child interactions. The symptoms of ODD do include defiance and non-compliance with directives, but they also include problems with acting out of spite, annoying and blaming others, having temper control difficulties, and being generally irritable and angry. In childhood, ODD is predictive of worsening parenting practices (Burke, Pardini & Loeber, 2008), family conflict and poor family cohesion (Greene et al., 2002; Tseng, Kawabata, & Gau, 2011). Additionally, it is associated with poor peer interactions (Munkvold, Lundervold, & Manger, 2011), negative social preference (Burke, Waldman & Lahey, 2010) and peer rejection as an element within a composite of early conduct problems (van Lier & Koot, 2010). ODD is also associated with poorer functioning in school settings (Greene, et al., 2002). Among a sample of adults with ADHD, a lifetime history of ODD obtained through retrospective recall was associated with a history of repeating school grades, regardless of CD status (Harpold et al., 2007). Thus the impairments associated with ODD are pervasive across settings and types of social interactions.
Although ODD is characterized as a disorder of childhood, it seems likely that these difficulties would not simply cease upon reaching adulthood. Rather, it seems more plausible that individuals with ODD likely continue to demonstrate problematic behavior during interactions with peers, coworkers, bosses and customers, and would have problems maintaining jobs and relationships. Nevertheless, apart from a growing body of evidence regarding increased rates of other psychopathology in adulthood associated with ODD, there remains a striking absence of information about the degree to which ODD confers risks for poor functional outcomes in adulthood.
ODD has long been recognized as a significant predictor of conduct disorder (CD; Burke, Loeber, & Birmaher, 2002; Lahey et al., 1995), although more recent evidence suggests that ODD may not always function as a robust predictor of CD. For instance, Rowe and colleagues (2010) found that a diagnosis of ODD in girls was not significantly predictive of the later development of CD. In addition, a growing body of evidence shows that other forms of psychopathology may also develop from ODD.
ODD has been shown to predict depression and anxiety (Boylan, Vallaincourt & Szatmari, 2012; Burke et al., 2005; Burke, Hipwell & Loeber, 2010; Copeland, Shanahan, Costello & Angold, 2009; Rowe, Maughan, Pickles, Costello & Angold, 2002) and borderline personality disorder (Burke & Stepp, 2011; Stepp et al., 2011). Much of this evidence has been focused on the proximate effects of ODD – for example, whether ODD increases the risk for CD or depression during the following year (e.g. Burke et al., 2005). Only a few studies have examined ODD as a predictor of psychopathology in adulthood. These have found robust effects for childhood ODD on adult outcomes including depression (Burke, 2012; Copeland et al., 2009; Stringaris, Cohen, Pine & Leibenluft, 2009) and borderline personality disorder (Burke & Stepp, 2012), even after accounting for the effects of other concurrent psychopathology. Whether ODD predicts antisocial personality disorder in adulthood over and above the effects of CD is less clear, with some evidence that it does (Langbehn, Cadoret, Yates, Troughton, & Stewart, 1998) and that it does not (Lahey, Loeber, Burke, & Applegate, 2005).
The outcome of ODD itself is somewhat unclear. When identified early in childhood, ODD persists later into childhood (Keenan et al., 2011) and into adolescence (Cohen et al., 1993; Offord et al., 1992). Prevalence rates across development also show persistence from childhood into adolescence (Boylan, Vaillancourt, Boyle, & Szatmari, 2007; Maughan, Rowe, Messer, Goodman & Meltzer, 2004). Examining the trajectory of oppositional defiant behaviors through late adolescence, Leadbeater, Thompson, & Gruppuso (2012) found that a level trajectory from 12 to 24 described the course for young men. This contrasted with the course of ODD behaviors for young women, who showed a curvilinear trajectory, with a slight decline in symptoms starting around ages 16 to 18. As Leadbeater and colleagues (2012) observed, these results suggest that, especially for young men, ODD symptoms might interfere with relationships with employers, parents, friends and romantic relationships in young adulthood.
The present study uses prospectively collected parent report of psychopathology in a clinic-referred sample of boys from childhood through adolescence to predict age 24 self-report of problems in interpersonal functioning, academic achievement, antisocial and rule breaking behavior, physical health and injuries. Specific hypotheses to be tested are: 1) ODD symptoms will predict poor outcomes over and above the effects of co-occurring child and adolescent CD, ADHD, depression and anxiety; and 2) Specific risk will be evident for problems of interpersonal functioning, whereas other types of problems, such as rule-violations or antisocial behavior will be predicted by CD or ADHD.
Method
Data for the present analyses come from the Developmental Trends Study (Loeber, Green, Lahey, Frick, & McBurnett, 2000), a sample of 177 boys aged between 7 and 12 who were recruited from general psychiatric clinics in Pennsylvania and Georgia. The referral process to the study was not specific to any particular disorder. Boys were followed up annually to age 17. Young adult assessments were conducted with the youth as the respondent at 24. All study procedures were approved and monitored by the Institutional Review Board of the University of Pittsburgh. Informed consent was obtained for all participants.
Enrollment criteria included: boys living with at least one biological parent; no history of mental retardation or psychosis, no inpatient psychiatric treatment within the last six months, and no psychotropic medication that could not be discontinued for two days prior to baseline assessment. Further details on this sample have been published previously (e.g. Loeber, et al., 2000). Retention rates through adolescence ranged from a high of 100% in Year 2 to 87.1% in Year 10, with an average across all years of 93.4%. There were 143 participants (80.8% of the original sample) assessed at age 24. The sample was composed of non-Hispanic white (70%) and African-American boys (30%).
Despite previous evidence in this sample that ADHD symptoms and low SES were particularly associated with wave to wave difficulty with contacts and interview completion (Cotter, Burke, Loeber, & Mutchka, 2005), no demographic factors (SES, urban residence, parent marital status, race) or measures of child psychopathology were significantly associated with missingness at age 24, although the lowest p value (p = 09) was that of ADHD symptoms. Measures
Disruptive Behavior Disorders
A modified version (Loeber et al., 1989) of the DISC (Costello et al., 1987) was used for this study. Parent report of symptoms of ODD, ADHD, and CD was obtained at each wave through age 17. Although child and teacher report were also collected, neither included assessment of all relevant symptoms beyond year 4 of the study. At year 1 of the study, parents reported a mean of 5.0 ODD symptoms (range 0 to 8), with a reliability alpha of .76. At year 1, parents reported a mean of 1.29 symptoms (sd=1.4) of CD (range 0 to 6). The reliability alpha for CD symptoms at baseline was low, at .58. Parents reported a mean of 8.15 symptoms (sd=3.5) of ADHD (range 0 to 14), with an reliability alpha of .83.
Based on symptom count by parent report, without regard to other criteria (notably impairment) as detailed in the DSM-III-R, boys in this study at baseline predominantly met criteria for behavioral disorders and showed a high degree of comorbidity. Specifically, 73.5% (n=130) met parent-reported symptom criteria for ODD, 64.9% (n = 115) met criteria for ADHD, and 19.2% (n = 34) met criteria for CD. Across these disorders, 84% (n = 149) met criteria for one of ADHD, ODD or CD at baseline.
Depression and anxiety
Parent DISC report was used to create a composite depression variable by combining reports of symptoms of dysthymia (DYS) and major depression (MD). As defined by the DSM (APA, 1994), MD includes anhedonia, psychomotor agitation or retardation and recurrent thoughts of death, whereas DYS does not. Conversely, DYS includes hopelessness, MD does not. To avoid counting overlapping symptoms twice, depression in these analyses is the sum of ten unique symptoms across MD and DYS. Further, irritability was not considered as a substitute for dysphoric mood in these analyses. Cronbach’s alpha for composite depression symptoms at baseline was .77. Parents reported an average of 1.43 symptoms (sd = 1.86), ranging from 0 to 8 symptoms at baseline.
Our measure of anxiety included assessments of overanxious disorder (OAD) and separation anxiety disorder (SAD). OAD measures general indicators of anxiety, such as unrealistic worry or preoccupation about past or future events, concerns about competence, and physical tension. SAD measures concerns about separation from caregivers, fears of harm befalling caregivers, and refusal to go to school or to fall asleep without being in proximity to caregivers. These items were summed together into one index of anxiety. At baseline, parents reported a range from 0 to 12 symptoms (m= 3.18, sd = 2.5). Cronbach’s alpha at baseline was .78.
Outcomes in young adulthood
Outcomes in young adulthood included dichotomous responses, Likert ratings and counts. For these analyses, all outcomes were dichotomized with an effort to contrast to the greatest extent possible the lowest (less desirable outcome) quartile with the remainder.
Work history
At age 24, participants were asked questions about their work history using a three point scale ranging from “worse” to “about average” to “better.” Since only 2 participants rated their interactions with co-workers as worse than average, ratings of “about average” or “worse” (n = 78; 55.3%) were combined as problems with co-workers. Similarly, only 6 participants rated their interactions with a boss as “worse”; when combined with “about average” ratings, 76 participants rated (54.7%) their problems with a boss as “about average” or “worse.” They were asked whether they were ever fired from a job (n = 53; 38.7%), and 19 (13.4%) said that if they had to look for another job, there was nobody to provide a recommendation for them.
Relationships
Participants were asked questions regarding relationships with family members, romantic relationships, and sexual behaviors. These included how well their mother is doing as a parent to them, how well their father or step-father is doing as a parent (rated on a six point scale from “very well” to “not so well.”). Values of 3 or lower were recoded as positive for having a poor relationship with their mother (n = 28; 20.1%) were coded as having a poor maternal relationship. One-quarter (n=31) of the participants responded with 5 or 6 regarding their father or step-father, and were coded as having a poor paternal relationship.
Participants were asked to name their closest friends, and the lowest quartile (n=36) in terms of number of friends (having named two or fewer friends), was coded as having a low number of friends. For the three closest friends, participants were asked about how long their friendship has lasted, in months. The lowest quartile of the average of these three scores was denoted by scores at or below 60 months, and was coded as a low duration of friendships. They were asked to rate, using a six-point Likert scale from “not so well” to “very well” how well they were doing with their friends; 41 (28.9%) rated themselves as 4 or lower on this scale, and were coded positive for doing poorly with friends.
Participants were asked whether they had a current romantic relationship and how well they got along, using a four point scale ranging from “very well” to “not well at all.” Those who reported having no romantic relationship or who rated their current relationship as less than “very well” were coded positive for poor romantic relationship (n = 84; 59.6%). They were also asked how many times in the past year they had sexual intercourse; 16 (11.4%) reported having had no sex in the past year.
Conflict Tactics Scale
Participants completed the Conflict Tactics Scale (Straus, Hamby, BoneyMcCoy, & Sugarman, 1996), including questions about whether or not they had assaulted their partner (n = 34, 25.4%) or their report of whether the partner had assaulted them (n = 38, 28.4%).
Other outcomes
Participants were asked at age 24 about their history of use of any illicit substances using a modification of the Drug Consumption Questionnaire (Elliott, Huizinga & Ageton, 1985); 16% (n=23) reported any use of illegal substances in the past year. They were asked about having been arrested or detained by the police in the past year, and 18.9% (n=27) indicated that they had. Participants reported on the presence of any health problems at age 24; 11.3% (n = 16) reported having two or more health problems. They were also asked about serious injuries in the form of severe burns or severe cuts, head injuries or internal injuries or broken bones; 32.4% reported having at least one instance of such over the past year. Additionally, 7.8% (n = 11) reported having experienced at least one injury from a gunshot or stabbing during the previous five years. Regarding academic achievement, 17.5% (n=25) reported having neither completed high school, nor having gotten a general equivalency degree (GED). Finally, 28.7% reported having ever had their driver’s license suspended.
Composite of functional outcomes
A composite of poor functional outcomes was created by summing across all outcomes described above. The mean of the composite was 5.37 (sd = 3.02), with a range from 0 to 15.
Statistical analyses
Logistic regression models were conducted for each individual outcome
Values at each measurement wave from childhood to adolescence were included as time-varying predictors of the outcome at 24. The primary focus was on prediction from parent report of psychopathology. In order to test for the potential effects of CD symptoms occurring outside of the parent’s knowledge, additional post-hoc analyses were conducted to examine child reported CD symptoms as well. Further details on these analyses are provided below. Observations were clustered by participant to account for within-individual correlation, and a robust estimator of variance was employed. Analyses of the summary composite outcome specified a Poisson distribution, as appropriate for count outcomes. The variance inflation factor (VIF) and tolerance statistics were examined for each model to ensure that multicollinearity was not a concern, using a VIF of 4 or greater as the criterion level for individual predictors, or 10 or greater for the model as a whole.
Age cohort effects
Because the study design resulted in an unbalanced design, younger participants at baseline contributed more waves of observations to the predictors in the study panel than older participants. For instance, baseline 7 year olds contributed five more years of data than baseline 12 year olds, baseline 8 year olds four more than 12 year olds, and so on. It is possible then that systematic differences between 7 year olds and 12 year olds could influence the results. The numbers in each cohort at baseline were approximately equivalent, ranging from 14% of the sample being age 10 at baseline to 20% being age 8.
To test for cohort effects, we examined the interaction between baseline age cohort and ODD symptoms for each outcome. In two individual instances, we found significant interactions: problems with coworkers and having nobody who would provide a recommendation. Additionally, this interaction was evident in the prediction to the composite of outcomes. In each case, the effect was stronger for the cohorts who were younger at baseline. Also in each case, removing the youngest cohort from the analyses resulted in a non-significant interaction term. Finally, the interaction between ODD symptoms and age was not significant, suggesting that the interaction between age cohort and ODD symptoms was influenced by the youngest cohort itself rather than a difference across ages over development. Since the exclusion of the youngest cohort did not meaningfully alter the results, all cohorts were included in the results that follow.
Multiple imputation
The creation of the composite of outcomes relied on casewise deletion where any case was missing on any one of the variables that contributed to the composite. This resulted in the number of valid cases dropping from 143 to 120. Because of this, it was possible that the implications of the results might be influenced artificially by the exclusion of those cases. We explored this by conducting multiple imputation of the missing observations. Slight differences were found. We report the results below from both the non-imputed and imputed data.
Results
Measures of association among psychopathology variables
Given the clinical nature of the present sample, a relatively high degree of association among measures of psychopathology was evident. Table 1 shows the association among symptom counts at Year 1 for the study. Additionally, Spearman’s rho for the association between the irritability and behavioral dimensions of ODD was .54. Multicollinearity was evaluated, as noted above. There were no models in which the VIF for an individual predictor exceeded 4, nor did any VIF exceed 10 for the model as a whole.
Table 1.
Association among symptom counts at year 1
| CD | ADHD | Depression | Anxiety | |
|---|---|---|---|---|
| ODD | .516 | .394 | .402 | .262 |
| CD | .437 | .315 | .159 | |
| ADHD | .164 | .222 | ||
| Dep | .435 |
Note: ODD = Oppositional Defiant Disorder, CD = Conduct Disorder, ADHD = Attention Deficit Hyperactivity Disorder. Values given are Spearman’s rho coefficients.
Prediction from ODD symptom count to young adult outcomes
The relationship between ODD symptoms and each outcome was tested independently from other covariates (apart from age). The odds ratio (OR) and 95% confidence interval are shown in the first two columns of Table 2. ODD symptoms were significantly predictive of poor peer relationships, having a low number of friends, having been fired from a job, having problems with coworkers, having nobody to provide a recommendation, having a poor maternal and paternal relationship, having a poor romantic relationship, and causing injury to a partner.
Table 2.
Prediction from ODD symptoms from childhood through late adolescence to social outcomes in young adulthood
| Parameter values for ODD symptom count through adolescence |
|||||
|---|---|---|---|---|---|
| Outcome | Simple OR |
95% CI | Multiple OR |
95% CI | Other predictors |
| Poor peer relationships | 1.11* | 1.00-1.24 | 1.11* | 1.00-1.24 | None |
| Low number of friends | 1.18** | 1.05-1.31 | 1.18** | 1.05-1.31 | None |
| Low duration of friendships | 1.07 | 0.95-1.20 | - | - | None |
| Been fired from a job | 1 17** | 1.06-1.30 | - | - | CD*** |
| Problems with boss | 1.07 | 0.97-1.18 | - | - | None |
| Problems with coworkers | 1.11* | 1.00-1.23 | - | - | CD** |
| Nobody to provide recommendation |
1.20** | 1.06-1.36 | 1.20** | 1.06-1.36 | None |
| Relationship with mother | 1 17** | 1.04-1.32 | - | - | CD*** |
| Relationship with father | 1.20** | 1.07-1.35 | 1.20** | 1.07-1.35 | none |
| Has not had sex in past year | 1.13 | 0.97-1.32 | - | - | DEP** |
| Poor romantic relationship | 1 19*** | 1.07-1.33 | 1 19*** | 1.07-1.33 | none |
| Assaulted partner | 1.09 | 0.98-1.21 | - | - | None |
| Was assaulted by partner | 1.10 | 0.98-1.23 | - | - | None |
| Did not finish high school | 1 19** | 1.05-1.36 | - | - | CD*** |
| Health problems | 1.02 | 0.89-1.17 | - | - | DEP* |
| Serious injuries | 1.01 | 0.91-1.11 | - | - | None |
| Gunshot or stabbed | 1.13 | 0.98-1.32 | - | - | ADHD*†, CD*** |
| License ever suspended | 1.07 | 0.96-1.20 | - | - | ADHD** |
| Arrested | 1.08 | 0.96-1.21 | - | - | DEP*†, ADHD*** |
| Illicit drug use past year | 1.08 | 0.98-1.18 | - | - | None- |
Note: Each model included age as a covariate. OR = odds ratio; ODD = oppositional defiant disorder.
< .05;
< .01;
< .001,
= inversely associated. Empty cells indicate that ODD was not retained in multivariate models using stepwise removal of non-significant predictors.
Prediction to young adult outcomes controlling for concurrent psychopathology
Each model was then tested in a regression including the symptom counts of ODD, CD, ADHD, depression and anxiety as predictors. A stepwise removal procedure was used to remove predictors with a criterion alpha value of greater than 0.1. The OR and 95% CI are shown in columns 3 and 4 of Table 2. The final column indicates which other psychopathology constructs were retained in the models. For many outcomes, ODD was retained as the only predictor, or none of the symptom counts for any type of psychopathology remaining in the model.
Composite of young adult social functioning
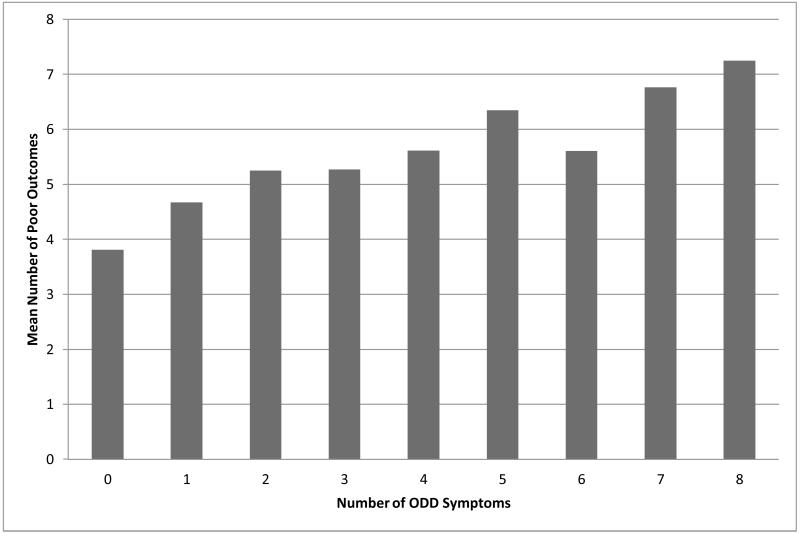
Finally, we tested a composite summary of social outcomes, using a Poisson regression model, and standardizing symptom counts to enhance comparison of parameters across psychopathology constructs. Figure 1 shows the average number of poor outcomes by the number of parent reported ODD symptoms. Since casewise deletion reduced the number of observations in the composite to 120, we also tested a composite using multiple imputation of missing observations.
Figure 1.
Mean number of poor outcomes in adulthood by the number of ODD symptoms present in childhood or adolescence
With casewise missing values and all psychopathology predictors in the model, only ODD predicted the composite of poor outcomes (IRR = 1.15, 95% CI = 1.05-1.26, p = .003). Slight differences were observed when predicting to the imputed composite (Table 3). Specifically, in addition to ODD predicting poor outcomes, ADHD was marginally predictive. A stepwise removal resulted in ODD (IRR = 1.16, 95% CI = 1.07-1.24, p <.001) and ADHD (IRR = 1.02, 95% CI = 1.00 – 1.16, p = .035) being retained in the model, along with age.
Table 3.
Prediction to young adult composite functional outcomes from psychopathology symptoms through late adolescence
| Parameter values for standardized symptom counts through adolescence |
||||
|---|---|---|---|---|
| IRR | p | 95% CI | ||
| ODD | 1.12 | .004 | 1.04 | 1.22 |
| CD | 1.03 | .148 | 0.98 | 1.08 |
| ADHD | 1.07 | .065 | 0.99 | 1.15 |
| Depression | 0.99 | .766 | 0.95 | 1.04 |
| Anxiety | 1.04 | .217 | 0.98 | 1.10 |
| Age | 1.02 | .015 | 1.00 | 1.04 |
Note: IRR = Incidence rate ratio, ODD = oppositional defiant disorder, CD = Conduct disorder, ADHD = Attention deficit hyperactivity disorder. This analysis was conducted using a multiple imputation strategy to impute missing composite variables. The predictors for this model have been standardized in order to facilitate direct comparison.
Post-hoc test of child-reported CD
It is possible that parent-reported CD might fail to predict poor outcomes if parents are not aware of their children’s antisocial behaviors (e.g. covert antisocial behaviors or behaviors the child shows in the community outside of the parent’s ability to observe). To test for this possibility, we re-ran each model including child reported CD. Doing so of course results in a more robust test of the effects of parent reported ODD, since the relationship between child-reported CD and self-reported adult outcomes may be influenced by having a common informant. Since self-reported ODD symptoms was not obtained after year 2, it was not possible to include them in these models.
Issues of multicollinearity were not evident
First, parental and child report of CD behaviors are known to show relatively modest concordance, and such was the case in the present data set (rho = .35). Second, no VIF or tolerance statistics suggested any problems with multicollinearity associated with the introduction of child reported CD symptoms in these models.
Each outcome was retested, including child-reported CD
Differences affecting prior findings regarding ODD were observed for poor peer relationships, where child-reported CD was predictive (IRR = 1.26, 95% CI = 1.07-1.49, p = .006) and parent reported ODD was no longer, and for having a low number of friends, where in addition to ODD, child-reported CD was also predictive (IRR = 1.13, 95% CI = 1.06-1.51, p = .01). Child report of CD symptoms replaced parent report of CD symptoms as the sole predictor of having been fired and of problems with co-workers. In two models where no psychopathology had been predictive, child-reported CD predicted assaulting a partner (IRR = 1.18, 95% CI = 1.01-1.38, p = .04) and illicit drug use in the past year (IRR = 1.20, 95% CI = 1.02–1.41, p = .03). Child-reported CD was also retained as a predictor of having been shot or stabbed in the past five years (IRR = 1.39, 95% CI = 1.19 - 1.63, p < .001), along with parent reported CD and ADHD symptoms.
Finally, child-reported CD influenced the prediction of the composite of functional outcomes (using multiple imputation of missing observations). It was significantly predictive (IRR = 1.07, 95% CI = 1.02-1.25, p = .012), along with ODD (IRR = 1.13, 95% CI = 1.06-1.23, p = .001), and ADHD was reduced to marginal significance (IRR = 1.08, 95% CI = 0.99-1.16, p = .06).
Discussion
ODD is a disorder associated with a variety of impairments in interactions with others. Rather than being a disorder of poor parent-child interactions alone, youth with ODD struggle with peers, with other adults, and in romantic relationships. The results of the present analyses suggest that in a clinically referred sample of boys, in comparison to other disorders in childhood and adolescence, ODD confers unique risk for specific types of problems in young adulthood. In particular, ODD predicted problems in the quality and number of positive peer relationships, romantic relationships, relationships with parents in young adulthood, and whether or not anyone would provide a recommendation letter for a job application. Impairments in these areas likely influence overall quality of life and overall adjustment in young adulthood markedly. When the quality of peer, romantic and parenting relationships is suboptimal, social support may be lacking. Deficits in social support appear to operate through several distinct mechanisms (Cohen, 2004) to buffer the effects of stressors on physical and mental health outcomes (Gallo, de Los Monteros & Shivpuri, 2009). As a result, youth with ODD who subsequently experience impaired interactions of the types identified in the present data are at greater risk for a variety of other poor health outcomes. In combination with the existing literature, the present results suggest that ODD is associated across the early lifespan with important functional impairments that go beyond noncompliance in the parent-child relationship.
These results also suggest that, rather than being a disorder with limited effects in childhood, ODD may instead have effects that persist into adulthood. While the present results come from a modestly sized clinical sample of boys, they are nevertheless clearly in accord with the suggestion made by Leadbeater and colleagues (2012) that youth with ODD may experience problems in adulthood with peer and romantic relationships. The symptoms and defining features of ODD suggest, in part, potential difficulties interacting with authority figures, yet the significant associations between childhood ODD and young adult functioning in the workplace in the present data were explained by concurrent CD symptoms. This limited lack of association may be due to the nature of the measures used in the present study. In particular, the present measures of workplace function allowed only three response options. Further investigation with more nuanced measures may help to clarify whether individuals with ODD do have difficulty in interactions in a variety of settings, including with coworkers and supervisors. Additionally, examining youth self-reported ODD in addition to parent report may yield additional evidence of the relationship between ODD symptoms through adolescence and functional outcomes in adulthood.
Where ODD predicted poor outcomes in the present analyses, they were somewhat circumscribed to interpersonal outcomes: relationships with peers, romantic relationships and family members. ODD symptoms were not predictive, after accounting for other psychopathology, of overt antisocial or criminal behavior, low educational attainment, problems with lawful driving behavior or physical health. An absence of unique prediction to antisocial outcomes from ODD is consistent with previous studies that have shown that in the absence of CD symptoms, ODD symptoms are not predictive of antisocial personality disorder (Burke, Waldman & Lahey, 2010; Lahey et al., 2002). The lack of prediction to other types of outcomes in the present study may suggest a particular risk for types of poor outcomes associated with ODD independent of other psychopathology.
If the effects of ODD may be said to persist into adulthood, it remains something of an open question as to whether the disorder itself does. Although it has been historically categorized as a disorder of childhood, there has been no diagnostic prohibition in the DSM-IV (APA, 1994) against assigning the diagnosis in adulthood. Whether or not ODD persists into adulthood has been given very little theoretical consideration or empirical investigation. Perhaps this is a reflection of the mistaken view that ODD is almost entirely a disorder of conflict with parents or teachers. The small set of studies in which ODD in adulthood has been considered are predominantly studies of samples of individuals with ADHD. These studies (e.g. Barkley, Edwards, Laneri, Fletcher, & Metevia, 2001; Harpold, et al., 2007) suggest that ODD remains a valid and diagnosable condition in young adulthood, at least among groups with ADHD.
The present data did not include the direct measurement of ODD symptoms in adulthood; further investigation is needed to help clarify to what degree ODD persists into adulthood and how it may affect important transitions into new or different social roles and expectations for independent functioning. The nature of ODD symptoms, and in particular the degree to which they involve persistent characteristics or typical difficulties in interacting with others may suggest a need to differentiate ODD symptoms in adults from personality disorders. Additionally, it may be necessary to evaluate whether alternative symptoms are more appropriate for identifying ODD in adulthood.
As noted, other psychopathology in childhood and adolescence was associated with some measures of poor adult functioning. In particular, although bivariate analyses initially suggested workplace problems were associated with ODD, outcomes of having been fired from a job and having problems with coworkers in young adulthood were better accounted for by the presence of CD symptoms. CD symptoms were also a stronger predictor of a poor maternal relationship, not finishing high school and reporting a history of gunshot or stabbing wounds. Depression was predictive of not having had sex during the past year, having multiple health problems, and was inversely related to being arrested. ADHD predicted having a driver’s license suspended and contributed to the prediction of gunshot or stabbings and to being arrested. Anxiety was not predictive, over and above the effects of other psychopathology, of the functional problems measured in this study. . These disorders almost assuredly would be predictive of other poor outcomes in and of themselves if observed outside of the comorbidity arising within this clinical sample of boys.
Relatedly, recent evidence has shown that those with ADHD through adolescence continue to experience poor outcomes in adulthood (e.g. Gjervan, Torgersen, Nordahl, & Rasmussen, 2012; Kuriyan et al., 2013). There are several similarities between the historical conceptualizations and investigation of ADHD and ODD. ADHD has traditionally been considered to be a disorder of childhood and was believed to desist over development into adulthood (e.g. Bolea et al., 2012). Presently there is great interest in defining and identifying adult ADHD (Martel, von Eye & Nigg, 2012) and controversy surrounding the persistence of ADHD into adulthood, at least from an anecdotal perspective, appears to be diminishing. In the present analyses, for a subset of functional outcomes, ODD is a stronger predictor of impairment than ADHD, which suggests that future studies of the transitions from childhood psychopathology into adulthood, and studies of functional outcomes associated with other disorders, should explicitly include ODD in their models.
Finally, post-hoc testing of child reported CD symptoms did not yield substantial changes to the results, despite the concern regarding common informant effects. Although the modest association between parent and child reported CD symptoms did suggest the potential that parents and children were reporting somewhat different perspectives on CD, the implications from models of solely parent-reported psychopathology were not markedly altered. These results highlight the utility of obtaining child-report of CD symptoms from a prognostic perspective. Replication in studies that have consistent measures of parent and child reported ODD may help to more fully evaluate multiple informant influences on risks associated with disruptive behavior in childhood and adolescence.
Limitations
The present data come from a selected sample of clinically referred boys. They likely represent the extreme end of the distribution of ODD-related behaviors. Answering questions about the extent to which more moderate demonstrations of ODD symptoms predict poor functioning in adulthood will require more representative samples. In addition, it seems reasonable to hypothesize that women, who may potentially experience different social roles and expectations, might suffer poor functional outcomes to a greater or lesser degree than men. Girls show relatively similar levels of ODD symptoms through adolescence (e.g. Boylan, Vaillancourt, Boyle, & Szatmari, 2007; Leadbeater, et al., 2012), although they may show a different, and declining, trajectory into adulthood (Leadbeater, et al., 2012). Nevertheless, it may be a mistake to discount risks for women associated with ODD as they transition into adulthood based on beliefs about gender differences in behavioral disorders. An additional limitation arises from the limited nature of the measures of functioning in young adulthood. For many of the outcomes, the present measures are relatively gross indicators, lacking nuance and allowing a limited estimate of variability in functioning. It is nevertheless worthwhile to examine which disorders are associated with relatively lower reported functioning, even if the contrasts in some cases are between good functioning and at best average functioning. To advance this literature, studies with measures of interpersonal functioning that are independent of the respondent’s perspective are needed.
Key points.
Oppositional defiant disorder measured from childhood through adolescence is robustly predictive of poor functioning in young adulthood.
Higher levels of oppositional defiant disorder symptoms were particularly associated with having fewer, and lower quality peer relationships, poor romantic relationships and impaired paternal relationships.
Problems involving rule violations or aggression tended to be predicted by CD or ADHD, whereas ODD was generally more predictive of outcomes involving poor social functioning.
Oppositional defiant disorder in adulthood should be given greater empirical attention.
Acknowledgments
Dr. Burke is with the Western Psychiatric Institute and Clinic at the University of Pittsburgh.
The authors are grateful to Drs. Rolf Loeber (R.L.) and Benjamin B. Lahey and colleagues for their input into the research program for which the study reported herein forms part. This work was supported by grants to J.D.B. (MH095969), and to R.L. (MH42529) from the National Institute of Mental Health.
Abbreviations
- ODD
oppositional defiant disorder
- ADHD
attention deficit hyperactivity disorder
- CD
conduct disorder
Footnotes
The authors have declared that they have no competing or potential conflicts of interest.
References
- American Psychiatric Association. American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV. 4th ed. American Psychiatric Association; Washington, DC: 1994. Task Force on DSM-IV. [Google Scholar]
- Barkley RA, Edwards G, Laneri M, Fletcher K, Metevia L. Executive functioning, temporal discounting, and sense of time in adolescents with attention deficit hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) Journal of Abnormal Child Psychology. 2001;29(6):541–556. doi: 10.1023/a:1012233310098. [DOI] [PubMed] [Google Scholar]
- Bolea B, Adamou M, Arif M, Asherson P, Gudjonsson G, Muller U, Young S. ADHD matures: time for practitioners to do the same? Journal of Psychopharmacology. 2012;26(6):766–770. doi: 10.1177/0269881111410898. [DOI] [PubMed] [Google Scholar]
- Boylan K, Vaillancourt T, Boyle M, Szatmari P. Comorbidity of internalizing disorders in children with oppositional defiant disorder. European Child & Adolescent Pscyhiatry. 2007;16(8):484–494. doi: 10.1007/s00787-007-0624-1. [DOI] [PubMed] [Google Scholar]
- Boylan K, Vaillancourt T, Szatmari P. Linking oppositional behaviour trajectories to the development of depressive symptoms in childhood. Child Psychiatry and Human Development. 2012;43:484–497. doi: 10.1007/s10578-011-0277-7. [DOI] [PubMed] [Google Scholar]
- Burke JD. An affective dimension within oppositional defiant disorder symptoms among boys: personality and psychopathology outcomes into early adulthood. Journal of Child Psychology & Psychiatry. 2012;53(11):1176–1183. doi: 10.1111/j.1469-7610.2012.02598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Hipwell AE, Loeber R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(5):484–492. doi: 10.1097/00004583-201005000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Birmaher B. Oppositional defiant disorder and conduct disorder: A review of the past 10 years, part II. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(11):1275–1293. doi: 10.1097/00004583-200211000-00009. [DOI] [PubMed] [Google Scholar]
- Burke JD, Pardini DA, Loeber R. Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. Journal of Abnormal Child Psychology. 2008;36(5):679–692. doi: 10.1007/s10802-008-9219-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Stepp SD. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. Journal of Abnormal Child Psychology. 2012;40(1):35–44. doi: 10.1007/s10802-011-9558-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Waldman I, Lahey BB. Predictive validity of childhood oppositional defiant disorder and conduct disorder: implications for the DSM-V. Journal of Abnormal Psychology. 2010;114:739–751. doi: 10.1037/a0019708. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. The American Psychologist. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen P, Cohen J, Brook J. An epidemiological study of disorder in late childhood and adolescence, II: persistence of disorders. Journal of Child Psychology and Psychiatry. 1993;34:869–877. doi: 10.1111/j.1469-7610.1993.tb01095.x. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotter RB, Burke JD, Loeber R, Mutchka J. Predictors of contact difficulty and refusal in a longitudinal study. Criminal Behaviour and Mental Health. 2005;15(2):126–137. doi: 10.1002/cbm.46. [DOI] [PubMed] [Google Scholar]
- Gallo LC, de Los Monteros KE, Shivpuri S. Socioeconomic Status and Health: What is the role of Reserve Capacity? Current Directions in Psychological Science. 2009;18:269–274. doi: 10.1111/j.1467-8721.2009.01650.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjervan B, Torgersen T, Nordahl HM, Rasmussen K. Functional impairment and occupational outcome in adults with ADHD. Journal of Attention Disorders. 2012;16:544–552. doi: 10.1177/1087054711413074. [DOI] [PubMed] [Google Scholar]
- Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, Faraone SV. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. American Journal of Psychiatry. 2002;159(7):1214–1224. doi: 10.1176/appi.ajp.159.7.1214. [DOI] [PubMed] [Google Scholar]
- Harpold T, Biederman J, Gignac M, Hammerness P, Surman C, Potter A, Mick E. Is oppositional defiant disorder a meaningful diagnosis in adults? Results from a large sample of adults with ADHD. Journal of Nervous and Mental Disorders. 2007;195:601–605. doi: 10.1097/NMD.0b013e318093f448. [DOI] [PubMed] [Google Scholar]
- Keenan K, Boeldt D, Chen D, Coyne C, Donald R, Duax J, Humphries M. Predictive validity of DSM-IV oppositional defiant and conduct disorders in clinically referred preschoolers. J Child Psychol Psychiatry. 2011;52(1):47–55. doi: 10.1111/j.1469-7610.2010.02290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriyan AB, Pelham WE, Jr., Molina BS, Waschbusch DA, Gnagy EM, Sibley MH, Kent KM. Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology. 2013;41:27–41. doi: 10.1007/s10802-012-9658-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke JD, Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. Journal of Consulting and Clinical Psychology. 2005;73:389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Hart EL, Frick PJ, Applegate B, Zhang Q, Russo MF. Four year longitudinal study of conduct disorder in boys: Patterns and predictors of persistence. Journal of Abnormal Psychology. 1995;104(1):83–93. doi: 10.1037/0021-843X.104.1.83. [DOI] [PubMed] [Google Scholar]
- Langbehn DR, Cadoret RJ, Yates WR, Troughton EP, Stewart MA. Distinct contributions of conduct and oppositional defiant symptoms to adult antisocial behavior: evidence from an adoption study. Archives of General Psychiatry. 1998;55:821–829. doi: 10.1001/archpsyc.55.9.821. [DOI] [PubMed] [Google Scholar]
- Leadbeater B, Thompson K, Gruppuso V. Co-occurring Trajectories of Symptoms of Anxiety, Depression, and Oppositional Defiance From Adolescence to Young Adulthood. Journal of Clinical Child & Adolescent Psychology. 2012;41:719–730. doi: 10.1080/15374416.2012.694608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Frick PJ, McBurnett K. Findings on disruptive behavior disorders from the first decade of the Developmental Trends Study. Clinical Child & Family Psychology Revivew. 2000;3:37–60. doi: 10.1023/a:1009567419190. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Stouthamer-Loeber M. Optimal informants on childhood disruptive behaviors. Development and Psychopathology. 1989;1:317–337. [Google Scholar]
- Martel MM, von Eye A, Nigg J. Developmental differences in structure of attention-deficit/hyperactivity disorder (ADHD) between childhood and adulthood. International Journal of Behavioral Development. 2012;36(4):279–292. doi: 10.1177/0165025412444077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: developmental epidemiology. J Child Psychol Psychiatry. 2004;45(3):609–621. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- Munkvold LH, Lundervold AJ, Manger T. Oppositional defiant disorder-gender differences in co-occurring symptoms of mental health problems in a general population of children. Journal of Abnormal Child Psychology. 2011;39(4):577–587. doi: 10.1007/s10802-011-9486-6. [DOI] [PubMed] [Google Scholar]
- Offord DR, Boyle MH, Racine YA, Fleming JE, Cadman DT, Blum HM, et al. Outcome, prognosis, and risk in a longitudinal follow-up study. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:916–923. doi: 10.1097/00004583-199209000-00021. [DOI] [PubMed] [Google Scholar]
- Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 2010;119:726–738. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe R, Maughan B, Pickles A, Costello EJ, Angold A. The relationship between DSM-IV oppositional defiant disorder and conduct disorder: findings from the Great Smoky Mountains Study. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2002;43:365–373. doi: 10.1111/1469-7610.00027. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, BoneyMcCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2) - Development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. American Journal of Psychiatry. 2009;166(9):1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng W-L, Kawabata Y, Gau SS-F. Social adjustment among Taiwanese children with symptoms of ADHD, ODD, and ADHD comorbid with ODD. Child Psychiatry and Human Development. 2011;42:134–151. doi: 10.1007/s10578-010-0204-3. [DOI] [PubMed] [Google Scholar]
- van Lier PAC, Koot HM. Developmental cascades of peer relations and symptoms of externalizing and internalizing problems from kindergarten to fourth-grade elementary school. Development and Psychopathology. 2010;22(3):569–582. doi: 10.1017/S0954579410000283. [DOI] [PubMed] [Google Scholar]